Abstract
Objectives.
This study assesses whether socioeconomic and demographic differences in reported mobility limitations are attributable to differential perceptions of mobility difficulty that result in the differential use of response categories.
Methods.
Data come from the Social Environment and Biomarkers of Aging Study and its parent study, the Taiwan Longitudinal Study of Aging. Ordered probit models with person-specific cut-points are used to test whether, after controlling for underlying mobility using objective performance measures, cut-points for reporting mobility limitations vary across groups defined by demographic and socioeconomic characteristics.
Results.
Age is the only characteristic that is consistently associated with the location of the cut-points for reporting mobility difficulty: At the same level of underlying mobility difficulty, older adults are more likely than younger adults are to report difficulty with all tasks except short walks. Other variables showed differences but only for one specific activity, for example, urban residents are more likely to report difficulty running than are rural residents with the same underlying level of mobility function.
Discussion.
For most mobility activities, there are no systematic differences in the perception of difficulty by individual characteristics. Thus, for older Taiwanese adults, differences in mobility limitations associated with socioeconomic status are more likely to reflect underlying differences in function than differences in how these groups report the same capacity. The usual loss of mobility with age, however, reflects both a decrease in capacity and a lowering of the threshold for reporting difficulty.
Keywords: Cut-point shifts, Mobility difficulty, Older adults, Taiwan
MOBILITY functioning is one of the most important factors that affects independence and quality of life in later years. Among older adults, difficulty with mobility is associated with less time spent outside the home and worse perceptions about general health status (Iezzoni, 2003; Singh-Manoux et al., 2006). Older adults with mobility limitations are also at higher risk of falling, developing disability, and dying earlier (Abellan van Kan et al., 2009; de Rekeneire et al., 2003; Newman et al., 2006; Simonsick et al., 2008). Given the potential impact that mobility limitations can have on the well-being of older adults, researchers have had a long-standing interest in whether mobility disability varies among groups defined by demographic characteristics and socioeconomic status.
Typically, measures used to assess disparities in mobility disability have been based on self-reported answers to questions regarding difficulty with various activities. Many surveys of older adults, for example, ask whether a respondent has difficulty (and if so, how much difficulty) with tasks such as walking 200–300 m, walking across a room, going up stairs, or getting into or out of a bed or chair. Responses to these types of questions often vary by such factors as age, sex, marital status, or socioeconomic status, suggesting the presence of disparities in mobility limitations.
However, differential understanding and use of self-reported response categories may contribute to these disparities (Bago d’Uva, O’Donnell, & van Doorslaer, 2008; Bago d’Uva, van Doorslaer, Lindeboom, & O’Donnell, 2008; Iburg, Salomon, Tandon, & Murray, 2001; Lindeboom & van Doorslaer, 2004). For instance, two individuals with the same underlying level of mobility function may report different levels of difficulty with mobility-related tasks because they may not have the same ideas and attitudes about what defines difficulty (Melzer, Lan, Tom, Deeg, & Guralnik, 2004). Differences in reporting difficulty also could result from varying expectations about health, differences in living environments that affect the ability to perform tasks, or from dissimilarities in the use of or access to combinations of personal and technological assistance with mobility-related activities (Bago d’Uva, van Doorslaer, et al., 2008; Melzer et al., 2004; Murray, Tandon, Salomon, Mathers, & Sadana, 2003; Salomon, Mathers, et al., 2003; Salomon, Tandon, Murray; World Health Survey Pilot Study Collaborating Group, 2004). In turn, these causes for differences in reporting behaviors may vary by individual characteristics resulting in systematic differences in reporting patterns and what is often referred to as reporting heterogeneity (Shmueli, 2003) or response category cut-point (threshold) shifts (Murray et al., 2003). For example, because income can afford many advantages, older adults with higher incomes may believe that they should be in good health. As a result, older adults with higher incomes may have higher thresholds for reporting difficulty (i.e., are less willing to acknowledge having difficulty) than older adults with lower incomes who may have lower expectations for health. Alternatively, the higher expectations of higher income adults could result in small problems making them feel that they are having difficulty, resulting in lower thresholds.
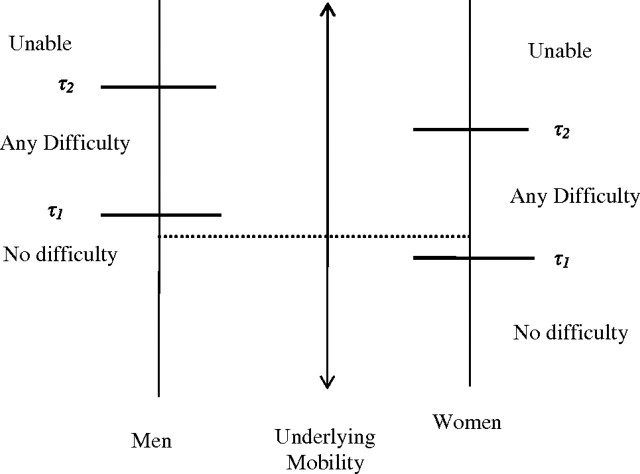
Cut-point shifts occur when, at a given level of “true” or underlying health, population subgroups systematically provide different evaluations of their health (Lindeboom & van Doorslaer, 2004; Murray et al., 2003; Shmueli, 2003). For example, Figure 1 shows how the same level of actual mobility functioning can be mapped into different categories of a three-category ordered response variable for difficulty walking (Bago d’Uva, O’Donnell, et al., 2008; Iburg et al., 2001; Salomon, Mathers, et al., 2003; Salomon et al., 2004; Tandon, Murray, Salomon, & King, 2003). The centerline represents the unobserved underlying level of difficulty walking a short distance. The scale on the left shows response category thresholds (τ1 and τ2) for men and the scale on the right shows the thresholds for women. The thresholds mark the levels of underlying mobility limitation at which an individual will choose one category over another (Bago d’Uva, O’Donnell, et al., 2008; Iburg et al., 2001; King, Murray, Salomon, & Tandon, 2004; Murray et al., 2003; Salomon et al., 2004). The lower thresholds mark the boundaries for reporting no difficulty with walking versus any difficulty with walking. The higher thresholds indicate the ability level for which a respondent would report the inability to walk rather than difficulty with walking. Given the true level of mobility indicated by the dotted line in Figure 1, a male respondent would report no difficulty, whereas a female respondent would indicate having difficulty. (Note that although Figure 1 shows that both thresholds are lower for women than for men, it is possible that one threshold could be lower and one higher; Bago d’Uva, O’Donnell, et al., 2008; Lindeboom & van Doorslaer, 2004.)
Figure 1.
Illustration of cut-point shifts by sex for difficulty walking (adapted from Bago d’Uva, O’Donnell, et al., 2008; Iburg et al., 2001; Murray et al., 2003; Salomon, Mathers, et al., 2003; Salomon et al., 2004; Tandon et al., 2003).
This analysis focuses on cut-point shifts in reporting mobility difficulty among older adults. Are differences in reported mobility difficulty attributable to differential perceptions of health that result in the differential use of response categories? We examine whether cut-points for reporting mobility limitations among older Taiwanese adults differ across demographic and socioeconomic groups.
Background
In addition to measurement error, variation in reports of difficulty is driven by two factors (King et al., 2004; Salomon, Tandon, Murray; World Health Survey Pilot Study Collaborating Group, 2003; Shmueli, 2003). First, reports of mobility difficulty are a function of underlying physiological capacity (King et al., 2004; Salomon, Tandon, et al., 2003; Shmueli, 2003; see also Freedman, 2009 and Verbrugge & Jette, 1994). Second, as the previous discussion of Figure 1 suggests, self-reports of mobility difficulty are also influenced by perceptions of difficulty that reflect differences in health expectations as well as differences in social and physical environments. These perceptions affect the translation of capacity into reports of difficulty. Demographic and socioeconomic disparities in measures of self-reported mobility difficulty, therefore, can emerge from group differences in underlying capacity and from group differences in perceptions of difficulty that result in cut-point shifts (King et al., 2004; Salomon, Tandon, et al., 2003; Shmueli, 2003).
Research on older adults that examines socioeconomic status and demographic variation in reports of mobility difficulty using techniques such as ordered logit or probit models assumes that all respondents use the same scale or criteria to define difficulty and, therefore, does not account for cut-point shifts (Salomon, Mathers, et al., 2003; Salomon, Tandon, et al., 2003; Tandon et al., 2003). In other words, all cross-group differences in reports of mobility difficulty are attributed to underlying mobility capacity, and the potential influence of differing perceptions is ignored. Results from such studies, therefore, may reflect both group differences in underlying capacity and group differences in the translation of capacity into reports of difficulty. Disregarding the association between demographic and socioeconomic characteristics and cut-points can lead to under- or overestimation of cross-population differences in underlying mobility capacity in the cross-section and changes in capacity over time (Bago d’Uva, O’Donnell, et al., 2008; Bago d’Uva, van Doorslaer, et al., 2008; Murray et al., 2003; Tandon et al., 2003). Studies that assume that respondents use difficulty scales in an identical manner cannot isolate and make cross-population comparisons of mobility capacity (some might argue that capacity is the preferred measure of health for cross-population comparisons; Salomon, Mathers, et al., 2003). These studies, however, can identify disparities in the disablement process, specifically disparities in the manifestation of capacity in the social and physical environment (Salomon, Mathers, et al., 2003).
A complementary line of research focuses on socioeconomic and demographic variation in perceptions of difficulty that results in cut-point shifts. The detection of cut-point shifts is rooted in a method that uses exogenous objective measures of health to fix the level of ability or standardize the underlying mobility scale so that remaining differences in reported difficulty can be attributed to cut-point shifts (Tandon et al., 2003). To analyze cut-point shifts, researchers have extended standard ordered probit models to allow the cut-points to vary by individual characteristics (King et al., 2004; Tandon et al., 2003). However, it is not possible to tease out the effects of a covariate on latent mobility capacity and on the cut-points without additional information or identifying assumptions (Tandon et al., 2003).
One school of work has used objective mobility performance tests in the hope that these measures capture the effects of background variables on latent mobility, leaving only their effects on the cut-points. Iburg and colleagues (2001) use seven measured performance tests to control for latent mobility in assessing the effect of background characteristics on the cut-points for self-reported and physician-assessed mobility ability. Melzer and colleagues (2004) use the MOBLI index of mobility limitations as a control in assessing cut-point shifts by age, sex, race, income, and education. Although these studies identify the presence (or absence) of cut-point shifts, it is possible that some sociodemographic differences in cut-points may also reflect sociodemographic differences in underlying capacity. Nonetheless, these studies provide insights into disparities in mobility difficulty by establishing whether part of the variation is attributable to differences in perceptions or how they are reported. Systematic variation in cut-points by socioeconomic and demographic characteristics indicates that perceptions play a role in disparities of reported mobility difficulty. Conversely, the absence of cut-point shifts across population subgroups, such as sex, suggests that differences in reported difficulty are more likely to reflect differences in underlying capacity rather than differences in perceptions (Melzer et al., 2004).
Another school of work has supplemented self-reported measures by preparing a set of vignettes intended to represent various levels of latent mobility and asking the respondent to classify these vignettes using the same categories as the self-reports (see Tandon et al., 2003 for details). Because all respondents classify the same vignettes, this additional information can be used to anchor the cut-points, permitting estimation of the effects of the same covariate on latent health and on the cut-points. However, because we do not have vignettes, we rely on the same type of exclusion restriction as the studies by Iburg and colleagues (2001) and Melzer and colleagues (2004) and use two mobility performance tests as controls in assessing differences in the perception of the cut-points by a number of socioeconomic status indicators and demographic characteristics.
This study expands on existing literature in a number of ways. First, we examine reporting heterogeneity in Taiwan. Because the translation of capacity into reports of difficulty occurs within a social environment (Freedman, 2009), patterns of cut-point shifts in Taiwan may differ from patterns in countries that have different social support and health care systems and different expectations for and beliefs about health. Unlike many Western populations examined in other studies of cut-point shifts, Taiwan has a social support system for older adults based more on family support and strong norms of familial obligation than on institutional or public assistance (Knodel, Ofstedal, & Hermalin, 2002); a universal health care system that supports the use of preventive care and the use of both Western and traditional Chinese medical providers (Ofstedal & Natividad, 2002); and beliefs about health and well-being that are influenced by several Chinese philosophies and religions, including Taoism, Buddhism, Confucianism, and the belief in Yin and Yang or the balance within one’s body and between the body and the environment (Chen, 2000; Lai & Surood, 2009). Examining cut-point shifts in a new setting will provide more insights into the role that the social and cultural context plays in the reporting of mobility limitations by older adults.
Second, we examine the potential effects of perceptions for multiple mobility-related activities. With some exceptions (e.g., Iburg et al., 2001), studies tend to focus on a single measure of general or gross mobility function (e.g., Bago d’Uva, O’Donnell, et al., 2008; Bago d’Uva, van Doorslaer, et al., 2008; Melzer et al., 2004). However, previous research shows that variation in reporting behaviors may be activity specific (Rahman & Liu, 2000; Shmueli, 2003). Therefore, when evaluating the mobility ability of older populations, it is important to know whether and how reporting differences may vary across specific mobility-related tasks.
Finally, we test for perceptual differences in mobility difficulty across infrequently examined demographic groups. Although previous research has also investigated health disparities by marital status and urban/rural residence, fewer studies have examined whether reporting heterogeneity exists for groups defined by these characteristics. The present study, therefore, also will shed additional light on whether differences in mobility difficulty by urban residence and marital status are more likely to reflect differences in capacity or a combination of capacity and perceptions.
METHODS
Data
The data used for the present analyses came from the Social Environment and Biomarkers of Aging Study (SEBAS) and its parent study, the Taiwan Longitudinal Study of Aging (TLSA). TLSA was first conducted in 1989 on a nationally representative sample of persons aged 60 and older (Hermalin, Liang, & Chang, 1989). Follow-up interviews have been conducted approximately every three years. The original 1989 sample has been extended twice to include a randomly selected representative sample of adults aged 50–66 years in 1996 and a randomly selected representative sample of adults aged 50–56 years in 2003. The first wave of SEBAS was conducted in 2000 and included a randomly selected subset of respondents interviewed in the 1999 wave of TLSA. SEBAS included both an in-home interview and a hospital-based physical exam (see Goldman et al., 2004 for a description of SEBAS). The sample for the second wave of SEBAS, which was conducted in 2006, consisted of the surviving exam participants from the first wave of SEBAS and a randomly selected sample of respondents who first entered the TLSA study in 2003.
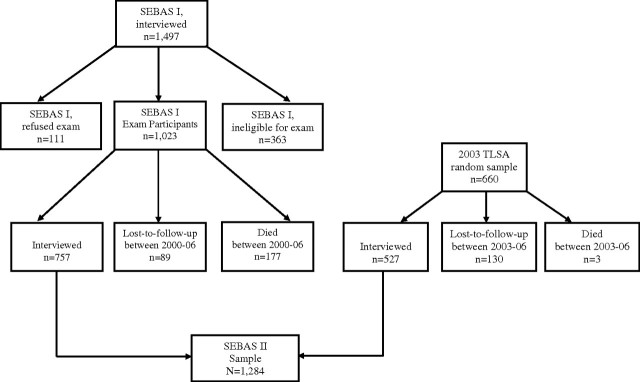
Our analyses focused on the 2006 wave of SEBAS, the first wave in which physical performance measures of mobility were collected. Of the 1,683 respondents eligible for the 2006 SEBAS, 1,284 were interviewed, 219 were lost-to-follow-up (LFU), and 180 died before the 2006 interview (see Figure 2). The response rate for the entire 2006 sample, therefore, was 85.4% (1,284 respondents of 1,503 respondents who survived and were eligible for SEBAS II). SEBAS I respondents who were LFU or who died between 2000 and 2006 were older, more likely to report difficulty with mobility-related activities, and more likely to report their ethnicity as Fukienese (vs. Hakka or Mainlander). Attrition of SEBAS I participants was not significantly related to sex or educational attainment. Respondents from the 2003 wave of the TLSA who were LFU or who died before being interviewed were more likely to be Fukienese but were no different from interviewed respondents in terms of age, sex, education, or mobility ability. Sample attrition, therefore, could result in under- or overestimation of cut-point differences by age and between ethnic groups.
Figure 2.
Construction of Social Environment and Biomarkers of Aging Study (SEBAS) II sample.
The final analysis sample excluded respondents who were missing data on key indicators. We excluded 39 cases that were missing either the performance-based measures (n = 31) or the self-reported mobility measures (n = 8) and an additional 54 cases missing covariates of interest. The resulting analysis sample contained 1,191 Taiwanese adults aged 53–94 years.
Measures
Performance-based measures.—
Analyses adjusted for underlying mobility function by incorporating two widely used measures of physical performance as the exogenous objective measures of mobility capacity: a timed 3-m walk and timed chair stands, both performed in the respondent’s home. Respondents were asked to walk a distance of 3 m at their usual walking speed. Because of space limitations, 12 respondents walked fewer than 3 m. For these respondents, who walked between 2 and 2.5 m, we scaled the time up proportionally. Respondents were allowed to use assistive devices if needed. Each respondent was timed for two walks. The Pearson correlation between the two walks was .9. Based on standard practices in the literature, the faster of the two walks was used (see, e.g., Guralnik et al., 2000; Rivera, Fried, Weiss, & Simonsick, 2008).
For the chair stand test, respondents were asked to stand up and sit down from an armless, straight back chair with a hard seat five times as quickly as possible. The back of the chair was placed against the wall and respondents were asked to keep their arms folded across their chest as they did the exercise. Respondents were timed from the starting seated position to the final standing position at the end of the fifth stand. Chair heights differed from home to home. Exploratory regressions of chair stand completion times on chair height, controlling for age, sex, and respondent’s height, revealed that chair height was significantly associated with completion times (results not shown). Chair stand test results, therefore, were adjusted to account for the variation in chair height. We regressed chair stand time on chair height, person height, and age separately for men and women. Based on these results, we adjust the observed completion time as follows:
,where ci represents the observed completion time for individual i, β is the coefficient for chair height,  is the mean chair height across the entire sample, and hi is the height of the chair used by the individual.
is the mean chair height across the entire sample, and hi is the height of the chair used by the individual.
Some respondents did not complete the timed walk or chair stand tests, most often for health or safety reasons. In order to include these respondents, we analyzed a number of different specifications of the timed walk and chair stand measures (results not shown). These analyses showed that (1) results were sensitive to the inclusion of those who could not perform the tests; (2) completion times for the walk and chair stand tests had a nonlinear relationship with the underlying level of mobility capacity; and (3) a small number of outliers on each test influenced this relationship. We, therefore, included for each performance measure a log transformation of the time it took to complete the test and a dummy variable indicating whether a respondent was unable to perform the test. We also examined a model including for each performance measure a linear term, quadratic term, and an indicator for inability (data not shown), but cut-point results varied little compared with the model using the log transformations. If a performance test was not completed because a respondent or the respondent’s family refused, the timed walk and chair stand measures were considered missing, and these respondents were excluded from analyses.
Self-reported mobility.—
We examined cut-point shifts in activities that require lower extremity function as a major component: running a short distance (20–30 m), walking 200–300 m, walking up two or three flights of stairs, squatting, and lifting or carrying something that weighs 11–12 kg. Respondents also reported on difficulty moving about the house and getting out of bed/standing up/sitting in a chair. However, because too few respondents reported difficulty with these activities, statistical models (described below) could not be run for these outcomes. For each of the other five activities, respondents were asked if they had any difficulty doing the activity and, if so, how much (some difficulty, great difficulty, or unable to do the activity). The small number of respondents reporting great difficulty prevented us from examining reporting differences across all four categories. Therefore, we examined cut-point differences between no difficulty (coded as 0), some or great difficulty (coded as 1), and unable to perform the task (coded as 2).
Demographic and socioeconomic characteristics.—
We examined cut-point shifts for groups defined by demographic characteristics, including age (53–64, 65–74, and 75 years or older), sex, marital status (currently married vs. not currently married), residence in an urban versus rural area, and ethnicity (Fukienese, Hakka, and Mainlander). Ethnic groups have been defined, in part, by the timing of their migration to Taiwan and the point of origin on mainland China. The Fukienese, coming from the southern Fukien province, and the Hakka, coming from the eastern Kwangtung province, began their migration from Mainland China as early as the 1600s (Lamely, 1981). A third wave of Chinese migration from Mainland China, beginning in 1949, consisted of nationalist military soldiers and nonmilitary supporters of the nationalist government (Mainlanders; Hermalin, Ofstedal, & Chang, 1996).
We also investigated whether reporting behaviors differed by socioeconomic status as measured by (1) the respondent’s and, if married, the spouse’s monthly income (measured in 2003 and categorized in quartiles) and (2) the respondent’s education (no formal education, primary, secondary, and postsecondary education).
Statistical Procedures
To examine whether demographic and socioeconomic differences in reported mobility difficulty are attributable to differential perceptions of mobility that result in the differential use of response categories, we use an ordered probit model that allows the cut-points to depend on individual characteristics (Bago d’Uva, van Doorslaer, et al., 2008; Iburg et al., 2001; King et al., 2004; Melzer et al., 2004; Tandon et al., 2003). The model is based on the assumptions that (1) there is an unobserved continuous latent variable that represents an individual’s perceived mobility level; (2) is normally distributed with a mean μi and variance of 1 and reflects the true underlying mobility level plus measurement error; and (3) μi is a function of a series of objective performance measures Xi (Iburg et al., 2001; King et al., 2004; Melzer et al., 2004; Tandon et al., 2003). Formally,
where is a row vector with the predictors of latent mobility based on the timed walk and timed chair stands.
The model further specifies that responses to the self-reported mobility items, yi, are observed assuming a cut-point model in which cut-points are allowed to depend on individual characteristics (Iburg et al., 2001; Melzer et al., 2004). Therefore, for a three-category outcome variable, responses yi, are observed as follows:
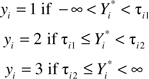 |
The cut-points, τij, are modeled as a function of individual characteristics (Iburg et al., 2001; King et al., 2004; Melzer et al., 2004; Tandon et al., 2003), so that:
and where is a row vector containing the individual-level characteristics, γ is a coefficient vector reflecting differences in the location of the first threshold, and δ is a coefficient vector reflecting differences in the distance between the two thresholds (King et al., 2004). Therefore, unlike a standard ordered probit model that ignores the potential influence of perceptions on reports of difficulty, this model accounts for the effect of perceptions by allowing the translation of mobility capacity into categories of the self-reported mobility measures (i.e., the cut-points) to vary by individual characteristics.
An important caveat is that the model assumes that, once we have controlled for the performance measures, socioeconomic characteristics are not associated with actual mobility functioning. If this assumption is incorrect, some of the cross-group differences in the cut-points could reflect differences in underlying capacity as well as perceptual differences in mobility difficulty.
The estimates of β, γ, and δ are derived using maximum likelihood methods, based on the assumption that responses are independent across study participants. A significant coefficient for a predictor of the cut-point between no difficulty and any difficulty, τi1, indicates that, controlling for the performance measures, the threshold for reporting difficulty varies by the predictor under examination. A significant δ coefficient signifies that, given the objective level of performance, the distance between the difficulty and inability cut-points (τi2 − τi1) differs by the characteristic of interest. For example, a significant negative coefficient for being female for the difficulty cut-point, with no effect on the perceived distance between the two cut-points (e.g., a significant γ coefficient and a nonsignificant δ coefficient), indicates that women have a lower threshold than men for reporting both difficulty and inability to complete a task. This scenario is depicted in Figure 1 in which the location of the cut-points for reporting difficulty, τ1, and inability, τ2, are lower for women than for men, but the distance between the first and second cut-point, τ2 − τ1, is the same for men and women. Thus, at the same level of underlying performance, women are more likely than men to report difficulty or inability with a task.
For each self-reported mobility outcome, we run a single model that includes the two performance measures to control for underlying mobility and simultaneously examines the effects of all socioeconomic and demographic covariates on the cut-points. For cut-point predictors with multiple categories—such as ethnicity, which has three—we perform a Wald test with a chi-square distribution to determine whether any of the categories differs from the others (StataCorp, 2007). Models are run in Stata 10.0 using the Generalized Linear Latent and Mixed Models procedure (Rabe-Hesketh, Skrondal, & Pickles, 2004; StataCorp, 2007).
RESULTS
Table 1 shows the distribution of the self-reported mobility difficulty measures overall and by sociodemographic characteristics. Overall, approximately 9%–16% of respondents report difficulty with a specific mobility-related activity (running, walking, going up stairs, squatting, and lifting or carrying 11–12 kg; see Table 1). The percentage reporting inability in an activity varies more widely, with as many as 18% reporting they are unable to run 20–30 m and as few as 8% reporting that they are unable to walk 200–300 m or walk up several flights of stairs.
Table 1.
Percent Reporting Each Level of Difficulty by Sociodemographic Characteristics
| Age |
Sex |
Marital status |
Ethnicity |
Income quartilesa |
Education attainment |
Urban residence |
||||||||||||||||
| 53–64 | 65–74 | 74+ | Men | Women | Not currently married | Currently married | Fukienese | Hakka | Mainlander | Q1 | Q2 | Q3 | Q4 | 0 years | 1–6 years | 7–12 years | 13+ years | Urban | Rural | N | Percent | |
| Run 20–30 m | ||||||||||||||||||||||
| No difficulty | 87.4 | 58.0 | 28.4* | 68.8 | 61.9* | 46.5 | 71.9* | 66.9 | 73.3 | 48.0* | 48.5 | 58.3 | 69.0 | 86.8* | 36.8 | 67.9 | 68.0 | 83.7* | 64.9 | 66.6 | 781 | 65.6 |
| With difficulty | 7.9 | 23.7 | 26.1 | 15.0 | 17.4 | 20.5 | 14.7 | 15.0 | 14.1 | 25.0 | 20.4 | 17.0 | 16.7 | 10.2 | 23.4 | 16.6 | 16.7 | 9.2 | 17.3 | 14.5 | 192 | 16.1 |
| Unable | 4.7 | 18.3 | 45.5 | 16.3 | 20.7 | 33.0 | 13.4 | 18.1 | 12.6 | 27.0 | 31.1 | 24.7 | 14.3 | 3.0 | 39.8 | 15.6 | 15.3 | 7.1 | 17.9 | 18.9 | 218 | 18.3 |
| Walk 200–300 m | ||||||||||||||||||||||
| No difficulty | 95.3 | 81.3 | 60.3* | 86.1 | 79.7* | 67.7 | 88.3* | 82.9 | 89.0 | 77.0 | 69.5 | 78.8 | 87.7 | 97.0* | 61.1 | 86.0 | 86.0 | 94.6* | 84.1 | 81.7 | 990 | 83.1 |
| With difficulty | 3.4 | 11.8 | 18.7 | 7.8 | 10.9 | 15.5 | 7.2 | 9.4 | 6.3 | 12.2 | 16.2 | 11.2 | 7.0 | 2.3 | 18.4 | 8.7 | 8.0 | 3.4 | 9.3 | 9.2 | 110 | 9.2 |
| Unable | 1.3 | 6.9 | 21.0 | 6.1 | 9.4 | 16.8 | 4.6 | 7.8 | 4.7 | 10.8 | 14.3 | 10.0 | 5.3 | 0.7 | 20.5 | 5.3 | 6.0 | 2.0 | 6.6 | 9.2 | 91 | 7.6 |
| Walk up 2–3 flight of stairs | ||||||||||||||||||||||
| No difficulty | 92.9 | 68.7 | 53.6* | 81.4 | 72.6* | 62.6 | 82.2* | 77.2 | 81.7 | 72.3 | 60.7 | 70.7 | 84.0 | 94.7* | 50.2 | 80.3 | 85.3 | 90.2* | 79.7 | 73.9* | 921 | 77.3 |
| With difficulty | 6.3 | 22.9 | 26.5 | 12.7 | 18.2 | 23.2 | 12.5 | 15.6 | 13.6 | 14.9 | 26.5 | 19.3 | 10.3 | 4.3 | 29.3 | 14.6 | 9.3 | 7.8 | 14.3 | 16.5 | 181 | 15.2 |
| Unable | 0.8 | 8.4 | 20.0 | 5.9 | 9.3 | 14.1 | 5.3 | 7.2 | 4.7 | 12.8 | 12.8 | 10.4 | 5.7 | 1.0 | 20.5 | 5.1 | 5.3 | 2.0 | 6.0 | 9.6 | 89 | 7.5 |
| Squatting | ||||||||||||||||||||||
| No difficulty | 87.6 | 23.4 | 45.8* | 75.3 | 66.8* | 56.9 | 76.2* | 71.8 | 75.9 | 62.8 | 56.7 | 66.8 | 74.3 | 88.2* | 49.8 | 73.0 | 72.0 | 85.8* | 69.9 | 72.4 | 850 | 71.4 |
| With difficulty | 89.9 | 22.9 | 23.9 | 14.8 | 17.1 | 19.9 | 14.5 | 16.0 | 11.5 | 21.0 | 21.0 | 20.1 | 14.3 | 8.2 | 23.4 | 16.0 | 14.7 | 10.2 | 14.7 | 16.7 | 189 | 15.9 |
| Unable | 3.6 | 13.7 | 30.3 | 9.8 | 16.2 | 23.2 | 9.3 | 12.2 | 12.6 | 16.2 | 22.3 | 13.1 | 11.3 | 3.6 | 26.8 | 11.1 | 13.3 | 4.1 | 15.5 | 10.9 | 152 | 12.8 |
| Lift or carry 11–12 kg | ||||||||||||||||||||||
| No difficulty | 88.2 | 68.3 | 45.8* | 82.2 | 61.9* | 54.9 | 78.8* | 73.0 | 78.0 | 64.9 | 56.1 | 68.7 | 78.7 | 88.5* | 47.7 | 75.4 | 80.0 | 85.1* | 71.9 | 73.4 | 867 | 72.8 |
| With difficulty | 8.4 | 17.9 | 22.6 | 9.1 | 20.2 | 21.6 | 11.7 | 13.5 | 13.1 | 19.6 | 20.4 | 14.3 | 13.0 | 8.6 | 22.6 | 13.2 | 11.3 | 10.5 | 14.1 | 14.3 | 169 | 14.2 |
| Unable | 3.4 | 13.7 | 31.6 | 8.8 | 18.0 | 23.6 | 9.5 | 13.5 | 8.9 | 15.5 | 23.5 | 17.0 | 8.3 | 3.0 | 29.7 | 11.4 | 8.7 | 4.4 | 14.1 | 12.3 | 155 | 13.0 |
| N | 619 | 262 | 310 | 640 | 551 | 297 | 894 | 852 | 191 | 148 | 328 | 259 | 300 | 304 | 239 | 507 | 150 | 295 | 700 | 491 | 1,191 | |
| Percent | 52.0 | 22.0 | 26.0 | 53.7 | 46.3 | 24.9 | 75.1 | 71.5 | 16.0 | 12.4 | 27.5 | 21.8 | 25.2 | 25.2 | 20.1 | 42.6 | 12.6 | 24.8 | 58.8 | 41.2 | 100.0 | |
Income quartiles are as follows: Q1 = $NT0 to $NT144,000; Q2 = $NT144,001 to $NT265,000; Q3 = $NT265,001 to $NT576,000; Q4 = $NT576,000+.
*Chi-square statistic significant at p < .05.
The average time to walk 3 m is 4.3 s (SD = 3.1), with 4.6% of respondents being unable to perform the test (data not shown). The average time to perform five chair stands is 10.9 s (SD = 4.6), with 10.7% of respondents unable to do the test (data not shown).
Reported difficulty with each of the five mobility-related activities varies significantly by sociodemographic characteristics (Table 1). For all five activities, difficulty differs by age, sex, marital status, income, and educational attainment. Specifically, reported difficulty increases with age, is worse for women than for men, and worse for respondents not currently married compared with currently married respondents. Reported difficulty is negatively associated with both income and education. In addition, difficulty running 20–30 m differs significantly by ethnicity (Mainlanders have the most difficulty), and walking up stairs differs by urban-rural residence, with residents of rural areas reporting more difficulty.
The results of tests for differences in thresholds for reporting impairment are shown in Table 2. In general, there is variation in the location of the threshold for reporting difficulty, τ1, but no significant differences in the spread of the thresholds for reporting difficulty and inability (i.e., no differences in log(τ2 − τ1)). Older adults have significantly lower thresholds for reporting difficulty versus no difficulty for all mobility-related activities except walking 200–300 m (for which differences in τ1 across age groups are not significant; χ2 = 4.17, p = .12). In other words, older adults are more likely to report difficulty with most mobility-related activities than are their younger counterparts with the same mobility capacity.
Table 2.
Results for the Cut-point Component of the Ordered Probit Model With Variable Cut-points
| Effects on the threshold between no difficulty and difficulty (τ1) |
Effects on the distance between difficulty and inability thresholds (log(τ2 − τ1)) |
|||||||||
| Run 20–30 m | Walk 200–300 m | Walk up stairs | Squatting | Carry 11–12 kg | Run 20–30 m | Walk 200–300 m | Walk up stairs | Squatting | Carry 11–12 kg | |
| Age (53–64 omitted), years | ||||||||||
| 65–74 | −0.93 (0.22)** | −0.42 (0.31) | −0.92 (0.26)** | −0.78 (0.22)** | −0.76 (0.23)** | 0.33 (0.19) | 0.04 (0.28) | −0.15 (0.21) | 0.03 (0.19) | −0.04 (0.21) |
| 75+ | −1.52 (0.25)** | −0.65 (0.32)* | −0.82 (0.29)** | −0.75 (0.25)** | −1.29 (0.26)** | 0.20 (0.20) | −0.10 (0.27) | −0.28 (0.22) | −0.16 (0.20) | −0.09 (0.23) |
| χ2 (2 df) | 39.11** | 4.17 | 13.68** | 14.29** | 25.33** | 3.09 | 0.48 | 1.74 | 1.34 | 0.18 |
| Women (men omitted) | −0.16 (0.19) | 0.02 (0.24) | −0.24 (0.21) | −0.30 (0.18) | −1.37 (0.20)** | 0.13 (0.15) | 0.06 (0.20) | −0.01 (0.15) | −0.08 (0.15) | 0.29 (0.18) |
| Married (not married omitted) | −0.05 (0.21) | 0.15 (0.25) | −0.27 (0.23) | −0.19 (0.20) | −0.06 (0.20) | −0.03 (0.15) | 0.18 (0.20) | −0.02 (0.15) | 0.07 (0.16) | −0.14 (0.16) |
| Ethnicity (Mainlander omitted) | ||||||||||
| Hakka | 0.90 (0.34)** | 0.58 (0.45) | 0.34 (0.39) | 0.31 (0.34) | 0.59 (0.34) | −0.26 (0.24) | −0.16 (0.37) | 0.22 (0.28) | −0.39 (0.27) | −0.20 (0.27) |
| Fukienese | 0.49 (0.28) | −0.08 (0.36) | 0.05 (0.32) | 0.10 (0.28) | 0.25 (0.28) | −0.35 (0.19) | −0.15 (0.27) | 0.16 (0.23) | −0.15 (0.21) | −0.35 (0.22) |
| χ2 (2 df) | 6.86* | 3.99 | 1.22 | 1.04 | 3.09 | 3.22 | 0.30 | 0.65 | 2.23 | 2.83 |
| Urban resident (rural residence omitted) | −0.53 (0.18)** | −0.14 (0.23) | 0.09 (0.20) | −0.06 (0.18) | −0.06 (0.18) | 0.18 (0.14) | 0.23 (0.20) | 0.16 (0.14) | 0.27 (0.15) | 0.03 (0.15) |
| Education (no formal education omitted) | ||||||||||
| Primary | 0.19 (0.23) | 0.19 (0.26) | 0.33 (0.23) | −0.14 (0.22) | −0.05 (0.22) | −0.12 (0.16) | 0.09 (0.20) | 0.01 (0.16) | −0.10 (0.17) | −0.15 (0.18) |
| Secondary | 0.50 (0.31) | 0.15 (0.39) | 0.67 (0.36) | −0.29 (0.30) | 0.28 (0.32) | −0.16 (0.23) | 0.00 (0.32) | −0.14 (0.27) | −0.31 (0.25) | −0.10 (0.27) |
| Postsecondary | 0.98 (0.33)** | 0.68 (0.44) | 0.34 (0.36) | 0.16 (0.32) | −0.21 (0.32) | −0.38 (0.26) | −0.10 (0.39) | 0.18 (0.27) | 0.00 (0.26) | 0.13 (0.25) |
| χ2 (3 df) | 10.45* | 2.46 | 3.90 | 2.62 | 2.11 | 2.17 | 0.41 | 0.92 | 1.93 | 1.92 |
| Income (first quartile omitted) | ||||||||||
| Second quartile | 0.07 (0.23) | 0.14 (0.28) | 0.02 (0.24) | 0.11 (0.23) | 0.19 (0.23) | −0.09 (0.17) | −0.28 (0.23) | −0.11 (0.17) | 0.11 (0.17) | −0.16 (0.19) |
| Third quartile | 0.10 (0.24) | 0.45 (0.31) | 0.56 (0.27)* | 0.07 (0.24) | 0.39 (0.24) | 0.15 (0.18) | −0.26 (0.27) | −0.23 (0.21) | −0.08 (0.19) | 0.10 (0.20) |
| Fourth quartile | 0.05 (0.30) | 0.68 (0.47) | 0.75 (0.39) | −0.02 (0.30) | 0.22 (0.31) | 0.53 (0.25)* | −0.08 (0.48) | −0.48 (0.35) | −0.13 (0.26) | 0.11 (0.27) |
| χ2 (3 df) | 0.20 | 3.25 | 7.37 | 0.37 | 2.53 | 6.58 | 1.70 | 2.57 | 1.38 | 1.87 |
Notes: Standard errors in parentheses.
*p < .05; ** p < .01.
Differences across other groups are less consistent. At the same level of function, women are more likely than men to report difficulty lifting and carrying heavy objects (i.e., women have lower thresholds than men). Hakka have higher thresholds than Mainlanders for reporting difficulty running a short distance and are, therefore, less likely to report difficulty with running than are Mainlanders with the same underlying ability. More educated respondents also have higher thresholds for reporting difficulty with running than their less educated counterparts. Urban residents, however, have lower thresholds for reports of difficulty with running. Thus, at the same level of underlying difficulty, urban residents are more likely to report running difficulty than are rural residents. Thresholds do not differ significantly by income.
Although there are no significant differences in the spread between cut-points, significant differences in the location of the first threshold imply that inability thresholds are also (1) lower for older adults in reports of inability to perform all mobility activities except walking a short distance; (2) lower for women than for men in reporting the inability to lift and carry heavy objects; (3) higher for Hakka than Mainlanders and for more educated than for less educated respondents in reports of the inability to run; and (4) lower for urban than for rural respondents in reporting the inability to run.
DISCUSSION
We identify cut-point differences in reporting mobility difficulty for groups defined by various demographic and socioeconomic characteristics. Two clear patterns emerge from the results. First, the location of thresholds for reporting difficulty versus no difficulty differs across some demographic and socioeconomic status groups but the spread between the thresholds for difficulty and inability do not. Perceptions, therefore, may have an effect on the absolute position of the thresholds but do not have an effect on the positioning of the thresholds relative to each other. Second, age emerges as the only characteristic that is consistently associated with difficulty cut-points. In the presence of controls for mobility capacity, older adults have lower thresholds for reporting impairment. In other words, at the same level of mobility performance, older adults are more likely than younger adults to report difficulty. Other respondent characteristics are not consistently related to reports of difficulty or inability for the mobility-related activities we examine. Therefore, with the exception of age differences, most of the socioeconomic and demographic differences in mobility difficulty reported in Table 1 are more likely to reflect differences in capacity rather than differences in perceptions that result in cut-point shifts.
Our results regarding age differences in thresholds for reporting mobility difficulty are consistent with findings from several studies. In both this study and the Melzer and colleagues (2004) study on older adults in the United States, younger respondents, compared with older respondents, tend to be more physically impaired before mobility difficulty is reported. Similarly, using the vignette approach, Boga d’Uva, O’Donnell and colleagues (2008) find that younger adults in China, India, and Indonesia are more likely than older adults with similar levels of actual mobility to report no difficulty moving around. These results suggest that younger and older adults may have different expectations for their health. Although older adults may find it acceptable to respond that they have difficulty, younger adults may not. Differences in reporting behaviors by age could also result from systematic age differences in the propensity to use assistive devices, in the availability and use of personal assistance, or in environmental demands (Melzer et al., 2004). It is also possible that these age differences may reflect cohort changes in perceptions of and expectations for health. Although the current generation of older adults has large families, low levels of education, and often worked in agriculture, future generations of elderly will have fewer children, more education, and more varied work experiences (Knodel et al., 2002). It will be interesting to see whether and how reporting heterogeneity changes over time in Taiwan.
Because patterns of cut-point shifts differ across the tasks we examine, our findings indicate that cut-point shifts are sensitive to the activity under review. For instance, we find differences by sex only for carrying 11–12 kg and urban-rural differences in thresholds exist only for jogging a short distance. Similarly, older adults have lower thresholds for all activities except walking 200–300 m. These patterns of reporting behavior could be related to the frequency with which an activity is done (Rahman & Liu, 2000). Women may not regularly carry heavy objects, and urban residents may not jog very often. Walking is a fairly common task for most older adults, but the other mobility-related activities examined here may be performed less often. Respondents who do not perform certain tasks regularly may be more likely to report difficulty than those who do the activity more often (Rahman & Liu, 2000). In a study of rural Bangladeshi men and women, Rahman and Liu (2000) found that differences by sex in reporting behaviors are largest for gendered activities and smallest for gender-neutral tasks.
Differences in reporting behaviors across tasks could also be related to the sensitivity with which the walking and chair stand tests capture the underlying functioning necessary to perform the mobility-related outcomes in the study. For example, we find the most sociodemographic differences in cut-points for running a short distance and no cut-point shifts for walking 200–300 m, which requires less exertion than running. Because we control specifically for walking ability, the model may better account for the level of functioning necessary for walking than for running. However, we also control for timed chair stands, which reflect, among other things, an individual’s level of exertion (Lord, Murray, Chapman, Munro, & Tiedemann, 2002; Lindemann et al., 2007). In fact, our results show that the chair stand test is a better predictor of underlying mobility functioning than is the walking test (see Supplementary Table 1) and, therefore, plays a more important role than the walking test in assessing individual heterogeneity in cut-points.
In the context of previous work, our study results suggest that reporting heterogeneity may be culture specific. Unlike many other studies of socioeconomic and demographic differences in thresholds for reporting mobility difficulty (e.g., Bago d’Uva, O’Donnell, et al., 2008; Bago d’Uva, van Doorslaer, et al., 2008; Iburg et al., 2001; Melzer et al., 2004), we find little evidence of systematic differences in reporting behaviors by sex, education, or income. Nor do we find evidence for threshold differences by marital status or urban residence. These differences across studies could be related to the homogeneity of the study population. In more homogeneous societies, cultural norms and values could more strongly influence health-reporting behaviors than do social or economic status, whereas the reverse may be true in more culturally heterogeneous populations. In Taiwan, dominant cultural norms and values are shaped by Confucian, Taoist, and Buddhist philosophies that stress, among other things, family interests and obligations over individual needs and the importance of balance and harmony between body and environment (Chen, 2000; Lai & Surood, 2009). Previous research on health in Chinese culture suggests that, given these underpinnings of Chinese society, older adults of Chinese descent may not only adapt more readily to age-related illness and deficits than older adults in Western societies but also may be more likely to regard age-related health changes as an accepted part of growing older (see, e.g., Leung, Wu, Lue, & Tang, 2004 and Ikles, 1998). As a result, many potential sources of socioeconomic and demographic differences in reporting behaviors—such as differences in health expectations, access to personal assistance and/or assistive technology, or living conditions with varying environmental demands—may be less relevant to reporting behaviors in Taiwan. However, as previously suggested, the age differences we report could indicate that cohort differences in reporting behaviors are emerging. Changing familial, educational, and work experiences of Taiwanese adults could lead to a shift in the relative influence of cultural norms versus social or economic status on reporting behaviors.
This research also points to the utility of collecting information on both self-reported mobility difficulty and mobility capacity as measured by physical performance tests. Self-reports of mobility difficulty are based on both underlying physiological capacity and perceptions of difficulty (King et al., 2004; Salomon, Tandon, et al., 2003; Shmueli, 2003; see also Freedman, 2009 and Verbrugge & Jette, 1994). These difficulty measures, therefore, reflect an individual’s belief of how well they have adapted to functional deficits within the environments in which they live. However, without measures of capacity, it is not possible to determine whether the translation of capacity into difficulty also reflects perceptions. At the same time, performance measures of capacity alone do not speak to whether or how well individuals may have adapted to functional limitations (Guralnik, Branch, Cummings, &, Curb, 1989). To fully understand the causes of, and potential interventions for mobility disability and disparities in mobility disability, information on both capacity and self-reported difficulty are needed.
There are several limitations to this study. Although we are able to detect whether there are threshold differences in reporting mobility problems for groups defined by demographic characteristics and socioeconomic status, the identification of effects in our model comes from two assumptions: First, the relatively mild assumption that the performance tests have no effect on the cut-points within groups defined by the background characteristics and second, the stronger assumption that the background characteristics have no effect on true latent mobility after controlling for the performance measures. If the objective tests fail to fully control for the effects of background characteristics, our estimates of cut-point shifts may reflect in part some differences in underlying mobility capacity. On the other hand, studies that ignore cut-point shifts attribute all observed differences to underlying capacity. We are also limited by having few respondents who reported difficulty with walking across a room or transferring in or out of a bed or chair, so we could not run the statistical models for these outcomes. Both of these activities frequently appear in aging surveys; it would be useful to understand whether there are differences in reporting behaviors for these tasks. Finally, because cultural differences in the aging experience affect analyses of cut-point shifts, these results cannot be generalized beyond the older Taiwanese population. The results do indicate, however, that future analyses of disability disparities in other settings need to account for or address the potential effects of reporting heterogeneity.
Mobility disability is most often assessed using self-reported responses to questions that ask respondents to indicate how much difficulty they have doing such tasks as jogging, walking 200–300 m, going up stairs, walking across the room, and the like. In general, the criteria respondents use to decide and report whether they have difficulty with an activity are unknown. Two individuals with the same underlying mobility ability, therefore, may have different perceptions of what constitutes difficulty, resulting in different reports of the level of difficulty with mobility tasks. The analyses presented here control for measured performance tests to detect whether perceptions of mobility difficulty vary across population subgroups. In general, with the exception of threshold differences across age groups, we find relatively little evidence of cut-point shifts for reporting mobility difficulty or inability among older Taiwanese adults. Therefore, within this population, differences in mobility limitations by sex, socioeconomic status, marital status, or urban residence are more likely to reflect differences in mobility capacity rather than differences in reporting behaviors stemming from varying perceptions of difficulty. The usual loss of mobility with age, however, reflects both a decrease in capacity and a lowering of the threshold for reporting difficulty.
FUNDING
This work was supported by the Demography and Epidemiology Unit of the Behavioral and Social Research Program of the National Institute of Aging (R01AG16790 and R01AG16661).
SUPPLEMENTARY MATERIAL
Supplementary material can be found at: http://psychsocgerontology.oxfordjournals.org/
Acknowledgments
Author contributions: J.C. Cornman planned the study, performed all statistical analyses, and wrote the paper. D. Glei contributed to designing and collecting data, advised on statistical procedures, and assisted with revising the paper. G. Rodríguez advised on statistical procedures and contributed to writing and revising the paper. N. Goldman contributed to designing and collecting data and to revising the paper. B.-S. Hurng contributed to the study design and field implementation and supervision. M. Weinstein contributed to designing and collecting the data, to conceptual planning of the paper, and to writing and revising the paper.
References
- Abellan van Kan G, Rolland Y, Andrieu S, Bauer J, Beauchet O, Bonnefoy M, Vellas B, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people: An International Academy on Nutrition and Aging (IANA) Task Force. Journal of Nutrition, Health and Aging. 2009;13:881–889. doi: 10.1007/s12603-009-0246-z. doi:10.1007/s12603-009-0246-z. [DOI] [PubMed] [Google Scholar]
- Bago d’Uva T, O’Donnell O, van Doorslaer E. Differential health reporting by education level and its impact on the measurement of health inequalities among older Europeans. International Journal of Epidemiology. 2008;37:1375–1383. doi: 10.1093/ije/dyn146. doi:10.1093/ije/dyn146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bago d’Uva T, van Doorslaer E, Lindeboom M, O’Donnell O. Does reporting heterogeneity bias the measurement of health disparities? Health Economics. 2008;17:351–375. doi: 10.1002/hec.1269. doi:10.1002/hec.1269. [DOI] [PubMed] [Google Scholar]
- Chen YC. Chinese values, health and nursing. Journal of Advanced Nursing. 2000;36:270–273. doi: 10.1046/j.1365-2648.2001.01968.x. [DOI] [PubMed] [Google Scholar]
- de Rekeneire N, Visser M, Peila R, Nevitt MC, Cauley JA, Tylavsky FA, Harris TB, et al. Is a fall just a fall: Correlates of falling in healthy older persons. The Health, Aging and Body Composition Study. Journal of the American Geriatrics Society. 2003;51:841–846. doi: 10.1046/j.1365-2389.2003.51267.x. doi:10.1046/j.1365-2389.2003.51267.x. [DOI] [PubMed] [Google Scholar]
- Freedman VA. Adopting the ICF language for studying late-life disability: A field of dreams? Journal of Gerontology Series A: Biological Sciences and Medical Sciences. 2009;64A:1172–1174. doi: 10.1093/gerona/glp095. doi:10.1093/gerona/glp095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman N, Weinstein M, Cornman J, Singer B, Seeman T, Chang M.-C. Sex differentials in biological risk factors for chronic disease: Estimates from population-based surveys. Journal of Women’s Health. 2004;13:393–403. doi: 10.1089/154099904323087088. doi:10.1089/154099904323087088. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Branch LG, Cummings SR, Curb JD. Physical performance measures in aging research. Journal of Gerontology: Medical Sciences. 1989;44:M141–M146. doi: 10.1093/geronj/44.5.m141. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, Wallace RB. Lower extremity function and subsequent disability: Consistency across studies, predictive models and value of gait speed alone compared with the short physical performance battery. Journal of Gerontology: Medical Sciences. 2000;55A:M221–M231. doi: 10.1093/gerona/55.4.m221. doi:10.1093/gerona/55.4.M221. [DOI] [PubMed] [Google Scholar]
- Hermalin AI, Liang J, Chang MC. Ann Arbor, MI: University of Michigan; 1989. Survey of health and living status of the elderly in Taiwan: Questionnaire and survey design (Comparative Study of the Elderly in Four Asian Countries Research Report No 1, PSC Publications) [Google Scholar]
- Hermalin AI, Ofstedal MB, Chang MC. Types of supports for the aged and their providers in Taiwan. In: Hareven T, editor. Aging and generational relations over the life course: A historical and cross-cultural perspective. New York: Walter de Gruyter; 1996. pp. 400–437. [Google Scholar]
- Iburg KM, Salomon JA, Tandon A, Murray CJL. Cross-population comparability of self-reported and physician-assessed mobility levels: Evidence from the Third National Health and Nutrition Examination Survey. 2001, November. Global Programme on Evidence for Health Policy, Discussion Paper No. 14. Geneva, Switzerland: World Health Organization. Retrieved from www.who.int/entity/healthinfo/paper14.pdf. [Google Scholar]
- Iezzoni L. When walking fails: Mobility problems of adults with chronic conditions. Berkeley: University of California Press; 2003. [Google Scholar]
- Ikles C. The experience of dementia in China. Culture, Medicine and Psychiatry. 1998;22:257–283. doi: 10.1023/a:1005399215185. doi:10.1023/A:1005399215185. [DOI] [PubMed] [Google Scholar]
- King G, Murray CJL, Salomon JA, Tandon A. Enhancing the validity and cross-cultural comparability of measurement in survey research. American Political Science Review. 2004;98:191–207. doi:10.1017/S000305540400108X. [Google Scholar]
- Knodel J, Ofstedal MB, Hermalin AI. The demographic, socioeconomic, and cultural context of the four study countries. In: Hermalin AI, editor. The well-being of the elderly in Asia: A four-country comparative study. Ann Arbor: University of Michigan Press; 2002. pp. 25–63. [Google Scholar]
- Lai DWL, Surood S. Chinese health beliefs of older Chinese in Canada. Journal of Aging and Health. 2009;21:38–62. doi: 10.1177/0898264308328636. doi:10.1177/0898264308328636. [DOI] [PubMed] [Google Scholar]
- Lamely HJ. Subethnic rivalry in the Ch’ing period. In: Ahern EM, Gates H, editors. The anthropology of Taiwanese society. Stanford, CA: Stanford University Press; 1981. pp. 282–313. [Google Scholar]
- Leung KK, Wu EC, Lue BH, Tang LY. The use of focus groups in evaluating quality of life components among elderly Chinese people. Quality of Life Research. 2004;13:179–190. doi: 10.1023/B:QURE.0000015291.79826.a8. doi:10.1023/B:QURE.0000015291.79826.a8. [DOI] [PubMed] [Google Scholar]
- Lindeboom M, van Doorslaer E. Cut-point shift and index shift in self-reported health. Journal of Health Economics. 2004;23:1083–1099. doi: 10.1016/j.jhealeco.2004.01.002. doi:10.1016/j.jhealecs.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Lindemann U, Muche R, Stuber M, Zijlstra W, Hauer K, Becker C. Coordination of strength exertion during the chair-rise movement in very old people. Journal of Gerontology: Medical Sciences. 2007;62A:636–640. doi: 10.1093/gerona/62.6.636. [DOI] [PubMed] [Google Scholar]
- Lord SR, Murray SM, Chapman K, Munro B, Tiedemann A. Sit-to-stand performance depends on sensation, speed, balance, & psychological status in addition to strength in older people. Journal of Gerontology: Medical Sciences. 2002;57A:M539–M543. doi: 10.1093/gerona/57.8.m539. doi:10.1093/gerona/57.8.M539. [DOI] [PubMed] [Google Scholar]
- Melzer D, Lan T.-Y., Tom BDM, Deeg DJH, Guralnik JM. Variation in thresholds for reporting mobility disability between national population subgroups and studies. Journal of Gerontology: Medical Sciences. 2004;59A:1295–1303. doi: 10.1093/gerona/59.12.1295. doi:10.1093/gerona/59.12.1295. [DOI] [PubMed] [Google Scholar]
- Murray CJL, Tandon A, Salomon JA, Mathers CD, Sadana R. Cross-population comparability of evidence for health policy. In: Murray CJL, Evans DB, editors. Health systems performance assessment: Debates, methods and empiricism. Geneva, Switzerland: World Health Organization; 2003. pp. 705–713. Retrieved from http://whqlibdoc.who.int/publications/2003/9241562455_%28part4%29_%28chp50-60%29.pdf. [Google Scholar]
- Newman AB, Simonsick EM, Naydeck BL, Boudreau RM, Kritchevsky SB, Nevitt MC, Harris TB. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. Journal of the American Medical Association. 2006;295:2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- Ofstedal MB, Natividad JN. Patterns of healthcare utilization. In: Hermalin AI, editor. The well-being of the elderly in Asia: A four-country comparative study. Ann Arbor: University of Michigan Press; 2002. pp. 25–63. [Google Scholar]
- Rabe-Hesketh S, Skrondal A, Pickles A. GLLAMM manual. 2004, October. U.C. Berkeley Division of Biostatistics Working Paper Series. Working Paper 160. Retrieved from http://www.gllamm.org/docum.html. [Google Scholar]
- Rahman MO, Liu J-H. Gender differences in functioning for older adults in rural Bangladesh: The impact of differential reporting? Journal of Gerontology: Medical Sciences. 2000;55:M28–M33. doi: 10.1093/gerona/55.1.m28. doi:10.1093/gerona/55.1.M28. [DOI] [PubMed] [Google Scholar]
- Rivera JA, Fried LP, Weiss CO, Simonsick EM. At the tipping point: Predicting severe mobility difficulty in vulnerable older women. Journal of American Geriatrics Society. 2008;56:1417–1423. doi: 10.1111/j.1532-5415.2008.01819.x. doi:10.1111/j.1532-5415.2008.01819.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon JA, Mathers CD, Chatterji S, Sadana R, Üstün BT, Murray CJL. Quantifying individual levels of health: Definitions, concepts and measurement issues. In: Murray CJL, Evans DB, editors. Health systems performance assessment: Debates, methods and empiricism. Geneva, Switzerland: World Health Organization; 2003. pp. 301–318. Retrieved from http://whqlibdoc.who.int/publications/2003/9241562455_%28part4%29_%28chp25-33%29.pdf. [Google Scholar]
- Salomon JA, Tandon A, Murray CJL. World Health Survey Pilot Study Collaborating Group. Unpacking health perceptions using anchoring vignettes. In: Murray CJL, Evans DB, editors. Health systems performance assessment: Debates, methods and empiricism. Geneva, Switzerland: World Health Organization; 2003. pp. 401–407. Retrieved from http://whqlibdoc.who.int/publications/2003/9241562455_%28part4%29_%28chp25-33%29.pdf. [Google Scholar]
- Salomon JA, Tandon A, Murray CJL World Health Survey Pilot Study Collaborating Group. Comparability of self rated health: Cross sectional multi-country survey using anchoring vignettes. British Medical Journal. 2004;328 doi: 10.1136/bmj.37963.691632.44. doi:10.1136/bmj.37963.691632.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shmueli A. Socio-economic and demographic variation in health and in its measures: The issue of reporting heterogeneity. Social Science & Medicine. 2003;57:125–134. doi: 10.1016/s0277-9536(02)00333-7. doi:10.1016/S0277-9536(02)00333-7. [DOI] [PubMed] [Google Scholar]
- Simonsick EM, Newman AB, Visser M, Goodpaster B, Kritchevsky SB, Rubin S …; Health, Aging and Body Composition Study. Mobility limitation in self-described well-functioning older adults: Importance of endurance walk testing. Journal of Gerontology Series A: Biological Sciences and Medical Sciences. 2008;63:841–847. doi: 10.1093/gerona/63.8.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh-Manoux A, Martikainen P, Ferrie J, Zins M, Marmot M, Goldberg M. What does self rated health measure? Results from the British Whitehall II and French Gazel cohort studies. Journal of Epidemiology and Community Health. 2006;60:364–372. doi: 10.1136/jech.2005.039883. doi:10.1136/jech.2005.039883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: Release 10. College Station, TX: StataCorp LP; 2007. [Google Scholar]
- Tandon A, Murray CJL, Salomon JA, King G. Statistical models for enhancing cross-population comparability. In: Murray CJL, Evans DB, editors. Health systems performance assessment: Debates, methods and empiricism. Geneva, Switzerland: World Health Organization; 2003. pp. 727–746. Retrieved from http://whqlibdoc.who.int/publications/2003/9241562455_%28part4%29_%28chp50-60%29.pdf. [Google Scholar]
- Verbrugge LM, Jette AM. The disablement process. Social Science & Medicine. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. doi:10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]