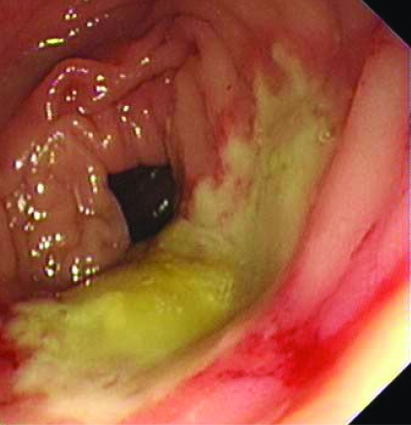
A 76-year-old lady was seen with angina; subsequent angiography showed severe left anterior descending artery (LAD) disease. Nicorandil 10 mg twice daily was added in April 2006 and increased in June to 20 mg twice daily. While awaiting percutaneous coronary intervention (PCI) to her LAD, she developed iron deficiency anaemia, weight loss and severe diarrhoea. PCI was deferred because of her physical deterioration and weight loss. Colonoscopy revealed extensive ulceration of the transverse and right colon (panel A). Histology was inconclusive but excluded Crohn’s disease and ischaemic colitis. A drug reaction was suspected and nicorandil discontinued in September 2006.
Panel A.
She was readmitted in December 2006 due to continuing weight loss. Whilst an inpatient she suffered a troponin-positive acute coronary syndrome (ACS) but PCI was felt to be too risky in face of iron deficiency anaemia due to the colitis.
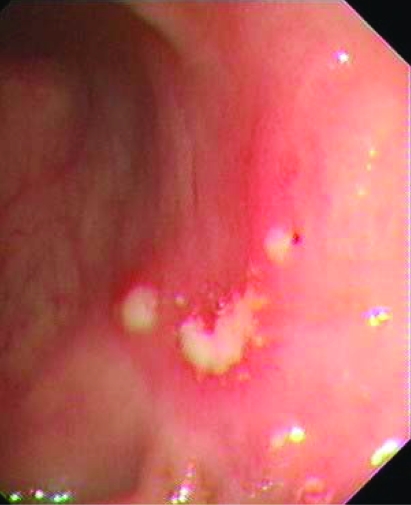
Four months later her weight had improved and diarrhoea settled, but she continued to experience frequent angina. In view of her previous blood loss we repeated a colonoscopy to ensure that dual antiplatelet therapy was not going to result in lower GI haemorrhage. Colonoscopy showed marked improvement (panel B), and she underwent successful angioplasty in June 2007.
Panel B.
Nicorandil-induced intestinal ulceration is becoming increasingly recognised. The pathogenesis is unknown. This rare and potentially fatal side effect usually occurs with higher doses and can take up to 3 months, and sometimes longer, to heal after drug withdrawal. Cardiologists need to be aware of this important side effect, which can occur without the more commonly recognised oral and anal ulceration.
Acknowledgments
This article has been adapted from Brown R, Lee A, Welfare M. Nicorandil-induced colonic ulceration Heart 2008;94:678
Footnotes
Competing interests: None.