Abstract
Objectives
To address the psychological impact of the transplant on quality of life including physical, psychological, social and spiritual for the patient and caregiver and to discuss the nurse’s emotional labor of caring and compassion fatigue for such an intense vulnerable population.
Data Sources
Psychological transplant studies, peer review journals, and textbooks.
Conclusions
The psychological impact after an experience of a transplant can leave an indelible impression on the patient, caregiver and nurse.
Implications for Nursing Practice
Suggestions are made for assessment and management of various potential psychological issues for the three mentioned populations. With these issues being better understood, nurses can actively lessen psychological morbidity.
Keywords: Hematopoietic stem cell transplantation (HSCT), Psychological, Quality of Life (QOL), Caregiver, Compassion Fatigue
The psychological impact after hematopoietic stem cell transplantation (HSCT) can be immense. HSCT is an intense and distinctive experience for patients and families and has the potential to cause prolonged psychological distress unlike other experiences with oncology patients.1, 2 The Institute of Medicine report identified that meeting psychosocial health needs of the patients and family is the current exception rather than the common occurrence in this current health care climate.3 Because of the unique nature of the transplant experience, psychosocial assessment and interventions should be a high priority. The transplant procedure itself is complex and although the mortality has improved over the years since transplants began in the 1970’s it continues to be a significant stressor. The recovery after transplant can come with prolonged physical and psychological set-backs, and extreme social strain on the patient’s caregiver, friends and family members. In addition, the transplant experience can include multiple hospital readmissions for acute complications, slow recovery and long-term issues. Often the psychological and social issues can be more challenging for the health care team than the medical issues.4
This article discusses the psychosocial issues of three populations surrounding the transplant experience: the patient, the caregiver and the nurse. The patient section is divided into 3 sections: overall psychosocial concerns and assessment, common in-depth issues such as depression, and suggested interventions.
PATIENTS
The transplant experience can be psychologically devastating and often health care professionals forget and fail to understand the depth of trauma possible. Greenfield 5 in his eloquent essay and personal reflection as both a psychologist and transplant patient described the reality that the “powerful experience” of transplant caused him to re-experience psychological vulnerabilities despite years of psychoanalysis and therapy to address his past issues.5 It is a poignant reminder that often we as nurses, need to remember that that the human soul and spirit is fragile.
Assessment
Although it is clear that the majority of patients experience good global quality of life after transplantation, identifying those patients who are more psychologically vulnerable is crucial.6 What are the risk factors that predict a poorer overall psychological outcome, and how can we integrate them into a psychological assessment to target those patients for intervention?
The first critical risk factor is previous psychiatric morbidity or history.7 Those patients who have negative affect such as anxiety or depression are at risk for poorer health outcomes, longer length of stay, and higher mortality.7–11 Having any overall mood, anxiety or adjustment disorder was associated with an 8% increase in length of stay after transplantation. Poor transplant functioning significantly predicts more need for counseling.10, 11 Although this study does not point to previous psychiatric morbidity, Siston et al 12 found that there was significant emotional distress among patients prior to admission into the hospital for an allogeneic transplant.1 Thirty-five percent of the patients before the transplant admission reported significant symptoms of intrusive and avoidance stress responses. Perhaps the 35% of the patients going into transplant with significant psychological distress contribute to psychiatric morbidity.
Other risk factors that predict a poorer outcome have also been identified. Pre-transplant non-compliance is also associated with poorer health outcomes and perception of symptoms.7, 8 Social support, not just the presence of support, but its stability and character throughout the transplant process has also been linked to positive health outcomes.13–15 Other identified risk factors are younger age, female sex, avoidant coping strategies, lower functional status upon admission, pain, recent smoking cessation before hospital admission, and higher regimen-related toxicity.7, 16
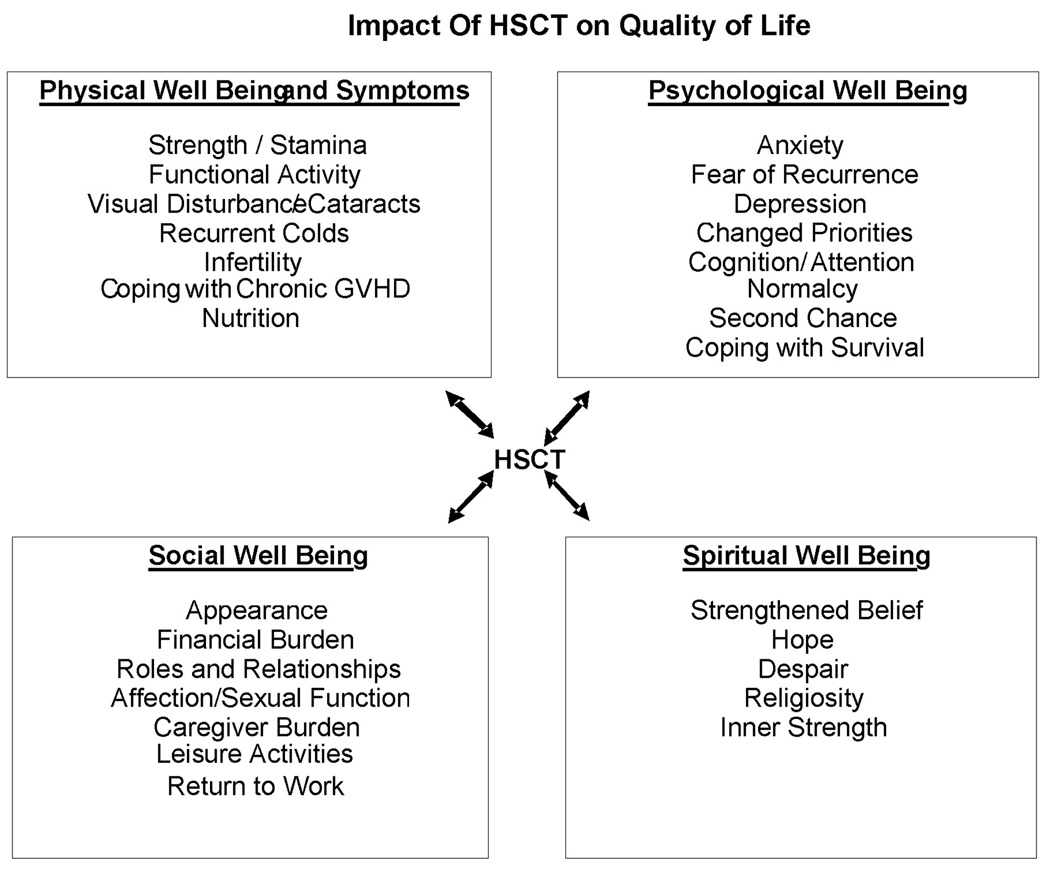
The literature is clear that the transplant experience impacts various aspects of quality of life. The following section will discuss various common psychological issues and how they are impacted by different domains of quality of life: physical, psychological, social and spiritual (See Figure 1).17–22 Prieto et al 7 found that the overall psychiatric disorder prevalence among transplant patients was 44%.7 Compared with non-transplant patients on a psychiatric consultation service, post transplant patients suffer complicated medical, psychiatric and social burdens.23
Figure 1 17, 18, 19–22.
Impact Of HSCT on Quality of Life
Physical Domain
Physical issues that patients face after transplantation affect psychological functioning. Higher depression rates are linked to slower physical recovery, and to patients with chronic graft versus host disease (cGVHD).24 In a support group setting, patients found the long-term issues of ongoing medical appointments, medications with side-effects, and long-term issues beyond a year frustrating.25 Most of the patients in the group, despite not having any visible signs of post-transplant physical changes, described feelings of being separate from “normal” people and had difficulty with reintegration. Patients felt unprepared for post-transplant life, found fatigue frustrating and limiting, had challenging cognitive changes, and most patient’s also experienced post-transplant sexual issues. Sexual difficulties such as vaginal dryness for women and erectile dysfunction in men have been discussed in the literature.25
Psychological Domain
Depression
Rates of depression among general cancer patients range from 10%–25%, whereas in some studies, rates of depression among the transplant population are higher, ranging from 25% to 50%.26–30 Higher levels of depression among transplant patients affect post transplant physical health symptoms, increase symptoms-related distress, may contribute to a higher suicide rate, and may decrease survival.26, 31, 32 Rates of depression after transplantation among several longitudinal studies report that depression increases soon after the transplantation and then seems to stabilize over time, although some studies continue to show rates of as much as 25% in patients one year after transplantation.27, 30 For the support group patients the experience of depression was different.25 These patients explained that for them depression did not occur until many months after discharge, anti-depressant medication was a definite necessity, and healing increased with the verbalization of the shared experience.
Distress
According to Jimmie Holland, a pioneer in the field of psychosocial oncology, 30% of cancer patients experience disabling “distress” resulting in the need for psychosocial treatment.33 The term “distress” was used by the National Comprehensive Cancer Network (NCCN) task force to develop standards for distress and a simple tool, The Distress Thermometer, for assessing distress among cancer patients.34, 35 The movement to label the psychosocial sequelae as “distress” rather than depression or anxiety made the term less stigmatizing and more acceptable for patients.35
As a population the transplant patients have high levels of distress, often thought to be due to the more intense treatment.36 Pre-transplant distress levels of 50% have been documented which is much higher than the average cancer population distress of 30%.37, 38 Transplant distress levels may also be high after transplantation. Rusiewitcz, et al,39 examined the distress of post-transplant patients at one year and found that 43% reported significant global psychological distress encompassing areas of existential concerns, obsessive-compulsiveness, loneliness, and ongoing health concerns such as memory loss.
Post Traumatic Stress Disorder
Interesting work has been developing in the psychosocial literature looking at the rates and characteristics of post-traumatic stress disorder (PTSD) among transplant patients since the transplant experience itself can classify as a “traumatic experience” which can trigger long-lasting psychological effects. Widows et al, 40 reported a rate of PTSD at 5%, and patients who had higher rates of PTSD symptoms had more negative appraisals of the transplantation experience, greater use of avoidance-based coping strategies, lower levels of social support, and greater social constraint. Another study examined the predictors for PTSD following transplant and found that social support and avoidance coping (escape-avoidance, distancing and denial) predicted PTSD symptoms.16 Social support was predictive of less PTSD with a high level of social support associated with 50% less PTSD symptoms. Analysis of the association of social support and the type of coping patients used after transplantation suggested that the presence of a supportive environment encouraged patients to use more healthy forms of coping to process the traumatic experience.
Social Domain
Throughout the data for psychological symptoms of transplant patients, social support continues to be a dominant factor for psychological recovery after transplantation. Social support predicts survival, higher QOL, decreased depression rates, less PTSD symptoms, and decreased psychosocial morbidity.13, 16, 30, 40–42 Rodrigue et al,13 indicated that not only the presence of support as important, but its stability since interpersonal conflict in patient’s lives may have unfavorable physical and psychosocial outcomes. Frick et al 15 identified the difference between harmful and helpful support, and reported that patients living with a partner displayed higher scores in positive interactions than patients living alone. They also showed that those relationships that had problematic interactions correlated significantly with poor emotional and social function. Patients in the support group setting verbalized relationship dynamics changes, role adjustments, differences in role expectations, and changes in interpersonal communications after the transplant experience.25 Patients stated that they felt safe in the support group expressing feelings whereas family members were sometimes unable to understand their fatigue; changes in values; physical, social and psychological impact of the transplant; and changes in communication style.
Another issue in the social domain is the ability to return to the school or work setting. Syrjala et al24 in her study of recovery after transplantation found that physical limitation reached a peak at 90 days followed by improvement at 1 year with no significant change beyond the 1 year improvement at 3 and 5 years. Of those patients with history of work outside the home, 20% returned to full-time work by 1 year and 31% by 2 years with risk factors for work delay being female sex, and extensive cGVHD. Descriptive data in the support group setting show that all patients altered their school or work experience after transplantation.25 Examples were changing majors in school, finding jobs that were less stressful, decreasing hours, dealing with fear of discrimination and not disclosing the transplant history, and meaningful work that was unlike the work setting.
Spiritual/existential Domain
Post-Traumatic Growth/Benefit Finding
The concept of post-traumatic growth (PTG), search for meaning or “benefit finding” after transplantation has been evolving in the literature over the past several years. By definition, the potential for PTG requires that patients experience a stressful event and subsequently experience positive psychological outcomes or benefits. As early as 1996 Fromm and colleagues43 identified positive sequelae possible after transplantation: development of a new philosophy of life, greater appreciation of life, making changes in personal characteristics, and improving relationships with family and friends. Potential predictors of PTG include good social support, the ability to approach rather than avoid, young age, less education, greater use of positive reinterpretation or cognitive appraisal, sense of mastery, and self-efficacy, problem solving, seeking alternative rewards, more stressful appraisal of the experience, and more negatively biased recall of pre-transplant levels of psychological distress.16, 40, 44
Survivorship
Survivorship issues have been brought to the forefront of cancer care within the last few decades, most recently with the Institute of Medicine report, From Cancer Patient to Cancer Survivor: Lost in Transition.45 Transplant patients recovering from the transplant procedure may face ongoing physical and psychological effects years after transplantation.46 Studies specifically with transplant patients report that even though most long-term HSCT survivors express satisfaction with their quality of life and describe themselves as productive, stable, and well-adjusted, most do not return to their pre-illness level of health.47, 48 Studies report that survivors continue to experience psychological distress related to the fear of recurrence, fear of secondary malignancies, body image issues, sexual functioning difficulties, distress about their families, uncertainty about the future, and professional reintegration concerns.6, 49
End-of-Life
Based on various hematological diseases at different stages the overall treatment-related mortality reported in the literature is approximately 15%–50%, and few studies have addressed end-of-life care for transplant patients.50, 51 Palliative care is not a routine component of care for patients with hematologic malignancies.52 Instead of dying at home, as other cancer patients frequently do, these patients are more likely to die in high-tech environments where the mortality rate can approach 100%.53 What is the reason for not including palliative care principles that are stressed by the Oncology Nursing Society and other organizations?54–56 Perhaps it can be explained in part because the goal of transplantation is aggressive cure and end-of-life options are often difficult for the patients, family and health-care professional to consider. An option is presented in a case study presentation of the role of the advanced nurse practitioner in transplant patients. At the end-of-life the nurse became the moral agent “holding” the family and patient’s existential hopes, communicating their wishes across disciplines, and creating an ethical environment.57
Risks
Table 1 provides a compilation of psychological morbidity risks identified from the literature regarding transplant patients. Because these risks have been identified in studies using varied transplant populations, small sample sizes, and various questionnaires and methodologies, it is impossible to quantify the effects of each factor on psychological morbidity or the relationships between factors. However, it represents an early step in the process of risk identification
Table 1.
HCT Patient Risk Factors for Psychological Morbidity
| Individual Patient Factors |
| Previous psychiatric morbidity |
| Pretransplant compliance issues |
| Younger age |
| Female sex |
| Avoidant coping strategy (escape-avoidance, distancing and denial) |
| Recent smoking cessation |
| Lower functional status upon admission |
| Environmental Patient Factors |
| Problems with presence, quality and perception of social support |
| The presence of difficult relationships |
| Professional reintegration concerns |
| Transplant-Related Patient Factors |
| Persistent symptoms such as chronic pain |
| Increased regimen-related toxicity |
| Slower physical recovery |
| Chronic Graft-versus-host disease |
| Negative appraisal of the transplant experience |
| Body image disturbance |
| Fears of relapse and secondary malignancies |
| Sexual function disruption |
Suggested Interventions
Based on the literature presented and the risk factors identified, a list of possible helpful interventions is listed below:
Antidepressants
“Accepting the reality of the person undergoing the experience is critical.”58 Antidepressants are effective for depression; however the obstacle lies with the acceptance of the rate of depression by health care professionals, and their ability to assess and intervene.26
Distress Thermometer
Using the distress thermometer as a simple tool for assessment is an easy step. The tool itself has been shown to compare favorably with longer measures for anxiety and depression, and it can be used to screen, and identify distress successfully throughout transplant recovery across various domains of QOL.37, 38, 59
Psychoeducational Interventions
Psychoeducational approaches for patients have been shown to have beneficial psychosocial benefits.60 Nurse-delivered psychoeducational approaches have been used in the oncology setting with good results. Strong, et al,61 described a cost-effective feasible intervention for depression for patients with cancer which decreased depression scores and had sustained results at 6 and 12 months. The sessions by the nurse included 1) problem-solving therapy to help overcome the feelings of helplessness, 2) education about depression and treatments and 3) counseling on communication with health care professionals about their symptoms. Another nurse specific intervention was described which outlined an APN-intervention for transplant patients within the first year after transplantation.57 This intervention described a total of 6 sessions which followed the QOL domain format addressing physical, psychological, social and spiritual/ existential issues.
Support Groups
The recent IOM report discussing psychosocial needs suggests the use of peer support groups.3 Group therapy can been helpful in the breast cancer population reducing depression and psychiatric symptoms, mood disturbance, and improving QOL; however no studies in the transplant population have been done to determine its effectiveness.62 A support group environment would possibly be helpful for patients who would benefit from a shared unique experience, especially one that family and friends may not be able to understand.25
Social Support
Social support is a critical factor, however no intervention trial was found in the transplant literature specifically focused on strengthening the caregiver and family coping. Bloch and Kissane62 proposed a family grief therapy model for families involved in end-of-life care which focused on improving functioning on cohesiveness, conflict and expressiveness. The intervention is intense, averaging 6–10 sessions over 6–12 months. Impressions from a pilot study are that the therapy is relevant and feasible; however a larger trial needs to be performed. Social support is a critical factor and supporting the caregiver and family in a more definitive, organized, standardized and research-based approach may be beneficial for the patients’ and families physical and psychological morbidity. Health care professionals in the transplant setting need to educate the patients’ and families on the importance of sustained social support throughout the entire inpatient and recovery period post transplant.30
Complementary and Alternative Medicine (CAM)
The only CAM therapy that has been studied in the transplant population has been relaxation techniques which have been found to be useful in reducing anxiety and depression.60, 63 Other uses of CAM therapies in the transplant patients have not been studied. In an elegant article by Chan and colleagues44, they challenge the field of psychosocial oncology to examine the “eastern approach” to health and healing in which trauma can be seen as a growth experience, encouraging a positive attitudes toward cancer and life, and restoration of energy and balance. Potential options for interventions could include diet, meditation, exercise, massage, self-care, cognitive restructuring, emotional expression, visualization of positive outcomes, counting blessings, group acceptance in support groups, sharing their experience through verbal, artistic or written expression, and giving back.
Cognitive and Behavioral Therapy (CBT)
CBT offering brief simple sessions provides effective relief for milder forms of psychological symptoms and seems effective for short-term management of anxiety and depression.60 It is also possible that CBT therapy may offer long-term effects on QOL.64
INFORMAL CAREGIVERS
Today there are more survivors of HSCT than at any other in large part because of the care and support provided by the informal caregiver. HSCT informal caregivers, usually a spouse, family member, friend or neighbor provides countless hours of unpaid assistance to HSCT recipients.65 While providing care can be a positive experience for most HSCT caregivers, especially for those who are able to find meaning in the experience, caregiving can be very exhaustive, emotionally draining as well as existentially challenging. As a consequence the informal caregiver is susceptible to negative psychological outcomes.
Impact of Care Giving
A growing body of evidence demonstrates the impact of cancer caregiving on the development of caregiver distress.66 Furthermore the American Cancer Society (ACS) estimates that caregivers will provide care to the 1.4 million newly diagnosed cancer patients. With five-year survival at 65%, up from 50% in 1974–1976, caregiving needs are increasing. Among caregivers in the United States almost 60% of caregivers either work or have worked while providing care.67 Nearly two thirds of caregivers reported having to make adjustments to their lives to provide care in order to juggle multiple roles. Women age 46 and older provide the majority of care, while men comprise nearly 40%. Forty percent of these female caregivers report having emotional distress associated with caregiving especially if there are multiple complex care needs.67 It is not surprising then that unmet caregiver needs have been identified: finding time for themselves (35%), managing emotional and physical stress (29%), and balancing work and family responsibilities (29%).67
Caregiving activities can be overwhelming and affect all aspects of the HSCT informal caregiver’s life. Unlike other cancers, the hematological cancer patient and caregiver grapple with diagnosis, treatment and then when treatment fails move on to the possibility of a life-saving stem cell transplant. The hope is always cure; the reality is approximately 20%–30% of patients will relapse and face end-of-life issues, another 30% will need to cope with lingering treatment related complications. Given the significant morbidity and mortality associated with the treatment and prolonged recovery from transplant, caregivers can potentially experience high stress levels due to the intense physical and emotional care needs of the HSCT recipient.68
Most informal caregivers are novices in providing care for the transplant recipient. They are often ill-prepared for the physical care and the emotional toll it takes over time. If the emotional toll of caregiving is left unchecked several adverse outcomes can ensue. For example, deteriorating caregiver mental and physical health has been reported. Waning caregiver commitment to caregiving may begin and poor transplant recipient outcomes may occur.69 Many HSCT caregivers describe being very involved in seeking information about what to expect, preparing their questions about the disease and treatment prior to meeting with the physician.65 Those caregivers who felt prepared for the role were more likely to report feelings of role satisfaction and rewards.68
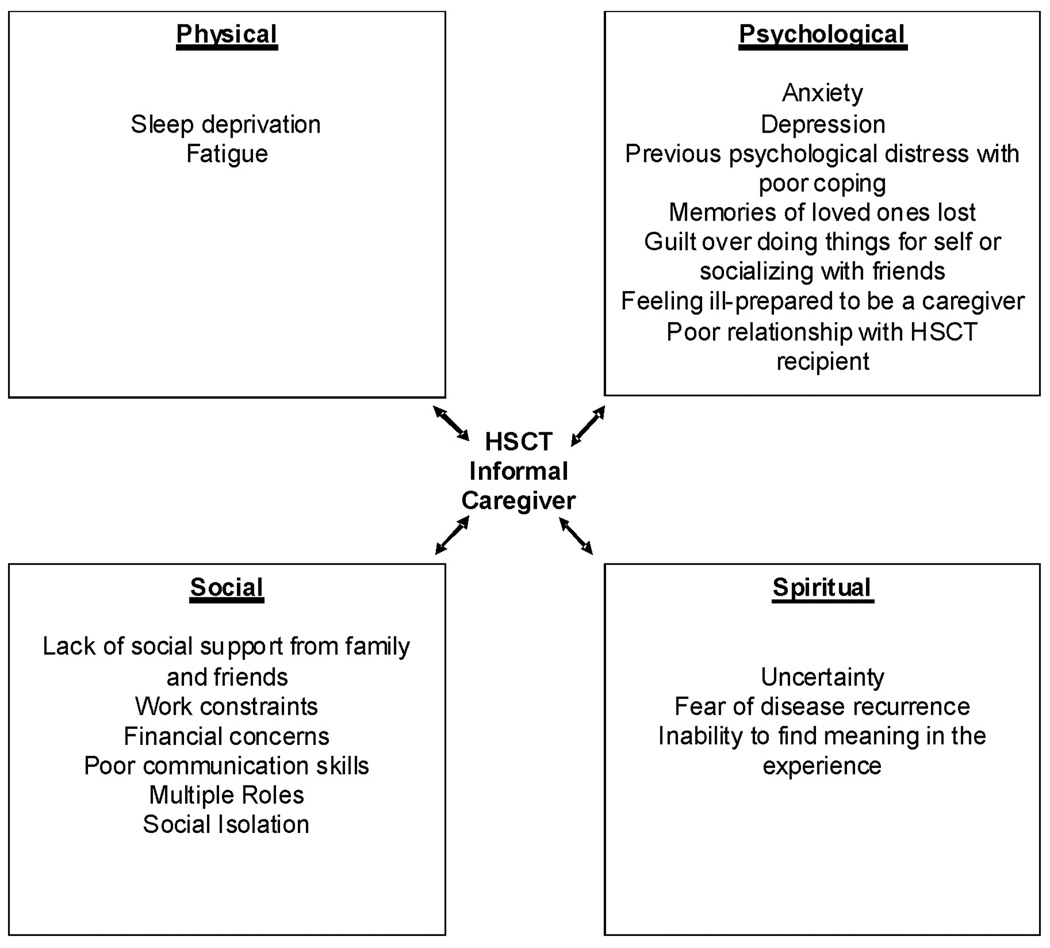
The concept of “quality of life” is an important outcome measure in cancer care. One widely used model developed at the City of Hope (COH) Medical Center assesses individual well-being in four domains: physical, psychological, social, and spiritual well-being and has been used with HSCT patients.70 Utilizing the COH-QOL Model as a framework the caregiving situation can be viewed in its entirety with an emphasis on the interplay among the various dimensions of care as it relates to caregiver psychological well-being (Figure 2).
Figure 2.
City of Hope Quality of Life Model HSCT Informal Caregiver
Although there is a paucity of blood and marrow transplant caregiver research, studies available describe how caregivers wrestle with psychological symptoms such as fear of the future,71, 72 loss of control, anxiety and depression, guilt, previous coping difficulties, and feelings of being ill-prepared for the caregiving role. Social issues such as isolation, lack of social support,73 relationship issues,74, 75 workforce issues, financial concerns; and physical symptoms such as sleep disruption76 and fatigue along with existential/religious issues77 may precipitate emotional distress among caregivers if not addressed.
How well the HSCT recipient is doing throughout the illness trajectory often determines how the caregiver will respond to the caregiving role. If the duration of recovery, treatment- related complications, symptom management, functional ability, and emotional well-being of the HSCT recipient are wearing then the caregiver might feel the strain of the situation leading to increased frustration, anxiety and depression. Women caregivers tend to experience more symptoms of anxiety and depression related to caregiving78 in comparison to male caregivers with the exception of those men who are caring for spouses with emotional issues.76
While young caregivers describe issues with juggling multiple roles (e.g. caregiver, parent, daughter/son, employee, and spouse) older caregivers describe difficulties with balancing their own health issues with that of the HSCT recipient. Spousal issues sometimes can influence caregiver emotional well-being. Langer et al 74 studied the marital dyad over a 12 month period post transplant. Findings revealed that matched perceptions of the relationship pre-transplant grew mismatched by 6 and 12 months post-transplant with female caregivers reporting lower levels of marital satisfaction compared to patients. Moreover, if there is a problematic pre-existing relationship between the caregiver and the HSCT recipient there is a three fold risk of mortality for the HSCT patient.79
Socially, HSCT informal caregivers report feeling as though their every day lives have been turned upside down. They report increased tension with other family members, resentment and frustration, social isolation, and financial concerns. Several studies describe how caregivers struggle to meet competing demands such as continuing to work outside the home while supporting the transplant recipient.65, 68, 73 Inability to meet conflicting work demands and caregiving might require the caregiver to stop working. Sixty seven percent of HSCT caregivers did suspend working to care for the transplant recipient.68 Adding to an already stressful situation worry about financial concerns resulting from suspension of employment can prompt psychological crisis for some.
HSCT caregivers often voice feelings of fear and uncertainty regarding their loved one’s future and the possibility of disease recurrence and death. These feelings of vulnerability are a significant part of the experience. How the caregiver responds to these feelings determines positive or negative health outcomes. The ability to find meaning and a sense of purpose as an HSCT caregiver can enhance their ability to cope with the challenges they face. Boyle et al73 explored caregiver and survivor perceptions post autologous transplant. Caregivers in this study found they gained new insights, were better able to prioritize life better and found they appreciated life more. Their coping strategies included acceptance, staying positive, looking at life differently, setting goals and praying with fears of recurrence as a concern. Similarly, findings from caregiver participants in focus groups record a number of strategies for dealing with the caregiving role and the ability to find meaning in the experience. Some of the strategies used include; 1) preparing for caregiving by acquiring information about services and resources, 2) managing care by providing physical care, keeping the patient safe and advocacy, 3)facing challenges by overcoming healthcare system barriers, 4) developing supportive strategies through journaling, maintaining family involvement, and utilizing perseverance and assertiveness, and 5) discovering unanticipated rewards and benefits such as increased ability to express their needs, appreciating what they have, and improved relationship with the HSCT recipient.65
Interventions
Current research suggests interventions likely to be effective in reducing caregiver strain include: 1) education related to the illness trajectory, skills acquisition and community resources, 2) problem solving/coping skills development, 3) referral to psychotherapy when indicated and 4) integration of health promotion self-care behaviors into caregiver lifestyle to buffer the impact of caregiving. Psychoeducational strategies are needed to support the caregiver through informational support and learning different coping styles to lessen the perceived burden of providing either direct or indirect care. Self-care strategies support the caregiver’s ability to manage health and well-being through activities such as exercise, massage, yoga, and meditation. Success of any proposed intervention is determined by the HSCT caregiver’s ability to participate in choosing the intervention and determining how it will be integrated into their life.
The psychological well-being of the HSCT informal caregiver can be influenced by a number of factors within the caregiving situation. If the HSCT caregiver is feeling overwhelmed, exhausted, fearful of the uncertain future, juggling multiple roles, worried about work or financial concerns, and lacking family/social support, then potential for poor coping exhibited by the development of anxiety, depression, guilt, and role conflict is likely. Thus, understanding how the HSCT informal caregiver appraises the situation, their ability to access resources/support and their ability to care for themselves will help the oncology nurse determine caregiver psychological well-being in order to implement timely evidence-based interventions. Integration of any proposed intervention done in partnership with the HSCT caregiver will ensure successful behavior change increasing caregiver psychological well-being. Lastly, through partnership with HSCT caregivers oncology nurses can recognize and affirm the valuable role HSCT caregiver plays in supporting the transplant recipient’s physical, psychological, social and spiritual well-being. Without continuous care and support of the HSCT caregiver transplant recipients’ health outcomes are in jeopardy.
The HSCT NURSE
Emotional Labor of Care Giving
An often unrecognized aspect of the work of nursing is emotional labor.80, 81 Emotional labor is the managing of emotion and emotional displays by professional care givers in order to produce a therapeutic outcome for the patient.81, 82 Emotional labor is governed by the social rules of the professional work group and may be associated with increased job satisfaction and/or increased job stress. 80, 81 Bone marrow transplant nursing has been characterized as a practice requiring rapid adaptation to changing protocols, prolonged periods of care delivered to patients in restrictive or protective environments, and the confrontation of existential issues associated with suffering and death.83 It is in the interest of nurses and patients to acknowledge emotional labor as an important aspect of practice and to develop effective strategies for managing its effects.
The consequences of emotional labor can include increased job satisfaction and feelings of personal accomplishment and/or increased job stress and decreased feelings of personal accomplishment.80 Job satisfaction and feelings of personal accomplishment may be enhanced when the emotional labor of nursing is conceived of by the nurse as part of the professional caring provided to patients that produces a therapeutic effect.80, 84, 85
Job satisfaction and feelings of personal accomplishment decline when the nurse experiences emotional labor as one kind of internal “felt” experience that does not match that which is displayed to the patient.81 An insincere smile that is used to illicit compliance rather than express pleasure is an example of this dissonance.80, 86 The consequence of undervalued or dissonant emotional labor is compassion fatigue that is expressed as disengagement and detachment from the needs and concerns of patients.87 Nursing disengagement from the needs of patients impacts many aspects of care including patient safety.88
Compassion Fatigue
Compassion fatigue has been defined as “…the stress resulting from helping or wanting to help a traumatized person…”.89 The critical element in this definition is that stress is triggered within the nurse by the desire to help in the face of another’s trauma.90 Features of practice that promote the stress response and compassion fatigue include beliefs that there is too much to do and not enough time to do it in, feelings of helplessness in the face of suffering and feelings of abandonment by leadership.91 Other factors that contribute to the development of compassion fatigue are workload, shift work and work with patients at end of life.92
Personal qualities of the nurse also contribute to the likelihood that a specific individual will experience compassion fatigue. Those qualities include inadequate professional boundaries that lead to over involvement with patients, satisfying personal needs for gratification through ministering to patients, unrealistic expectations, and personal characteristics that do not match the demands of the job.92 Circumstances such as divorce, death and other major life transitions can also contribute to the emergence of compassion fatigue. Life experiences (history of trauma), coping style (reliance on avoidance and/or isolation) and untreated anxiety or depression may also predispose the nurse to compassion fatigue.90
Personal qualities not only predispose someone to the development of compassion fatigue. They can, also, reduce the risk that the nurse will experience compassion fatigue. Individuals who have cultivated a network of active social support and who display the characteristics of hardiness and resilience across their lives seem to experience a measure of protection from the development of compassion fatigue even when exposed to a challenging work environment.93
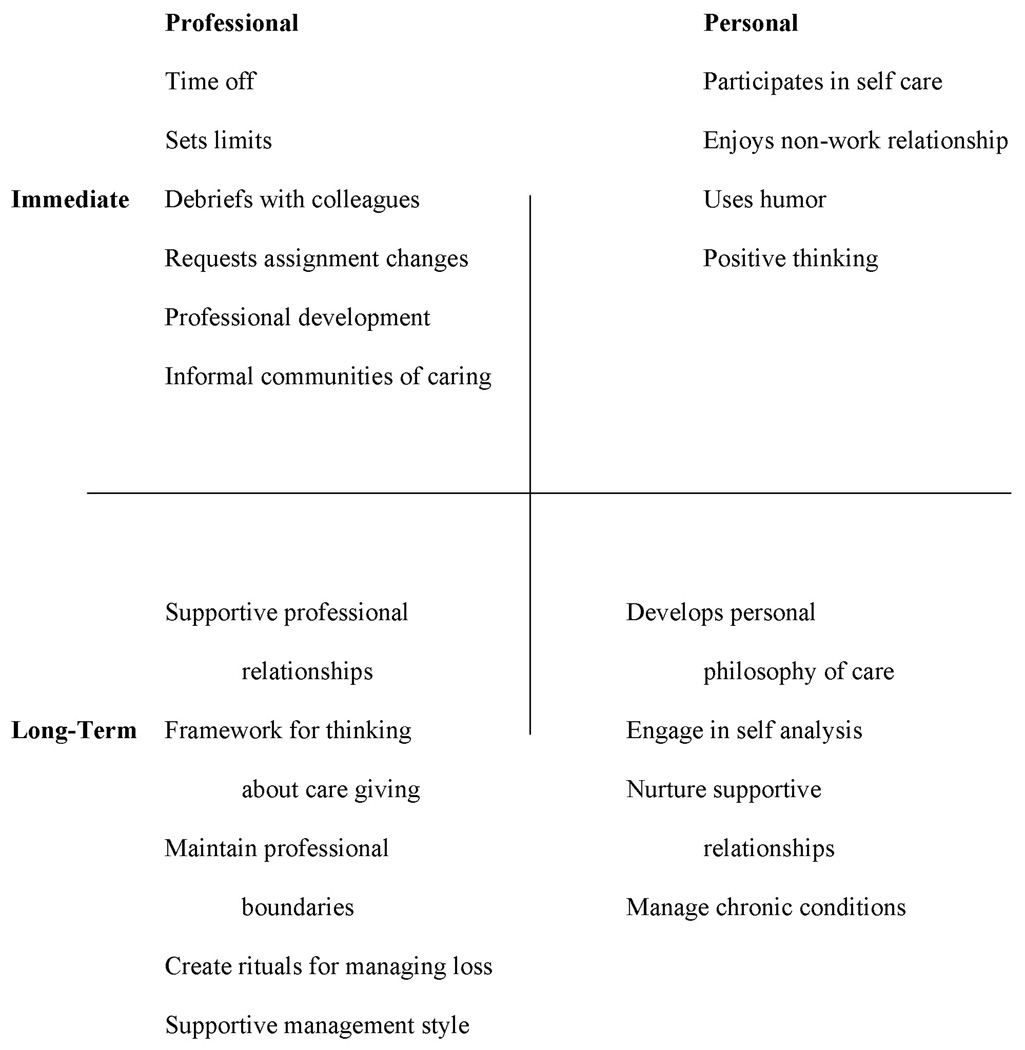
Compassion fatigue occurs over time as a result of a dynamic exchange between external variables (i.e.: workload) and internal variables (i.e.: isolation as a coping mechanism). Strategies that respond to this dynamic must therefore be multifaceted and include interventions that will be effective relatively quickly and those that will have a more long-term benefit. (See Figure 3) Examples of successful strategies that have both short- and long- term benefit include communities of caring, clear professional boundaries, and an enriched personal life.91, 94
Figure 3.
(Adapted from Maytum, Heiman, and Garwick, 91)
Create a Community of Caring
Bone marrow transplants are routinely conducted within a specified clinical area of a hospital that is staffed with a consistent team of well-educated nurses. Emotional labor is performed by the individual nurse and is also performed by the team of nurses who share the responsibility for providing care. Within this context, there is an opportunity to share the emotional labor and diminish its negative impact by creating informal communities of caring.94 These are not support groups or formally generated activities of any kind. These communities of caring arise organically from the very natural process of nurses sharing personal responses to common experiences with others who have had those same experiences. By and large, these communities evolve from the nurses themselves. They may begin with a conversation about the day’s work as shared by two nurses in the parking lot following the end of their shift. A supportive management environment will acknowledge and encourage the process and its benefits.91
Professional Boundaries
Lack of professional boundaries leading to an unnecessary investment in patients and their lives has been cited as a common factor leading to compassion fatigue.91 Professional boundaries can be compromised by deficits in understanding the role of a professional nurse and by attempts to meet unmet personal needs through the patient/nurse relationship.90 Developing a comprehensive view of the nursing role can be useful in clarifying professional boundaries. Addressing inadequate professional boundaries that are products of attempts to meet unmet needs requires the nurse to engage in ongoing personal analysis of the intentions that motivate patient care actions and to choose to act only in ways that place the patient’s needs in the forefront.91 For example, a nurse can ask herself before a patient encounter, “Am I doing this to meet the patient’s need or my need?” Sometimes the answer to this question is surprising.
Enriched Personal Life
Cultivation of an enriched personal life provides many benefits. In addition to those already described, an enriched personal life promotes an active rewarding social support system, facilitates positive physical health and leads to a positive sense of self esteem.95 Choosing to be engaged fully with a rich and varied personal life facilitates balance and limits the tendency to become over involved with and exhausted by patient care.
The work of nursing requires commitment of personal and professional energies. The wise nurse seeks a balance between the two and works to maintain engagement in an active personal life as well as a professional one.
Grant Support Acknowledgement
This article was supported in part by National Cancer Institute research study: R01 CA107446, Standardized Nursing Intervention Protocol.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Andrykowski MA. Psychosocial factors in bone marrow transplantation: a review and recommendations for research. Bone Marrow Transplant. 1994;13:357–375. [PubMed] [Google Scholar]
- 2.Andrykowski MA. Psychiatric and psychosocial aspects of bone marrow transplantation. Psychosomatics. 1994;35(1):13–24. doi: 10.1016/S0033-3182(94)71803-X. [DOI] [PubMed] [Google Scholar]
- 3.Adler Nancy E, Page Ann E.K., editors. Institute of Medicine (IOM) Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington, DC: The National Academies Press; 2008. [PubMed] [Google Scholar]
- 4.Eldredge DH, Nail LM, Maziarz RT, Hansen LK, Ewing D, Archbold PG. Explaining family caregiver role strain following autologous blood and marrow transplantation. J Psychosoc Oncol. 2006;24(3):53–74. doi: 10.1300/J077v24n03_03. [DOI] [PubMed] [Google Scholar]
- 5.Greenfield RM. Reflections on leukemia and adult stem-cell transplantation: some personal psychological factors. Palliat Supportive Care. 2007;5:415–418. doi: 10.1017/s1478951507000624. [DOI] [PubMed] [Google Scholar]
- 6.Saleh US, Brockopp DY. Quality of life one year following bone marrow transplantation: psychometric evaluation of the quality of life in bone marrow transplant survivors tool. Oncol Nurs Forum. 2001;28:1457–1464. [PubMed] [Google Scholar]
- 7.Prieto JM, Blanch J, Atala J, et al. Stem cell transplantation: risk factors for psychiatric morbidity. Eur J Cancer. 2006;42:514–520. doi: 10.1016/j.ejca.2005.07.037. [DOI] [PubMed] [Google Scholar]
- 8.Garcia C, Jr, Botega NJ, De Souza CA. A psychosocial assessment interview of candidates for hematopoietic stem cell transplantation. Haematologica. 2005;90:570–572. [PubMed] [Google Scholar]
- 9.Prieto JM, Blanch J, Atala J, et al. Psychiatric morbidity and impact on hospital length of stay among hematologic cancer patients receiving stem-cell transplantation. J Clin Oncol. 2002;20:1907–1917. doi: 10.1200/JCO.2002.07.101. [DOI] [PubMed] [Google Scholar]
- 10.Goetzmann L, Klaghofer R, Wagner-Huber R, et al. Psychosocial need for counselling before and after a lung, liver or allogenic bone marrow transplant--results of a prospective study. Z Psychosom Med Psychother. 2006;52:230–242. doi: 10.13109/zptm.2006.52.3.230. [DOI] [PubMed] [Google Scholar]
- 11.Goetzmann L, Klaghofer R, Wagner-Huber R, et al. Quality of life and psychosocial situation before and after a lung, liver or an allogeneic bone marrow transplant. Swiss Med Wkly. 2006;136(17–18):281–290. doi: 10.4414/smw.2006.11362. [DOI] [PubMed] [Google Scholar]
- 12.Siston AK, List MA, Daugherty CK, et al. Psychosocial adjustment of patients and caregivers prior to allogeneic bone marrow transplantation. Bone Marrow Transplant. 2001;27:1181–1188. doi: 10.1038/sj.bmt.1703059. [DOI] [PubMed] [Google Scholar]
- 13.Rodrigue JR, Pearman TP, Moreb J. Morbidity and mortality following bone marrow transplantation: predictive utility of Pre-BMT affective functioning, compliance, and social support stability. Int J Behav Med. 1999;6:241–254. doi: 10.1207/s15327558ijbm0603_3. [DOI] [PubMed] [Google Scholar]
- 14.Lim JW, Zebrack B. Social networks and quality of life for long-term survivors of leukemia and lymphoma. Support Care Cancer. 2006;14:185–192. doi: 10.1007/s00520-005-0856-x. [DOI] [PubMed] [Google Scholar]
- 15.Frick E, Ramm G, Bumeder I, Schultz-Kindermann F, Tyroller M, Fischer N, Hasenbring M. Social support and quality of life of patients prior to stem cell or bone marrow transplantation. Brit J Health Psychol. 2006;11(Pt 3):451–462. doi: 10.1348/135910705X53849. [DOI] [PubMed] [Google Scholar]
- 16.Jacobsen PB, Sadler IJ, Booth-Jones M, Soety E, Weitzner MA, Fields KK. Predictors of posttraumatic stress disorder symptomatology following bone marrow transplantation for cancer. J Consult Clin Psychol. 2002;70:235–240. doi: 10.1037//0022-006x.70.1.235. [DOI] [PubMed] [Google Scholar]
- 17.Ferrell B, Grant M, Schmidt GM, et al. The meaning of quality of life for bone marrow transplant survivors. Part 2. Improving quality of life for bone marrow transplant survivors. Cancer Nurs. 1992;15:247–253. [PubMed] [Google Scholar]
- 18.Ferrell B, Grant M, Schmidt GM, et al. The meaning of quality of life for bone marrow transplant survivors. Part 1. The impact of bone marrow transplant on quality of life. Cancer Nurs. 1992;15:153–160. [PubMed] [Google Scholar]
- 19.Grant M, Ferrell B, Schmidt GM, Fonbuena P, Niland JC, Forman SJ. Measurement of quality of life in bone marrow transplantation survivors. Qual Life Res. 1992;1:375–384. doi: 10.1007/BF00704432. [DOI] [PubMed] [Google Scholar]
- 20.King CR, Ferrell BR, Grant M, Sakurai C. Nurses' perceptions of the meaning of quality of life for bone marrow transplant survivors. Cancer Nurs. 1995;18:118–129. [PubMed] [Google Scholar]
- 21.Schmidt GM, Niland JC, Forman SJ, et al. Extended follow-up in 212 long-term allogeneic bone marrow transplant survivors. Issues of quality of life. Transplantation. 1993;55:551–557. doi: 10.1097/00007890-199303000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Whedon M, Ferrell BR. Quality of life in adult bone marrow transplant patients: beyond the first year. Semin Oncol Nurs. 1994;10:42–57. doi: 10.1016/s0749-2081(05)80044-0. [DOI] [PubMed] [Google Scholar]
- 23.Kishi Y, Meller WH, Swigart SE, Kathol RG. Are the patients with post-transplant psychiatric consultation different from other medical-surgical consultation inpatients? Psychiatry Clin Neurosci. 2005;59(1):19–24. doi: 10.1111/j.1440-1819.2005.01326.x. [DOI] [PubMed] [Google Scholar]
- 24.Syrjala KL, Langer SL, Abrams JR, et al. Recovery and long-term function after hematopoietic cell transplantation for leukemia or lymphoma. JAMA. 2004;291:2335–2343. doi: 10.1001/jama.291.19.2335. [DOI] [PubMed] [Google Scholar]
- 25.Sherman RS, Cooke E, Grant M. Dialogue among survivors of hematopoietic cell transplantation support-group themes. J Psychosoc Oncol. 2005;23:1–24. doi: 10.1300/J077v23n01_01. [DOI] [PubMed] [Google Scholar]
- 26.Pirl WF. Evidence report on the occurrence, assessment, and treatment of depression in cancer patients. J Natl Cancer Inst Monogr. 2004;32:32–39. doi: 10.1093/jncimonographs/lgh026. [DOI] [PubMed] [Google Scholar]
- 27.Broers S, Kaptein AA, Le Cessie S, Fibbe W, Hengeveld MW. Psychological functioning and quality of life following bone marrow transplantation: a 3-year follow-up study. J Psychosom Res. 2000;48:11–21. doi: 10.1016/s0022-3999(99)00059-8. [DOI] [PubMed] [Google Scholar]
- 28.Jenkins PL, Linington A, Whittaker JA. A retrospective study of psychosocial morbidity in bone marrow transplant recipients. Psychosomatics. 1991;32:65–71. doi: 10.1016/S0033-3182(91)72113-0. [DOI] [PubMed] [Google Scholar]
- 29.Keogh F, O'Riordan J, McNamara C, Duggan C, McCann SR. Psychosocial adaptation of patients and families following bone marrow transplantation: a prospective, longitudinal study. Bone Marrow Transplant. 1998;22:905–911. doi: 10.1038/sj.bmt.1701443. [DOI] [PubMed] [Google Scholar]
- 30.Jenks Kettman JD, Altmaier EM. Social support and depression among bone marrow transplant patients. J Health Psychol. 2008;13:39–46. doi: 10.1177/1359105307084310. [DOI] [PubMed] [Google Scholar]
- 31.Pearman T. Mortiality and morbidity following bone marrow transplantation: predictive utility of psychological variables. Dissertation Abstracts International. 1998;58(7):3932B. [Google Scholar]
- 32.Colon EA, Callies AL, Popkin MK, McGlave PB. Depressed mood and other variables related to bone marrow transplantation survival in acute leukemia. Psychosomatics. 1991;32:420–425. doi: 10.1016/S0033-3182(91)72045-8. [DOI] [PubMed] [Google Scholar]
- 33.Rosenthal E. Psycho-oncology pioneer Jimmie Holland on her fight to have cancer patients' distress recognized. Oncology Times. 2007 October 25;:8–12. 2007. [Google Scholar]
- 34.Holland J. NCCN practice guidelines for the management of psychosocial distress. National Comprehensive Cancer Network. Oncology (Huntington) 1999;13:113–147. [PubMed] [Google Scholar]
- 35.Kash KM, Mago R, Kunkel EJ. Psychosocial oncology: supportive care for the cancer patient. Semin Oncol. 2005;32:211–218. doi: 10.1053/j.seminoncol.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 36.Kornblith AB. Psychosocial adaptation of cancer survivors. In: Holland JC, editor. Psycho-oncology. New York, NY: Oxford University Press; 1998. pp. 223–256. [Google Scholar]
- 37.Lee SJ, Loberiza FR, Antin JH, et al. Routine screening for psychosocial distress following hematopoietic stem cell transplantation. Bone Marrow Transplant. 2005;35:77–83. doi: 10.1038/sj.bmt.1704709. [DOI] [PubMed] [Google Scholar]
- 38.Trask PC, Paterson A, Riba M, et al. Assessment of psychological distress in prospective bone marrow transplant patients. Bone Marrow Transplant. 2002;29:917–925. doi: 10.1038/sj.bmt.1703557. [DOI] [PubMed] [Google Scholar]
- 39.Rusiewicz A, DuHamel KN, Burkhalter J, et al. Psychological distress in long-term survivors of hematopoietic stem cell transplantation. Psychooncology. 2008;17:329–337. doi: 10.1002/pon.1221. [DOI] [PubMed] [Google Scholar]
- 40.Widows MR, Jacobsen PB, Booth-Jones M, Fields KK. Predictors of posttraumatic growth following bone marrow transplantation for cancer. Health Psychol. 2005;24:266–273. doi: 10.1037/0278-6133.24.3.266. [DOI] [PubMed] [Google Scholar]
- 41.Grassi L, Indelli M, Marzola M, et al. Depressive symptoms and quality of life in home-care-assisted cancer patients. J Pain Symptom Manage. 1996;12:300–307. doi: 10.1016/s0885-3924(96)00181-9. [DOI] [PubMed] [Google Scholar]
- 42.Lloyd-Williams M, Friedman T. Depression in palliative care patients--a prospective study. Eur J Cancer Care (Engl) 2001;10:270–274. doi: 10.1046/j.1365-2354.2001.00290.x. [DOI] [PubMed] [Google Scholar]
- 43.Fromm K, Andrykowski MA, Hunt J. Positive and negative psychosocial sequelae of bone marrow transplantation: implications for quality of life assessment. J Behav Med. 1996;19:221–240. doi: 10.1007/BF01857767. [DOI] [PubMed] [Google Scholar]
- 44.Chan CL, Ho RT, Fu W, Chow AY. Turning curses into blessings: an Eastern approach to psychosocial oncology. J Psychosoc Oncol. 2006;24:15–32. doi: 10.1300/J077v24n04_02. [DOI] [PubMed] [Google Scholar]
- 45.Hewitt Maria, Greenfield Sheldon, Stovall Ellen., editors. Institute of Medicine (IOM) From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: National Academies Press; 2005. [Google Scholar]
- 46.Rizzo JD, Wingard JR, Tichelli A, et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation: joint recommendations of the European Group for Blood and Marrow Transplantation, the Center for International Blood and Marrow Transplant Research, and the American Society of Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2006;12:138–151. doi: 10.1016/j.bbmt.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 47.Tierney DK. Intangible results: quality of life issues following hematopoietic cell transplantation. Stanford Nurse. 2008 Spring;:14. [Google Scholar]
- 48.Andrykowski MA, McQuellon RP. Psychosocial issues in hematopoietic cell transplantation. In: Blume KG, Forman SJ, Appelbaum F, editors. Thomas' Hematopoietic Cell Transplantation (3rd ed) Malden, MA: Blackwell Publishing Ltd; 2004. pp. 497–506. [Google Scholar]
- 49.Gruber U, Fegg M, Buchmann M, Kolb HJ, Hiddemann W. The long-term psychosocial effects of haematopoetic stem cell transplantation. Eur J Cancer Care (Engl) 2003;12:249–256. [PubMed] [Google Scholar]
- 50.Parimon T, Au DH, Martin PJ, Chien JW. A risk score for mortality after allogeneic hematopoietic cell transplantation. Ann Intern Med. 2006;144:407–414. doi: 10.7326/0003-4819-144-6-200603210-00007. [DOI] [PubMed] [Google Scholar]
- 51.Program NMD. Transplant outcomes by disease and disease stage. [Accessed 9-15-08];2008 [Google Scholar]
- 52.McGrath P. Caregivers' insights on the dying trajectory in hematology oncology. Cancer Nurs. 2001;24:413–421. doi: 10.1097/00002820-200110000-00014. [DOI] [PubMed] [Google Scholar]
- 53.Gupta D, Goyal GN, Chauhan H, Mishra S, Bhatnagar S. An initiative to end-of-life decisions in cancer care. Internet J Gynecol Obstet. 2008;9(2) [Google Scholar]
- 54.Oncology Nursing Society and Association of Oncology Social Work joint position on palliative and end-of-life care. Oncol Nurs Forum. 2007;34:1097–1098. [PubMed] [Google Scholar]
- 55.National Consensus Project for Quality Palliative Care: Clinical Practice Guidelines for quality palliative care, executive summary. J Palliat Med. 2004;7:611–627. doi: 10.1089/jpm.2004.7.611. [DOI] [PubMed] [Google Scholar]
- 56.Wasserman LS. Respectful death: A model of end-of-life care. Clin J Oncol Nurs. 2008;12:621–626. doi: 10.1188/08.CJON.621-626. [DOI] [PubMed] [Google Scholar]
- 57.Cooke L, Gemmill R, Grant M. Advanced practice nurses core competencies: a framework for developing and testing an advanced practice nurse discharge intervention. Clin Nurse Spec. 2008;22:218–225. doi: 10.1097/01.NUR.0000325366.15927.2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nail LM. I'm coping as fast as I can: psychosocial adjustment to cancer and cancer treatment. Oncol Nurs Forum. 2001;28:967–970. [PubMed] [Google Scholar]
- 59.Vachon M. Psychosocial distress and coping after cancer treatment. How clinicians can assess distress and which interventions are appropriate--what we know and what we don't. Am J Nurs. 2006;106(3 Suppl):26–31. doi: 10.1097/00000446-200603003-00011. [DOI] [PubMed] [Google Scholar]
- 60.Jacobsen PB, Jim HS. Psychosocial interventions for anxiety and depression in adult cancer patients: achievements and challenges. CA Cancer J Clin. 2008;58:214–230. doi: 10.3322/CA.2008.0003. [DOI] [PubMed] [Google Scholar]
- 61.Strong V, Waters R, Hibberd C, et al. Management of depression for people with cancer (SMaRT oncology 1): a randomised trial. Lancet. 2008;372(9632):40–48. doi: 10.1016/S0140-6736(08)60991-5. [DOI] [PubMed] [Google Scholar]
- 62.Simpson JS, Carlson LE, Trew ME. Effect of group therapy for breast cancer on healthcare utilization. Cancer Pract. 2001;9:19–26. doi: 10.1046/j.1523-5394.2001.91005.x. [DOI] [PubMed] [Google Scholar]
- 63.Fritzsche K, Struss Y, Stein B, Spahn C. Psychosomatic liaison service in hematological oncology: need for psychotherapeutic interventions and their realization. Hematol Oncol. 2003;21:83–89. doi: 10.1002/hon.711. [DOI] [PubMed] [Google Scholar]
- 64.Osborn RL, Demoncada AC, Feuerstein M. Psychosocial interventions for depression, anxiety, and quality of life in cancer survivors: meta-analyses. Int J Psychiatry Med. 2006;36:13–34. doi: 10.2190/EUFN-RV1K-Y3TR-FK0L. [DOI] [PubMed] [Google Scholar]
- 65.Stetz KM, McDonald JC, Compton K. Needs and experiences of family caregivers during marrow transplantation. Oncol Nurs Forum. 1996;23:1422–1427. [PubMed] [Google Scholar]
- 66.Given BA, Given CW, Kozachik S. Family support in advanced cancer. CA Cancer J Clin. 2001;51:213–231. doi: 10.3322/canjclin.51.4.213. [DOI] [PubMed] [Google Scholar]
- 67.National Alliance for Caregiving and AARP. Caregiving in the US. 2004 [Google Scholar]
- 68.Eldredge DH, Nail LM, Maziarz RT, Hansen LK, Ewing D, Archbold PG. Explaining family caregiver role strain following autologous blood and marrow transplantation. J Psychosoc Oncol. 2006;24:53–74. doi: 10.1300/J077v24n03_03. [DOI] [PubMed] [Google Scholar]
- 69.Foster LW, McLellan LJ, Rybicki LA, Sassano DA, Hsu A, Bolwell BJ. Survival of patients who have undergone allogeneic bone marrow transplantation: the relative importance of in-hospital lay care-partner support. J Psychosoc Oncol. 2004;22:1–20. [Google Scholar]
- 70.Ferrell BR. The quality of lives: 1,525 voices of cancer. Oncol Nurs Forum. 1996;23:909–916. [PubMed] [Google Scholar]
- 71.Aslan O, Kav S, Meral C, et al. Needs of lay caregivers of bone marrow transplant patients in Turkey: a multicenter study. Cancer Nurs. 2006;29:E1–E7. doi: 10.1097/00002820-200611000-00014. [DOI] [PubMed] [Google Scholar]
- 72.Foxall MJ, Gaston-Johansson F. Burden and health outcomes of family caregivers of hospitalized bone marrow transplant patients. J Adv Nurs. 1996;24:915–923. doi: 10.1111/j.1365-2648.1996.tb02926.x. [DOI] [PubMed] [Google Scholar]
- 73.Boyle D, Blodgett L, Gnesdiloff S, et al. Caregiver quality of life after autologous bone marrow transplantation. Cancer Nurs. 2000;23:193–203. doi: 10.1097/00002820-200006000-00006. quiz 204-195. [DOI] [PubMed] [Google Scholar]
- 74.Langer S, Abrams J, Syrjala K. Caregiver and patient marital satisfaction and affect following hematopoietic stem cell transplantation: a prospective, longitudinal investigation. Psychooncology. 2003;12:239–253. doi: 10.1002/pon.633. [DOI] [PubMed] [Google Scholar]
- 75.Keogh F, O'Riordan J, McNamara C, Duggan C, McCann SR. Psychosocial adaptation of patients and families following bone marrow transplantation: a prospective, longitudinal study. Bone Marrow Transplant. 1998;22:905–911. doi: 10.1038/sj.bmt.1701443. [DOI] [PubMed] [Google Scholar]
- 76.Siston AK, List MA, Daugherty CK, et al. Psychosocial adjustment of patients and caregivers prior to allogeneic bone marrow transplantation. Bone Marrow Transplant. 2001;27:1181–1188. doi: 10.1038/sj.bmt.1703059. [DOI] [PubMed] [Google Scholar]
- 77.Williams LA. Whatever it takes: informal caregiving dynamics in blood and marrow transplantation. Oncol Nurs Forum. 2007;34:379–387. doi: 10.1188/07.ONF.379-387. [DOI] [PubMed] [Google Scholar]
- 78.Gaston-Johansson F, Lachica EM, Fall-Dickson JM, Kennedy MJ. Psychological distress, fatigue, burden of care, and quality of life in primary caregivers of patients with breast cancer undergoing autologous bone marrow transplantation. Oncol Nurs Forum. 2004;31:1161–1169. doi: 10.1188/04.ONF.1161-1169. [DOI] [PubMed] [Google Scholar]
- 79.Frick E, Motzke C, Fischer N, Busch R, Bumeder I. Is perceived social support a predictor of survival for patients undergoing autologous peripheral blood stem cell transplantation? Psychooncology. 2005;14:759–770. doi: 10.1002/pon.908. [DOI] [PubMed] [Google Scholar]
- 80.Mann S, Cowburn J. Emotional labour and stress within mental health nursing. J Psychiatr Ment Health Nurs. 2005;12:154–162. doi: 10.1111/j.1365-2850.2004.00807.x. [DOI] [PubMed] [Google Scholar]
- 81.Bolton SC. Changing faces: Nurses as emotional jugglers. Sociol Health Illness. 2001;23:85–100. [Google Scholar]
- 82.Hochschild AR. The managed heart: commercialization of human feeling. Berkeley, CA: University of California Press; 1983. [Google Scholar]
- 83.Kelly D, Ross S, Gray B, Smith P. Death, dying and emotional labour: problematic dimensions of the bone marrow transplant nursing role? J Adv Nurs. 2000;32:952–960. [PubMed] [Google Scholar]
- 84.Bolton SC. Who cares? Offering emotion work as a 'gift' in the nursing labour process. J Adv Nurs. 2000;32:580–586. doi: 10.1046/j.1365-2648.2000.01516.x. [DOI] [PubMed] [Google Scholar]
- 85.Smith P, Gray B. Emotional labour of nursing revisited: caring and learning 2000. Nurs Educ Pract. 2001;1:42–49. doi: 10.1054/nepr.2001.0004. [DOI] [PubMed] [Google Scholar]
- 86.Mann S. A health-care model of emotional labour: an evaluation of the literature and development of a model. J Health Organiz Manag. 2005;19(4–5):304–317. doi: 10.1108/14777260510615369. [DOI] [PubMed] [Google Scholar]
- 87.Henderson A. Emotional labor and nursing: an under-appreciated aspect of caring work. Nurs Inq. 2001;8:130–138. doi: 10.1046/j.1440-1800.2001.00097.x. [DOI] [PubMed] [Google Scholar]
- 88.Aiken LH, Clarke SP, Sloane DM. Hospital staffing, organization, and quality of care: Cross-national findings. Nurs Outlook. 2002;50:187–194. doi: 10.1067/mno.2002.126696. [DOI] [PubMed] [Google Scholar]
- 89.Figley CR. Compassion Fatigue: Coping with Traumatic Stress Disorder in Those Who Treat the Traumatized. New York, NY: Brunner-Mazel; 1995. [Google Scholar]
- 90.Abendroth M, Flannery J. Predicting the risk of compassion fatigue: a study of hospice nurses. J Hosp Palliat Nurs. 2006;8:346–356. [Google Scholar]
- 91.Maytum JC, Heiman MB, Garwick AW. Compassion fatigue and burnout in nurses who work with children with chronic conditions and their families. J Pediatr Health Care. 2004;18:171–179. doi: 10.1016/j.pedhc.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 92.Brotheridge CM, Grandey AA. Emotional labor and burnout: comparing two perspectives of "People Work". J Vocational Behav. 2002;60(1):17–39. [Google Scholar]
- 93.Sabo BM. Compassion fatigue and nursing work: can we accurately capture the consequences of caring work? Int J Nurs Pract. 2006;12:136–142. doi: 10.1111/j.1440-172X.2006.00562.x. [DOI] [PubMed] [Google Scholar]
- 94.Korczynski M. Communities of coping: collective emotional labor in service work. Organization. 2003;10:55–79. [Google Scholar]
- 95.McLeod BW. Self-care: The Path to Wholeness. In: Doka KJ, editor. Caregiving and Loss: Family Needs, Professional Responses. Hospice Foundation of America; 2003. [Google Scholar]