Synopsis
The purpose of the present review is to provide a comprehensive update of current epidemiological studies that have assessed the association between sleep and obesity risk. Data from 29 studies conducted in 16 countries suggest that short sleep is associated with an increased risk for being or becoming overweight/obese or having increased body fat. Late bedtimes were also found to be a risk factor for overweight/obesity. Findings also suggest that changes in eating pathways may lead to increased body fat. Future experimental studies are needed to enhance our understanding of the underlying mechanisms through which sleep may play a role in the development and maintenance of childhood obesity.
Keywords: sleep, obesity, adiposity, eating behaviors, activity behaviors
Introduction
Pediatric obesity is considered an epidemic with 32% of U.S. children and adolescents 2-19 years old considered overweight or obese in 2007-2008.1 The medical and psychosocial risks associated with being overweight and obese as a child or adolescent have been well documented. Multiple studies have demonstrated the increased risk for Type 2 diabetes and a number of cardiovascular disease risks, including elevations in cholesterol, diastolic and systolic blood pressure, fasting insulin levels, and triglycerides.2-4 Children and adolescents who are overweight and obese report lower health related quality of life compared to their normal weight peers, and may be at increased risk of poorer self-esteem, greater body dissatisfaction, and increased peer teasing.5,6 The importance of addressing this epidemic is underscored by a number of national policy efforts and by the proposed goals for Healthy People 2020.7
Given the precipitous rise in pediatric obesity and its associated risks, increasing attention has been paid to efforts to enhance prevention and treatment approaches. Current prevention approaches have demonstrated variable impact on weight outcomes8 with some efficacy shown for school-based approaches that combine diet and physical activity.9 A number of intervention approaches for children and adolescents who are overweight and obese have demonstrated efficacy, including those that combine dietary and physical activity prescriptions with the use of effective behavioral strategies.10 Use of weight loss medication also has demonstrated efficacy10, and surgical approaches also show some promise11 within adolescent populations. However, each of these approaches has limitations, and despite their effectiveness, seldom help children and adolescents achieve non-obese status. Thus it is imperative to identify novel targets to enhance current treatment approaches.
A number of factors suggest that enhancing children's sleep may be an effective strategy for preventing and treating pediatric obesity. Over the past 20-30 years, as rates of pediatric obesity have climbed, children's nocturnal sleep duration has declined. 12,13 Data from the 2004 National Sleep Foundation's (NSF) Sleep in America Poll show that the mean sleep length for school-age children (1st to 5th grade) is 9.4 hours/night.14 These data are in contrast to recommendations by sleep experts that children in this age group should obtain 10-11 hours/night.15,16 Thus, children may not be achieving sufficient sleep length.
In addition to above, experimental studies with adults have documented physiological and behavioral changes in response to sleep deprivation, which, if chronic, may promote weight gain. The secretion of a number of hormones, including growth hormone, prolactin, cortisol, thyrotropin, and insulin, are influenced by sleep.17 For example, studies suggest that sleep restriction leads to decreased circulating leptin18,19 and increased ghrelin20 both of which are associated with increased hunger, appetite, motivation to eat, and food intake.21-23 Further, more recent experimental studies with adults have demonstrated increases in caloric intake from both snack foods24 and from main meals25 when sleep is restricted, suggesting that less sleep may increase the risk of obesity via neuroendocrine changes that increase food intake. Finally, although less is known in this regard, it is hypothesized that sleep deprivation may also lead to changes in physical and sedentary activities, which could promote weight gain. Limited support for this hypothesis comes from studies with adults that have demonstrated subsequent decreases in activity level following sleep deprivation.26,27
To our knowledge, no experimental studies involving the manipulation of sleep in children and weight-related outcomes have been reported (although there are ongoing trials). However, there are considerable epidemiological data with children and adolescents examining the association between sleep duration (typically nocturnal sleep) and weight status. Findings from both cross-sectional and prospective studies, although limited by their inability to demonstrate causation (i.e., that less sleep at night leads to increased weight status), are important for helping to shape our understanding of the potential role that sleep may play in the current obesity epidemic. Prospective studies, in particular, help to establish temporal relationships between sleep and pediatric obesity. The purpose of the present review is to provide a comprehensive update of current epidemiological studies that have assessed the association between sleep and obesity risk. Although obstructive sleep apnea is also associated with obesity risk, it is beyond the scope of the present paper. The reader is referred to Ievers-Landis & Redline28 as well as the paper by (cite authors) in this Special Issue for a more comprehensive review. To build upon previous reviews, the present paper includes information on anthropometric indices (i.e., waist circumference, percent body fat) other than BMI, includes findings regarding sleep timing and quality (as opposed to only focusing on sleep duration), and reviews findings regarding possible mediators of the sleep-weight relationship.
Methods
A systematic search for publications was performed using the PubMed database that included published studies through July 2010. Combinations of key words specific to sleep (e.g., sleep and sleeping), weight status (e.g., BMI, overweight, obesity, adiposity, weight fatness, food diet, and energy expenditure), and childhood and adolescence (e.g., child, children, adolescent, adolescence) were used. In addition, reference lists of relevant articles, and previously conducted relevant review papers/meta-analyses were reviewed to identify additional studies. Only studies that focused on children and adolescents (i.e., birth-18 years), and represented original empirical work (i.e., reviews and editorials were excluded) were included in the present review. Questions regarding inclusion of studies were decided by consensus. This resulted in the inclusion of 38 studies (with 2 additional duplicates) in the present review.
Results
Sleep Duration and Obesity Risk
Table 1 presents findings from studies that assessed the association between sleep duration and obesity risk in children and adolescents. 29-58 It represents 30 studies from 16 countries. For ease of comparison, studies presented in the Table are those in which main findings are presented as odds ratios. Two groups published subsequent studies using the same data set, but controlling for additional confounding variables. These subsequent studies were consistent with initial findings and are referenced as footnotes to the Table. The majority of studies present cross-sectional findings (N = 24) with 6 studies assessing the association between sleep duration and weight status prospectively. As can be seen in the table, the majority of studies assessed the construct of sleep duration exclusively through parent- or self-report (N = 28)29-32,34-40,42-57 with two additional studies assessing sleep length via actigraphy.33,41 In contrast, the majority of studies (N = 27) used measured height and weight to calculate body mass index in children with only two studies using parent- or self-report38,46,58, and one additional study in which it was unclear whether caretaker report or measured height and weight were obtained.56
Table 1.
Description of Findings of Studies that Assessed the Association between Sleep Duration and Obesity Risk in Children and Adolescents (N = 30).
| STUDY COUNTRY | SAMPLE CHARACTERISTICS | SLEEP MEASURE and REFERENCE VALUE | MEASURE OF BMI STATUSa | CONFOUNDERS CONTROLLED | MAIN FINDINGS |
|---|---|---|---|---|---|
| CROSS-SECTIONAL STUDIES | |||||
| Locard et al. (1992) FRANCE | 5 years old (N=1,031) | Caretaker-reported Referent ≥ 11 hrs |
Measured height and weight; weight-for-height and sex Zscore > 2 = OB | --------- | OB : < 11 hrs: OR = 1.4 (1.0-2.0) |
| Sekine et al. (2002)b JAPAN | 2.5 to 4.3 years old (N=8,941) | Caretaker-report (24-hour sleep) Referent ≥11 hrs |
Measured height and weight; OB: age/sex BMI cut-off points by Cole et al |
Age, gender, parental OB, and outdoor playing time | OB: <9 hrs: N/S 9 to 10 hrs: ORadj = 1.34 (1.05 – 1.72) 10 to 11 hrs: N/S |
| Sekine et al. (2002)b JAPAN | 6 to 7 years (N=8,274) | Caretaker-report (24-hour sleep) Referent ≥10 hrs |
Measured height and weight; OB: age/sex BMI cut-off points by Cole et al |
Age, sex, parental OB, PA%, TV watching, frequency of breakfast, and frequency of snack | OB : 9 to 10 hrs: ORadj = 1.49 (1.08 – 2.14) 8 to 9hrs: 1.89 (1.34 – 2.73) < 8hrs: 2.87 (1.61 – 5.05) |
| Von Kries et al. (2002) GERMANY | 5 to 6.99 years (N=6,645) | Caretaker-report (WD$ sleep) Referent ≤10 hrs |
Measured height and weight; OW: age/sex BMI > 90th centile, OB >97th centile based on local norms | Parent education, parent OB, single parent, and maternal smoking | OW: 10.5 to 11 hrs: ORadj = .77 (.59 - .99) ≥11 hrs .54 (.40 - .73) OB: 10.5 to 11 hrs: ORadj = .53 (.35 - .80) ≥11 hrs .45 (.28 - .75) |
| Gupta et al. (2002) USA | 11 to 16 years old (N=308) | Actigraphy (1 night) Referent: sleep duration as continuous |
Measured height and weight; BMI > 85th percentile (CDC) | For every additional hour of sleep time, odds of OB decreased by 80%: OR = .20 (95th CI = 0.11) |
|
| Hui et al. (2003) CHINA | 6 to 7 years old (N = 343) | Caretaker-reported Referent: < 9 hrs |
Measured height and weight; BMI ≥ 92nd centile, using Hong Kong cross-sectional growth survey as reference | Paternal and maternal obesity | OW: 9 to 11 hrs: ORadj = .54 (0.30-0.97) ≥ 11 hrs = .31 (0.11-0.87) |
| Padez et al. (2005)d PORTUGAL | 7 to 9.5 years (N = 4,511) | Caretaker-reported Referent: 8 hrs |
Measured height and weight; age/sex BMI cut-off points by Cole et al | Sex and age | OW: 9 to 10 hrs: ORadj = .46 (.40 - .51) ≥11 hrs .44 (.38 - .49) OB: 9 to 10 hrs: ORadj = .44 (.40 - .47) ≥11 hrs .39 (.35 - .42) |
| Chen et al. (2006) TAIWAN | 13 to 18 years (N = 656) | Self-report of 6 to 8 hrs of sleep (WD sleep) Referent ≥4 nights/week |
Measured height and weight; OW: BMI ≥85thpercentile for age/sex (DOH) | -------- | OW: < 4 nights/week: OR = 1.74 (1.3 – 2.4) |
| Chaput et al. (2006) CANADA | 5 to 10 years (N=422) | Caretaker-report (WD sleep) Referent: 12 to 13 hrs |
Measured height and weight; OW/OB: age/sex BMI cut-off points by Cole et al |
Age, sex, parental OB | 10.5 to 11.5 hrs: ORadj = 1.42 (1.09 - 1.98) 8 to 10 hrs 3.45 (2.61 – 4.67) *Relationship stronger for males (per personal communication) |
| Eisenmann et al. (2006)c AUSTRALIA | 12.4 years (N=6,321) | Self-report Referent ≥10 hrs |
Measured height and weight; OW/OB: age/sex BMI cut-off points by Cole et al |
Age | OW/OB: Males only: 9 to 10 hrs: ORadj = 1.61 (1.19 - 2.17) 8 to 9 hrs 1.83 (1.30 – 2.58) ≤ 8 hrs 3.06 (2.11 – 4.46) |
| Seicean et al. (2007) USA | 15.6 +/- 1.23 years (N = 509) | Self-reported (WD sleep) Referent >8 hrs |
Self-reported height and weight (30% weighed themselves using a scale on scene); OW: age/sex ZBMI >85th percentile; OB > 95th percentile (CDC) | Gender, age, irregular eating, health status, and caffeine intake | OW: < 5 hrs: ORadj = 7.65 (1.87 -31.30) 5 to 6: N/S 7 to 8: N/S 6 to 7 hrs 2.55 (1.02 – 6.38) |
| Kuriyan et al. (2007) INDIA | 6 to 16 years (N = 598) | Caretaker-report (younger) or Self-report (older) Referent >9.5 hrs |
Measured height and weight; OW: age/sex BMI cut-off points by Cole et al | Age, gender, living location, and SES | OW: ≤8 hrs: ORadj = 6.7 (1.5 – 30.2) |
| Knutson et al. (2007) USA | 10 to 19 years (N=1,546) | A) Self-report B) Self-report using time diaries Referents: A) 9.2 to 19.0 hrs B)10.08-16.17 hrs |
Measured height and weight; OW: BMI ≥95th percentile for age and gender (CDC) | Race, age, family income, education, TV viewing, physical activity, and media use | OW: A) 7 to 8 hrs ORadj = 1.85: (1.01 – 3.38) 8.1 to 9 hrs: 1.93 (1.10 – 3.37) B) All sleep categories NS. |
| Nixon et al. (2008) NEW ZEALAND | 7.3 years (N=519) | Actigraphy (1 night) Referent ≥9 hrs |
Measured height and weight; OW/OB: age/sex BMI cut-off points by Cole et al |
Maternal BMI, maternal age, gender, hrs of TV, and sedentary activity | OW/OB: < 9hrs : ORadj = 3.32 (1.40 – 7.87) |
| Ivers-Landis et al. (2008) USA | 8 to 11 years (N=819) | A) Caretaker-report of sleep duration B) Caretaker-assisted report using 7-day sleep diary Referent: duration as continuous |
Measured height and weight (PC); OB: age/sex BMI ≥95th percentile (CDC) |
Age, gender, preterm status, psychosocial functioning, and parental stress | OB: A) ORadj = 1.41 (1.12 – 1.76) Odd of being OB increase by 41% with every 1 hour of sleep decline B) ORadj = 1.45 (1.09 – 1.94) Odds of being OB increase by 45% with every 1 hour of sleep decline |
| Liu et al. (2008) USA | 7 to 17 years (N=335) | Self-reported 7-day sleep diary Referent: duration as continuous |
Measured height and weight; at risk: age/sex ZBMI 85th to 95th percentile; OW ZBMI ≥ 95th percentile (CDC) | Age, sex, SESΩ, ethnicity, puberty, and psychiatric diagnosis | OW: Reduced sleep (1 hour less of): ORadj = 2.12 (1.05 – 4.28) |
| Wells et al. (2008) BRAZIL | 10 to 12 years (N=4,452) | Self-report (WD sleep) Referent < 9 hrs |
Measured height & weight; IOTF guidelines used to define OW & OB | Sex, birth weight & length, maternal smoking and alcohol consumption during pregnancy, maternal pre-pregnancy BMI, SES, PA, systolic & diastolic BP, TV hrs | OB: ORadj = 9-10 N/S >10h N/S Odds of being OB decreased by 14% with every additional hour of sleep |
| Bawazeer et al. (2009) SAUDI ARABIA | 10 to 19 years (N=5,877) | Caretaker-report Referent >7 hrs |
Measured height, weight, waist circumference & hip circumference; OB defined as >95th percentile BMI for age & gender | ------ | OB: Males ≤ 7h: OR = 1.28 (1.09 - 1.50) Females ≤ 7h 1.38 (1.02 - 1.89) |
| Wing et al. (2009) CHINA | 5 to 15 years (N=5,159) | Caretaker-report Referent > 10 hrs |
Parent report of height & weight converted to ZBMI (OW ZBMI between 85th and 95th percentile; OB ZBMI > 95th percentile per CDC guidelines) | Age, gender, TV viewing, time to do homework, parent education, & eating 1 hr before going to bed. | OW/OB: Weekdays: ≤ 8hrs: ORadj = 1.74 (1.23-2.45) 8.01-9 hrs 1.51 (1.13-2.03) 9.01-10 hr 1.30 (0.97-1.76) Weekends: ≤ 8hrs: ORadj = 1.80 (1.05-3.09) 8.01-9 hrs 1.66 (1.30-2.13) 9.01-10 hrs 1.36 (1.12-1.66) |
| Hitze et al. (2009) GERMANY | 6 to 19 years (N=414) | Caretaker-report (younger) and self-report (older) (WD sleep) Referent: “Long sleep” (9 to 10 hrs for younger; 8 to 9 hrs for older) |
Measured height & weight; German references used to define OW & OB | Paternal BMI, birth weight, change in weight birth-2 years, duration of breastfeeding | OB: Girls only: Short sleep: ORadj = 5.5 (1.3-23.5) |
| Jiang et al. (2009) CHINA | 3 to 4 years (N=1,311) | Caretaker-report Referent ≥ 11 hrs |
Measured height & weight; Country norms used to define obesity (>95th percentile) | Age, sex, appetite, birth weight, maternal age at delivery, mother & father education, household income, & geographic location. | OB: <9hrs 4.76: ORadj = (1.28-17.69) 9hrs 3.42 (1.12-10.46) 9.5 hrs = N/S 10 hrs = N/S 10.5 hrs = N/S |
| Ozturk et al. (2009) TURKEY | 6 to 7 years (N=5,358) | Caretaker-report Referent ≥10 hrs |
Measured height & weight; IOTF guidelines used to define OW & OB | ------ | OW/OB: Boys only: ≤8h: OR = 2.06 (1.31-3.24) 8.1- 8.9hrs 1.74 (1.10-2.75) 9.0-9.9hrs 1.86 (1.17-2.97) |
| Sun et al. (2009)b JAPAN | 12 to 13 years (N=5,753) | Self-report Referent 8 to 9 hrs |
Measured height & weight; IOTF guidelines used to define OW & OB | Age, paternal overweight, maternal overweight, breakfast frequency, snacking frequency, nighttime snacking, eating speed, eating volume, physical activity, TV watching, video game playing. | OW: Girls only: <7hrs: ORadj = 1.81 (1.21-2.72) 7-8 hrs 1.37 (1.00-1.88) ≥9 hrs = NS |
| Anderson & Whitaker (2010) USA | ∼ 4 years (N=8,750) | Caretaker-report Referent ≥ 10.5 hrs |
Measured height & weight; CDC guidelines used to define OB (≥ 95th percentile for age & gender) | Eating dinner as a family, screen viewing time, child age, gender, race/ethnic group, household income-to-poverty ratio, single-parent household, maternal education, maternal BMI, & maternal age. | OB: < 10.5 hrs: ORadj = .86 (0.71-1.03) |
| LONGITUDINAL STUDIES | |||||
| Reilly et al. (2005) UK | 30 months to 7 years (N=7,758) | Caretaker-report (nocturnal sleep duration at 30 months) Referent >12 hrs |
Measured height and weight at 7 years; OB = BMI ≥95th centile using UK reference data | Maternal education, child's sex, and energy intake at 3 years | OB: < 10.5 hrs: ORadj = 1.45 (1.10 – 1.89) 10.5 to 10.9 hrs 1.35 (1.02 -1.79) |
| Snell et al. (2007) USA | 3 to 18 years (Time 1: 3 to 12 years; Time 2: 8 to 18 years; N = 1,441) | Caretaker-report (younger) or self-report (older) | Measured height at all time points, caretaker-reported weight at T1; OW/OB: age/sex BMI cut-off points by Cole et al |
Race, age, sex, BMI at T1, parent income, and parent education | Sleeping > 11 hrs relative to 9 – 9.9 hrs associated with a 17.1% reduction in OW Every additional hr at T1 decreased BMI at T2 by .75 kg/m |
| Lumeng et al. (2007) USA | 9 years to ∼12 years (N=785) | Caretaker-report (24-hour sleep) Referent: duration as a continuous variable |
Measured height and weight; OW: BMI ≥95th percentile for age and gender (NCHS) | Gender, race, maternal education, ZBMI in 3rd grade, and change in sleep duration | OW: Longitudinal: ORadj =.60 (.36 - .99) For every additional hour of sleep at 9 yrs child 40% less likely to be OW at 12 yrs Cross-sectional: For every additional hour of sleep in 6th grade, child ∼20% less likely to be OW |
| Landhuis et al. (2008) NEW ZEALAND | 5 through 32 years (N=780) | Caretaker-report (averaged over ages 5, 7, 9, and 11) Referent: duration as a continuous variable |
Measured height and weight at 32 years; BMI calculated | Sex, SES, parent BMI, TV, parental control, smoking as an adult, and adult PA | OB: ORadj =.65 (.43 - .97) For every additional hour of sleep in childhood, 35% less likely to be OB at 32 |
| Touchette et al. (2008) CANADA | 2.5 to 6 years (N=1,138) | Caretaker-report (averaged over 2.5, 3.5, 4, 5 and 6 yrs) Referent: 11-hr persistent sleep duration |
BMI calculated at 2.5 & 6 yrs; IOTF guidelines used to define OW and OB. | Perinatal variables (e.g., birth weight, parent education), child weight & nap duration at 2.5 yrs; lifestyle variables (e.g., child overeating, snacking, snoring, TV, PA) | OW/OB: Short persistent sleepers (< 10 hrs/night): ORadj = 2.9 (1.0-8.5) Short increasing & 10-hr persistent = NS. |
| Taveras et al. (2008) USA | 6 months to 3 years (N=915) | Caretaker-reported (24-hour sleep averaged over the 6 month, 1 year, and 2 year assessment) Referent ≥12 hrs per day |
Measured height and weight; OW: age/sex BMI ≥95th percentile; (NCHS) | Maternal education, income, prepregnancy BMI, marital status, prenatal smoking, breastfeeding duration, child's race/ethnicity, birth weight, 6-month weight for length, average TV viewing, and daily active play | OW: ORadj = 2.04 (1.07 – 3.91) |
BMI: Body Mass Index; OW: Overweight; OB: Obese; OR = Odds ratio (OR = raw; ORadj = adjusted for confounders); PA = physical activity; WD = weekday; CDC = Centers for Disease Control;PC = Personal communication; SES = Socio-economic status; IOTF = The International Obesity Task Force; ZBMI = Body Mass Index Z-score for sex and age; NCHS = National Center for Health Statistics; DOH = Department of Heath
OR (Confidence Interval [CI])s reflect comparison to sleep referent for that study;
represents studies sampled from the Toyama Birth Cohort;
Biggs and Dollman (2007) supported these findings on the same dataset controlling for PA and diet;
Padez et al. (2009) presented similar findings on the sample controlling for parent education, parent obesity, PA, and TV watching.
As can be seen in the Table, for cross-sectional studies, the reference values for sleep length used to determine obesity risk varied from less than 7 hours of sleep/night to ≥ 12 hours/night. Despite these differences in how referents were defined, all studies demonstrated negative associations between sleep duration and obesity risk. It is important to note that most studies found significant results even after controlling for potential confounding variables (e.g., parental BMI, birth weight, television viewing; see Table for specific confounders controlled for in each study). However, it is also important to note that not every category of sleep was associated with increased risk of obesity. For example, Sekine et al._ENREF_14 found that in comparison to children who slept 11 hours or more each night, there was no increased risk for obesity for children sleeping less than 9 hours or 10-11 hours per night, but that there was an increased risk for obesity for children sleeping 9-10 hours per night.30 Furthermore, when associations were examined separately in boys and girls, some studies found significant results for one gender but not the other.37,47,49,50
In addition to those studies presented in Table 1, six additional studies were conducted, but did not present findings in terms of odds ratios._ENREF_44,_ENREF_4759-64 All six studies found consistent results with less sleep being associated with an increased risk of obesity. However, one study only assessed this association in adolescent females,63 and a second study only found significant results in females.61
Six prospective studies were also identified (see Table52-57). Findings are consistent with cross-sectional studies. For example, Snell and colleagues found that for every additional hour of sleep obtained at time 1 (when children were 3-12 years of age), caretaker-reported BMI decreased by 0.75 kg/m2 at time 2 (when children were 8-18 years old)_ENREF_37.53 Similarly, Touchette and colleagues found that between 2 ½ years and 6 years of age, children who consistently obtained “short sleep” were 2.9 times more likely to be overweight or obese than children who consistently slept 11 hours or more each night even after controlling for potential confounding factors _ENREF_40.56 Consistent with these findings, but over a much longer follow-up, Landhuis et al. found that for every additional hour of sleep obtained during childhood (averaged across 5-11 years), individuals had a 35% reduced risk of obesity at age 32 years_ENREF_39.55
Sleep Duration and Other Anthropometric Indices
In addition to risk for overweight and obesity, more recent studies assessed the association between sleep duration and other indices of body composition. Eleven studies were identified; three of which used two or more measures to assess body fat_ENREF_35.47,49,61 Five studies utilized skinfold thickness34,49,57,62,65, four used waist circumference37,47,49,61, and three used bioelectrical impedence analysis (BIA).32,41,66 Two additional studies used another measure such as dual x-ray absorptiometry (DEXA)61 and air displacement plethysmography.47 Regardless of measure, however, an increase in sleep duration was consistently found to be associated with lower body fat.
For example, Nixon and colleagues found that compared to 7-year-old children sleeping 9 hours or more/night (as measured by actigraphy), children sleeping less than 9 hours/night had an increase of 3.34% body fat (as measured by BIA)_ENREF_25.41 Similarly, von Kries et al. found that when compared with 5-6-year-old children sleeping less than 10 hours/night, children sleeping 11 ½ hours or more/night had a decreased risk for high body fat (defined as excessive fat mass >90th percentile for age and gender using BIA)_ENREF_16.32
It should be noted that three studies found that significant findings varied across gender. In a sample of 10-20-year-old twins, Yu et al. found that shortened sleep length (<8 hrs/night) was negatively associated with total body fat and truncal fat, and positively associated with percent lean body mass as measured by DEXA in females only_ENREF_44.61 Similarly, although Hitze et al. found that short sleep was associated with increased fat free mass in both genders (using air displacement plethysmography), they only found differences in percent body fat in females_ENREF_31.47
Findings regarding waist circumference and nocturnal sleep length were less consistent than above with one study finding that greater sleep duration was associated with smaller waist circumferences,49 and the three remaining studies finding significant results varying depending upon gender.37,47,61 For example, although Hitze et al. found significant findings across genders in linear analyses, when comparing short versus long sleepers, only short sleeping females had significantly larger waist circumferences_ENREF_31.47 Yu et al. also found a significant association between sleep duration and waist circumference in females only_ENREF_44.61 In contrast, Eisenmann et al. found that greater sleep duration was associated with decreased waist circumference in boys 7-16 years old, and only in 7-10-year-old girls (but not their older counterparts)37 _ENREF_21.
Additional Sleep Indices and Obesity Risk
In addition to the assessment of sleep duration, several studies assessed other sleep measures to determine whether additional sleep parameters may be associated with obesity risk. The primary variable of interest was the timing of sleep (i.e. bedtime and rise time)30,31,53,63,64, which was typically assessed with a single-item question (e.g. “over the past week, what was your typical bedtime?”). Together, these studies suggest that later bedtimes are associated with increased risk of obesity.31,53,63,64_ENREF_15 However, no association between rise time and obesity risk was found in these studies.31,53 Of note, one study with preschool-age children (3 years) found that early rise time (i.e., ≤7:00am) was associated with an increased obesity risk, but that later bedtime was not.30
In addition to bedtime and rise time, three additional studies assessed the association between irregular or problematic sleep and obesity risk. In the first study, parent report of “irregular sleep habits” at 2 to 4 years of age was independently associated with obesity risk in young adulthood (i.e., at 21 years).67 Furthermore, Wing and colleagues attempted to assess how “catching up” on sleep on weekends and holidays may influence children's risk for obesity.46 Findings suggested that compared to children who slept greater than 10 hours/night, children who persistently slept 8 hours or less on weekdays and weekends or on weekdays and during holidays, were at the greatest risk for obesity (OR adj = 2.59 [1.22-5.48] and 2.32 [1.00-5.53], respectively). In contrast to findings from these studies, after adjusting for potential confounding variables, no association was found between parent reported sleep problems (using a modified version of the Children's Sleep Habits Questionnaire) in the 3rd or 6th grades and obesity risk in the 6th grade.54
Finally, two studies assessed the association between stages of sleep and obesity risk. In the first study (which is also presented in part in the Table), Liu et al. found that reduced rapid eye movement (REM) time and reduced REM density were each associated with increased obesity risk in children 7-17 years old.43 In a second study of 52 adolescents 12-18 years who presented to a sleep clinic, greater stage 1 sleep was found for adolescents who were obese compared to those who were normal weight, and greater slow wave sleep was also found in adolescents who were categorized as overweight compared to those who were obese.68
Potential Mediators of the Sleep-Weight Association
Several studies have moved beyond documenting sleep-weight associations to examining variables (e.g. eating) that may mediate the relationship between sleep and obesity risk. For example, Landis et al. found that food cravings were higher in those with more daytime/less nocturnal sleep.69 Touchette et al found that parent report of child overeating (at 6 years old) may play a small role in the association between short sleep and BMI.56 When removed from the statistical model to predict BMI, there was a small increase in the odds for children classified as “short persistent” sleepers to be obese (see table 1). Finally, Westerlund et al. found that shorter sleep was associated with greater consumption of energy-dense foods such as pizza, pasta, and refined sugars.70 This relationship was stronger in boys and on weekdays. Additional gender differences included greater problems with waking in the morning being associated with increased intake of energy-dense foods in boys, and longer weekday sleep duration being associated with greater consumption of nutrient-dense foods (i.e., fruits and vegetables) in girls.
Discussion
Our understanding of the role of sleep duration in the current pediatric obesity epidemic is rapidly unfolding. Pediatric studies identified and included in the present review suggest that children who sleep less are at increased risk for being and/or becoming overweight/obese. This significant relationship was found in both cross-sectional and prospective studies, and persisted in most studies even after controlling for potential confounders such as parental BMI, birth weight, and television viewing. Findings from the present review are consistent with conclusions drawn from other systematic reviews and meta-analyses71-76 including two meta-analyses that demonstrated that children with “shortened sleep” were at a 56-89% increased risk for obesity.72,75 Findings also build upon previous reviews by demonstrating the potential influence of sleep length on other measures of adiposity such as waist circumference and percent body fat. The consistency in findings across anthropometric measures increases confidence in findings, and suggests that increased BMI associated with less sleep is likely due to increased deposits of adipose tissue.62
Also building upon previous work, studies included in the present review examined the association between additional sleep indices (other than sleep duration) and weight-related outcomes. Studies with school-age children and adolescents consistently found that later bedtimes were associated with increased obesity risk while rise times were unrelated.31,53,63,64 It is possible that later bedtimes are simply a proxy for shorter sleep duration, which would account for their significant association with obesity risk. However, it is also possible that circadian phase-delay may play a role in establishing risk of overweight/obesity, particularly given research suggesting the importance of circadian clocks in metabolism and obesity.77
Beyond later bedtimes, it is unclear what other sleep indices may confer obesity risk and/or protection. While findings from Wing et al. regarding the protective benefit of “catching up” on sleep on weekends and holidays are interesting, it is unclear how these findings would translate into clinical practice recommendations given the importance of consistent sleep-wake habits for the promotion of good sleep in children.46 Future studies are needed to further assess the role of “catching up” on sleep as well as the potential influence of other irregular/problematic sleep habits, including measures of sleep quality and sleep staging, on obesity risk.
An additional focus of more recent studies is attempting to better understand the potential pathways through which sleep affects BMI. These studies have focused on eating behaviors and suggest that they may be influenced by sleep duration.56,69,70 However, findings are largely limited by reliance on self-report measures, inconsistencies in findings both across and within studies, and lack of experimental manipulation of sleep duration. To strengthen confidence in the association between sleep and obesity risk via eating pathways, experimental and/or intervention research studies need to be conducted with children.
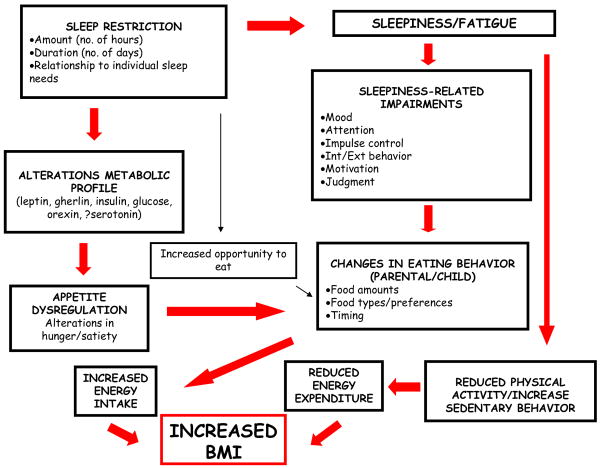
Furthermore, although change in food intake may represent one pathway through which sleep duration influences obesity risk, a number of additional pathways are possible. As shown in the Figure, a number of factors, including daytime sleepiness/fatigue and subsequent changes in activity level as well as metabolic changes may play an important role in the sleep-weight relationship. For example, cross-sectional research demonstrate that sleep is negatively impacted by engagement in sedentary activities such as television viewing,78-80 and positively associated with engagement in exercise (Chen et al., 2006). However, it remains unclear whether shortened sleep results in subsequent changes in children's activity choices. Furthermore, experimental studies with adults have demonstrated physiological changes as a result of shortened sleep, which may promote weight gain. These include changes in growth hormone, prolactin, cortisol, thyrotropin, and insulin17 as well as leptin18,19 and ghrelin20 both of which are associated with increased hunger, appetite, motivation to eat, and food intake.21-23 Studies with children in this regard are sparse, and to our knowledge, no experimental studies with children have been published. However, extant correlational research with children demonstrate an association between sleep and metabolic abnormalities, including lower fasting C-peptide,81 hyperglycemia82 as well as higher fasting insulin, peak insulin, and insulin resistance (i.e., increased HOMA-IR levels and lower WBISI levels).83 Taken together, study findings suggest the need to further explore the multiple pathways through which sleep duration influences obesity risk.
Figure 1.
Hypothesized Pathways through which Sleep Duration may Increase Obesity Risk*.
*Courtesy of Judith Owens, M.D.
Despite the consistency in findings, a number of limitations of studies should be noted. First, the reviewed studies were predominantly cross-sectional in nature. Thus, the potential causal influence of sleep duration on obesity risk cannot be established. Although six prospective studies were identified and aid in our understanding of the temporal relationship between sleep length and obesity risk, they cannot demonstrate that less sleep causes increases in weight status, and hence obesity. As noted above, future experimental research will need to be conducted prior to being able to determine causal links. Second, the measurement of sleep length in reviewed studies was primarily based on self- or parent-report, which calls into question reliability and validity of measures, particularly when single-item measures were used. Only three studies evaluated sleep length with more objective measures such as actigraphy and PSG (and were often limited by having only one day of measurement). Third, studies often used different reference values for sleep length in analyses, which makes comparisons across studies challenging. Finally, findings across studies were not always consistent across sleep categories or across gender. Inconsistencies across sleep categories may suggest that the effect of sleep on obesity risk may be small in size. However, findings regarding inconsistencies across gender are less clear since some studies found significant results in males rather than females and others found contrary results. Some of these gender differences may be due to an interaction of child gender with child age, ethnicity and/or race and pubertal status. Systematic assessment of how demographic factors may interact with sleep length in conferring obesity risk could help to explain these discrepant findings.
Taken together, study findings suggest that sleep length is associated with obesity risk. Findings also point towards changes in eating pathways that may lead to increased accumulation of adipose tissue as a potential mediator of this association. However, more research is needed to establish shortened sleep duration as a true risk factor that can be targeted in pediatric weight control interventions. Although it may not yet be prudent to prescribe changes in sleep to prevent obesity at a population level, there is ample, accumulated data, which strongly argues for systematically evaluating the potential role that enhancing sleep may have in combating the current obesity epidemic. Evidence also suggests a number of points of intervention for providers when working with children who are overweight and obese. These are highlighted below.
First, given the fact that multiple studies have shown that shortened sleep length is associated with increased BMI, assessment of sleep duration in children who are overweight and obese is important.71 Simple questions regarding obese children's sleep habits on weekdays and weekends could identify a number of children who could benefit from recommendations to obtain a good night's sleep. Given the well-documented deleterious effects of sleep on children's mood and daytime functioning, such a minimal intervention could promote a number of benefits across multiple domains. Furthermore, given the sensitive nature of addressing weight-related concerns with families, discussion of sleep may provide a nice point of entry to begin to discuss the importance of healthy lifestyles (including eating and activity behaviors) for promoting optimal health in childhood and beyond. In addition to assessment of sleep duration, providers should also consider concurrent treatment of sleep and weight problems.71 At the heart of treatments for both shortened sleep duration and overweight/obesity are the use of effective behavioral strategies, and the importance of targeting key behaviors such as television viewing.
It is clear from recent reviews, including the present one, that we are only beginning to understand the role of sleep in our current obesity epidemic. Consistency in study findings suggest that it is now time to begin to assess for sleep disturbances in children who are overweight and obese, to consider targeting sleep and obesity as comorbid conditions, and to begin to explore through experimental studies how changes in sleep length may influence obesity risk. Sleep duration represents an intriguing and potentially effective tool for promoting healthier weight in children and adolescents. It is time to move beyond epidemiological studies to further our understanding regarding how effective an approach it will be.
Acknowledgments
This work was supported in part by Grant Nos. 1-09-JF-22 from the American Diabetes Association, U01 CA150387 from the National Institutes of Health, T32 HL076134 from the National Institutes of Health.
Footnotes
The authors have nothing to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Chantelle N. Hart, Assistant Professor (Research), Department of Psychiatry & Human Behavior, The Warren Alpert Medical School of Brown University; and Staff Psychologist, Weight Control & Diabetes Research Center, The Miriam Hospital.
Alyssa Cairns, Postdoctoral Research Fellow, Department of Psychiatry & Human Behavior, The Warren Alpert Medical School of Brown University, and Weight Control & Diabetes Research Center, The Miriam Hospital.
Elissa Jelalian, Associate Professor, Department of Psychiatry & Human Behavior, The Warren Alpert Medical School of Brown University; and Staff Psychologist, Weight Control & Diabetes Research Center, The Miriam Hospital.
References
- 1.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of high body mass index in US children and adolescents, 2007-2008. Jama. 2010;303:242. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.Daniels SR. The consequences of childhood overweight and obesity. Future Child. 2006;16:47. doi: 10.1353/foc.2006.0004. [DOI] [PubMed] [Google Scholar]
- 3.Freedman DS, Dietz WH, Srinivasan SR, et al. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103:1175. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 4.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001;357:505. doi: 10.1016/S0140-6736(00)04041-1. [DOI] [PubMed] [Google Scholar]
- 5.Wardle J, Cooke L. The impact of obesity on psychological well-being. Best Pract Res Clin Endocrinol Metab. 2005;19:421. doi: 10.1016/j.beem.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 6.Jelalian E, Hart CN. Pediatric Obesity. In: Roberts MC, Steele RG, editors. Handbook of Pediatric Psychology. Fourth. New York: Guilford Press; 2009. [Google Scholar]
- 7.Services USDoHaH: Developing Healthy People 2020, in Nutrition and Weight Status. 2010 [Google Scholar]
- 8.Summerbell CD, Waters E, Edmunds LD, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev:CD001871. 2005 doi: 10.1002/14651858.CD001871.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Brown T, Summerbell C. Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obes Rev. 2009;10:110. doi: 10.1111/j.1467-789X.2008.00515.x. [DOI] [PubMed] [Google Scholar]
- 10.Oude Luttikhuis H, Baur L, Jansen H, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev:CD001872. 2009 doi: 10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Pratt JS, Lenders CM, Dionne EA, et al. Best practice updates for pediatric/adolescent weight loss surgery. Obesity (Silver Spring) 2009;17:901. doi: 10.1038/oby.2008.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iglowstein I, Jenni OG, Molinari L, et al. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003;111:302. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- 13.Dollman J, Ridley K, Olds T, et al. Trends in the duration of school-day sleep among 10- to 15-year-old South Australians between 1985 and 2004. Acta Paediatr. 2007;96:1011. doi: 10.1111/j.1651-2227.2007.00278.x. [DOI] [PubMed] [Google Scholar]
- 14.NSF. Sleep in America Poll. 2004 [Google Scholar]
- 15.Mindell J, Owens JA, editors. A clinical guide to pediatric sleep. Philadelphia: Lipincott Williams & Wilkins; 2003. [Google Scholar]
- 16.Ferber R. Childhood Sleep Disorders. Neurologic Clinics. 1996;14:493. doi: 10.1016/s0733-8619(05)70271-1. [DOI] [PubMed] [Google Scholar]
- 17.Copinschi G. Metabolic and endocrine effects of sleep deprivation. Essent Psychopharmacol. 2005;6:341. [PubMed] [Google Scholar]
- 18.Christian G, Nelson BP, Sandra M, et al. Preliminary observations on the effects of sleep time in a sleep restriction paradigm. Sleep Medicine. 2003;4:177. doi: 10.1016/s1389-9457(03)00061-3. [DOI] [PubMed] [Google Scholar]
- 19.Spiegel K, Leproult R, L'Hermite-Baleriaux M, et al. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab. 2004;89:5762. doi: 10.1210/jc.2004-1003. [DOI] [PubMed] [Google Scholar]
- 20.Taheri S, Lin L, Austin D, et al. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:210. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wren AM, Seal LJ, Cohen MA, et al. Ghrelin enhances appetite and increases food intake in humans. Journal of Clinical and Endocrinology Metabolism. 2001;86:5992. doi: 10.1210/jcem.86.12.8111. [DOI] [PubMed] [Google Scholar]
- 22.Levin F, Edholm T, Schmidt PT, et al. Ghrelin stimulates gastric emptying and hunger in normal-weight humans. J Clin Endocrinol Metab. 2006;91:3296. doi: 10.1210/jc.2005-2638. [DOI] [PubMed] [Google Scholar]
- 23.Mars M, de Graaf C, de Groot CP, et al. Fasting leptin and appetite responses induced by a 4-day 65%-energy-restricted diet. Int J Obes (Lond) 2006;30:122. doi: 10.1038/sj.ijo.0803070. [DOI] [PubMed] [Google Scholar]
- 24.Nedeltcheva AV, Kilkus JM, Imperial J, et al. Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr. 2009;89:126. doi: 10.3945/ajcn.2008.26574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brondel L, Romer MA, Nougues PM, et al. Acute partial sleep deprivation increases food intake in healthy men. Am J Clin Nutr. 2010;91:1550. doi: 10.3945/ajcn.2009.28523. [DOI] [PubMed] [Google Scholar]
- 26.Dru M, Bruge P, Benoit O, et al. Overnight duty impairs behaviour, awake activity and sleep in medical doctors. Eur J Emerg Med. 2007;14:199. doi: 10.1097/MEJ.0b013e3280bef7b0. [DOI] [PubMed] [Google Scholar]
- 27.Schmid SM, Hallschmid M, Jauch-Chara K, et al. Short-term sleep loss decreases physical activity under free-living conditions but does not increase food intake under time-deprived laboratory conditions in healthy men. Am J Clin Nutr. 2009;90:1476. doi: 10.3945/ajcn.2009.27984. [DOI] [PubMed] [Google Scholar]
- 28.Ievers-Landis CE, Redline S. Pediatric sleep apnea: implications of the epidemic of childhood overweight. Am J Respir Crit Care Med. 2007;175:436. doi: 10.1164/rccm.200606-790PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Locard E, Mamelle N, Billette A, et al. Risk factors of obesity in a five year old population. Parental versus environmental factors. Int J Obes Relat Metab Disord. 1992;16:721. [PubMed] [Google Scholar]
- 30.Sekine M, Yamagami T, Hamanishi S, et al. Parental obesity, lifestyle factors and obesity in preschool children: results of the Toyama Birth Cohort study. J Epidemiol. 2002;12:33. doi: 10.2188/jea.12.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sekine M, Yamagami T, Handa K, et al. A dose-response relationship between short sleeping hours and childhood obesity: results of the Toyama Birth Cohort Study. Child Care Health and Development. 2002;28:163. doi: 10.1046/j.1365-2214.2002.00260.x. [DOI] [PubMed] [Google Scholar]
- 32.von Kries R, Toschke AM, Wurmser H, et al. Reduced risk for overweight and obesity in 5- and 6-y-old children by duration of sleep--a cross-sectional study. International Journal of Obesity. 2002;26:710. doi: 10.1038/sj.ijo.0801980. [DOI] [PubMed] [Google Scholar]
- 33.Gupta NK, Mueller WH, Chan W, et al. Is obesity associated with poor sleep quality in adolescents? Am J Hum Biol. 2002;14:762. doi: 10.1002/ajhb.10093. [DOI] [PubMed] [Google Scholar]
- 34.Padez C, Mourao I, Moreira P, et al. Prevalence and risk factors for overweight and obesity in Portuguese children. Acta Paediatr. 2005;94:1550. doi: 10.1080/08035250510042924. [DOI] [PubMed] [Google Scholar]
- 35.Chen MY, Wang EK, Jeng YJ. Adequate sleep among adolescents is positively associated with health status and health-related behaviors. BMC Public Health. 2006;6:59. doi: 10.1186/1471-2458-6-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chaput JP, Brunet M, Tremblay A. Relationship between short sleeping hours and childhood overweight/obesity: results from the ‘Quebec en Forme’ Project. International Journal of Obesity (London) 2006;30:1080. doi: 10.1038/sj.ijo.0803291. [DOI] [PubMed] [Google Scholar]
- 37.Eisenmann JC, Ekkekakis P, Holmes M. Sleep duration and overweight among Australian children and adolescents. Acta Paediatr. 2006;95:956. doi: 10.1080/08035250600731965. [DOI] [PubMed] [Google Scholar]
- 38.Seicean A, Redline S, Seicean S, et al. Association between short sleeping hours and overweight in adolescents: results from a US Suburban High School survey. Sleep Breath. 2007;11:285. doi: 10.1007/s11325-007-0108-z. [DOI] [PubMed] [Google Scholar]
- 39.Kuriyan R, Bhat S, Thomas T, et al. Television viewing and sleep are associated with overweight among urban and semi-urban South Indian children. Nutr J. 2007;6:25. doi: 10.1186/1475-2891-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Knutson KL, Lauderdale DS. Sleep duration and overweight in adolescents: self-reported sleep hours versus time diaries. Pediatrics. 2007;119:e1056. doi: 10.1542/peds.2006-2597. [DOI] [PubMed] [Google Scholar]
- 41.Nixon GM, Thompson JM, Han DY, et al. Short sleep duration in middle childhood: risk factors and consequences. Sleep. 2008;31:71. doi: 10.1093/sleep/31.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ievers-Landis CE, Storfer-Isser A, Rosen C, et al. Relationship of sleep parameters, child psychological functioning, and parenting stress to obesity status among preadolescent children. J Dev Behav Pediatr. 2008;29:243. doi: 10.1097/DBP.0b013e31816d923d. [DOI] [PubMed] [Google Scholar]
- 43.Liu X, Forbes EE, Ryan ND, et al. Rapid eye movement sleep in relation to overweight in children and adolescents. Arch Gen Psychiatry. 2008;65:924. doi: 10.1001/archpsyc.65.8.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wells JC, Hallal PC, Reichert FF, et al. Sleep patterns and television viewing in relation to obesity and blood pressure: evidence from an adolescent Brazilian birth cohort. Int J Obes (Lond) 2008;32:1042. doi: 10.1038/ijo.2008.37. [DOI] [PubMed] [Google Scholar]
- 45.Bawazeer NM, Al-Daghri NM, Valsamakis G, et al. Sleep duration and quality associated with obesity among Arab children. Obesity (Silver Spring) 2009;17:2251. doi: 10.1038/oby.2009.169. [DOI] [PubMed] [Google Scholar]
- 46.Wing YK, Li SX, Li AM, et al. The effect of weekend and holiday sleep compensation on childhood overweight and obesity. Pediatrics. 2009;124:e994. doi: 10.1542/peds.2008-3602. [DOI] [PubMed] [Google Scholar]
- 47.Hitze B, Bosy-Westphal A, Bielfeldt F, et al. Determinants and impact of sleep duration in children and adolescents: data of the Kiel Obesity Prevention Study. Eur J Clin Nutr. 2009;63:739. doi: 10.1038/ejcn.2008.41. [DOI] [PubMed] [Google Scholar]
- 48.Jiang F, Zhu S, Yan C, et al. Sleep and obesity in preschool children. J Pediatr. 2009;154:814. doi: 10.1016/j.jpeds.2008.12.043. [DOI] [PubMed] [Google Scholar]
- 49.Ozturk A, Mazicioglu M, Poyrazoglu S, et al. The relationship between sleep duration and obesity in Turkish children and adolescents. Acta Paediatr. 2009;98:699. doi: 10.1111/j.1651-2227.2008.01169.x. [DOI] [PubMed] [Google Scholar]
- 50.Sun Y, Sekine M, Kagamimori S. Lifestyle and overweight among Japanese adolescents: the Toyama Birth Cohort Study. J Epidemiol. 2009;19:303. doi: 10.2188/jea.JE20080095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Anderson SE, Whitaker RC. Household routines and obesity in US preschool-aged children. Pediatrics. 2010;125:420. doi: 10.1542/peds.2009-0417. [DOI] [PubMed] [Google Scholar]
- 52.Reilly JJ, Armstrong J, Dorosty AR, et al. Early life risk factors for obesity in childhood: cohort study. British Medical Journal. 2005;330:1357. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Snell EK, Adam EK, Duncan GJ. Sleep and the body mass index and overweight status of children and adolescents. Child Development. 2007;78:309. doi: 10.1111/j.1467-8624.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 54.Lumeng JC, Somashekar D, Appugliese D, et al. Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics. 2007;120:1020. doi: 10.1542/peds.2006-3295. [DOI] [PubMed] [Google Scholar]
- 55.Landhuis CE, Poulton R, Welch D, et al. Childhood Sleep Time and Long-Term Risk for Obesity: A 32-Year Prospective Birth Cohort Study. Pediatrics. 2008;122:955. doi: 10.1542/peds.2007-3521. [DOI] [PubMed] [Google Scholar]
- 56.Touchette E, Petit D, Tremblay RE, et al. Associations between sleep duration patterns and overweight/obesity at age 6. Sleep. 2008;31:1507. doi: 10.1093/sleep/31.11.1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Taveras EM, Rifas-Shiman SL, Oken E, et al. Short sleep duration in infancy and risk of childhood overweight. Arch Pediatr Adolesc Med. 2008;162:305. doi: 10.1001/archpedi.162.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hui LL, Nelson EA, Yu LM, et al. Risk factors for childhood overweight in 6- to 7-y-old Hong Kong children. Int J Obes Relat Metab Disord. 2003;27:1411. doi: 10.1038/sj.ijo.0802423. [DOI] [PubMed] [Google Scholar]
- 59.Kagamimori S, Yamagami T, Sokejima S, et al. The relationship between lifestyle, social characteristics and obesity in 3-year-old Japanese children. Child Care Health Dev. 1999;25:235. doi: 10.1046/j.1365-2214.1999.00127.x. [DOI] [PubMed] [Google Scholar]
- 60.Agras WS, Hammer LD, McNicholas F, et al. Risk factors for childhood overweight: a prospective study from birth to 9.5 years. J Pediatr. 2004;145:20. doi: 10.1016/j.jpeds.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 61.Yu Y, Lu BS, Wang B, et al. Short sleep duration and adiposity in Chinese adolescents. Sleep. 2007;30:1688. doi: 10.1093/sleep/30.12.1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bayer O, Rosario AS, Wabitsch M, et al. Sleep duration and obesity in children: is the association dependent on age and choice of the outcome parameter? Sleep. 2009;32:1183. doi: 10.1093/sleep/32.9.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Maddah M, Rashidi A, Mohammadpour B, et al. In-school snacking, breakfast consumption, and sleeping patterns of normal and overweight Iranian high school girls: a study in urban and rural areas in Guilan, Iran. J Nutr Educ Behav. 2009;41:27. doi: 10.1016/j.jneb.2008.03.115. [DOI] [PubMed] [Google Scholar]
- 64.Olds T, Blunden S, Dollman J, et al. Day type and the relationship between weight status and sleep duration in children and adolescents. Australian and New Zealand Journal of Public Health. 2010;34:165. doi: 10.1111/j.1753-6405.2010.00502.x. [DOI] [PubMed] [Google Scholar]
- 65.Giugliano R, Carneiro EC. Factors associated with obesity in school children. J Pediatr (Rio J) 2004;80:17. [PubMed] [Google Scholar]
- 66.Duncan JS, Schofield G, Duncan EK, et al. Risk factors for excess body fatness in New Zealand children. Asia Pac J Clin Nutr. 2008;17:138. [PubMed] [Google Scholar]
- 67.Al Mamun A, Lawlor DA, Cramb S, et al. Do childhood sleeping problems predict obesity in young adulthood? Evidence from a prospective birth cohort study. Am J Epidemiol. 2007;166:1368. doi: 10.1093/aje/kwm224. [DOI] [PubMed] [Google Scholar]
- 68.Landis AM, Parker KP. A Retrospective Examination of the Relationship between Body Mass Index and Polysomnographic Measures of Sleep in Adolescents. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2007;40:89. doi: 10.1016/j.jadohealth.2006.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Landis AM, Parker KP, Dunbar SB. Sleep, hunger, satiety, food cravings, and caloric intake in adolescents. J Nurs Scholarsh. 2009;41:115. doi: 10.1111/j.1547-5069.2009.01262.x. [DOI] [PubMed] [Google Scholar]
- 70.Westerlund L, Ray C, Roos E. Associations between sleeping habits and food consumption patterns among 10-11-year-old children in Finland. Br J Nutr. 2009;102:1531. doi: 10.1017/S0007114509990730. [DOI] [PubMed] [Google Scholar]
- 71.Hart CN, Jelalian E. Shortened sleep duration is associated with pediatric overweight. Behav Sleep Med. 2008;6:251. doi: 10.1080/15402000802371379. [DOI] [PubMed] [Google Scholar]
- 72.Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev. 2008;12:289. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 74.Taheri S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Archives of Disease in Childhood. 2006;91:881. doi: 10.1136/adc.2005.093013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity (Silver Spring) 2008;16:265. doi: 10.1038/oby.2007.63. [DOI] [PubMed] [Google Scholar]
- 76.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 2008;16:643. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bray MS, Young ME. Circadian rhythms in the development of obesity: potential role for the circadian clock within the adipocyte. Obesity Reviews. 2007;8:169. doi: 10.1111/j.1467-789X.2006.00277.x. [DOI] [PubMed] [Google Scholar]
- 78.Adam EK, Snell EK, Pendry P. Sleep timing and quantity in ecological and family context: a nationally representative time-diary study. J Fam Psychol. 2007;21:4. doi: 10.1037/0893-3200.21.1.4. [DOI] [PubMed] [Google Scholar]
- 79.Owens J, Maxim R, McGuinn M, et al. Television-viewing habits and sleep disturbance in school children. Pediatrics. 1999;104:e27. doi: 10.1542/peds.104.3.e27. [DOI] [PubMed] [Google Scholar]
- 80.Thompson DA, Christakis DA. The association between television viewing and irregular sleep schedules among children less than 3 years of age. Pediatrics. 2005;116:851. doi: 10.1542/peds.2004-2788. [DOI] [PubMed] [Google Scholar]
- 81.Verhulst SL, Schrauwen N, Haentjens D, et al. Sleep duration and metabolic dysregulation in overweight children and adolescents. Arch Dis Child. 2008;93:89. doi: 10.1136/adc.2007.124768. [DOI] [PubMed] [Google Scholar]
- 82.Tian Z, Ye T, Zhang X, et al. Sleep duration and hyperglycemia among obese and nonobese children aged 3 to 6 years. Arch Pediatr Adolesc Med. 2010;164:46. doi: 10.1001/archpediatrics.2009.233. [DOI] [PubMed] [Google Scholar]
- 83.Flint J, Kothare SV, Zihlif M, et al. Association between inadequate sleep and insulin resistance in obese children. J Pediatr. 2007;150:364. doi: 10.1016/j.jpeds.2006.08.063. [DOI] [PubMed] [Google Scholar]