Abstract
Introduction
A mandatory multidisciplinary plan for individual care, the ‘Individual care Plan’, was introduced by law in Norway in 2001. The regulation was established to meet the need for improved efficiency and quality of health and social services, and to increase patient involvement. The plan was intended for patients with long-term and complex needs for coordinated care. The aim of this study was to elaborate on knowledge of such planning processes in Norwegian municipalities.
Method
A piloted questionnaire was sent to 92 randomly selected municipalities in 2005–2006, addressing local organization and participation in the work with individual care plans. Local political governance, size of the population, funds available for health care, and problems related to living conditions were indicators for analysing the extent to which the individual care plan was used five years after the regulation was introduced.
Results
Our results showed that 0.5% as opposed to an expected 3% of the population had an individual care plan. This was independent of the political, social and financial situation in the municipalities or the way the planning process had been carried out. The planning process was mostly taken care of by local health and social care professionals, rather than by hospital staff and general practitioners.
Discussion and conclusion
The low number of care plans and the oblique responsibility among professionals for planning showed that the objectives of the national initiative had not been achieved. More research is needed to determine the reasons for this lack of success and to contribute to solutions for improved multidisciplinary cooperation.
Keywords: health policy, health planning, patient care management, primary health care, patient centred care, individual care plan
Introduction
According to both scientific and government publications, a growing number of people need better coordination of care across health and social services that involve a number of carers [1–5]. International research shows that coordinating models have been initiated and established mainly at local levels and as projects more often than as permanent services [6]. The Norwegian government decided to try another approach. The ‘Individual care Plan’ was introduced by law in 2001 at national level, giving patients the right to receive managed and coordinated care and to be involved in the process of shaping their own services [7].
Since the law was passed, all kinds of patients in need of wide-ranging health and social services over time have had a legal right to an individual care plan including a named person to coordinate the services. It has been estimated that about 30 per 10,000 people or 3% of the population might benefit from such a plan. The numbers are based on statistics for illness and disability in Norway [3]. An individual care plan includes an outline of the patient’s objectives and resources as well as the services required, independent of diagnosis or age or level of care. Typical patients covered by the legislation include people with a severe psychiatric diagnosis, disability, or drug addiction, as well as elderly patients with comorbid conditions who need coordinated care across organizational boundaries. The planning process is to be started as soon as requested by any party, including the patient, next of kin or legal guardian. The health or social provider is expected to offer an individual plan as a natural part of treatment. This plan is not a substitute for the patient record and does not contain detailed social or health personal data. The areas mapped are mainly needs and resources in health, finances, housing, and social life as well as kindergarten, education or work. The main function is administrative: to define goals and tasks for selected areas, specify the responsible providers and indicate a schedule or timetable. The collaborative process is essential and even professionals outside health and social care, mainly teachers, can initiate and participate in the care planning process. Teachers typically contact the health visitor or social welfare officer to start the collaborative planning process. They can mutually benefit in their work in relation to, for instance, a disabled child by cooperating across organizational boundaries.
The Norwegian Directorate of Health has prepared guidelines, held courses, and initiated projects to inform professionals and managers about individual care plans and to ensure that both hospitals and municipalities achieve proper planning processes. Although great efforts have been made to stimulate the use of individual care plans, a national survey has indicated that interest in using individual care plans has been low or modest [8].
The purpose of this study was to explore the use of individual care plans in Norwegian municipalities that are responsible for primary care and social services:
How extensive is the use of individual care plans?
Is deployment of the plans influenced by the municipality’s size, local political dominance, or financial situation, or by indicators of living conditions in the municipality?
How do municipalities initiate and organize the process of implementing individual care plans?
Norwegian municipalities are run by local councils. Most of their health and social care duties are regulated by law and are financed by general grants or national earmarked grants. However, there are variations due to local political government, prioritizing of available resources, and differing needs [9–10]. There are also variations in living conditions [11].
Methods
Selection of participants
A sample of all 420 municipalities was selected in two steps following the approach suggested by Groves et al. [12]. First, the municipalities were proportionally stratified into three groups according to size following the classification provided by Statistics Norway (SSB): small (<5000 inhabitants), medium-sized (5000–19,999 inhabitants) and large (≥20,000 inhabitants) [13]. From each group, 20% was randomly chosen by throwing a dice, i.e., 46 small, 30 medium-sized and 16 large municipalities. The largest municipalities were represented by drawing one or two internal districts according to their size.
Questionnaire
We did not identify any validated questionnaire suitable for our purpose and had to develop one from scratch. National and international literature and theory describing coordinated and multidisciplinary care as well as our own experience with individual care plans were used as the background [5, 14–16]. The first section in the questionnaire covered information about characteristics of the municipalities, such as size and deployment of individual care plans. The second section comprised questions about who initiated an individual care plan, who managed the plan, and who participated throughout the planning process, including patients and next of kin. We used a combination of yes/no questions and 5-point Likert scales where 1=‘always’ and 5=‘never’. The questionnaire was piloted by asking 11 nurses, social workers and patients who were familiar with the concept of individual care plans to go through it [17]. They were then interviewed about their opinion of both the questions and the layout of the questionnaire. A few minor changes were made as a result.
Data collection and analyses
The questionnaires were distributed by post in November 2005. Two reminders were sent, and the last response was received in July 2006. As there are minor organizational variations nationwide, we decided to simply ask the municipality administration to identify the person who had the best local overview of, or knowledge about use of individual care plans and hand over the questionnaire to this person.
The municipality reference number was used to link the questionnaire with additional demographic information about each municipality from the public information source in [9–12]. An index was used for living condition problems, based on the sub-indices social assistance, mortality, disabled pensioners, rehabilitation assistance, violence, unemployment, transitional benefits and proportion with schooling limited to compulsory education [10]. Data were analysed using SPSS version 16.0. Frequencies were used to describe the distribution and organizational aspects of the care plan processes. One-way analysis of variance (ANOVA) tests were carried out to analyse structural correlations between characteristics of the municipalities and distribution of individual care plans. One-way ANOVA tests were also conducted to analyse coherence between distribution of individual plans and organizational factors.
Ethical considerations
The survey was approved by both the Norwegian Social Science Data Services (NSD) and the Regional Committee of Medical Research Ethics (REK).
Results
In total, 61 (66%) municipalities responded out of the 92 municipalities to which the questionnaire was sent (small municipalities 31/46 (66%), medium-sized 21/30 (70%) and large municipalities 9/16 (56%). Thirty-two (53%) leaders in health or social care and 27 professionals (44%) answered the questionnaires. Altogether 50 (82%) municipalities stated the number of patients with an individual care plan in their municipality, including 23 (38%) which gave an approximate number of plans. Thirty (49%) municipalities knew the exact number of plans. Municipalities that gave the exact or approximate numbers of plans are treated alike in analysing prevalence of plans. All municipalities were included in analysing organizational matters.
Individual care plans in relation to municipality characteristics
In the municipalities that had stated their number of individual plans, the average number of people with individual care plans was 50/10,000 inhabitants (range 40–150 of 10,000) consequently, of the eligible patient group expected by health authorities, just under 1700/10,000 (17%) had a plan.
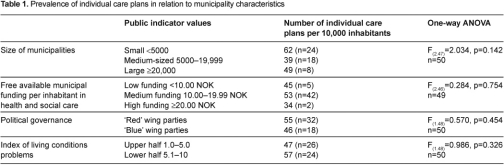
Table 1 shows that the size of the municipality had no significant influence on its relative number of plans. Neither did we find any significant relation between the number of individual care plans and municipal health and social care funding, political governance or the municipal index for living condition problems.
Management of individual care plans in the municipalities
The planning process was divided into three phases: initiation of plan, appointment of individual care plan manager, and the collaborative planning process.
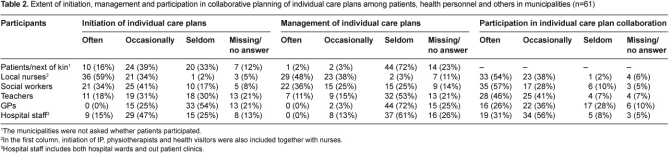
Table 2 shows that nurses initiated and managed individual care plans most often, compared with others. Social workers, nurses, and teachers participated most frequently in the collaboration. Patients or next of kin did not often initiate plans themselves. Hospital staff and general practitioners (GPs) participated overall to a low extent. We found a relationship between levels of initiation and management in the groups of nurses, social workers and general practitioners. Analysing municipal distribution of plans with variables in Table 2 showed no significant correlation.
Collaboration and documentation methods
We asked for collaborative and documentation routines in order to map organizational aspects relating to the development of individual care plans.
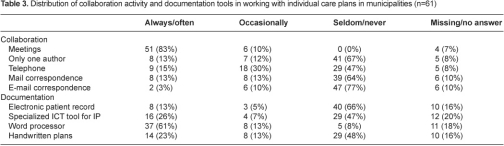
Table 3 shows that drawing up an individual care plan is usually a collaborative process. Meetings were the most common form of collaboration, followed by telephone conversations. Our survey showed that nearly all the professionals participating in planning processes had access to ICT tools, but specific templates or applications for plans were seldom used in the documentation. A word processor seemed to be the preferred tool. Even handwriting was still fairly extensively used. Analysing coherence between prevalence of individual plans in the municipalities and planning activity methods yielded no significant results.
Discussion
This survey shows that the deployment of individual care plans is still far from covering the expected needs, five years after they became a legal right and after other initiatives launched by health authorities. Municipality authorities are responsible for the implementation of individual care plans, but local demographics or organization of planning processes do not seem to influence the deployment.
Study limitations
Professionals in different positions answered the questionnaire, because local authorities were able to choose the respondent on behalf of the municipality. Many municipalities did not have a complete overview of the local work done in relation to individual care plans and could not answer some of the questions. This may have introduced a bias of which we are unaware.
A larger sample might have improved the statistical reliability in general. The sample size covering a fifth of the population was considered sufficient for analysis due to the stratification and overall homogenous, nationally regulated structures in Norwegian municipalities. We did not find any demographic or geographic differences between respondent and non-respondent municipalities. We do not believe that the non-respondents would have caused results favourable to the deployment or use of individual care plans [18]. In all, we do not expect that an increase in the population size would have influenced our conclusion.
Another weakness is that all the information we have obtained about patients’ experience and involvement in the use of individual care plans comes from answers given by the service providers.
Deployment of individual care plans
Individual care plans have been regarded as an aspect of integrated care internationally [19]. We believe that Norway’s systematic national approach to care planning is unique in being mandatory for all service providers on an equal basis. It assumes and requires multilevel and multidisciplinary collaboration that is broader and includes more services than has been customary in many instances [6, 20]. According to political statements in Norway, the use of individual care plans is an important indicator of quality of care and user satisfaction [21].
However, our study provides no explanation for the low number of plans and the lack of overview of their number of plans. This may indicate modest interest or local barriers to individual care plans as a model of care. Small municipalities have generally invested more in health care services than large ones, and municipalities with a high degree of funding at their disposal for health and social care have spent more money on elder care than other municipalities [22, 23]. We did not find that this pattern applied to individual care plans. Political views and financial allocations are important at national level, but—as demonstrated here and by others—the differences between political wings fade away locally [24].
Municipal organization of the work with individual care plans
National health authorities manage specialist care in Norway, but the municipalities have considerable autonomy in their organization and implementation of social and primary care. To achieve well-organized individual care plans of high quality, the need for suitable structures for collaboration and understanding of roles as well as for patient empowerment is emphasized [25–27]. Few patients had claimed an individual care plan on their own initiative in spite of intensive information campaigns and their statutory right to such a plan. One reason might be uncertainty among patients about the benefits [28]. Another reason may be that information was not perceived as expected [29]. Patients who have an adequate individual care plan, however, report that it has contributed to better quality of life [30].
The association between initiation and management of individual care plans we found may indicate that initiating professionals end up managing the plan. Such mechanisms can easily lead to a skewed workload among staff, and might thus have become a barrier to further deployment of plans. Our survey revealed that in the complex coordination of the plans, some professions (e.g., nurses and teachers) were more committed to the planning process than others. This did not follow the traditional hierarchy of patient treatment presented in literature on professions, but showed other layers of responsibility as this management work may have a lower status than other clinical decisions and treatment [31–33].
The low participation of general practitioners in work with individual care plans does not harmonize with the situation of chronically ill patients who depend on and expect involvement from their general practitioners in rehabilitation [34]. Reasons suggested include work patterns socialized in medical education as well as workload [35, 36]. Instead, general practitioners leave multidisciplinary collaborative work to other personnel in the municipality. Hospitals expect municipalities to work out individual care plans, although hospitals have the same independent obligations [37].
The analysis did not explain why teachers initiated plans and participated in the way they did, as they are not formally included in the scope of the law on individual care plans. There is a close working relationship between schools, health visitors and the social care system in Norwegian municipalities, as well as between general practitioners and hospitals, so there must be other reasons. One could be that all disabled children in Norway are integrated into ordinary schools, and rehabilitation of children was one of the areas given priority in connection with the concept of the individual care plan.
Our study supports the view that the organization of the work with individual care plan has been more or less arbitrary. A previous study showed that municipalities and hospitals had not established organizational structures to support individual care plans. This study also shows that there was no connection between measures proposed in individual care plans and health services being provided [37].
Our results may indicate a lack of suitable ICT tools to support the work with individual care plans, as we know from a recent study that 60% of the nursing care services in the municipalities had access to electronic patient record systems including templates for individual care plans [38]. Our study shows that these templates in the EPR were not widely used.
We believe that health and social care services in other countries may learn from Norwegian experience indicating that the implementation success of integrated care processes cannot easily be explored. Legislation, supervision and training programmes have not increased deployment of individual care planning or collaboration processes to an acceptable level. The somewhat skewed distribution of participants being involved across legislation demands should be taken into consideration in plans for similar solutions for integrated care. Although the law assigns equal responsibility for the planning process, our analyses revealed a different reality. The involvement of teachers shows that planning process strategies may benefit from being open even to participants outside health and social care.
Conclusion
Our study supports earlier research indicating that establishing sustainable integrated collaborative care is complicated. Despite legal obligations and national initiatives by the authorities, multidisciplinary teamwork across organizational boundaries in health and social care is challenging. There may be reasons below supervisory economic and political levels that should be explored.
Authors’ contribution
Jorunn Bjerkan has been in charge of the data collection and writing process as part of her PhD project. Marie Richter participated in developing and carrying out the questionnaire process, as well as in capturing and analysing the statistical material. Ragnhild Hellesø, Anders Grimsmo and Jytte Brender provided ongoing critical appraisal and contribution of the approach, writing process and interpretation of the results. All authors have accepted the final version of the article.
Acknowledgments
Thanks to Morten Wold Henriksen for participating in the development of the questionnaire, Kyrre Svarva for consultancy services in relation to statistical analyses, Anne Hollingen for adding valuable information from field research, and Margaret Forbes for improving the language.
Contributor Information
Jorunn Bjerkan, Norwegian Centre of Electronic Health Records (NSEP), Faculty of Medicine, Norwegian University of Science and Technology, Medisinsk teknisk forskningssenter [Research Centre of Medical Technology], NO-7489 Trondheim, Norway.
Marie Richter, Faculty of Medicine, Norwegian University of Science and Technology, Medisinsk teknisk forskningssenter [Research Centre of Medical Technology], NO-7489 Trondheim, Norway.
Anders Grimsmo, Faculty of Medicine, Norwegian University of Science and Technology, Medisinsk teknisk forskningssenter [Research Centre of Medical Technology], NO-7489 Trondheim, Norway.
Ragnhild Hellesø, Faculty of Medicine, Institute of Health and Society, Department of Nursing and Health Sciences, University of Oslo, P.O. Box 1153 Blindern, NO-0318 Oslo, Norway.
Jytte Brender, Aalborg University, Department of Health Science and Technology, and Virtual Center of Health Informatics, Fredrik BajersVej 7D, DK-9220 Aalborg East, Denmark.
Reviewers
Elizabeth Borycki, RN, PhD, Assistant Professor, School of Health Information Science, University of Victoria, Victoria, British Columbia, Canada
Anna-Karin Edberg, PhD, Professor, Swedish Institute for Health Sciences and Kristianstad University, Sweden
Laurann Yen, Associate Director, Menzies Centre for Health Policy, ANU, Australia
References
- 1.Murray CJL, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: global burden of disease study. The Lancet. 1997;349(9064):1498–504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 2.Battersby MW The S.A. HealthPlus Team. Health reform through coordinated care: S.A. HealthPlus. British Medical Journal. 2005;330(7492):662–5. doi: 10.1136/bmj.330.7492.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bernt JF, Braut GS, Dale JH, Gullestad B, Halvorsen M, Kjellevold A, et al. Helhet og plan i sosial- og helsetjenestene. Samordning og samhandling i kommunale sosial- og helsetjenester. [Completeness and planning in social and health care. Cooperation and collaboration in municipal health and social services]. Statens forvaltningstjeneste, informasjonsforvaltning; 2004. [cited 2009 Dec 05]. Available from: http://www.regjeringen.no/Rpub/NOU/20042004/018/PDFS/NOU200420040018000DDDPDFS.pdf. [in Norwegian] [Google Scholar]
- 4.Ehrlich C, Kendall E, Muenchberger H, Armstrong K. Coordinated care: what does that really mean? Health and Social Care in the Community. 2009;17(6):619–27. doi: 10.1111/j.1365-2524.2009.00863.x. [DOI] [PubMed] [Google Scholar]
- 5.Normann T, Sandvin JT, Thommesen H, Stultz C, Giskeødegård IK. A holistic approach to rehabilitation. Oslo: Kommuneforlaget; 2004. [Google Scholar]
- 6.Leichsenring K. Developing integrated health and social care services for older persons in Europe. International Journal of Integrated Care [Serial online] 2004 Sep 3;4 doi: 10.5334/ijic.107. [cited 2010 Apr 21]. Available from: http://www.ijic.org. URN:NBN:NL:UI:10-1-100349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Helse- og omsorgsdepartementet. Stortingsmelding 25. Åpenhet og helhet—Om psykiske lidelser og tjenestetilbudene. [Report no. 25 to the Storting (1996–97) openness and wholeness: mental illness and mental health services]. Oslo: Helse- og omsorgsdepartementet; 1996–97. [in Norwegian] [Google Scholar]
- 8.Helsetilsynet. Oppsummering av landsomfattende tilsyn i 2007 med kommunale helse- og sosialtjenester til voksne med psykiske lidelser. [National summary of governmental inspections within local health and social services for adults with mental disorders]. Oslo: Helsetilsynet; 2008. [in Norwegian] [Google Scholar]
- 9.Norsk samfunnsvitenskapelig datatjeneste. NSDs kommunedatabase, Valg, kommunestyrevalg. [Data on the political system—PolSys, local government election]. [webpage on the internet]. 2003 [cited 2009 Dec 15]. Available from http://www.nsd.uib.no/. [in Norwegian] [Google Scholar]
- 10.Statistics Norway. Helse- og sosialsektorens brutto- og netto driftsutgifter. Tabell 10, 2005. [Gross and net operating expenses of the health and social sector. Table 10, 2005]. SSB Hjulet: Municipal health and social data; [webpage on the internet]. 2006 [cited 2010 Jan 07]. Available from: http://www.ssb.no/emner/03/hjulet/hjulet2006/tabell-10.html. [in Norwegian] [Google Scholar]
- 11.SSB, Statistics Norway. Challenges in municipal health and social services. Official statistics of Norway Oslo. [webpage on the internet]. 2005 [cited 2010 Jan 10]. Available from: http://www.ssb.no/english/subjects/03/hjulet_en/ [Google Scholar]
- 12.Groves RM, Fowler F, Couper MP, Lepkowski JM. Survey methodology. Hoboken, NJ: Wiley and sons; 2009. [Google Scholar]
- 13.SSB, Statistics Norway. Regionale inndelinger. En oversikt over standarder i norsk offisiell statsitikk. [Regional divisions. A summary of standards in Norwegian public statistics. Official statistics of Norway]. [webpage on the internet]. 1999 [cited 2009 05.12]. Available from: http://www.ssb.no/emner/00/00/20/nos_c513/nos_c513.pdf. [in Norwegian] [Google Scholar]
- 14.Gröne O, Garcia-Barbero M. Integrated Care. A position paper of the WHO European office for integrated health care services. International Journal of Integrated Care [Serial online] 2001 Jun 1;1 [cited 2010 Apr 21]. Available from: http://www.ijic.org. URN:NBN:NL:UI:10-1-100270. [PMC free article] [PubMed] [Google Scholar]
- 15.Bjerkan J. A web-based collaborative tool for community individual care plans in Norway, a scientific demonstration. Proceedings of the 10th International Nursing Informatics; 2009 July 1–4; Vanajanlinna, Finland. [Google Scholar]
- 16.Crawford MJ, Rutter D, Manley C, Weaver T, Bhui K, Fulop N, et al. Systematic review of involving patients in the planning and development of health care. British Medical Journal. 2002;325(7375):1263. doi: 10.1136/bmj.325.7375.1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buckingham A, Saunders P. Cambridge: Polity Press; 2004. The Survey Methods Workbook. [Google Scholar]
- 18.Polit DF, Beck CT. Nursing research: principles and methods. Philadelphia, PA: Lippincott Williams and Wilkins; 2004. [Google Scholar]
- 19.Ouwens M, Wollersheim H, Hermens R, Hulscher M, Grol R. Integrated care programmes for chronically ill patients: a review of systematic reviews. International Journal for Quality in Health Care. 2005;17(2):141–6. doi: 10.1093/intqhc/mzi016. [DOI] [PubMed] [Google Scholar]
- 20.Ahgren B, Axelsson S, Axelsson R. Evaluating intersectoral collaboration: a model for assessment by service users. International Journal of Integrated Care [Serial online] 2009 Feb 26;9 doi: 10.5334/ijic.304. [cited 2010 Apr 21]. Available from: http://www.ijic.org. URN:NBN:NL:UI:10-1-100546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sosial- og helsedepartementet. St.meld. nr. 21. Ansvar og meistring. Mot en heilskapeleg rehabiliteringspolitikk. [Report no. 21 to the Storting, 1998–1999. Responsibility and Empowerment: Toward a Holistic Rehabilitation Policy]. Oslo: Sosial og helsedepartementet; 1998. [in Norwegian] [Google Scholar]
- 22.Huseby BM, Paulsen B. Eldreomsorgen i Norge: Helt utilstrekkelig—eller best i verden? [Welfare services for elderly people in Norway: Completely inadequate—or the world’s best?]. Trondheim: Sintef helsetjenesteforskning; 2009. SINTEF A11522. [in Norwegian] [Google Scholar]
- 23.Martinussen PE, Pettersen I, Hofstad T. Kommunenes utgiftsbehov og produksjonskostnader innenfor pleie- og omsorgssektoren: analyser av brukerdata og kommunespesifikke data. [Municipal expenditure requirements and production costs in the nursing and care sector: analyses of user data and municipality-specific behaviour]. Trondheim: SINTEF Helse; 2005. Contract No.: STF78 A055018. [in Norwegian] [Google Scholar]
- 24.Skare A. Jo mer lokalpolitikk, dess mindre partipolitikk. Om partienes rolle i lokalpolitikken. [The more local the politics, the less the party politics. The roles of political parties in local politics]. Norsk statsvitenskapelig tidsskrift. 1996;12(3):239. [in Norwegian] [Google Scholar]
- 25.Kodner D, Spreeuwenberg C. Integrated care: meaning, logic, applications, and implications—a discussion paper. International Journal of Integrated Care [Serial online] 2002 Nov 14;2 doi: 10.5334/ijic.67. [cited 2010 Apr 21]. Available from: http://www.ijic.org. URN:NBN:NL:UI:10-1-100309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wagner EH. The role of patient care teams in chronic disease management. British Medical Journal. 2000;320(7234):569–72. doi: 10.1136/bmj.320.7234.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Truman C, Raine P. Experience and meaning of user involvement: some explorations from a community mental health project. Health and Social Care in the Community. 2002;10(3):136–43. doi: 10.1046/j.1365-2524.2002.00351.x. [DOI] [PubMed] [Google Scholar]
- 28.Thommesen H, Norman T, Sandvin JT. Individuell plan—et sesam, sesam? [Individual care plan—an OpenSesame?]. Oslo: Kommuneforlaget; 2003. [in Norwegian] [Google Scholar]
- 29.Brown B, Crawford P, Carter R. Evidence-based health communication. Maidenhead: Open University Press; 2006. [Google Scholar]
- 30.Vatne S. Computer-based individual plan can make a difference in patients’ subjective quality of life. Persons with mental illness living in the community. [Submitted article; 2010] [Google Scholar]
- 31.Freidson E. Professionalism. The third logic. Cambridge: Polity Press; 2001. [Google Scholar]
- 32.Chambliss DF. Beyond caring: hospitals, nurses, and the social organization of ethics. Chicago, Illinois: University of Chicago Press; 1996. [Google Scholar]
- 33.Abbott A. The system of professions: an essay on the division of expert labor. Chicago, Illinois: University of Chicago Press; 1988. [Google Scholar]
- 34.Laine C, Davidoff F, Lewis CE, Nelson EC, Nelson E, Kessler RC, et al. Important elements of outpatient care: a comparison of patients’ and physicians’ opinions. Annals of Internal Medicine. 1996;125(8):640–5. doi: 10.7326/0003-4819-125-8-199610150-00003. [DOI] [PubMed] [Google Scholar]
- 35.Mechanic D. Managed care and the imperative for a new professional ethic. Health Affairs. 2000;19(5):100–11. doi: 10.1377/hlthaff.19.5.100. [DOI] [PubMed] [Google Scholar]
- 36.Richards A, Carley J, Jenkins-Clarke S, Richards DA. Skill mix between nurses and doctors working in primary care—delegation or allocation: a review of the literature. International Journal of Nursing Studies. 2000;37(3):185–97. doi: 10.1016/s0020-7489(00)00005-5. [DOI] [PubMed] [Google Scholar]
- 37.Hansen GV. Samarbeid uten fellesskap, om individuell planer i kommunalt psykisk helsearbeid. [Coordination without collaboration—about individual care plans in municipal mental health services]. Karlstad: University of Karlstad; 2007. [in Norwegian] [Google Scholar]
- 38.Norsk senter for elektronisk pasientjournal, Helsedirektoratet. EPJ monitor, 2008 Oversikt over utbredelse og bruk av IKT i helsetjenesten. [EPR Monitor. Annual report 2008—Overview of prevalence and use of ICT in healthcare services]. Trondheim: NTNU; 2008. [in Norwegian] [Google Scholar]