Lead Summary
Some athletes may be more susceptible to at-risk knee positions during sports activities, but the underlying causes are not clearly defined. This manuscripts synthesizes in vivo, in vitro and in-silica (computer simulated) data to delineate likely risk factors to the mechanism(s) of non-contact ACL injuries. From these identified risk factors, we will discuss newly developed real-time screening techniques that can be used in training sessions to identify modifiable risk factors. Techniques provided will target and correct altered mechanics which may reduce or eliminate risk factors and aid in the prevention of non-contact ACL injuries in high risk athletes.
Keywords: Anterior cruciate ligament injury, knee, drop vertical jump landing, young athletes
Determination of the Potential Risk Factors for ACL Injury
Most ACL injuries in female sports occur during a non-contact episode, typically during deceleration, lateral pivoting, or landing tasks that are associated with high loads on the knee joint (Figure 1 A).(7, 59) Sports maneuvers may lead to high external knee loads in both sexes. Why these tasks result in greater incidence of ACL injury in females has, until recently, remained unclear. Three major etiological theories have been proposed to explain the gender disparity observed in ACL injury rates: anatomic, hormonal and neuromuscular.(20, 47) A number of studies of ACL injury risk factors have focused on anatomic or anthropometric measures such as thigh length, (5) joint laxity(56) and femoral notch width.(66) However, static anatomic measures such as Q-angle often do not appear to correlate to the mechanics associated with dynamic injury mechanism(48, 51) Hormonal factors, particularly those associated with the follicular and ovulatory phases of the menstrual cycle have also been linked to ACL injury risk.(1, 20, 27, 68, 75, 76, 79) However, the precise means by which they may contribute to ACL injury risk and the extent to which these hormonal factors can be modified remains unclear.(10)
Figure 1.
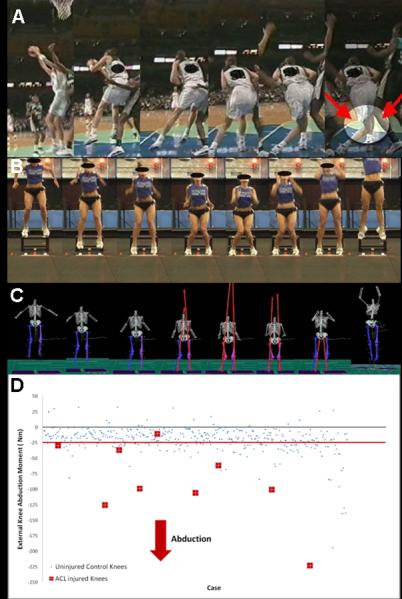
A. ACL injury mechanism with high knee abduction angle that is related to high LOAD.
B. Videographic depiction of athlete with kinematic pattern that is likely to demonstrate high LOAD.
C. Motion analysis depiction of athlete with kinematic and kinetic pattern indicative of high LOAD.
D. Scatterplot of data comparing those who went onto ACL injury to uninjured control subject. Red-line indicates established cut-point which provided maximum sensitivity and specificity to predict ACL injured status. Athletes who demonstrate LOAD beyond (negative values indicate increased LOAD) red line may be at “high risk” for ACL injury during competition (figure 1A).
Determination of Potential Modifiable Risk Factors for ACL Injury in Females
The study of modifiable risk factors has focused on the working hypothesis that ACL injury risks are related to measurable deficits in neuromuscular control in female athletes.(11, 13, 25) Neuromuscular control deficits are defined as muscle strength, power or activation patterns that lead to increased knee joint and ACL loads.(47) Female athletes demonstrate neuromuscular control deficits that increase lower extremity joint loads during sports activities.(26)
One neuromuscular deficit, which is operationally termed “ligament dominance,” can be defined as an imbalance between the neuromuscular and ligamentous control of dynamic knee joint stability.(47) This control imbalance is demonstrated by an inability to control lower extremity frontal plane motion during landing and cutting. A second modifiable neuromuscular control deficit often observed in female athletes, which is termed “quadriceps dominance,” can be defined as an imbalance between knee extensor and flexor strength, recruitment and coordination.(47) A third neuromuscular control deficit, often observed in female athletes is “leg dominance,” which can be defined as an imbalance between the two lower extremities in strength, coordination and control.(47) The fourth and final neuromuscular control deficit, often observed in female athletes is “truck dominance `core' dysfunction,” which can be defined as an imbalance between the inertial demands of the trunk and control and coordination to resist it.
During landing, pivoting, or deceleration, the motion of the female athlete's trunk is often excessive and directed, to a greater extent, by that body segment's inertia, than by the athlete's core muscle function. This decreased core control and ability to dissipate force result in excessive trunk motion, especially in the frontal plane, as well as, high ground reaction forces and knee joint abduction torques (knee load).(23)
These four potential neuromuscular control deficits, operationally defined above, are postulated to be important contributors to knee and ACL injury incidence in female athletes.(25, 44, 63, 78) ACL injury likely occurs under conditions of high dynamic loading of the knee joint, when active muscular restraints do not compensate for and dampen joint loads adequately (Figure 1A).(6) Decreased neuromuscular control of the joint may place stress on the passive ligamentous structures that may exceed their strength limit and potentially lead to mechanical failure.(35, 40) External abduction moment (LOAD) is the lab-based kinetic measure that is predictive of future injury and likely contributes to the stress on an ACL during injury (Figure 1C and Figure 1D).(25, 65) The term “valgus” is used to describe the video evidenced mechanism of injury (Figure 1A) and is visually associated with a knock-kneed position during dynamic tasks (Figure 1B).
Neuromuscular control of high load movements is required to maintain dynamic knee stability during landing and pivoting.(3, 35) Deficits in the active neuromuscular control system likely affect dynamic knee stability and possibly increase the risk of an ACL injury. Methods to identify neuromuscular control deficits during tasks related to ACL injury mechanisms, such as landing, cutting and decelerating, may offer the greatest potential for the development and application of neuromuscular screening interventions targeted to high risk populations.(7, 59)
The authors currently employ a two-pronged approach to the prevention of ACL injuries in young female athletes. We incorporate both risk screening and dynamic neuromuscular training as dual interventions to prevent these devastating injuries. Myer et al. demonstrated that those athletes that subject their knees to higher joint loads benefit to a greater extent from our dynamic neuromuscular training protocols than those who do not.(46) Therefore, we first screen athletes for high risk status and then intervene with neuromuscular training designed to ameliorate those specific neuromuscular imbalances that those specific athletes demonstrate. This dual approach likely results in greater efficacy of both avenues of intervention.
Potential Modifiable Risk Factors Associated with Dynamic Movements
Hewett et al.(26) tested the hypothesis that insufficient neuromuscular control of lower limb biomechanics, particularly the knee joint, leads to high risk patterns in female athletes during execution of common, albeit potentially hazardous, movements. The results of this study demonstrated that peak landing forces were significantly predicted by knee abduction torques (LOAD) at the knee in females, that females developed decreased relative knee flexor torque during landing compared to males and that females had greater side to side differences in normalized hamstrings peak torque compared to males.
Ford et al.(11) reported similar gender differences during the performance of a drop vertical jump (Figure 1B). This study determined that female athletes landed with a greater maximum valgus knee angle and greater total valgus knee motion than male athletes (Figure 1C). Female athletes also demonstrated significant differences between their dominant and non-dominant side in maximum valgus knee angle. These differences in valgus measures (ligament dominance) and limb-to- limb asymmetries (leg dominance) reflect neuromuscular deficits that may be indicative of decreased dynamic knee joint control in female athletes.(11)
Subsequent studies systematically evaluated neuromuscular control at the hip in female athletes.(22, 80) The evidence from multiple, potentially high-risk, movements indicated that variables at the hip contributed to dynamic valgus. In addition, electromyographic (EMG) data demonstrated female to male differences in firing patterns of the hip musculature.(80) The purpose of these studies was to identify sex differences in hip motion, kinetics and muscle firing patterns during single leg agility and landing maneuvers. It was hypothesized that female athletes would display increased hip adduction angles and external adduction moments during this multi-component dynamic maneuver that may contribute to lower extremity valgus.
The results demonstrated that female athletes had greater hip adduction angles and torques than males during multi-directional single-leg landing. These differences were limited to the frontal plane and were not observed in the sagittal plane. EMG patterns showed increased quadriceps and decreased gluteal firing in females.(80) Another study examined sex differences during single leg landings from either a medial or lateral direction.(14) In addition to greater knee abduction angles, female athletes also exhibited increased hip frontal plane excursion compared to males during both types of landings.(14) The increased hip adduction (hip varus) motion seen in the frontal plane during athletic activities likely contributes to the dynamic valgus knee position that may place the athlete at increased risk of ACL injury (Figure 1D).(14, 22)
Proliferation of ACL Injury Risk Factors during Adolescent Growth
Males demonstrate power, strength and coordination increases with increasing chronological age that correlate to maturational stage, while females show significantly smaller changes throughout puberty.(4, 38) Correlations between height, weight and neuromuscular performance observed in males are absent in pubescent females. For example, vertical jump height (a measure of whole-body power) increases steadily in males during puberty, but not in females.(31, 38, 64) Musculoskeletal growth during puberty, in the absence of corresponding neuromuscular adaptation, may facilitate the development of certain intrinsic ACL injury risk factors.(16, 24) These intrinsic risk factors, if not addressed at the proper time, may continue through adolescence into maturity and predispose athletes to ACL injuries.
Neuromuscular training programs have been successful at reducing measures of knee abduction.(26, 46, 54, 55) A comprehensive review of ACL injury prevention programs indicates that neuromuscular training appears to decrease ACL injury rates in female athletes.(21) These programs typically incorporate plyometric training and technique analysis. Ongoing studies show that knee abduction measures may be useful for the identification of those females who are at increased risk of ACL injury.(25) In a recent longitudinal study, Ford et al. (17) identified that during a landing task pubertal females have an increased change in knee abduction motion during a year of adolescent growth. In addition, important reported risk factors of knee abduction motion and torque were significantly greater across consecutive years in young post-pubertal female athletes compared to males. (17)
Figure 2A, B, C presents a representative subject whose combination of decreased tibia length and mass prior to her rapid growth spurt diminish risk to demonstrate high knee LOAD landing mechanics. Conversely, Figure 2D, E, F provides an example of representative subject whose combination of increased tibia length and mass associated with her rapid growth contribute to her increased risk to demonstrate high knee LOAD landing mechanics when using the clinic-based ACL injury risk prediction algorithm.
Figure 2.
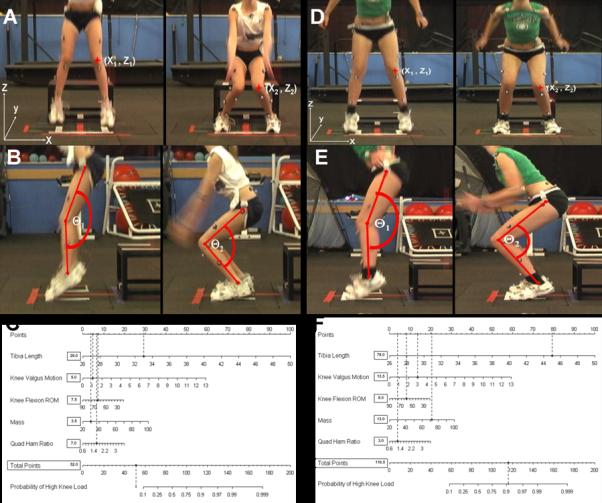
A. Representative subject whose combination of decreased tibia length and mass prior to her rapid growth spurt diminish risk to demonstrate high LOAD landing mechanics. Knee valgus motion during the drop vertical jump is calculated as the displacement measure between the two marked knee alignment in the X plane measured at the frame prior to initial contact and the frame with maximum knee flexion (X2− X1).
B. Knee flexion range of ROM during the drop vertical jump is calculated as the difference in knee flexion angle between initial contact and maximum knee flexion positions (ϴ1−ϴ2).
C. Completed nomogram for the representative subject (Tibia length: 32.5 cm; Knee valgus motion: 4.2 cm; Knee flexion ROM: 74.1°; mass: 30.7 kg; QuadHam: 1.64). Based on her demonstrated measurements this subject would have a 12% (62.5 points) percent chance to demonstrate high LOAD during the drop vertical jump. Her actual LOAD measure for the presented drop vertical jump that was quantified simultaneously with 3D motion analysis was 13.4 Nm of knee abduction load.
D. Example of representative subject whose combination of increased tibia length and mass associated with her rapid growth contribute to her increased risk to demonstrate high LOAD landing mechanics when using the clinic-based ACL injury risk prediction algorithm. Knee valgus motion during the drop vertical jump is calculated (X2− X1).
E. Knee flexion range of ROM during the drop vertical jump is calculated (ϴ1−ϴ2).
F. Completed nomogram for the representative subject (Tibia length: 45 cm; Knee valgus motion: 3.0 cm; Knee flexion ROM: 60.0°; mass: 71 kg; QuadHam: 1.19). Based on her demonstrated measurements this subject would have a 91% (116.5 points) percent chance to demonstrate high LOAD during the drop vertical jump. Her actual LOAD measure for the presented drop vertical jump that was quantified simultaneously with 3D motion analysis was 48.5 Nm of knee abduction load.
Determination the timing of athlete specific maturation
Somatic maturational assessments are traditionally the best way to identify rapid adolescent growth.(38) The Khamis-Roche method of estimated adult stature was developed from the Fels Longitudinal Study that collected data on families residing in southwestern Ohio.(32) The subject's stature, mass, midparental stature and age was utilized to develop regression equations for boys and girls. This equation can be used to estimate the current percentage of height compared to their final estimated height.
Early puberty may be an appropriate time during maturation to institute intervention programs that aim to control knee abduction motion and torque as well to induce a neuromuscular spurt through targeted neuromuscular training. The pubertal female group in our recent study was approximately 12 years old and estimated to be at 88 percent of adult stature (17). Therefore, training programs may be most beneficial prior to timing when girls are growing the fastest during adolescence (peak height velocity) which is near 92 percent of adult stature.
Screening for High Risk Athletes
Laboratory based screening tools demonstrate that altered neuromuscular strategies or decreased neuromuscular control during the execution of sports movements, as evidenced by abnormal lower limb joint mechanics (motions and loads), may underlie the increased risk of ACL injury in female athletes.(9, 11, 15, 25, 41, 54) Prospective measures of external knee abduction moment during landing predict non-contact ACL injury risk in young female athletes (Figure 1A–D).(25)
Calculation of knee injury risk factors such as knee abduction moment, through inverse dynamics, requires complex laboratory-based three-dimensional kinematic and kinetic measurement techniques. However, a recent report has isolated biomechanical measures that contribute to nearly 80% of the measured variance in knee abduction moment during landing.(51) These biomechanical predictors of knee abduction moment, which include increased knee abduction angle, increased relative quadriceps recruitment and decreased knee flexion range of motion (ROM), concomitant with increased tibia length and mass normalized to body height that accompanies growth, are also measurements that have all been related to increased risk of ACL injury in previous prospective and retrospective epidemiological reports.(7, 25, 60, 70) Unfortunately, expensive biomechanical laboratories, with the costly and labor intensive measurement tools to test individual athletes, are required for these measurements. This restricts the potential to perform athletes' risk assessments on a large scale, in particular limiting the potential to target high injury risk athletes with the appropriate intervention strategies.
To achieve the objective of reduction of non-contact ACL injury risk in female athletes, identification of those athletes who preferentially demonstrate high knee abduction moment landing mechanics appears salient. Therefore, a field-based assessment algorithm was systematically developed and validated that aimed to improve the potential to identify and target injury prevention training to female athletes with increased knee abduction moment.(50, 52, 53) The validated field-based assessment algorithm delineated five biomechanical factors that could be captured in clinic and field settings that combined to identify high knee abduction moment during landing with high accuracy.(50, 52, 53) This clinic-based assessment tool can be administered in a clinic or field setting, is validated by the highly accurate laboratory-based assessment, and can help to facilitate screening for ACL injury risk on a more widespread basis (Figure 2).
While the clinic-based assessment tool is valuable to identify athletes who should be targeted with neuromuscular training, it was imperative to develop a “Coach Friendly” plyometric exercise landing assessment and technique training tool to target high risk ACL injury mechanisms. For this reason the tuck jump assessment tool was developed to aid coach's decision making during training sessions (Figure 3).(49)
Figure 3.

TJA assessment tool can be utilized to score deficits during a jumping and landing sequence movement. To perform the tuck jump assessment the athlete is instructed to start in the athletic position with her feet shoulder-width apart (on line marked 35 cm apart). They are instructed to initiate the jump with a slight crouch downward while they extend their arms behind her. They then swing their arms forward as she simultaneously jumps straight up and pulls her knees up as high as possible. At the highest point of the jump the athlete is instructed to pull her thighs parallel to the ground. When landing, the athlete should immediately begin the next tuck jump. Encourage the athlete to land softly, using a toe to mid-foot rocker landing and land in the same footprint with each jump. The athlete is instructed to perform the tuck jump exercise for 10 seconds and should be instructed to not continue this jump if they demonstrate a sharp decline in technique during the allotted time frame. Figure reproduced from Myer, G. D., K. R. Ford, et al. (2008). “Tuck Jump Assessment for Reducing Anterior Cruciate Ligament Injury Risk.“ Athletic Therapy Today 13(5): 39–44 with permission from the editor.
Real Time Field Assessment and Training Tool
The tuck jump exercise may be useful to the strength coach for the identification of lower extremity technical flaws during a plyometric activity (Figure 4).(47) The tuck jump requires a high effort level from the athlete. Because of this, the strength coach may readily identify potential deficits (Figure 3), especially during the first few repetitions. In addition, the tuck jump exercise may be used to assess improvement in lower extremity biomechanics as the athlete progresses through their training.(47, 49)
Figure 4.
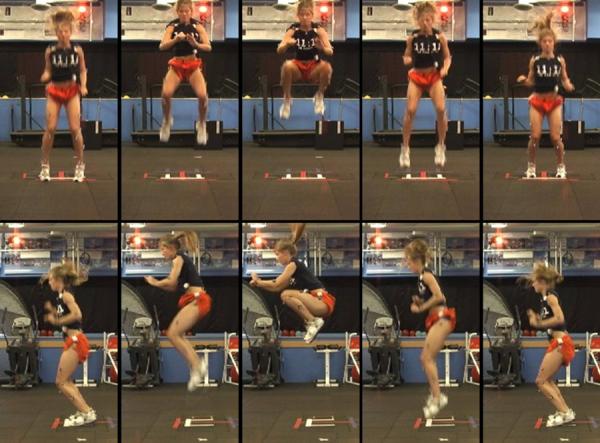
Desired technical performance of the tuck jump exercise.
Figure 3 provides the “coach friendly” landing technique assessment tool strength coaches may use to monitor an athlete's performance of the tuck jump before, during and after training. Specifically, the athlete performs repeated tuck jumps for 10 seconds, which allows the coach to visually grade the outlined criteria. To further improve accuracy of the assessment, a standard 2D camera in the frontal and sagittal planes may be utilized to assist the coach. The athlete's techniques (Figure 3) are subjectively rated as either having an apparent deficit (checked) or not. The deficits are then tallied for the final assessment score. Indicators of flawed techniques should be noted for each athlete and should be the focus of feedback during subsequent training sessions. The athlete's baseline performance can be compared to repeated assessments performed at the midpoint and conclusion of training protocols, to objectively track improvement with jumping and landing technique (Figure 3).
Ligament Dominance Criteria of the Tuck Jump Assessment
For ease of presentation, criteria assessed using the tuck jump tool can be grouped into modifiable risk factor categories (Figure 5). As mentioned previously, ligament dominance is defined as an imbalance between the neuromuscular and ligamentous control of dynamic knee joint stability.(47) This imbalance in control of dynamic knee joint stability is demonstrated by an inability to control lower extremity frontal plane motion during landing and cutting. External abduction moment (LOAD) is the lab-based kinetic measure that is predictive of future injury and likely contributes to the stress on an ACL during injury (Figure 1 C and Figure 1D).(25, 65) The term “valgus” is used to describe the video evidenced mechanism of injury (Figure 1A) and is visually associated with a knock-kneed position during dynamic tasks (Figure 1B). Figure 6 presents a “ligament dominant” athlete who lacks sufficient frontal plane control of her lower extremity during performance of the tuck jump. Figure 7 presents secondary assessment of ligament dominance with the criteria that assesses if foot placement is maintained shoulder width apart during landing. This athlete's reduced ligament dominant landing mechanics may be driven from lack of frontal plane control at the hip which may be improved with targeted training for the trunk and hip.(42, 43, 47, 55, 62)
Figure 5.
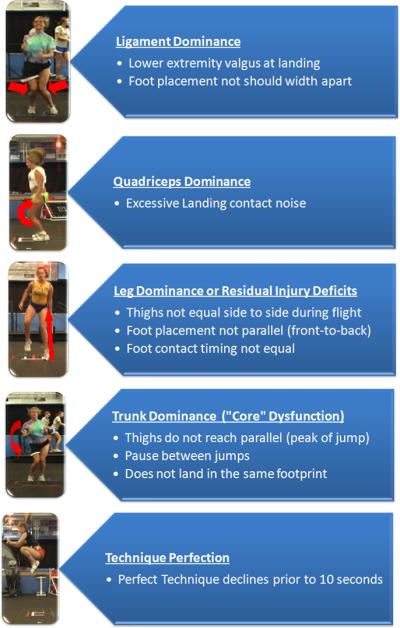
Tuck jump criteria grouped by modifiable risk factor categorizations.
Figure 6.

Lower extremity valgus at landing. This is indicated by the athlete displaying a “knock-kneed” position while in contact with the ground.
Figure 7.

Foot placement not shoulder width apart. This deficit can be manifested with feet either closer together or farther apart.
Quadriceps Dominance Criteria of the Tuck Jump Assessment
A second modifiable neuromuscular control deficit often observed in female athletes, which was termed “quadriceps dominance,” is defined as an imbalance between knee extensor and flexor strength, recruitment and coordination.(47) Landing with the knee at nearly full extension is a commonly associated mechanism of ACL injury.(7) Decreased hamstrings strength relative to the quadriceps is implicated as a potential mechanism for increased lower extremity injuries.(12, 18, 33, 44, 69) and potentially ACL injury risk in female athletes.(47) Joint stability through hamstrings and quadriceps co-contraction may be necessary when the joint experiences high quadriceps activation or when the passive structures are compromised.(67, 73) Withrow and colleagues reported that increased hamstrings force during the flexion phase of simulated jump landings greatly decreased relative strain on the ACL.(74)
Another proposed theory related to neuromuscular imbalances and increased ACL injury risk in females is the relatively low knee flexor to extensor recruitment that may be reflective of a closed chain dynamic hamstrings/quadriceps peak torque output.(26, 39) For example, hamstrings activation can decrease the load on the passive restraints of the knee,(37) increase the knee joint compression force and stabilize the knee from external varus/valgus load.(36) Hewett et al. reported that males demonstrated knee flexor moments, measured using inverse dynamics, that were three-fold higher than females during deceleration from a landing.(26) This group of females also demonstrated decreased isokinetic H/Q ratio and increased knee abduction (valgus) moments compared to male subjects. The increased knee valgus moment significantly correlated to the peak impact forces during the maneuver and is purported to increase ACL injury risk in female athletes.(25, 26) Ford and colleagues reported that females showed an absence of matched increased hamstrings muscle activation relative to quadriceps and overall low amplitude during the landing phase of a jump.(12)
This tendency of female athletes to preferentially activate the quadriceps relative to the hamstrings during high demand activities may limit their abilities to maintain dynamic knee control during high risk maneuvers. Athletes that demonstrate quadriceps dominance may increase their risk of ACL injury when they cut and land with low knee flexion angles. An athlete who lands with small knee flexion angles and flat foot position demonstrate characteristics of a quadriceps dominant athlete (figure 8) and will likely demonstrate excessive landing contact noise. This criterion assessed using the tuck jump tool can be grouped into quadriceps dominance modifiable risk factor category (Figure 5) and if identified with the tuck jump assessment should be targeted with posterior chain and deep knee flexion exercises.(44, 45, 47, 54, 55)
Figure 8.

Excessive Landing contact noise. This is typically displayed by the athlete through landing with flat feet and is typically accompanied by a lack of knee and hip flexion during the stance phase.
Leg Dominance/Residual Injury Deficits Criteria of the Tuck Jump Assessment
A third neuromuscular control deficit, frequently observed in female athletes is “leg dominance,” which is defined as an imbalance between the two lower extremities in strength, coordination and control.(47) Coaches should be cognizant during their risk assessment that side-to-side imbalances in neuromuscular strength, flexibility and coordination can be important predictors of increased injury risk.(2, 25, 33) Specific to ACL injury risk in female athletes, leg-to-leg differences in dynamic valgus measures were observed in injured, but not uninjured females. Importantly, side-to-side differences in knee LOAD were 6.4× greater in ACL-injured versus the uninjured females. Female athletes tend to demonstrate side-to-side differences in visually evident maximum knee valgus angle during a box drop vertical jump.(11) In addition, female athletes often demonstrate leg-leg deficits following injury that increase their risk of subsequent injury.(61, 63) Leg dominance or residual injury deficits may be evident in the grouped tuck jump criteria including: thighs not equal side to side during flight (figure 9), foot placement not parallel (front-to-back) (figure 10), foot contact timing not equal (figure 11). Athletes identified with leg to leg deficit should be targeted with integrated training that combines both plyometric and dynamic stabilization to improve leg-to-leg symmetry during dynamic tasks.(45, 54)
Figure 9.

Thighs not equal side to side during flight. Side dominance often is visible when an athlete has one thigh that does not achieve the same height as their contralateral thigh.
Figure 10.

Foot placement not parallel (front-to-back). Often an athlete will “drop” one foot behind the other while on the ground to help minimize forces on an injured or weaker limb.
Figure 11.

Foot contact timing not equal. Similar to not placing the feel parallel, the athlete will occasionally change the timing of the foot contacts to protect an injured or weaker limb.
“Core” Dysfunction Dominance Criteria of the Tuck Jump Assessment
The fourth neuromuscular control deficit, often observed in female athletes is “core” dysfunction dominance, which may be defined as an imbalance between the inertial demands of the trunk and core control and coordination to resist it. We have developed a concept of trunk and lower extremity function that identifies the body's “core” as a critical modulator of lower extremity alignments and loads during dynamic tasks.(43) The trunk and hip stabilizers may pre-activate to counterbalance trunk motion and regulate lower extremity postures.(28, 29, 71) Reduced pre-activation of the trunk and hip stabilizers may allow increased lateral trunk positions that can incite knee abduction loads.(72)
Decreased “core stability” and muscular synergism of the trunk and hip stabilizers may affect performance in power activities and may increase the incidence of injury secondary to lack of control of the center of mass, especially in female athletes.(30, 61, 63, 77) Zazulak et al. reported that factors related to core stability predicted risk of knee injuries in female athletes but not in male athletes.(78) Thus, the current evidence indicates that compromised function of the trunk and hip stabilizers, as they relate to “core” neuromuscular control, may underlie the mechanisms of increased ACL injury risk in female athletes.(25, 34, 59, 78)
Core dysfunction imbalance may be evident in the athlete's tuck jump criteria including thighs do not reach parallel (peak of jump) (figure 12), pause between jumps, and the athlete does not land in the same footprint (figure 13). Athletes identified with these deficits should be targeted with trunk and hip training to improve “core” control.(42, 43)
Figure 12.

Thighs do not reach parallel (peak of jump). This deficit is typically a product of the athlete's inability to create enough power to achieve a height at which the legs can become properly tucked.
Figure 13.

Does not land in the same footprint. Many times an athlete will tend to float around the jumping area due to a lack of full body or “core” control. When this deficit is present, the coach should be careful in determining the cause so that training can be properly applied.
Technique Perfection Criteria of the Tuck Jump Assessment
The tuck jump assessment tool can be utilized to improve high risk techniques during an exercise that requires a high effort level from the athlete. As suggested earlier, an athlete may place most of his or her cognitive efforts solely on the performance of this difficult jump and demonstrate many technical flaws that are indicative of increased risk for injury. However, if she can improve her neuromuscular control and biomechanics during this difficult jump and maintain control during the entire jump-landing sequence, she may gain dynamic neuromuscular control of the lower extremity and create a learned skill that can be transferred to competitive play (Figure 4). We recommend that athletes who do not improve their scores, or who demonstrate six or more flawed techniques, should be targeted for further technique training. These data indicate that the tuck jump assessment is best utilized for a single coach to re-assess athletes to determine changes in technical performance of the tuck jump exercise.(57, 58)
Effect of Training on Tuck Jump Assessment Criteria
Cumulatively, research indicates that ACL intervention training can be utilized to reduce measured deficits during the tuck jump assessment and may help prevent risk of ACL injury. A pilot study was conducted to test the effects of pre-season and in-season neuromuscular training on the tuck jump assessment scores to determine if both training periods were vital to a training protocol.(8) The data from this study indicate that preseason neuromuscular training should be considered paramount within the yearly strength and conditioning program to help minimize the risk factors associated with ACL injury.
The tuck jump assessment allows a coach or clinician to evaluate an athlete's risk of injury as well as identify specific deficiencies. By using this test throughout the yearly training cycle, overall progress can be monitored and training can be more thoroughly directed. The results also indicate a potential dose-response to the neuromuscular training targeted to prevent ACL injury training. Preliminary results indicate that additional training throughout the competitive season has added benefits in terms of reducing risk of ACL injury based on improvements to the athlete's tuck jump assessment score. Future research is warranted to determine the relationship of reduced deficits gained from utilization of the presented techniques with actual reduction of injury in athletes treated with targeted training.
CONCLUSIONS
To achieve the objective of reduction of non-contact ACL injury risk in female athletes, identification and treatment of those who preferentially demonstrate “high risk” landing mechanics appears salient. The provided tuck jump assessment tool provides an integrated approach to guide targeted dynamic neuromuscular analysis training to specifically address and correct neuromuscular deficits that increase high LOAD risk within the algorithm. Theoretically, through identification of female athletes at greater risk for ACL injury, prevention strategies to reduce an ACL injury could be substantially improved. Current non-targeted neuromuscular training programs require application to 89 female athletes to prevent one ACL injury.(19)
Female athletes who demonstrate “high risk” landing mechanics are at increased risk for ACL injury and are more likely to benefit from neuromuscular training targeted to these risk factors.(46) Utilization of the developed field-based assessment and training tool may guide the application of appropriate interventions that will have greater potential to reduce their injury risk. Targeted correction of high risk factors for injury is important for both optimal biomechanics of athletic movements that maximize sport performance and ultimately the reduction of knee ligament injury incidence in female athletes.
ACKNOWLEDGEMENTS
The authors would like to acknowledge funding support from National Institutes of Health/NIAMS Grants R01-AR049735, R01-AR05563 and R01-AR056259. The authors would like to thank Boone County Kentucky, School District, especially School Superintendent Randy Poe, for participation in this study. We would also like to thank Mike Blevins, Ed Massey, Dr. Brian Blavatt and the athletes of Boone County public school district for their participation in this study. The authors would also like to acknowledge the Cincinnati Children's Sports Medicine Biodynamics Center Team who have contributed both physically and intellectually to the presented research outcomes.
The Cincinnati Children's Hospital Medical Center and Rocky Mountain University of Health Professions Institutional Review Boards approved this study.
Biography
Gregory D. Myer, PhD, CSCS is Co-Director of the Human Performance Laboratory and holds a primary appointment as a Research Instructor of Pediatrics within Sports Medicine at Cincinnati Children's Hospital Medical Center.
Jensen L. Brent, CSCS is a Biomechanist in the Sports Medicine Biodynamics Center Human Performance Laboratory at Cincinnati Children's Hospital Medical Center. Mr. Brent is also the Head Strength and Conditioning Coach for the Cincinnati Kelts Rugby Football Club.
Kevin R. Ford, PhD, FACSM is Co-Director of the Human Performance Laboratory and holds a primary appointment as an Assistant Professor within Sports Medicine at Cincinnati Children's Hospital Medical Center.
Timothy E. Hewett PhD, FACSM is Professor and Director of Research at Ohio State University Sports Medicine and Professor of Pediatrics and Director of the Sports Medicine Biodynamics Center at Cincinnati Children's Hospital Medical Center.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Arendt EA, Bershadsky B, Agel J. Periodicity of noncontact anterior cruciate ligament injuries during the menstrual cycle. J Gend Specif Med. 2002;5:19–26. [PubMed] [Google Scholar]
- 2.Baumhauer J, Alosa D, Renstrom A, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sport Med. 1995;23:564–570. doi: 10.1177/036354659502300508. [DOI] [PubMed] [Google Scholar]
- 3.Besier TF, Lloyd DG, Cochrane JL, Ackland TR. External loading of the knee joint during running and cutting maneuvers. Med Sci Sports Exerc. 2001;33:1168–75. doi: 10.1097/00005768-200107000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Beunen G, Malina RM. Growth and physical performance relative to the timing of the adolescent spurt. Exerc Sport Sci Rev. 1988;16:503–40. [PubMed] [Google Scholar]
- 5.Beynnon B, Slauterbeck J, Padua D, Hewett TE. Update on ACL risk factors and prevention strategies in the female athlete. National Athletic Trainers' Association 52nd Annual Meeting and clinical Symposia.2001. pp. 15–18. [Google Scholar]
- 6.Beynnon BD, Fleming BC. Anterior cruciate ligament strain in-vivo: a review of previous work. J Biomech. 1998;31:519–25. doi: 10.1016/s0021-9290(98)00044-x. [DOI] [PubMed] [Google Scholar]
- 7.Boden BP, Dean GS, Feagin JA, Garrett WE. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 8.Brent JL, Klugman MA, Myer GD, Hewett TE. The Effects of Pre-Season and In-Season Neuromuscular Training on the Tuck Jump Assessment: a Test Used to Identify Risk of ACL Injury in Female Athletes. National Strength and Conditioning Association Annual Meeting; Orlando, Florida. 2010. [Google Scholar]
- 9.Chappell JD, Yu B, Kirkendall DT, Garrett WE. A comparison of knee kinetics between male and female recreational athletes in stop-jump tasks. Am J Sports Med. 2002;30:261–7. doi: 10.1177/03635465020300021901. [DOI] [PubMed] [Google Scholar]
- 10.Chaudhari AM, Lindenfeld TN, Andriacchi TP, Hewett TE, Riccobene J, Myer GD, Noyes FR. Knee and hip loading patterns at different phases in the menstrual cycle: implications for the gender difference in anterior cruciate ligament injury rates. Am J Sports Med. 2007;35:793–800. doi: 10.1177/0363546506297537. [DOI] [PubMed] [Google Scholar]
- 11.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35:1745–50. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- 12.Ford KR, Myer GD, Schmitt LC, Van den Bogert AJ, Hewett TE. Effect of drop height on lower extremity biomechanical measures in female athletes. Medicine & Science in Sports & Exercise. 2008;40:S80. [Google Scholar]
- 13.Ford KR, Myer GD, Smith RL, Byrnes RN, Dopirak SE, Hewett TE. Use of an overhead goal alters vertical jump performance and biomechanics. Journal of Strength and Conditioning Research. 2005;19:394–9. doi: 10.1519/15834.1. [DOI] [PubMed] [Google Scholar]
- 14.Ford KR, Myer GD, Smith RL, Vianello RM, Seiwert SL, Hewett TE. A comparison of dynamic coronal plane excursion between matched male and female athletes when performing single leg landings. Clinical Biomechanics. 2006;21:33–40. doi: 10.1016/j.clinbiomech.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 15.Ford KR, Myer GD, Toms HE, Hewett TE. Gender differences in the kinematics of unanticipated cutting in young athletes. Medicine & Science in Sports. 2005;37:124–9. [PubMed] [Google Scholar]
- 16.Ford KR, Shapiro R, Myer GD, AJ VDB, Hewett TE. Longitudinal Sex Differences during Landing in Knee Abduction in Young Athletes. Med Sci Sports Exerc. 2010;42:1923–1931. doi: 10.1249/MSS.0b013e3181dc99b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ford KR, Shapiro R, Myer GD, van den Bogert AJ, Hewett TE. Longitudinal Sex Differences during Landing in Knee Abduction in Young Athletes. Med Sci Sports Exerc. 2010 doi: 10.1249/MSS.0b013e3181dc99b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ford KR, van den Bogert AJ, Myer GD, Shapiro R, Hewett TE. The effects of age and skill level on knee musculature co-contraction during functional activities: a systematic review. Br J Sports Med. 2008;42:561–6. doi: 10.1136/bjsm.2007.044883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grindstaff TL, Hammill RR, Tuzson AE, Hertel J. Neuromuscular control training programs and noncontact anterior cruciate ligament injury rates in female athletes: a numbers-needed-to-treat analysis. J Athl Train. 2006;41:450–6. [PMC free article] [PubMed] [Google Scholar]
- 20.Hewett TE. Neuromuscular and Hormonal Factors Associated With Knee Injuries in Female Athletes: Strategies for Intervention. Sports Medicine. 2000;29:313–327. doi: 10.2165/00007256-200029050-00003. [DOI] [PubMed] [Google Scholar]
- 21.Hewett TE, Ford KR, Myer GD. Anterior Cruciate Ligament Injuries in Female Athletes: Part 2, A Meta-analysis of Neuromuscular Interventions Aimed at Injury Prevention. Am J Sports Med. 2006;34:490–8. doi: 10.1177/0363546505282619. [DOI] [PubMed] [Google Scholar]
- 22.Hewett TE, Ford KR, Myer GD, Wanstrath K, Scheper M. Gender Differences in Hip Adduction Motion and Torque During a Single Leg Agility Maneuver. J Orthop Res. 2006;24:416–421. doi: 10.1002/jor.20056. [DOI] [PubMed] [Google Scholar]
- 23.Hewett TE, Johnson DL. ACL prevention programs: fact or fiction? Orthopedics. 2010;33:36–9. doi: 10.3928/01477447-20091124-19. [DOI] [PubMed] [Google Scholar]
- 24.Hewett TE, Myer GD, Ford KR. Decrease in neuromuscular control about the knee with maturation in female athletes. J Bone Joint Surg Am. 2004;86-A:1601–1608. doi: 10.2106/00004623-200408000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Hewett TE, Myer GD, Ford KR, Heidt RS, Jr., Colosimo AJ, McLean SG, van den Bogert AJ, Paterno MV, Succop P. Biomechanical Measures of Neuromuscular Control and Valgus Loading of the Knee Predict Anterior Cruciate Ligament Injury Risk in Female Athletes: A Prospective Study. Am J Sports Med. 2005;33:492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 26.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes. Decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24:765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 27.Hewett TE, Zazulak BT, Myer GD. Effects of the menstrual cycle on anterior cruciate ligament injury risk: a systematic review. Am J Sports Med. 2007;35:659–68. doi: 10.1177/0363546506295699. [DOI] [PubMed] [Google Scholar]
- 28.Hodges PW, Richardson CA. Contraction of the abdominal muscles associated with movement of the lower limb. Phys Ther. 1997;77:132–42. doi: 10.1093/ptj/77.2.132. discussion 142–4. [DOI] [PubMed] [Google Scholar]
- 29.Hodges PW, Richardson CA. Feedforward contraction of transversus abdominis is not influenced by the direction of arm movement. Exp Brain Res. 1997;114:362–70. doi: 10.1007/pl00005644. [DOI] [PubMed] [Google Scholar]
- 30.Ireland ML. The female ACL: why is it more prone to injury? Orthop Clin North Am. 2002;33:637–51. doi: 10.1016/s0030-5898(02)00028-7. [DOI] [PubMed] [Google Scholar]
- 31.Kellis E, Tsitskaris GK, Nikopoulou MD, Moiusikou KC. The evaluation of jumping ability of male and female basketball players according to their chronological age and major leagues. J Strength Cond Res. 1999;13:40–46. [Google Scholar]
- 32.Khamis HJ, Roche AF. Predicting adult stature without using skeletal age: the Khamis-Roche method. Pediatrics. 1994;94:504–7. [PubMed] [Google Scholar]
- 33.Knapik JJ, Bauman CL, Jones BH, Harris JM, Vaughan L. Preseason strength and flexibility imbalances associated with athletic injuries in female collegiate athletes. Am J Sports Med. 1991;19:76–81. doi: 10.1177/036354659101900113. [DOI] [PubMed] [Google Scholar]
- 34.Krosshaug T, Nakamae A, Boden BP, Engebretsen L, Smith G, Slauterbeck JR, Hewett TE, Bahr R. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35:359–67. doi: 10.1177/0363546506293899. [DOI] [PubMed] [Google Scholar]
- 35.Li G, Rudy TW, Sakane M, Kanamori A, Ma CB, Woo SL. The importance of quadriceps and hamstring muscle loading on knee kinematics and in-situ forces in the ACL. J Biomech. 1999;32:395–400. doi: 10.1016/s0021-9290(98)00181-x. [DOI] [PubMed] [Google Scholar]
- 36.Lloyd DG, Buchanan TS. Strategies of muscular support of varus and valgus isometric loads at the human knee. J Biomech. 2001;34:1257–67. doi: 10.1016/s0021-9290(01)00095-1. [DOI] [PubMed] [Google Scholar]
- 37.MacWilliams BA, Wilson DR, DesJardins JD, Romero J, Chao EY. Hamstrings cocontraction reduces internal rotation, anterior translation, and anterior cruciate ligament load in weight-bearing flexion. J Orthop Res. 1999;17:817–22. doi: 10.1002/jor.1100170605. [DOI] [PubMed] [Google Scholar]
- 38.Malina RM, Bouchard C. Growth, maturation, and physical activity. Human Kinetics; Champaign, Il: 1991. Timing and sequence of changes in growth, maturation, and performance during adolescence; pp. 267–272. [Google Scholar]
- 39.Malinzak RA, Colby SM, Kirkendall DT, Yu B, Garrett WE. A comparison of knee joint motion patterns between men and women in selected athletic tasks. Clin Biomech. 2001;16:438–45. doi: 10.1016/s0268-0033(01)00019-5. [DOI] [PubMed] [Google Scholar]
- 40.Markolf KL, Graff-Redford A, Amstutz HC. In vivo knee stability: A quantitative assessment using an instrumented clinical testing apparatus. J Bone Joint Surg. 1978;60A:664–674. [PubMed] [Google Scholar]
- 41.McLean SG, Lipfert SW, van den Bogert AJ. Effect of gender and defensive opponent on the biomechanics of sidestep cutting. Med Sci Sports Exerc. 2004;36:1008–16. doi: 10.1249/01.mss.0000128180.51443.83. [DOI] [PubMed] [Google Scholar]
- 42.Myer GD, Brent JL, Ford KR, Hewett TE. A pilot study to determine the effect of trunk and hip focused neuromuscular training on hip and knee isokinetic strength. Br J Sports Med. 2008;42:614–9. doi: 10.1136/bjsm.2007.046086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Myer GD, Chu DA, Brent JL, Hewett TE. Trunk and hip control neuromuscular training for the prevention of knee joint injury. Clin Sports Med. 2008;27:425–48. ix. doi: 10.1016/j.csm.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Myer GD, Ford KR, Barber Foss KD, Liu C, Nick TG, Hewett TE. The relationship of hamstrings and quadriceps strength to anterior cruciate ligament injury in female athletes. Clin J Sport Med. 2009;19:3–8. doi: 10.1097/JSM.0b013e318190bddb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Myer GD, Ford KR, Brent JL, Hewett TE. The Effects of Plyometric versus Dynamic Balance Training on Power, Balance and Landing Force in Female Athletes. J Strength Cond Res. 2006;20:345–353. doi: 10.1519/R-17955.1. [DOI] [PubMed] [Google Scholar]
- 46.Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8:1–7. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Myer GD, Ford KR, Hewett TE. Rationale and Clinical Techniques for Anterior Cruciate Ligament Injury Prevention Among Female Athletes. J Athl Train. 2004;39:352–364. [PMC free article] [PubMed] [Google Scholar]
- 48.Myer GD, Ford KR, Hewett TE. The effects of gender on quadriceps muscle activation strategies during a maneuver that mimics a high ACL injury risk position. J Electromyogr Kinesiol. 2005;15:181–89. doi: 10.1016/j.jelekin.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 49.Myer GD, Ford KR, Hewett TE. Tuck Jump Assessment for Reducing Anterior Cruciate Ligament Injury Risk. Athletic Therapy Today. 2008;13:39–44. doi: 10.1123/att.13.5.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Myer GD, Ford KR, Hewett TE. New method to identify athletes at high risk of ACL injury using clinic-based measurements and freeware computer analysis. Br J Sports Med. 2010 doi: 10.1136/bjsm.2010.072843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Biomechanics laboratory-based prediction algorithm to identify female athletes with high knee loads that increase risk of ACL injury. Br J Sports Med. 2010 doi: 10.1136/bjsm.2009.069351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Clinical correlates to laboratory measures for use in non-contact anterior cruciate ligament injury risk prediction algorithm. Clin Biomech (Bristol, Avon) 2010;25:693–9. doi: 10.1016/j.clinbiomech.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Development and validation of a clinic-based prediction tool to identify female athletes at high risk for anterior cruciate ligament injury. Am J Sports Med. 2010;38:2025–33. doi: 10.1177/0363546510370933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Myer GD, Ford KR, McLean SG, Hewett TE. The Effects of Plyometric Versus Dynamic Stabilization and Balance Training on Lower Extremity Biomechanics. Am J Sports Med. 2006;34:490–8. doi: 10.1177/0363546505281241. [DOI] [PubMed] [Google Scholar]
- 55.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19:51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 56.Myer GD, Ford KR, Paterno MV, Nick TG, Hewett TE. The effects of generalized joint laxity on risk of anterior cruciate ligament injury in young female athletes. Am J Sports Med. 2008;36:1073–80. doi: 10.1177/0363546507313572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Myer GD, Paterno MV, Ford KR, Hewett TE. Neuromuscular Training Techniques to Target Deficits Before Return to Sport After Anterior Cruciate Ligament Reconstruction. J Strength Cond Res. 2008;22:987–1014. doi: 10.1519/JSC.0b013e31816a86cd. [DOI] [PubMed] [Google Scholar]
- 58.Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after Anterior Cruciate Ligament Reconstruction: Criteria Based Progression Through the Return to Sport Phase. J Orthop Sports Phys Ther. 2006;36:385–402. doi: 10.2519/jospt.2006.2222. [DOI] [PubMed] [Google Scholar]
- 59.Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32:1002–12. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 60.Padua DA, Marshall SW, Beutler AI, Garrett WE. Prospective cohort study of biomechanical risk factors of ACL injury: The JUMP-ACL Study. American Orthopaedic Society of Sports Medicine Annual Meeting; Keystone, CO. 2009. pp. 393–395. [Google Scholar]
- 61.Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007;17:258–62. doi: 10.1097/JSM.0b013e31804c77ea. [DOI] [PubMed] [Google Scholar]
- 62.Paterno MV, Myer GD, Ford KR, Hewett TE. Neuromuscular training improves single-limb stability in young female athletes. J Orthop Sports Phys Ther. 2004;34:305–317. doi: 10.2519/jospt.2004.34.6.305. [DOI] [PubMed] [Google Scholar]
- 63.Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B, Hewett TE. Biomechanical Measures During Landing and Postural Stability Predict Second Anterior Cruciate Ligament Injury After Anterior Cruciate Ligament Reconstruction and Return to Sport. Am J Sports Med. 2010 doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Quatman CE, Ford KR, Myer GD, Hewett TE. Maturation Leads to Gender Differences in Landing Force and Vertical Jump Performance: A Longitudinal Study. Am J Sports Med. 2006;34:806–13. doi: 10.1177/0363546505281916. [DOI] [PubMed] [Google Scholar]
- 65.Quatman CE, Quatman-Yates CC, Hewett TE. A `plane' explanation of anterior cruciate ligament injury mechanisms: a systematic review. Sports Med. 2010;40:729–46. doi: 10.2165/11534950-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 66.Scoville CR, Williams GN, Uhorchak JM, Arciero RA, Taylor DC. Risk factors associated with anterior cruciate ligament injury. Proceedings of the 68th Annual Meeting of the American Academy of Orthopaedic Surgeons; Rosemont, IL: American Academy of Orthopaedic Surgeons; 2001. p. 564. [Google Scholar]
- 67.Sell TC, Ferris CM, Abt JP, Tsai YS, Myers JB, Fu FH, Lephart SM. Predictors of proximal tibia anterior shear force during a vertical stop-jump. J Orthop Res. 2007;25:1589–97. doi: 10.1002/jor.20459. [DOI] [PubMed] [Google Scholar]
- 68.Slauterbeck JR, Hardy DM. Sex hormones and knee ligament injuries in female athletes. Am J Med Sci. 2001;322:196–9. doi: 10.1097/00000441-200110000-00008. [DOI] [PubMed] [Google Scholar]
- 69.Soderman K, Alfredson H, Pietila T, Werner S. Risk factors for leg injuries in female soccer players: a prospective investigation during one out-door season. Knee Surg Sports Traumatol Arthrosc. 2001;9:313–21. doi: 10.1007/s001670100228. [DOI] [PubMed] [Google Scholar]
- 70.Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003;31:831–42. doi: 10.1177/03635465030310061801. [DOI] [PubMed] [Google Scholar]
- 71.Wilson JD, Dougherty CP, Ireland ML, Davis IM. Core Stability and Its Relationship to Lower Extremity Function and Injury. J Am Acad Orthop Surg. 2005;13:316–325. doi: 10.5435/00124635-200509000-00005. [DOI] [PubMed] [Google Scholar]
- 72.Winter DA. Biomechanics and Motor Control of Human Movement. John Wiley & Sons, Inc.; New York: 2005. [Google Scholar]
- 73.Withrow TJ, Huston LJ, Wojtys EM, Ashton-Miller JA. The relationship between quadriceps muscle force, knee flexion, and anterior cruciate ligament strain in an in vitro simulated jump landing. Am J Sports Med. 2006;34:269–74. doi: 10.1177/0363546505280906. [DOI] [PubMed] [Google Scholar]
- 74.Withrow TJ, Huston LJ, Wojtys EM, Ashton-Miller JA. Effect of varying hamstring tension on anterior cruciate ligament strain during in vitro impulsive knee flexion and compression loading. J Bone Joint Surg Am. 2008;90:815–23. doi: 10.2106/JBJS.F.01352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wojtys EM, Ashton-Miller JA, Huston LJ. A gender-related difference in the contribution of the knee musculature to sagittal-plane shear stiffness in subjects with similar knee laxity. J Bone Joint Surg Am. 2002;84-A:10–6. doi: 10.2106/00004623-200201000-00002. [DOI] [PubMed] [Google Scholar]
- 76.Wojtys EM, Huston LJ, Lindenfeld TN, Hewett TE, Greenfield MLVH. Association between the menstrual cycle and anterior cruciate ligament injuries in female athletes. Am J Sport Med. 1998;26:614–619. doi: 10.1177/03635465980260050301. [DOI] [PubMed] [Google Scholar]
- 77.Zatsiorsky VM. Science and practice of strength training. Human Kinetics; Champaign, IL: 1995. [Google Scholar]
- 78.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. The effects of core proprioception on knee injury: a prospective biomechanicalepidemiological study. Am J Sports Med. 2007;35:368–73. doi: 10.1177/0363546506297909. [DOI] [PubMed] [Google Scholar]
- 79.Zazulak BT, Paterno M, Myer GD, Romani WA, Hewett TE. The effects of the menstrual cycle on anterior knee laxity: a systematic review. Sports Med. 2006;36:847–62. doi: 10.2165/00007256-200636100-00004. [DOI] [PubMed] [Google Scholar]
- 80.Zazulak BT, Ponce PL, Straub SJ, Medvecky MJ, Avedisian L, Hewett TE. Gender comparison of hip muscle activity during single-leg landing. J Orthop Sports Phys Ther. 2005;35:292–9. doi: 10.2519/jospt.2005.35.5.292. [DOI] [PubMed] [Google Scholar]


