Abstract
Background.
Although weight loss reduces risk for comorbid diseases, many observational studies suggest that weight loss is associated with increased mortality risk, leading to reluctance by clinicians to consider weight reduction as a strategy to maintain health and independence in older adults. However, whether the observed weight loss is intentional is difficult to determine and may not accurately represent the mortality risk associated with intentional weight reduction. Data from the Arthritis, Diet, and Activity Promotion Trial (ADAPT) were used to determine whether randomization to a weight reduction program was associated with total mortality in overweight/obese older adults.
Methods.
ADAPT (n = 318; mean age 69 ± 6 years, body mass index 34 ± 5 kg/m2, 72% female) assessed the influence of weight loss (achieved through dietary counseling and lifestyle modification) and/or exercise on function in overweight/obese older adults with knee osteoarthritis. ADAPT ended in December 1999. Participant vital was ascertained status through December 2006 using the National Death and Social Security Indexes.
Results.
The mortality rate for those randomized to the 18-month weight loss intervention (n = 159, mean weight loss = −4.8 kg, 15 deaths) was lower than that for those not randomized to the weight loss intervention (n = 159, mean weight loss = −1.4 kg, 30 deaths; hazard rate ratio = 0.5, 95% confidence interval 0.3–1.0). Results were not appreciably changed when analyses were stratified by age, gender, baseline weight status, or magnitude of weight loss.
Conclusions.
In older adults, intentional weight loss was not associated with increased total mortality and may reduce mortality risk. Observational studies of weight loss, especially when intentionality cannot be rigorously established, may be misleading with respect to the effect of weight loss on mortality.
Keywords: Intentional weight loss, Mortality, Aging, Obesity
CONTROVERSY surrounds the potential risks and benefits of weight loss in older adults. On the one hand, outcomes of weight loss trials demonstrate that weight loss positively influences several weight-related comorbidities in older adults (1–4). On the other hand, data from observational studies show that weight loss is associated with increased risk of mortality (5–8). It is well recognized that sudden unexpected weight loss can be a presenting sign of underlying subclinical disease, which may explain some of the observational data. Some investigators have tried to distinguish intentional from unintentional weight loss, with mixed results (6–11), and it is not entirely clear that the self-report of weight loss intention is accurate enough to completely address the issue in an observational context. Therefore, associations from observational studies cannot fully resolve the question of whether intentional weight loss is beneficial or harmful, an issue that is important, given the increasing prevalence of obesity among this segment of the population (12,13). A randomized clinical trial can address this question because the randomization process resolves the issue of confounding by subclinical disease, and virtually all the weight loss observed would be expected to be intentional. The resolution of the association between weight loss and mortality is clinically important because there is a reluctance to recommend weight loss to obese older adults, a group in whom the theoretical harms of weight loss would be most apparent, given the findings from observational studies.
In order to evaluate the effect of intentional weight loss on mortality risk of older adults, we determined the vital status of the participants randomized in the Arthritis, Diet, and Activity Promotion Trial (ADAPT), an 18-month randomized trial of weight loss and/or exercise in overweight and obese older adults with osteoarthritis (OA) of the knee. The mortality rates between those randomized to the weight loss intervention and those not randomized to the weight loss intervention were compared.
METHODS
Participants
The ADAPT study was a single-blind randomized controlled intervention trial designed to determine whether dietary weight loss and long-term exercise training, alone or in combination, could improve physical function and mobility and reduce pain in overweight and obese (mean baseline body mass index [BMI] 34 kg/m2) men and women aged 60 years and older with knee OA. Between November 1996 and June 1998, overweight and obese older men and women with knee OA from North Carolina were recruited and randomized to one of the four treatment groups: dietary weight loss, exercise, dietary weight loss + exercise, or a healthy lifestyle control. Study exclusion criteria included known cardiovascular disease, severe hypertension, chronic obstructive pulmonary disease, and other comorbidities that could limit mobility and participation in regular exercise. All ADAPT study participants provided written informed consent, and this study was approved by the Institutional Review Board at Wake Forest University Health Sciences and is registered with clinicaltrials.gov (NCT00979043).
The number of participants in the present analysis differs slightly from the primary analysis of ADAPT, which included 316 participants, 158 randomized to a weight loss intervention and 158 to a non–weight loss intervention (1). There were two participants who were randomized but never participated in the ADAPT intervention (one in a weight loss intervention group and one in a non–weight loss intervention group) and were not included in the analyses of primary ADAPT outcomes (1). However, these two participants were included in our unadjusted primary analysis, so that our intention-to-treat sample had 159 participants each in the weight loss and in the non–weight loss intervention groups. However, pertinent covariate information was not available on these two participants, so we were unable to include them in the stratified analyses. Therefore, the final sample for our stratified analyses included the 158 participants in the non–weight loss intervention and the 158 participants in the weight loss intervention, who were included in the analysis of the ADAPT primary outcomes (Figure 1).
Figure 1.
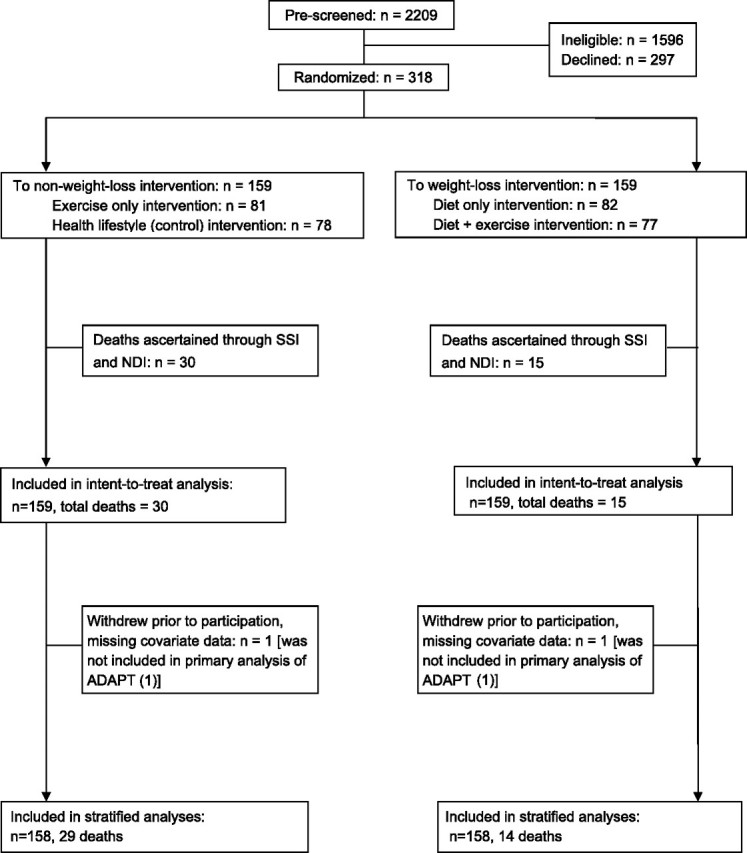
Participation and death ascertainment in the Arthritis, Diet, and Activity Promotion Trial (ADAPT).
Interventions
The dietary weight loss and exercise interventions are described in detail elsewhere (1). Briefly, the dietary weight loss intervention was divided into three phases for a period of 18 months: intensive (Months 1–4, to increase awareness if the need for behavior modification to change eating habits), transition (Months 5–6, to set new goals in order to prevent relapse or to lose weight in participants who had not achieved weight loss goals), and maintenance (Months 7–18, to maintain weight loss or provide additional support in participants who had difficulty losing weight). The goal of the dietary weight loss was to lose 5% of baseline body weight for a period of 18 months. The exercise intervention consisted of 3 days/week of an aerobic exercise phase (15 minutes of walking within 50%–75% of heart rate reserve), resistance training (15 minutes, included two sets of 12 reps of lower body strength training), a second aerobic phase (15 minutes), and a cooldown (15 minutes) for a period of 18 months. Participants in the dietary weight loss + exercise group followed both programs. The healthy lifestyle control group attended 3 monthly health education programs on OA, obesity, and exercise for the first 3 months followed by monthly phone contact for Months 4–6 and then bimonthly phone contact for Months 7–18.
Data Collection
Death ascertainment.—
All death adjudication was completed without knowledge of randomization group. Deaths during follow-up were ascertained using the Social Security Index (SSI) and the National Death Index (NDI), which has improved specificity and sensitivity compared with the SSI (14). Recently, the agreement in death ascertainment between the two databases was reported to be greater than 94% when identification information similar to what was available in our study was used (15). Two deaths occurred during the ADAPT trial (1), and 43 posttrial deaths were ascertained through the NDI and SSI searches. Because NDI data are available through December 31, 2006, that was used as the censoring date for all analyses. No attempt was made to identify cause of death.
Covariates.—
Body weight and height (without shoes) were measured at baseline and at 6 and 18 months of follow-up using the same calibrated scale. BMI was calculated as weight (kg)/height (m)2. Demographic information was obtained from self-report, and prevalence of comorbid conditions was based on medical history and physical examination.
Statistical Analyses
Because our primary purpose was to determine the effect of intentional weight loss on total mortality, participants in the dietary weight loss group and in the dietary weight loss + exercise group were combined as “weight loss intervention” and those in the exercise-only intervention and in the healthy lifestyle control were combined as “non–weight loss intervention.” The weight loss and non–weight loss groups were compared at baseline using Student's t test for independent samples and the chi-square test for difference in proportions, for continuous and categorical outcomes, respectively. The total mortality rate of those randomized to a weight loss intervention was compared with those not randomized to a weight loss intervention, using Cox proportional hazard regression. The intent-to-treat unadjusted analysis included 318 randomized participants and is presented as hazard rate ratio (HR) and 95% confidence interval (CI). However, two participants who were randomized withdrew prior to participation in ADAPT, and covariate data were not retained by the parent study, so our stratified analyses included 316 participants (Figure 1). To examine whether the effect of weight loss on mortality differed by sex, age, initial body weight, we repeated all analyses stratified by sex, age (less than or equal to or greater than the median age of 67.1 years at baseline), and BMI (less than or equal to or greater than the median BMI of 33.5 kg/m2 at baseline). In addition to the two in-trial deaths, there were four deaths ascertained within the first 2 years of follow-up, so we were unable to examine whether the effect of weight loss on total mortality differed by duration of follow-up. However, we did examine for differences in mortality among participants for more than 2 years of follow-up only. Because the amount of weight lost may influence mortality risk among participants in the weight loss groups, we compared (a) the mortality rates of those who lost greater than the median of initial body weight (3.6 kg) with those who lost less than or equal to the median of initial body weight and (b) the mortality rates of those who lost greater than or equal to 5% of initial body weight (the goal of the weight loss intervention) with those who lost less than 5% of initial body weight. We also compared the total mortality rates of the four separate intervention groups and determined the effect of randomization with the exercise intervention on total mortality using Cox proportional hazard regression. Person-time was calculated from date of randomization to the date of death or censoring (December 31, 2006). All analyses were carried out using SAS 9.1 (SAS Institute Inc., Cary, NC), and results were considered statistically significant if p < .05.
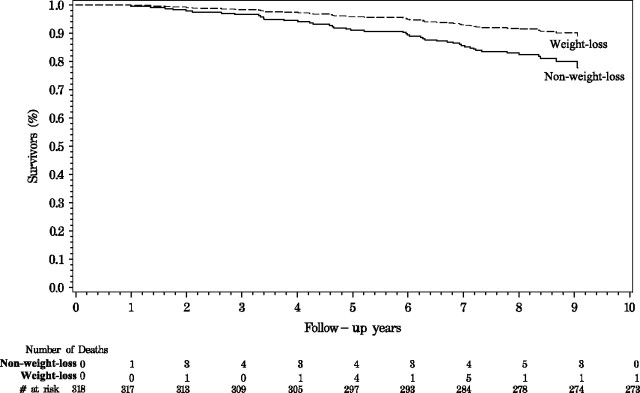
RESULTS
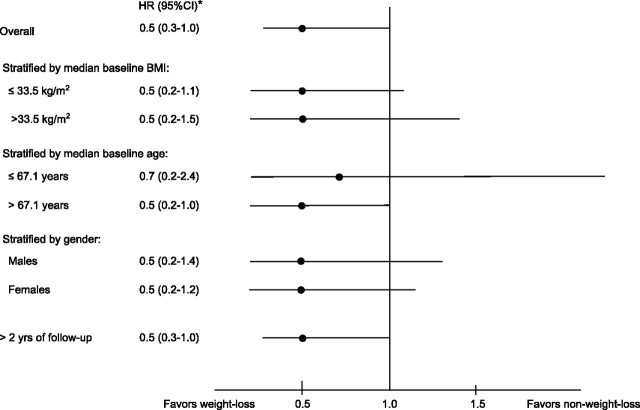
The baseline characteristics of the weight loss groups and non–weight loss groups are presented in Table 1. Overall, the mean age was 68.5 years, and more than 75% of participants were considered obese at baseline. Compared with the non–weight loss group, the weight loss intervention group lost significantly more weight at 6 months (4.4 ± 5.3 kg vs 0.3 ± 3.0 kg, p < .01) and at 18 months (4.8 ± 7.5 kg vs 1.4 ± 5.1 kg, p < .01) of follow-up. The mean follow-up time was longer in the weight loss group than in the non–weight loss group (8.2 ± 1.1 years vs 7.8 ± 1.7 years, respectively, p = .01). Overall, there were 15 deaths in the weight loss intervention groups and 30 deaths in the non–weight loss intervention groups, including two in-trial deaths. In the unadjusted intent-to-treat analysis (n = 318), those randomized to the weight loss intervention had a lower mortality rate compared with those who were randomized to a non–weight loss intervention (HR [95% CI] = 0.5 [0.3–0.9], p = .01; Figure 2). After adjustment for age, sex, and exercise treatment, the HR for mortality associated with intentional weight loss did not differ from the unadjusted intent-to-treat analysis (HR [95% CI] = 0.5 [0.3–1.0], p = .03; Table 2). There were no differences in total mortality between those randomized to the weight loss intervention and those randomized to a non–weight loss intervention among those less than the median age at baseline, among those with a baseline BMI less than or equal to the median (33.5 kg/m2), among those with a BMI greater than the median at baseline, or among men or women, as shown in Figure 3. Among older participants (defined as greater than the median age of 67.1 years at baseline), those randomized to a weight loss intervention had a lower mortality rate compared with those randomized to a non–weight loss intervention (HR [95% CI] = 0.4 [0.2–1.0], p = .04; Figure 3). Among participants randomized to a weight loss intervention group, the total mortality rate of participants who lost greater than the median of initial body weight (3.6 kg) was not different from those who lost less than or equal to median of initial body weight (HR [95% CI] = 1.2 [0.3–4.6], p = .75) and the total mortality rate of those who loss at least 5% of initial body weight (which was the goal of the weight loss intervention) was not different from those who lost less than 5% of initial body weight (HR [95% CI] = 1.5 [0.4–5.5], p = .58). Overall, there was no effect of randomization to the exercise intervention on total mortality, and the total mortality rates of the dietary weight loss, dietary weight loss + exercise, and the exercise-only intervention groups did not significantly differ from the control group (Table 2).
Table 1.
Participant Characteristics at Baseline According to Weight Loss Intervention*
| Randomized to Weight Loss Intervention (n = 159) | Not Randomized to Weight Loss Intervention (n = 159) | p Value | |
| % Female | 72.3 | 71.2 | .83 |
| % White | 74.7 | 76.8 | .67 |
| Age, M ± SD, y | 68.2 ± 6.1 | 69.0 ± 6.3 | .31 |
| BMI, M ± SD, kg/m2 | 34.3 ± 5.3 | 34.2 ± 4.9 | .87 |
| Weight, M ± SD, kg | 93.6± 16.2 | 93.9± 16.9 | .85 |
| Comorbid illness (%) | |||
| Obesity (BMI ≥ 30) | 76.0 | 80.7 | .32 |
| Coronary heart disease | 40.9 | 48.4 | .19 |
| Diabetes | 9.5 | 10.5 | .79 |
Notes: BMI = body mass index.
Two participants missing all measures except gender, age, and date of death.
Figure 2.
Unadjusted estimates of survival time among participants in Arthritis, Diet, and Activity Promotion Trial randomized to weight loss or non–weight loss intervention in intention-to-treat analyses.
Table 2.
Total Mortality Rate of Arthritis, Diet, and Activity Promotion Trial Participants According to Randomized Group
| n | Person-Years | Deaths (n = 45) | Death Rate (per 100 person-years) | Rate Ratio (95% CI) | p | Adjusted RR (95% CI)* | p | |
| Stratum results | ||||||||
| Control | 78 | 611.9 | 13 | 2.12 | Reference | Reference | ||
| Weight loss only | 82 | 680.0 | 7 | 1.03 | 0.5 (0.2–1.2) | .12 | 0.5 (0.2–1.4) | .19 |
| Weight loss + exercise | 77 | 626.2 | 8 | 1.28 | 0.6 (0.3–1.4) | .22 | 0.6 (0.3–1.5) | .31 |
| Exercise only | 81 | 626.1 | 17 | 2.72 | 1.3 (0.7–2.4) | .43 | 1.3 (0.6–2.8) | .48 |
| Main effects results | ||||||||
| Exercise | ||||||||
| Not randomized to exercise intervention | 160 | 1291.9 | 20 | 1.55 | Reference | Reference | ||
| Randomized to exercise intervention | 158 | 1252.3 | 25 | 2.00 | 1.3 (0.7–2.2) | .83 | 1.3 (0.7–2.4)† | .38 |
| Dietary weight loss | ||||||||
| Not randomized to weight loss intervention | 159 | 1238.0 | 30 | 2.42 | Reference | Reference | ||
| Randomized to weight loss intervention | 159 | 1306.2 | 15 | 1.15 | 0.5 (0.3–0.9) | .01 | 0.5 (0.3–1.0)‡ | .03 |
Notes: *Adjusted for age and sex.
Further adjusted for dietary weight loss treatment.
Further adjusted for exercise treatment.
RR = relative risk.
Figure 3.
Adjusted rates of total mortality among participants in Arthritis, Diet, and Activity Promotion Trial randomized to weight loss or non–weight loss interventions. Asterisk indicates adjusted for age, gender, and exercise treatment, unless stratified on that variable.
DISCUSSION
Over an average of 8.0 years of follow-up, the mortality rate of older overweight and obese men and women who intentionally lost weight during an 18-month randomized controlled weight loss was not greater than that of those who did not intentionally lose weight. When the dietary weight loss and dietary weight loss + exercise groups were combined, the total mortality rate of those randomized to a weight loss intervention was lower than the mortality rate of those not randomized to a non–weight loss intervention (the exercise and control groups combined). To the best of our knowledge, this analysis is the first to report on the effect of intentional weight loss on total mortality, utilizing a randomized controlled study design. The results of the stratified analyses suggest that voluntary weight loss may lower mortality among older adults (greater than the median age of 67.1 years) and over longer follow-up (>2 years) in particular. The mortality rates of the individual intervention groups did not significantly differ from that of the control group, and there was no significant difference in mortality between those randomized to a weight loss intervention and those not, even among the other subgroups analyzed, supporting that intentional weight loss among older men and women does not increase risk for overall mortality.
To date, the association between weight loss and mortality has been investigated in longitudinal observational studies, with inconsistent results. In a recently published meta-analysis of longitudinal weight loss studies, among the studies of healthy adults that did not discern whether or not weight loss was intentional, weight loss was associated with a 38% increase in total mortality risk (relative risk [RR] [95% CI] = 1.38 [1.27–1.49]) (16). However, the failure to differentiate intentional from unintentional weight loss has led some to question the value of these studies (17). Subsequent studies have attempted to stratify according to weight loss intent, with likewise equivocal results (7–11,18–20). In the same recently published meta-analysis, weight loss that was reported to be intentional was associated with a slight increase in risk for total mortality (RR [95% CI] = 1.11 [1.00–1.22]) (16) among overweight but otherwise healthy men and women, although the risk ratios of the individual studies ranged from 0.59 to 1.87 (7–11,16,18–20), suggesting that the matter of intent, which is difficult to ascertain, is critically important with respect to weight loss. This importance is substantiated by an analysis of type 2 diabetic patients in whom unintentional weight loss was associated with a 58% increase in mortality rate, whereas those who reported trying to lose weight had a 17% lower mortality rate (21). Even still, our data are inconsistent with the best estimate of the association between weight loss and mortality derived from observational studies, as our 95% CI well excludes the 1.11 estimate of RR from the recent meta-analysis (16).
Overweight and obese older adults are at greater risk for several age-related comorbid diseases and disability. Our finding that overweight and obese older adults who intentionally lost weight had a lower total mortality rate compared with those who did not lose weight is consistent with the outcomes of randomized weight loss trials that have demonstrated a beneficial effect of weight loss on improving weight-related comorbidities, such as OA, hypertension, type 2 diabetes, and risk for cardiovascular disease (1–4), which have themselves been associated with lowering mortality risk (22,23). Given that weight loss can exacerbate lean tissue and bone loss, and potentially compromise the strength and physical function of older adults, it has been recommended that weight loss therapy for older adults should maximize fat loss and minimize muscle and skeletal tissue loss by incorporating adequate intakes of protein, calcium and vitamin D, and regular physical activity into a lifestyle modification (24).
The fundamental strength of this study is that it is the first report of the effect of intentional weight loss on total mortality following a randomized controlled study design, a methodological advantage that resolves the matter of intent. Yet, there are certain limitations to acknowledge. As reported by the ADAPT parent study, weight loss was associated with better physical function in overweight patients with knee OA, after 18 months (1), and it is plausible that these improvements may have influenced total mortality among study participants. Because we examined the effect of intentional weight loss on total mortality, and did not differentiate among cause-specific mortality, we cannot speculate as to whether intentional weight loss differentially influenced cardiovascular disease mortality or other cause-specific mortality. The participants of the ADAPT study were selected according to the diagnosis of knee OA, and of the screened participants, 14% were randomized, so our results may not be generalizable to older adults with other weight-related comorbidities or to less healthy people with knee OA. In addition, information on postintervention health or lifestyle factors was not available, so we were unable to control for these factors in our analyses.
We acknowledge that magnitude of the lower HR associated with intentional weight loss (0.5 [95% CI = 0.3–1.0]) in our adjusted analysis was unexpected, and certainly, type I error is a possible explanation. However, if our estimate that a mean intentional weight loss of 4.4 ± 7.0 kg (corresponding to approximately 5% of initial body weight) is associated with a 50% lower rate of mortality is confirmed, not only would this be clinically important with respect to recommending therapeutic weight loss to older patients, it would be relevant for the design and implementation of future weight loss intervention trials in older adults. Among participants who were randomized to a weight loss intervention, we found no association between magnitude of intentional weight loss and total mortality. Although these results are in agreement with larger studies that reported modest weight loss was not associated with total mortality (11,19), there were only 15 deaths in the weight loss group, which is not likely to be a sufficient number to detect an association. Therefore, results should be interpreted cautiously until confirmed by larger randomized weight loss trials. Overall, these results support the finding that intentional weight loss does not increase mortality risk and provides new evidence for clinicians to consider, given that weight loss can improve risk for several chronic diseases and physical disability (2,4,25). Nevertheless, we acknowledge that replication of these findings is necessary before clinical recommendations should be made.
In summary, this analysis of a randomized controlled weight loss intervention study demonstrates that modest intentional weight loss in overweight older adults does not increase risk for all-cause mortality. In fact, it may reduce mortality risk over the long-term. Furthermore, our results suggest that the ability to determine intentionality of weight loss in observational studies may not be fully adequate to test the hypothesis about weight loss and mortality (12,13). Thus, recommendations based on observational studies should be made with caution.
FUNDING
This work was supported by the Wake Forest University Claude D. Pepper Older Americans Independence Center (P30-AG21332).
References
- 1.Messier SP, Loeser RF, Miller GD, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet, and Activity Promotion Trial. Arthritis Rheum. 2004;50(5):1501–1510. doi: 10.1002/art.20256. [DOI] [PubMed] [Google Scholar]
- 2.Pi-Sunyer X, Blackburn G, Brancati FL, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care. 2007;30(6):1374–1383. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Villareal DT, Miller BV, III, Banks M, Fontana L, Sinacore DR, Klein S. Effect of lifestyle intervention on metabolic coronary heart disease risk factors in obese older adults. Am J Clin Nutr. 2006;84(6):1317–1323. doi: 10.1093/ajcn/84.6.1317. [DOI] [PubMed] [Google Scholar]
- 4.Whelton PK, Appel LJ, Espeland MA, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA. 1998;279(11):839–846. doi: 10.1001/jama.279.11.839. [DOI] [PubMed] [Google Scholar]
- 5.Sorensen TI. Weight loss causes increased mortality: pros. Obes Rev. 2003;4(1):3–7. doi: 10.1046/j.1467-789x.2003.00090.x. [DOI] [PubMed] [Google Scholar]
- 6.Knudtson MD, Klein BE, Klein R, Shankar A. Associations with weight loss and subsequent mortality risk. Ann Epidemiol. 2005;15(7):483–491. doi: 10.1016/j.annepidem.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 7.Sorensen TI, Rissanen A, Korkeila M, Kaprio J. Intention to lose weight, weight changes, and 18-y mortality in overweight individuals without co-morbidities. PLoS Med. 2005;2(6):e171. doi: 10.1371/journal.pmed.0020171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yaari S, Goldbourt U. Voluntary and involuntary weight loss: associations with long term mortality in 9,228 middle-aged and elderly men. Am J Epidemiol. 1998;148(6):546–555. doi: 10.1093/oxfordjournals.aje.a009680. [DOI] [PubMed] [Google Scholar]
- 9.French SA, Folsom AR, Jeffery RW, Williamson DF. Prospective study of intentionality of weight loss and mortality in older women: the Iowa Women's Health Study. Am J Epidemiol. 1999;149(6):504–514. doi: 10.1093/oxfordjournals.aje.a009844. [DOI] [PubMed] [Google Scholar]
- 10.Gregg EW, Gerzoff RB, Thompson TJ, Williamson DF. Intentional weight loss and death in overweight and obese U.S. adults 35 years of age and older. Ann Intern Med. 2003;138(5):383–389. doi: 10.7326/0003-4819-138-5-200303040-00007. [DOI] [PubMed] [Google Scholar]
- 11.Williamson DF, Pamuk E, Thun M, Flanders D, Byers T, Heath C. Prospective study of intentional weight loss and mortality in never-smoking overweight US white women aged 40-64 years. Am J Epidemiol. 1995;141(12):1128–1141. doi: 10.1093/oxfordjournals.aje.a117386. [DOI] [PubMed] [Google Scholar]
- 12.Kuller LH. Invited commentary on “Prospective study of intentionality of weight loss and mortality in older women: the Iowa Women's Health Study” and “Prospective study of intentional weight loss and mortality in overweight white men aged 40-64 years.”. Am J Epidemiol. 1999;149(6):515–516. doi: 10.1093/oxfordjournals.aje.a009845. [DOI] [PubMed] [Google Scholar]
- 13.Yang D, Fontaine KR, Wang C, Allison DB. Weight loss causes increased mortality: cons. Obes Rev. 2003;4(1):9–16. doi: 10.1046/j.1467-789x.2003.00092.x. [DOI] [PubMed] [Google Scholar]
- 14.Lash TL, Silliman RA. A comparison of the National Death Index and Social Security Administration databases to ascertain vital status. Epidemiology. 2001;12(2):259–261. doi: 10.1097/00001648-200103000-00021. [DOI] [PubMed] [Google Scholar]
- 15.Fillenbaum GG, Burchett BM, Blazer DG. Identifying a national death index match. Am J Epidemiol. 2009;170(4):515–518. doi: 10.1093/aje/kwp155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harrington M, Gibson S, Cottrell RC. A review and meta-analysis of the effect of weight loss on all-cause mortality risk. Nutr Res Rev. 2009;22(1):93–108. doi: 10.1017/S0954422409990035. [DOI] [PubMed] [Google Scholar]
- 17.Fontaine KR, Allison DB. Does intentional weight loss affect mortality rate? Eat Behav. 2001;2(2):87–95. doi: 10.1016/s1471-0153(01)00024-1. [DOI] [PubMed] [Google Scholar]
- 18.Wannamethee SG, Shaper AG, Walker M. Weight change, weight fluctuation, and mortality. Arch Intern Med. 2002;162(22):2575–2580. doi: 10.1001/archinte.162.22.2575. [DOI] [PubMed] [Google Scholar]
- 19.Williamson DF, Pamuk E, Thun M, Flanders D, Byers T, Heath C. Prospective study of intentional weight loss and mortality in overweight white men aged 40-64 years. Am J Epidemiol. 1999;149(6):491–503. doi: 10.1093/oxfordjournals.aje.a009843. [DOI] [PubMed] [Google Scholar]
- 20.Wedick NM, Barrett-Connor E, Knoke JD, Wingard DL. The relationship between weight loss and all-cause mortality in older men and women with and without diabetes mellitus: the Rancho Bernardo study. J Am Geriatr Soc. 2002;50(11):1810–1815. doi: 10.1046/j.1532-5415.2002.50509.x. [DOI] [PubMed] [Google Scholar]
- 21.Gregg EW, Gerzoff RB, Thompson TJ, Williamson DF. Trying to lose weight, losing weight, and 9-year mortality in overweight U.S. adults with diabetes. Diabetes Care. 2004;27(3):657–662. doi: 10.2337/diacare.27.3.657. [DOI] [PubMed] [Google Scholar]
- 22.Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887–1898. doi: 10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]
- 23.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–1589. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 24.Villareal DT, Apovian CM, Kushner RF, Klein S. Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Obes Res. 2005;13(11):1849–1863. doi: 10.1038/oby.2005.228. [DOI] [PubMed] [Google Scholar]
- 25.Villareal DT, Banks M, Sinacore DR, Siener C, Klein S. Effect of weight loss and exercise on frailty in obese older adults. Arch Intern Med. 2006;166(8):860–866. doi: 10.1001/archinte.166.8.860. [DOI] [PubMed] [Google Scholar]