Abstract
Background
Length of hospital stay after acute myocardial infarction declined significantly in the 1980's and 1990's. Whether length of stay has continued to decline during the 2000's, and the impact of decreasing length of stay on rehospitalization and mortality, is unclear. We describe decade long (1995–2005) trends in length of stay after acute myocardial infarction, and examine whether declining length of stay has impacted early rehospitalization and post-discharge mortality in a population-based sample of hospitalized patients.
Methods
The study sample consisted of 4,184 patients hospitalized with acute myocardial infarction in a central New England metropolitan area during 6 annual periods (1995, 1997, 1999, 2001, 2003, 2005).
Results
The average age of the study sample was 71 years and 54% were men. The average length of stay declined by nearly one third over the 10-year study period from 7.2 days in 1995 to 5.0 days in 2005 (p<0.001). Younger patients (<65 years), men, and patients with an uncomplicated hospital stay had significantly shorter lengths of stay than respective comparison groups. Lengths of stay shorter than the median were not associated with significantly higher odds of hospital readmission at 7 or 30-days post-discharge, or with mortality in the year after discharge. In contrast, longer lengths of stay were associated with significantly higher odds of short-term mortality. These findings did not vary by year under study.
Conclusions
Length of stay in patients hospitalized for acute myocardial infarction declined significantly between 1995 and 2005. Declining length of stay is not associated with an increased risk for early readmission or all-cause mortality.
Keywords: Epidemiology, Acute myocardial infarction, DNR Orders
Length of hospital stay in patients with acute myocardial infarction has declined significantly over the past two decades from an average duration of more than 10 days in the 1980s to between 6 and 8 days in the 1990s.1–3 Declining length of stay potentially results in a greater number of patients at risk for early hospital readmission and for dying in the weeks following hospital discharge.
While post discharge mortality rates after hospitalization for acute myocardial infarction have declined over the past 2 decades, it remains unclear whether shorter lengths of stay are associated with higher death and rehospitalization rates after hospital discharge for acute myocardial infarction.4–6 In a study of more than 8,600 Medicare patients hospitalized with acute myocardial infarction between 1991 and 1997, significant declines in length of stay were associated with increases in hospital readmissions within 30 days of the index event.1 In addition, while declining length of stay was not associated with higher 30-day death rates in all patients, increased post-discharge mortality was observed in patients hospitalized for acute myocardial infarction who had early do-not-resuscitate (DNR) orders, suggesting that certain groups may be at risk for poorer outcomes following shorter hospital stays.
While the economic benefit and safety of `early' hospital discharge in patients with an uncomplicated acute myocardial infarction has been noted in previous clinical trials carried out during the 1990's,7–10 there remains uncertainty about the optimal timing of discharge after acute myocardial infarction, particularly from a contemporary, population-based perspective. The objectives of this study were to describe decade long (1995–2005) trends in length of stay after acute myocardial infarction and examine whether declining length of stay was associated with an increased risk of early rehospitalization and post-discharge all-cause mortality among residents of a large metropolitan area in New England.
METHODS
Data for this study were derived from the Worcester Heart Attack Study.11–13 This is an ongoing population-based investigation that is examining long-term trends in the incidence, hospital, and post-discharge case-fatality rates of acute myocardial infarction among residents of the Worcester (MA) metropolitan area hospitalized at all area medical centers. The details of this study have been described previously.12, 13 In brief, the medical records of area residents (2000 census estimate = 478,000) hospitalized for possible acute myocardial infarction at all area medical centers were individually reviewed and a diagnosis of acute myocardial infarction was validated according to predefined criteria. Patients who developed acute myocardial infarction secondary to an interventional procedure or surgery were excluded from the study sample.
A total of 4,184 patients who satisfied the diagnostic criteria for acute myocardial infarction during the 6 annual periods examined (1995, 1997, 1999, 2001, 2003, 2005), and were discharged alive during the years under study, constituted the population of this report. Patients with a hospital stay longer than 1 month, transfers (in or out of study hospitals), and those undergoing coronary artery bypass graft surgery were excluded due to extremely long average lengths of stay in these patients.
Data Collection
Demographic, medical history, and clinical data were abstracted from hospital medical records by trained study physicians and nurses. Information was collected about patient's age, sex, body mass index, comorbidities (e.g., hypertension, heart failure, stroke), acute myocardial infarction order (initial vs. prior), location (anterior vs inferior/posterior), and type (Q wave vs. non–Q wave), hospital treatment approaches, and hospital discharge status. Information was also collected about the occurrence of in-hospital complications including stroke,14 atrial fibrillation,15 heart failure,16 and cardiogenic shock.17 Information about the use of DNR orders was collected through the review of hospital records and physician's progress notes. Survival status after hospital discharge was ascertained through a review of the medical records for additional hospitalizations and statewide and national searches of death records for area residents.
Data Analysis
We examined differences in the distribution of selected characteristics in patients with varying lengths of stay using chi-square tests. We used multivariate logistic regression to examine the association between demographic, clinical, and treatment variables and a length of stay shorter than the median. We controlled for several variables including age, sex, insurance payer status, medical history, acute myocardial infarction associated characteristics, hospital clinical complications, receipt of effective cardiac medications (e.g., β-blockers, angiotensin-converting enzyme (ACE) inhibitors), and receipt of cardiac procedures (cardiac catheterization or percutaneous revascularization) during the index hospitalization.
Logistic multivariable regression was used to examine the association between length of stay and post-discharge mortality at 30 days after hospital admission and 90-days after hospital discharge. Logistic regression was also used to examine the association between length of stay and rehospitalization at 7 and 30 days after discharge, controlling for previously described potentially confounding factors. A Cox proportional hazards regression approach was used to examine differences in rehospitalization in the 12-months following hospital discharge according to length of stay while controlling for duration of follow-up and potentially confounding demographic and clinical factors.
RESULTS
Length of Hospital Stay
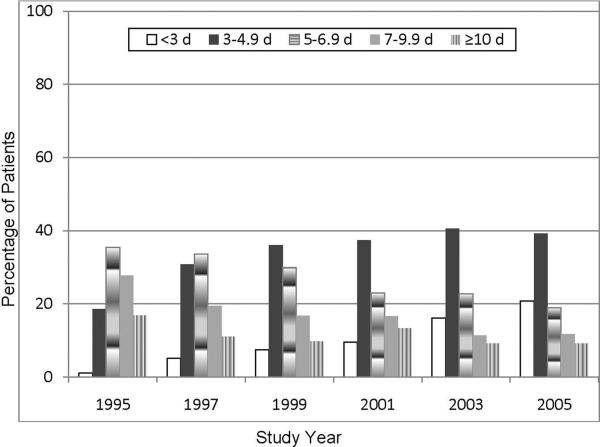
There have been marked changes in the distribution of length of stay for greater Worcester residents hospitalized with acute myocardial infarction during the period under study (1995–2005) (Figure 1). The average length of stay declined by more than 2 days over the 10-year study period from 7.2 days in 1995 to 5.0 days in 2005, corresponding to a 30% overall decline in length of stay over this period. In 1995, <20% of patients were hospitalized for less than 5 days compared with approximately 60% of patients in 2005. Extremely long lengths of stay (≥10 days) declined from nearly one fifth of patients in 1995 to less than 10% in 2005.
Figure 1.
Trends in length of stay in patients hospitalized with acute myocardial infarction. (The Worcester Heart Attack Study)
Study Sample Characteristics
Duration of hospitalization was categorized into 5 strata based on the distribution of our data and based on what was considered to be long and short hospital stays for patients hospitalized with acute myocardial infarction during the period under study. Patients with shorter hospital stays were younger, more likely to be men, and were more likely to be enrolled in an HMO (Table 1). These patients were less likely to have a medical history of selected comorbidities and to present with an ST segment -elevation MI; they were less likely to present with an anterior MI. Patients with shorter hospital stays were significantly less likely to develop each of the clinical complications examined and were less likely to have a DNR order compared to patients with longer hospitalizations.
Table 1.
Characteristics of patients with acute myocardial infarction (AMI) according to length of hospital stay (Worcester Heart Attack Study).
| Length of Hospital Stay, days | ||||||
|---|---|---|---|---|---|---|
| Characteristic | <3 (n=428) | 3–4.9 (n=1429) | 5–6.9 (n=1131) | 7–9.9 (n=713) | ≥10 (n=483) | P-value |
| Age, years, % | ||||||
| <65 | 43.9 | 37.9 | 27.6 | 20.1 | 21.3 | |
| 65–74 | 18.7 | 20.2 | 22.6 | 24.3 | 26.7 | |
| 75–84 | 20.3 | 24.3 | 28.7 | 35.3 | 36.2 | |
| ≥85 | 17.1 | 17.6 | 21.0 | 20.3 | 15.7 | <0.001 |
| Men(%) | 61.7 | 59.7 | 53.9 | 46.8 | 47.0 | <0.001 |
| Payer(%) | ||||||
| Private payment | 1.9 | 1.8 | 2.0 | 1.3 | 2.3 | |
| Private insurance | 2.6 | 3.6 | 2.6 | 2.8 | 2.5 | |
| Blue Cross | 9.6 | 6.4 | 4.7 | 3.7 | 5.2 | |
| Medicaide | 4.0 | 3.1 | 2.6 | 2.5 | 4.0 | |
| Medicare | 36.8 | 39.6 | 51.4 | 57.6 | 60.0 | |
| HMO | 38.9 | 38.8 | 31.1 | 28.4 | 22.8 | |
| Other | 6.3 | 6.7 | 5.6 | 3.7 | 3.1 | <0.001 |
| Medical history(%) | ||||||
| Hypertension | 68.2 | 65.4 | 66.8 | 69.4 | 72.6 | 0.04 |
| Diabetes | 36.6 | 29.9 | 30.4 | 35.9 | 40.3 | <0.001 |
| Stroke | 7.7 | 8.6 | 8.6 | 11.4 | 12.7 | 0.01 |
| Heart failure | 23.6 | 20.0 | 24.0 | 31.4 | 31.3 | <0.001 |
| Angina | 21.7 | 20.0 | 23.3 | 26.5 | 21.3 | 0.01 |
| AMI associated characteristics(%) | ||||||
| Initial | 61.7 | 66.4 | 62.6 | 59.9 | 64.0 | 0.04 |
| Q Wave | 14.2 | 24.6 | 26.2 | 23.3 | 27.1 | <0.001 |
| Anterior | 12.9 | 15.0 | 18.9 | 22.4 | 19.1 | <0.001 |
| STEMI | 30.8 | 33.4 | 29.4 | 26.1 | 27.5 | 0.005 |
| Do not resuscitate order (%) | 17.3 | 18.9 | 19.9 | 24.1 | 26.7 | <0.001 |
| Complications during hospitalization (%) | ||||||
| Cardiogenic shock | 0.7 | 0.7 | 1.1 | 2.5 | 11.2 | <0.001 |
| Heart failure | 22.2 | 25.8 | 36.3 | 48.4 | 65.0 | <0.001 |
| Recurrent angina | 12.2 | 17.2 | 24.3 | 23.7 | 32.8 | <0.001 |
| Stroke | 0.2 | 0.7 | 0.8 | 2.7 | 4.2 | <0.001 |
| Atrial fibrillation | 11.5 | 11.9 | 14.0 | 19.4 | 28.6 | <0.001 |
| Therapies(%) | ||||||
| Aspirin | 94.6 | 93.9 | 93.8 | 92.8 | 92.1 | 0.48 |
| ACE inhibitors | 58.9 | 58.8 | 52.7 | 56.7 | 66.1 | <0.001 |
| B-blockers | 90.6 | 89.0 | 86.9 | 86.4 | 82.0 | <0.001 |
| Calcium antagonists | 26.4 | 22.1 | 29.4 | 30.1 | 36.9 | <0.001 |
| Lipid lowering agents | 62.2 | 56.4 | 42.3 | 39.0 | 38.1 | <0.001 |
| Thrombolitics | 2.3 | 10.0 | 14.2 | 12.9 | 9.5 | <0.001 |
| Procedures during hospitalization(%) | ||||||
| Cardiac catheterization | 55.6 | 47.6 | 40.4 | 44.9 | 50.2 | <0.001 |
| PTCA | 43.7 | 35.9 | 25.2 | 27.7 | 30.3 | <0.001 |
Patients with shorter lengths of stay were more likely to be treated with β-blockers and lipid lowering agents but were less likely to be treated with thrombolytic agents. Patients in the longest length of stay strata (≥10 days) were significantly more likely to be treated with ACE inhibitors than were all other patients. The use of cardiac catheterization was highest among patients at the extremes of length of stay (long and short) compared with those with more intermediate stays while patients with shorter lengths of stay were more likely to undergo a percutanous coronary intervention (PCI).
We also examined whether patient characteristics stratified according to median length of stay were different across the various periods under study (Table 2). The median length of stay was 6 days for patients hospitalized in our initial 2 study years (1995/97), 5 days for those hospitalized during 1999/2001, and 4 days for those hospitalized during 2003/2005. History of several medical comorbidities, including stroke, heart failure, and diabetes, were significantly associated with longer length of stay only during the most recent study years. In contrast, the associations between length of stay and in-hospital treatment with ACE inhibitors, cardiac catheterization, and PCI were attenuated in later study years. Fewer patients presented with Q-wave and anterior acute myocardial infarctions, whereas a greater proportion of patients presented with ST segment -elevation MIs, during the most recent study years. Acute myocardial infarction characteristics did not vary over time according to length of stay.
Table 2.
Characteristics of patients with acute myocardial infarction (AMI) according to length of hospital stay (Worcester Heart Attack Study).
| 1995/1997 (n=1,323) | 1999/2001 (n=1,409) | 2003/2005 (n=1,448) | ||||
|---|---|---|---|---|---|---|
| Length of stay | Length of stay | Length of stay | ||||
| Characteristic | <Median | ≥Median | <Median | ≥Median | <Median | ≥Median |
| Age (yrs) | ||||||
| <65 | 37.2 | 27.1 | 38.6 | 22.4 | 44.4 | 21.7 |
| 65–74 | 27.1 | 26.9 | 19.1 | 23.0 | 17.4 | 19.5 |
| 75–84 | 25.0 | 31.0 | 23.3 | 34.1 | 19.8 | 33.1 |
| ≥85 | 10.7 | 15.1 | 19.1 | 20.6 | 18.4 | 25.7 |
| Men (%) | 62.3 | 51.2 | 58.6 | 51.2 | 62.3 | 47.2 |
| Medical History (%) | ||||||
| Angina pectoris | 24.6 | 26.9 | 19.7 | 24.0 | 19.8 | 19.1 |
| Stroke | 10.5 | 10.5 | 10.2 | 14.1 | 9.0 | 14.0 |
| Hypertension | 55.3 | 65.8 | 65.2 | 69.1 | 69.4 | 79.4 |
| Diabetes mellitus | 29.6 | 32.1 | 29.2 | 32.0 | 27.5 | 40.3 |
| Heart Failure | 15.9 | 20.9 | 20.8 | 32.2 | 21.6 | 32.5 |
| AMI associated characteristics (%) | ||||||
| Initial | 66.3 | 63.2 | 65.3 | 60.6 | 64.7 | 62.2 |
| Q-wave | 29.4 | 32.4 | 24.1 | 22.1 | 18.1 | 19.0 |
| Anterior | 24.7 | 27.5 | 15.8 | 14.4 | 11.0 | 12.9 |
| STEMI | 24.5 | 19.4 | 40.3 | 37.2 | 30.6 | 28.8 |
| Clinical complications (%) | ||||||
| Heart failure | 22.0 | 42.5 | 26.9 | 46.2 | 23.5 | 49.8 |
| Cardiogenic shock | 0.3 | 3.6 | 0.3 | 3.9 | 1.2 | 3.5 |
| Recurrent angina | 17.1 | 34.6 | 16.3 | 28.7 | 14.2 | 23.8 |
| Atrial fibrillation | 6.4 | 12.8 | 10.0 | 20.2 | 14.2 | 25.5 |
| Stroke | 0.2 | 1.8 | 0.6 | 2.3 | 0.7 | 2.2 |
| Do not resuscitate order | 10.9 | 16.5 | 21.2 | 26.2 | 17.4 | 28.7 |
| Therapies(%) | ||||||
| Aspirin | 94.7 | 93.5 | 92.8 | 90.9 | 95.1 | 94.6 |
| ACE inhibitors | 37.8 | 47.8 | 55.4 | 60.9 | 68.6 | 71.0 |
| B-blockers | 81.4 | 81.5 | 87.7 | 84.4 | 95.3 | 94.2 |
| Calcium antagonists | 29.6 | 31.8 | 24.1 | 30.6 | 19.1 | 28.5 |
| Lipid lowering agents | 18.9 | 14.2 | 55.8 | 48.4 | 76.7 | 71.5 |
| Thrombolitics | 20.4 | 21.1 | 12.5 | 10.7 | 0.5 | 1.4 |
| Procedures during hospitalization(%) | ||||||
| Cardiac catheterization | 26.5 | 38.2 | 43.8 | 44.4 | 68.4 | 55.5 |
| PTCA | 12.5 | 16.5 | 31.6 | 27.1 | 56.7 | 45.2 |
Factors Associated with Shorter Hospital Stays
We examined the multivariable adjusted association between various patient demographic and clinical characteristics with hospital length of stay less than the median (5 days) using logistic regression. Patients aged <65 years were significantly more likely to have shorter hospitalizations compared with older patients (Table 3). Male sex and an uncomplicated hospital stay were associated with shorter lengths of stay. Patients presenting with a non Q-Wave or inferior/posterior acute myocardial infarction, compared to those presenting with a Q-wave or anterior acute myocardial infarction, were significantly more likely to have a hospital stay <5 days. The development of cardiogenic shock and stroke during hospitalization were strongly associated with longer lengths of stay. Compared with patients with Blue Cross/Blue Shield insurance, those who were covered under Medicare were significantly more likely to have a prolonged hospital stay. Length of stay did not vary significantly according to other payment types or treatment with effective cardiac medications or coronary interventional procedures.
Table 3.
Factors associated with length of stay shorter than the median in patients hospitalized with acute myocardial infarction (AMI) in the full cohort and in select study years. (Worcester Heart Attack Study)
| Characteristic | Total Cohort (N=4,184) Odds Ratio (95% CI) | 1995/1997 (n=1,323) Odds Ratio (95% CI) | 2003/2005 (n=1,448) Odds Ratio (95% CI) |
|---|---|---|---|
| Age (yrs) | |||
| 65–74 | 0.65 (0.53, 0.80) | 0.70 (0.46, 1.06) | 0.51 (0.36, 0.73) |
| 75–84 | 0.59 (0.48, 0.73) | 0.52 (0.33, 0.82) | 0.37 (0.26, 0.53) |
| ≥85 | 0.78 (0.60, 1.00) | 0.46 (0.27, 0.80) | 0.49 (0.32, 0.75) |
| Women | 0.79 (0.68, 0.91) | 0.73 (0.56, 0.94) | 0.72 (0.56, 0.92) |
| Medical History | |||
| Angina pectoris | 0.95 (0.80, 1.12) | 1.19 (0.89, 1.59) | 1.46 (1.08, 1.98) |
| Stroke | 0.97 (0.77, 1.23) | 1.15 (0.72, 1.85) | 0.90 (0.60, 1.34) |
| Hypertension | 0.94 (0.81, 1.10) | 1.14 (0.88, 1.47) | 1.49 (1.12, 1.99) |
| Diabetes mellitus | 0.97 (0.83, 1.13) | 0.97 (0.74, 1.26) | 0.72 (0.55, 0.93) |
| Heart Failure | 1.03 (0.86, 1.23) | 1.02 (0.72, 1.45) | 1.13 (0.82, 1.55) |
| AMI associated characteristics | |||
| Initial | 0.99 (0.85, 1.15) | 1.18 (0.89, 1.57) | 0.84 (0.65, 1.10) |
| Q-wave | 0.72 (0.61, 0.85) | 0.84 (0.64, 1.12) | 0.60 (0.43, 0.85) |
| Anterior | 0.71 (0.60, 0.85) | 0.96 (0.73, 1.27) | 0.92 (0.63, 1.35) |
| Clinical complications | |||
| Heart failure | 0.43 (0.67, 0.50) | 0.42 (0.31, 0.55) | 0.38 (0.30, 0.51) |
| Cardiogenic shock | 0.29 (0.16, 0.53) | 0.12 (0.03, 0.53) | 0.52 (0.21, 1.30) |
| Recurrent angina | 0.41 (0.35, 0.49) | 0.41 (0.30, 0.54) | 0.39 (0.28, 0.53) |
| Atrial fibrillation | 0.75 (0.62, 0.91) | 0.67 (0.43, 1.03) | 0.71 (0.52, 1.00) |
| Stroke | 0.31 (0.16, 0.62) | 0.09 (0.01, 0.73) | 0.41 (0.13, 1.26) |
| Do not resuscitate order | 0.82 (0.67, 1.00) | 1.16 (0.77, 1.73) | 1.07 (0.76, 1.49) |
| Payer | |||
| Private payment | 0.58 (0.34, 1.02) | 1.11 (0.40, 3.04) | 0.52 (0.20, 1.32) |
| Private insurance | 0.84 (0.53, 1.34) | 0.42 (0.16, 1.12) | 0.71 (0.36, 1.38) |
| Medicaid | 0.70 (0.45, 1.11) | 0.94 (0.36, 2.46) | 0.70 (0.35, 1.41) |
| Medicare | 0.59 (0.45, 0.79) | 0.86 (0.42, 1.77) | 0.88 (0.60, 1.30) |
| HMO | 0.96 (0.72, 1.27) | 0.85 (0.42, 1.73) | 0.90 (0.61, 1.31) |
| Other | 0.98 (0.66, 1.43) | 1.11 (0.46, 2.65) | 0.88 (0.43, 1.77) |
| Therapies | |||
| Effective Cardiac Medications | 1.68 (0.87, 3.23) | 0.73 (0.28, 1.92) | 999.99 (0.01, >999.99) |
| Any Intervention procedures | 1.04 (0.89, 1.21) | 0.45 (0.34, 0.61) | 1.07 (0.78, 1.45) |
Note. *Respective referent categories = age<65 years, male sex, absence of selected medical history variables, prior AMI, Non-Q-wave AMI, inferior or posterior AMI, absence of selected clinical complications, absence of a do not resuscitate order, Blue Cross Blue Shield insurance, not receiving cardiac medications, and not undergoing cardiac procedures.
Effective cardiac medications: aspirin, β-blockers, angiotensin-converting enzyme (ACE) inhibitors, lipid lowering agents, and thrombolytics
We also examined whether factors associated with shorter length of stay varied during the period under study using multivariable adjusted logistic regression analyses (Table 3). After adjusting for previously described covariates, demographic factors associated with a length of stay shorter than the median (younger age and male sex) did not differ over these 3 time periods. With the exception of diabetes, which was associated with a longer length of stay in 2003/2005, none of the medical comorbidities were associated with length of stay during the time periods examined. Patients whose hospitalizations were not complicated by the development of heart failure, recurrent angina, or atrial fibrillation were significantly more likely to have a shorter length of stay during all periods under study. In contrast, the associations between the development of cardiogenic shock and stroke with length of stay were attenuated in the most recent study years (Table 3).
The association between in-hospital cardiac procedures (e.g., PCI, cardiac catheterization) and length of stay was also attenuated in later study years (Table 3). Other factors associated with prolonged hospital stays (payer and absence of treatment with effective cardiac medications) did not vary according to the period under study (data not shown).
Length of Hospital Stay and Post-Discharge Mortality
We carried out a series of multivariable adjusted models to examine the association between length of stay and post discharge all-cause death rates. In these analyses, 5–6.9 days represented the reference category since it contained the median length of stay. We found that very long hospital stays (≥10 days) were associated with a significantly higher risk of dying during the 30 and 90 days post discharge compared to hospital stays of 5–6.9 days (Table 4). Patients hospitalized for <5 days were no more likely to die in the 30 or 90 days following hospital discharge than were our reference group of patients. The adjusted association between 30 and 90-day mortality and length of stay did not vary according to the presence of DNR orders (data not shown).
Table 4.
Likelihood of dying after hospital discharge for AMI according to length of stay during index hospitalization. (Worcester Heart Attack Study)
| Adjusted OR | ||||
|---|---|---|---|---|
| Length of Stay, d | Number of Deaths | Postdischarge Death Rate, % | Multivariable Odds of Dying, Model 1† | Multivariable Odds of Dying, Model 2 |
| 30 Days After Discharge | ||||
| <3 | 18 | 4.2 | 1.36 (0.76, 2.42) | 1.25 (0.70, 2.25) |
| 3–4.9 | 69 | 4.8 | 1.38 (0.93, 2.03) | 1.28 (0.87, 1.89) |
| 5–6.9 | 51 | 4.5 | 1.0* | 1.0* |
| 7–9.9 | 45 | 6.3 | 1.27 (0.82, 1.95) | 1.38 (0.89, 2.12) |
| ≥10 | 49 | 10.1 | 2.38 (1.55, 3.65) | 2.68 (1.74, 4.15) |
| 90 Days After Discharge | ||||
| <3 | 35 | 8.2 | 1.25 (0.81, 1.92) | 1.18 (0.76, 1.82) |
| 3–4.9 | 126 | 8.8 | 1.22 (0.91, 1.63) | 1.16 (0.86, 1.55) |
| 5–6.9 | 102 | 9.0 | 1.0 | 1.0 |
| 7–9.9 | 100 | 14.0 | 1.51 (1.11, 2.06) | 1.67 (1.22, 2.29) |
| ≥10 | 96 | 19.9 | 2.53 (1.83, 3.50) | 2.88 (2.07, 4.01) |
Adjusted for age, sex, payor status, history of medical comorbidities, AMI-associated characteristics, and occurrence of any acute clinical complications.
Adjusted for all variables in the previous model plus in-hospital use of any cardiac medications and coronary intervention procedures.
Indicates reference category
When we restricted the sample to patients with uncomplicated MIs only [defined as the absence of all in-hospital complications (cardiogenic shock, atrial fibrillation, heart failure, stroke, recurrent angina)], and examined the association between length of stay and post discharge mortality, findings were similar to those reported in the total study sample. Patients with length of stay shorter than the median were no more likely to die in the 30 or 90-days after discharge than were the reference group who were hospitalized for 5–6 days. Extremely long hospital stays (>10 days) were associated with significantly higher 30-day (OR=4.33, 95%CI 1.2, 15.9) and 90-day (OR=4.01, 95%CI 1.7, 9.6) mortality.
We also compared length of stay and post discharge mortality in older (≥65 years) versus younger patients (<65 years). Similar to findings in the overall sample, both older and younger patients hospitalized for 7 days or longer were significantly more likely to have died in the 30 and 90 days following hospital discharge, although the association was much stronger in younger patients (Table 5).
Table 5.
Likelihood of dying after hospital discharge for AMI according to length of stay during index hospitalization according to age. (Worcester Heart Attack Study)
| Age, Years | ||
|---|---|---|
| Length of Stay, d | <65 Multivariable Odds of Dying | 65+ Multivariable Odds of Dying |
| 30-Days After Discharge | ||
| <3 | 0.71 (0.6, 8.93) | 1.29 (0.71, 2.34) |
| 3–4.9 | 1.25 (0.19, 8.19) | 1.25 (0.84, 1.87) |
| 5–6.9 | 1.0 | 1.0 |
| 7–9.9 | 2.47 (0.31, 19.89) | 1.33 (0.86, 2.06) |
| ≥10 | 6.82 (1.23, 41.23) | 2.24 (1.43, 3.49) |
| 90-Days After Discharge | ||
| <3 | 1.09 (0.21, 5.49) | 1.18 (0.75, 1.85) |
| 3–4.9 | 1.95 (0.56, 6.89) | 1.09 (0.81, 1.47) |
| 5–6.9 | 1.0 | 1.0 |
| 7–9.9 | 2.35 (0.53, 10.44) | 1.56 (1.13, 2.14) |
| ≥10 | 6.93 (1.83, 26.12) | 2.43 (1.73, 3.42) |
Adjusted for sex, payor status, history of medical comorbidities, AMI-associated characteristics, occurrence of any acute clinical complications, in-hospital use of any cardiac medications and coronary intervention procedures.
Length of Stay and Hospital Readmission
Hospital readmission data were only available for patients hospitalized with acute myocardial infarction during our 2 most recent study years of 2003 and 2005. During these years, nearly one half (46%) of all patients were rehospitalized for any cause within the ensuing 12-months. Rates of rehospitalization differed according to length of stay during the index hospitalization for acute myocardial infarction. Compared with patients hospitalized for shorter than the median length of stay during 2003 and 2005 (4 days), those who were hospitalized for 4 or more days had lower rates of rehospitalization at 7-days (5.7% vs 5.0%) but higher rates at 1 month (14.5% vs 17.9%), 3 months (24.7% vs 31.0%), and 1 year (41.3% vs 48.4%) after hospital discharge.
Logistic regression was used to examine the association between length of stay and rehospitalization in the 7 and 30 days after hospital discharge for acute myocardial infarction. After adjusting for several potential confounding variables, the association between length of stay and rehospitalization was attenuated. At both 7 and 30 days post discharge, the odds of rehospitalization among patients whose index hospitalization was shorter than the median number of days did not differ significantly from those with longer hospital stays (7-day OR =1.28, 95% CI 0.79, 2.08; 30-day OR =0.94, 95% CI 0.70, 1.27). We found similar results when we used a proportional hazards regression analysis to examine the association of length of stay with rehospitalization during the first year after hospital discharge. The odds of rehospitalization after a length of stay shorter than the median did not differ significantly from longer stays (adjusted OR = 0.90, 95% CI 0.74, 1.08) and the association did not differ by year (2003 OR =0.91, 95% CI 0.68, 1.19; 2005 OR =0.83, 95% CI 0.64, 1.10).
DISCUSSION
The results of this population-based observational study suggest that the average length of stay in patients hospitalized with validated acute myocardial infarction in a large New England community declined between 1995 and 2005. Additionally, we found that shorter lengths of stay did not adversely affect the risk of hospital readmission 7 and 30 days after hospital discharge or mortality in the 30 and 90 days following discharge.
A number of studies have shown that, despite the advanced age and greater frequency of comorbidities in patients hospitalized with acute myocardial infarction during recent years, length of stay has declined significantly over the past 2 decades.1, 2, 18–20 A study of 8,612 Medicare patients in northeast Ohio hospitalized with acute myocardial infarction reported a 25% decrease in average length of stay between 1991 and 1997;1 a recent report on 4,458 patients with acute myocardial infarction in Minneapolis-St. Paul, Minnesota, found a more than 50% decline in the median length of stay between 1985 and 2001.2 We found a nearly one third decrease in the average and median length of stay over the 10-year period examined in the present study (1995–2005).
Mortality rates after hospital discharge are a potential indicator of whether or not these declines in length of stay represent optimal patient care. The two large, previously described, cohorts of patients hospitalized with acute myocardial infarction have reported on the association between decreasing length of stay and post-discharge mortality with varying results.1, 2 The northeast Ohio study of Medicare patients reported that the 30-day mortality rate among patients with acute myocardial infarction increased nearly 50% between 1991 and 1997, particularly in patients with early DNR orders.1 In contrast, in the Minnesota Heart Survey, declining length of stay between 1985 and 2001 was not associated with an increased risk of dying in the 6-months post-hospital discharge.2 We found that extended lengths of stay (≥10 days) were associated with a significantly higher risk of dying at 30 and 90-days post discharge but that length of stay shorter than the median was not associated with poorer long-term outcomes. In addition the association between length of stay and post discharge mortality did not vary according to DNR status in our cohort.
There has been concern that shorter hospital stays may result in an increased risk of rehospitalization, although several studies reported no change in rehospitalization rates over periods during which lengths of stay declined significantly.1, 20 Similarly, we found that the adjusted odds of rehospitalization in the year after hospital discharge did not differ significantly by length of stay. Our findings on rehospitalization rates must, however, be interpreted with caution since these data were available only for patients hospitalized for acute myocardial infarction during the two most recent years under study (2003 and 2005).
There are a number of factors that may contribute to declining lengths of stay among patients hospitalized with acute myocardial infarction. These factors include improvements in medical management and the timing of these therapies, changing physician practices, patient preferences, and economic pressures to improve the efficiency of hospitalizations. Several effective cardiac therapies have been shown to be associated with significantly shorter hospital stays18, 19 and increasing use of these therapies over time21 may account, in part, for the declining length of stay of patients that we observed. Similarly, increasing use of PCI in patients with acute myocardial infarction allows for immediate revascularization, identifies other coronary lesions, and may eliminate the need for further in-hospital risk stratification which would also be expected to decrease length of stay.22
Study Strengths and Limitations
The strengths of this study include our population-based design that included all patients hospitalized for acute myocardial infarction from a well-characterized community. All cases of possible acute myocardial infarction were independently validated according to standardized criteria and we were also able to control for a number of potentially confounding factors. The limitations of this study were that we were unable to examine physician visits and home care services that may have increased as a result of shorter hospital stays. In addition, this cohort consists largely of white patients and thus may lack generalizability to other racial/ethnic groups. While our diagnostic criteria for acute myocardial infarction have remained unchanged during the years under study, it is possible that less severely ill patients may have been hospitalized during more recent study years. Similarly, changing patient demographic and clinical characteristics, other unmeasured variables, as well as the extent of information collected and recorded in hospital medical records may have changed during the years of this investigation which may have affected some of the results observed.
CONCLUSIONS
New classifications of patients at low risk for poor outcomes (e.g., uncomplicated acute myocardial infarction) may help identify patients who may benefit from early hospital discharge.23 The results of this population-based study show that shorter hospital stays are not associated with higher rates of rehospitalization or of post-discharge mortality. However, further studies are needed to identify the optimal length of hospital stay for patients who have experienced an acute myocardial infarction.
Acknowledgements
This research was made possible by the cooperation of participating hospitals in the Worcester metropolitan area and through funding provided by the National Institutes of Health (RO1 HL35434).
This research was funded by the National Institutes of Health (RO1 HL35434).
Footnotes
The authors have no conflicts of interest to report.
All authors had access to the data and a role in writing the manuscript.
References
- 1.Baker DW, Einstadter D, Husak SS, Cebul RD. Trends in Postdischarge Mortality and Readmissions: Has Length of Stay Declined Too Far? Arch Intern Med. 2004;164:538–544. doi: 10.1001/archinte.164.5.538. [DOI] [PubMed] [Google Scholar]
- 2.Berger AK, Duval S, Jacobs DR, Jr, et al. Relation of Length of Hospital Stay in Acute Myocardial Infarction to Postdischarge Mortality. Am J Cardiol. 2008;101:428–434. doi: 10.1016/j.amjcard.2007.09.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spencer FA, Lessard D, Gore JM, Yarzebski J, Goldberg RJ. Declining Length of Hospital Stay for Acute Myocardial Infarction and Postdischarge Outcomes: A Community-Wide Perspective. Arch Intern Med. 2004;164:733–740. doi: 10.1001/archinte.164.7.733. [DOI] [PubMed] [Google Scholar]
- 4.Botkin NF, Spencer FA, Goldberg RJ, Lessard D, Yarzebski J, Gore JM. Changing trends in the long-term prognosis of patients with acute myocardial infarction: A population-based perspective. Am Heart J. 2006;151:199–205. doi: 10.1016/j.ahj.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 5.Parikh NI, Gona P, Larson MG, et al. Long-Term Trends in Myocardial Infarction Incidence and Case Fatality in the National Heart, Lung, and Blood Institute's Framingham Heart Study. Circulation. 2009;119:1203–1210. doi: 10.1161/CIRCULATIONAHA.108.825364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Masoudi FA, Foody JM, Havranek EP, et al. Trends in Acute Myocardial Infarction in 4 US States Between 1992 and 2001: Clinical Characteristics, Quality of Care, and Outcomes. Circulation. 2006;114:2806–2814. doi: 10.1161/CIRCULATIONAHA.106.611707. [DOI] [PubMed] [Google Scholar]
- 7.Desideri A, Fioretti PM, Cortigiani L, et al. Cost of strategies after myocardial infarction (COSTAMI): A multicentre, international, randomized trial for cost-effective discharge after uncomplicated myocardial infarction. Eur Heart J. 2003;24:1630–1639. doi: 10.1016/s0195-668x(03)00308-7. [DOI] [PubMed] [Google Scholar]
- 8.Topol EJ, Burek K, O'Neill WW, et al. A randomized controlled trial of hospital discharge three days after myocardial infarction in the era of reperfusion. N Engl J Med. 1988;318:1083–8. doi: 10.1056/NEJM198804283181702. [DOI] [PubMed] [Google Scholar]
- 9.Newby LK, Eisenstein EL, Califf RM, et al. Cost Effectiveness of Early Discharge after Uncomplicated Acute Myocardial Infarction. N Engl J Med. 2000;342:749–755. doi: 10.1056/NEJM200003163421101. [DOI] [PubMed] [Google Scholar]
- 10.Mark DB, Sigmon K, Topol EJ, et al. Identification of acute myocardial infarction patients suitable for early hospital discharge after aggressive interventional therapy. Results from the Thrombolysis and Angioplasty in Acute Myocardial Infarction Registry. Circulation. 1991;83:1186–1193. doi: 10.1161/01.cir.83.4.1186. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in attack and survival rates of acute myocardial infarction (1975 through 1981). The Worcester Heart Attack Study. JAMA. 1986;255:2774–9. [PubMed] [Google Scholar]
- 12.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Incidence and case fatality rates of acute myocardial infarction (1975–1984): The Worcester Heart Attack Study. Am Heart J. 1988;115:761–767. doi: 10.1016/0002-8703(88)90876-9. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decades (1975 to 1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: a community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 14.Saczynski JS, Spencer FA, Gore JM, et al. Twenty-Year Trends in the Incidence of Stroke Complicating Acute Myocardial Infarction: Worcester Heart Attack Study. Arch Intern Med. 2008;168:2104–2110. doi: 10.1001/archinte.168.19.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saczynski J, McManus D, Zhou Z, et al. Trends in Atrial Fibrillation Complicating Acute Myocardial Infarction. Am J Cadiol. doi: 10.1016/j.amjcard.2009.03.011. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spencer FA, Meyer TE, Goldberg RJ, et al. Twenty year trends (1975–1995) in the incidence, in-hospital and long-term death rates associated with heart failure complicating acute myocardial infarction : A community-wide perspective. J Am Coll Cardiol. 1999;34:1378–1387. doi: 10.1016/s0735-1097(99)00390-3. [DOI] [PubMed] [Google Scholar]
- 17.Goldberg RJ, Spencer FA, Gore JM, Lessard D, Yarzebski J. Thirty-Year Trends (1975 to 2005) in the Magnitude of, Management of, and Hospital Death Rates Associated With Cardiogenic Shock in Patients With Acute Myocardial Infarction: A Population-Based Perspective. Circulation. 2009;119:1211–1219. doi: 10.1161/CIRCULATIONAHA.108.814947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Every NR, Spertus J, Fihn SD, Hlatky M, Martin JS, Weaver WD. Length of hospital stay after acute myocardial infarction in the Myocardial Infarction Triage and Intervention (MITI) Project registry. J Am Coll Cardiol. 1996;28:287–293. doi: 10.1016/0735-1097(96)00168-4. [DOI] [PubMed] [Google Scholar]
- 19.Sgura FA, Wright RS, Kopecky SL, Grill JP, Reeder GS. Length of stay in myocardial infarction. Cost Qual. 2001:12–20. 25. [PubMed] [Google Scholar]
- 20.Harrison ML, Graff LA, Roos NP, Brownell MD. Discharging patients earlier from Winnipeg hospitals: does it adversely affect quality of care? CMAJ. 1995;153:745–51. [PMC free article] [PubMed] [Google Scholar]
- 21.Goldberg RJ, Spencer FA, Yarzebski J, et al. A 25-year perspective into the changing landscape of patients hospitalized with acute myocardial infarction (the Worcester Heart Attack Study) Am J Cardiol. 2004;94:1373–1378. doi: 10.1016/j.amjcard.2004.07.142. [DOI] [PubMed] [Google Scholar]
- 22.Floyd KC, Yarzebski J, Spencer FA, et al. A 30-year perspective (1975–2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Newby K, CM R, Guerci A, et al. Early discharge in the thrombolytic era: An analysis of criteria for uncomplicated infarction from the global utilization of streptokinase and t-PA for occluded coronary arteries (GUSTO) trial. J Am Coll Cardiol. 1996;27:625–632. doi: 10.1016/0735-1097(95)00513-7. [DOI] [PubMed] [Google Scholar]