Abstract
We observed an independent association between vitamin D insufficiency and higher carotid intima-media thickness in a cross-sectional analysis of 139 HIV-infected persons. If confirmed, these findings support a clinical trial of vitamin D supplementation to reduce cardiovascular events in HIV-infected persons.
Human immunodeficiency virus (HIV)–infected persons have high rates of vitamin D insufficiency, but little is known about its effect on cardiovascular disease [1]. We conducted this study to identify factors associated with vitamin D insufficiency and to describe the association of vitamin D insufficiency with subclinical atherosclerosis, measured by carotid intima-media thickness (cIMT), in HIV-infected persons.
METHODS
Participants were selected from a prospective study of bone metabolism and cardiovascular risk factors from the University of California–San Francisco (UCSF) Study of the Consequences of the Protease Inhibitor Era cohort, an ongoing study of the long-term clinical outcomes associated with antiretroviral therapy (ART) in HIV-infected adults [2–3]. Study investigators conducted structured interviews and detailed chart reviews to obtain sociodemographic characteristics (age, sex, and self-reported race), HIV disease history (current and cumulative ART exposure, CD4+ cell count nadir, hepatitis C or B co-infection, and history of opportunistic infection), comorbidities (cardiovascular disease, hypertension, diabetes, and dyslipidemia), health-related behaviors (alcoholism and smoking), and medication exposures (multivitamin or calcium supplementation). Other measurements included body mass index (BMI, defined as the weight in kilograms divided by the square of height in meters) and the waist-to-hip ratio. The study was approved by the UCSF Committee on Human Research.
Carotid B-mode ultrasound recordings were obtained using the standardized protocol of the Atherosclerosis Risk in Communities Study within 1 week of the structured interview, physical examination, and blood sampling [4]. cIMT was measured in 12 predefined segments (the right and left common carotid artery, carotid bifurcation, and internal carotid artery at both the near and far wall segments). All scans were performed by and measurements obtained on digital images using manual calipers by a single experienced vascular technician who was blinded to the participant's clinical characteristics. The mean cIMT value (in mm) was calculated for each subject on the basis of the 12 measurements at the predefined segments.
All study subjects had 25-OH vitamin D (“vitamin D”), 1,25-OH vitamin D, and intact parathyroid hormone (PTH) levels measured by Quest Diagnostics (San Juan Capistrano, CA). Vitamin D levels were measured by radioimmunoassay, 1,25-OH vitamin D levels were measured by liquid chromatography tandem mass spectrometry, and intact PTH levels were measured by immunoassay spectrophotometry. Vitamin D levels ≤30 ng/mL were classified as insufficient on the basis of consensus definitions [5]. Total cholesterol, high-density lipoprotein cholesterol (HDL), triglycerides, low-density lipoprotein cholesterol (LDL), and plasma glucose levels were obtained in the fasting state. Elevated fasting glucose levels were defined by a level >125 mg/dL. CD4+ cell counts and HIV viral load measurements were obtained for all individuals. Individuals with an estimated glomerular filtration rate (GFR) <60 mL/min/1.73 m2 were designated as having kidney disease.
We conducted 2 cross-sectional analyses. We first determined the prevalence of and risk factors for vitamin D insufficiency. Because the outcome (vitamin D deficiency) was common, the use of logistic regression to estimate odds ratios would not closely approximate prevalence ratios, which could potentially lead to incorrect interpretations [6]. We have therefore used a Poisson working model with robust standard errors to directly estimate prevalence ratios [7]. We conducted unadjusted comparisons between all characteristics and the outcome of vitamin D insufficiency and included variables with P <.1 in multivariable regression analysis; age, sex, and race were forced into the final model.
We next examined the association between vitamin D insufficiency and mean cIMT using multivariable linear regression. We performed covariate selection on the basis of a causal directed acyclic graph (DAG) approach [8]. We included variables that were identified as confounders in the DAG on the basis of established biological relationships. We also excluded variables that were identified as “colliders” in the DAG. Collider bias occurs when the association of 2 variables (X and Y) under investigation spuriously changes upon adjustment for a third variable (Z), which is caused by both X and Y. As an example, we did not include history of cardiovascular disease in our DAG model, because it is influenced (directly or indirectly) by both vitamin D insufficiency and IMT.
We also tested an alternative approach and included in the multivariable model all covariates with P <.1 in unadjusted comparisons; age, sex, and race were forced into the model. In the final model for the outcome of cIMT, we additionally included corrected calcium, alkaline phosphatase, PTH, and 1,25-OH vitamin D levels to determine whether the association between vitamin D insufficiency and cIMT would be independent of bone-related mineral factors.
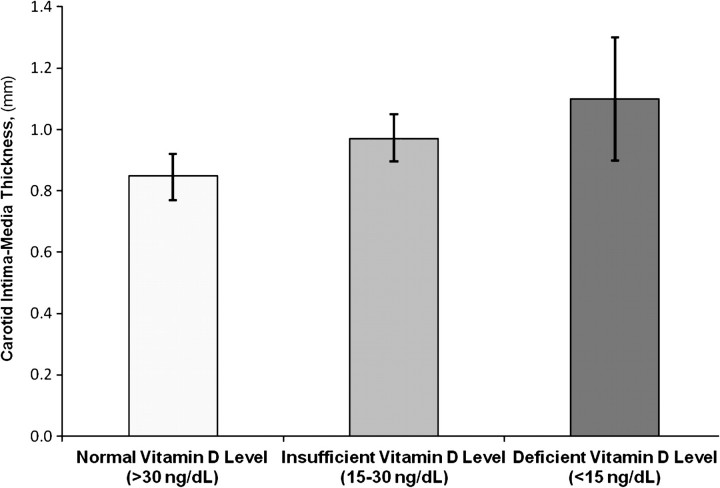
Adjusted IMT levels in Figure 1 were calculated for each vitamin D category using population marginal means from a linear regression model with dependent variable of IMT, containing all terms in the final model. Population marginal means are within-group means adjusted for other effects in the model [9].
Figure 1.
Adjusted Mean Carotid Intima-Media Thickness by Vitamin D Category*After adjustment for traditional cardiovascular risk factors and HIV-related factors, a graded relationship between vitamin D levels and carotid IMT was observed, P = .021). *Carotid intima-media thickness predicted by the multivariable linear regression model after adjustment for age, sex, race, coronary heart disease, hypertension, dyslipidemia, pack-years of smoking, NRTI duration, HIV duration, season, total cholesterol, LDL, waist to hip ratio, and calcium supplementation, corrected calcium, alkaline phosphatase, parathyroid hormone, and 1,25-OH vitamin D level. Error bars represent 95% confidence intervals.
RESULTS
The mean age of the study population (n = 139) was 45 years; 84% were male, 54% were white, and 32% were black (Table S1). Most patients (76%) were receiving ART at the time of examination. Among these individuals, 75% had suppressed HIV viral load (<1000 copies/mL) with a median CD4+ cell count of 336 cells/ mm3 (interquartile range 224–589 cells/mm3). The prevalence of cardiovascular disease and traditional risk factors, such as diabetes (6%) and kidney disease (5%), were uncommon; however, other risk factors, such as hypertension, smoking, and dyslipidemia, were present in 20%–30% of the study population.
Vitamin D insufficiency was found in 52% of participants. In unadjusted comparisons (Table S2), subjects with vitamin D insufficiency were more likely to be female, more likely to be black, and were exposed to shorter durations of ART (nonnucleoside reverse transcriptase inhibitors [NNRTIs], nucleoside reverse transcriptase inhibitors [NRTIs], and protease inhibitors [PIs]). Compared with study subjects with normal levels of vitamin D, individuals with vitamin D insufficiency also had higher BMI, glucose levels, and HDL cholesterol levels and had lower triglyceride levels. In multivariable models, black race (relative risk [RR], 2.62; 95% confidence interval [CI], 1.80– - 3.82) and higher BMI (RR, 1.25 per BMI increase of 5; 95% CI, 1.03– - 1.51) were positively associated with vitamin D insufficiency. Those individuals who received multivitamin supplementation were less likely to be vitamin D insufficient (RR, .70; 95% CI, 0.52–0 - .95). Compared with individuals who did not receive NNRTIs, subjects who used NNRTIs for <6 months were 2.5 times more likely to have vitamin D insufficiency. However, the risk of vitamin D insufficiency associated with NNRTI exposure did not extend beyond the 6-month period. Female sex, lipid and glucose levels, and exposure to PIs were not associated with vitamin D insufficiency in multivariable models.
In multivariable linear regression models, vitamin D insufficiency was associated with higher mean cIMT levels (Table S3). In Model 2, which included age, sex, race, HIV viral load, CD4+ cell count, duration of NNRTI therapy, duration of PI therapy, duration of NRTI therapy, LDL level, HDL level, serum glucose level, and pack-years of smoking, cIMT was 0.13 mm greater in those with vitamin D insufficiency, compared with cIMT for those with normal vitamin D status. In Model 3, which included covariates with a P < .1 in unadjusted models of cIMT, results were nearly identical between groups. This association remained significant despite further adjustment for bone-related mineral factors. As a sensitivity analysis, we constructed a more parsimonious model that excluded variables with P values >.1; this model yielded results similar to those of the primary multivariable model reported in Table S3. Next, we examined whether there was a graded, independent association between vitamin D status and mean cIMT. We found that the mean cIMT increased in a stepwise manner in those individuals with vitamin D insufficiency and deficiency after adjustment for all of the aforementioned variables (P = .021; Figure 1).
DISCUSSION
To our knowledge, this study is the first to report the association between vitamin D status and atherosclerotic vascular disease, measured by cIMT, in HIV-infected persons. We found that vitamin D insufficiency was common, and it was significantly associated with cIMT independent of traditional and HIV-related risk factors.
Our study adds to previous reports of vitamin D insufficiency in HIV-infected persons, which have also documented a high prevalence of this condition in this population [1, 10–11]. Consistent with earlier research, our findings indicated that vitamin D insufficiency was common in this ethnically diverse study population, affecting over half of the participants. Previous studies involving HIV-infected persons have also identified black race and NNRTI exposure as significant risk factors for vitamin D deficiency [11], whereas studies conducted in cohorts of HIV-uninfected persons have reported an inverse correlation between BMI and vitamin D level [12]. In our study, we found that risk factors for vitamin D insufficiency included black race and higher BMI; additionally, we found that vitamin D insufficiency in our cohort may be associated with short-term exposure to NNRTIs for <6 months, which is a finding that will need to be re-evaluated in other cohorts with longer NNRTI exposure. Unfortunately, we were not able to examine the effect of specific drugs (such as efavirenz) on vitamin D insufficiency. The effect of NNRTI over time may depend on the proportion and duration of treatment of individuals with specific NNRTI agents, such as efavirenz and nevirapine; unfortunately, we do not have this data available in our cohort, but we hope to evaluate this in future studies. Additional work to identify the mechanisms underlying these associations is needed to enhance the safe administration of these drugs.
cIMT is a marker of atherosclerosis and a strong predictor of future clinical events. We found that HIV-infected persons with vitamin D insufficiency had a mean cIMT that was 0.13 mm greater than the mean cIMT for those with normal vitamin D levels, even after extensive risk factor adjustment. These differences in cIMT may carry important cardiovascular risk implications, because in the general population, the adjusted relative risk of stroke is increased by 18% and the risk of myocardial infarction is increased by 15% per 0.10 mm increase in cIMT [13]. The addition of vitamin D to the list of risk factors for atherosclerosis may also have potential clinical applications. Although risk factors, such as elevated lipid levels and inflammation, are difficult to treat in HIV-infected persons, vitamin D insufficiency is a readily modifiable risk factor. Vitamin D insufficiency can be diagnosed using laboratory testing that is already widely available, and it is remediable with high-dose exogenous supplementation. Although these findings need to be replicated prospectively in a larger cohort of HIV-infected persons, they provide evidence to support a study of vitamin D supplementation to reduce cardiovascular risk in HIV-infected persons.
In summary, we observed an independent association between vitamin D level and carotid artery atherosclerosis. Although this investigation was limited by its cross-sectional study design, these findings provide the basis for future studies that prospectively examine the risk of clinical cardiovascular disease associated with vitamin D status over time and the effects of high-dose vitamin D supplementation on cIMT.
Supplementary Material
Supplementary materials are available at Clinical Infectious Diseases online (http://www.oxfordjournals.org/our_journals/cid/).
Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author.
Acknowledgments
Financial support. The National Institutes of Health (K23DK080645-01A1, K23AI65244, K24AI069994, K23AI066885, R01HL095130), the Center for AIDS Research at the University of California–San Francisco (UCSF) (P30 AI027763), the UCSF Clinical and Translational Science Institute (UL1 RR024131-01), and the National Center for Research Resources (KL2 RR024130).
Potential conflicts of interest. All authors: no conflicts.
References
- 1.Rosenvinge MM, Gedela K, Copas A, et al. Tenofovir-linked hyperparathyroidism is independently associated with the presence of vitamin D deficiency. J Acquir Immune Defic Syndr. 2010 doi: 10.1097/qai.0b013e3181caebaa. [DOI] [PubMed] [Google Scholar]
- 2.Lo JC, Kazemi MR, Hsue PY, et al. The relationship between nucleoside analogue treatment duration, insulin resistance, and fasting arterialized lactate level in patients with HIV infection. Clin Infect Dis. 2005;41:1335–1340. doi: 10.1086/496981. [DOI] [PubMed] [Google Scholar]
- 3.Hsue PY, Hunt PW, Sinclair E, et al. Increased carotid intima-media thickness in HIV patients is associated with increased cytomegalovirus-specific T-cell responses. AIDS. 2006;20:2275–2283. doi: 10.1097/QAD.0b013e3280108704. [DOI] [PubMed] [Google Scholar]
- 4.Chambless LE, Heiss G, Folsom AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987–1993. Am J Epidemiol. 1997;146:483–494. doi: 10.1093/oxfordjournals.aje.a009302. [DOI] [PubMed] [Google Scholar]
- 5.K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003;42(4 Suppl 3):S1–201. [PubMed] [Google Scholar]
- 6.Lumley T, Kronmal RA, Ma S. Relative risk regression in medical research: models, contrasts, estimators and algorithms. Seattle, WA: University of Washington, 2006. Biostatistics Working Paper Series, paper 293; . http://wwwbepresscom/uwbiostat/paper293. Accessed 19 July 2006. [Google Scholar]
- 7.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 8.Shrier I, Platt RW. Reducing bias through directed acyclic graphs. BMC Med Res Methodol. 2008;8:70. doi: 10.1186/1471-2288-8-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Searle S, Speed F, Milliken G. Populations marginal means in the linear model: an alternative to least squares means. Am Statist. 1980;34:216–221. [Google Scholar]
- 10.Rodriguez M, Daniels B, Gunawardene S, Robbins GK. High frequency of vitamin D deficiency in ambulatory HIV-positive patients. AIDS Res Hum Retroviruses. 2009;25:9–14. doi: 10.1089/aid.2008.0183. [DOI] [PubMed] [Google Scholar]
- 11.Van Den Bout-Van Den Beukel CJ, Fievez L, Michels M, et al. Vitamin D deficiency among HIV type 1-infected individuals in the Netherlands: effects of antiretroviral therapy. AIDS Res Hum Retroviruses. 2008;24:1375–1382. doi: 10.1089/aid.2008.0058. [DOI] [PubMed] [Google Scholar]
- 12.Melamed ML, Michos ED, Post W, Astor B. 25-hydroxyvitamin D levels and the risk of mortality in the general population. Arch Intern Med. 2008;168:1629–1637. doi: 10.1001/archinte.168.15.1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115:459–467. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.