Abstract
Context
Falls cause injury and death for persons of all ages, but risk of falls increases markedly with age. Hospitalization further increases risk, yet no evidence exists to support short-stay hospital-based fall prevention strategies to reduce patient falls.
Objective
To investigate whether a fall prevention tool kit (FPTK) using health information technology (HIT) decreases patient falls in hospitals.
Design, Setting, and Patients
Cluster randomized study conducted January 1, 2009, through June 30, 2009, comparing patient fall rates in 4 urban US hospitals in units that received usual care (4 units and 5104 patients) or the intervention (4 units and 5160 patients).
Intervention
The FPTK integrated existing communication and workflow patterns into the HIT application. Based on a valid fall risk assessment scale completed by a nurse, the FPTK software tailored fall prevention interventions to address patients’ specific determinants of fall risk. The FPTK produced bed posters composed of brief text with an accompanying icon, patient education handouts, and plans of care, all communicating patient-specific alerts to key stakeholders.
Main Outcome Measures
The primary outcome was patient falls per 1000 patient-days adjusted for site and patient care unit. A secondary outcome was fall-related injuries.
Results
During the 6-month intervention period, the number of patients with falls differed between control (n=87) and intervention (n=67) units (P=.02). Site-adjusted fall rates were significantly higher in control units (4.18 [95% confidence interval {CI}, 3.45-5.06] per 1000 patient-days) than in intervention units (3.15 [95% CI, 2.54-3.90] per 1000 patient-days; P=.04). The FPTK was found to be particularly effective with patients aged 65 years or older (adjusted rate difference, 2.08 [95% CI, 0.61-3.56] per 1000 patient-days; P=.003). No significant effect was noted in fall-related injuries.
Conclusion
The use of a fall prevention tool kit in hospital units compared with usual care significantly reduced rate of falls.
Falls are a public health problem worldwide.1,2 Hospitalization increases fall risk3 because of the unfamiliar environment, illnesses, and treatments. Patient falls and fall-related injuries are devastating to patients, clinicians, and the health care system. A single fall may result in a fear of falling4 and begin a downward spiral of reduced mobility, leading to loss of function and greater risk of falls. Older adults are more likely to be injured from a fall.5 Injurious falls increase hospital costs and lengths of stay.5,6
Fall risk assessment and health information technology (HIT) have been underused in fall prevention efforts. Fall risk assessment provides a baseline measure of risk status to guide interventions to counteract identified risks.7 Currently, insufficient evidence exists to link specific fall prevention protocols with decreased fall rates in short-stay hospitals.7-9 The Institute of Medicine reported on the significant number of errors that occur in hospitals and advocates for the use of HIT.10 HIT improves communication and facilitates information access and decision support.11 To date, no reports of HIT applications to reduce patient falls have been published.
We developed a fall prevention tool kit (FPTK) that used a valid fall risk assessment scale as the foundation for a HIT application that provides fall prevention decision support and communication at the bedside. We used a randomized study design to test the effectiveness of the FPTK on patient fall rates in 4 short-stay hospitals.
METHODS
A cluster randomized study was conducted at 4 hospitals in the Partners HealthCare System in the Boston, Massachusetts, area. Initial work standardized fall risk assessment to use of the Morse Falls Scale (MFS).12,13 The MFS has been prospectively validated in inpatient settings and meets established standards for clinical credibility, accuracy, and generality necessary for adoption.14
Preliminary Work
Our research team conducted 3 phases of study to develop and test components of the FPTK. In phase 1, we used qualitative inquiry to identify barriers and facilitators to fall risk communication and interventions. Participants reported that alerts related to patient-specific fall risk status and interventions to prevent falls were unavailable yet clearly needed at the bedside.15
In phase 2, the study team developed the prototype FPTK by using the MFS risk factors12,13 as the foundation for the initial template. Decision rules and interventions were based on evidence from the literature and findings from phase 1 interviews. The MFS (scores range from 0-125) consists of 6 risk foci: (1) recent history of falling (25 points); (2) presence of secondary diagnosis (eg, >1 medical diagnosis listed in patient record) (15 points); (3) need for ambulatory aid (0-30 points); (4) receiving intravenous therapy (20 points); (5) gait characteristics (0-20 points); and (6) impaired mental status (15 points). An illustrator was added to the study team to develop icons to address the need for bedside alerts while simplifying and standardizing communication across stakeholders, including those with low literacy levels.16
In phase 3, we used an iterative process involving domain experts, end users, and an illustrator to identify valid icons for the FPTK. The 11 icons that received the highest ratings for congruence with the text of the fall risk and prevention plan were retained to populate the FPTK (eFigure 1; available at http://www.jama.com).17 The final FPTK included the MFS (Figure 1) that, when completed, automatically presented corresponding interventions tailored to patient-specific areas of risk. Once the recommended interventions were reviewed, tailored if needed, and approved, the FPTK printed a bed poster, a patient education handout, and a plan of care (eFigure 2).
Figure 1.
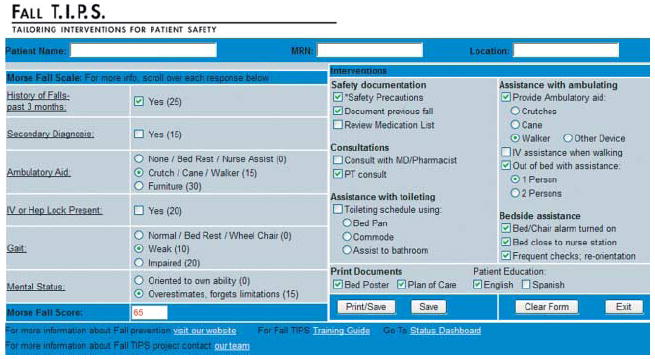
Fall Prevention Tool Kit User Interface
Reproduced with permission from Partners HealthCare System.
Study Design
In phase 4, a cluster randomized design was conducted to test the FPTK. We identified unit census, length of stay, and historical data on fall rates. Medical units with fall rates higher than the mean for the institution the year before the study were matched to units with similar fall rates and patient-days. Units were eligible if they had a match and were not involved in other performance improvement efforts specific to fall prevention. A total of 2 medical units from each hospital met these criteria. Patient fall was defined as an “unplanned descent to the floor during the course of their hospital stay.”18 At each hospital, the 2 matched units were randomized to be the intervention or control unit (Figure 2). The study protocol and waiver of informed consent were approved by the institutional review boards at each hospital. All patients admitted or transferred to selected units from January 1, 2009, through June 30, 2009, were included in the study.
Figure 2.
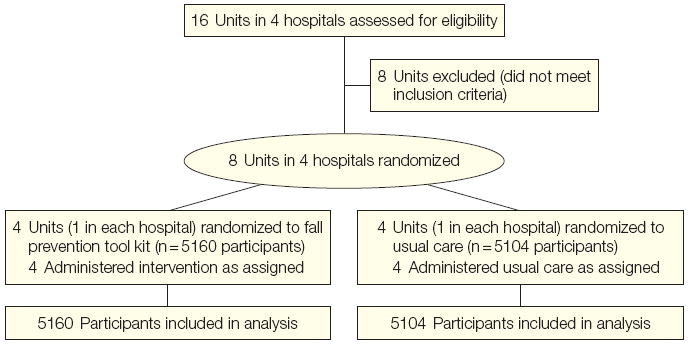
Flow of Hospital Units and Patients
FPTK Intervention
We developed the FPTK software. Figure 1 illustrates the 6-item MFS and specific fall prevention interventions based on a hypothetical patient’s fall risk. To overcome the lack of effectiveness in recent randomized controlled trials of fall prevention, we used the Institute for Healthcare Improvement’s Framework for Spread19 to promote unit-level buy-in.20,21 The FPTK included an adherence dashboard to facilitate monitoring.
Control units continued to provide usual care related to fall prevention. An educational program on fall risk assessment and prevention was used in the control units. Fall prevention education for clinicians has been found to be effective in the short term but not over time.22 The fall prevention protocols in control vs intervention units are compared in Table 1.
Table 1.
Fall Prevention Tool Kit (FPTK) Protocol in Control and Intervention Units
| Control Units (Usual Care) | Intervention Units (FPTK) | |
|---|---|---|
| Fall risk assessment (at admission, daily, and with change in status) | Complete Morse Falls Scale (MFS)16,17 using existing paper or electronic forms. | Complete MFS using FPTK. Evidence-based/feasible interventions are automatically selected and tailored by nurse based on knowledge of patient. |
| Bedside alert to all stakeholders | Place generic “high risk for falls” sign above bed for patients scoring >45 on MFS. | Tailored bed poster automatically prints and is placed above bed for all patients at risk; updated with change in status. |
| Patient education (control and intervention materials available in English and Spanish) | Educate patient/family members, providing booklets or other handouts as needed. | Educate patient/family members using tailored handout (automatically prints, updated with change in status). |
| Documentation of fall prevention plan | Document plan manually in paper or electronic record. | Tailored plan is automatically generated by FPTK from fall risk assessment. |
Outcomes
The primary outcome was patient falls per 1000 patient-days in targeted units during the study period. A secondary outcome was patient falls with injury. Reporting of patient falls and injurious falls is required at all hospitals and routinely recorded in an event reporting system in all units by the clinician caring for the patient at the time of a fall. Incidents are validated by unit managers and hospital quality personnel. Patient demographic characteristics were collected at admission to each hospital. Standard federal race and ethnicity data23 are self-reported by all patients and entered into the health care system database.
Statistical Analysis
We used a stratified, cluster randomization design, with the randomized intervention at the unit (cluster) level within hospital (strata) and falls measured at the patient level. The trial consisted of 2 units (clusters) within each of 4 hospitals (strata). Main end points were the number of falls per 1000 patient-days in the 2 study groups and fall-related injuries as a secondary outcome. Because randomization was implemented within a hospital, the hospital was controlled for in the statistical analysis when comparing rates of falls and falls with injury across the 2 study conditions. Thus, to test for differences in the rate of falls across the intervention and control groups, our a priori Poisson regression model contained an intervention effect and fixed effects for hospitals. Generalized estimating equation methods were used to test for any residual effect of clustering within unit after controlling for hospital.
Patient characteristics across treatment groups were calculated using proportions, means with standard deviations, and medians with interquartile ranges. Because randomization was at the cluster level (and there were only 8 clusters), patient-level characteristics would not be as likely to balance out as randomization would at the patient level. Covariate balance was checked using a stratified Wilcoxon test24 (with hospitals as strata) for continuous confounders (eg, age), and fixed-effects multinomial logistic regression (with site as fixed effect) for categorical confounders (eg, insurance status); both analyses were also adjusted for any possible clustering within unit. All reported P values are 2-sided and P<.05 is considered statistically significant. Because of the small number of a priori tests performed for the main outcome (comparison of fall rates between treatment groups), no adjustments were made for multiple testing. Statistical analyses were performed with the use of SAS software, version 9.2 (SAS Institute Inc, Cary, North Carolina).
Our target sample was 5100 patients in each group (1275 patients in each of the 8 units), estimated to provide 80% power (with α=.05) to detect a decrease in the fall rate from 4.8 falls per 1000 patients-days in the usual care group to 3.5 falls per 1000 patient-days (based on preliminary data obtained from quality departments at each hospital) in the intervention group using generalized estimating equations Poisson regression with fixed effects for hospital and an intracluster (within-unit) correlation of 0.0000001.
RESULTS
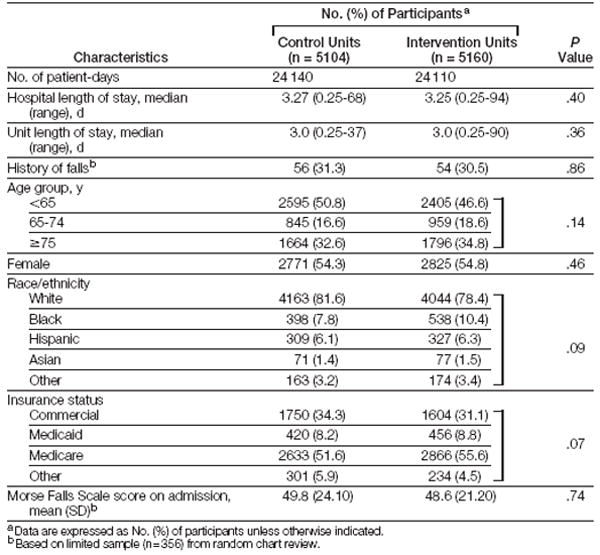
The study involved 10 264 patients and 48 250 patient-days. No units withdrew from the study. Patient characteristics are summarized in Table 2. Patients in control and intervention units were similar, but patients in the control units were more likely to be younger and of white race and to have commercial insurance. Although none of these differences were significant, we adjusted for potential confounders (Table 2) that had P=.05 to P=.10. We also adjusted for trend by month of the study. Patients in control and intervention units had similar fall risk scores at admission (49.8 and 48.6 of a possible 0-125; P=.74). There were no differences in length of stay or sex. Since these possible confounders were not significant, we did not adjust for them when comparing the main outcome across study groups. Slightly more than half (51.3%) of patients were aged 65 years or older. The mean age among patients aged 65 years or older was 78.8 (SD, 8.4) years and among patients younger than 65 years was 47.9 (SD, 11.9) years.
Table 2.
Participant Characteristics
|
Adherence to the protocol was measured through random assessment of MFS25 completion in control units and the use of FPTK components (including MFS completion) in intervention units. The percentage of adherence to daily MFS completion was 81% in control units and 94% in intervention units. Fall prevention tool kit outputs were printed for 93.2% of patients, with 89% adherence in placing the bed poster above the patient’s bed.
There were fewer patients with falls in intervention units (n=67; range across units, 10-28) than in control units (n=87; range across units, 15-33) (Table 3). Furthermore, the intervention units had a significantly lower adjusted2 fall rate (3.15 [95% confidence interval {CI}, 2.54-3.90] per 1000 patient-days) than control units (4.18 [95% CI, 3.45-5.06] per 1000 patient-days), with a rate difference of 1.03 (95% CI, 0.57-2.01) per 1000 patient-days (P=.04). We hypothesized (post hoc) that the intervention effect may be stronger in older patients. Testing an interaction between age and treatment group, we found that the intervention effect in older patients was significantly different than in younger patients (P=.02). In particular, we found that patients aged 65 or older benefited most from the FPTK (adjusted rate difference, 2.08 [95% CI, 0.61-3.56] per 1000 patient-days; P=.003). Although fewer falls occurred overall in intervention units, this difference was noted only for patients aged 65 years or older, in whom it was found to be significant. One older patient in an intervention unit and 2 in control units experienced a repeat fall (P=.50), and fall-related injuries were experienced by 7 in the intervention units vs 9 in the control units (P=.66), but neither of these differences were statistically significant.
Table 3.
Participant Falls and Adjusted Fall Rates in Control vs Intervention Units
| Control Units | Intervention Units | Rate Difference | P Value | |
|---|---|---|---|---|
| All patients | ||||
| Baseline fall rate per 1000 patient-daysa,b | 5.56 | 5.85 | -0.29 | .61 |
|
| ||||
| No. of patients with falls/total No. of patients | 87/5104 | 67/5160 | .02 | |
|
| ||||
| Total No. of falls | 89 | 71 | ||
|
| ||||
| No. of repeat falls | 2 | 4 | .46 | |
|
| ||||
| Fall rate (95% CI) per 1000 patient-daysb | 4.64 (3.86 to 5.57) | 3.48 (2.83 to 4.28) | 1.16 (0.17 to 2.16) | .04 |
|
| ||||
| Fall rate (95% CI) per 1000 patient-days adjusted for site, sex, race, insurance, age | 4.18 (3.45 to 5.06) | 3.15 (2.54 to 3.90) | 1.03 (0.57 to 2.01) | .04 |
|
| ||||
| Observed No. of falls with injury | 12 | 14 | .64 | |
|
| ||||
| Patients aged <65 y | ||||
| Baseline fall rate per 1000 patient-daysa,b | 4.93 | 4.73 | 0.20 | .81 |
|
| ||||
| No. of patients with falls/total No. of patients | 36/2595 | 33/2405 | .72 | |
|
| ||||
| Total No. of falls | 36 | 36 | ||
|
| ||||
| No. of repeat falls | 0 | 3 | .23 | |
|
| ||||
| Fall rate (95% CI) per 1000 patient-daysb | 4.02 (2.96 to 5.46) | 4.02 (2.93 to 5.54) | 0.00 (-1.72 to 1.70) | .99 |
|
| ||||
| Fall rate (95% CI) per 1000 patient-days adjusted for site, sex, race, insurance | 3.76 (2.66 to 5.30) | 3.72 (2.60 to 5.32) | 0.04 (-1.56 to 1.63) | .97 |
|
| ||||
| Observed No. of falls with injury | 3 | 7 | .20 | |
|
| ||||
| Patients aged ≥65 y | ||||
| Baseline fall rate per 1000 patient-daysa,b | 5.22 | 5.97 | -0.75 | .34 |
|
| ||||
| No. of patients with falls/total No. of patients | 51/2509 | 34/2755 | .004 | |
|
| ||||
| Total No. of falls | 53 | 35 | ||
|
| ||||
| No. of repeat falls | 2 | 1 | .50 | |
|
| ||||
| Fall rate (95% CI) per 1000 patient-daysb | 5.05 (3.74 to 6.83) | 2.76 (1.94 to 3.93) | 2.29 (0.63 to 3.95) | .005 |
|
| ||||
| Fall rate (95% CI) per 1000 patient-days adjusted for site, sex, race | 4.75 (3.44 to 6.54) | 2.66 (1.87 to 3.80) | 2.08 (0.61 to 3.56) | .003 |
|
| ||||
| Observed No. of falls with injury | 9 | 7 | .66 | |
July-September 2008.
Fall rate is site-adjusted.
Based on our results, the FPTK can prevent 1 fall per 862 patient-days (eg, the number needed to treat is 287 patients during a typical 3-day stay). There are two 862-patient-day periods each week in the 8 study units (control and intervention). Therefore, the FPTK could potentially prevent 1 fall every 4 days, 7.5 falls each month, and about 90 falls each year in the study units alone.
COMMENT
To our knowledge, this is the first fall prevention clinical trial that provides evidence for using a specific HIT intervention to reduce falls in short-stay hospitals. In intervention units, the mean adjusted fall rate per 1000 patient-days (3.15) declined to less than the Massachusetts state mean (3.99),26 while mean fall rates in control units remained slightly higher (4.18). The variability of fall rates in medical units in hospitals reported in the literature makes it difficult to estimate how the patient fall rates in this study or the mean rates in Massachusetts compare with rates in medical units reported in the literature nationally (5.09-6.64)5 or internationally (1.09-9.26).27-29
Older age increases risk of falls,30 and patient fall rates are generally higher in geriatric and general medical units than in surgical units.29 The effectiveness of the FPTK in older patients provides evidence that a HIT program that tailors interventions to address patient-specific determinants of risk and is implemented within existing workflows is effective in acute care hospitals with older adults.
Because patient falls in hospitals are a major risk factor for fractures and other injuries, reducing falls is an important first step toward injury prevention, and any reduction in patient falls has clinical significance. The FPTK was designed specifically to reduce falls. We believe that reducing falls will ultimately reduce injury, but the FPTK was not designed to affect fall-related injury directly. Additional work is needed to identify the barriers and facilitators of fall-related injury prevention and to identify a set of interventions to target determinants of risk of fall with injury.
In developing the FPTK intervention, we found that inadequate communication contributes to incomplete understanding of fall risk status15 and the fall prevention plan, consistent with results previously reported.31 Specifically, 20% of nurse-generated solutions to prevent patient falls in hospitals relate to inadequate caregiver communication and 13% relate to inadequate assessment and reassessment of fall risk status. While fall risk screening is a common practice in hospitals, the use of patient-specific screening results to tailor a prevention plan is less frequent.9 The FPTK standardized communication of risk status and made the fall prevention plan available at the bedside.
A major component of the FPTK is the 3-item output to communicate both fall risk alerts and actions to take to prevent falls (eFigure 2): (1) the over-bed poster; (2) the patient/family education handout (tailored plan and interventions at a consumer level of literacy); and (3) the plan of care (tailored plan and interventions at a health care professional level of literacy). These outputs are available to all key stakeholders, are located where they are needed, and are immediately visible through the use of icons and plaintext language so that alerts can be quickly recognized and acted on by team members. Of the 11 icons used to populate the FPTK, 3 communicate how the patient toilets. An additional 5 icons illustrate the type of assistance needed to get out of bed to toilet (eFigure 1). In one community hospital, 45.2% of falls were related to toileting.32 Bedside alerts that communicate safe toileting strategies tailored to the needs of individual patients are particularly important for preventing falls in older adults, in whom toileting-related falls are most common and more likely to result in injury.33
Using the Institute for Healthcare Improvement’s Framework for Spread to implement the FPTK enhanced its adoption and adherence.25 Other investigators have found that staff champions are essential to changing the practices needed to reduce patient falls.34 The lack of effectiveness in recent trials of fall prevention programs highlights the significant role of local buy-in.20,21,27 We agree with Tinetti35 that direct management by local caregivers is paramount to the success of fall prevention interventions. However, a mechanism is needed to ensure the fidelity of the intervention. The lack of efficacy related to the results of a recent evaluation of a fall prevention program was attributed to considerable discrepancy between the “ideal” (the intervention as planned by the researchers) and the implemented (what actually was carried out by those implementing the experiment) versions of the same program.21 Fall prevention programs must be consistent with existing workflows, and tools are needed, like the FPTK dashboard, to support ongoing evaluation of the protocol.
This study has limitations. It was conducted in 4 hospitals within a single health care system. However, the hospitals were diverse (2 academic medical centers and 2 community teaching hospitals). We believe that including hospitals with diverse clinical information and documentation systems enhanced the FPTK generalizability. No differences were found in patient characteristics across units. These complex medical patients are anticipated to be similar to medical patients in other US hospitals. An increased emphasis on fall prevention brought about by the knowledge that costs of fall-related injury would not be reimbursed36 may have contributed to an overall downward trend in fall rates noted in this study. However, because this same safety emphasis and reimbursement issue was consistent across both study groups and the rate difference remained significantly larger in the experimental units when adjusted for trend by month of study in the analysis (1.03 [95% CI, 0.57-2.01] per 1000 patient-days; P=.04), it was not considered to be a limitation.
The intervention was not blinded, and falls were reported by unit-based caregivers who implemented fall prevention interventions. Although this potentially introduces bias, we believe that using existing reporting mechanisms that were the same in control and intervention units and were validated by the quality departments at each hospital limits this potential source of bias.
The FPTK was not effective with younger patients. The overall fall rate did not differ in this group, and patients younger than 65 years in intervention units had more falls with injury and more repeat falls than patients in control units (although the differences were not significant). These preliminary findings beg the question of whether the FPTK should be applied solely to elderly patients. However, hospitalization places all patients at risk of falls.3 Fall risk assessment is completed in all patients. When identified, clinicians have an obligation to mitigate risk. Additional research is called for to evaluate whether a different set of interventions are needed to diminish fall and injury risk in younger patients or whether care team members may be less likely to carry out recommended interventions on younger patients. Protocol adherence data were collected at the unit level. While overall adherence was high, we do not know if adherence differed between younger and older patients. This possibility will need to be evaluated in future work. One of the benefits of information technology is that once the appropriate interventions are identified, logic can be programmed into the system to offer decision support tailored to patient characteristics.
The final limitation is that the sample size did not have sufficient power to examine whether the FPTK was effective in preventing repeat falls or falls with injury. Our goal was to test the capacity of the FPTK intervention to prevent falls. There is much concern related to the recent decision by the Centers for Medicare and Medicaid Services to include patient falls among the hospital-acquired conditions that will no longer qualify for higher-paying diagnosis-related group reimbursement.36 This study provides some initial evidence regarding a strategy for reducing preventable falls in hospitals in older patients. However, the FPTK interventions are designed specifically to prevent falls. Additional work is needed to identify interventions that reduce fall-related injuries and trauma. Moreover, the FPTK did not prevent repeat falls, although the numbers were small. As with falls with injury, an additional set of interventions may be needed to protect patients who fall in the hospital despite the presence of a tailored communication and intervention plan.
In summary, the results of our study indicate that a HIT intervention targeting underlying areas of risk can prevent patient falls in older patients in acute care hospitals. Further study is needed to determine if a similar program evaluated over a longer period of time can significantly reduce repeat falls. Moreover, work is needed to develop a set of interventions that will prevent fall-related injuries. However, the FPTK was effective at reducing numbers of falls in intervention vs control units.
Acknowledgments
Funding/Support: This work was supported by a grant from the Robert Wood Johnson Foundation Interdisciplinary Nursing Quality Research Initiative (Translating Fall Risk Status Into Interventions to Prevent Patient Falls).
Role of the Sponsor: The Robert Wood Johnson Foundation had no role in the design and conduct of the study; collection, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Drs Dykes and Lipsitz had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Dykes, Carroll, Hurley, Lipsitz, Middleton.
Acquisition of data: Dykes, Hurley, Benoit, Chang, Meltzer, Tsurikova, Zuyov.
Analysis and interpretation of data: Dykes, Carroll, Hurley, Lipsitz.
Drafting of the manuscript: Dykes, Carroll, Hurley, Lipsitz.
Critical revision of the manuscript for important intellectual content: Dykes, Carroll, Hurley, Lipsitz, Benoit, Chang, Meltzer, Tsurikova, Zuyov, Middleton.
Statistical analysis: Lipsitz.
Obtained funding: Dykes, Carroll, Hurley, Middleton. Administrative, technical, or material support: Dykes, Hurley, Benoit, Chang, Meltzer, Tsurikova, Zuyov, Middleton.
Study supervision: Dykes, Middleton.
Additional Contributions: We thank the Partners Healthcare System Chief Nurse Council, the Partners Healthcare System Fall Prevention Task Force, and the nurses, clinical staff, and patients who participated in this study for their support of development and testing of the FPTK. In addition, we thank John S. Dykes, BFA, for icon development and design.
Financial Disclosures: None reported.
Online-Only Materials: eFigures 1 and 2 are available online at http://www.jama.com.
References
- 1.Chen LH, Warner M, Fingerhut L, Makuc D. Injury episodes and circumstances: National Health Interview Survey, 1997-2007. Vital Health Stat 10. 2009;10(241):1–55. [PubMed] [Google Scholar]
- 2.Kannus P, Sievänen H, Palvanen M, Järvinen T, Parkkari J. Prevention of falls and consequent injuries in elderly people. Lancet. 2005;366(9500):1885–1893. doi: 10.1016/S0140-6736(05)67604-0. [DOI] [PubMed] [Google Scholar]
- 3.Evans D, Hodgkinson B, Lambert L, Wood J. Falls risk factors in the hospital setting: a systematic review. Int J Nurs Pract. 2001;7(1):38–45. doi: 10.1046/j.1440-172x.2001.00269.x. [DOI] [PubMed] [Google Scholar]
- 4.Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45(6):239–243. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]
- 5.Krauss MJ, Nguyen SL, Dunagan WC, et al. Circumstances of patient falls and injuries in 9 hospitals in a Midwestern healthcare system. Infect Control Hosp Epidemiol. 2007;28(5):544–550. doi: 10.1086/513725. [DOI] [PubMed] [Google Scholar]
- 6.Bates DW, Pruess K, Souney P, Platt R. Serious falls in hospitalized patients: correlates and resource utilization. Am J Med. 1995;99(2):137–143. doi: 10.1016/s0002-9343(99)80133-8. [DOI] [PubMed] [Google Scholar]
- 7.Oliver D, Hopper A, Seed P. Do hospital fall prevention programs work? a systematic review. J Am Geriatr Soc. 2000;48(12):1679–1689. doi: 10.1111/j.1532-5415.2000.tb03883.x. [DOI] [PubMed] [Google Scholar]
- 8.Cameron ID, Murray GR, Gillespie LD, et al. Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database Syst Rev. 2010;(1):CD005465. doi: 10.1002/14651858.CD005465.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Coussement J, De Paepe L, Schwendimann R, Denhaerynck K, Dejaeger E, Milisen K. Interventions for preventing falls in acute- and chronic-care hospitals: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56(1):29–36. doi: 10.1111/j.1532-5415.2007.01508.x. [DOI] [PubMed] [Google Scholar]
- 10.Kohn L, Corrigan J, Donaldson M. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 1999. [PubMed] [Google Scholar]
- 11.Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med. 2003;348(25):2526–2534. doi: 10.1056/NEJMsa020847. [DOI] [PubMed] [Google Scholar]
- 12.Morse JM. Preventing Patient Falls: Establishing a Fall Intervention Program. Vol. 2. New York, NY: Springer; 2008. [Google Scholar]
- 13.Morse JM, Morse RM, Tylko SJ. Development of a scale to identify the fall-prone patient. Can J Aging. 1989;8(4):366–377. [Google Scholar]
- 14.Oliver D, Daly F, Martin FC, McMurdo ME. Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age Ageing. 2004;33(2):122–130. doi: 10.1093/ageing/afh017. [DOI] [PubMed] [Google Scholar]
- 15.Dykes PC, Carroll DL, Hurley AC, Benoit A, Middleton B. Why do patients in acute care hospitals fall? can falls be prevented? J Nurs Adm. 2009;39(6):299–304. doi: 10.1097/NNA.0b013e3181a7788a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Payne PR, Starren JB. Quantifying visual similarity in clinical iconic graphics. J Am Med Inform Assoc. 2005;12(3):338–345. doi: 10.1197/jamia.M1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hurley AC, Dykes PC, Carroll DL, Dykes JS, Middleton B. Fall TIP: validation of icons to communicate fall risk status and tailored interventions to prevent patient falls. Stud Health Technol Inform. 2009;146:455–459. [PMC free article] [PubMed] [Google Scholar]
- 18.Joint Commission. National Quality Forum (NQF) endorsed nursing-sensitive care performance measures. [April 11, 2010]; http://www.jointcommission.org/performancemeasurement/measurereservelibrary/nqf_nursing.htm.
- 19.Massoud M, Nielsen G, Nolan K, Schall M, Sevin C. A Framework for Spread: From Local Improvements to System-Wide Change. Cambridge, MA: Institute for Healthcare Improvement; 2006. [April 11, 2010]. http://www.ihi.org/IHI/Results/WhitePapers/AFrameworkforSpreadWhitePaper.htm. [Google Scholar]
- 20.Elley CR, Robertson MC, Garrett S, et al. Effectiveness of a falls-and-fracture nurse coordinator to reduce falls: a randomized, controlled trial of at-risk older adults. J Am Geriatr Soc. 2008;56(8):1383–1389. doi: 10.1111/j.1532-5415.2008.01802.x. [DOI] [PubMed] [Google Scholar]
- 21.Hendriks MR, Bleijlevens MH, van Haastregt JC, et al. Lack of effectiveness of a multidisciplinary fall-prevention program in elderly people at risk: a randomized, controlled trial. J Am Geriatr Soc. 2008;56(8):1390–1397. doi: 10.1111/j.1532-5415.2008.01803.x. [DOI] [PubMed] [Google Scholar]
- 22.Krauss MJ, Tutlam N, Costantinou E, Johnson S, Jackson D, Fraser VJ. Intervention to prevent falls on the medical service in a teaching hospital. Infect Control Hosp Epidemiol. 2008;29(6):539–545. doi: 10.1086/588222. [DOI] [PubMed] [Google Scholar]
- 23.US Food and Drug Administration. Guidance for Industry Collection of Race and Ethnicity Data in Clinical Trials. Rockville, MD: US Food and Drug Administration; 2005. p. 18. [Google Scholar]
- 24.Klein JP, Moeschberger ML. Survival Analysis: Techniques for Censored and Truncated Data. New York, NY: Springer-Verlag; 1997. [Google Scholar]
- 25.Dykes PC, Carroll DL, Hurley A, et al. Fall TIPS: strategies to promote adoption and use of a fall prevention tool kit. AMIA Annu Symp Proc. 2009;2009:153–157. [PMC free article] [PubMed] [Google Scholar]
- 26.Massachusetts Hospital Association Patient Care Link. Patient falls per 1000 patient days June 2008-June 2009. [April 11, 2010]; http://www.patientcarelink.org/hospital-data/performance-measures.aspx.
- 27.Cumming RG, Sherrington C, Lord SR, et al. Prevention of Older People’s Injury Falls Prevention in Hospitals Research Group. Cluster randomised trial of a targeted multifactorial intervention to prevent falls among older people in hospital. BMJ. 2008;336(7647):758–760. doi: 10.1136/bmj.39499.546030.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koh SL, Hafizah N, Lee JY, Loo YL, Muthu R. Impact of a fall prevention programme in acute hospital settings in Singapore. Singapore Med J. 2009;50(4):425–432. [PubMed] [Google Scholar]
- 29.Schwendimann R, Bühler H, De Geest S, Milisen K. Falls and consequent injuries in hospitalized patients: effects of an interdisciplinary falls prevention program. BMC Health Serv Res. 2006;6:69. doi: 10.1186/1472-6963-6-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lakatos BE, Capasso V, Mitchell MT, et al. Falls in the general hospital: association with delirium, advanced age, and specific surgical procedures. Psychosomatics. 2009;50(3):218–226. doi: 10.1176/appi.psy.50.3.218. [DOI] [PubMed] [Google Scholar]
- 31.Tzeng HM, Yin CY. Nurses’ solutions to prevent inpatient falls in hospital patient rooms. Nurs Econ. 2008;26(3):179–187. [PubMed] [Google Scholar]
- 32.Tzeng HM. Understanding the prevalence of in-patient falls associated with toileting in adult acute care settings. J Nurs Care Qual. 2010;25(1):22–30. doi: 10.1097/NCQ.0b013e3181afa321. [DOI] [PubMed] [Google Scholar]
- 33.Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med. 2004;19(7):732–739. doi: 10.1111/j.1525-1497.2004.30387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gutierrez F, Smith K. Reducing falls in a definitive observation unit: an evidence-based practice institute consortium project. Crit Care Nurs Q. 2008;31(2):127–139. doi: 10.1097/01.CNQ.0000314473.72001.b4. [DOI] [PubMed] [Google Scholar]
- 35.Tinetti ME. Multifactorial fall-prevention strategies: time to retreat or advance. J Am Geriatr Soc. 2008;56(8):1563–1565. doi: 10.1111/j.1532-5415.2008.01800.x. [DOI] [PubMed] [Google Scholar]
- 36.Inouye SK, Brown CJ, Tinetti ME. Medicare nonpayment, hospital falls, and unintended consequences. N Engl J Med. 2009;360(23):2390–2393. doi: 10.1056/NEJMp0900963. [DOI] [PubMed] [Google Scholar]


