Abstract
Objective To conduct a meta-analytic review of psychosocial adjustment of youth with inflammatory bowel disease (IBD). Methods Nineteen studies with a total of 1167 youth with IBD (M age = 14.33, 50% female) were included. Effect size (ES) estimates were calculated for anxiety symptoms & disorders, depressive symptoms & disorders, internalizing symptoms & disorders, externalizing symptoms, quality of life (QOL), social functioning, and self-esteem. Separate ESs were calculated for comparisons between IBD and youth with chronic illnesses versus healthy youth. Results Youth with IBD had higher rates of depressive disorders and internalizing disorders than youth with other chronic conditions. Youth with IBD had higher parent-reported internalizing symptoms, lower parent- and youth-reported QOL, and lower youth-reported social functioning compared to healthy youth. Conclusions Clinical attention to depressive disorders, QOL, and social functioning may be particularly salient in the context of pediatric IBD.
Keywords: inflammatory bowel disease, meta-analysis, psychosocial functioning, quality of life
Introduction
Inflammatory bowel disease (IBD) is a condition characterized by chronic inflammation of the gastrointestinal (GI) tract that affects approximately 71 of every 100,000 children (Kappelman, Rifas-Shiman, Kleinman, et al., 2007). It is generally divided into two subtypes, Crohn’s disease (CD) and ulcerative colitis (UC), which differ in anatomical location and the nature of the inflammation. For cases in which the presentation is not clearly classifiable as CD or UC, the designation of indeterminate colitis is used. Approximately 20–30% of individuals with IBD are diagnosed in childhood (Hanauer, 2006). IBD has a relapsing and remitting course, and the most common symptoms in children include frequent diarrhea, abdominal pain, and weight loss or growth delay. Associated symptoms can include fatigue, decreased appetite, fever, perianal disease, arthritis, and delayed puberty. IBD differs from functional GI disorders such as irritable bowel syndrome and recurrent abdominal pain in that the functional disorders are not associated with any known structural or biochemical abnormalities. There is no cure for IBD, so the focus of treatment is on controlling the inflammation that causes the symptoms. Corticosteroids are frequently used, and they often have negative side effects such as weight gain, acne, hair growth, irritability, depression, emotional lability, and sleep difficulty. Surgical intervention is another possible course of treatment. More than a third of people with childhood-onset IBD will require surgery within 20 years of diagnosis (Langholz, Munkholm, Krasilnikoff, & Binder, 1997).
IBD presents many potential challenges to psychosocial adjustment. It is an unpredictable and potentially embarrassing disease. Youth with IBD may be embarrassed about their symptoms and frequent visits to the bathroom. They may fear being the target of the “bathroom humor” that is popular among children. They may limit their social activities to those with a bathroom nearby, or they may unexpectedly cancel planned activities due to disease flares. Short stature and delayed puberty can also contribute to appearing and feeling different from peers.
The psychosocial adjustment of youth with IBD has been investigated in multiple studies and summarized in a few review articles, most recently by Mackner and Crandall (2007). As reported in that review, both specific symptoms of behavioral/emotional functioning and elevated rates of psychological disorders have been reported. Studies of specific symptoms have used measures that cover a range of symptoms such as the Child Behavior Checklist (CBCL; Achenbach & Rescola, 2001), as well as those that target narrower areas of functioning, primarily depression and anxiety symptoms. Among studies employing a broad measure such as the CBCL that also included a comparison group, all but one study reported that children with IBD had significantly more behavioral/emotional symptoms overall and/or more internalizing symptoms than healthy children. There were few differences between children with IBD and children with other chronic illnesses (Mackner & Crandall, 2007). When examining measures of specific symptom areas, significant differences in anxiety symptoms have not been found when children with IBD were compared to healthy children or another chronic illness group. Only one study reported that children with IBD had significantly more depression symptoms than healthy children. Furthermore, among all of the studies using the CBCL and measures of specific symptoms that provided normative scores, all of the mean scores were within the average range.
The rates of psychiatric disorders that have been reported range considerably, from 10% to 73% (Burke et al., 1989; Szajnberg, Krall, Davis, Treem, & Hyams, 1993), with studies using smaller samples and less reliable methodology reporting higher rates (Mackner & Crandall, 2007). Among the studies using samples larger than 20 participants and methodology such as interviewer reliability checks, rates of current depression diagnosis ranged from 10% to 25%. Lifetime prevalence of a depressive disorder was significantly higher in a sample of children with IBD than children with cystic fibrosis in one study (25% vs. 12%; Burke et al., 1989). This study also examined lifetime and current rates of anxiety disorders and found no significant differences between the IBD and cystic fibrosis groups. Thus, findings differ based on methodology. Studies using measures such as the CBCL have reported that children with IBD have significantly higher total scores and/or higher internalizing scores than healthy children, but studies using measures of specific symptoms areas such as depression symptoms have not typically found significant differences. However, studies of diagnoses such as depressive diagnoses suggest that they are higher in children with IBD than healthy children. Conclusions regarding the behavioral/emotional adjustment of youth with IBD remain unclear.
Research in the area of self-esteem has also been equivocal. Mackner and Crandall (2007) reported that two of three studies employing healthy comparison groups found that youth with IBD have significantly lower self-esteem, but studies comparing youth with IBD to normative data have reported mean scores in the average range. In the area of social functioning, results appear to be dependent on the rater: there are few differences between children with IBD and healthy children according to child report, but typically significant differences are reported when parents provide information (DeBoer, Martha Grootenhuis, Derkx & Last, 2005; Engstrom, 1992; Mackner & Crandall, 2005, 2006; Raymer, Weininger & Hamilton, 1984; Youssef, Murphy, Langseder & Rosh, 2006).
Only two studies in the area of social functioning have been included in reviews of the literature, and the results were conflicting. Research in the area of quality of life (QOL) in pediatric IBD has not been reviewed since 2004. Qualitative and descriptive studies were primarily reviewed then (Mackner, Sisson, & Crandall, 2004), and at least six additional studies have been published in this area since this review. Several of the newer studies compared the QOL of children with IBD to healthy children and reported significantly lower QOL in the children with IBD, although not all areas of QOL were consistently significantly lower (Cunningham, Drotar, Palermo, McGowan & Arendt, 2007; DeBoer et al., 2005; Loonen, Grootenhuis, Last, Koopman & Derkx, 2002).
To summarize, while IBD certainly has the potential to affect psychosocial functioning, the current state of the literature limits conclusions about the adjustment of youth with IBD. Conflicting results have been reported, and some areas of adjustment have not been summarized recently despite additional publications in these areas. The goal of this study is to review empirically research on the psychosocial adjustment of youth with IBD using meta-analytic techniques, with a focus on examining differences in the adjustment of youth with IBD in comparison to healthy youth as well as youth with other chronic medical conditions. We were particularly interested in documenting adjustment in specific psychosocial domains, including anxiety symptoms, depressive symptoms, internalizing symptoms, externalizing symptoms, QOL, social functioning, and self-esteem, as well as the presence of several psychiatric disorders. An improved understanding of the adjustment of youth with IBD in specific domains has the potential to identify precise, rather than global areas of psychosocial risk, thereby informing targeted intervention efforts.
Methods
Selection of Studies
Four methods were utilized to identify relevant studies. First, literature searches were conducted on Medline, Comprehensive Index to Nursing and Allied Health Literature (CINAHL), PsychInfo, and the Cochrane Database of Intervention Studies to identify psychological studies conducted with pediatric IBD populations from the earliest years available for these databases through June 2008. Published studies and dissertation abstracts were included in the search. Independent searches were conducted by two authors and included the following combinations of terms: inflammatory bowel disease/IBD/Crohn’s disease/ulcerative colitis; child/youth/adolescent/patient; functioning/adaptation/adjustment/distress/QOL/ depression/anxiety/coping. Second, manual searches were conducted for the last 10 years (1998–2008) in the Journal of Pediatric Psychology, Inflammatory Bowel Diseases, and Journal of Pediatric Gastroenterology and Nutrition, journals that often publish studies on psychological adjustment in pediatric IBD. Third, review chapters and articles regarding pediatric IBD and psychosocial adjustment were examined for possible relevant articles. Finally, citations included in identified publications were inspected for additional potential studies. A total of 173 studies published between 1949 and 2008 were identified by this process and were reviewed for potential inclusion in this meta-analysis.
Requirements for Inclusion
To be eligible for inclusion, each study needed to meet five criteria. First, the study must have included a sample of youth with IBD [CD, UC, indeterminate colitis (IC), or some combination of these three]. Biopsy confirmation of diagnosis within each study was not required given the need to include survey studies which may not have had such documentation available. Second, studies must have been limited to youth 18 years of age or younger. Studies that included participants whose ages exceeded this range were included only if separate analyses were reported for youth in the 0–18 age range. Third, the study must have included a quantitative measure of youth psychological functioning in one of the following domains: depressive symptoms or disorders, anxiety symptoms or disorders, QOL, behavioral functioning, social functioning, or self-esteem. Fourth, the study must have been published in English. Fifth, the study needed to include a comparison group (either youth with a chronic medical condition or a healthy comparison group), or if comparison group data were not available, it must have utilized a validated assessment tool for which published normative data exists.
Of the 173 studies identified, 146 were excluded for failure to meet the above criteria. Fifty-five studies were excluded because the participants did not fall within the specified age range (n = 54) or the age range of participants was not specified (n = 1). Three studies did not utilize a sample of IBD patients upon further review. Forty-eight studies were excluded because they did not include a quantifiable outcome (e.g., qualitative studies, literature reviews, commentaries; n = 46) or sufficient quantitative information to compute an ES (n = 2). Two meta-analyses which utilized some studies of youth with IBD but did not focus exclusively on IBD were also excluded since the data presented overlapped with data from the original sources. Twenty-two studies were excluded because of lack of focus on one of the above psychosocial functioning domains of interest. Fourteen studies were excluded because they did not utilize a comparison group or use measures for which normative data was available. Finally, two studies were excluded because they focused exclusively on a sample of depressed adolescents with IBD, and as such, the data from these studies was not representative of the population of youth with IBD.
Of the 27 studies meeting inclusion criteria, two were excluded because the author of the study was not able to provide necessary data for inclusion, and six were excluded because the data presented in the study overlapped with data presented in other publications that were included in ES computations. Thus, 19 studies were included in the current meta-analysis.
Analytic Plan
All analyses were conducted using MIX 1.7 Meta-analysis software. For studies that included between group designs or for which normative data allowed for a between groups comparison, Hedge’s g (Hedges, 1981) was computed as a measure of effect size (ES). Hedge’s g represents the difference between the two means divided by the pooled standard deviation, with an adjustment for small sample bias. Hedges' g is a standardized mean difference, and like Cohen’s d, one that is often used for continuous outcomes that are not on the same scale. Its values are similar to Cohen’s d, but are corrected for small sample bias. Guidelines for interpretation of the Hedges’ g magnitude of effect parallel those established for Cohn’s d (i.e., small = .20, medium = .50, large = .80). The 95% confidence intervals (CIs) associated with ESs were also calculated.
Meta-analyses can be conducted using either fixed effects or random effects assumptions. In fixed effects models, all studies are assumed to be estimating the same population parameter, while in random effects models, studies are assumed to be from a population of studies that share the same mean. Hedges and Vevea (1998) suggest that a fixed effects model allows for inferences only to studies highly like those included in the meta-analysis, while the random effects model allows for a broader universe of generalization. Since generalizability from this analysis was sought, a random effects model under inverse variance weighted method was utilized since the variation between studies was assumed to be approximately normal (i.e., each study was treated as a random effect). Many investigators consider the random effects approach to be a preferred choice over the fixed effects approach (Caldwell, Ades, & Higgins, 2005; DerSimonian & Laird, 1985; Fleiss & Gross, 1991).
For studies that presented frequency data, logged odds ratios (ORs) and 95% CIs were obtained by reconstructing the tables for the proportions in each group. Logged ORs were then transformed back to OR for ease of interpretation. The between group variance Tau  was computed as an estimate of heterogeneity in random effect analysis, and DerSimonian–Laird weighted method was applied in estimates. Note that if
was computed as an estimate of heterogeneity in random effect analysis, and DerSimonian–Laird weighted method was applied in estimates. Note that if  then there is no or very little statistical heterogeneity (Higgins, Thompson, Deeks, & Altman, 2002).
then there is no or very little statistical heterogeneity (Higgins, Thompson, Deeks, & Altman, 2002).
Funnel plots were utilized as a visual tool for investigating publication or other forms of bias (Sackett, 1979; Scargle, 2000). A funnel plot is a scatter plot of treatment effect against a measure of study size. It is used as a visual aid to detect bias or systematic heterogeneity. A symmetric inverted funnel shape arises from a “well-behaved” data set in which publication bias is unlikely. An asymmetric funnel indicates a relationship between treatment effect and study size. This suggests the possibility of either publication bias or a systematic difference between smaller and larger studies (“small study effects”). The name “funnel plot” is based on the precision in the estimation of the underlying treatment effect increasing as the sample size of component studies increases. Therefore, in the absence of bias, results from small studies will scatter widely at the bottom of the graph, with the spread narrowing among larger studies. Although a funnel plot is an informal method of assessment of publication bias, it is more appropriate for use than formal methods in the current analyses as formal methods are not reliable for small numbers of studies in each domain (Egger, Smith, Schneider, & Minder, 2007; Sterne & Egger, 2001).
To maintain independence of each study, only one ES was included for each study within each psychosocial domain (e.g., depression, anxiety, QOL, etc). If a study contained more than one ES relevant to an analysis, the following plan was utilized. If a total score for the measure was provided (e.g., overall QOL), this score was utilized instead of a domain or subscale score. If a total score was not available, the ES of the subscale or domain score which most closely represented the total score was included. In cases in which a total score was not available, two authors independently reviewed the available subscale scores and selected which subscale score most closely represented the construct of interest (e.g., overall QOL). The authors were in 100% agreement of which subscale score this should be and the ES associated with that subscale score was utilized in the analyses. This approach was chosen rather than utilizing a mean study ES because averaging ESs of different instruments creates a value that is no longer an ES and no longer retains the distribution properties of each of the contributing ESs. Thus interpretation of that mean ES is difficult. Additionally, for any longitudinal studies, only the ES from the baseline assessment was included. Finally, given literature to support discrepancies between parent and youth perspectives on youth psychosocial functioning (Youngstrom, Loeber, & Stouthamer-Loeber, 2000), separate analyses were conducted for parental and youth reports of a particular construct of interest (e.g., QOL). If there was no ES or only one ES for a given reporter in a given domain (e.g., no parent report of depressive symptom ES), then no ES was computed.
Results
Description of Studies and Study Participants
Participant Demographics
There were 1167 youth with IBD who participated across the 19 studies [M (SD) sample size = 61.42 (49.55)]. The majority of participants had CD (63%; n = 729), followed by UC (27%; n = 315), and IC (1% n = 13). Mean age of child participants (weighted by sample size) across the 13 studies providing demographic information was 14.33 years (based on n = 967). Fifty percent of participants were female (n = 481), based on data from the 13 studies providing this information. Sixteen of 19 studies were conducted in North America, while three were conducted in Europe (n = 1 Sweden, n = 2 Netherlands). All studies reporting ethnicity (n = 10) utilized samples of primarily American or European Caucasian youth (range = 63–100%). The range of African-American participants across studies was 0–37% (6–37% in studies conducted in North America). Four studies provided information about family composition, with data from these studies indicating the majority of participants came from intact families (range = 77–90%). Estimates of socioeconomic status or annual family income were reported in only 3 of 19 studies. Thirteen studies provided information on IBD duration of illness (n = 5), age at diagnosis (n = 1), or mean time since diagnosis (n = 8). Mean time since diagnosis across studies was 3.23 years.
Comparison Group Composition
Six studies (32%) utilized healthy comparison groups, with a total of 225 healthy youth included in these groups. An additional 10 studies utilized a measure with available normative data from a community population. Six studies (32%) utilized a chronic illness comparison group with those illness groups including three (n = 112 total participants) with cystic fibrosis, two (n = 40 total participants) with diabetes; two (n = 91 total participants) with functional GI disorders, and one each with chronic headaches (n = 20 total participants) and cancer (n = 38 total participants). An additional two studies utilized a measure with normative data available for a chronic illness group available.
Study Designs
The majority of studies (n = 17; 89%) were cross sectional in nature, with only two longitudinal designs. Most studies (n = 12; 63%) were conducted within the past 10 years, with nearly half of all studies (n = 9; 47%) having been conducted within the past 5 years. The majority of studies recruited participants via outpatient clinics only (n = 15; 79%). Other recruitment sites included inpatient and outpatient settings (n = 1; 5%), hospital setting unspecified (n = 1; 5%), or an IBD summer camp (n = 1; 5%). One study did not specify the site of participant recruitment. In the majority of cases, data were collected via in person research visits (n = 15; 79%). Other sites of data collection included via mail (n = 2; 11%) or a combination of in person and mail strategies (n = 2; 11%).
Study Measures
Only three of 19 studies utilized multiple methods (questionnaire and interview) to assess youth psychosocial functioning. The remaining 16 studies utilized questionnaire assessments only (n = 12), interview only (n = 2), or card sort (n = 1).
Psychosocial Adjustment
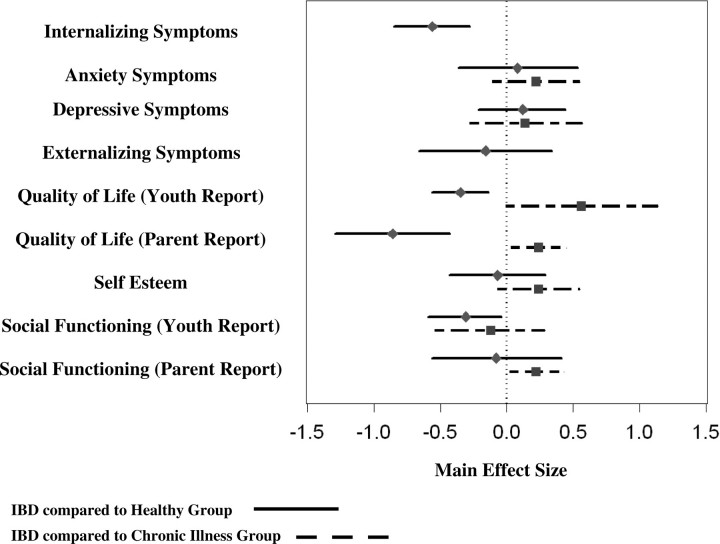
See Figure 1 for a plot of the mean ESs and 95% CIs for each psychosocial outcome domain.
Fig. 1.
Average effect sizes and 95% confidence intervals by domain for analyses comparing IBD to chronic illness group and IBD to healthy comparison group
Internalizing Symptoms
Three studies reported on internalizing symptoms via parent report on the Child Behavior Checklist (CBCL; Achenbach, 1991). One study included data from a chronic illness comparison group and three allowed for comparison with healthy youth (n = 2 with comparison group and n = 1 with normative data). Parent reported internalizing symptoms were significantly higher in youth with IBD in comparison to healthy youth (g = −.56, 95% CI = −0.85, −0.28, p < .0001). Given that only one study examined differences between youth with IBD and youth with a chronic illness, ES estimates were not computed.
Anxiety Symptoms
Three studies reported on anxiety symptoms, and all relied on youth report of anxiety. Two studies included data from a chronic illness comparison group and two allowed for comparison with healthy normative data. Measures of anxiety included the Revised Children’s Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, 1978), State Trait Anxiety Inventory for Children (Spielberger, 1973), and the Leyton Obsessional Inventory (Berg, Rapoport, & Flament, 1986). Symptom reports of anxiety were not different for youth with IBD compared to healthy youth (g = .17, 95% CI = −0.36, 0.53, p = .19) or to youth with other chronic medical conditions (g = .22, 95% CI = −0.11, 0.55, p = .18).
Depressive Symptoms
Seven studies reported on depressive symptoms, and all utilized youth report on the Children’s Depression Inventory (Kovacs, 1992). Three studies included data from a chronic illness comparison group and seven allowed for comparison with healthy youth (n = 3 with comparison group and n = 4 with normative data). Surprisingly, symptom reports of depression were found to be no different for youth with IBD in comparison to healthy youth (g = .12, 95% CI = −0.21, 0.44, p = .49) or youth with chronic medical conditions (g = .14, 95% CI = −0.28, 0.57, p = .51).
Externalizing Symptoms
Three studies reported on externalizing problems via parent report on the CBCL (Achenbach, 1991). One study included data from a chronic illness comparison group and three allowed for comparison with healthy youth (n = 2 with comparison group and n = 1 with normative data). Externalizing symptoms were not found to be significantly different between youth with IBD and healthy youth (g = −.16, 95% CI = −0.66, 0.34, p = .52). Because only one study examined differences between youth with IBD and youth with a chronic illness, ESs were not computed.
Overall QOL
Six studies reported on youth overall QOL, with 4 (67%) including both parent and youth reports and 2 (33%) including only youth report. Of the four studies including parent report on QOL, three allowed for comparison with chronically ill youth (n = 1 chronic illness comparison group and n = 2 chronic illness normative data) and four allowed for comparison with healthy youth (n = 2 with comparison group and n = 2 with normative data). Of the six studies utilizing youth report of QOL, three allowed for comparison with chronically ill youth (n = 1 chronic illness comparison group and n = 2 chronic illness normative data) and six allowed for comparison with healthy youth (n = 3 healthy comparison group, n = 3 normative data). Measures of QOL included the PedsQL total score (Varni, Seid, & Kurtin, 2001; n = 3), the Children’s Health Questionnaire general health perceptions scale (CHQ; Landergraf, Abetz, & Ware, 1996; n = 2), and The Dutch Children’s AZL/TNO Quality of Life Questionnaire (TACQOL; Vogels et al., 2000; n = 1) Total score.
Interestingly, parent proxy report of youth QOL was significantly lower among youth with IBD in comparison to healthy youth (g = −.86, 95% CI = −1.29, −0.43, p < .0001), but higher than youth with other chronic illnesses (g = .24, 95% CI = 0.03, 0.45, p = .03). Youth report of overall QOL indicated significantly lower QOL among youth with IBD in comparison to healthy youth (g = −.35, 95% CI = −0.56, −0.14, p = .001), a finding which parallels parent proxy report. Similar to findings of parent-reported youth QOL, youth-reported QOL was marginally higher among youth with IBD when compared to youth with other chronic illnesses (g = .56, 95% CI = −0.01, 1.14, p = .06).
Self-esteem
Youth self-esteem was examined in six studies. Five of six studies (83%) relied on youth report, while one study incorporated both parent and youth reports. Measures of self-esteem included the Jag Tycker Jag Ar (JTJA; Ouvinen-Birgerstam, 1985; n = 1), the Piers–Harris Children’s Self-Concept Scale (Piers, 1996; n = 3), the Coopersmith Self-esteem Inventory (Form A; Coopersmith, 1967; n = 1), and the self-esteem subscale of the CHQ (Landergraf et al., 1996; n = 1).
To avoid multiple ESs from the same study, only youth reports of self-esteem were included in ES computations. Of the six studies, three studies allowed for comparison with chronically ill comparison groups and six allowed for comparison with healthy youth (n = 4 with comparison group and n = 2 with normative data). Interestingly, self-esteem levels of youth with IBD did not significantly differ from those of healthy youth (g = −.07, 95% CI = −0.43, 0.29, p = .70) or youth with other chronic illnesses (g = .24, 95% CI = −0.07, 0.55, p < .13).
Social Functioning
Eight studies examined the social functioning of youth with IBD. Three studies (38%) utilized both parent and youth report, three studies (38%) relied exclusively on parent report, and two utilized youth report solely (25%). Of the six studies including parent report of youth social functioning, four studies allowed for comparison with chronically ill youth (n = 3 chronic illness comparison group and n = 1 chronic illness normative data) and six allowed for comparison with healthy youth (n = 3 with comparison group and n = 3 with normative data). Of the five studies including youth report of social functioning, three studies allowed for comparison with chronically ill youth (n = 2 chronic illness comparison group and n = 1 chronic illness normative data) and five allowed for comparison with healthy youth (n = 2 with comparison group and n = 3 with normative data). Measures of social functioning included the CBCL social competence score (Achenbach, 1991; n = 3), the TACQOL social functioning subscale (n = 2), the PedsQL social functioning subscale (Varni et al., 2001; n = 2) and the Personal Adjustment Inventory (Rogers, 1961; n = 1).
Surprisingly, based on parent report, youth with IBD did not differ in social functioning when compared to healthy youth (g = −.08, 95% CI = −0.56, 0.41. p = .76), and had better social functioning than youth with other chronic conditions (g = .22, 95% CI = 0.02, 0.43, p = .03). However, based on youth report of their own social functioning, youth with IBD had poorer social functioning in comparison to healthy youth (g = −.31, 95% CI = −0.59, −0.04, p = .03). Interestingly, no differences in social functioning were found between youth with IBD and youth with other chronic illnesses (g = −.12, 95% CI = −0.54, 0.29, p = .56) despite the GI symptoms associated with IBD.
Psychiatric Disorders
Anxiety Disorders
Only two studies reported on anxiety disorders. One study utilized the Schedule for Affective Disorders and Schizophrenia for School-Age Children (KSADS) interview directed at both parent and youth (Chambers et al., 1985) and one utilized the Child Assessment Schedule (CAS) interview directed at the child (Hodges, Kline, Fitch, McKnew, & Cytryn, 1981). Findings revealed no difference between youth with IBD and youth with other chronic conditions (OR = 1.90, 95% CI = 0.47, 7.69, p = .37). Only one study compared youth with IBD with healthy youth so this OR was not computed.
Depressive Disorders
Two studies examined rates of depressive disorders, with one utilizing the KSADS interview directed at both parent and youth (Chambers et al., 1985) and the other utilizing the CAS interview of the child (Hodges et al., 1981). Analyses revealed that the IBD group was at higher risk for depressive disorders than youth with other chronic illnesses (OR = 5.80, 95% CI = 1.60, 21.03, p = .007). Only one study compared youth with IBD with healthy youth so this OR was not computed.
Internalizing Disorders
Three studies examined rates of internalizing disorders (i.e., diagnoses of either anxiety or depressive disorders). One study utilized the KSADS (Chambers et al., 1985) interview of both youth and parents, one utilized the CAS youth interview (Hodges et al., 1981), and one used the Diagnostic Interview Schedule for Children (DISC-2.1) interview of both youth and parents (Shaffer, Fisher, Piacentini, Schwab-Stone, & Wicks, 1990). Findings suggested that the IBD group was at higher risk for internalizing disorders than youth with other chronic conditions (OR = 2.01, 95% CI = 1.11, 3.64, p = .02). Only one study compared youth with IBD with healthy youth so this OR was not computed.
Assessment of Study Heterogeneity
As measured by τ2 there is little heterogeneity. For means, there are 18 τ2 (n = 2 missing). The range of τ2s is 0 to 0.32 and the median is 0.065. For ORs, there are 3 τ2s ranging from 0 to 0.5 with a median of 0.
Assessment of Publication Bias
Examination of the funnel plots suggests the following. First, in comparisons between IBD and healthy samples, evidence of bias was documented in the following cases: internalizing symptoms, anxiety symptoms, depressive symptoms, parent and youth reports of total QOL, parent and youth reports of social functioning, and self-esteem. In comparisons between IBD and chronic illness samples, evidence of bias was documented in the following cases: youth report of total QOL and youth report of social functioning.
Discussion
The results of this meta-analytic review indicated that pediatric IBD patients demonstrate elevations in certain psychosocial domains compared to healthy controls and youth with other chronic illnesses. Specifically, youth with IBD were found to have elevated parent-reported internalizing symptoms compared to healthy children. Interestingly, measures of depressive and anxiety symptoms, which relied primarily on youth report of symptoms, did not reveal differences between youth with IBD and either healthy controls or children with other chronic illnesses. However, children with IBD were found to be at higher risk for depressive disorders compared to youth with other chronic illnesses. There are several possible explanations for these discrepant findings. First, assessments of depressive disorders were obtained from clinical interviews, whereas assessments of depressive symptoms relied on patient report. Patients may have under-reported symptoms or may have attributed certain depressive symptoms (e.g., fatigue, low appetite) to the disease process and not endorsed these as depressive symptoms, whereas clinical interviewers may have included such symptoms as characteristics of a depressive disorder. The discrepancy may also suggest that current measures of internalizing problems are too restricted with respect to the range of emotional issues that can underlie internalizing disorders such as hopelessness, dysthymic mood, feelings of helplessness, and negative disease related or unrelated causal attributions. These findings might also indicate that, although depressive symptoms are not elevated across the IBD population, those patients who develop symptoms of depression are more likely to experience clinically elevated symptoms and increased risk for a major depressive disorder. However, while this hypothesis seems plausible, it requires additional empirical attention since only two studies examined rates of depressive disorders using diagnostic assessments whereas others used symptom severity assessments.
The QOL of youth with IBD was also perceived to be lower by both patients and their parents compared to healthy controls. Compared to children with other chronic illnesses, QOL was either higher or marginally higher in children with IBD. Thus, while IBD patients may fair better than children with other chronic conditions with respect to overall well-being, they demonstrate significant impairment in this domain compared to their healthy peers.
With respect to social functioning, discordant parent and child ratings were observed across studies. Parents of IBD patients reported no differences in social functioning compared to healthy controls and better social functioning compared to children with other chronic illnesses; IBD patients reported poorer social functioning compared to healthy controls and no differences compared to children with other chronic illnesses. Thus, social functioning may represent a particularly poorly understood, yet salient, psychosocial outcome in IBD. On measures specifically assessing this construct, IBD patients appear to demonstrate levels of social functioning that is poorer than healthy children, but comparable to children with other chronic illnesses. The discordance between children with IBD and their parents on ratings of social functioning may represent an important miscommunication between these parents and children regarding the social challenges they face. It may also suggest that, given the personal nature of social functioning, IBD patients provide more proximal and meaningful evaluation of their social functioning than parents are able to with an inherently distal assessment. Our results also suggest that although youth with IBD are at risk for negative adjustment outcomes in the aforementioned domains, their self-esteem appears to be comparable to that of youth with other chronic conditions, as well as to that of healthy youth. Moreover, no differences in externalizing symptoms were documented in comparison to healthy youth.
There are certain limitations with meta-analytic techniques, including overestimation of the significance of results in the individual studies being analyzed and influence of systematic biases in those individual studies (Shapiro, 1994), and behavioral studies are certainly susceptible to biased reporting (Table I). However, the primary problems arising from the interpretation of meta-analyses in observational cross-sectional study data is the inference of causation. This is clearly not the interpretation of the current study. Indeed, the results of this study should be viewed as an analytic summary of the extant research on psychosocial functioning in pediatric IBD, and evidence that further research utilizing more controlled methodology to yield definitive findings is a high priority in this population. Another limitation of this study concerns the relatively small number of studies that met criteria for inclusion. Although this is the result of the stringent inclusion criteria applied to this meta-analysis, the findings are nevertheless based on a moderate number of studies, and caution is warranted in applying these findings to the broad pediatric IBD population. A small sample of studies overall also resulted in certain sets of analyses having a small number of independent ESs that were included in analyses of a given domain (e.g., three ESs comparing anxiety symptoms among youth with IBD to healthy youth). Although a small number of ESs in each domain limits power to detect significant differences between groups, the alternative option of combining heterogeneous outcomes under a broader domain of psychosocial functioning leads to difficulty in interpretation, thereby undermining the usefulness of the meta-analysis in advancing future research and clinical interventions. In our analytic approach, ESs that were statistically significant were typically of the medium to large magnitude (one exception to this is in the case of anxiety disorders in which an OR = 1.90 was not statistically significant). However, other findings that may have clinical importance failed to reach statistical significance given the small number of ESs included in a domain (e.g., two ESs comparing anxiety disorder rates in IBD vs. healthy youth). Clearly, the dearth of research in pediatric IBD and, in particular, in rates of anxiety symptoms, anxiety disorders, and depressive disorders is an area in need of future research attention. Additionally, because many of the comparisons were conducted with normative data rather than matched comparison samples, differences in demographic factors between the IBD and normative groups may have exaggerated between group differences. Moreover, although several studies were excluded from this meta-analysis, including any study not published in English, these studies still provide useful information in understanding the multitude of psychosocial challenges faced by patients with IBD. Finally, the primary aims of the current study and those included in this analysis precluded any determination of the relative risk of poor medical outcome in patients with increased psychosocial difficulties.
Table I.
Characteristics of Individual Studies Included in the Meta-analysis
| Study | IBD (N) | Healthy sample | Healthy sample (N) | Chronic illness sample | Chronic illness sample (N) | Psychosocial domains assessed | Measures included |
|---|---|---|---|---|---|---|---|
| Burke, Meyer, Kocoshis, Orenstein, Chandra, Nord, et al. (1989) | 55 | None | – | Cystic Fibrosis | 52 | Anxiety Disorders, Depressive Disorders, Internalizing Disorders | Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS; Parent & Youth Interview) |
| Burke, Meyer, Kocoshis, Orenstein, Chandra, et al. (1989) | 44 | None | – | Cystic Fibrosis | 46 | Anxiety Symptoms | Leyton Obsession Inventory (Youth Report) |
| Canning, Hanser, Shade, & Boyce (1992) | 11 | None | – | Cystic Fibrosis, Type 1 Diabetes Mellitus, Cancer | 72 | Internalizing Disorders | Diagnostic Schedule Interview for Children-2 (DISC-2; Parent & Youth Interview) |
| Cunningham, Drotar, Palermo, McGowan, & Arendt (2007) | 49 | Healthy Comparison Group | 49 | None | – | Quality of Life (QOL) Self-esteem | Children’s Health Questionnaire Parent Form 50 (CHQ-PF 50) General Health Perceptions Scale (Parent Report); CHQ Child Form 87 (CHQ-CF 87) General Health Perceptions Scale (Youth Report) CHQ-PF 50 Self-esteem Scale (Parent Report); CHQ-CF 87 Self-esteem Scale (Youth Report) |
| DeBoer, Grootenhuis, Derkx, & Last (2005) | 40 | Normative Data | 266 | None | – | QOL Social Functioning | TACQOL Total Score (Youth Report) TACQOL Social Functioning Subscale (Youth Report) |
| Engstrom (1992) | 20 | Healthy Comparison Group | 20 | Headache Type 1 Diabetes Mellitus | 20 20 | Anxiety Disorders, Depressive Disorders, Internalizing Disorders Anxiety Symptoms Depressive Symptoms Externalizing Symptoms Internalizing symptoms Self-esteem Social Functioning | Child Assessment Schedule (CAS; Youth Interview) Revised Children’s Manifest Anxiety Scale (RCMAS) Total Anxiety (Youth Report) Children’s Depression Inventory (CDI; Youth Report) Children’s Behavior Checklist (CBCL) Total Externalizing Symptoms Raw Score (Parent Report) CBCL Total Internalizing Problems Raw Score (Parent Report) Jag Tycker Ar Self-esteem Total Score (Youth Report) CBCL Social Competence Total Raw Score (Parent Report) |
| Gold, Issenman, Roberts & Watt (1991) | 36 | Normative Data | 1148 for CDI 1765 for Piers Harris 1022 for CBCL | Recurrent Abdominal Pain, Functional Mega Colon | 26 | Depressive Symptoms Self-esteem Social Functioning | CDI (Youth Report) Piers Harris Self Concept Total Score (Youth Report) CBCL Social Competence Total T Score (Parent Report) |
| Hommel, Davis, & Baldassano (2008) | 36 | Normative Data | 1148 for CDI 717 for PedsQL | Normative Data | 662 for PedsQL | Depressive Symptoms QOL Social Functioning | CDI (Youth Report) PedsQL Total Score (Parent and Youth Reports) PedsQL Social Functioning Subscale Score (Parent & Youth Report) |
| Loonen, Derkx, Koopman, & Heymans (2002) | 83 | Normative Data | 266 | None | – | Social Functioning | TACQOL Social Functioning Subscale (Parent and Youth Report) |
| Mackner & Crandall (2006) | 50 | Healthy Comparison Group | 42 | None | – | Externalizing Symptoms Internalizing Symptoms Social Functioning | CBCL Total Externalizing Problems T Score CBCL Total Internalizing Problems T Score CBCL Social Competence Total T Score (Parent Report) |
| Mackner & Crandall (2005) | 50 | Healthy Comparison Group | 42 | None | – | Depressive Symptoms Self-esteem | CDI (Youth Report) Piers-Harris Self- Concept Total Score (Youth Report) |
| Otley, Smith, Nicholas, Munk, Avolio, & Sherman, et al. (2002) | 147 | Normative Data | 232 for CHQ = CF 87 1765 for Piers Harris | None | – | QOL Self-esteem | CHQ-CF 87 General Health Perceptions (Youth Report) Piers-Harris Self-Concept Total Score (Youth Report) |
| Perrin, Kuhlthau, Chughtai, Romm, Kirschner, Ferry, et al. (2008) | 220 | Normative Data | 717 | Normative Data | 662 | QOL | PedsQL Total Score (Parent and Youth Reports) |
| Raymer, Weininger, & Hamilton (1984) | 44 | Healthy Comparison Group | 30 | None | – | Depressive Symptoms Self-esteem Social Functioning | CDI (Youth Report) Coopersmith Self-esteem Inventory Total Score (Youth Report) Personal Adjustment Inventory (Youth Report) |
| Shepanski, Hurd, Culton, Markowitz, Mamula, & Baldassano (2005) | 55 | Normative Data | 1554 | None | – | Anxiety Symptoms | State Trait Anxiety Inventory for Children (STAIC) Trait Anxiety Score (Youth Report) |
| Szajnberg, Krall, Davis, Treem, & Hyams (1993) | 21 | Normative Data | 2368 for CBCL | None | – | Externalizing Symptoms Internalizing Symptoms | CBCL Total Externalizing Problems T Score CBCL Total Internalizing Problems T Score |
| Szigethy, Levy-Warren, Whitton, Bousvaros, Kimberlee, Leichtner, et al. (2004) | 102 | Normative Data | 1148 | None | – | Depressive Symptoms | CDI (Youth Report) |
| Tojek, Lumley, Corlis, Ondersma, & Tolia (2000) | 62 | Normative Data | 1148 | None | – | Depressive Symptoms | CDI (Youth Report) |
| Youssef, Murphy, Langseder, & Rosh (2006) | 42 | Healthy Comparison Group | 42 | Functional Abdominal Pain | 65 | QOL Social Functioning | PedsQL Total Score (Parent and Youth Reports) PedsQL Social Subscale Score (Parent and Youth Reports) |
This study identified important gaps in the current pediatric IBD psychosocial literature. Consequently, there are several areas upon which future research efforts should be focused. First, the comprehensiveness of the description of results in published articles is an important area for improvement. In order to accurately summarize and analyze data from existing studies, there needs to be better clarity of the methods and findings so that those studies can be included in analyses or critical reviews. Inclusion of additional disease related details including the level of disease activity, length of disease, presence of surgical intervention, and nature of the medication regimen would also be of value in understanding the potential role of disease factors in influencing youth adjustment. Second, the measures that have been employed in prior studies may not be appropriate and/or sensitive enough to examine the nuances of psychosocial dysfunction in this population. Measures of depression and anxiety are appropriate diagnostic tools, but may not articulate other problematic internalizing issues (e.g., helplessness, hopelessness, and negative disease-related attributions). Indeed, diagnostic assessments, while important for treatment, may not accurately detect sub-clinical pathology that is equally important for treatment as it may maintain overall psychosocial dysfunction. Third, there is a significant need for large-scale longitudinal studies in pediatric IBD that examine trajectories of psychosocial development, particularly in relation to disease outcomes. Such studies would offer more definitive results and clarify the impact of psychosocial functioning on disease parameters. The inclusion of demographically matched comparison samples in future studies would help to more clearly elucidate the unique risks associated with IBD. Finally, given the findings of this study, specific constructs on which future research should focus include QOL, social functioning, and internalizing disorder diagnoses, and how these factors relate to each other and to health outcomes. We anticipate that attention to these recommendations will result in high quality research that better informs treatment recommendations and leads to improved psychosocial and health outcomes in the pediatric IBD population.
Funding
NIDDK K23 DK079037 (to K.H., Partial), PHS Grant P30 DK 078392 (to K.H., Partial).
Conflicts of interest: None declared.
Acknowledgments
We thank Kara Guilfoyle and Elizabeth Hente for assistance with data abstraction.
References
*References marked with an asterisk indicate studies included in the meta-analysis.
- Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Berg CJ, Rapoport JL, Flament M. The Leyton Obsessional Inventory-Child Version. Journal of the American Academy of Child Psychiatry. 1986;25:84–91. doi: 10.1016/s0002-7138(09)60602-6. [DOI] [PubMed] [Google Scholar]
- Burke P, Meyer V, Kocoshis S, Orenstein DM, Chandra R, Nord DJ, et al. Depression and anxiety in pediatric inflammatory bowel disease and cystic fibrosis. Journal of the American Academy of Child and Adolescent Psychiatry. 1989;28:948–951. doi: 10.1097/00004583-198911000-00022. [*] [DOI] [PubMed] [Google Scholar]
- Burke P, Meyer V, Kocoshis S, Orenstein D, Chandra R, Sauer J. Obsessive-compulsive symptoms in childhood inflammatory bowel disease and cystic fibrosis. Journal of the American Academy of Child & Adolescent Psychiatry. 1989;28:525–527. doi: 10.1097/00004583-198907000-00009. [*] [DOI] [PubMed] [Google Scholar]
- Caldwell DM, Ades AE, Higgins J. PT. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. British Medical Journal. 2005;331:897–900. doi: 10.1136/bmj.331.7521.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canning EH, Hanser S, Shade K, Boyce W. Mental disorders in chronically ill children: Parent-child discrepancy and physician identification. Pediatrics. 1992;90:692–696. [*] [PubMed] [Google Scholar]
- Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, Davies M. The assessment of affective disorders in children and adolescents by semistructured interview. Archives of General Psychiatry. 1985;42:696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- Coopersmith S. The antecedents of self-esteem. San Francisco, CA: W. H. Freedman; 1967. [Google Scholar]
- Cunningham C, Drotar D, Palermo TM, McGowan K, Arendt R. Health-related quality of life in children and adolescents with inflammatory bowel disease. Children’s Healthcare. 2007;36(1):29–43. [*] [Google Scholar]
- DeBoer M, Grootenhuis M, Derkx B, Last B. Health-related quality of life and psychosocial functioning of adolescents with inflammatory bowel disease. Inflammatory Bowel Diseases. 2005;11(4):400–406. doi: 10.1097/01.mib.0000164024.10848.0a. [*] [DOI] [PubMed] [Google Scholar]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple graphical test. British Medical Journal. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engstrom I. Mental health and psychological functioning in children and adolescents with inflammatory bowel disease: a comparison with children having other chronic illnesses and with healthy children. Journal of Child Psychology and Psychiatry. 1992;33(3):563–582. doi: 10.1111/j.1469-7610.1992.tb00891.x. [*] [DOI] [PubMed] [Google Scholar]
- Fleiss JL, Gross AJ. Meta-analysis in epidemiology, with special reference to studies of the association between exposure to environmental tobacco smoke and lung cancer: A critique. Journal of Clinical Epidemiology. 1991;44:127–139. doi: 10.1016/0895-4356(91)90261-7. [DOI] [PubMed] [Google Scholar]
- Gold N, Issenman R, Roberts J, Watt S. Well-adjusted children: An alternate view of children with inflammatory bowel disease and functional gastrointestinal complaints. Inflammatory Bowel Diseases. 2000;6:1–7. doi: 10.1097/00054725-200002000-00001. [*] [DOI] [PubMed] [Google Scholar]
- Hanauer SB. Inflammatory bowel disease: Epidemiology, pathogenesis, and therapeutic opportunities. Inflammatory Bowel Diseases. 2006;12:S3–S9. doi: 10.1097/01.mib.0000195385.19268.68. [DOI] [PubMed] [Google Scholar]
- Hedges LV. Distribution theory for Glass's; estimator of effect size and related estimators. Journal of Educational Statistics. 1981;6:107–128. [Google Scholar]
- Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychological Methods. 1998;3:486–504. [Google Scholar]
- Higgins J, Thompson S, Deeks J, Altman D. Statistical heterogeneity in systematic reviews of clinical trials: A critical appraisal of guidelines and practice. Journal of Health Services Research and Policy. 2002;7:51–61. doi: 10.1258/1355819021927674. [DOI] [PubMed] [Google Scholar]
- Hodges K, Kline J, Fitch P, McKnew D, Cytryn L. The Child Assessment Schedule: A diagnostic interview for research and clinical use. Catalog of Selected Documents in Psychology. 1981;11:56. [Google Scholar]
- Hommel KA, Davis CM, Baldassano RN. Medication adherence and quality of life in pediatric inflammatory bowel disease. Journal of Pediatric Psychology. 2008;33:867–874. doi: 10.1093/jpepsy/jsn022. [*] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory. North Tonawanda, NY: Multi-Health Systems; 1992. [Google Scholar]
- Landergraf JM, Abetz L, Ware JE. The CHQ User’s Manual. 1st edition. Boston, MA: The Health Institute, New England Medical Center; 1996. [Google Scholar]
- Langholz E, Munkholm P, Karsilnikoff PA, Binder V. Inflammatory bowel disease with onset in childhood. Scandinavian Journal of Gastroenterology. 1997;32:139–147. doi: 10.3109/00365529709000184. [DOI] [PubMed] [Google Scholar]
- Loonen HJ, Grootenhuis MA, Last BF, Koopman HM, Derkx H. HF. Quality of life in paediatric inflammatory bowel disease measured by a generic and a disease-specific questionnaire. Acta Paediatrica. 2002;91:348–352. doi: 10.1080/08035250252834049. [DOI] [PubMed] [Google Scholar]
- Loonen H, Derkx B. HF, Koopman H, Heymans H. SA. Are parents able to rate the symptoms and quality of life of their offspring with IBD? Inflammatory Bowel Diseases. 2002;8(4):270–276. doi: 10.1097/00054725-200207000-00006. [*] [DOI] [PubMed] [Google Scholar]
- Mackner LM, Crandall WV. Psychological factors affecting pediatric inflammatory bowel disease. Current Opinion in Pediatrics. 2007;19:548–552. doi: 10.1097/MOP.0b013e3282ef4426. [DOI] [PubMed] [Google Scholar]
- Mackner LM, Crandall W. Brief report: Psychosocial adjustment in adolescents with inflammatory bowel disease. Journal of Pediatric Psychology. 2006;31(3):281–285. doi: 10.1093/jpepsy/jsj023. [DOI] [PubMed] [Google Scholar]
- Mackner LM, Crandall WV. Oral medication adherence in pediatric inflammatory bowel disease. Inflammatory Bowel Diseases. 2005;11:1006–1012. doi: 10.1097/01.mib.0000186409.15392.54. [DOI] [PubMed] [Google Scholar]
- Mackner LM, Sisson DP, Crandall WV. Review: Psychosocial issues in pediatric inflammatory bowel disease. Journal of Pediatric Psychology. 2004;29:243–257. doi: 10.1093/jpepsy/jsh027. [DOI] [PubMed] [Google Scholar]
- Otley AR, Smith C, Nicholas D, Munk M, Avolio J, Sherman PM, et al. The IMPACT questionnaire: A valid measure of health-related quality of life in pediatric inflammatory bowel disease. Journal of Pediatric Gastroenterology and Nutrition. 2002;35(4):557–563. doi: 10.1097/00005176-200210000-00018. [*] [DOI] [PubMed] [Google Scholar]
- Ouvinen-Birgerstam P. Jag Tyker Jag Ar Manual. 1985. (in Swedish). Stockholm: Psykologiforlaget. [Google Scholar]
- Perrin J, Kuhlthau K, Chughtai A, Romm D, Kirschner B, Ferry G, et al. Measuring quality of life in pediatric patients with inflammatory bowel disease: Psychometric and clinical characteristics. Journal of Pediatric Gastroenterology and Nutrition. 2008;46:164–171. doi: 10.1097/MPG.0b013e31812f7f4e. [*] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piers EV. Piers-Harris Children’s Self-Concept Scale. Los Angeles, CA: Western Psychological Services; 1996. [Google Scholar]
- Raymer D, Weininger O, Hamilton J. Psychological problems in children with abdominal pain. Lancet. 1984;1(8374):439–440. doi: 10.1016/s0140-6736(84)91763-x. [*] [DOI] [PubMed] [Google Scholar]
- Reynolds CR, Richmond BO. What I think and feel: A revised measure of children’s manifest anxiety. Journal of Abnormal Child Psychology. 1978;6:271–280. doi: 10.1007/BF00919131. [DOI] [PubMed] [Google Scholar]
- Rogers CR. Personal adjustment inventory—Boys and girls. New York: Association Press; 1961. [Google Scholar]
- Sackett DL. Bias in analytic research. Journal of Chronic Diseases. 1979;32:51–63. doi: 10.1016/0021-9681(79)90012-2. [DOI] [PubMed] [Google Scholar]
- Scargle JD. Publication bias: The file drawer problem in scientific interference. Journal of Scientific Exploration. 2000;14:94–106. [Google Scholar]
- Shaffer D, Fisher P, Piacentini J, Schwab-Stone M, Wicks J. Diagnostic Interview Schedule for Children. New York, NY: New York State Psychiatric Institute; 1990. [Google Scholar]
- Shapiro S. Meta-analysis/shmeta-analysis. American Journal of Epidemiology. 1994;140(9):771–778. doi: 10.1093/oxfordjournals.aje.a117324. [DOI] [PubMed] [Google Scholar]
- Shepanski M, Hurd L, Culton K, Markowitz J, Mamula P, Baldassano R. Health-related quality of life improves in children and adolescents with inflammatory bowel disease after attending a camp sponsored by the Crohn's; and Colitis Foundation of America. Inflammatory Bowel Diseases. 2005;11(2):164–170. doi: 10.1097/00054725-200502000-00010. [*] [DOI] [PubMed] [Google Scholar]
- Spielberger CD. State-Trait Anxiety Inventory for Children Manual. Redwood City, CA: Mind Garden Inc; 1973. [Google Scholar]
- Stern JAC, Egger M. Funnel plots for detecting bias in meta-analysis: Guidelines on choice of axis. Journal of Clinical Epidemiology. 2001;54:1046–1055. doi: 10.1016/s0895-4356(01)00377-8. [DOI] [PubMed] [Google Scholar]
- Szajnberg N, Krall V, Davis P, Treem W, Hyams J. Psychopathology and relationship measures in children with inflammatory bowel disease and their parents. Child Psychiatry and Human Development. 1993;23:215–232. doi: 10.1007/BF00707151. [*] [DOI] [PubMed] [Google Scholar]
- Szigethy E, Levy-Warren A, Whitton S, Bousvaros A, Kimberlee G, Leichtner AM, et al. Depressive symptoms and inflammatory bowel disease in children and adolescents: A cross-sectional study. Journal of Pediatric Gastroenterology and Nutrition. 2004;39(4):395–403. doi: 10.1097/00005176-200410000-00017. [*] [DOI] [PubMed] [Google Scholar]
- Tojek T, Lumley M, Corlis M, Ondersma S, Tolia V. Maternal correlates of health status in adolescents with inflammatory bowel disease. Journal of Psychosomatic Research. 2002;52:173–179. doi: 10.1016/s0022-3999(01)00291-4. [*] [DOI] [PubMed] [Google Scholar]
- Varni JW, Seid M, Kurtin PS. PedsQL 4.0: Reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Medical Care. 2001;39:800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- Vogels T, Verrips G. HW, Koopman HM, Theunissen H. CM, Fekkes M, Kamphuis RP. TACQOL Manual: Parent Form and Child Form. Leiden: Leiden Center for Child Health and Pediatrics; 2000. [Google Scholar]
- Youngstrom E, Loeber R, Stouthamer-Loeber M. Patterns and correlates of agreement between parent, teacher, and male adolescent ratings of externalizing and internalizing problems. Journal of Consulting and Clinical Psychology. 2000;68:1038–1050. doi: 10.1037//0022-006x.68.6.1038. [DOI] [PubMed] [Google Scholar]
- Youssef N, Murphy T, Langseder A, Rosh J. Quality of life for children with functional abdominal pain: A comparison study of patients' and parents' perceptions. Pediatrics. 2006;117:54–59. doi: 10.1542/peds.2005-0114. [*] [DOI] [PubMed] [Google Scholar]