Abstract
Health services utilization has been the object of many books and papers in the literature. Measures associated with utilization are often a function of volume of services. The objective of this paper is to present a comprehensive approach to the evaluation of health services utilization and of associated measures, using databases. Based on the theoretical framework of Starfield (1998), we analyze health services utilization with the help of indicators that are not directly linked to volume but that indirectly provide an estimate, while also documenting the qualitative aspects of utilization. The indicators mark accessibility, continuity, comprehensiveness and productivity of care. Once the concepts have been defined, we propose their operationalization using the databases. We then present the advantages of multidimensional conceptualization of health services utilization through a simultaneous analysis of these indicators. Researchers and decision-makers in public health and health planning have much to gain from this innovative multidimensional approach, which presents a dynamic conceptualization of health services utilization based on health administrative data.
This paper was originally published in French, in the journal Pratiques et Organisation des Soins 2011 42(1): 11–18.
Abstract
Dans les nombreuses publications sur l'utilisation des services de santé, les mesures portent le plus souvent sur le volume de services. L'objectif de cet article est de présenter une approche globale d'évaluation de l'utilisation des services de santé de première ligne, et des mesures qui y sont associées à partir des banques de données. En nous basant sur le cadre théorique de Starfield (1998), nous proposons d'analyser l'utilisation des services à l'aide d'indicateurs qui ne sont pas directement liés au volume, mais qui indirectement en donnent une approximation, tout en documentant les aspects qualitatifs de l'utilisation. Ces indicateurs relèvent de l'accessibilité, la continuité, la globalité, et la productivité des soins. Après avoir défini chacun des concepts, nous en proposons leur opérationnalisation à partir des bases de données. Nous présentons ensuite l'intérêt de cette conceptualisation multidimensionnelle de l'utilisation des services à l'aide de l'analyse simultanée de ces indicateurs. Les chercheurs et décideurs en santé publique et en planification de la santé trouveront avantage dans l'utilisation de cette approche multidimensionnelle novatrice. Elle offre une conceptualisation de l'utilisation des services de santé dynamique en s'appuyant sur des bases de données médico-administratives.
Article publié en français dans la revue Pratiques et Organisation des Soins 2011 42(1): 11–18.
Health services utilization has been the subject of many books and papers published in recent years. Utilization is defined as the outcome of the interaction between health professionals and patients (Donabedian 1973). In economic terms, it corresponds to the production of health services and, more specifically in this paper, to the production of health services by physicians (Folland et al. 2006). It is customary to use medical administrative data banks to analyze health services utilization. Measures traditionally associated with health services utilization have often been expressed by outcomes and volume of services. Yet, utilization is a multidimensional process (Donabedian 1973; Starfield 1998).
The objective of this paper is to present a comprehensive, multidimensional and dynamic approach to evaluating health services utilization and its associated measures, using medical administrative databases. Services utilization is considered from the viewpoint of provision of services by physicians.
First, we present various approaches employed to evaluate health services utilization beyond mere volume indicators. Using Starfield's (1998) theoretical framework, we propose a multidimensional evaluation framework for health services utilization. We then highlight various ways of operationalizing indicators. Finally, we illustrate the usefulness of such an approach through an example.
Approaches Used in National and International Institutions
Over the past few years, a number of international organizations have undertaken analyses of health services utilization and health systems, using multidimensional conceptualizations that go beyond mere outcomes. In a 2008 report, the World Health Organization described characteristics of primary care based on several features: “person-centredness, comprehensiveness and integration, and continuity of care, with a regular point of entry into the health system, so that it becomes possible to build an enduring relationship of trust between people and their health-care providers” (Van Lerberghe et al. 2008). These components recognize multidimensional aspects of primary care.
The Organisation for Economic Co-operation and Development (OECD) has developed indicators for years and published reports on the performance of health systems. Countries are classified using weighted sums of scores obtained for each indicator.
Funded by Canada's federal government, the Conference Board of Canada is an organization that offers consulting services. It has also analyzed the performance of health systems, based on several indicators. In its latest health report, the Conference Board uses OECD data to compare the performance of 17 health systems in industrialized countries, using 11 health-related indicators.
The Commonwealth Fund also compares member countries based on indicators for quality of care, accessibility, efficiency, equity and healthcare expenses (Davis et al. 2004; Shea et al. 2007). A report by the Canadian Institute for Health Information (CIHI/ICIS) also puts forward a health indicator framework that includes four dimensions (ICIS 2009). In this report, the indicators are presented independently of one another, with no concern for a comprehensive or multidimensional view.
All these organizations employ several indicators to analyze or compare health systems and health services utilization. This approach opens the door to analyses based on multidimensional conceptualization. However, although these studies take into account numerous indicators in their analyses of health systems, they simply add up scores on each indicator for a given country. Aggregating indicators reduces the available information to a single overall score. The studies rank countries based on their final score, without taking into account the interdependence and possible relationships among indicators. Moreover, when an overall score is used to analyze the performance of health systems and to rank countries, it is impossible to see the indicators for which countries obtain the best and worst scores. Insofar as we agree with the fact that one indicator cannot be substituted for another (e.g., continuity and accessibility), we must move beyond these methods that consist of performing weighted sums of indicator outcomes. It would be more enlightening to think in terms of indicator profiles and relationships among indicators than in terms of aggregation of indicators.
To analyze the performance of Quebec's health system, Sicotte and colleagues (1998) put forward a theoretical framework based on the work of Parsons (1951). The authors reviewed the state of knowledge about performance and integrated it into a multidimensional theoretical framework that can be broken down into four dimensions: adaptation, goal attainment, integration and latency (Sicotte et al. 1998). A performance evaluation report of Quebec's health and social services system, written by the Health and Welfare Commissioner (Levesque 2009), drew inspiration from Sicotte's theoretical framework. It used four dimensions to assess the health system's performance: adaptation, production, development and maintenance of organizational culture, and attainment of goals. A number of indicators were developed for each dimension. The authors then performed a systematic and comprehensive analysis of the indicators within each dimension. They conducted an evaluation of primary care, based on a comprehensive and integrated performance assessment, which was itself based on a configurational vision (Levesque 2009).
Among the studies cited above, we find a will to perform multidimensional evaluations that go beyond mere results-based approaches. However, whatever the level of analysis (macro or micro), most studies analyze services utilization or the health system using synthetic or aggregate indicators. Only Quebec's Health and Welfare Commissioner, who employed a configurational perspective, puts forward a dynamic, multidimensional and integrated approach to evaluation of health services analysis (Levesque 2009).
How to Conduct a Multidimensional Assessment of Primary Care Services Utilization
Services utilization can be assessed from two perspectives: the patient's or the physician's. The first – the patient's perspective – is somewhat subjective because it is based on patient-reported services. A study by Haggerty and colleagues (2008) is a good example of an analysis of health services utilization from the patient's point of view. The second perspective is more objective, because it hinges on volume of medical services offered by physicians to patients and recorded in databases. It is this perspective that we explore in this paper.
Measure of services utilization, from the physician's perspective, is often based on economic indicators based on volume, such as number of hospitalizations per year, number of medical acts, number of patients and number of visits (Andersen and Newman 1973; Beland 1988). An evaluation of services utilization initially involves a volume analysis. In the literature, numerous studies perform services utilization analyses with multivariate analyses based on volume indicators such as medical visits. However, the results of many of these studies are disappointing because of the low percentage of variance explained (Beland 1982). According to Mechanic (1979), the difficulties such studies encounter depend on how the issues are conceptualized, the type of indicators used, the way data are aggregated and the analytical methods chosen. Therefore, we propose to analyze health services utilization with indicators not directly linked to volume through indirectly estimating it, which also document the qualitative aspects of utilization.
A Four-Dimensional Approach
According to Starfield (1998), four essential elements are required for achieving quality of primary care: first contact, longitudinality, comprehensiveness and coordination (integration). First contact implies accessibility: each person who wishes to use health services should have access. Longitudinality refers to continuity, to management of care over time. Comprehensiveness means that a range of services should be available. In the following paragraphs, we describe three of Starfield's indicators of quality: continuity, comprehensiveness and accessibility. Because we are exploring utilization from the angle of service delivery by physicians, we will add productivity to these three indicators, for its relevance to volume and quality. Productivity imparts a non-static image of volume because it makes a connection between production and resources. After defining the four concepts, we suggest possible operationalizations for each of them, using linking data from Régie d'assurance maladie du Québec and from Collège des médecins du Québec. This linked database includes information concerning hours worked, income, acts, patients, and number of visits and days worked billed, for all general practitioners.
Continuity
Continuity refers to the extent to which healthcare is provided uninterrupted over time, within a single care episode or several (Starfield 1998; Lamarche et al. 2003; Levesque et al. 2003). Continuity thus corresponds to ongoing provision of care and integrates a notion of longitudinality. The concept of continuity has not yet been clearly defined (Saultz 2003). In their knowledge synthesis, Haggerty and colleagues (2003) attempt to define three types of continuity: informational, management and relational. Informational continuity refers to the availability and use of past events and circumstances (e.g., prior visits, laboratory results, consultations, referrals) to ensure appropriate current care for the patient. Management continuity guarantees that the care given by several providers is coherent. Management continuity is especially important for chronic health problems. Relational continuity acknowledges the importance of knowing the patient as a person. It refers to an ongoing therapeutic relationship between a patient and one or more care providers.
Comprehensiveness
Comprehensiveness is a two-dimensional concept: it refers to the person as a whole and to all the care that person might need. In other words, it implies a comprehensive approach to individuals in which the full range of their health needs are recognized. There are several levels of health needs: biological, psychological and social. The second aspect of comprehensiveness, and this is the one of interest to us, refers to the range of services offered by a physician or a healthcare organization. Services include preventive, treatment and even palliative care. Identifying needs and offering an array of services to meet these needs are two key elements of comprehensiveness (Starfield 1998; Levesque et al. 2003). Comprehensiveness can be seen as an attribute to both utilization and service delivery.
Chan (2002) has assessed the declining comprehensiveness of primary care by looking at whether physicians perform a minimum threshold number of services from among the following: emergencies, nursing homes, hospitals (50 visits a year), house calls (10 visits a year) and at least two deliveries a year. In this study, Chan measures comprehensiveness by range of services offered. Starfield's (1998) approach is similar in that she indicates that comprehensiveness of health services is measured through range of services. Comprehensiveness can thus be easily determined using data banks. It is a matter of choosing a range of acts billed by physicians that represent the comprehensiveness of services offered.
Accessibility
The notion of accessibility is an attribute of an institution or service that can be accessed (Donabedian 1973; Frenk 1992). It refers to characteristics that facilitate or hinder efforts to reach care services (Pineault and Daveluy 1995). Donabedian (1973) describes access as a group of factors that intervene between capacity to provide services and actual provision or consumption of services. Accessibility is a characteristic of the resources themselves that renders these resources more or less easy to use. According to Levesque and colleagues (2003), several dimensions of access can be measured. Geographical accessibility (geographical availability) is based on (physical and temporal) distance between the location of users and the provision of services. Organizational accessibility (organizational availability) is based on schedules and procedures to follow that constitute constraints for individuals. Social accessibility involves compatibility between services offered and the social and cultural characteristics of individuals. Finally, economic accessibility is linked to the costs of services in relation to individuals' socio-economic status (Starfield 1998).
It is difficult to measure the full concept of accessibility using data banks. However, some aspects of accessibility can be assessed through medical services billed by physicians. Let us look at organizational accessibility, for example. The literature shows that it is possible to use such measures as walk-in visits and availability of after-hours care (Forrest and Starfield 1998) and house calls (Safran et al. 2000).
Productivity
Productivity is defined as the relationship between the production of goods or services and the quantity of factors of production. The notion of productivity refers to a system's capacity to generate a volume of services based on resources available. According to Donabedian (1973), productivity is an intervening factor between resources and production that leads to the conversion of a quantity of resources into a volume of activity. In short, to analyze productivity it is necessary to look at the way resources are employed to produce services (Contandriopoulos et al. 1993). In economic terms, these definitions of productivity express a function of production that links resources to services. The derivative of this function of production provides indications of marginal productivity. In the area of health, work makes up a large part of production factors. As a result, productivity can be measured by the work input-to-output ratio. An increase in worker productivity in the health system increases the output level (Folland et al. 2006).
Concept Operationalization
Continuity
No single operational measure can fully capture the concept of continuity as a whole (Reid et al. 2002). Most indicators of measures of continuity, constructed from medical administrative databases, use chronology of care over time between a patient and a health professional. Concentration over time of services provided by a professional to a patient is evaluated to determine continuity of care. It is possible, for example, to use the number of visits to a physician per patient over a given period of time. The higher the number of visits per patient, the more continuity of care a physician provides to his or her patients. This type of measurement can assess relational continuity because it measures the strength of the patient–doctor interpersonal relationship. Indeed, we assume that prolonged or repeated contact with the same professional builds a stronger relationship, better utilization and information transfer, and more coherent care management (Breslau et al. 2008). Concentrated patient visits to a physician is a good indicator of patient affiliation with a physician and, therefore, relational continuity. A forthcoming study by Burge and Haggerty (2011) indicates that with the concept of relational continuity we can appreciate a physician's knowledge of a patient as well as the concentration of care. In addition, various forms of continuity, as measured in a study by Pineault and colleagues (2008), are correlated. Recent studies thus show that there is a relationship among the three aspects of continuity. By measuring only one of these aspects, it is possible to learn something about continuity as a whole.
Comprehensiveness
In Quebec, general practitioners can bill for the following acts: regular examinations, complete examinations and detailed complete examinations. A regular examination includes at least one of the following: a questionnaire and examination needed for diagnosis and treatment of a minor ailment, initiation of treatment, assessment of a course of treatment and observation of illness evolution. A complete examination involves two elements: a patient questionnaire and a clinical examination of one or several organs or systems related to the reason for the consultation. A detailed complete examination includes a complete patient questionnaire, a clinical examination, recommendations for the patient and recording significant data identified by the physician in the file (Régie de l'assurance maladie du Québec 2010). Only one detailed complete examination can be billed per patient each year. We have analyzed the distributions of these three types of acts for all physicians for a year.
Regular examinations were grouped into three types:
A practice composed of fewer than 35% of regular examinations
A practice composed of 35% to 45% of regular examinations
A practice composed more than 45% of regular examinations
Complete examinations were grouped into three types:
A practice composed of fewer than 45% of complete examinations
A practice composed of 45% to 60% of complete examinations
A practice composed of more than 60% of complete examinations
Detailed complete examinations were grouped into three types:
A practice composed of fewer than 5% of detailed complete examinations
A practice composed of 5% to 15% of detailed complete examinations
A practice composed of more than 15% of detailed complete examinations
Based on these three variables, we constructed an indicator for comprehensiveness of care. Practices composed of more than 15% of detailed complete examinations were defined as highly comprehensive. Likewise, practices composed of average types in all three categories of acts were qualified as highly comprehensive. Practices with fewer than 5% of detailed complete examinations and at least one type that is weak for one of the other two acts were qualified as low in comprehensiveness. These three types of acts shed some light on the scope of services offered by general practitioners. When we combine them, we obtain an estimate of comprehensiveness of services provided by physicians (Borgès Da Silva 2010).
Accessibility
The organizational aspect of accessibility can be analyzed. The literature shows that it is possible to use such measures as density of walk-in visits and availability of after-hours care. In Quebec, physicians can bill for certain acts or types of service packages for services provided on-call and outside office hours. When we combine them, we obtain an estimate of organizational accessibility.
Productivity
To measure productivity of service delivery, we analyze the work output factor and, more specifically, the physician's work. Input is measured in terms of work time, usually referred to as hours worked.
The definition of output is more complex. As Reinhardt (1972) noted, we can use number of patient visits, number of visits in private clinics or patient billing. We can also use variables such as number of acts, number of patients or income (Donabedian 1973).
Therefore, the productivity measure consists in calculating an indicator that provides information on the relationship between number of hours worked by physicians in this context and an output chosen among those listed in the previous paragraph. The output we propose to use is physicians' total clinical income. The input we propose to use is number of hours per year dedicated to clinical activities. Productivity is thus measured using income per hour.
Multidimensional Conceptualization Needed
Based on Starfield's (1998) theoretical framework, we have presented concepts associated with analysis of health services utilization and measures using data banks. The fact of using indicators that go beyond volume and that enable us to view services utilization as a multidimensional, dynamic and integrated process provides a global picture of services utilization that considers the essential components identified by Starfield (1998). Adding productivity, an indicator of volume relating input and output of health services utilization, enriches evaluation of services utilization, seen from an angle of service delivery, using databases. This approach helps us move beyond static analysis of services utilization by volume, and take into account the multidimensional aspects inherent to services utilization. Indeed, indicators interact continually and evolve simultaneously by mutually influencing one another. Thus, they are interdependent and dynamic.
In the literature, very few studies have examined the relationship between these indicators, pair by pair. The indicators are often considered from the patient's point of view. For example, Haggerty and colleagues (2008) used surveys to analyze the characteristics of physicians' practices associated with patient-reported accessibility, continuity and coordinated care. What emerges is that it is difficult to attain a balance between continuity and accessibility. Physicians often organize their practices around continuity at the expense of accessibility. Yet, a minimum of accessibility is required to be able to provide continuity.
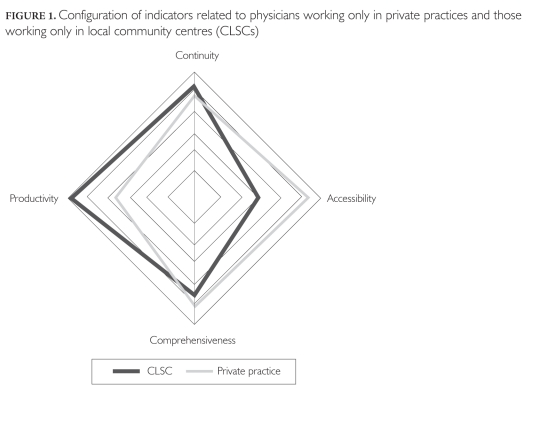
A recent study based on this type of multidimensional and dynamic approach shows results on service utilization seen from the standpoint of provision of services by physicians. It appears that physicians in private clinics provide high continuity and productivity at the expense of accessibility. Physicians working in local community centres (CLSCs) show higher levels of comprehensiveness and accessibility than the average for physicians in Quebec, but productivity and continuity are weaker (Borgès Da Silva 2010) (see Figure 1). This multidimensional approach to services utilization allows, for example, highlighting differences in services delivery by physicians, based on practice setting.
FIGURE 1.
Configuration of indicators related to physicians working only in private practices and those working only in local community centres (CLSCs)
Conclusion
We have presented a comprehensive, dynamic and integrated approach to health services utilization from the perspective of health services delivery. It is based on process indicators (accessibility, continuity and comprehensiveness) and outcome indicators (productivity) that evolve simultaneously while influencing one another. Our indicators were constructed from medical administrative databases, an approach that increases the generalizability of our study. This approach could be generalized at a meso or macro level to obtain a dynamic multidimensional analysis of the health system.
Public health and health planning researchers and decision-makers will benefit from this type of innovative multidimensional approach. It sets out a dynamic conceptualization of health services utilization while relying on medical administrative databases.
Contributor Information
Roxane Borgès Da Silva, Post-Doctoral Fellow, Montreal Public Health Department and Institut national de santé publique du Québec, St. Mary's Research Center, McGill University, Montreal, QC.
André-Pierre Contandriopoulos, Full Professor, Département d'administration de la santé and IRSPUM, Faculty of Medicine, University of Montreal, Montreal, QC.
Raynald Pineault, Medical Consultant, Montreal Public Health Department and Institut national de santé publique du Québec, Professor Emeritus, Faculty of Medicine, University of Montreal, Montreal, QC.
Pierre Tousignant, Medical Consultant, Montreal Public Health Department and Institut national de santé publique du Québec, Montreal, QC.
References
- Andersen R., Newman J.F. Societal and Individual Determinants of Medical Care Utilization in the United States. Milbank Memorial Fund Quarterly Health Society. 1973;51:95–124. [PubMed] [Google Scholar]
- Beland F. The Utilization of Health Services. Sequence of Visits to General Practitioners. Social Science and Medicine. 1982;16:2065–72. doi: 10.1016/0277-9536(82)90162-9. [DOI] [PubMed] [Google Scholar]
- Beland F. Utilization of Health Services as Events: An Exploratory Study. Health Services Research. 1988;23:295–310. [PMC free article] [PubMed] [Google Scholar]
- Borgès Da Silva R. 2010. La Pratique médicale des omnipraticiens: influence des contextes organisationnel et géographique Unpublished doctoral thesis, Université de Montréal; [Google Scholar]
- Breslau N., Reeb K.G. 1975. Continuity of Care in a University-Based Practice. Journal of Medical Education 50: 965 69 [DOI] [PubMed] [Google Scholar]
- Burge F., Haggerty J. 2011. (forthcoming). Comparison of Primary Health Care Evaluation Instruments That Evaluate Relational Continuity of Care from the Consumer Perspective. Healthcare Policy. [Google Scholar]
- Chan B.T. The Declining Comprehensiveness of Primary Care. Canadian Medical Association Journal. 2002;166:429–34. [PMC free article] [PubMed] [Google Scholar]
- Contandriopoulos A.P., Champagne F., Baris E. 1993. La Rémunération des professionnels de santé. Journal d'économie médicale 10: 405 21 [Google Scholar]
- Davis K., Schoen C., Schoenbaum S.C., Audet A.M.J., Doty M.M., Tenney K. 2004. Mirror, Mirror on the Wall: Looking at the Quality of American Health Care through the Patient's Lens New York: The Commonwealth Fund; [Google Scholar]
- Donabedian A. 1973. Aspects of Medical Care Administration: Specifying Requirements for Health Care Cambridge, MA: Harvard University Press; [Google Scholar]
- Folland S., Goodman A.C., Stano M.L. 2006. The Economics of Health and Health Care (5th ed.). Upper Saddle River, NJ: Prentice Hall; [Google Scholar]
- Forrest C.B., Starfield B.H. Entry into Primary Care and Continuity: The Effects of Success. American Journal of Public Health. 1998;88:1330–36. doi: 10.2105/ajph.88.9.1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenk J. 1992. The Concept and Measurement of Accessibility. In White K.L., Frenk J., Ordonez C., Paganini J.M., Starfield B., eds., Health Services Research: An Anthology (pp. 842 55). PAHO Scientific Publication No. 534. Washington, DC: Pan American Health Organization; [Google Scholar]
- Haggerty J.L., Pineault R., Beaulieu M.D., Brunelle Y., Gauthier J., Goulet F., et al. Practice Features Associated with Patient-Reported Accessibility, Continuity, and Coordination of Primary Health Care. Annals of Family Medicine. 2008;6:116–23. doi: 10.1370/afm.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haggerty J.L., Reid R.J., Freeman G.K., Starfield B.H., Adair C.E., McKendry R. Continuity of Care: A Multidisciplinary Review. British Medical Journal. 2003;327:1219–21. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institut canadien d'information sur la santé (ICIS) 2009. Indicateurs de santé 2009 Ottawa: Author; [Google Scholar]
- Lamarche P., Beaulieu M.D., Pineault R., Contandriopoulos A.P., Denis J.L., Haggerty J. 2003. Choices for Change: The Path for Restructuring Primary Healthcare Services in Canada Ottawa: Canadian Health Services Research Foundation; [Google Scholar]
- Levesque J.F. 2009. Rapport d'appréciation de la performance du système de santé et de services sociaux Québec: Commissaire à la santé et au bien-être; [Google Scholar]
- Levesque J.F., Beaulne G., Feldman D., Hamel M., Jalhay J.M., Ouellet D., et al. 2003. L'Organisation des services de première ligne, l'accès aux services, les attributs de l'expérience de soins et la santé: concepts, mesure et effets. Montréal: Direction de santé publique de Montréal; [Google Scholar]
- Mechanic D. 1979. Correlates of Physician Utilization: Why Do Major Multivariate Studies of Physician Utilization Find Trivial Psychosocial and Organizational Effects? Journal of Health and Social Behavior 20: 387 96 [PubMed] [Google Scholar]
- Parsons T. 1951. The Social System New York: The Free Press/Macmillan; [Google Scholar]
- Pineault R., Daveluy C. 1995. La Planification de la santé: concepts, méthodes, stratégies Montréal: Éditions Nouvelles; [Google Scholar]
- Pineault R., Levesque J.F., Roberge D., Hamel M., Lamarche P., Haggerty J. 2008. L'Accessibilité et la continuité des services de santé: une étude sur la première ligne au Québec Rapport de recherche. Montréal: Direction de santé publique de l'Agence de la santé et des services sociaux de Montréal, Institut national de santé publique, Centre de recherche de l'Hôpital Charles LeMoyne; [Google Scholar]
- Régie de l'assurance maladie du Québec 2010. Manuel de facturation des médecins omnipraticiens du Québec Québec: Author; [Google Scholar]
- Reid R., Haggerty J., McKendry R. 2002. Dissiper la confusion: concepts et mesures de la continuité des soins Comité consultatif des services de santé de la Conférence fédérale–provinciale–territoriale des sous-ministres de la santé. Ottawa: Institut canadien d'information sur la santé; [Google Scholar]
- Reinhardt U. A Production Function for Physician Services. Review of Economics and Statistics. 1972;54:55–66. [Google Scholar]
- Safran D.G., Rogers W.H., Tarlov A.R., Inui T.S., Taira D.A., Montgomery J.E., et al. 2000. Organizational and Financial Characteristics of Health Plans: Are They Related to Primary Care Performance? Archives of Internal Medicine 160: 69 76 [DOI] [PubMed] [Google Scholar]
- Saultz J.W. Defining and Measuring Interpersonal Continuity of Care. Annals of Family Medicine. 2003;1:134–43. doi: 10.1370/afm.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shea K.K., Holmgren A.L., Osborn R., Schoen C. 2007. Health System Performance in Selected Nations: A Chartpack New York: The Commonwealth Fund; [Google Scholar]
- Sicotte C., Champagne F., Contandriopoulos A.P., Barnsley J., Béland F., Leggat S.G., et al. A Conceptual Framework for the Analysis of Health Care Organizations' Performance. Health Services Management Research. 1998;11:24–41. doi: 10.1177/095148489801100106. [DOI] [PubMed] [Google Scholar]
- Starfield B. 1998. Primary Care: Balancing Health Needs, Services and Technology (rev. ed.). New York: Oxford University Press; [Google Scholar]
- Van Lerberghe W., Evans T., Rasanathan K., Mechbal A. 2008. The World Health Report 2008: Primary Health Care—Now More Than Ever Geneva: World Health Organization; [Google Scholar]