Abstract
It is impossible to know with certainty the first time that an influenza virus infected humans or when the first influenza pandemic occurred. However, many historians agree that the year 1510 a.d.—500 years ago—marks the first recognition of pandemic influenza. On this significant anniversary it is timely to ask: what were the circumstances surrounding the emergence of the 1510 pandemic, and what have we learned about this important disease over the subsequent five centuries?We conclude that in recent decades significant progress has been made in diagnosis, prevention, control, and treatment of influenza. It seems likely that, in the foreseeable future, we may be able to greatly reduce the burden of influenza pandemics with improved vaccines and other scientific and public health approaches.
It is impossible to know with certainty the first time an influenza virus infected humans or when the first influenza pandemic occurred. However, many historians agree that the year 1510 a.d.—500 years ago—marks the first recognition of pandemic influenza. On this significant anniversary, it is timely to ask, what were the circumstances surrounding the emergence of the 1510 pandemic, and what have we learned about this important disease over the subsequent 5 centuries?
In Europe, the year 1510 ended 2 decades of profound change. The NewWorld, “discovered” by Columbus 18 years earlier, now was greeting waves of European conquistadores vigorously mapping a larger-than-imagined globe, charting faraway regions populated by exotic peoples, settling these lands, and importing African slave laborers to establish lucrative new businesses. They brought back to Europe not only descriptions of New World societies dominated by women warriors, akin to the Amazons of Greek mythology, but also such exotic emerging diseases as syphilis [1]. Some accounts suggest that 1510 was a year of “firsts”—the earliest description of a Christmas tree, the first successful slave revolt (on Hispaniola), and the advent of pocket watches, pretzel bows, and Benedictine liquor. Florentine painter Allessandro Botticelli died that year, but Renaissance art flourished under da Vinci (1452–1519), Dürer (1471–1528), Michelangelo (1475–1564), and others. In 1510, medical literature was almost nonexistent, but the recent developments of the printing press and moveable type were beginning to provide the wealthy with books, the most transformative technological product in centuries.
Europe in 1510 was still recovering from massive depopulation caused by the Black Death in the 1340s and was struggling with a less fatal but still horrifying epidemic of syphilis [1]. Explosive European-wide or local epidemics of respiratory disease with fever, coughing, and pneumonia had been documented for at least 650 years. British/European epidemics of “sweate” (Sudor Anglicus; English sweating sickness), plausibly attributed to influenza [2, 3], had been recurring for 25 years, but influenza pandemics had never been identified.
Then suddenly, in July and August 1510, a “gasping oppression” with cough, fever, and a sensation of constriction of the heart and lungs began to rage, seemingly everywhere at once [4]. Said to have first arisen in Asia, the disease spread to almost every part of the known world, prominently excepting the New World. It arrived in Sicily and Italy along trade routes from Africa and quickly spread throughout Europe, moving north to northwest [5]. In September 1510, French King Louis XII convened a national assembly of Bishops, Prelates, and university professors that was disrupted by the disease [6].
The pandemic was documented by individuals of that era who lived through it and wrote about the event decades later, when books began to become available to scholars and the general public, including physician John Caius and surgeon Ambroise Paré (both born in 1510) and historian Jean Bouchet (appointed to Court in 1510). Fortunately, the pandemic burned out soon after it started. It had a high attack rate but few recognized deaths [4], occurring mostly in children or after excessive blood-letting [5], a common 16th century treatment for febrile and other diseases. The 8-year-old future Pope Gregory XIII became dangerously ill with the disease but fully recovered.
That the 1510 pandemic might be the same disease as earlier febrile coughing epidemics gradually became apparent with documentation of subsequent episodes of (probable) seasonal influenza and with new influenza pandemics in 1557 and 1580 [7]. To observers later in the 16th century, influenza came to be recognized as a distinct disease with consistent clinical features including acute onset of fever, headache, cough, and myalgia, with uncommon complications that included pneumonia and fatal outcomes in pregnant women and their fetuses, in infants and young children, and in the old and debilitated. Its epidemiologic featureswere understood to include explosive spread with high attack rates and directional movement along travel or trade routes, prevalence in a town or city for no more than 4–6 weeks, appearance at unpredictable intervals and at any time of year (influenza was frequent in the summer months until the 19th century 8]), and low-to-moderate population mortality.
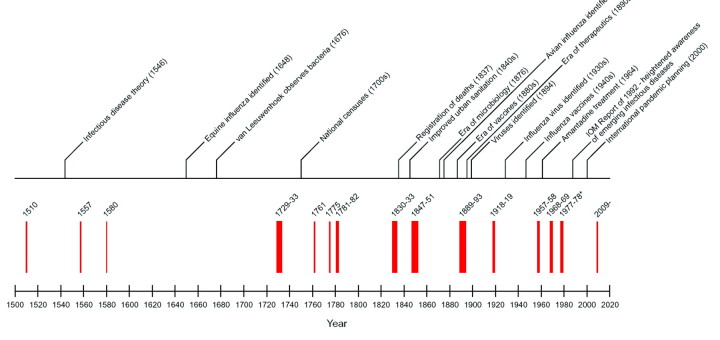
Although we recognize the same disease today, we have learned much in the intervening five centuries (Figure 1) [7]. Contagion was understood in 1510, but no plausible infectious disease theory would be proposed until 1546 [9]. It took another century for microbes to be discovered (in 1676 [10]) and 2 more to link microbes to human diseases (in 1876 [11]). Although 2 immunizing agents had been identified in the 18th century (inoculated smallpox and cowpox viruses became widely used in Europe after 1720 and 1798, respectively), establishment of the field of microbiology in the 1870s led to more sophisticated understanding of immunologic mechanisms, leading in turn to development in the 1880s of new vaccines to prevent, and in the 1890s immune sera to treat, human diseases. Microbiology fostered new epidemiologic concepts of infectious diseases that supported better prevention measures, including the discovery that infectious diseases could be transmitted by persons before the onset of clinically apparent illness and in the absence of illness (carriers).
Figure 1.
Five centuries of documented influenza pandemics [7] with a timeline of selected significant events related to understanding and controlling influenza, 1510–2010. *The pandemic of 1977–1978 is often not considered a pandemic, because it represented the return of a 1950s-era descendant of the 1918 pandemic virus [7].
In the same time period, public health data infrastructures were established.Western nations began conducting national censuses in the 1700s and establishing causeof- death registries in the 1830s. The influenza pandemics of the 1830s and 1840s were investigated with increasinglymodern epidemiologic methods, including calculation of case-fatality rates and age-specific death rates, leading to an understanding of the enormous impact that a disease of low case-fatality but high incidence, such as influenza, can have. A large body of evidence had been accumulating since the mid-17th century that influenza was both a human and a mammalian disease [8]; in 1878, avian influenza was recognized [12] and was soon linked to transmission to humans [13].
By the time of the next pandemic, in 1889–1894, influenza had become an easily recognizable disease, and the general principles of pandemicity were understood. A putative causative microbial agent, Pfeiffer's bacillus, was identified in 1892 (incorrectly, as it later turned out [13, 14]—the organism in question, now named Haemophilus influenzae, still retains the mistaken attribution nosologically), and the geographic progression of the pandemic was readily traced from east to west along railroad lines and other routes of human travel [15]. Even greater progress has been made over the past century, under the shadow of the devastating pandemic of 1918–1919, whose viral descendants still persist in 2010. Discovery of both swine and human influenza viruses in the 1930s [13], followed rapidly by the association of human disease with viral infection of ferrets, by prevention of ferret infection with convalescent serum, and by growth of virus in embryonated hens' eggs, led directly to influenza vaccines in the 1940s and public vaccination programs in the 1950s. Influenza antivirals were first used in the 1960s.
Despite continuing progress in many areas, including enhanced human and animal surveillance and large-scale viral genomic screening, we are probably no better able today to anticipate and prevent the emergence of pandemic influenza than 5 centuries ago, as shown by the completely unexpected emergence of the 2009 novel H1N1 pandemic virus. However, unlike our predecessors, we now have an armamentarium of vaccines against influenza viruses and complicating bacteria, rapid and point-of-care diagnostic tests, effective drugs and other treatments, and an expanding knowledge base that should one day lead to additional significant advances in influenza prevention, control and treatment.
In particular, the past decade has seen sophisticated national and international pandemic planning, which was broadly tested in the 2009–2010 pandemic of novel swine H1N1 virus. Moreover, there is a growing appreciation among the general public of the importance of influenza and of both the “common sense” (such as avoiding exposures to infection and good hygienic practices) and biomedical tools available to prevent the disease, providing a potentially important base to build upon with new prevention information and with up-to date-vaccines and immunization programs when pandemics occur. Substantial effort is now directed at the development of so-called “universal vaccines” that target immune responses to all influenza A viruses. Such vaccines potentially could be used to address the issue of seasonal variations in influenza viruses, as well as to control pandemics as soon as they emerge or, theoretically, even prevent their emergence.
The past 500 years of pandemic influenza have witnessed considerable suffering and death as well as important scientific advances that have led to many important tools to fight this important disease. We can anticipate with optimism that this progress will help us to greatly reduce the burden of both seasonal and pandemic influenza during the centuries to come.
Acknowledgments
Financial support. Intramural funds of the National Institute of Allergy and Infectious Diseases and the National Institutes of Health.
Potential conflicts of interest. All authors: no conflicts.
References
- 1.Morens D, Folkers G, Fauci A. Emerging infections: a perpetual challenge. Lancet Infect Dis. 2008;8:710–719. doi: 10.1016/S1473-3099(08)70256-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hecker J. The sweating sickness. In: Hecker J, editor. The epidemics of the middle ages. 3rd ed. London: Trübner & Co; 1859. [Google Scholar]
- 3.Hamer W. The Milroy Lectures on epidemic disease in England—the evidence of variability and persistency of type. Lancet. 1906;1:569–574. [Google Scholar]
- 4.Fernel J. Leiden: Brill; 2005. On the pestilent diseases: that their cause is hidden; pp. 563–595. [Google Scholar]
- 5.Short T. London: Longman, T; Millar, A; 1749. A general chronological history of the air, weather, seasons, meteors, &c. in sundry places and different times; more particularly for the space of 250 years. Together with some of their most remarkable effects on animal (especially human) bodies, and vegetables. In two volumes. [Google Scholar]
- 6.Bouchet J. Le maladie Universelle [ou] la coqueluche. In: Bouchet J, editor. Les Annales Dacquitaine. 1535. [Google Scholar]
- 7.Taubenberger J, Morens D. Pandemic influenza-including a risk assessment of H5N1. Rev Sci Tech. 2009;28((1)):187–202. doi: 10.20506/rst.28.1.1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morens D, Taubenberger J. Historical thoughts on influenza viral ecosystems, or behold a pale horse, dead dogs, failing fowl, and sick swine. Influenza Other Resp Vir. 2010;4((6)):327–337. doi: 10.1111/j.1750-2659.2010.00148.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fracastoro G. De contagione et contagiosis morbis et curatione. Venetiis [Venice]: Apud heredes L[ucaeantonii] Iuntae [Florentini]; 1546. De sympathia et antipathia rerum liber unus. [Google Scholar]
- 10.van Leeuwenhoek A. An abstract of a letter… Sep. 17, 1683 containing some microscopical observations, about animals in the scurf of the teeth. Phil Trans. 1684;14:568–574. [Google Scholar]
- 11.Koch R. Die Aetiologie der Milzbrand-Krankheit, begründet auf die Entwicklungsgeschichte der Bacillus Anthracis. Beiträge zur Biologie der Pflanzen (Breslau [Wroclaw]) 1876;2:277–310. [Google Scholar]
- 12.Perroncito E. Epizoozia tifoide nei gallinacei. Ann Accad Agric Torino. 1878;21:87–126. [Google Scholar]
- 13.Taubenberger JK, Hultin JV, Morens DM. Discovery and characterization of the 1918 pandemic influenza virus in historical context. Antivir Ther. 2007;12((4 Pt B)):581–591. [PMC free article] [PubMed] [Google Scholar]
- 14.Pfeiffer R. Die Aetiologie der Influenza: Zeitschrift für Hygiene und Infektionskrankheiten; medizinische Mikrobiologie. Immunologie und Virologie. 1893;13:357–85. [Google Scholar]
- 15.Clemow F. The recent pandemic of influenza: its place of origin and mode of spread. Lancet. 1894;1:139–143. [Google Scholar]