Abstract
Hospital-acquired pneumonia represents one of the most difficult treatment challenges in infectious diseases. Many studies suggest that the timely administration of appropriate, pathogen-directed therapy can be lifesaving. Because results of culture and antimicrobial susceptibility testing can take 48 h or longer, physicians currently rely on clinical, epidemiological, and demographic factors to assist with the choice of empiric therapy for antibiotic-resistant pathogens. At present, a number of rapid molecular tests are being developed that identify pathogens and the presence of genetic determinants of antimicrobial resistance (eg, GeneXpert [Cepheid], ResPlex [Qiagen], FilmArray [Idaho Technologies], and Microarray [Check-Points]). In this review, the potential impact that molecular diagnostics has to identify and characterize pathogens that cause hospital-acquired bacterial pneumonia at an early stage is examined. In addition, a perspective on a novel technology, polymerase chain reaction followed by electrospray ionization mass spectrometry, is presented, and its prospective use in the diagnosis of pneumonia is also discussed. The complexities of the pulmonary microbiome represent a novel challenge to clinicians, but many questions still remain even as these technologies improve.
THE DIFFICULTIES OF TREATING HOSPITAL-ACQUIRED PNEUMONIA
Acute bacterial pneumonia in hospitalized patients remains one of the most serious infections that physicians treat. Hospital-acquired pneumonia (HAP) is the second most common nosocomial infection and accounts for ∼25% of all infections in the intensive care unit. According to the American Thoracic Society (ATS) and Infectious Diseases Society of America (IDSA), HAP occurs at a rate of 5–10 cases per 1,000 hospital admissions, with the incidence increasing by as much as 6–20-fold among mechanically ventilated patients [1]. Although the incidence of HAP varies depending on how each study defines this entity, ATS estimates that HAP accounts for >50% of the antibiotics prescribed [1–4]. Despite significant advances in antimicrobial chemotherapy (ie, the introduction of very potent antibiotics), patient support services, and radiological imaging, HAP still carries considerable morbidity and mortality (range, 25%–50%), and approximately one-half of all HAP-related deaths are directly attributable to pneumonia [2–4]. The microbiological identification of the pathogen lies at the center of this problem.
Physicians struggle to determine the true microbial etiology of HAP, especially in patients hospitalized for >7 days (ie, late onset HAP). Conventional diagnosis is based on microbial culture, a time-consuming and often times an inaccurate process. Clinicians rely on sputum samples obtained at the bedside, endotracheal aspirates, or quantitative cultures obtained by protected specimen brush or by bronchoalveolar lavage [1]. Even after culture data are known, physicians are uncertain about the cause of the disease. Are the pathogens colonizers or causing infection? How does one best decide in the presence of fever, infiltrate, and leukocytosis? To illustrate, Streptococcus pneumoniae can be cultured from the upper respiratory tract in up to 68% of children and 15% of adults in the absence of respiratory tract infection [5]. Clinicians recognize that the outcome of pneumonia depends on the complex interplay of factors such as (1) delay in antimicrobial therapy (a major risk factor in mortality); (2) diversity of the patient population; (3) comorbidities and immune status of the host; (4) virulence of the bacteria causing the infection; (5) inflammatory responses in the lung; and (6) the concomitant presence of a viral pathogen [6–11]. The choice, timing, duration, and activity of antibiotics (ie, process of care) also significantly impact the outcome of patients being treated for pneumonia [12]. Correctly identifying and appropriately treating HAP is essential, as mortality is high and there is an association between successful outcome and the adequacy of therapy [4, 12]. Studies show that failing to deliver appropriate, pathogen-directed therapy for pneumonia in a timely manner results in high morbidity and mortality [7].
Risk factors that clinicians should consider when suspecting antibiotic-resistant or multidrug-resistant (MDR) pathogens that cause HAP are summarized in Table 1 [1, 4]. In the case of HAP, MDR pathogens are defined as bacteria that are resistant to ≥3 different classes of antibiotics [1]. The antibiotics that are usually recommended for the empiric treatment of HAP when resistant Gram-negative pathogens are suspected include ureidopenicillins (piperacillin), extended-spectrum cephalosporins (eg, ceftazidime or cefepime), aminoglycosides (gentamicin, tobramycin, or amikacin), antipseudomonal quinolones (ciprofloxacin or levofloxacin), β-lactam/β-lactamase inhibitor combinations (eg, piperacillin/tazobactam), and carbapenems (imipenem, meropenem, or doripenem). If methicillin-resistant Staphylococcus aureus (MRSA) is suspected, then linezolid or vancomycin can be used [4]. Despite our best efforts at understanding the mechanism of action and appropriate use of these agents, questions still remain as to which is the best empiric antibiotic or best empiric combination of antibiotics for treatment. The reason for this uncertainty largely depends on the identity and resistance phenotype of the pathogen. At best, clinicians can predict the pathogens causing HAP 80%–90% of the time [4].
Table 1.
Risk Factors for Antibiotic-Resistant Pathogens in Hospital-Acquired Pneumonia
| Risk factors |
| Antimicrobial therapy in preceding 90 d |
| Extremes of age (<2 years old or >65 years old) |
| Alcohol use |
| Previous (<90 d) or current (>2 d) hospitalization |
| High frequency of antibiotic resistance in the hospital unit or community |
| Day care or long-term care |
| Home antibiotic therapy |
| Chronic dialysis within 30 d |
| Home wound care |
| Family member infected with multidrug-resistant pathogen |
| Immunosuppressive disease and/or therapy |
| Entotracheal intubation |
| High gastric pH |
| Co-existing cardiac pulmonary or renal insufficiency |
| Postoperative care (and age >70 years) after abdominal or thoracic surgery |
| Dependant functional status |
Recently, the IDSA highlighted a group of drug-resistant pathogens that impact the choice of therapy. These so-called ESKAPE pathogens, represented by Enterococcus faecium, S. aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter spp., are major problems in U.S. hospitals [13–15]. In general, clinicians become very concerned when faced with ESKAPE pathogens as the cause of HAP because treatment options can be limited due to antibiotic resistance. In the case of K. pneumoniae and Escherichia coli, the fear of resistance to extended-spectrum cephalosporins as a result of production of extended-spectrum β-lactamases (ESBLs) or by expression of a plasmid or chromosomally encoded AmpC cephalosporinase requires that clinicians use carbapenems if a β-lactam regimen is considered [16, 17]. Regrettably, even the use of carbapenems is threatened by the emergence of carbapenem resistance mediated by loss of outer membrane proteins (porins), efflux pumps, or carbapenemases [18]. These carbapenemases undermine even these last-line agents [19–26]. In these extreme cases, physicians use polymyxins (ie, polymyxin B or colistin) in desperation [27–31]. For staphylococci, resistance to all β-lactams as a result of the MRSA phenotype limits therapy to vancomycin or linezolid (daptomycin, tigecycline, and streptogramins are not approved for the treatment of HAP due to MRSA). The appearance of S. aureus with intermediate susceptibility to vancomycin [32] or full resistance to vancomycin is manifested by the acquisition of the same genetic elements that are responsible for the vancomycin-resistant phenotype in the Enterococcus spp. (VanA or VanB) and is an emerging threat [33–37]. Recently, resistance even to linezolid has been reported [38–48]. Therefore, real-time assessment of these resistant pathogens is urgently needed [49].
A RATIONALE FOR RAPID DIAGNOSIS
Given these considerations, the rapid determination of the bacterial etiology of HAP is critical. Despite the enormous clinical challenges that are present, the development and optimization of a quick molecular assay that can be performed on properly obtained lower respiratory tract samples offers the opportunity for increased sensitivity and specificity of the diagnosis and improved outcomes. To achieve this goal, the diagnostic method must employ robust technology that provides highly accurate and reproducible pathogen detection in an assay format that is easy to perform in a routine clinical laboratory.
Automated systems that are used to identify microorganisms cultured from respiratory tract samples were introduced into clinical microbiology laboratories in the 1970s [50]. Currently, clinical laboratories use the MicroScan WalkAway (Siemens Healthcare Diagnostics), the VITEK 1 and VITEK 2 Advanced Expert system (bioMérieux), and the Phoenix Automated Microbiology system (BD Diagnostic Systems). Automated susceptibility testing systems can require at least 48 h to yield a result. Unfortunately, these conventional methods can also be inaccurate when testing susceptibility to certain antibiotics [51–54]. This inaccuracy can have serious implications on the interpretation of susceptibility tests [55, 56]. Select examples of this are (1) detection of carbapenem resistance mediated by Klebsiella pneumoniae carbapenemases (KPCs) [19]; (2) ESBL and cephalosporinase detection [55, 57–59]; and (3) testing of some β-lactams against P. aeruginosa [54].
In response to this problem, a number of molecular assays are being developed to decrease the detection time of pathogens. The basis for most molecular assays includes polymerase chain reaction (PCR, which amplifies DNA) or reverse-transcription PCR (RT-PCR) and nucleic-acid-sequence-based amplification. Many molecular assays target the bacterial DNA of 16S ribosomal RNA (rRNA) genes or 16S–23S rRNA gene spacer regions [60]. These DNA segments contain variable ribosomal coding sequences that confer genus and species information and are used to identify bacteria. Moreover, variable sequences are flanked by highly conserved DNA that permit universal amplification of the targets, utilizing a limited primer set. The basis of these nucleic-acid-based assays requires the genes and/or products sought to be unique, so the probe used for detection must be sensitive and specific and the specimen needs to possess a sufficient number of bacteria. A list of the methods to be discussed herein is offered in Table 2.
Table 2.
Summary of Selected Molecular Diagnostic Tests Discussed Here and Their Applications
| Commercial kit/molecular assay (manufacturer) | Advantages | Application to bacterial pneumonia and/or point-of-care testing |
| GeneXpert System (Cepheid) | Detects MRSA in 1 h in blood cultures and wound swabs | Undetermined |
| AccuProbe (Gen-Probe) | Detects Staphylococcus aureus, Streptococcus pneumoniae, Mycoplasma pneumoniae, and Legionella pneumophila | Mostly for point-of-care L. pneumophila testing |
| GeneOhm (Becton-Dickinson) | Detects MRSA, MSSA, and CoNS | Undetermined |
| ResPlex and StaphPlex (Qiagen) | Detects S. pneumoniae, Neisseria meningitidis, Haemophilus influenzae, L. pneumophila, M. pneumoniae, Chlamydophila pneumonia, and S.aureus | Yes, but large clinical trials are needed for point-of-care S. aureus testing |
| Light Cycler (Roche) | Detects MRSA | Undetermined |
| MALDI-TOF MS/Autoflex II (Bruker Daltonic) | Protein-based assays with broad microbiological applicability | Undetermined |
| FilmArray systems (Idaho Technologies) | Detects Bortedella pertussis, L. pneumophila, C. pneumoniae, and M. pneumoniae | Undetermined |
| Check KPC/ESBL microarray (Check-Points) | Detects β-lactamase resistance genes conferring resistance to cephalosporins and carbapenems in 7–8 h | Undetermined |
| T5000 and PLEX-ID PCR/ESI-MS Biosensors (Abbott Molecular, Inc.) | Multiple species detected and typed and resistance genes mapped (gyrA, parC, mecA, and blaKPC) | Undetermined |
NOTE. CoNS, coagulase-negative staphylococci; ESBL, extended-spectrum β-lactamase; KPC, Klebsiella pneumoniae carbapenemase; MALDI-TOF MS, matrix-assisted laser desorption ionization time-of-flight mass spectrometry; MRSA, methicillin-resistant S. aureus; MSSA, methicillin-susceptible S. aureus; PCR/ESI-MS, polymerase chain reaction followed by electrospray ionization mass spectrometry.
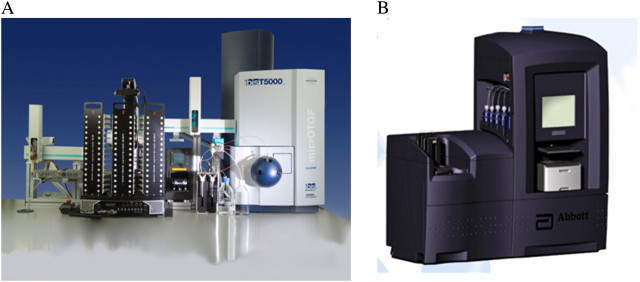
Thus far, most of the development has focused on detecting S. aureus, especially MRSA. Representative assays to detect MRSA include the GeneXpert system (Cepheid), AccuProbe (Gen-Probe), the GeneOhm MRSA assay (Becton-Dickinson), the StaphPlex and ResPlex systems (Qiagen), the Light Cycler (Roche), matrix-assisted laser desorption ionization time-of-flight (MALDI-TOF) mass spectrometry (MS), and FilmArray systems (Idaho Technologies). The most recent molecular assay to be introduced is the T5000 Biosensor and the next-generation PLEX-ID Biosensor (Ibis Biosciences, a subsidiary of Abbott Molecular, Inc.). The platform in the T5000 and PLEX-ID combines PCR with highly accurate electrospay ionizatiion mass spectrometry (PCR/ESI-MS) to detect species-specific amplicons [61–64] (Figure 1).
Figure 1.
T5000 biosensor (A) and PLEX-ID biosensor and (B) (Ibis Biosciences, a subsidiary of Abbott Molecular, Inc.).
RAPID MOLECULAR METHODS
GeneXpert
Cepheid's GeneXpert system can detect MRSA from an isolated colony in a little less than 1 h. This is an automated microfluidic procedure that depends on real-time PCR [65, 66]. In the original study by Huletsky et al [65], a real-time PCR assay was first developed to target DNA sequences in the region of orfX where the staphylococcal cassette chromosome mec (SCCmec) integrates into the S. aureus chromosome [67, 68]. In 2007, a new real-time PCR MRSA assay that also targeted DNA sequences in the chromosomal orfX-SCCmec junction became available [66]. With this latter assay, GeneXpert exhibited sensitivities of 95% and 97% for detecting MRSA from nasal and groin/perineum specimens, respectively. A recent multicenter study showed that the GeneXpert system yielded a sensitivity and specificity of 94.3% and 93.2%, respectively, when compared with CHROMagar MRSA plates [69]. The GeneXpert system has now advanced to detect S. aureus in blood cultures [70] and wound swabs [71, 72]. To date, there are no reports yet of the use of this method in the diagnosis of MRSA pneumonia.
AccuProbe
AccuProbe (Gen-Probe) uses a chemiluminescent DNA probe to detect the rRNA and nucleic acids of the target organisms. This nucleic acid hybridization assay is based on the ability of complementary nucleic acid strands to come together to form stable double-stranded complexes. The use of multicopy rRNA as the target molecule also increases the sensitivity and specificity of the assay. At present, many products and applications are available for clinical use, such as AccuProbe assays for human immunodeficiency virus and hepatitis C virus identification and quantification and detection assays for Chlamydophila pneumoniae, Neisseria gonorrhoeae, group B streptococci, Listeria monocytogenes, and Campylobacter spp. (see http://www.gen-probe.com). With regard to respiratory tract infections, assays for identification of influenza A virus, influenza B virus, parainfluenza viruses, human metapneumovirus, respiratory syncytial virus, fungi (Blastomyces dermatitidis, Coccidioides immitis, and Histoplasma capsulatum), mycobacteria, group A streptococci, S. pneumoniae, S. aureus, Legionella spp., Mycoplasma spp., Chlamydophila spp., and Haemophilus influenzae type B are commercially available, but not in the United States.
In contrast to the GeneXpert system, AccuProbe can be used to readily identify S. aureus, S. pneumoniae, Mycoplasma pneumoniae, and Legionella pneumophila in respiratory tract samples from patients with pneumonia. In the case of S. aureus, the sensitivity and specificity of the AccuProbe system are reported as 100% and 96%, respectively. In addition, there is good agreement between quantitative cultures and probes in 96.3% of cases. With the AccuProbe assay, there may be some difficulties in diagnosing infection with atypical pneumococci with sputum samples compared with diagnosis using PCR for the pneumolysin gene, but these setbacks are uncommon [73–76].
BD GeneOhm StaphSR and BD GeneOhm MRSA Assays
The BD GeneOhm MRSA assay (Becton-Dickinson) is a qualitative in vitro diagnostic test for the rapid detection of MRSA. The assay can be performed in <2 h (in many instances, it can be performed in 1.5 h) and can also be performed directly from clinical specimens [77–79]. In principle, these assays use rapid nucleic acid tests to differentiate between coagulase-negative staphylococci, methicillin-susceptible S. aureus (MSSA), and MRSA. Similar to GeneXpert, the assay uses a multiplex real-time PCR method to amplify a specific target sequence of S. aureus near the SCCmec insertion site and the orfX junction gene [65]. The assay works well in a low-prevalence setting to detect MRSA from nasal, skin, and throat samples [80]. The ability of this assay to detect MRSA in all situations is still under evaluation [81]. In one study, the assay failed to detect the predominant Australian nosocomial clone (AUS2/3 clone; strain type 239-MRSA-III) and a community-acquired clone prevalent in eastern Australia (South West Pacific clone; strain type 30-MRSA-IV) [82]. Nevertheless, the ability to differentiate bloodstream infection caused by MSSA and MRSA from that caused by other Gram-positive cocci is a major advantage [83]. Although reports have been published regarding the ability of this test to detect MRSA in nasal and groin samples [71, 72], studies are still needed to determine and validate whether this assay is effective in the diagnosis of MRSA pneumonia.
ResPlex and StaphPlex
Using microarray technology, Qiagen developed a series of assays—the ResPlex and StaphPlex panels. These panels incorporate multiplex PCR reactions that allow parallel detection of bacterial and viral targets in a single reaction (hence, they are called microarrays). The ResPlex assay amplifies and detects gene-specific DNA sequences for S. pneumoniae (lytA), Neisseria meningitidis (ctrA), encapsulated or nonencapsulated H. influenzae (bexA and ompP2), L. pneumophila (mip), M. pneumoniae (adenosine triphosphatase), and C. pneumoniae (ompA) [84, 85]. The StaphPlex panel allows identification of MRSA by amplifying and detecting 18 gene targets simultaneously [86]. These primers target information-rich genes in staphylococci such as tuf for coagulase-negative staphylococci, nuc for S. aureus, Panton-Valentine leukocidin (PVL) genes, and antimicrobial resistance determinants of staphylococci (mecA, SCCmecI-IV, aacA, ermA, ermB, tetM, and tetK) [86]. A similar system was developed and used to screen for MRSA in nasal swabs [87]. While the StaphPlex offers more robust features, the ResPlex assay has clear potential to be used in the determination of the etiology of HAP [88].
Roche LightCycler MRSA and SeptiFast MecA Tests
The LightCycler MRSA Advanced test (Roche) is a qualitative in vitro diagnostic test for the direct detection of nasal colonization by MRSA to aid in the prevention and control of MRSA infections in health care settings. The test is performed on the LightCycler 2.0 instrument with nasal swab specimens from patients. The method uses swab extraction and mechanical lysis for specimen preparation, followed by PCR for the amplification of MRSA DNA and fluorogenic target-specific hybridization probes for the detection of the amplified DNA. The LightCycler MRSA Advanced test is designated for nasal specimens, and the LightCycler SeptiFast MecA test is used for detection of MRSA in bloodstream infections.
Originally, a 188-bp fragment within the mecA gene and a 178-bp fragment within the S. aureus–specific Sa442 gene were used for amplification. In the current version of this test, part of the ITS region (internal transcribed spacer between 16S and 23S gene) is targeted [89]. The LightCycler MRSA Advanced test (nasal detection) is designed to aid in the prevention and control of MRSA infections in health-care settings. The SeptiFast test may be useful in determining bloodstream infections due to MRSA. Recent evidence indicates that the latter test may prove better than the conventional test currently performed in the laboratory in cases of infective endocarditis in patients treated with antibiotics before admission [90]. To date, the application of these methods to determine whether MRSA is the causative agent of pneumonia is still forthcoming.
MALDI-TOF MS
MALDI-TOF MS is a protein/peptide-based diagnostic MS method that can be used to assist with the rapid and accurate identification of pathogens [91–93]. Because this method successfully detects pathogens in blood cultures (in the best set of analyses where 125 Gram-negative isolates were tested, there was correct identification in 94%), there is hope that it can be applied to HAP. In a recent article in Clinical Infectious Diseases [93], ≥1,600 clinical isolates were studied, and identification by MALDI-TOF MS was compared with that by conventional culture methods (ie, Gram stain and Vitek or Analytical Profile Index testing). MALDI-TOF MS demonstrated a sensitivity of 95% and specificity of 84.1% of the samples at the species level. Seng and colleagues [93] found that it takes ∼6 min per isolate for identification, and the cost is 22%–32% less than that of current methods of identification. In most cases, absence of identification or erroneous identification was due to construction of a less complete database (MALDI-TOF MS requires ∼10 reference samples in the database to be accurate). When the investigators looked at the actual performance of MALDI-TOF MS compared with that of conventional methods, MALDI-TOF MS required less investment of time and energy, was also highly specific, and did not increase the cost of identifying pathogens. So far, MALDI-TOF has not been tested as a detector of pathogens in sputum or as a point-of-care diagnostic instrument.
An interesting feature of MALDI-TOF MS is its ability to identify PVL [91]. However, limitations to MALDI-TOF MS exist. The large number of different staphylococci—either S. aureus or coagulase-negative staphylococi—interferes with the sensitivity and specificity of this assay [92, 93]. Moreover, the identification of viridans streptococci also presents significant problems. More relevant to the application in HAP is the clear limitation of MALDI-TOF MS in correctly identifying a mixture of species. In the study by La Scola and Raoult [92], when a mixture of pathogens was presented, only 1 species was correctly identified, and false identification occurred. The performance characteristics of MALDI-TOF MS will have to be carefully monitored because sputum samples from patients with HAP can have staphylococci, streptococci, and a mixture of Gram-negative organisms.
Molecular Beacons
Molecular beacons are single-stranded oligonucleotide hybridization probes that form a hairpin-type stem-and-loop structure. As single-stranded probes, molecular beacons are extraordinarily sensitive and specific and are suitable for single-nucleotide allele discrimination. The target sequence is recognized by the sequence in the loop; the stem is formed by the annealing of complementary arm sequences that are located on either side of the probe sequence. A quencher is covalently linked to the end of one arm, and a fluorophore is covalently linked to the end of the other arm. In free solution, the molecular beacon does not emit light because the quencher is in proximity to the fluorophore. However, when they hybridize to a nucleic acid strand containing a target sequence, the fluorphore and quencher are separated, resulting in bright fluorescence. Thus, molecular beacons are considered to be molecular switches that turn on when on their target and are off when in solution.
Molecular beacons have now been designed for the identification of >110 different pathogens. Chakravorty et al [60] recently developed mismatch-tolerant molecular beacons. These so-called sloppy beacons enhance the diagnostic potential of the assay by allowing less stringent detection of the molecular target and present an important advance. The major bacterial pathogens (ie, S. aureus, S. pneumoniae, and P. aeruginosa) are detected with this method.
In clinical specimens, S. pneumoniae (lytA gene), H. influenzae (16S rRNA), M. pneumoniae (16S rRNA), C. pneumoniae (16S rRNA), L. pneumophila (mip gene), and Streptococcus pyogenes (16S rRNA) are readily detected by molecular beacons [94]. The reported sensitivity and specificity of this real-time PCR assay relative to conventional cultures were 96.2% and 93.2% for S. pneumoniae, 95.8% and 95.4% for H. influenzae, and 100% and 100% for S. pyogenes, respectively. Clinical experience with molecular beacons to detect resistant pathogens is still required in cases of HAP.
FilmArray System
Idaho Technology is developing the FilmArray system to assist in rapid molecular diagnostics. The FilmArray system is based on microfluidics technology and promises to identify ≥30 pathogens in ∼60 min. This method combines RT-PCR with a uniquely designed lab-in-a-pouch system: a benchtop instrument performs all the steps of the assay in an automated fashion, from nucleic acid extraction to nested multiplex PCR and data analysis. By using nested multiplex PCR, the targeting of conserved housekeeping genes can accurately detect bacteria. The completely automated assay takes <60 min to run.
Primers are designed to be broad-range and are based on alignments of housekeeping gene targets (ie, rpoB, gyrB, and ompA). These outer primers target their domains by use of degenerate nucleotides to provide cross-species recognition. Next, species-specific inner primers are created and are placed in locations where the 3′ end includes a characteristic nucleic acid signature that is conserved among isolates of the same, but not different, species. Currently, the FilmArray system detects the following bacterial species in respiratory tract samples: Bordetella pertussis, C. pneumoniae, and M. pneumoniae. A wider clinical application of this technology is still forthcoming (hence, there have been no studies published on the use of this technology to detect resistant Gram-negative bacteria). This approach comprises a potential point-of-care diagnostic tool because the support system to perform these assays is readily mobile and inexpensive.
Microarray Technologies Detecting β-Lactamases
As shown above, microarrays possess a high multiplexing capacity and can be used for detecting an unlimited number of genes within a reaction mixture. Recently, microarrays have been applied to detect different β-lactamase (bla) genes that are present in an isolate. The Check-Points Check KPC/ESBL microarray system uses a method called multiplex ligation detection reaction. In brief, a series of specially designed DNA probes are used that assist with PCR amplification. Next, the PCR products are detected by hybridization to a low-density DNA microarray. When there is hybridization, detection is accomplished using a biotin label incorporated in one of the PCR primers. Although this method does not identify the pathogen at the source of the infection (ie, it cannot yet be used as a point-of-care test or for a clinical specimen), this microarray can assist clinicians in directing specific antimicrobial therapy once the resistance background of the pathogen is determined. Moreover, the assay takes 7–8 hours (1 typical working day). Endimiani and colleagues [95] evaluated the ability of this microarray system in the detection and identification of bla genes belonging to the TEM, SHV, CTX-M, and KPC β-lactamases. This group reported a sensitivity and specificity of 96.4%–100% when the test was performed in a blinded fashion on previously characterized isolates. In a complementary analysis performed by Naas et al [96], Check KPC/ESBL microarray was also used prospectively on clinical samples obtained directly from the microbiology laboratory collected in a 3-month period and demonstrated a similar sensitivity and specificity (up to 100%). Currently, this assay is being further evaluated to detect other β-lactamase genes such as plasmid-mediated AmpCs and NDM-1 metallo-β-lactamase. To date, the use of this assay in assisting with antibiotic choices in cases of HAP due to antibiotic-resistant gram-negative pathogens remains to be studied.
PCR Followed by ElectroSpray Ionization MS (PCR/ESI-MS)
PCR/ESI-MS uses a rapid and highly accurate multilocus sequencing typing (MLST) method that allows (1) identification of a very wide and diverse range of pathogens; (2) determination of their genetic relatedness (clonality) compared with other analyzed strains; (3) identification of virulence factors; and (4) determination of resistance genotypes [62].
PCR/ESI-MS employs a robust bioinformatics infrastructure that contains comprehensive gene sequence data [63, 64, 97]. With this database, multiple PCR amplification primers are designed to amplify selected areas of the bacterial genome. These PCR primers are broad-range and target ribosomal subunits (ribosomal primers; 16S and 23S), unique housekeeping genes, or other signature sequences from bacteria. In addition, by selecting regions of variability, the primers yield 60–140-bp amplification products that are information-rich. Next, the amplified double-stranded DNA is desalted and heated to separate the strands, and each strand is injected into a highly accurate mass spectrometer. The mass of the single-stranded DNA is determined in 30 seconds. An accurate sequence analysis is deduced from the mass of the nucleotides and the DNA sequence is unambiguously determined and compared with known DNA sequences that are present in microbial genomes (http://www.ncbi.nlm.nih.gov/genomes/lproks.cgi). When primers are strategically designed, ∼6 PCR reactions and gene sequences (http://www.ncbi.nlm.nih.gov) can identify almost all bacteria at a species level [98].
By means of a mathematical process called triangulation, microorganisms with specific DNA sequences are further distinguished using precise DNA sequence information. An added advantage to this approach is that primers can be designed to also identify previously unknown members of a species—this capability was demonstrated in the recent influenza pandemic [61]. Information from several PCR/ESI-MS reactions triangulates the identities of the organisms that are present. None of the primers are designed to be specific for any one microorganism, but instead the primers are designed to cover many pathogens by use of a nested-coverage approach. This enables identification of any bacterial species and even previously unknown organisms with a single test [99–103].
Clinical Experience With PCR/ESI-MS
The first early study with the T5000 (Ibis Biosciences) involved an outbreak of respiratory tract infection among recruits at a military base in San Diego, California, during the years 2002–2003. Ecker and colleagues [98] used the T5000 platform to identify the responsible pathogens and to determine the pathogen-strain genotype. Hundreds of recruits became ill; 160 patients in this outbreak were hospitalized, and 1 death was reported. By using specific primers targeted to 23S ribosomal DNA, 3 predominant pathogens were identified: H. influenzae, N. meningititis, and S. pyogenes in throat swab samples (note that in this study, isolates were examined from pure culture as well as from direct throat swabs). Interestingly, the investigators did not detect S. pneumoniae. This was a proof-of-concept study; PCR/ESI-MS was able to diagnose multiple pathogens causing respiratory tract infections.
Can one detect genes that confer resistance to antibiotics, and can one perform epidemiological analyses with PCR/ESI-MS? For this application, the target genes amplified by PCR/ESI-MS need to be specific (unique), possess genetic uniformity, and be conserved. So far, this has been applied to gyrA, parC, mecA, and blaKPC. In a study designed to test this notion in ciprofloxacin-resistant A. baumannii, performed by Hujer et al [104], 6 primer pairs for conserved genes that encode amino acids in the quinolone-resistance-determining regions of gyrA and parC of A. baumannii were evaluated. The primers used were able to identify mutations detected by PCR/ESI-MS in gyrA and parC. This PCR/ESI-MS analysis accurately correlated with susceptibility testing and sequencing results. Recently, Endimiani et al [105] used this approach to detect the carbapenemase gene, blaKPC, in K. pneumoniae with a high degree of sensitivity (100%) and specificity (100%).
Wolk et al [106], identified the presence of the mecA gene and showed very good correlation with the identification of the MRSA phenotype. Furthermore, the identification of toxin genes (ie, PVL and Toxic Shock Syndrome Toxin-1, TSST-1) by PCR/ESI-MS correlated with independent PCR analyses for the presence of these genes. Significantly, isolates were also correctly classified into genotypic groups that correlated with genetic clonal complexes, repetitive-element-based PCR patterns, or pulsed-field gel electrophoresis (PFGE) types [107]. These examples show that this diagnostic approach (ie, pathogen and resistance gene identification) could be applied to HAP.
Can this technology determine genetic relatedness? Can we use PCR/ESI-MS to track the clonal expansion of a particular strain type during a specific epidemic? This approach was reported as successful in the analysis of S. pyogenes affecting military recruits [98]; the identical streptococcal genotype was found in almost all of the samples tested. In a study performed with Acinetobacter spp., Ecker and colleagues studied 267 Acinetobacter spp. (216 clinical isolates and 51 reference strains) [108]. In this collection, 47 different A. baumannii strain types were identified. PCR/ESI-MS proved to be a significant advance compared with Multi Locus Sequence Typing (MLST), as the former was able to provide a real-time surveillance capability with assay results available in <6 h. A subsequent study by Hujer et al [104], using Acinetobacter spp.isolates obtained from the Walter Reed Army Medical Center, revealed that 16 different clonal types were present in that collection (8 major clone types). Many of the same strain types (eg, ST10, ST11, and ST14) were present in the analysis by Ecker et al [108]. Interestingly, one of these strain types (ST11) was also responsible for a case of occupational transmission of A. baumannii [109] to a nurse. So far, the distribution of strain types between military and civilian hospitals is different [110]. This understanding may change as more outbreaks are analyzed. In Ohio, Perez et al [111] showed that the T5000 biosensor was able to track an outbreak of MDR A. baumannii infection through a health care system, identify the main strain types (ST10 and ST12), and link the Ohio strain types to the European clone II.
Jacobs and colleagues [112] showed that PCR/ESI-MS could also be used to characterize S. pneumoniae isolates from serogroup 6. In this study, PCR/ESI-MS was employed to perform MLST analysis and distinguish the distribution and the origin of serotype 6C strains. Recently, Endimiani and colleagues [39] studied clonal complexes among linezolid-resistant isolates of S. aureus. The linezolid-resistant isolates of S. aureus were found to be grouped as part of clonal complex 5; USA 100 and USA 800 strain types were detected by PFGE, and ST5 was detected by MLST.
The early clinical experience with PCR/ESI-MS in the detection of S. pyogenes, S. pneumoniae, S. aureus, A. baumannii, and P. aeruginosa is promising. PCR/ESI-MS can also assist in the choice of targeted therapy by identifying genes that can confer resistance to antibiotics and can help determine the clonal relatedness of strains—an additional feature that can enhance infection control practices.
Can PCR/ESI-MS be applied to sputum samples? In one case, a sputum sample from a patient with cystic fibrosis was studied, and the T5000 detected P. aeruginosa plus multiple other potential bacterial pathogens (Chlamydophila spp., S. aureus, S. pneumoniae, and Streptomyces rimosus) [62].
WHAT DOES THIS ALL MEAN FOR US?
These technologies offer the promise of dramatically improving our ability to identify bacterial pathogens in respiratory tract specimens with much needed sensitivity. These data from such enhanced applications (ie, Check-Points or T5000 and PLEX-ID, among others) can also be electronically integrated into shared molecular databases. Clinicians and epidemiologists can access such databases to ascertain local, regional, national, and international trends. This likely will come forth as a major feature of the next-generation instruments.
Yet we must keep in mind that these new tools will not guarantee that we will always get the best samples to analyze or make correct antibiotic choices. Microbial recognition by highly sensitive rapid diagnostic methods such as these will still require good samples. Clinicians will still face difficult questions about the meaning of these results. Most relevant to the methods that detect nucleic acids is the question, does finding DNA have the same impact as recovering living pathogens? In addition, the extreme sensitivity of these assays (1 colony-forming unit) may result in simultaneous detection of multiple pathogens from clinical specimens. If this is true, what will be our new gold standard, and will this information impact therapy? In short, for unparalleled accuracy and sensitivity, are we replacing one level of ambiguity with new layers of uncertainty?
Right now, clinical trials are desperately needed to provide evidence to help us decide which methods are the best and how to apply this knowledge. Notwithstanding, we must also accept that our comprehension of the microbial and metagenomic diversity of the respiratory tract in health and disease is in its infancy. Will we be able to use this information to help us reduce morbidity and mortality and explain why patients fail to respond to antimicrobial therapy for lung infections? Or will all the information obtained by each of these methods serve to overwhelm the clinician? How will we use biomarkers to help us decide what these pathogens mean in HAP? The significance of finding bacterial DNA in the absence of a positive culture in respiratory tract specimens will surely reveal the complexities of the pulmonary microbiome. It also indicates that we do not have a strong understanding of the ecology of the airway and suffer from an inability to distinguish between infecting and colonizing organisms. The new technologies reviewed here have opened novel vistas for detecting potential pathogens. We now need to understand the clinical significance of our newfound information. Information may be power, but we should be careful what we wish for.
Acknowledgments
Financial support. This work was supported by the Veterans Affairs Merit Review Program (R. A. B.); the National Institutes of Health (grants R01-AI063517, R03-AI081036, and R01-AI072219 to R. A. B.); and the Geriatric Research Education and Clinical Center VISN 10 (R. A. B.). Dr. Perlin is supported by the National Institutes of Health.
Supplement sponsorship. This article was published as part of a supplement entitled “Workshop on Molecular Diagnostics for Respiratory Tract Infections.” The Food and Drug Administration and the Infectious Diseases Society of America sponsored the workshop. AstraZeneca Pharmaceuticals, Bio Merieux, Inc., Cepheid, Gilead Sciences, Intelligent MDX, Inc., Inverness Medical Innovations, and Roche Molecular Systems provided financial support solely for the purpose of publishing the supplement.
Potential conflicts of interest. R. A. B. is a recipient of a research grant from Pfizer and Steris Corporation and has collaborated with Ibis Biosciences and Abbott Molecular, Inc., on publications in the screening of bacterial isolates. D. S. P. receives grant support from Merck, Pfizer, Astellas, Celgene, bioMerieux, and the National Institutes of Health and serves on advisory boards for Merck, Pfizer, Astellas, and Myconostica. All other authors: no conflicts.
References
- 1.American Thoracic Society and Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 2.Esperatti M, Ferrer M, Theessen A, et al. Nosocomial pneumonia in the intensive care unit acquired by mechanically ventilated versus nonventilated patients. Am J Respir Crit Care Med. 2010;182:1533–9. doi: 10.1164/rccm.201001-0094OC. [DOI] [PubMed] [Google Scholar]
- 3.Ferrer M, Liapikou A, Valencia M, et al. Validation of the American Thoracic Society-Infectious Diseases Society of America guidelines for hospital-acquired pneumonia in the intensive care unit. Clin Infect Dis. 2010;50:945–52. doi: 10.1086/651075. [DOI] [PubMed] [Google Scholar]
- 4.Torres A, Ferrer M, Badia JR. Treatment guidelines and outcomes of hospital-acquired and ventilator-associated pneumonia. Clin Infect Dis. 2010;51(suppl 1):S48–53. doi: 10.1086/653049. [DOI] [PubMed] [Google Scholar]
- 5.Greenberg D, Broides A, Blancovich I, Peled N, Givon-Lavi N, Dagan R. Relative importance of nasopharyngeal versus oropharyngeal sampling for isolation of Streptococcus pneumoniae and Haemophilus influenzae from healthy and sick individuals varies with age. J Clin Microbiol. 2004;42:4604–9. doi: 10.1128/JCM.42.10.4604-4609.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bartlett JG, Breiman RF, Mandell LA, File TM., Jr Community-acquired pneumonia in adults: guidelines for management. The Infectious Diseases Society of America. Clin Infect Dis. 1998;26:811–38. doi: 10.1086/513953. [DOI] [PubMed] [Google Scholar]
- 7.Houck PM, Bratzler DW, Nsa W, Ma A, Bartlett JG. Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Arch Intern Med. 2004;164:637–44. doi: 10.1001/archinte.164.6.637. [DOI] [PubMed] [Google Scholar]
- 8.Mandell LA, Niederman MS. Community-acquired pneumonia. N Engl J Med. 1996;334:861. doi: 10.1056/NEJM199603283341312. [DOI] [PubMed] [Google Scholar]
- 9.Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344:665–71. doi: 10.1056/NEJM200103013440908. [DOI] [PubMed] [Google Scholar]
- 10.Mizgerd JP. Acute lower respiratory tract infection. N Engl J Med. 2008;358:716–27. doi: 10.1056/NEJMra074111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Niederman MS. Review of treatment guidelines for community-acquired pneumonia. Am J Med. 2004;117(suppl 3A):51S–7S. doi: 10.1016/j.amjmed.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 12.Iregui M, Ward S, Sherman G, Fraser VJ, Kollef MH. Clinical importance of delays in the initiation of appropriate antibiotic treatment for ventilator-associated pneumonia. Chest. 2002;122:262–8. doi: 10.1378/chest.122.1.262. [DOI] [PubMed] [Google Scholar]
- 13.Boucher HW, Talbot GH, Bradley JS, et al. Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:1–12. doi: 10.1086/595011. [DOI] [PubMed] [Google Scholar]
- 14.Rice LB. Federal funding for the study of antimicrobial resistance in nosocomial pathogens: no ESKAPE. J Infect Dis. 2008;197:1079–81. doi: 10.1086/533452. [DOI] [PubMed] [Google Scholar]
- 15.Ritchie DJ, Alexander BT, Finnegan PM. New antimicrobial agents for use in the intensive care unit. Infect Dis Clin North Am. 2009;23:665–81. doi: 10.1016/j.idc.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 16.Endimiani A, Paterson DL. Optimizing therapy for infections caused by enterobacteriaceae producing extended-spectrum beta-lactamases. Semin Respir Crit Care Med. 2007;28:646–55. doi: 10.1055/s-2007-996411. [DOI] [PubMed] [Google Scholar]
- 17.Paterson DL, Bonomo RA. Extended-spectrum beta-lactamases: a clinical update. Clin Microbiol Rev. 2005;18:657–86. doi: 10.1128/CMR.18.4.657-686.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Queenan AM, Bush K. Carbapenemases: the versatile beta-lactamases. Clin Microbiol Rev. 2007;20:440–58. doi: 10.1128/CMR.00001-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bratu S, Mooty M, Nichani S, et al. Emergence of KPC-possessing Klebsiella pneumoniae in Brooklyn, New York: epidemiology and recommendations for detection. Antimicrob Agents Chemother. 2005;49:3018–20. doi: 10.1128/AAC.49.7.3018-3020.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Endimiani A, Carias LL, Hujer AM, et al. Presence of plasmid-mediated quinolone resistance in Klebsiella pneumoniae isolates possessing blaKPC in the United States. Antimicrob Agents Chemother. 2008;52:2680–2. doi: 10.1128/AAC.00158-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nordmann P, Cuzon G, Naas T. The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria. Lancet Infect Dis. 2009;9:228–36. doi: 10.1016/S1473-3099(09)70054-4. [DOI] [PubMed] [Google Scholar]
- 22.Rice LB, Carias LL, Hutton RA, Rudin SD, Endimiani A, Bonomo RA. The KQ element, a complex genetic region conferring transferable resistance to carbapenems, aminoglycosides, and fluoroquinolones in Klebsiella pneumoniae. Antimicrob Agents Chemother. 2008;52:3427–9. doi: 10.1128/AAC.00493-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Villegas MV, Lolans K, Correa A, Kattan JN, Lopez JA, Quinn JP. First identification of Pseudomonas aeruginosa isolates producing a KPC-type carbapenem-hydrolyzing beta-lactamase. Antimicrob Agents Chemother. 2007;51:1553–5. doi: 10.1128/AAC.01405-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Woodford N, Tierno PM, Jr., Young K, et al. Outbreak of Klebsiella pneumoniae producing a new carbapenem-hydrolyzing class A beta-lactamase, KPC-3, in a New York Medical Center. Antimicrob Agents Chemother. 2004;48:4793–9. doi: 10.1128/AAC.48.12.4793-4799.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yigit H, Queenan AM, Anderson GJ, et al. Novel carbapenem-hydrolyzing beta-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrob Agents Chemother. 2001;45:1151–61. doi: 10.1128/AAC.45.4.1151-1161.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yigit H, Queenan AM, Rasheed JK, et al. Carbapenem-resistant strain of Klebsiella oxytoca harboring carbapenem-hydrolyzing beta-lactamase KPC-2. Antimicrob Agents Chemother. 2003;47:3881–9. doi: 10.1128/AAC.47.12.3881-3889.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Falagas ME, Grammatikos AP, Michalopoulos A. Potential of old-generation antibiotics to address current need for new antibiotics. Expert Rev Anti Infect Ther. 2008;6:593–600. doi: 10.1586/14787210.6.5.593. [DOI] [PubMed] [Google Scholar]
- 28.Falagas ME, Rafailidis PI, Matthaiou DK, Virtzili S, Nikita D, Michalopoulos A. Pandrug-resistant Klebsiella pneumoniae, Pseudomonas aeruginosa and Acinetobacter baumannii infections: characteristics and outcome in a series of 28 patients. Int J Antimicrob Agents. 2008;32:450–4. doi: 10.1016/j.ijantimicag.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 29.Giamarellou H, Poulakou G. Multidrug-resistant Gram-negative infections: what are the treatment options? Drugs. 2009;69:1879–901. doi: 10.2165/11315690-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 30.Michalopoulos A, Falagas ME. Colistin and polymyxin B in critical care. Crit Care Clin. 2008;24:377–91. doi: 10.1016/j.ccc.2007.12.003. x. [DOI] [PubMed] [Google Scholar]
- 31.Pappas G, Saplaoura K, Falagas ME. Current treatment of pseudomonal infections in the elderly. Drugs Aging. 2009;26:363–79. doi: 10.2165/00002512-200926050-00001. [DOI] [PubMed] [Google Scholar]
- 32.Howden BP, Davies JK, Johnson PD, Stinear TP, Grayson ML. Reduced vancomycin susceptibility in Staphylococcus aureus, including vancomycin-intermediate and heterogeneous vancomycin-intermediate strains: resistance mechanisms, laboratory detection, and clinical implications. Clin Microbiol Rev. 2010;23:99–139. doi: 10.1128/CMR.00042-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Appelbaum PC. MRSA–the tip of the iceberg. Clin Microbiol Infect. 2006;12(suppl 2):3–10. doi: 10.1111/j.1469-0691.2006.01402.x. [DOI] [PubMed] [Google Scholar]
- 34.Cosgrove SE, Carroll KC, Perl TM. Staphylococcus aureus with reduced susceptibility to vancomycin. Clin Infect Dis. 2004;39:539–45. doi: 10.1086/422458. [DOI] [PubMed] [Google Scholar]
- 35.Sievert DM, Rudrik JT, Patel JB, McDonald LC, Wilkins MJ, Hageman JC. Vancomycin-resistant Staphylococcus aureus in the United States, 2002–2006. Clin Infect Dis. 2008;46:668–74. doi: 10.1086/527392. [DOI] [PubMed] [Google Scholar]
- 36.Tenover FC, Weigel LM, Appelbaum PC, et al. Vancomycin-resistant Staphylococcus aureus isolate from a patient in Pennsylvania. Antimicrob Agents Chemother. 2004;48:275–80. doi: 10.1128/AAC.48.1.275-280.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Whitener CJ, Park SY, Browne FA, et al. Vancomycin-resistant Staphylococcus aureus in the absence of vancomycin exposure. Clin Infect Dis. 2004;38:1049–55. doi: 10.1086/382357. [DOI] [PubMed] [Google Scholar]
- 38.Brauers J, Kresken M, Hafner D, Shah PM. Surveillance of linezolid resistance in Germany, 2001–2002. Clin Microbiol Infect. 2005;11:39–46. doi: 10.1111/j.1469-0691.2004.01036.x. [DOI] [PubMed] [Google Scholar]
- 39.Endimiani A, Blackford M, Dasenbrook EC, et al. Emergence of linezolid-resistant clonal complex 5 Staphylococcus aureus with unique ribosomal mutations among cystic fibrosis patients. Antimicrob agents Chemother. 2011 doi: 10.1128/AAC.01308-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gales AC, Sader HS, Andrade SS, Lutz L, Machado A, Barth AL. Emergence of linezolid-resistant Staphylococcus aureus during treatment of pulmonary infection in a patient with cystic fibrosis. Int J Antimicrob Agents. 2006;27:300–2. doi: 10.1016/j.ijantimicag.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 41.Hill RL, Kearns AM, Nash J, et al. Linezolid-resistant ST36 methicillin-resistant Staphylococcus aureus associated with prolonged linezolid treatment in two paediatric cystic fibrosis patients. J Antimicrob Chemother. 2010;65:442–5. doi: 10.1093/jac/dkp494. [DOI] [PubMed] [Google Scholar]
- 42.Kola A, Kirschner P, Gohrbandt B, et al. An infection with linezolid-resistant S. aureus in a patient with left ventricular assist system. Scand J Infect Dis. 2007;39:463–5. doi: 10.1080/00365540601071875. [DOI] [PubMed] [Google Scholar]
- 43.Morales G, Picazo JJ, Baos E, et al. Resistance to linezolid is mediated by the cfr gene in the first report of an outbreak of linezolid-resistant Staphylococcus aureus. Clin Infect Dis. 2010;50:821–5. doi: 10.1086/650574. [DOI] [PubMed] [Google Scholar]
- 44.Peeters MJ, Sarria JC. Clinical characteristics of linezolid-resistant Staphylococcus aureus infections. Am J Med Sci. 2005;330:102–4. doi: 10.1097/00000441-200508000-00007. [DOI] [PubMed] [Google Scholar]
- 45.Pillai SK, Sakoulas G, Wennersten C, et al. Linezolid resistance in Staphylococcus aureus: characterization and stability of resistant phenotype. J Infect Dis. 2002;186:1603–7. doi: 10.1086/345368. [DOI] [PubMed] [Google Scholar]
- 46.Roberts SM, Freeman AF, Harrington SM, Holland SM, Murray PR, Zelazny AM. Linezolid-resistant Staphylococcus aureus in two pediatric patients receiving low-dose linezolid therapy. Pediatr Infect Dis J. 2006;25:562–4. doi: 10.1097/01.inf.0000219401.70804.1a. [DOI] [PubMed] [Google Scholar]
- 47.Trevino M, Martinez-Lamas L, Romero-Jung PA, Giraldez JM, Alvarez-Escudero J, Regueiro BJ. Endemic linezolid-resistant Staphylococcus epidermidis in a critical care unit. Eur J Clin Microbiol Infect Dis. 2009;28:527–33. doi: 10.1007/s10096-008-0657-5. [DOI] [PubMed] [Google Scholar]
- 48.Yoshida K, Shoji H, Hanaki H, et al. Linezolid-resistant methicillin-resistant Staphylococcus aureus isolated after long-term, repeated use of linezolid. J Infect Chemother. 2009;15:417–9. doi: 10.1007/s10156-009-0727-3. [DOI] [PubMed] [Google Scholar]
- 49.Kollef MH. Moving towards real-time antimicrobial management of ventilator-associated pneumonia. Clin Infect Dis. 2007;44:388–90. doi: 10.1086/510595. [DOI] [PubMed] [Google Scholar]
- 50.Stager CE, Davis JR. Automated systems for identification of microorganisms. Clin Microbiol Rev. 1992;5:302–27. doi: 10.1128/cmr.5.3.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Doern GV, Brueggemann AB, Perla R, et al. Multicenter laboratory evaluation of the bioMerieux Vitek antimicrobial susceptibility testing system with 11 antimicrobial agents versus members of the family Enterobacteriaceae and Pseudomonas aeruginosa. J Clin Microbiol. 1997;35:2115–9. doi: 10.1128/jcm.35.8.2115-2119.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tenover FC, Swenson JM, O'Hara CM, Stocker SA. Ability of commercial and reference antimicrobial susceptibility testing methods to detect vancomycin resistance in enterococci. J Clin Microbiol. 1995;33:1524–7. doi: 10.1128/jcm.33.6.1524-1527.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tenover FC, Williams PP, Stocker S, et al. Accuracy of six antimicrobial susceptibility methods for testing linezolid against staphylococci and enterococci. J Clin Microbiol. 2007;45:2917–22. doi: 10.1128/JCM.00913-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Torres E, Villanueva R, Bou G. Comparison of different methods of determining beta-lactam susceptibility in clinical strains of Pseudomonas aeruginosa. J Med Microbiol. 2009;58:625–9. doi: 10.1099/jmm.0.005587-0. [DOI] [PubMed] [Google Scholar]
- 55.Luzzaro F, Gesu G, Endimiani A, et al. Performance in detection and reporting beta-lactam resistance phenotypes in Enterobacteriaceae: a nationwide proficiency study in Italian laboratories. Diagn Microbiol Infect Dis. 2006;55:311–8. doi: 10.1016/j.diagmicrobio.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 56.Micek ST, Lloyd AE, Ritchie DJ, Reichley RM, Fraser VJ, Kollef MH. Pseudomonas aeruginosa bloodstream infection: importance of appropriate initial antimicrobial treatment. Antimicrob Agents Chemother. 2005;49:1306–11. doi: 10.1128/AAC.49.4.1306-1311.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Steward CD, Rasheed JK, Hubert SK, et al. Characterization of clinical isolates of Klebsiella pneumoniae from 19 laboratories using the National Committee for Clinical Laboratory Standards extended-spectrum beta-lactamase detection methods. J Clin Microbiol. 2001;39:2864–72. doi: 10.1128/JCM.39.8.2864-2872.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tenover FC, Emery SL, Spiegel CA, et al. Identification of plasmid-mediated AmpC beta-lactamases in Escherichia coli, Klebsiella spp., and proteus species can potentially improve reporting of cephalosporin susceptibility testing results. J Clin Microbiol. 2009;47:294–9. doi: 10.1128/JCM.01797-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tenover FC, Mohammed MJ, Gorton TS, Dembek ZF. Detection and reporting of organisms producing extended-spectrum beta-lactamases: survey of laboratories in Connecticut. J Clin Microbiol. 1999;37:4065–70. doi: 10.1128/jcm.37.12.4065-4070.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chakravorty S, Aladegbami B, Burday M, et al. Rapid universal identification of bacterial pathogens from clinical cultures by using a novel sloppy molecular beacon melting temperature signature technique. J Clin Microbiol. 2010;48:258–67. doi: 10.1128/JCM.01725-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ecker DJ, Massire C, Blyn LB, et al. Molecular genotyping of microbes by multilocus PCR and mass spectrometry: a new tool for hospital infection control and public health surveillance. Methods Mol Biol. 2009;551:71–87. doi: 10.1007/978-1-60327-999-4_7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ecker DJ, Sampath R, Massire C, et al. Ibis T5000: a universal biosensor approach for microbiology. Nat Rev Microbiol. 2008;6:553–8. doi: 10.1038/nrmicro1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ecker DJ, Sampath R, Willett P, et al. The Microbial Rosetta Stone database: a common structure for microbial biosecurity threat agents. J Forensic Sci. 2005;50:1380–5. [PubMed] [Google Scholar]
- 64.Ecker DJ, Sampath R, Willett P, et al. The Microbial Rosetta Stone database: a compilation of global and emerging infectious microorganisms and bioterrorist threat agents. BMC Microbiol. 2005;5:19. doi: 10.1186/1471-2180-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Huletsky A, Giroux R, Rossbach V, et al. New real-time PCR assay for rapid detection of methicillin-resistant Staphylococcus aureus directly from specimens containing a mixture of staphylococci. J Clin Microbiol. 2004;42:1875–84. doi: 10.1128/JCM.42.5.1875-1884.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rossney AS, Herra CM, Brennan GI, Morgan PM, O'Connell B. Evaluation of the Xpert methicillin-resistant Staphylococcus aureus (MRSA) assay using the GeneXpert real-time PCR platform for rapid detection of MRSA from screening specimens. J Clin Microbiol. 2008;46:3285–90. doi: 10.1128/JCM.02487-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hiramatsu K, Katayama Y, Yuzawa H, Ito T. Molecular genetics of methicillin-resistant Staphylococcus aureus. Int J Med Microbiol. 2002;292:67–74. doi: 10.1078/1438-4221-00192. [DOI] [PubMed] [Google Scholar]
- 68.Kuroda M, Ohta T, Uchiyama I, et al. Whole genome sequencing of methicillin-resistant Staphylococcus aureus. Lancet. 2001;357:1225–40. doi: 10.1016/s0140-6736(00)04403-2. [DOI] [PubMed] [Google Scholar]
- 69.Wolk DM, Picton E, Johnson D, et al. Multicenter evaluation of the Cepheid Xpert methicillin-resistant Staphylococcus aureus (MRSA) test as a rapid screening method for detection of MRSA in nares. J Clin Microbiol. 2009;47:758–64. doi: 10.1128/JCM.01714-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Parta M, Goebel M, Matloobi M, Stager C, Musher DM. Identification of methicillin-resistant or methicillin-susceptible Staphylococcus aureus in blood cultures and wound swabs by GeneXpert. J Clin Microbiol. 2009;47:1609–10. doi: 10.1128/JCM.00351-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hombach M, Pfyffer GE, Roos M, Lucke K. Detection of methicillin-resistant Staphylococcus aureus (MRSA) in specimens from various body sites: performance characteristics of the BD GeneOhm MRSA assay, the Xpert MRSA assay, and broth-enriched culture in an area with a low prevalence of MRSA infections. J Clin Microbiol. 2010;48:3882–7. doi: 10.1128/JCM.00670-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Malhotra-Kumar S, Van Heirstraeten L, Lee A, et al. Evaluation of molecular assays for rapid detection of methicillin-resistant Staphylococcus aureus. J Clin Microbiol. 2010;48:4598–601. doi: 10.1128/JCM.00004-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Allaouchiche B, Meugnier H, Freney J, Fleurette J, Motin J. Rapid identification of Staphylococcus aureus in bronchoalveolar lavage fluid using a DNA probe (Accuprobe) Intensive Care Med. 1996;22:683–7. doi: 10.1007/BF01709747. [DOI] [PubMed] [Google Scholar]
- 74.Finkelstein R, Brown P, Palutke WA, et al. Diagnostic efficacy of a DNA probe in pneumonia caused by Legionella species. J Med Microbiol. 1993;38:183–6. doi: 10.1099/00222615-38-3-183. [DOI] [PubMed] [Google Scholar]
- 75.Kaijalainen T, Rintamaki S, Herva E, Leinonen M. Evaluation of gene-technological and conventional methods in the identification of Streptococcus pneumoniae. J Microbiol Methods. 2002;51:111–8. doi: 10.1016/s0167-7012(02)00061-1. [DOI] [PubMed] [Google Scholar]
- 76.Kleemola M, Jokinen C. Outbreak of Mycoplasma pneumoniae infection among hospital personnel studied by a nucleic acid hybridization test. J Hosp Infect. 1992;21:213–21. doi: 10.1016/0195-6701(92)90078-z. [DOI] [PubMed] [Google Scholar]
- 77.Grobner S, Dion M, Plante M, Kempf VA. Evaluation of the BD GeneOhm StaphSR assay for detection of methicillin-resistant and methicillin-susceptible Staphylococcus aureus isolates from spiked positive blood culture bottles. J Clin Microbiol. 2009;47:1689–94. doi: 10.1128/JCM.02179-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Paule SM, Hacek DM, Kufner B, et al. Performance of the BD GeneOhm methicillin-resistant Staphylococcus aureus test before and during high-volume clinical use. J Clin Microbiol. 2007;45:2993–8. doi: 10.1128/JCM.00670-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wang XP, Ginocchio CC. Automation of the BD GeneOhm methicillin-resistant Staphylococcus aureus assay for high-throughput screening of nasal swab specimens. J Clin Microbiol. 2009;47:1546–8. doi: 10.1128/JCM.00114-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Svent-Kucina N, Pirs M, Mueller-Premru M, Cvitkovic-Spik V, Kofol R, Seme K. One-year experience with modified BD GeneOhm MRSA assay for detection of methicillin-resistant Staphylococcus aureus from pooled nasal, skin, and throat samples. Diagn Microbiol Infect Dis. 2009;63:132–9. doi: 10.1016/j.diagmicrobio.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 81.Bartels MD, Boye K, Rohde SM, et al. A common variant of staphylococcal cassette chromosome mec type IVa in isolates from Copenhagen, Denmark, is not detected by the BD GeneOhm methicillin-resistant Staphylococcus aureus assay. J Clin Microbiol. 2009;47:1524–7. doi: 10.1128/JCM.02153-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Thomas L, van Hal S, O'Sullivan M, Kyme P, Iredell J. Failure of the BD GeneOhm StaphS/R assay for identification of Australian methicillin-resistant Staphylococcus aureus strains: duplex assays as the “gold standard” in settings of unknown SCCmec epidemiology. J Clin Microbiol. 2008;46:4116–7. doi: 10.1128/JCM.01146-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stamper PD, Cai M, Howard T, Speser S, Carroll KC. Clinical validation of the molecular BD GeneOhm StaphSR assay for direct detection of Staphylococcus aureus and methicillin-resistant Staphylococcus aureus in positive blood cultures. J Clin Microbiol. 2007;45:2191–6. doi: 10.1128/JCM.00552-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Benson R, Tondella ML, Bhatnagar J, et al. Development and evaluation of a novel multiplex PCR technology for molecular differential detection of bacterial respiratory disease pathogens. J Clin Microbiol. 2008;46:2074–7. doi: 10.1128/JCM.01858-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Winchell JM, Thurman KA, Mitchell SL, Thacker WL, Fields BS. Evaluation of three real-time PCR assays for detection of Mycoplasma pneumoniae in an outbreak investigation. J Clin Microbiol. 2008;46:3116–8. doi: 10.1128/JCM.00440-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tang YW, Kilic A, Yang Q, et al. StaphPlex system for rapid and simultaneous identification of antibiotic resistance determinants and Panton-Valentine leukocidin detection of staphylococci from positive blood cultures. J Clin Microbiol. 2007;45:1867–73. doi: 10.1128/JCM.02100-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Podzorski RP, Li H, Han J, Tang YW. MVPlex assay for direct detection of methicillin-resistant Staphylococcus aureus in naris and other swab specimens. J Clin Microbiol. 2008;46:3107–9. doi: 10.1128/JCM.02347-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Balada-Llasat JM, Larue H, Kelly C, Rigali L, Pancholi P. Evaluation of commercial ResPlex II v2.0, MultiCode((R))-PLx, and xTAG((R)) respiratory viral panels for the diagnosis of respiratory viral infections in adults. J Clin Virol. 2011;50:42–5. doi: 10.1016/j.jcv.2010.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Shrestha NK, Tuohy MJ, Padmanabhan RA, Hall GS, Procop GW. Evaluation of the LightCycler Staphylococcus M GRADE kits on positive blood cultures that contained gram-positive cocci in clusters. J Clin Microbiol. 2005;43:6144–6. doi: 10.1128/JCM.43.12.6144-6146.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Casalta JP, Gouriet F, Roux V, Thuny F, Habib G, Raoult D. Evaluation of the LightCycler SeptiFast test in the rapid etiologic diagnostic of infectious endocarditis. Eur J Clin Microbiol Infect Dis. 2009;28:569–73. doi: 10.1007/s10096-008-0672-6. [DOI] [PubMed] [Google Scholar]
- 91.Bittar F, Ouchenane Z, Smati F, Raoult D, Rolain JM. MALDI-TOF-MS for rapid detection of staphylococcal Panton-Valentine leukocidin. Int J Antimicrob Agents. 2009;34:467–70. doi: 10.1016/j.ijantimicag.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 92.La Scola B, Raoult D. Direct identification of bacteria in positive blood culture bottles by matrix-assisted laser desorption ionisation time-of-flight mass spectrometry. PLoS One. 2009;4:e8041. doi: 10.1371/journal.pone.0008041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Seng P, Drancourt M, Gouriet F, et al. Ongoing revolution in bacteriology: routine identification of bacteria by matrix-assisted laser desorption ionization time-of-flight mass spectrometry. Clin Infect Dis. 2009;49:543–51. doi: 10.1086/600885. [DOI] [PubMed] [Google Scholar]
- 94.Morozumi M, Nakayama E, Iwata S, et al. Simultaneous detection of pathogens in clinical samples from patients with community-acquired pneumonia by real-time PCR with pathogen-specific molecular beacon probes. J Clin Microbiol. 2006;44:1440–6. doi: 10.1128/JCM.44.4.1440-1446.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Endimiani A, Hujer AM, Hujer KM, et al. Evaluation of a commercial microarray system for detection of SHV-, TEM-, CTX-M-, and KPC-type beta-lactamase genes in Gram-negative isolates. J Clin Microbiol. 2010;48:2618–22. doi: 10.1128/JCM.00568-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Naas T, Cuzon G, Truong H, Bernabeu S, Nordmann P. Evaluation of a DNA microarray, the check-points ESBL/KPC array, for rapid detection of TEM, SHV, and CTX-M extended-spectrum beta-lactamases and KPC carbapenemases. Antimicrob Agents Chemother. 2010;54:3086–92. doi: 10.1128/AAC.01298-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hari KL, Goates AT, Jain R, et al. The Microbial Rosetta Stone: a database system for tracking infectious microorganisms. Int J Legal Med. 2009;123:65–9. doi: 10.1007/s00414-008-0247-1. [DOI] [PubMed] [Google Scholar]
- 98.Ecker DJ, Sampath R, Blyn LB, et al. Rapid identification and strain-typing of respiratory pathogens for epidemic surveillance. Proc Natl Acad Sci U S A. 2005;102:8012–7. doi: 10.1073/pnas.0409920102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Deyde VM, Sampath R, Garten RJ. Genomic signature-based identification of influenza A viruses using RT-PCR/electro-spray ionization mass spectrometry (ESI-MS) technology. PLoS One. 2010;5:e13293. doi: 10.1371/journal.pone.0013293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Metzgar D, Baynes D, Myers CA, et al. Initial identification and characterization of an emerging zoonotic influenza virus prior to pandemic spread. J Clin Microbiol. 2010;48:4228–34. doi: 10.1128/JCM.01336-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sampath R, Hall TA, Massire C, et al. Rapid identification of emerging infectious agents using PCR and electrospray ionization mass spectrometry. Ann N Y Acad Sci. 2007;1102:109–20. doi: 10.1196/annals.1408.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sampath R, Russell KL, Massire C, et al. Global surveillance of emerging influenza virus genotypes by mass spectrometry. PLoS One. 2007;2:e489. doi: 10.1371/journal.pone.0000489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sauer S, Kliem M. Mass spectrometry tools for the classification and identification of bacteria. Nat Rev Microbiol. 2010;8:74–82. doi: 10.1038/nrmicro2243. [DOI] [PubMed] [Google Scholar]
- 104.Hujer KM, Hujer AM, Endimiani A, et al. Rapid determination of quinolone resistance in Acinetobacter spp. J Clin Microbiol. 2009;47:1436–2. doi: 10.1128/JCM.02380-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Endimiani A, Hujer KM, Hujer AM, Sampath R, Ecker DJ, Bonomo RA. Rapid identification of blaKPC-possessing Enterobacteriaceae by PCR/electrospray ionization-mass spectrometry. J Antimicrob Chemother. 2010;65:1833–34. doi: 10.1093/jac/dkq207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wolk DM, Blyn LB, Hall TA, et al. Pathogen profiling: rapid molecular characterization of Staphylococcus aureus by PCR/electrospray ionization-mass spectrometry and correlation with phenotype. J Clin Microbiol. 2009;47:3129–37. doi: 10.1128/JCM.00709-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hall TA, Sampath R, Blyn LB, et al. Rapid molecular genotyping and clonal complex assignment of Staphylococcus aureus isolates by PCR coupled to electrospray ionization-mass spectrometry. J Clin Microbiol. 2009;47:1733–41. doi: 10.1128/JCM.02175-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ecker JA, Massire C, Hall TA, et al. Identification of Acinetobacter species and genotyping of Acinetobacter baumannii by multilocus PCR and mass spectrometry. J Clin Microbiol. 2006;44:2921–32. doi: 10.1128/JCM.00619-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Whitman TJ, Qasba SS, Timpone JG, et al. Occupational transmission of Acinetobacter baumannii from a United States serviceman wounded in Iraq to a health care worker. Clin Infect Dis. 2008;47:439–43. doi: 10.1086/589247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wortmann G, Weintrob A, Barber M, et al. Genotypic evolution of Acinetobacter baumannii strains in an outbreak associated with war trauma. Infect Control Hosp Epidemiol. 2008;29:553–5. doi: 10.1086/588221. [DOI] [PubMed] [Google Scholar]
- 111.Perez F, Ray AJ, Endimiani A, et al. Carbapenem-resistant Klebsiella pneumoniae across a hospital system: impact of post-acute care facilities on dissemination. J Antimicrob Chemother. 2010;65:1807–13. doi: 10.1093/jac/dkq191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Jacobs MR, Bajaksouzian S, Bonomo RA, et al. Occurrence, distribution, and origins of Streptococcus pneumoniae Serotype 6C, a recently recognized serotype. J Clin Microbiol. 2009;47:64–72. doi: 10.1128/JCM.01524-08. [DOI] [PMC free article] [PubMed] [Google Scholar]