Poor engagement in HIV care is common in the United States and worsens HIV treatment outcomes. In addition, poor engagement in care is likely to drastically reduce the effectiveness of “test and treat” HIV prevention strategies.
Abstract
(See the editorial commentary by Lange, on pages 801–802.)
For individuals with human immunodeficiency virus (HIV) infection to fully benefit from potent combination antiretroviral therapy, they need to know that they are HIV infected, be engaged in regular HIV care, and receive and adhere to effective antiretroviral therapy. Test-and-treat strategies for HIV prevention posit that expanded testing and earlier treatment of HIV infection could markedly decrease ongoing HIV transmission, stemming the HIV epidemic. However, poor engagement in care for HIV-infected individuals will substantially limit the effectiveness of test-and-treat strategies. We review the spectrum of engagement in care for HIV-infected individuals in the United States and apply this information to help understand the magnitude of the challenges that poor engagement in care will pose to test-and-treat strategies for HIV prevention.
Over the past decade, antiretroviral therapy has become more potent, better tolerated, and less complex. Today, most human immunodeficiency virus (HIV)–infected individuals receiving combination antiretroviral therapy achieve an undetectable plasma HIV - RNA level [1, 2]. Nevertheless, deficits in the spectrum of engagement in HIV care (Figure 1) including late HIV diagnosis, suboptimal linkage to and retention in HIV care, insufficient use of antiretroviral therapy, and suboptimal adherence to therapy, pose significant barriers to achieving optimal treatment outcomes [3].
Figure 1.
Health Resources and Services Administration (HRSA) continuum of HIV care, describing the spectrum of engagement in HIV care. Adapted from Eldred et al [3].
These impediments to engagement in HIV care also pose considerable obstacles to the successful implementation of strategies that suggest that early identification of all HIV-infected individuals (“test”) and initiation of antiretroviral therapy in these individuals (“treat”) could lead to dramatic reductions in the incidence of HIV infection [4–6]. A test-and-treat strategy for HIV prevention is supported by mathematical models and epidemiological data [5, 7, 8]. In addition, locations with high antiretroviral coverage have decreasing incidence of HIV infection [2, 9, 10]. Despite these initial suggestions of success, the barriers to implementation of test-and-treat strategies need to be more fully evaluated.
The first objective of this review is to describe and quantify the spectrum of engagement in HIV care. We then apply these findings to better understand how gaps in the continuum of HIV care affect virological outcomes in the United States and how these gaps need to be addressed for test-and-treat to become a successful HIV prevention strategy. Finally, we explore the possible effects of interventions to improve components of engagement in HIV care.
HIV Infection in the United States
Prevalence and Incidence of HIV Infection
At the end of 2006, ∼1.1 million adults and adolescents were living with HIV infection in the United States (prevalence, .45%) [11]. Geographic variability is substantial. In some US cities, HIV seroprevalence exceeds 1%–2%, whereas in populations at high risk of infection, such as men who have sex with men in New York City, HIV seroprevalence exceeds 13% [12–14]. Since 2000, the incidence of HIV infection in the United States has remained stable at ∼56,300 new infections per year [15].
Undiagnosed HIV Infection
Of the 1.1 million individuals living with HIV infection in the United States, 232,700 (21%) are estimated to be unaware of their HIV infection [16]. These individuals cannot engage in treatment that reduces morbidity and mortality, may participate more often in high-risk HIV transmission behavior, and have a higher risk of transmitting HIV to others than do those who are aware of their HIV infection [16–20]. Furthermore, among those newly diagnosed, many already have advanced disease. In the United States, 35%–45% of individuals with newly diagnosed HIV infection have AIDS within 1 year after diagnosis [21–27].
Linkage to and Retention in HIV Care
Linkage to Care
Failure to initiate timely HIV care after diagnosis is common. Longer delays in linkage with medical care are associated with greater likelihood of progression to AIDS by CD4 cell criteria. Similar to individuals with undiagnosed infection, HIV-infected individuals not engaged in care pose a greater risk of ongoing HIV transmission [28].
Two prospective, population-based studies have evaluated the extent to which individuals with newly diagnosed HIV infection link to care. In St. Louis, Missouri, 73% of individuals with newly diagnosed HIV infection during 1997–2002 had evidence of having received HIV care within 1 year after diagnosis of HIV infection [29]. In New York City, 64% of individuals with newly diagnosed HIV infection initiated care within 3 months, and 83% entered care within 4 years [30]. In the Antiretroviral Treatment and Access Study, 60% of participants who received only passive referrals to care linked to HIV care within 6 months [31]. In summary, we conclude that ∼75% of individuals with newly diagnosed HIV infection successfully link to HIV care within 6–12 months after diagnosis; 80%–90% link within 3–5 years.
Retention in Care
Successful HIV treatment requires sustained engagement in HIV care [32–34]. Opportunistic illnesses, such as Pneumocystis jirovecii pneumonia, are most common in individuals with unknown HIV serostatus and in those who are not receiving HIV care [35, 36]. Three population-based studies from the United States have found that 45%–55% of known HIV-infected individuals fail to receive HIV care during any year [29, 37, 38]. Over longer periods, approximately one-third of HIV-infected individuals fail to access care for 3 consecutive years in some communities [29, 38]. Multiple cohort studies have found that 25%–44% of HIV-infected individuals are entirely lost to follow-up in many settings [39–42], although these individuals may eventually re-establish care. Three European studies found that 27%–60% of out of care HIV-infected individuals return to care in 1–2 years [39,42–44].
In summary, ∼50% of known HIV-infected individuals are not engaged in regular HIV care. As a result, these individuals do not have sustained access to antiretroviral therapy, prophylactic medications, or other medical services. Those who receive antiretroviral therapy intermittently are at increased risk of viral resistance [45]. For these reasons, poor engagement in care is associated with poor health outcomes, including increased mortality [32, 33]. In addition, these individuals contribute to ongoing HIV transmission in the community.
Antiretroviral Therapy
HIV-infected individuals who are engaged in care have 4 main barriers to successful treatment with antiretroviral medications: delay or failure to initiate therapy, lack of persistence with therapy, poor adherence to therapy, and viral resistance to antiretroviral medication. In the United States in 2003, ∼67% of HIV-infected individuals in care were eligible for antiretroviral therapy on the basis of a CD4 cell count ≤350 cells/μL; however, 21% of these individuals were not receiving therapy [46]. A more recent analysis from British Columbia found that 89% of individuals in care required antiretroviral therapy, but ∼27% declined or failed to initiate therapy [47]. We estimate that 80% of in-care HIV-infected individuals in the United States should be receiving antiretroviral therapy but that 25% of these individuals are not receiving therapy. Recent guidelines recommend considering antiretroviral therapy initiation when CD4 cell counts decrease to <500 cells/μL, which would increase the proportion of in-care individuals eligible for treatment [48, 49].
Persistence with Antiretroviral Therapy
Nonpersistence occurs when therapy is halted prematurely. Patients may stop their medications as a result of medication adverse effects or competing priorities [50, 51], and providers may recommend cessation of therapy in response to clinical or laboratory adverse events or barriers to adherence [52, 53]. In 3 large cohort studies, 4%–6% of individuals who remained in care discontinued their antiretroviral regimen each year [52, 54, 55].
Adherence to Antiretroviral Therapy
A meta-analysis of 31 North American adherence studies found that 55% of HIV-infected individuals achieve adequate adherence [56]. Because antiretroviral therapy has become more potent, better treatment outcomes can be achieved despite lower adherence. With modern initial antiretroviral regimens, 70%–80% adherence leads to durable viral suppression in most individuals [57, 58]. In 2 recent studies from large North American cohorts, 60%–80% of individuals achieved adequate levels of adherence by this new standard [59, 60]. As a consequence of successful viral suppression at lower levels of adherence, the population effectiveness of antiretroviral therapy has increased. Two recent studies found that 78%–87% of individuals receiving antiretroviral therapy, including individuals receiving initial and subsequent regimens, had an undetectable viral load [1, 2].
Resistance to Antiretroviral Medications
Antiretroviral resistance accumulates during virological failure. Antiretroviral resistance also contributes to the failure of antiretroviral therapy. The contribution of antiretroviral medication resistance to regimen failure is unclear but appears to be small, particularly with the advent of new antiretroviral medications and classes. On a population level, rates of transmitted and prevalent resistance are stable or decreasing in some resource-rich settings [1, 61, 62]. This is likely attributable to the high genetic barrier to resistance and/or high potency of the most frequently used regimens [63]. In a large US study from 2006, 15% of individuals with newly diagnosed HIV infection had transmitted antiretroviral resistance—a slightly higher percentage than in prior studies [64].
Nonpersistence, nonadherence, and antiretroviral resistance are barriers to effective antiretroviral therapy, contributing to detectable HIV viremia in 15%–25% of individuals receiving therapy. However, the majority of individuals receiving antiretroviral therapy in 2010 have undetectable viral loads. Thus, most HIV-infected individuals receiving therapy are at low risk for clinical progression and low risk to transmit HIV to others.
The Spectrum of Engagement in Care: By the Numbers
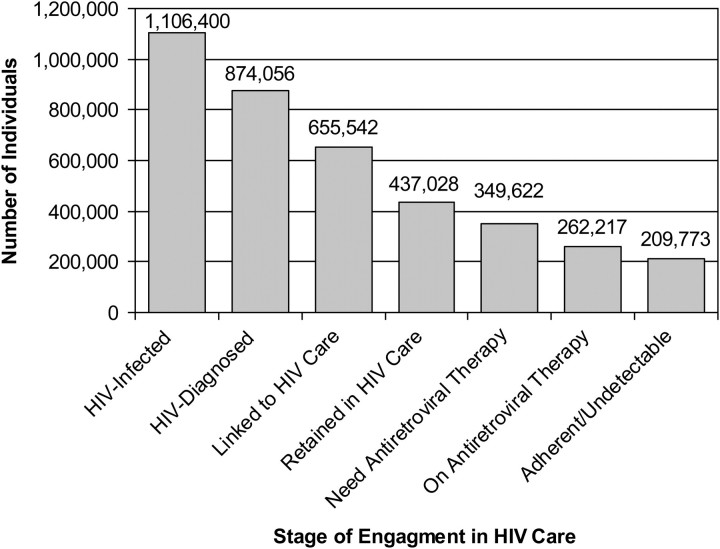
In Figures 2 and 3a, we synthesize these findings to estimate the spectrum of engagement in HIV care in the United States and the proportion of the HIV-infected population who have an HIV load <50 copies/mL. Approximately 79% of HIV-infected individuals are aware of their HIV infection, but ∼50% are not adequately engaged in HIV care. Thus, 60% of HIV-infected individuals in the United States are not receiving regular HIV care because of deficits in diagnosis of HIV infection, linkage to care, or retention in care. Of the remaining 40% of individuals, ∼80% require antiretroviral therapy, 75% of whom receive it. Finally, ∼80% of treated individuals have an undetectable viral load (defined as < 50 copies/mL). These 210,000 HIV-infected individuals with undetectable viral loads constitute just 19% of the HIV-infected population in the United States. With >80% of HIV-infected individuals in the United States having detectable HIV viremia, it is not surprising that the incidence of HIV infection has not decreased in the United States despite almost 15 years of widespread access to combination antiretroviral therapy. The model in Figure 2 is simplistic, but we are unaware of data from cohorts of individuals tracked over the engagement-in-care continuum that can more precisely determine the true proportion of HIV-infected individuals in the United States with an undetectable HIV load.
Figure 2.
The spectrum of engagement in HIV care in the United States spanning from HIV acquisition to full engagement in care, receipt of antiretroviral therapy, and achievement of complete viral suppression. We estimate that only 19% of HIV-infected individuals in the United States have an undetectable HIV load.
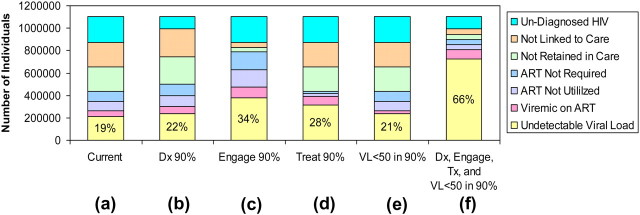
Figure 3.
Six simple simulations (a–f) assessing different levels of engagement in care. a, Current estimates for engagement in HIV care in the United States: 79% aware of their HIV diagnosis, 50% engaged in care (25% not linked, 25% not retained), 80% require antiretroviral therapy (ART), 75% receive ART, and 80% have an undetectable viral load while receiving ART. For the remaining simulations only the parameter(s) discussed are different. b, Assumption that 90% of HIV-infected individuals are aware of their diagnosis. c, Assumption that 90% of HIV-infected individuals who have received a diagnosis are engaged in care. d, Assumption that 90% of individuals in care receive ART. e, Assumption that viral suppression to <50 copies/mL in 90% of individuals receiving ART. f, Combination of columns b–e by assuming 90% known HIV diagnosis, 90% engagement in HIV care, 90% receipt of ART, and 90% achievement of an undetectable viral load.
These estimates can be used to explore the potential impact of interventions to improve engagement in care on the proportion of HIV-infected individuals with an undetectable HIV load. These simple simulations will also help demonstrate the impact of uncertainty in our engagement-in-care estimates on the projected proportion of HIV-infected individuals in the United States with undetectable HIV loads.
Test-and-Treat Implications
Although there is now a burgeoning interest in the impact of widespread antiretroviral therapy on HIV prevention, this is not new. Approximately 10 years ago, mathematical models were first published to suggest that widespread use of antiretroviral therapy in HIV-infected individuals could reduce the incidence of HIV infection [65–67]. Since that time, epidemiological data have suggested that antiretroviral therapy reduces the risk of HIV transmission in heterosexual sero-discordant couples by 92%–98% [7, 8, 68, 69]. In addition, ecological data have revealed that the incidence of HIV infection may be decreasing in communities with high treatment coverage [2, 9, 10]. Newer mathematical models, using this accumulating data, are more optimistic about the potential usefulness of HIV treatment for the prevention of HIV transmission [5, 70, 71]. In Figure 3, we present simulations of the impact of successful interventions to improve specific components of engagement in care on the proportion of individuals with an undetectable HIV load—a surrogate for individuals unlikely to transmit HIV infection to others. These are not intended to be definitive mathematical models. Instead, these are presented to provide rough estimates of the magnitude of the barriers that inadequate engagement in care pose to test-and-treat strategies.
Figure 3(b-e) demonstrates that improvement in any single component of engagement in care will have minimal impact on the proportion of HIV-infected individuals in the United States with an undetectable viral load. This occurs because achievement of an undetectable viral load is dependent on overcoming multiple, sequential barriers, each of which has only a modest impact on overall engagement in care. However, individuals who cannot overcome a specific barrier cannot engage at any subsequent step. Thus, improvement in the entire continuum of engagement in care will be required for test-and-treat strategies to substantially increase the proportion of persons with undetectable viral loads, as shown in Figure 3f. Diagnosis of 90% of HIV infections, achievement of 90% engagement in care, treatment of 90% of engaged individuals, and suppression of viremia in 90% of treated individuals could lead to considerable improvement in the proportion of HIV-infected individuals in the United States with undetectable viral loads. However, even in this ideal scenario, ∼34% of HIV-infected individuals will remain viremic, with the potential to spread HIV infection to others.
DISCUSSION
This review demonstrates that incomplete engagement in HIV care is common in the United States and that incompletely engaged individuals account for the largest proportion of HIV-infected individuals with detectable viremia. These findings have direct implications for test-and-treat programs, because disengaged individuals continue to contribute to the ongoing transmission of HIV infection. Although improvements in testing for HIV infection and treatment of HIV-infected individuals will be vital for test-and-treat programmatic success, engagement of HIV-infected individuals in care will be critical for individual health and the prevention of HIV transmission to others.
Although nonadherence to antiretroviral therapy and antiretroviral medication resistance were long viewed as barriers to controlling the HIV epidemic, the advent of more potent regimens has shifted the challenge toward earlier steps in the process of recognition and treatment of HIV infection. A new set of clinical and public health strategies are necessary to address this problem, particularly if test-and-treat programs are to be successful. Little is known about the best ways to link and retain HIV-infected individuals in HIV care. A strengths-based case-management intervention was shown to increase 6-month linkage to care, compared with passive referral, from 60% to 78% [31]. This intervention is widely accepted as the current standard for initial linkage to HIV care, and its results were confirmed in a subsequent community implementation study [72]. The effect of this intervention on retention in care at 1 year was attenuated, however, and overall, less is known about the best ways to retain individuals in care over time.
Soon after the introduction of potent combination antiretroviral therapy, a series of studies funded through a US Health Resources and Services Administration (HRSA) Special Programs of National Significance (SPNS) found that greater engagement in HIV care was associated with greater use of case-management services, mental health services, substance abuse treatment, transportation assistance, and housing assistance [73]. Subsequently, HRSA identified case management and outreach as a priority for interventions designed to improve retention in HIV care [74]. Interventions funded through a subsequent SPNS initiative included behavioral interventions, intensive case management, patient navigation, life skills training, literacy training, and home-based outreach [75]. As an example of effect size, 4 of the SPNS sites used patient navigation-like interventions, and engagement in care improved from 64% at baseline to 79% at 12 months [76]. The overall conclusion from the HRSA initiative was that outreach activities held promise for engaging and retaining out-of-care persons in HIV medical care [77]. Although costly and labor intensive, such interventions exemplify strategies that simultaneously address several of the barriers described here. Such approaches provide the best current hope for comprehensive management.
Additional research on best practices to link and retain HIV-infected individuals in care is needed. Research will need to be multifaceted to approach the problem of poor retention in care from many angles. Interventions targeting HIV-infected populations, such as provision of mental health or substance abuse services, are important but will need to be complemented by more structural interventions that target the system of health care delivery. The latter may be particularly beneficial, because they should be easier to implement, are more sustainable, and might enhance patient-provider relationships, which clearly promotes successful long-term engagement in HIV care [78]. Patient navigation, intensive case management, cell phone or text-messaging based systems, and integrated informatics to identify at-risk or out-of-care individuals hold promise for further development. Finally, information on the extent to which perceptions of stigma impede engagement in HIV care and interventions should be pursued [79, 80].
One of the limitations of this review is that few studies have assessed the extent to which financial barriers impede access to HIV care in the United States. These barriers include lack of insurance coverage, exclusion of HIV infection as a pre-existing condition, and the high costs of care borne by insured individuals through copayment or coinsurance requirements or coverage limitations. The US Government provides financial support for HIV care for low-income individuals through Ryan White–funded programs [81]. These help support clinical care in many circumstances but do not completely remove the influence and perceived influence of financial barriers on engagement in care. The potential impact of current and future reforms to the US health care system is unknown at this time, but more HIV-infected individuals are likely to qualify for and benefit from coverage under the new system.
Another limitation of this review is the large amount of overlap in the stages of engagement in care. It is difficult to delineate the independent contribution of, for example, poor retention in care, delayed initiation of antiretroviral therapy, and poor adherence to antiretroviral therapy, when the same individuals are prone to deficits in all of these areas. We have made best estimates from available data, but these are further limited by our cross-sectional representation of the longitudinal process of engagement in care. This limitation in our study is also a limitation of the existing literature, which has not clearly described this series of barriers in patient cohorts over time. Finally, this review is focused on the spectrum of engagement in HIV care in the United States and other resource-rich settings. Obstacles to diagnosis of HIV infection, linkage to and retention in HIV care, and receipt of and adherence to antiretroviral therapy in resource-limited settings are of critical importance to the global HIV epidemic and deserve their own review. Although many of the issues may be similar, the magnitude, causes, and solutions may be quite different.
Proponents of a test-and-treat strategy for HIV prevention are aware of the importance and formidable challenge posed by poor engagement in HIV care [4, 82]. A National Institutes of Health–funded feasibility study called TLC-Plus (Test, Link, and Care-Plus; HIV Prevention Trials Network [HPTN] 065) will assess programs for expanding HIV testing and treatment and linkage to appropriate HIV care and services [83]. Data from this and other studies will help inform the feasibility of test-and-treat strategies. Although complete eradication of HIV infection through test-and-treat programs is unlikely, incremental improvements in methods to overcome the greatest HIV care challenges today in the United States—undiagnosed HIV infection and inadequate engagement in HIV care—will improve the care of HIV-infected populations and decrease the incidence of HIV infection in the future.
Acknowledgments
Financial support. This work was supported by the US National Institute of Mental Health (R34 MH090870 to EMG) and the US National Institute of Allergy and Infectious Diseases (K01 AI067063 to EMG).
Potential conflicts of interest. All authors: no conflicts.
References
- 1.Gill VS, Lima VD, Zhang W, et al. Improved virological outcomes in British Columbia concomitant with decreasing incidence of HIV type 1 drug resistance detection. Clin Infect Dis. 2010;50:98–105. doi: 10.1086/648729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Das M, Chu PL, Santos GM, et al. Decreases in community viral load are accompanied by reductions in new HIV infections in San Francisco. PLoS One. 2010;5:e11068. doi: 10.1371/journal.pone.0011068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eldred L, Malitz F. Introduction [to the supplemental issue on the HRSA SPNS Outreach Initiative] AIDS Patient Care STDS. 2007;21(Suppl 1):S1–S2. [Google Scholar]
- 4.Dieffenbach CW, Fauci AS. Universal voluntary testing and treatment for prevention of HIV transmission. JAMA. 2009;301:2380–2. doi: 10.1001/jama.2009.828. [DOI] [PubMed] [Google Scholar]
- 5.Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373:48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- 6.Montaner JS, Hogg R, Wood E, et al. The case for expanding access to highly active antiretroviral therapy to curb the growth of the HIV epidemic. Lancet. 2006;368:531–6. doi: 10.1016/S0140-6736(06)69162-9. [DOI] [PubMed] [Google Scholar]
- 7.Attia S, Egger M, Muller M, Zwahlen M, Low N. Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. AIDS. 2009;23:1397–404. doi: 10.1097/QAD.0b013e32832b7dca. [DOI] [PubMed] [Google Scholar]
- 8.Donnell D, Baeten JM, Kiarie J, et al. Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: a prospective cohort analysis. Lancet. 2010;375:2092–8. doi: 10.1016/S0140-6736(10)60705-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wood E, Kerr T, Marshall BD, et al. Longitudinal community plasma HIV-1 RNA concentrations and incidence of HIV-1 among injecting drug users: prospective cohort study. BMJ. 2009;338:b1649. doi: 10.1136/bmj.b1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fang CT, Hsu HM, Twu SJ, et al. Decreased HIV transmission after a policy of providing free access to highly active antiretroviral therapy in Taiwan. J Infect Dis. 2004;190:879–85. doi: 10.1086/422601. [DOI] [PubMed] [Google Scholar]
- 11.HIV prevalence estimates–United States, 2006. MMWR Morb Mortal Wkly Rep. 2008;57:1073–6. [PubMed] [Google Scholar]
- 12.District of Columbia HIV/AIDS epidemiology update 2008. Washington, DC: Government of the District of Columbia, Department of Health, HIV/AIDS Administration; Available at: http://dchealth.dc.gov/DOH/frames.asp?doc=/doh/lib/doh/pdf/dc_hiv-aids_2008_updatereport.pdf. Accessed 28 June 2010. [Google Scholar]
- 13.Frew P, Omer S, Hixson B, Del Rio C. Spatial Clustering of HIV prevalence in Atlanta, Georgia, and population characteristics associated with case concentrations. San Francisco, CA, USA: 17th Conference on Retroviruses and Opportunistic Infections; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen TQ, Gwynn RC, Kellerman SE, et al. Population prevalence of reported and unreported HIV and related behaviors among the household adult population in New York City, 2004. AIDS. 2008;22:281–7. doi: 10.1097/QAD.0b013e3282f2ef58. [DOI] [PubMed] [Google Scholar]
- 15.Hall HI, Song R, Rhodes P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300:520–9. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campsmith ML, Rhodes PH, Hall HI, Green TA. Undiagnosed HIV prevalence among adults and adolescents in the United States at the end of 2006. J Acquir Immune Defic Syndr. 2010;53:619–24. doi: 10.1097/QAI.0b013e3181bf1c45. [DOI] [PubMed] [Google Scholar]
- 17.Pinkerton SD, Holtgrave DR, Galletly CL. Infections prevented by increasing HIV serostatus awareness in the United States, 2001 to 2004. J Acquir Immune Defic Syndr. 2008;47:354–7. doi: 10.1097/QAI.0b013e318160d57e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marks G, Crepaz N, Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS. 2006;20:1447–50. doi: 10.1097/01.aids.0000233579.79714.8d. [DOI] [PubMed] [Google Scholar]
- 19.Bhaskaran K, Hamouda O, Sannes M, et al. Changes in the risk of death after HIV seroconversion compared with mortality in the general population. JAMA. 2008;300:51–9. doi: 10.1001/jama.300.1.51. [DOI] [PubMed] [Google Scholar]
- 20.Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39:446–53. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- 21.Klein D, Hurley LB, Merrill D, Quesenberry CP., Jr Review of medical encounters in the 5 years before a diagnosis of HIV-1 infection: implications for early detection. J Acquir Immune Defic Syndr. 2003;32:143–52. doi: 10.1097/00126334-200302010-00005. [DOI] [PubMed] [Google Scholar]
- 22.Dybul M, Bolan R, Condoluci D, et al. Evaluation of initial CD4+ T cell counts in individuals with newly diagnosed human immunodeficiency virus infection, by sex and race, in urban settings. J Infect Dis. 2002;185:1818–21. doi: 10.1086/340650. [DOI] [PubMed] [Google Scholar]
- 23.Krawczyk CS, Funkhouser E, Kilby JM, Kaslow RA, Bey AK, Vermund SH. Factors associated with delayed initiation of HIV medical care among infected persons attending a southern HIV/AIDS clinic. South Med J. 2006;99:472–81. doi: 10.1097/01.smj.0000215639.59563.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jenkins TC, Gardner EM, Thrun MW, Cohn DL, Burman WJ. Risk-based human immunodeficiency virus (HIV) testing fails to detect the majority of HIV-infected persons in medical care Settings. Sex Transm Dis. 2006;33:329–33. doi: 10.1097/01.olq.0000194617.91454.3f. [DOI] [PubMed] [Google Scholar]
- 25.Missed opportunities for earlier diagnosis of HIV infection–South Carolina, 1997-2005. MMWR Morb Mortal Wkly Rep. 2006;55:1269–72. [PubMed] [Google Scholar]
- 26.Chadborn TR, Delpech VC, Sabin CA, Sinka K, Evans BG. The late diagnosis and consequent short-term mortality of HIV-infected heterosexuals (England and Wales, 2000–2004) AIDS. 2006;20:2371–9. doi: 10.1097/QAD.0b013e32801138f7. [DOI] [PubMed] [Google Scholar]
- 27.Schwarcz S, Hsu L, Dilley JW, Loeb L, Nelson K, Boyd S. Late diagnosis of HIV infection: trends, prevalence, and characteristics of persons whose HIV diagnosis occurred within 12 months of developing AIDS. J Acquir Immune Defic Syndr. 2006;43:491–4. doi: 10.1097/01.qai.0000243114.37035.de. [DOI] [PubMed] [Google Scholar]
- 28.Metsch LR, Pereyra M, Messinger S, et al. HIV transmission risk behaviors among HIV-infected persons who are successfully linked to care. Clin Infect Dis. 2008;47:577–84. doi: 10.1086/590153. [DOI] [PubMed] [Google Scholar]
- 29.Perkins D, Meyerson BE, Klinkenberg D, Laffoon BT. Assessing HIV care and unmet need: eight data bases and a bit of perseverance. AIDS Care. 2008;20:318–26. doi: 10.1080/09540120701594784. [DOI] [PubMed] [Google Scholar]
- 30.Torian LV, Wiewel EW, Liu KL, Sackoff JE, Frieden TR. Risk factors for delayed initiation of medical care after diagnosis of human immunodeficiency virus. Arch Intern Med. 2008;168:1181–7. doi: 10.1001/archinte.168.11.1181. [DOI] [PubMed] [Google Scholar]
- 31.Gardner LI, Metsch LR, Anderson-Mahoney P, et al. Efficacy of a brief case management intervention to link recently diagnosed HIV-infected persons to care. AIDS. 2005;19:423–31. doi: 10.1097/01.aids.0000161772.51900.eb. [DOI] [PubMed] [Google Scholar]
- 32.Giordano TP, Gifford AL, White AC, Jr., et al. Retention in care: a challenge to survival with HIV infection. Clin Infect Dis. 2007;44:1493–9. doi: 10.1086/516778. [DOI] [PubMed] [Google Scholar]
- 33.Mugavero MJ, Lin HY, Willig JH, et al. Missed visits and mortality among patients establishing initial outpatient HIV treatment. Clin Infect Dis. 2009;48:248–56. doi: 10.1086/595705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Park WB, Choe PG, Kim SH, et al. One-year adherence to clinic visits after highly active antiretroviral therapy: a predictor of clinical progress in HIV patients. J Intern Med. 2007;261:268–75. doi: 10.1111/j.1365-2796.2006.01762.x. [DOI] [PubMed] [Google Scholar]
- 35.Lundberg BE, Davidson AJ, Burman WJ. Epidemiology of Pneumocystis carinii pneumonia in an era of effective prophylaxis: the relative contribution of non-adherence and drug failure. AIDS. 2000;14:2559–66. doi: 10.1097/00002030-200011100-00019. [DOI] [PubMed] [Google Scholar]
- 36.Walzer PD, Evans HE, Copas AJ, Edwards SG, Grant AD, Miller RF. Early predictors of mortality from Pneumocystis jirovecii pneumonia in HIV-infected patients: 1985–2006. Clin Infect Dis. 2008;46:625–33. doi: 10.1086/526778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ikard K, Janney J, Hsu LC, et al. Estimation of unmet need for HIV primary medical care: a framework and three case studies. AIDS Educ Prev. 2005;17:26–38. doi: 10.1521/aeap.2005.17.Supplement_B.26. [DOI] [PubMed] [Google Scholar]
- 38.Olatosi BA, Probst JC, Stoskopf CH, Martin AB, Duffus WA. Patterns of engagement in care by HIV-infected adults: South Carolina, 2004–2006. AIDS. 2009;23:725–30. doi: 10.1097/QAD.0b013e328326f546. [DOI] [PubMed] [Google Scholar]
- 39.Hill T, Bansi L, Sabin C, et al. Data linkage reduces loss to follow-up in an observational HIV cohort study. J Clin Epidemiol. 2010;11:432–8. doi: 10.1016/j.jclinepi.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 40.Arici C, Ripamonti D, Maggiolo F, et al. Factors associated with the failure of HIV-positive persons to return for scheduled medical visits. HIV Clin Trials. 2002;3:52–7. doi: 10.1310/2XAK-VBT8-9NU9-6VAK. [DOI] [PubMed] [Google Scholar]
- 41.Coleman S, Boehmer U, Kanaya F, Grasso C, Tan J, Bradford J. Retention challenges for a community-based HIV primary care clinic and implications for intervention. AIDS Patient Care STDS. 2007;21:691–701. doi: 10.1089/apc.2006.0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mocroft A, Kirk O, Aldins P, et al. Loss to follow-up in an international, multicentre observational study. HIV Med. 2008;9:261–9. doi: 10.1111/j.1468-1293.2008.00557.x. [DOI] [PubMed] [Google Scholar]
- 43.Ndiaye B, Ould-Kaci K, Salleron J, et al. Incidence rate and risk factors for loss to follow-up in HIV-infected patients from five French clinical centres in Northern France - January 1997 to December 2006. Antivir Ther. 2009;14:567–75. [PubMed] [Google Scholar]
- 44.Ndiaye B, Ould-Kaci K, Salleron J, et al. Characteristics of and outcomes in HIV-infected patients who return to care after loss to follow-up. AIDS. 2009;23:1786–9. doi: 10.1097/QAD.0b013e32832e3469. [DOI] [PubMed] [Google Scholar]
- 45.Parienti JJ, Massari V, Descamps D, et al. Predictors of virologic failure and resistance in HIV-infected patients treated with nevirapine- or efavirenz-based antiretroviral therapy. Clin Infect Dis. 2004;38:1311–6. doi: 10.1086/383572. [DOI] [PubMed] [Google Scholar]
- 46.Teshale E, Kamimoto L, Harris N, Li J, Wang H. McKenna M. 12th Conference on Retroviruses and Opportunistic Infections. Boston, MA, USA: 2005. Estimated number of HIV-infected persons eligible for and receiving HIV antiretroviral therapy, 2003-United States [abstract] [Google Scholar]
- 47.Lima VD, Hogg RS, Montaner JS. Expanding HAART treatment to all currently eligible individuals under the 2008 IAS-USA Guidelines in British Columbia, Canada. PLoS One. 2010;5:e10991. doi: 10.1371/journal.pone.0010991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thompson MA, Aberg JA, Cahn P, et al. Antiretroviral treatment of adult HIV infection: 2010 recommendations of the International AIDS Society-USA panel. JAMA. 2010;304:321–33. doi: 10.1001/jama.2010.1004. [DOI] [PubMed] [Google Scholar]
- 49.Panel on Antiretroviral Guidelines for Adults, and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services; 2009. pp. 1–161. Available at: http:www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf. Accessed 20 September 2010. [Google Scholar]
- 50.Hart E, Curtis H, Wilkins E, Johnson M. National review of first treatment change after starting highly active antiretroviral therapy in antiretroviral-naive patients. HIV Med. 2007;8:186–91. doi: 10.1111/j.1468-1293.2007.00451.x. [DOI] [PubMed] [Google Scholar]
- 51.Yuan Y, L'Italien G, Mukherjee J, Iloeje UH. Determinants of discontinuation of initial highly active antiretroviral therapy regimens in a US HIV-infected patient cohort. HIV Med. 2006;7:156–62. doi: 10.1111/j.1468-1293.2006.00355.x. [DOI] [PubMed] [Google Scholar]
- 52.Li X, Margolick JB, Conover CS, et al. Interruption and discontinuation of highly active antiretroviral therapy in the multicenter AIDS cohort study. J Acquir Immune Defic Syndr. 2005;38:320–8. [PubMed] [Google Scholar]
- 53.Vo TT, Ledergerber B, Keiser O, et al. Durability and outcome of initial antiretroviral treatments received during 2000–2005 by patients in the Swiss HIV Cohort Study. J Infect Dis. 2008;197:1685–94. doi: 10.1086/588141. [DOI] [PubMed] [Google Scholar]
- 54.Mocroft A, Phillips AN, Soriano V, et al. Reasons for stopping antiretrovirals used in an initial highly active antiretroviral regimen: increased incidence of stopping due to toxicity or patient/physician choice in patients with hepatitis C coinfection. AIDS Res Hum Retroviruses. 2005;21:743–52. doi: 10.1089/aid.2005.21.743. [DOI] [PubMed] [Google Scholar]
- 55.Ahdieh-Grant L, Tarwater PM, Schneider MF, et al. Factors and temporal trends associated with highly active antiretroviral therapy discontinuation in the Women's Interagency HIV Study. J Acquir Immune Defic Syndr. 2005;38:500–3. doi: 10.1097/01.qai.0000138160.91568.19. [DOI] [PubMed] [Google Scholar]
- 56.Mills EJ, Nachega JB, Buchan I, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. JAMA. 2006;296:679–90. doi: 10.1001/jama.296.6.679. [DOI] [PubMed] [Google Scholar]
- 57.Bangsberg DR. Less than 95% adherence to nonnucleoside reverse-transcriptase inhibitor therapy can lead to viral suppression. Clin Infect Dis. 2006;43:939–41. doi: 10.1086/507526. [DOI] [PubMed] [Google Scholar]
- 58.Maggiolo F, Airoldi M, Kleinloog HD, et al. Effect of adherence to HAART on virologic outcome and on the selection of resistance-conferring mutations in NNRTI- or PI-treated patients. HIV Clin Trials. 2007;8:282–92. doi: 10.1310/hct0805-282. [DOI] [PubMed] [Google Scholar]
- 59.Horberg MA, Silverberg MJ, Hurley LB, et al. Effects of depression and selective serotonin reuptake inhibitor use on adherence to highly active antiretroviral therapy and on clinical outcomes in HIV-infected patients. J Acquir Immune Defic Syndr. 2008;47:384–90. doi: 10.1097/QAI.0b013e318160d53e. [DOI] [PubMed] [Google Scholar]
- 60.Lima VD, Harrigan R, Bangsberg DR, et al. The combined effect of modern highly active antiretroviral therapy regimens and adherence on mortality over time. J Acquir Immune Defic Syndr. 2009;50:529–36. doi: 10.1097/QAI.0b013e31819675e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lohse N, Obel N, Kronborg G, et al. Declining prevalence of HIV-infected individuals at risk of transmitting drug-resistant HIV in Denmark during 1997–2004. Antivir Ther. 2006;11:591–600. [PubMed] [Google Scholar]
- 62.von Wyl V, Yerly S, Burgisser P, et al. Long-term trends of HIV type 1 drug resistance prevalence among antiretroviral treatment-experienced patients in Switzerland. Clin Infect Dis. 2009;48:979–87. doi: 10.1086/597352. [DOI] [PubMed] [Google Scholar]
- 63.Gardner EM, Burman WJ, Steiner JF, Anderson PL, Bangsberg DR. Antiretroviral medication adherence and the development of class-specific antiretroviral resistance. AIDS. 2009;23:1035–46. doi: 10.1097/QAD.0b013e32832ba8ec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wheeler WH, Ziebell RA, Zabina H, et al. Prevalence of transmitted drug resistance associated mutations and HIV-1 subtypes in new HIV-1 diagnoses, U.S.-2006. AIDS. 2010;24:1203–12. doi: 10.1097/QAD.0b013e3283388742. [DOI] [PubMed] [Google Scholar]
- 65.Blower SM, Gershengorn HB, Grant RM. A tale of two futures: HIV and antiretroviral therapy in San Francisco. Science. 2000;287:650–4. doi: 10.1126/science.287.5453.650. [DOI] [PubMed] [Google Scholar]
- 66.Velasco-Hernandez JX, Gershengorn HB, Blower SM. Could widespread use of combination antiretroviral therapy eradicate HIV epidemics? Lancet Infect Dis. 2002;2:487–93. doi: 10.1016/s1473-3099(02)00346-8. [DOI] [PubMed] [Google Scholar]
- 67.Law MG, Prestage G, Grulich A, Van de Ven P, Kippax S. Modelling the effect of combination antiretroviral treatments on HIV incidence. AIDS. 2001;15:1287–94. doi: 10.1097/00002030-200107060-00011. [DOI] [PubMed] [Google Scholar]
- 68.Del Romero J, Castilla J, Hernando V, Rodriguez C, Garcia S. Combined antiretroviral treatment and heterosexual transmission of HIV-1: cross sectional and prospective cohort study. BMJ. 2010;340:c2205. doi: 10.1136/bmj.c2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bunnell R, Ekwaru JP, Solberg P, et al. Changes in sexual behavior and risk of HIV transmission after antiretroviral therapy and prevention interventions in rural Uganda. AIDS. 2006;20:85–92. doi: 10.1097/01.aids.0000196566.40702.28. [DOI] [PubMed] [Google Scholar]
- 70.Dodd PJ, Garnett GP, Hallett TB. Examining the promise of HIV elimination by ‘test and treat' in hyperendemic settings. AIDS. 2010;24:729–35. doi: 10.1097/QAD.0b013e32833433fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lima VD, Johnston K, Hogg RS, et al. Expanded access to highly active antiretroviral therapy: a potentially powerful strategy to curb the growth of the HIV epidemic. J Infect Dis. 2008;198:59–67. doi: 10.1086/588673. [DOI] [PubMed] [Google Scholar]
- 72.Craw JA, Gardner LI, Marks G, et al. Brief strengths-based case management promotes entry into HIV medical care: results of the antiretroviral treatment access study-II. J Acquir Immune Defic Syndr. 2008;47:597–606. doi: 10.1097/QAI.0b013e3181684c51. [DOI] [PubMed] [Google Scholar]
- 73.Conviser R, Pounds MB. The role of ancillary services in client-centred systems of care. AIDS Care. 2002;14(Suppl 1):S119–31. doi: 10.1080/09540120220150018. [DOI] [PubMed] [Google Scholar]
- 74.Tobias C, Cunningham WE, Cunningham CO, Pounds MB. Making the connection: the importance of engagement and retention in HIV medical care. AIDS Patient Care STDS. 2007;21(Suppl 1):S3–8. doi: 10.1089/apc.2007.9992. [DOI] [PubMed] [Google Scholar]
- 75.Rajabiun S, Cabral H, Tobias C, Relf M. Program design and evaluation strategies for the Special Projects of National Significance Outreach Initiative. AIDS Patient Care STDS. 2007;21(Suppl 1):S9–19. doi: 10.1089/apc.2007.9991. [DOI] [PubMed] [Google Scholar]
- 76.Bradford JB, Coleman S, Cunningham W. HIV System Navigation: an emerging model to improve HIV care access. AIDS Patient Care STDS. 2007;21(Suppl 1):S49–58. doi: 10.1089/apc.2007.9987. [DOI] [PubMed] [Google Scholar]
- 77.Bradford JB. The promise of outreach for engaging and retaining out-of-care persons in HIV medical care. AIDS Patient Care STDS. 2007;21(Suppl 1):S85–91. doi: 10.1089/apc.2007.9983. [DOI] [PubMed] [Google Scholar]
- 78.Mallinson RK, Rajabiun S, Coleman S. The provider role in client engagement in HIV care. AIDS Patient Care STDS. 2007;21(Suppl 1):S77–84. doi: 10.1089/apc.2007.9984. [DOI] [PubMed] [Google Scholar]
- 79.Logie C, Gadalla TM. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care. 2009;21:742–53. doi: 10.1080/09540120802511877. [DOI] [PubMed] [Google Scholar]
- 80.Naar-King S, Bradford J, Coleman S, Green-Jones M, Cabral H, Tobias C. Retention in care of persons newly diagnosed with HIV: outcomes of the Outreach Initiative. AIDS Patient Care STDS. 2007;21(Suppl 1):S40–8. doi: 10.1089/apc.2007.9988. [DOI] [PubMed] [Google Scholar]
- 81.The HIV/AIDS Program: Legislation. Available at: http://hab.hrsa.gov/law/leg.htm. Accessed 1 July 2010. [Google Scholar]
- 82.Johnston R, Collins C. Can we treat our way out of HIV?. AIDS Res Hum Retroviruses. 2010;26:1–4. doi: 10.1089/aid.2009.0267. [DOI] [PubMed] [Google Scholar]
- 83.Vermund SH, Hodder SL, Justman JE, et al. Addressing research priorities for prevention of HIV infection in the United States. Clin Infect Dis. 2010;50(Suppl 3):S149–55. doi: 10.1086/651485. [DOI] [PMC free article] [PubMed] [Google Scholar]