Abstract
Study Design
Randomized trial with concurrent observational cohort. 1171 patients were divided into subgroups by educational attainment: high school or less, some college, and college degree or above.
Objective
To assess the influence of education level on outcomes for treatment of lumbar disk herniation.
Summary of Background Data
Educational attainment has been demonstrated to have an inverse relationship with pain perception, co-morbidities, and mortality.
Methods
The Spine Patient Outcomes Research Trial enrolled surgical candidates (imaging-confirmed disk herniation with at least 6 weeks of persistent signs and symptoms of radiculopathy) from 13 multidisciplinary spine clinics in 11 US states. Treatments were standard open diskectomy vs. non-operative treatment. Outcomes were changes from baseline for SF-36 bodily pain (BP) and physical function (PF) scales and the modified Oswestry Disability Index (ODI) at 6 weeks, 3 months, 6 months, and yearly through 4 years.
Results
Substantial improvement was seen in all patient cohorts. Surgical outcomes did not differ by level of education. For non-operative outcomes, however, higher levels of education were associated with significantly greater overall improvement over 4 years in BP (p=0.007), PF (p=0.001) and ODI (p=0.003). At 4 years a “dose-response” type relationship was shown for BP (high school or less 25.5; some college 31; college graduate or above 36.3; p= 0.004); results were similar for PF and ODI. The success of non-operative treatment in the more educated cohort resulted in an attenuation of the relative benefit of surgery.
Conclusions
Patients with higher educational attainment demonstrated significantly greater improvement with non-operative treatment while educational attainment was not associated with surgical outcomes.
Keywords: Lumbar disk herniation, education, clinical trial, patient outcomes
Introduction
Socioeconomic status, as measured by educational attainment, occupation, and income, has repeatedly been demonstrated to have a profound influence on health. Lower levels of socioeconomic status are associated with higher rates of multiple health maladies including cardiovascular disease,1, 2 cancer,1 obesity,3 disability,4 injury,5–7 and overall mortality.1, 8–10 It has been noted that the health disparities attributed to socioeconomic status are so large that eliminating their underlying causes could rival all current medical interventions as a way to control disease.9, 11 Educational attainment is an especially powerful measure of socioeconomic status because of its potential for intervention outside the healthcare system, in addition to its added social and political ramifications.12 Education is also a stable variable, is not dependent on recall, and serves as a powerful surrogate for many social and economic variables.13 Further, lower levels of educational attainment have been associated with higher levels of smoking, other health compromising behaviors, and lower levels of treatment adherence.10 For this reason, educational attainment could logically be expected to influence patients’ response to treatment.
Rates of self-reported pain have also been demonstrated to be associated with educational attainment. Data from the Health and Retirement Study (HRS) found rates of older people troubled by pain ranged from 26% for those with a college education to 55% for those without a high school diploma.14 Differences continue to persist even after controlling for obvious reasons such as type of occupation and industry.14
In the Maine Lumbar Spine Study, 34% of patients who did not complete high school reported leg or back pain “almost always” or “always” compared with just 9% for college graduates, up to 10 years from enrollment.14 The most important predictive factor of long-term pain outcomes was education level.14 Other studies have demonstrated a host of variables including education can negatively impact outcomes.15
Based upon these findings, our objective was specifically to investigate the impact of educational attainment on patient outcomes of The Spine Patient Outcomes Research Trial (SPORT). SPORT is a large multi-center, randomized controlled trial with a concurrent observational cohort, which was designed to assess the relative efficacy and cost-effectiveness of surgical and non-surgical treatment modalities for conditions of the lower back, including, spinal stenosis, degenerative spondylolisthesis, and lumbar disk herniation.16 Although several articles have been published regarding the outcomes of this study,16–19 it remains unclear how these outcomes were influenced by socioeconomic factors, specifically educational attainment. We specifically investigated how educational attainment was correlated with response to surgical and non-surgical treatment modalities within the SPORT design.
Methods
SPORT Study Design
Details regarding the SPORT study design and its respective patient population were described previously.16, 20 SPORT enrolled patients with intervertebral disc herniation between March 2000 and November 2004 from 13 multidisciplinary spine clinics in 11 US states. Eligible participants were surgical candidates (mean age, 42 years; 42% women) with imaging-confirmed disk herniation with persistent signs and symptoms of radiculopathy for at least 6 weeks. A total of 1171 participants had available data on educational attainment and at least one follow-up and were included in the current analysis.
Study Interventions
Study interventions, including operative and non-operative treatments were described previously.16, 21 Surgery included a standard open diskectomy with examination of the involved nerve root. The non-operative treatment group received “usual care,” with the minimum nonsurgical treatment to include at least active physical therapy, education/counseling with home exercise instruction, and nonsteroidal anti-inflammatory drugs, if tolerated.
Study Measures
SPORT’s primary measures were the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) bodily pain (BP) and physical function (PF) scales22 and the American Academy of Orthopaedic Surgeons MODEMS version of the Oswestry Disability Index (ODI).23 Higher scores are better in the BP and PF scales, therefore positive change scores are indicative of improvement. Lower scores are better on the ODI, therefore making negative changes indicative of improvement.
SPORT’s secondary measures included patient employment status24 and symptom severity. Symptom severity was measured by the Low Back Pain Bothersomeness (range, 0–6; higher scores represent worse symptoms) and the Sciatica Bothersomeness Index (range, 0–24; higher scores represent worse symptoms).25, 26 Lower scores are better on the bothersomeness scales, therefore negative change scores are indicative of improvement.
We stratified our study sample into three cohorts: 1) high school diploma or less; 2) some college; and 3) college graduates or greater. We conducted our analysis using data from the lumbar intervertebral disk herniation group within SPORT because this is a relatively young age group. Educational attainment is known to be an influential and stable measure of socioeconomic status (SES) within this age group.8
Statistical Analysis
Primary analyses for SPORT compared surgical and non-operative treatments using changes from baseline at each follow-up, with a mixed effects longitudinal regression model including a random individual effect to account for correlation between repeated measurements within individuals. We use this analytic technique to correct for multiple measures because repeated measures across time and within individuals have less variability than measures between individuals. Because of the crossover, analyses were based on treatments actually received in the combined randomized and observational cohorts. The treatment effect was defined as the difference between the mean surgical and non-operative changes from baseline. In these as-treated analyses, the treatment indicator was a time-varying covariate, allowing for variable times of surgery. In the surgical cohort, time is measured from the time of surgery to post-surgical outcomes. In the non-operative cohort, time was measured from time of enrollment. Patients’ experiences prior to surgery were attributed to the non-operative treatment arm. Predetermined end points for the study included results at 6 weeks, 3 months, 6 months, 1 year, 2 years, 3 years, and 4 years. Statistical analysis accounting for missing data and assessment for correlations has been reported previously.16 To adjust for confounding and the possible effect of missing data on the study results, we used a longitudinal mixed model with random effects controlling for covariates associated with missed visits and treatment received; for this paper, we added educational attainment as a covariate.27 We specifically test the statistical interaction between treatment (surgical vs. non-operative) and education level. The interaction term was also included in the model. Because or analytic method accounts for multiple measures over time and no other subgroups analyses were performed, we used P < 0.05 (2-sided) as our threshold for statistical significance with no adjustments made for multiple comparisons.
This was a post-hoc analysis of collected data. The outcomes were stratified by educational attainment and comparisons in outcomes between these sub-groups were made at each time-point with multiple degrees of freedom Wald tests; across the four-year follow-up overall comparisons of area-under-the-curve were made by using a Wald test.
Computations were done using SAS procedures PROC MIXED for continuous data with normal random effects and PROC GENMOD for binary and non-normal secondary outcomes in SAS software, version 9.1 (SAS Institute).
Results
Patient Characteristics
The baseline demographics of patients within the three levels of educational attainment as shown in Table 1 demonstrated no significant differences in age (p=0.10), gender (p=0.41), ethnicity (p=0.84) or race (p=0.45). Physical exam and radiographic findings were also similar across all 3 groups. However, there were several significant differences among the three groups. The lowest education cohort was more likely to have a household income less than $50,000 (p<0.001), less likely to be working full time; p<0.001), more likely to consider the ability to lift heavy objects “very important”(p<0.001) and more likely to receive worker’s compensation (p<0.001). Further, the lowest education groups had correspondingly lower baseline SF-36 scores in bodily pain (p<0.001) and physical functioning (p<0.001) but higher mental component summary (p<0.001), higher self-reported disability as measured by the ODI (p<0.001), higher Sciatica Bothersomeness Index, and higher Low Back Pain Bothersomeness scores (both with p<0.001). Thus, the lower education groups had greater self-reported physical dysfunction from their spine condition but better psychological function than more highly educated patients. The lower education group were also more likely to be very dissatisfied with symptoms (p=0.004) and have worse self-assessment of their health trend in the past year (p=0.002). Patients with lower levels of educational had significantly higher body mass index (BMI) were more likely to smoke (p<0.001), to prefer surgery (p=0.018) and to have received surgery (p=0.016) when compared to patients with higher educational. No significant differences in number of co-morbidities (p=0.31) were noted for the various educational levels.
Table 1.
Patient Baseline Demographic Characteristics, Comorbid Conditions, Clinical Findings, and Health Status Measures.
| Characteristics | High School or Less (n=287) | Some College (n=321) | College grad or above (n=563) | p-value |
|---|---|---|---|---|
| Age years, mean (SD) | 42.9 (11.4) | 40.9 (11.8) | 41.5 (11) | 0.10 |
| Female sex - no. (%) | 126 (44%) | 146 (45%) | 231 (41%) | 0.41 |
| Ethnicity: Non Hispanic | 273 (95%) | 306 (95%) | 540 (96%) | 0.84 |
| Race - White† | 244 (85%) | 279 (87%) | 496 (88%) | 0.45 |
| Income - Under $50,000 - no. (%) | 165 (57%) | 173 (54%) | 190 (34%) | <0.001 |
| Married - no. (%) | 220 (77%) | 215 (67%) | 394 (70%) | 0.027 |
| Employment status - no. (%) | <0.001 | |||
| Full or part time | 126 (44%) | 184 (57%) | 402 (71%) | |
| Disabled | 69 (24%) | 46 (14%) | 39 (7%) | |
| Other | 92 (32%) | 91 (28%) | 122 (22%) | |
| Work Lift | <0.001 | |||
| Very important | 154 (54%) | 102 (32%) | 99 (18%) | |
| Somewhat important | 75 (26%) | 101 (31%) | 153 (27%) | |
| Not very important | 58 (20%) | 118 (37%) | 311 (55%) | |
| Compensation - no. (%)‡ | 81 (28%) | 62 (19%) | 62 (11%) | <0.001 |
| Body-mass index (SD)§ | 29 (6) | 28.6 (5.6) | 27 (5.1) | <0.001 |
| Current smoker - no. (%) | 96 (33%) | 99 (31%) | 82 (15%) | <0.001 |
| Coexisting conditions - no. (%) | ||||
| Depression | 35 (12%) | 41 (13%) | 65 (12%) | 0.86 |
| Joint Problem | 54 (19%) | 60 (19%) | 103 (18%) | 0.98 |
| Other¶ | 132 (46%) | 157 (49%) | 228 (40%) | 0.041 |
| Total Number of Comorbidities - no. (%) | 0.31 | |||
| None or one | 197 (69%) | 222 (69%) | 421 (75%) | |
| Two or three | 66 (23%) | 71 (22%) | 105 (19%) | |
| Four or more | 22 (8%) | 25 (8%) | 34 (6%) | |
| Symptom duration < 6 mo since recent episode - no. (%) | 215 (75%) | 250 (78%) | 449 (80%) | 0.27 |
| SF-36 scores, mean (SD)†† | ||||
| Bodily Pain | 21.6 (17.4) | 25 (18.3) | 31.1 (21.5) | <0.001 |
| Physical Functioning | 31.6 (24.2) | 34.7 (24.5) | 42.2 (26) | <0.001 |
| Mental Component Summary | 43.6 (12.4) | 43.8 (11.5) | 46.8 (11) | <0.001 |
| Oswestry Disability Index (SD)‡‡ | 54.1 (20.8) | 51 (20) | 46.4 (21.9) | <0.001 |
| Sciatica Bothersomeness Index (SD)§§ | 16.5 (5.1) | 15.9 (5) | 15 (5.4) | <0.001 |
| Low Back Pain Bothersomeness (SD)¶¶ | 4.3 (1.8) | 3.9 (1.9) | 3.7 (1.8) | <0.001 |
| Very dissatisfied with symptoms - no. (%) | 243 (85%) | 260 (81%) | 436 (77%) | 0.04 |
| Self-assessment of health trend - no. (%) | 0.002 | |||
| Problem getting better | 31 (11%) | 42 (13%) | 104 (18%) | |
| Problem staying about the same | 120 (42%) | 148 (46%) | 259 (46%) | |
| Problem getting worse | 135 (47%) | 128 (40%) | 197 (35%) | |
| Treatment preference at baseline - no. (%) | 0.018 | |||
| Prefer nonsurgical treatment | 81 (28%) | 101 (31%) | 204 (36%) | |
| Not sure | 42 (15%) | 66 (21%) | 85 (15%) | |
| Prefer surgery | 164 (57%) | 154 (48%) | 272 (48%) | |
| Dermatomal pain radiation - no. (%) | 284 (99%) | 309 (96%) | 549 (98%) | 0.10 |
| Pain with straight-leg raise - no. (%) | ||||
| Ipsilateral | 182 (63%) | 207 (64%) | 349 (62%) | 0.75 |
| Contralateral/both | 48 (17%) | 48 (15%) | 88 (16%) | 0.83 |
| Any neurological deficit - no. (%) | 222 (77%) | 242 (75%) | 425 (75%) | 0.81 |
| Asymmetric reflex depressed | 111 (39%) | 130 (40%) | 231 (41%) | 0.80 |
| Asymmetric sensory decrease | 158 (55%) | 157 (49%) | 282 (50%) | 0.27 |
| Asymmetric motor weakness | 113 (39%) | 140 (44%) | 239 (42%) | 0.55 |
| Herniation Level - no. (%)* | 0.47 | |||
| L2–L3/L3–L4 | 25 (9%) | 19 (6%) | 41 (7%) | |
| L4–L5 | 109 (38%) | 115 (36%) | 223 (40%) | |
| L5-S1 | 152 (53%) | 187 (58%) | 299 (53%) | |
| Herniation Type - no. (%) | 0.56 | |||
| Protruding | 78 (27%) | 88 (27%) | 152 (27%) | |
| Extruded | 182 (63%) | 208 (65%) | 377 (67%) | |
| Sequestered | 26 (9%) | 25 (8%) | 34 (6%) | |
| Posterolateral herniation - no. (%) | 219 (76%) | 250 (78%) | 438 (78%) | 0.87 |
| Received surgery - no. (%) | 203 (71%) | 222 (69%) | 349 (62%) | 0.016 |
Race or ethnic group was self-assessed. Whites and blacks could be either Hispanic or non-Hispanic.
This category includes patients who were receiving or had applications pending for workers compensation, Social Security compensation, or other compensation.
The body-mass index is the weight in kilograms divided by the square of the height in meters.
Other indicates problems related to stroke, diabetes, osteoporosis, cancer, fibromyalgia, CFS, PTSD, alcohol, drug dependence, heart, lung, liver, kidney, blood vessel, nervous system, hypertension, migraine, anxiety, stomach or bowel.
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms.
The Sciatica Bothersomeness index range from 0 to 24, with lower scores indicating less severe symptoms.
The Low Back Pain Bothersomness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms
The diagnosis for approximately 97% of patients were evaluated with magnetic resonance imaging and 3% with computed tomography.
Outcome Measures
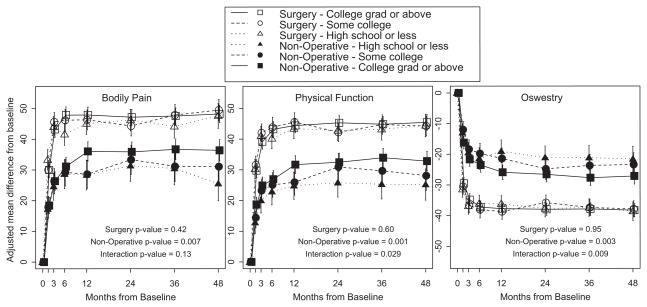
Figure 1 demonstrates the primary outcomes for bodily pain, physical function, and Oswestry disability index among the operative and non-operative treatment groups over the 4 year follow-up period. Outcomes from surgery were better than non-operative treatment groups across all times periods regardless of educational attainment. There were no differences in surgical outcomes among the various educational cohorts with regard to bodily pain, physical function, or disability at any point in time out to 4 years. The results for non-operative care, however, did differ significantly by education level in which the higher the educational attainment, the better the outcome from non-operative treatment (p=0.007 for Bodily Pain, p=0.001 for Physical Function, p=0.003 for Oswestry Disability Index).
Figure 1.
Primary outcomes over time for ‘High school or less’, ‘Some college’ and ‘College grad or above’.
- The surgery p-value compares ‘High school or less,’ ‘Some college’ and ‘College grad or above’ among Surgery patients.
- The non-operative p-value compares ‘High school or less,’ ‘Some college’ and ‘College grad or above’ among Non-operative patients.
- The interaction p-value compares treatment effect (surgery vs. non-operative) among ‘High school or less,’ ‘Some college’ and ‘College grad or above’
* P-values are time-weighted averages at 4 years (area under the curve p-values)
Table 2 shows the details of the individual time points in our model. The p-values reported under the treatment effect column include the interaction term for treatment by education level after statistical adjustment for all other covariates. At one year, for the non-operative treatment groups, patients with higher education demonstrated a better outcome for bodily pain (p=0.005), physical function (p=0.011), and improvement in disability as measured by ODI (p=0.004). These differences of educational attainment among the non-operative treatment group persisted out to 4 year’s with bodily pain (p= 0.004) and physical function (p=0.027). Differences in ODI at 4 years were not significant (p=0.053). The treatment effect of surgery (outcome in surgery group minus the outcome on non-operative group) was in large part attenuated by higher levels of education.
Table 2.
Change Scores and Treatment Effects by Education for Primary Outcomes in the Randomized and Observational Cohorts Combined, According to Treatment Received.*
| Outcome |
Education | 1-Year |
2-Year |
3-Year |
4-Year |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Surgical | Non-operative | Treatment Effect† (95% CI) | Surgical | Non-operative | Treatment Effect† (95% CI) | Surgical | Non-operative | Treatment Effect† (95% CI) | Surgical | Non-operative | Treatment Effect† (95% CI) | ||
| SF-36 Bodily Pain (BP) (0–100) (SE)†† |
High school or less | 45.1 (1.8) | 28.3 (2.5) | 16.8 (11.1, 22.4) | 46.2 (1.8) | 31.3 (2.6) | 14.9 (9, 20.8) | 44.1 (1.9) | 30.4 (2.7) | 13.7 (7.5, 19.9) | 47.5 (2) | 25.5 (2.8) | 22 (15.4, 28.7) |
| Some college | 46.3 (1.7) | 28.6 (2.3) | 17.7 (12.4, 23.1) | 44.3 (1.7) | 33.3 (2.4) | 11 (5.5, 16.5) | 47.9 (1.7) | 31.1 (2.5) | 16.8 (11, 22.5) | 49.4 (1.8) | 31 (2.6) | 18.4 (12.4, 24.5) | |
| College grad or above | 47.9 (1.3) | 36 (1.6) | 11.9 (8, 15.7) | 47.2 (1.3) | 35.9 (1.6) | 11.3 (7.3, 15.2) | 47.6 (1.3) | 36.7 (1.7) | 10.8 (6.7, 15) | 48.2 (1.4) | 36.3 (1.8) | 11.9 (7.6, 16.2) | |
| pvalue | 0.43 | 0.005 | 0.13 | 0.40 | 0.30 | 0.54 | 0.27 | 0.056 | 0.23 | 0.76 | 0.004 | 0.02 | |
| SF-36 Physical Function (PF) (0–100) (SE)†† |
High school or less | 43.4 (1.7) | 24.8 (2.3) | 18.6 (13.5, 23.7) | 42.7 (1.7) | 25.7 (2.4) | 17 (11.7, 22.3) | 43.1 (1.8) | 25.2 (2.4) | 17.9 (12.3, 23.4) | 44.4 (1.9) | 25.2 (2.6) | 19.2 (13.3, 25.2) |
| Some college | 45.5 (1.5) | 25.9 (2.1) | 19.7 (14.8, 24.5) | 42.2 (1.5) | 30.9 (2.2) | 11.3 (6.3, 16.3) | 44.7 (1.6) | 29.6 (2.3) | 15.1 (9.9, 20.3) | 44.2 (1.6) | 28 (2.4) | 16.2 (10.8, 21.7) | |
| College grad or above | 44.4 (1.2) | 31.7 (1.5) | 12.7 (9.2, 16.3) | 45.3 (1.2) | 32.4 (1.5) | 12.8 (9.3, 16.4) | 44.8 (1.2) | 33.9 (1.6) | 10.9 (7.2, 14.6) | 45.4 (1.3) | 32.8 (1.6) | 12.6 (8.8, 16.5) | |
| pvalue | 0.62 | 0.011 | 0.032 | 0.23 | 0.055 | 0.26 | 0.72 | 0.009 | 0.089 | 0.82 | 0.027 | 0.15 | |
| Oswestry Disability Index (ODI) (0–100) (SE) ‡‡ | High school or less | −36.2 (1.4) | −19 (1.9) | −17.1 (−21.3, −12.9) | −37.7 (1.4) | −21.1 (1.9) | −16.6 (−20.9, −12.3) | −37.4 (1.5) | −21.1 (2) | −16.2 (−20.8, −11.7) | −38.6 (1.5) | −21.6 (2.1) | −17 (−21.9, −12.2) |
| Some college | −38.7 (1.3) | −21.4 (1.7) | −17.3 (−21.2, −13.3) | −35.8 (1.3) | −24.8 (1.8) | −11 (−15.1, −7) | −37.4 (1.3) | −23.7 (1.8) | −13.7 (−17.9, −9.5) | −37.9 (1.4) | −23.4 (2) | −14.5 (−18.9, −10.1) | |
| College grad or above | −37.7 (1) | −25.9 (1.2) | −11.8 (−14.7, −9) | −37.9 (1) | −26.6 (1.2) | −11.4 (−14.3, −8.5) | −37.9 (1) | −27.7 (1.3) | −10.2 (−13.2, −7.2) | −38.2 (1.1) | −27.1 (1.3) | −11.1 (−14.3, −8) | |
| pvalue | 0.39 | 0.004 | 0.027 | 0.39 | 0.061 | 0.088 | 0.95 | 0.015 | 0.067 | 0.93 | 0.053 | 0.10 | |
Adjusted for age, gender, body mass index, income, work lift, race, marital status, smoking status, working status, compensation, duration of most recent episode, herniation location, stomach comorbidity, depression, other** comorbidity, self-rated health trend, treatment preference, baseline score (for SF-36, ODI, and Sciatica Bothersomeness Index), and center.
Treatment effect is the difference between the surgical and non-operative mean change from baseline. Analysis is done using a mixed model with a random subject intercept term. Treatment is a time-varying covariate where a patients’ experience prior to surgery is attributed to the non-operative arm and time is measured from enrollment and his/her post-surgery outcomes are attributed to the surgical arm and time is measured from time of surgery.
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms.
Other comorbidities include: stroke, diabetes, osteoporosis, cancer, fibromyalgia, cfs, PTSD, alcohol, drug dependency, heart, lung, liver, kidney, blood vessel, nervous system, hypertension, migraine, anxiety, stomach, bowel.
No consistent significant differences were demonstrated across the education subgroups for the secondary outcome measures of sciatica bothersomeness, low back pain, or work status.
Discussion
Consistent with previous SPORT reports on intervertebral disk herniation, all treatment cohorts demonstrated improvement over the 4 year post treatment survellience.16, 28 The benefit of surgery on primary outcomes was significantly better for all postoperative time intervals, regardless of level of education compared to non-operative treatment. The most striking finding in the current study was that those patients treated non-operatively who had higher levels of education improved to a greater degree compared to those with lower levels of education. This resulted in an attenuation of the treatment effect for surgery in patients with higher levels of education, particularly in the college graduate and above category. In other words, the benefit of surgery relative to non-operative treatment was less pronounced among those with the highest levels of education on all primary outcomes compared to those with less education. This was evident with SF-36 Bodily Pain scores at 1 and 4 years, SF-36 Physical Function scores at 3 months and 1 year, and ODI scores at 3 months and 1 year. The reasons for these differences are not clear but they remained even after adjusting for several factors previously demonstrated to influence low back and leg symptoms, such as gender, occupation, obesity, smoking, and other comorbidities.14 As expected, patients in the lower education groups reported lower income and more physical demands which may have contributed to the differences in outcomes. Notably, however, we found persistent effects of education, even after controlling for income and work demand. Again, it is important to note that this was a post-hoc analysis of SPORT and therefore the findings inherent in this study need to be confirmed with further research.
In many studies, psychosocial and work environmental factors have been found to be far more accurate predictors of self-reported low back pain disability than physical factors. Specifically work environment, relationship to supervisors, elevated scores on the MMPI scales of hysteria, hypochondriasis, and depression, perception of compensability, and the duration of the current episode have all been demonstrated to be significant predictors.29, 30 In our current study, we attempted to control for many of these factors by adjusting for baseline SF-36 scores, depression, compensation status, duration of most recent episode, and self-rated health trends. In this study it was interesting to find that the lower education groups had greater self-reported physical dysfunction from their spine condition but better psychological function than more highly educated patients.
It has been demonstrated that the actual number of existing co-morbidities at the time of surgery is related to outcomes following spine surgery.15 We were, however, unable to find differences in number of co-morbidities between the various education groups which could account for differences in outcomes.
Several other factors that we could not fully analyze with our research design might explain this relationship. In previous studies, those in lower socioeconomic classes are less likely to have health insurance,31 access to health care,32, 33 and have lower quality of care33 than those in higher socioeconomic classes. Lower levels of education can be associated with higher illiteracy rates, resulting in barriers to medical care ranging from seeking less care to having difficulties navigating the complexities of our fragmented medical system34 or understanding alternative options for care. However, in the current study, those with lower educational attainment were more likely to receive surgery for their herniated disc, which suggests that insurance and access to care was not a major problem. However, it is possible they were less able to distinguish between the benefits of surgical and non-surgical treatment options, though video decision aids were used in this trial in lieu of written pamphlets partly in order to limit any such effect in this study.35, 36
One explanation to help explain these differences may have to do with locus of control. Originally described by Dr. Julian Rotter in 1954,37 this theory proposes control of one’s life and choices can be primarily modified either internally or externally. Those with higher levels of education have a greater locus of internal control,38 which is associated with higher levels of self-rated health,39 as well as better health behaviors and health outcomes.40 Surgical treatment shifts the control to an external locus whereas non-operative treatment requires a patient to exercise greater internal locus of control. This theory could explain the differences between the groups but must be tested for verification.
Our study is not without limitations. It is a secondary subgroup analysis based upon established literature regarding socioeconomic status, educational attainment, and health outcomes, and our own clinical observations. Our hypothesis was that lower educational attainment would be associated with worse outcomes for both surgical and non-surgical groups. This hypothesis was not specified prior to the SPORT. However, measurement of educational attainment was completed prior to randomization or treatment allocation and it was the only subgroup strata assessed for this project. Kemper et al. suggest evidence of subgroup differences, like this, from secondary analyses should be considered preliminary and validation in future work is still required. 41
Concern could arise regarding the performance of multiple statistical comparisons in our analysis. Yet, we performed just three multivariable analyses, one each for Bodily Pain score, Physical Function score and Oswestry Disability Index. For each outcome we used a mixed effects longitudinal regression model including a random individual effect to account for correlation between repeated measurements within individuals. We do not further adjust for multiple comparisons. The danger with not accounting for multiple comparisons is that we could see significance where none exists. This is a post-hoc secondary analysis, therefore we do not put too much emphasis on any one statistical comparison. Instead, we focus on the overall effect of educational attainment on surgical and non-operative spinal treatment.
Those patients with a high school education or less shared other characterstics that differed from patients with some college and those who completed college. Yet, the differences in outcomes for patients with lower educational attainment persisted even after adjusting for the baseline differences.
It is critical that clinicians take care to identify educational attainment status among their patients. As suggested by our study, this information can be useful for managing personal and patient expectations. Clinicians should also be aware and prepared for the needs of patients in lower socioeconomic positions for greater pain management, assistance, and support regarding their functional limitations and disability. More importantly, the choice of surgery versus continued non-operative treatment is elective and preference-based for the majority of patients with lumbar disc herniations. Therefore, designing educational programs to aid patients in making an informed choice must take into account differences in educational level. On a social policy level, our study is yet further evidence in support of the profound influence of education on health outcomes.
Acknowledgments
Funding
The authors would like to acknowledge funding from the following sources:
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444) and the Office of Research on Women’s Health, the National Institutes of Health, and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention. The Multidisciplinary Clinical Research Center in Musculoskeletal Diseases is funded by NIAMS (P60-AR048094).
The funding sources had no role in design or conduct of the study; the collection, management, analysis, or interpretation of the data; or the preparation, review, or approval of the manuscript.
Footnotes
Trial Registration: clinicaltrials.gov Identifier: NCT00000410
Summary of Conflicts Disclosure
Dr. Lurie reports receiving consulting fees from Pacific Business Group on Health, the Foundation for Informed Medical Decision-Making, and Regeneron Pharmaceuticals; and salary support from the NIH.; Dr. Weinstein reports receiving salary, staff and materials support from the NIH.
Contributor Information
Patrick R. Olson, Email: patricku.olson@hitchcock.org, Department of Orthopaedics, Dartmouth-Hitchcock Medical Center.
Jon D. Lurie, Department of Medicine, Dartmouth-Hitchcock Medical Center, and The Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth College.
John Frymoyer, College of Medicine, University of Vermont.
Thomas Walsh, The Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth College.
Wenyan Zhao, The Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth College.
William A. Abdu, Dartmouth Medical School and Director, The Spine Center at Dartmouth-Hitchcock Medical Center.
James N. Weinstein, The Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth College; Chair, Department of Orthopaedics, Dartmouth-Hitchcock Medical Center; One Medical Center Dr., Lebanon, NH 30756.
References
- 1.Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med. 2002;347(20):1585–92. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- 2.Albert MA, Glynn RJ, Buring J, Ridker PM. Impact of traditional and novel risk factors on the relationship between socioeconomic status and incident cardiovascular events. Circulation. 2006;114(24):2619–26. doi: 10.1161/CIRCULATIONAHA.106.660043. [DOI] [PubMed] [Google Scholar]
- 3.Sulander TT, Uutela AK. Obesity and education: recent trends and disparities among 65- to 84-year-old men and women in Finland. Prev Med. 2007;45(2–3):153–6. doi: 10.1016/j.ypmed.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Isaacs SL, Schroeder SA. Class - the ignored determinant of the nation’s health. N Engl J Med. 2004;351(11):1137–42. doi: 10.1056/NEJMsb040329. [DOI] [PubMed] [Google Scholar]
- 5.Whitlock G, Norton R, Clark T, Pledger M, Jackson R, MacMahon S. Motor vehicle driver injury and socioeconomic status: a cohort study with prospective and retrospective driver injuries. J Epidemiol Community Health. 2003;57:512–16. doi: 10.1136/jech.57.7.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steenland K, Halperin W, Hu S, Walker J. Deaths due to injuries among employed adults: the effects of socioeconomic class. Epidemiology. 2003;14:74–79. doi: 10.1097/00001648-200301000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Cubbin C, Smith G. Socioeconomic inequalities in injury: critical issues in design and analysis. Annu Rev Public Health. 2002;23:349–75. doi: 10.1146/annurev.publhealth.23.100901.140548. [DOI] [PubMed] [Google Scholar]
- 8.Jemal A, Thun M, Ward E, Henley J, Cokkinides V, Murray T. Mortality from leading causes by education and race in the United States, 2001. American Journal of Preventive Medicine. 2008;34(1):1–8. doi: 10.1016/j.amepre.2007.09.017. [DOI] [PubMed] [Google Scholar]
- 9.Woolf S, Johnson R, Phillips R, Philipsen M. Giving everyone the health of the educated: an examination of whether social change would save more lives than medical advances. Journal of Public Health. 2007;97:679–83. doi: 10.2105/AJPH.2005.084848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laaksonen M, Talala K, Martelin T, Rahkonen O, Roos E, Helakorpi S, et al. Health behaviours as explanations for educational level differences in cardiovascular and all-cause mortality: a follow-up of 60 000 men and women over 23 years. Eur J Public Health. 2008;18(1):38–43. doi: 10.1093/eurpub/ckm051. [DOI] [PubMed] [Google Scholar]
- 11.Woolf S. Potential health and economic consequences of misplaced priorities. JAMA. 2007;297(5):523–26. doi: 10.1001/jama.297.5.523. [DOI] [PubMed] [Google Scholar]
- 12.Mechanic D. Population health: challenges for science and society. The Milbank Quarterly. 2007;85(3):533–59. doi: 10.1111/j.1468-0009.2007.00498.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dionne C, Von Korff M, Koepsell T, Deyo R, Barlow W, Checkoway H. Formal education and back pain: a review. J Epidemiol Community Health. 2001;55:455–68. doi: 10.1136/jech.55.7.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Atlas SJ, Skinner J. Education and the Prevalence of Pain. NBER Conference on Aging; 2007. [Google Scholar]
- 15.Slover J, Abdu WA, Hanscom B, Weinstein JN. The impact of comorbidities on the change in Short-Form 36 and Oswestry scores following lumbar spine surgery. Spine. 2006;31(17):1974–098. doi: 10.1097/01.brs.0000229252.30903.b9. [DOI] [PubMed] [Google Scholar]
- 16.Weinstein J, Tosteson T, Lurie J, Tosteson A, Hanscom B, Skinner J, Abdu W, Hilibrand A, Boden S, Deyo R. Surgical vs. nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296(20):2441–50. doi: 10.1001/jama.296.20.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weinstein JN, Lurie JD, Tosteson TD, Skinner JS, Hanscom B, Tosteson AN, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. Jama. 2006;296(20):2451–9. doi: 10.1001/jama.296.20.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weinstein J, Tosteson T, Lurie J, Tosteson A, Blood E, Hanscom B, Herkowitz H, Cammisa F, Albert T, Boden S, Hilibrand A, Goldberg H, Berven S, An H. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 2008;358(8):794–810. doi: 10.1056/NEJMoa0707136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weinstein J, Lurie J, Tosteson T, Hanscom B, Tosteson A, Blood E, Birkmeyer N, Hilibrand A, Herkowitz H, Cammisa F, Albert T, Emery S, Lenke L, Abdu W, Longley M, Errico T, Hu S. Surgical versus nonsurgical treatment for lumber degenerative spondylolisthesis. N Engl J Med. 2007;356(22):2257–70. doi: 10.1056/NEJMoa070302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Birkmeyer N, Weinstein J, Tosteson A, Tosteson T, Skinner J, Lurie J, Deyo R, Wennberg J. Design of the Spine Patient Outcomes Research Trial (SPORT) Spine. 2002;27(12):1361–72. doi: 10.1097/00007632-200206150-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cummins J, Lurie J, Tosteson T, Hanscom B, Abdu W, Birkmeyer N, Herkowitz H, Weinstein J. Descriptive epidemiology and prior healthcare utilization of patients in the Spine Patient Outcomes Research Trial’s (SPORT) three observational cohorts: disc herniation, spinal stenosis, and degenerative spondylolisthesis. Spine. 2006;37(1):806–14. doi: 10.1097/01.brs.0000207473.09030.0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32(1):40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Daltroy LH, Cats-Baril WL, Katz JN, Fossel AH, Liang MH. The North American spine society lumbar spine outcome assessment Instrument: reliability and validity tests. Spine. 1996;21(6):741–9. doi: 10.1097/00007632-199603150-00017. [DOI] [PubMed] [Google Scholar]
- 24.Deyo RA, Diehl AK. Patient satisfaction with medical care for low-back pain. Spine. 1986;11(1):28–30. doi: 10.1097/00007632-198601000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Atlas SJ, Deyo RA, Patrick DL, Convery K, Keller RB, Singer DE. The Quebec Task Force classification for Spinal Disorders and the severity, treatment, and outcomes of sciatica and lumbar spinal stenosis. Spine. 1996;21(24):2885–92. doi: 10.1097/00007632-199612150-00020. [DOI] [PubMed] [Google Scholar]
- 26.Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB. Assessing health-related quality of life in patients with sciatica. Spine. 1995;20(17):1899–908. doi: 10.1097/00007632-199509000-00011. discussion 909. [DOI] [PubMed] [Google Scholar]
- 27.Little R, Rubin D. Statistical Analysis with Missing Data. 2. Philadephia, PA: John Wiley & Sons; 2002. [Google Scholar]
- 28.Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the maine lumbar spine study. Spine. 2005;30(8):927–35. doi: 10.1097/01.brs.0000158954.68522.2a. [DOI] [PubMed] [Google Scholar]
- 29.Bigos SJ, Battie MC, Spengler DM, Fisher LD, Fordyce WE, Hansson T, et al. A longitudinal, prospective study of industrial back injury reporting. Clin Orthop Relat Res. 1992;(279):21–34. [PubMed] [Google Scholar]
- 30.Frymoyer JW. Predicting disability from low back pain. Clin Orthop Relat Res. 1992;(279):101–9. [PubMed] [Google Scholar]
- 31.Sudano JJ, Baker DW. Explaining US racial/ethnic disparities in health declines and mortality in late middle age: the roles of socioeconomic status, health behaviors, and health insurance. Soc Sci Med. 2006;62(4):909–22. doi: 10.1016/j.socscimed.2005.06.041. [DOI] [PubMed] [Google Scholar]
- 32.Heck KE, Parker JD. Family structure, socioeconomic status, and access to health care for children. Health Serv Res. 2002;37(1):173–86. [PubMed] [Google Scholar]
- 33.Key Themes and Highlights from the National Healthcare Disparities Report. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ); 2007. [Google Scholar]
- 34.Marcus EN. The silent epidemic--the health effects of illiteracy. N Engl J Med. 2006;355(4):339–41. doi: 10.1056/NEJMp058328. [DOI] [PubMed] [Google Scholar]
- 35.Phelan EA, Deyo RA, Cherkin DC, Weinstein JN, Ciol MA, Kreuter W, et al. Helping patients decide about back surgery: a randomized trial of an interactive video program. Spine. 2001;26(2):206–11. doi: 10.1097/00007632-200101150-00016. discussion 12. [DOI] [PubMed] [Google Scholar]
- 36.Deyo RA, Cherkin DC, Weinstein J, Howe J, Ciol M, Mulley AG., Jr Involving patients in clinical decisions: impact of an interactive video program on use of back surgery. Med Care. 2000;38(9):959–69. doi: 10.1097/00005650-200009000-00009. [DOI] [PubMed] [Google Scholar]
- 37.Rotter JB. Social learning and clinical psychology. New York: Prentice-Hall; 1954. [Google Scholar]
- 38.Flouri E. Parental interest in children’s education, children’s self-esteem and locus of control, and later educational attainment: twenty-six year follow-up of the 1970 British Birth Cohort. Br J Educ Psychol. 2006;76(Pt 1):41–55. doi: 10.1348/000709905X52508. [DOI] [PubMed] [Google Scholar]
- 39.Poortinga W, Dunstan FD, Fone DL. Health locus of control beliefs and socioeconomic differences in self-rated health. Prev Med. 2008;46(4):374–80. doi: 10.1016/j.ypmed.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 40.Gale CR, Batty GD, Deary IJ. Locus of control at age 10 years and health outcomes and behaviors at age 30 years: the 1970 British Cohort Study. Psychosom Med. 2008;70(4):397–403. doi: 10.1097/PSY.0b013e31816a719e. [DOI] [PubMed] [Google Scholar]
- 41.Kamper SJ, Maher CG, Hancock MJ, Koes BW, Croft PR, Hay E. Treatment-based subgroups of low back pain: a guide to appraisal of research studies and a summary of current evidence. Best Pract Res Clin Rheumatol. 2010;24(2):181–91. doi: 10.1016/j.berh.2009.11.003. [DOI] [PubMed] [Google Scholar]