Abstract
Aim
This paper is a report of the development and testing of the Self-Efficacy for Preventing Falls Nurse and Assistant scales.
Background
Patient falls and fall-related injuries are traumatic ordeals for patients, family members and providers, and carry a toll for hospitals. Self-efficacy is an important factor in determining actions persons take and levels of performance they achieve. Performance of individual caregivers is linked to the overall performance of hospitals. Scales to assess nurses and certified nursing assistants’ self-efficacy to prevent patients from falling would allow for targeting resources to increase SE, resulting in improved individual performance and ultimately decreased numbers of patient falls.
Method
Four phases of instrument development were carried out to (1) generate individual items from eight focus groups (four each nurse and assistant conducted in October 2007), (2) develop prototype scales, (3) determine content validity during a second series of four nurse and assistant focus groups (January 2008) and (4) conduct item analysis, paired t-tests, Student’s t-tests and internal consistency reliability to refine and confirm the scales. Data were collected during February–December, 2008.
Results
The 11-item Self-Efficacy for Preventing Falls Nurse had an alpha of 0·89 with all items in the range criterion of 0·3–0·7 for item total correlation. The 8-item Self-Efficacy for Preventing Falls Assistant had an alpha of 0·74 and all items had item total correlations in the 0·3–0·7 range.
Conclusions
The Self-Efficacy for Preventing Falls Nurse and Self-Efficacy for Preventing Falls Assistant scales demonstrated psychometric adequacy and are recommended to measure bedside staff’s self-efficacy beliefs in preventing patient falls.
Keywords: falls, hospital, instrument development, nursing, safety, self-efficacy
Introduction
Patient falls are serious and long-standing problems in acute care hospitals with published reports in the nursing literature dating from 1979 (Walshe & Rosen 1979). Falls on hospital medical units have been reported to be as high as almost 3% (Vassallo et al. 2000). Falls are devastating to patients, family members, providers and the healthcare system with 34% of falls leading to injury and 6% to serious injury (Fischer et al. 2005).
There are abundant opinion reports on why hospitalized patients fall, tools to facilitate categorization of patients into high risk or low risk for falling, scales to identify specific risk factors for falling, and strategies to prevent patients from falling. Yet, almost 30 years since the first paper on falls in hospitalized patients (Walshe & Rosen 1979), falls remain a significant human ordeal for patients. Falls are also financially costly to hospitals as the Centers for Medicare and Medicaid Services do not reimburse hospitals for additional costs to care for fall-related injuries (Inouye et al. 2009).
Risks for falling
Being hospitalized increases the risk for falls (Evans et al. 2001) secondary to the unfamiliar environment, acute illness, surgery, bed rest, medications, treatments and the placement of various tubes and catheters. Advancing age is another risk as patients aged between 76 and 85 years have a fivefold risk of falling compared with younger hospitalized patients (Halfon et al. 2001). Older adults are more likely to sustain injuries with falls (Schwendimann et al. 2006, Krauss et al. 2007) and injurious falls drive up hospital costs and length of stay (Bates et al. 1995).
The higher risk older adults have for falling while hospitalized is compounded by the fact that the elderly are the fastest growing segment of the population. In general, hospitals have long been considered dangerous places for elderly patients (Cassel 2004). A single fall may result in a fear of falling (Tinetti et al. 1990) that can begin a downward spiral of reduced mobility, leading to loss of function and further risk for falls.
There are many published articles describing risk factors for falling and suggesting tools for assessing fall risk. In a systematic review of 47 such reports, two scales, the Morse Fall Scale (MFS) (Morse 1997) and STRATIFY (Oliver et al. 1997) fulfilled the criteria of prospective validation with adequate sensitivity/specificity values (Oliver et al. 2004). The MFS consists of six areas of risk and STRATIFY consists of five factors independently related to a high risk of falling. When similar items are combined, there is a parsimonious list of eight fall risk factors: (1) recent history of falling or fall as a presenting complaint, (2) presence of secondary diagnosis, (3) need for ambulatory aid, (4) receiving intravenous therapy, (5) gait problems or transfer or mobility problem, (6) impaired mental status or patient agitation assessed by a nurse who knows the patient well, (7) need for frequent toileting and (8) visual impairment. However, risk assessment alone does not prevent falls. Interventions prevent falls.
Fall prevention
Many resources have been devoted to fall prevention as evidenced in three decades of reports of fall prevention research. However, several systematic reviews published in the last few years were largely inconclusive in their overall findings of the efficacy of interventions to reduce fall rates in residential care, nursing home and hospital facilities (Oliver et al. 2007, Coussement et al. 2008, Cusimano et al. 2008, Cameron et al. 2010). Post hoc subgroup analyses in these reviews revealed that two individual components of multifactorial interventions, vitamin D supplementation and supervised exercise, were effective (Cameron et al. 2010). However, positive effects of these interventions are unlikely to be realized during a typical 4-day hospitalization when patients are focused on recovering from surgery or from an acute medical problem. Results from the few studies on fall prevention programmes specific for hospitals have been unsuccessful in identifying interventions to keep patients from falling (Schwendimann et al. 2006, Krauss et al. 2008).
Why patients fall
Patients fall for a variety of reasons. Data from eight focus groups [four RN and four certified nursing assistants (CNAs)] revealed six major reasons why patients fall: (1) inadequate patient report, (2) lack of information access, (3) poor signage, (4) unsafe environment, (5) lack of teamwork and (6) not involving the patient and family (Dykes et al. 2009). Patients could have prevented some falls and staff could have prevented other falls.
Patients
When surveyed, older adults suggested that their balance, inattention and medical conditions were the most frequent reasons for falls (Zecevic et al. 2006). When interviewed about a recent fall in the hospital, the major reason patients said they fell was the need to use the toilet coupled with loss of balance and unexpected weakness (Carroll et al. in press). Older females were not willing to face their risk of falling, and often rejected fall prevention advice because they saw it as a threat to their autonomy and identity (McInnes & Askie 2004).
Staff
Bedside caregivers are the second line of defence for fall prevention, by helping patients do what they would do if they had the capability (Henderson 1977). Morse reported that 78% of patient falls can be categorized as having an ‘anticipated physiological’ cause, meaning that a known physiological cause has placed the patient at increased risk for falling (Morse 1997). Regrettably, after staff evaluate hospitalized patients’ risk of falling, very often, strategies that would counteract those risk factors are not carried out (Oliver et al. 2004). Interventions that are written on a care plan, but not implemented properly, do not prevent falls (Hendriks et al. 2008).
Background
A safety platform
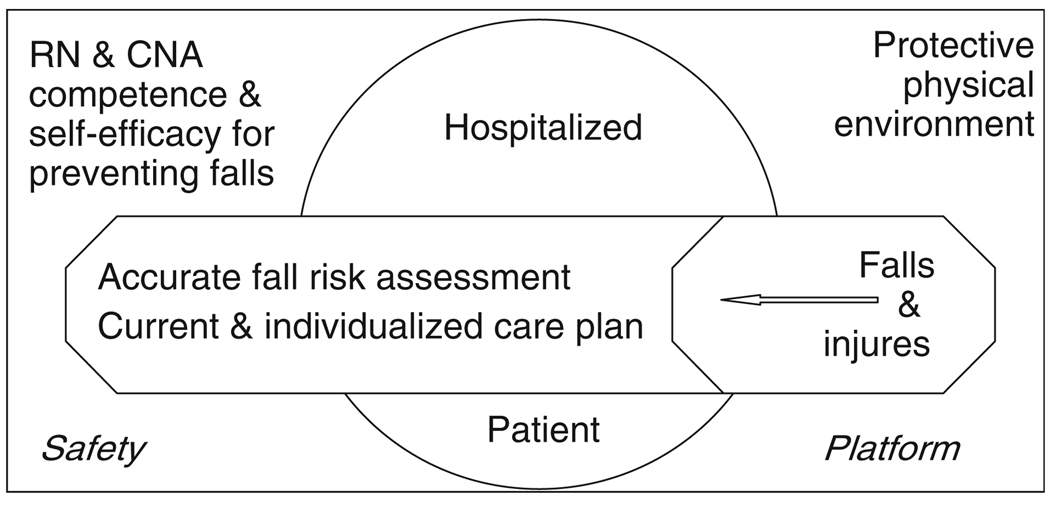
We developed a model to depict how the patient, caregivers and environment are crucial to prevent falls. We modified the Home Safety/Injury Model (Hurley et al. 2004) used to guide research to make homes safer for persons with Alzheimer’s disease (Horvath et al. 2005) and a working model to frame patient safety initiatives in hospitals (Kruger et al. 2006) to illustrate a safety platform for protecting patients from falls and fall-related injuries (Figure 1). The patient is in the centre. A patient care plan including current and accurate fall risk status with associated tailored and feasible interventions needs to be easily and immediately accessible to the entire healthcare team, patients and family (Dykes et al. 2009).
Figure 1.
Safety platform for protecting patients from falls and injuries.
The safety platform consists of two components, a protective physical environment and bedside caregivers who have both competence and SE beliefs in their ability to prevent falls. A protective physical environment includes having immediate access to necessary assistive devices and the presence of safe surroundings without unsafe conditions, e.g. call bell close at hand, a clear path to the bathroom, bed alarm if needed, durable call light pull-cords in the bathroom, intravenous poles with a wide base of support, and no frayed carpet, hazardous floor treads, or floor washing when patients are likely to be in that area (Kruger et al. 2006).
Bedside caregiver competence means that RNs and CNAs have the knowledge and skills needed to carry out the care plan. RNs and CNAs must know (1) the patient’s specific risk factors for falling, (2) explicit interventions to decrease, manage or ameliorate those risks and (3) how to carry out those prescribed interventions. RNs and CNAs must be proficient in the actions they take to prevent patient falls. However, knowing exactly what to do and having the capacity to do it capably are insufficient in preventing falls. RNs and CNAs must expend the degree of effort required and be persistent in carrying out necessary actions to prevent patients from falling. Self-efficacy beliefs determine the magnitude of effort persons will employ and how long they will persevere in their actions, in this case, to prevent patients from falling.
Self-efficacy and patient falls
Self-efficacy
The self-efficacy (SE) concept was first proposed by Bandura (1977) to understand why persons would engage in certain behaviours to achieve their goals. SE is the major concept in social cognitive theory (Bandura 1986) and is concerned with the actions that people take rather than the outcomes that are expected to follow. The first scales to operationalize and measure SE were used to study phobic behaviour(Bandura et al. 1977, 1982), hypertension (Rudd et al. 2004), chronic illness management (Lorig et al. 2001) and caregiving (Steffen et al. 2002). Bandura (1986) suggested that SE was a powerful psychosocial variable capable of predicting the enactment of health-related behaviours, which several decades of research have so confirmed. SE research, summarized in nine meta-analyses from diverse methodological and analytic strategies, has affirmed the central role of SE in influencing actions (Bandura & Locke 2003).
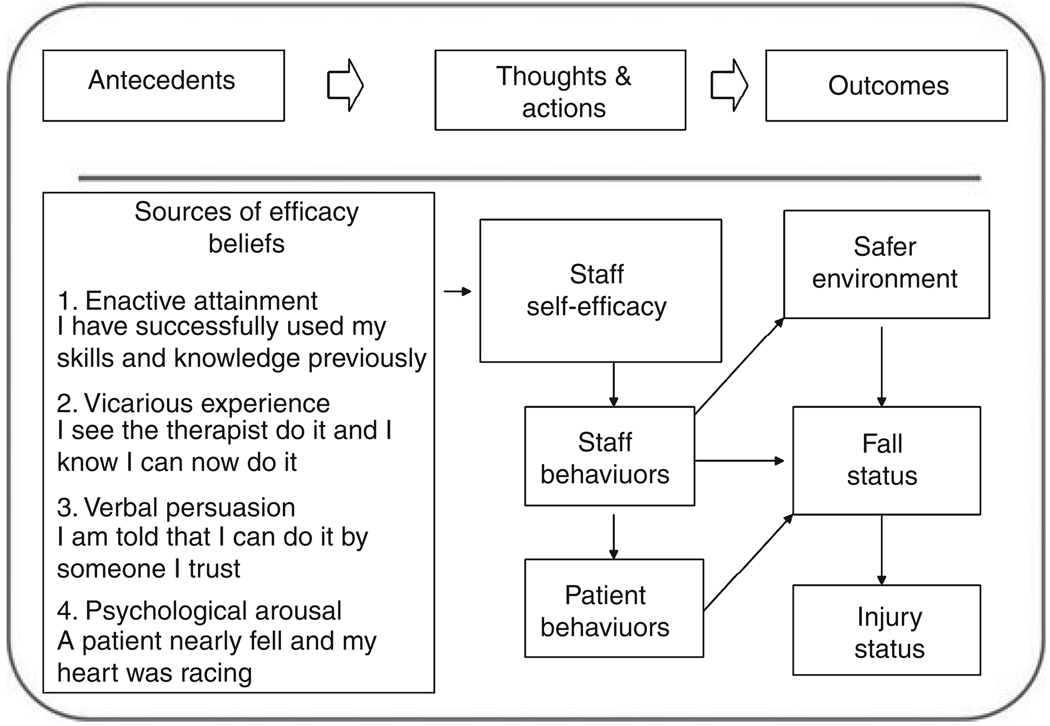
SE is a belief in one’s capability to carry out actions necessary to meet given situational demands. RNs and CNAs, who have high levels of SE for preventing falls, will work hard and persist in carrying out necessary actions to prevent patients from falling. Persons who perceive themselves as efficacious are confident in their ability and expend sufficient effort to achieve a certain level of performance. This performance, when well executed, results in successful outcomes. Findings from a meta-analysis of 114 studies of SE for work-related performance revealed that SE was positively and strongly related to work performance, moderated by task complexity – so that the relationship is the strongest for lower levels of task complexity (Stajkovic & Luthans 1998). Actions required to prevent patients from falling are not complex; e.g. the patient needs two helpers to transfer from bed, requires a bed-alarm, and voids by using a commode at the bedside. SE for the work-related performance of carrying out actions to prevent falls is important because bedside RNs and CNAs are in key positions to prevent falls and thus, fall-related injury (see Figure 2).
Figure 2.
SE for the work-related performance of carrying out actions to prevent falls.
Determinates of self-efficacy
Persons develop their SE beliefs from four hierarchically ordered sources (Bandura 1986). (1) Enactive attainment is a mastery experience, ‘success breeds success’. (2) Vicarious experience is a process of self-comparison to a peer. (3) Verbal persuasion is listening to something that alters one’s confidence. (4) Physiological arousal is a physical indicator given by the person’s own body. Fall prevention examples are used in Figure 2 to illustrate the four determinants of SE.
RN and CNA SE for fall prevention was the only component of the safety platform (Figure 1) lacking in a quantification method. For this study, SE for preventing falls means confidence in one’s ability to prevent patients from falling.
The study
Aims
The purpose of this study was to develop and test the Self Efficacy for Preventing Falls – Nurse (SEPFN) and Self Efficacy for Preventing Falls – Assistant (SEPFA) scales to allow hospital leaders to quantify bedside staffs’ SE beliefs in preventing patient falls.
Methodology
Four phases of investigation were carried out to develop and test individual items and the SEPFN and SEPFA scales. Procedures based on classical measurement theory (Waltz et al. 2005) were employed to assure empirical, conceptual and psychometric adequacy. Established criteria were followed to ensure that both individual items and the SEPFN and SEPFA scales would be: (1) empirically grounded (Tinetti et al. 1990), (2) judged to have content validity (CV; Waltz et al. 2005), (3) accepted by RNs and CNAs (Wyatt & Altman 1995) and (4) reliable by meeting accepted standards of internal consistency (Nunnally & Bernstein 1994).
Ethical considerations
Institutional Review Board (IRB) approval was received at the original four sites to conduct group interviews and to use web-based and paper surveys. Separate IRB approval was obtained at the additional sites for the survey phase using electronic dissemination via institutional listservs.
Each participant in the focus groups obtained verbal consent. Implied consent was provided for completing the surveys. Survey instructions included the sentences: ‘This project has received approval from the Human Research Committee. Responding to these items indicates that you recognize this is a research project in which you have volunteered to participate. You may skip any items you choose not to answer’.
Four study phases
Participants from four acute hospitals, two urban academic medical centres (800–1000 licensed beds) and two suburban teaching hospitals (250–500 licensed beds) in the same hospital system, took part in phases one, three and four. These non-profit hospitals had no religious affiliation. Three additional hospital sites (non-profit, no religious affiliation, 250–500 licensed beds) were included in phase four (reliability testing). There were missing work site data on 199 RN participants and 171 CNA participants.
Phases one and three were qualitative descriptive components of the overall study. Participants were recruited from medical units in the four acute hospitals with mean fall rates higher than the hospital mean. RN and CNA potential participants were identified by nursing leadership who recommended potentially ‘good informants’, RNs and CNAs nurses who had both experienced the phenomena (in this case, being successful or not in preventing patients from falling) and could articulate their experiences (Morse 1987). Additional participants were recruited by flyers, e-mail and personal invitation. Informed consent was provided.
Phase one
Data (collected in October, 2007) obtained from four RN and four CNA audio-taped focus style group interviews (Dykes et al. 2009) were used to construct the qualitative database. A combination of pre-planned questions, e.g. ‘How do you know if a patient is at risk for falling?’ ‘How do you know what to do to prevent patient falls?,’ requests for clarification, e.g. ‘help me understand’ and ‘tell me more about’, and group discussion was used.
Interviews were transcribed verbatim into a word processing package, reviewed/corrected for transcription accuracy and removal/masking of any identifying characteristics of patients or providers, and converted into NVIVO for coding and support of qualitative analysis. We used a two-person consensus for identification of participants’ text to be considered for the item pools following basic content analysis methods (Miles & Huberman 1994).
Phase two
Three nurse members of the research team (PD, DC, AH) with knowledge of professional practice issues surrounding hospital-based care and an understanding of the complex, technical and interdisciplinary care required by patients in which preventing falls is one of many safety concerns, identified statements to be considered for the SEPFN and SEPFA (December, 2007). Guided by the definition of self-efficacy for preventing falls, items were combined, refined, and edited until consensus was reached for 37 SEPFN and 33 SEPFA items.
Phase three
A second series of four RN and four CNA focus groups were held (data collected in January, 2008). Participants used a four-point scale to rate each item for CV and relevance with the definition of SEPF. As the paired t-test statistic was to be used in phase-four, an additional assessment was conducted to test participants’ understanding of and ability to follow instructions to create a private identifier, called the ‘SUM’ to match participants’ surveys. The ‘SUM’, used in our previous research with only nurses (Hurley et al. 2006, 2007), is the last four digits of participants’ social security number added to the last four digits of participants’ home telephone number.
Participants were given verbal instructions and score sheets for rating items’ CV and writing their ‘SUM’. In the CNA focus groups, there were several participants who could not complete the ‘SUM’ and additional participants who did not have the English reading capacity to complete the CV rating form independently. Refinement of items and instructions was guided by group discussions to assure credibility (Wyatt & Altman 1995). Learning empirically from potential endpoint users, items and scale administration procedures were revised and found acceptable.
The 90% average congruency percentage standard was used to retain items. A 21-item SEPFN and 22-item SEPFA resulted and constituted the prototype scales. The confidential indicator was expanded to allow respondents to select the ‘SUM’ or a familiar word they would remember; e.g. the street where they grew up, favourite pet, etc. We learned that CNAs with low English literacy would need an alternative to SEPFA self-administration on a website to take part in phase-four.
Phase four
Reliability testing was accomplished in this final phase (data collected April–August, 2008). A six-point Likert scoring system anchored with descriptors (completely confident) and (not at all confident) was used. Two identical SEPFN and SEPFA prototypes, with all positively worded items (to be reverse-scored) and instructions for creating a confidential identifier using a word or numbers, were uploaded to SurveyMonkey, a web-based survey tool. The time-1 link was disseminated to collect data through electronic dissemination via institutional listservs. Print copies were provided as requested and research staff uploaded the data into the SurveyMonkey database. A week later, the time-2 link was e-mailed and print copies were distributed as requested and uploaded to collect data for examining re-test stability.
RNs and CNAs who provide direct bedside care were sought for reliability testing using a snowball sampling method. A recruitment email with the link to the T-1 SEPFN and SEPFA surveys and instructions was sent to collaborators at the four original sites, to other local hospitals and to contacts through the Health Information Management System Society Nursing Informatics Task Force. The email was forwarded with the survey link using local listservs and printed copies of the scales were provided to allow CNAs the option of taking the SEPFA on paper privately or receiving assistance to use the paper version.
Data from printed versions were entered onto the form into the SurveyMonkey database. The complete data sets were downloaded from SurveyMonkey and converted to SPSS (Chicago, IL, USA) for the analysis.
Decision rules
Decision rules were established to guide the analysis to retain only well performing individual items to assure both reliable items and parsimonious and psychometrically adequate scales that could detect overall differences in SE for preventing falls. T1 groups (G) were randomly divided into two (G1, G2) to examine the data and make item reduction decisions with G1 and evaluate psychometric properties with G2. A data set of participants with identical confidential identifiers in T1 and T2 (matched) was used to examine item stability. Three iterative decision rules were followed to delete poorly performing items if: (1) ≥80% participants (G1 data sets) did not score the item (not credible) or scored ‘strongly agree’ (lack of differentiation capacity), (2) < 0·5 Pearson correlation (matched data sets) and/or the probability of the t-value < 0·1 (not highly correlated and/or dissimilar means – indicating lack of item stability evidenced by different scores for the same item when responded to at a 2-week interval) and (3) internal consistency reliability examination by item-total correlation (G1 data sets) of < 0·3 (poor fit) or > 0·7 (redundant).
After deleting poorly performing items following the sequence of the decision rules described above, both the retained items and SEPFN and SEPFA were evaluated. Mean scores were used; the theoretical range is 1 (not at all confident) to 6 (completely confident) in ability to prevent patients from falling. Scales were evaluated for internal consistency (G1) and stability (matched data sets). The final examination consisted of a Student’s t-test to compare G1 and G2 data sets. SEPF scales’ descriptive data and variability were computed using the complete T1 data sets.
Sample/participants
A total of 36 RNs participated in phases one and three and 562 RNs responded to the T-1 survey, of whom 73 provided confidential identifiers and were included in the matched data set. A total of 27 CNAs participated in phases one and three and 269 CNAs responded to the T-1 survey, of whom 83 provided confidential identifiers and were included in the matched data set. Demographic characteristics are provided for the total T1 RN and CNA respondents only as matched participants were drawn from those groups and there were no differences between those participants who provided a confidential identifier and those who did not. Table 1 compares RN study participants with the most recent survey of United States of America (USA) RNs (U.S. Department of Health and Human Services, HRSA, BuHP, & Division of Nursing, 2010) and Table 2 compares CNA study participants with available CNA national data (Squillace et al. 2009).
Table 1.
Comparison of RN study participants with RNs in USA employed in hospitals*
| Study participants | |||
|---|---|---|---|
| RNs in USA employed in hospitals in 2008 |
|||
| Phases 1 and 3 |
Phase 4 | ||
| Number | 36 | 562 | 1,615,085 |
| Age in years | Median = 44 | Median = 40 | Mean = 47·0 |
| Percentage of male | 6 | 15 | Not reported† |
| Percentage of non-Caucasian race/ethnicity | 9 | 15 | 16·9 |
| Percentage with BS/BSN or higher | 81 | 68 | 50·7 |
The report states ‘While predominately White and female… (p. 11), but the 2008 report did not provide data on gender’. The previous statistics on gender from the registered nurse work force using 2004 data reported that 5.8% employed nurses were male (U.S. Department of Health and Human Services, HRSA, BuHP, & Division of Nursing 2004).
Table 2.
Comparison of CNA study participants with CNAs employed in USA nursing homes
| Study participants | |||
|---|---|---|---|
| Estimates*from CNAs working in US nursing homes in 2004 |
|||
| Phases 1 and 3 | Phase 4 | ||
| Number | 27 | 269 | 3017 |
| Age in years | 26–69, Median = 44 | 17–69, Median = 36 | <25–≥55, Median = 38 |
| Percentage of male | 18 | 11 | 8 |
| Percentage of non-Caucasian | 75 | 46 | 47 |
| Years of education | 4–18 years, Median = 12 | 6–16 years, Median = 13.5 | 68% ≥high school |
| Years of CNA experience | <1–40 years, Median = 10 | <1–42 years, Median = 7 | 54% = 6–>20 years |
| Years of experience at site | <1–31 years, Median = 7 | <1–42 years, Median = 4 | Median = 2·4 years |
Estimates* = Nationally representative survey (Squillace et al. 2009). (1) Site selection. 1500 nursing homes randomly selected from 16,628 in the US licensed for ≥3 beds and certified by Medicare or Medicaid or licensed by the sate. (2) Respondents. Of 4542 sampled CNAs, 3017 (71%) completed an interview.
A greater percentage of RN study participants in all phases had a baccalaureate degree and were younger than RNs employed in US hospitals. A greater percentage of CNA study participants in phases one and three were not Caucasian, were older and had more experience at their work site than CNA participants in phase four had.
Instruments/results
Ten SEPFN items were deleted because they did not achieve the criteria of decision rules one and two by not being credible, lacking differentiation capacity, or being unstable. The final 11-item SEPFN (Table 3) achieved high internal consistency levels when examined with G1 (N = 281, α= 0·87, all items in the 0·3–0·7 criterion for item total correlation) and G2 (N = 281, α = 0·90, all items in the 0·3–0·7 criterion for item total correlation) samples. During the 10 days between the test and retest, SEPFN scores increased slightly by 0·12 on the 6-point scale, but the difference was not statistically significant (r = 0·81, P = 0·000; t = 1·7, P = 0·09); scores were highly correlated and had similar means. The t-test comparing G1 and G2 groups was not statistically significant (t = 0·46, P = 0·69), indicating that the mean scores of 5·09 and 5·07 were similar. The overall alpha was 0·89 (Mean = 5·1, sd = 0·8, Median = 5·27).
Table 3.
Self-efficacy for preventing falls – nurse (11-item SEPFN, N = 562)
| No. | I am confident about my ability to prevent patients from falling because |
ITC | X̄* | sd |
|---|---|---|---|---|
| 1 | I receive a verbal report about my patients’ fall risk | 0·7 | 4·7 | 1·4 |
| 2 | The nurse from the previous shift tells me what to do to prevent my patients from falling | 0·7 | 4·3 | 1·5 |
| 3 | I have easy access to information about why patients are at risk to fall | 0·6 | 5·1 | 1·1 |
| 4 | I have easy access to information on how to prevent patients from falling | 0·6 | 5·2 | 1·0 |
| 5 | I do a fall risk assessment during my shift | 0·4 | 5·7 | 0·8 |
| 6 | I work with families/visitors to carry out the fall prevention plan | 0·5 | 5·2 | 1·0 |
| 7 | I give nursing assistants face-to-face report about their patients’ fall risk | 0·7 | 5·1 | 1·2 |
| 8 | I give nursing assistants face-to-face information about how to prevent their patients from falling | 0·7 | 5·1 | 1·2 |
| 9 | I give a fall risk report to the next shift | 0·7 | 5·3 | 1·1 |
| 10 | I tell the nurse on the next shift what to do to prevent our patients from falling | 0·7 | 4·9 | 1·3 |
| 11 | We all work together as a team | 0·4 | 5·4 | 0·9 |
ITC = item total correlation.
Range = 1 (lowest) to 6 (highest).
Fourteen SEPFA items were deleted because they were not credible, lacked differentiation capacity, or were unstable (decision rules one and two). The final 8-item SEPFA (Table 4) achieved acceptable internal consistency levels when examined with G1 (N = 135, α = 0·69, slightly lower than the 0·7 criterion (Nunnally & Bernstein 1994) for a new scale,) all items in the 0·3–0·7 criterion for item total correlation) and G2 (N = 134, α = 0·78, all items in the 0·3–0·7 criterion for item total correlation) samples. Mean SEPFA scores increased slightly by 0·07 on the 6-point scale in the 12 days between the test and retest, but the difference was not statistically significant (r = 0·87, P = 0·000; t = 1·5, P = 0·11), revealing scale stability. G1 and G2 mean scores were each 5·1; the t-test comparing groups was not statistically significant (t = 0·06, P = 0·95). See Table 4 for the variability of individual items and overall SEPFA summary statistics. The overall SEPFA alpha was 0·74, Mean = 5·1, sd = 0·7, median = 5·25.
Table 4.
Self-efficacy for preventing falls – assistant (8-item SEPFA, N = 269)
| No. | I am confident about my ability to prevent patients from falling because |
ITC | X̄* | sd |
|---|---|---|---|---|
| 1 | I receive a verbal report about my patients’ fall risk | 0·6 | 4·8 | 1·4 |
| 2 | The nurse tells me what to do to prevent my patients from falling | 0·6 | 4·6 | 1·5 |
| 3 | I write down information about my patients’ fall risk | 0·4 | 4·8 | 1·6 |
| 4 | I go to the nurse and ask what I should do to prevent a patient from falling | 0·5 | 4·9 | 1·5 |
| 5 | I have all the equipment my patients need to prevent them from falling | 0·4 | 5·7 | 0·5 |
| 6 | I make sure that there is a clear path to the bathroom | 0·4 | 5·0 | 1·2 |
| 7 | I answer any call light rapidly | 0·4 | 5·6 | 0·5 |
| 8 | We all work together as a team | 0·3 | 5·2 | 1·2 |
ITC, item total correlation.
Range = 1 (lowest) to 6 (highest).
Discussion
Many aspects of preventing falls in acute care hospitals present some degree of difficulty. Patients are not admitted to hospitals to be prevented from falling, but are admitted and treated for health problems serious enough to require acute care hospitalization. Preventing patients from falling is just one of many actions staff perform as they provide care and very comprehensive therapeutic interventions to extremely ill patients who typically have several comorbid conditions.
Limitations
Phases one and three were conducted with RNs and CNAs from one healthcare system. However, the four units where study RNs and CNAs worked provided care for sick adult medical patients who were presumably similar to medical patients cared for in USA acute care hospitals vs. patients requiring speciality/intensive care.
Non-probability sampling methods were employed to recruit participants in all phases. The sample may not be representative of all bedside RNs and CNAs. Limitations associated with internet surveys are well known, including sampling bias and inability to calculate a response rate (Wyatt 2000).
There were age, gender, race/ethnicity and educational differences between RNs in the two qualitative phases, the reliability testing survey phase, and employed in USA hospitals in 2008 (U.S. Department of Health and Human Services et al., 2010). We could find no data on the relationship of gender, or race/ethnicity or educational level and self-efficacy for any type of work-related performance. Although SE has been found to influence academic achievement in school (Bandura et al. 1996), it remains unknown if a higher level of education would influence work-related SE. It is known that patient outcomes are better for those hospitals with high rates of nurses with a baccalaureate degree (Aiken et al. 2003, Kutney-Lee & Aiken 2008). We recognize this educational difference, but believe that study results are generalizable to hospital-based RNs because we were not seeking the application of a complex nursing judgment, but SE beliefs in preventing patients from falling and SE for work-related performance are stronger when related actions are not complex (Stajkovic & Luthans 1998).
CNAs in the two qualitative phases were older, more likely to be male and not Caucasian, and had more work experience at their current hospital than CNAs in the reliability testing survey phase and CNAs employed in USA nursing homes in 2004 had (Squillace et al. 2009). However, we are not aware if these demographic characteristics influence SE for fall prevention.
Conclusion
Suggestions for using the SEFPN and SEPFA scales
Both individual items and the scale totals can be used to assess RNs and CNAs SE for preventing hospitalized patients from falling and should be tested with RNs and CNAs in other settings where patients may fall. For example, the item ‘I am confident in my ability to prevent patients from falling because we all work together as a team’ is in both SEPFN and SEPFA scales, has satisfactory psychometric properties, and could be one way to evaluate the efficacy of a fall prevention programme that incorporated team building. If health information technology is used to streamline fall risk communication for nurses, the items concerning confidence in ability because of having easy access to information about why a patient is at risk to fall and how to prevent a patient from falling could be used as an evaluation mechanism.
What is already known about this topic
Patient falls are traumatic for patients, their families and care providers. Patient falls, a measure of hospital quality, constitute serious problems in acute care hospitals, which may result in hospitals not being reimbursed for fall-related costs.
Self-efficacy (SE) is related to work performance by determining the amount of effort persons will take to accomplish specific actions, which if carried out correctly, lead to higher levels of individual achievement. Work-related performance of individuals is linked to the overall performance of the work site.
What this paper adds
The methods for assessing RNs’ and CNAs’ self-efficacy beliefs about their ability to prevent patients from falling allow for quantifying the self-efficacy concept for preventing patient falls and testing the safety platform model.
Implications for practice and/or policy
Use of the SEPFN and SEPFA scales can identify RNs and CNAs with high and low self-efficacy for preventing falls; the former can act as role models for the latter group to assist in invoking two sources of efficacy beliefs, enactive attainment and verbal persuasion.
Both scales and selected individual items may be used as outcome measures to evaluate staff education or fall prevention programmes.
Additional suggested research
Testing the SEPFN and SEPFA scales
We recommend that additional psychometric testing be performed with larger samples in different hospitals and in settings such as long-term/residential care settings where older patients reside, to ensure that both individual items and the scales are relatively stable. The elderly are at more risk for falling while hospitalized and suffering greater negative consequences from falling than younger patients. Older patients are living longer lives and have very complex health needs, and there may not be adequate numbers of healthcare providers with the knowledge and skills to care for them adequately (Institute of Medicine, 2010). The recent Institute of Medicine report, ‘Retooling for an aging America: Building the health care workforce’ (Institute of Medicine, 2010), stated that all providers need to have the core competencies in caring for older persons during general training, lifelong, and when needed. The SEPFN and SEPFA are two new resources to use to promote the goal of fall and injury prevention and should be examined in all sites where RNs and CNAs provide care.
Additional research
We recommend that the safety platform model developed for this project (Figure 1) be examined. The two new scales can measure RN and CNA SE for fall prevention. RN and CNA competency can be tested by standardized evaluations of knowledge, e.g. RNs at the health system where phases one and three were conducted must demonstrate accurate use of the MFS (Morse 1997) annually. The degree to which the environment is protective can be examined by using patient safety walk rounds (Frankel et al. 2003). Medical record audits can identify the completion of fall risk assessments and subsequent fall prevention interventions and the degree to which interventions are carried out. Particular attention should be given to the hospitalized elderly as they are at great risk for falling and are the fastest growing segment of the population.
Interventions examined in previous fall prevention research that looked promising, but did not achieve statistical significance in the hospital setting for reducing falls, should be re-tried with the addition of RN SE for preventing falls. For example, the results of a recent evaluation of a multifactorial fall prevention programme were attributed to considerable discrepancy between the intervention planned by the researchers and what actually was carried out by those persons implementing the experiment (Hendriks et al. 2008). It is important that the persons who implement fall prevention interventions maintain the necessary degree of effort required to carry out the protocol accurately and persist in their actions to do so.
In summary, the SEPFN and SEPFA scales are suggested for use in any site where fall prevention is a goal. We hope that suggestions for future research will help solve the serious problem of falls in hospitalized patients.
Acknowledgments
Funding
This study was supported by the Brigham and Women’s Hospital Center for Nursing Excellence, the Brigham and Women’s Hospital Lily Kravitz Nursing Studies Award, Brigham and Women’s Hospital Department of General Medicine, and the Robert Wood Johnson Foundation Interdisciplinary Nursing Quality Research Initiative.
Footnotes
Author contributions
PCD, DLC and ACH were responsible for the study conception and design, drafting of the manuscript. PCD, DLC, KM, LC and LZ performed the data collection. PCD, DLC, ACH, SRL and BM performed the data analysis. KM, SRL, LC, LZ and BM made critical revisions to the paper for important intellectual content. LZ provided statistical expertise. PCD, DLC, ACH and BM obtained funding. KM and LZ provided administrative, technical or material support. PCD and ACH supervised the study.
Conflict of interest
No conflict of interest has been declared by the authors.
Contributor Information
Patricia C. Dykes, Clinical Informatics Research and Development, Partners HealthCare System, Boston, Massachusetts, USA.
Diane Carroll, Munn Center for Nursing Research, Massachusetts General Hospital, Boston, Massachusetts, USA.
Kerry McColgan, Clinical Informatics Research and Development, Partners HealthCare System, Boston, Massachusetts, USA.
Ann C. Hurley, Brigham and Women’s Hospital, Center for Nursing Excellence, Boston, Massachusetts, USA.
Stuart R. Lipsitz, Department of General Medicine, Brigham and Women’s Hospital, Boston, Massachusetts, and, Harvard Medical School, Boston, Massachusetts, USA.
Lisa Colombo, Health Alliance Hospitals, Milton, Massachusetts, USA.
Lyubov Zuyev, Massachusetts General Hospital, Boston, Massachusetts, USA.
Blackford Middleton, Clinical Informatics Research and Development, Partners HealthCare System, Department of General Medicine, Brigham and Women’s Hospital, Boston, Massachusetts, USA.
References
- Aiken LH, Clarke SP, Cheung RB, Sloane DM, Silber JH. Educational levels of hospital nurses and surgical patient mortality. Journal of the American Medical Association. 2003;290:1617–1623. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- Bandura A, Locke EA. Negative self-efficacy and goal effects revisited. Journal of Applied Psychology. 2003;88:87–99. doi: 10.1037/0021-9010.88.1.87. [DOI] [PubMed] [Google Scholar]
- Bandura A, Adams N, Beyer J. Cognitive processes mediating behavioral change. Journal of Personality and Social Psychology. 1977;35:125–139. doi: 10.1037//0022-3514.35.3.125. [DOI] [PubMed] [Google Scholar]
- Bandura A, Adams N, Beyer J. Microanalysis of action and fear arousal as a function of differential levels of perceived self-efficacy. Journal of Personality and Social Psychology. 1982;43:5–21. doi: 10.1037//0022-3514.43.1.5. [DOI] [PubMed] [Google Scholar]
- Bandura A, Barbaranelli C, Caprara GV, Pastorelli C. Multifaceted impact of self-efficacy beliefs on academic functioning. Child Development. 1996;67:1206–1222. [PubMed] [Google Scholar]
- Bates DW, Pruess K, Souney P, Platt R. Serious falls in hospitalized patients: correlates and resource utilization. The American Journal of Medicine. 1995;99:137–143. doi: 10.1016/s0002-9343(99)80133-8. [DOI] [PubMed] [Google Scholar]
- Cameron ID, Murray GR, Gillespie LD, Robertson MC, Hill KD, Cumming RG, Kerse N. Interventions for preventing falls in older people in nursing care facilities and hospitals [Systematic Review] Cochrane Database of Systematic Reviews. 2010;1 doi: 10.1002/14651858.CD005465.pub2. CD005465. [DOI] [PubMed] [Google Scholar]
- Carroll DL, Dykes PC, Hurley AC. Patients’ perspectives of falling while in an acute care hospital and suggestions for prevention. Applied Nursing Research. doi: 10.1016/j.apnr.2008.10.003. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassel CK. Geriatrics: A vital core of hospital medicine. Caring for the hospitalized elderly: Current best practice and new horizons. The Hospitalist: A Special Supplement. 2004:2–3. [Google Scholar]
- Coussement J, De PL, Schwendimann R, Denhaerynck K, Dejaeger E, Milisen K. Interventions for preventing falls in acute- and chronic-care hospitals: a systematic review and meta-analysis. Journal of the American Geriatrics Society. 2008;56:29–36. doi: 10.1111/j.1532-5415.2007.01508.x. [DOI] [PubMed] [Google Scholar]
- Cusimano MD, Kwok J, Spadafora K. Effectiveness of multifaceted fall-prevention programs for the elderly in residential care. Injury Prevention. 2008;14:113–122. doi: 10.1136/ip.2007.017533. [DOI] [PubMed] [Google Scholar]
- Dykes PC, Carroll DL, Hurley AC, Benoit A, Middleton B. Why do patients in acute care hospitals fall? Can falls be prevented? Journal of Nursing Administration. 2009;39:299–304. doi: 10.1097/NNA.0b013e3181a7788a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans D, Hodgkinson B, Lambert L, Wood J. Falls risk factors in the hospital setting: a systematic review. International Journal of Nursing Practice. 2001;7:38–45. doi: 10.1046/j.1440-172x.2001.00269.x. [DOI] [PubMed] [Google Scholar]
- Fischer ID, Krauss MJ, Dunagan WC, Birge S, Hitcho E, Johnson S, Costantinou E, Fraser VJ. Patterns and predictors of inpatient falls and fall-related injuries in a large academic hospital. Infection Control and Hospital Epidemiology. 2005;26:822–827. doi: 10.1086/502500. [DOI] [PubMed] [Google Scholar]
- Frankel A, Graydon-Baker E, Neppl C, Simmonds T, Gustafson M, Gandhi TK. Patient safety leadership walkrounds. Joint Commission Journal on Quality and Safety. 2003;29:16–26. doi: 10.1016/s1549-3741(03)29003-1. [DOI] [PubMed] [Google Scholar]
- Halfon P, Eggli Y, Van Melle G, Vagnair A. Risk of falls for hospitalized patients: a predictive model based on routinely available data. Journal of Clinical Epidemiology. 2001;54:1258–1266. doi: 10.1016/s0895-4356(01)00406-1. [DOI] [PubMed] [Google Scholar]
- Henderson V. Basic Principles of Nursing Care (rev. edn.) Geneva: International Council of Nurses; 1977. [Google Scholar]
- Hendriks MR, Bleijlevens MH, van Haastregt JC, Crebolder HF, Diederiks JP, Evers SM, Mulder WJ, Kempen GI, van Rossum E, Ruijgrok JM, Stalenhoef PA, van Eijk JT. Lack of effectiveness of a multidisciplinary fall-prevention program in elderly people at risk: a randomized, controlled trial. Journal of the American Geriatrics Society. 2008;56:1390–1397. doi: 10.1111/j.1532-5415.2008.01803.x. [DOI] [PubMed] [Google Scholar]
- Horvath KJ, Hurley AC, Duffy ME, Gauthier MA, Harvey RM, Trudeau SA, Cipolloni PB, Smith SJ. Caregiver competence to prevent home injury to the care recipient with dementia. Rehabilitation Nursing. 2005;30:189–196. doi: 10.1002/j.2048-7940.2005.tb00109.x. [DOI] [PubMed] [Google Scholar]
- Hurley AC, Gauthier MA, Horvath KJ, Harvey R, Smith SJ, Trudeau S, Cipolloni PB, Hendricks A, Duffy M. Promoting safer home environments for persons with Alzheimer’s disease. Journal of Gerontological Nursing. 2004;30:43–51. doi: 10.3928/0098-9134-20040601-09. [DOI] [PubMed] [Google Scholar]
- Hurley AC, Lancaster D, Hayes J, Wilson-Chase C, Bane A, Griffin M, Warden V, Duffy ME, Poon EG, Gandhi TK. The Medication Administration System - Nurses Assessment of Satisfaction (MAS-NAS) Scale. Journal of Nursing Scholarship. 2006;38:298–300. doi: 10.1111/j.1547-5069.2006.00117.x. [DOI] [PubMed] [Google Scholar]
- Hurley AC, Bane A, Fotakis S, Duffy ME, Sevigny A, Poon EG, Gandhi TK. Nurses’ satisfaction with medication administration point-of-care technology. Journal of Nursing Administration. 2007;37:343–349. doi: 10.1097/01.nna.0000285114.60689.02. [DOI] [PubMed] [Google Scholar]
- Inouye SK, Brown CJ, Tinetti ME. Medicare nonpayment, hospital falls, and unintended consequences. New England Journal of Medicine. 2009;360:2390–2393. doi: 10.1056/NEJMp0900963. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Retooling for an Aging America: Building the Health Care Workforce. Washington, DC: National Academy Press; 2010. [PubMed] [Google Scholar]
- Krauss MJ, Nguyen SL, Dunagan WC, Birge S, Costantinou E, Johnson S, Caleca B, Fraser VJ. Circumstances of patient falls and injuries in 9 hospitals in a midwestern healthcare system. Infection Control and Hospital Epidemiology. 2007;28:544–550. doi: 10.1086/513725. [DOI] [PubMed] [Google Scholar]
- Krauss MJ, Tutlam N, Costantinou E, Johnson S, Jackson D, Fraser VJ. Intervention to prevent falls on the medical service in a teaching hospital. Infection Control and Hospital Epidemiology. 2008;29:539–545. doi: 10.1086/588222. [DOI] [PubMed] [Google Scholar]
- Kruger NK, Hurley AC, Gustafson M. Framing patient safety initiatives: working model and case example. Journal of Nursing Administration. 2006;36:200–204. doi: 10.1097/00005110-200604000-00009. [DOI] [PubMed] [Google Scholar]
- Kutney-Lee A, Aiken LH. Effect of nurse staffing and education on the outcomes of surgical patients with comorbid serious mental illness. Psychiatric Services. 2008;59(12):1466–1469. doi: 10.1176/appi.ps.59.12.1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW, Jr, Bandura A, Gonzalez VM, Laurent DD, Holman HR. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care. 2001;39:1217–1223. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- McInnes E, Askie L. Evidence review on older people’s views and experiences of falls prevention strategies. Worldviews on Evidence-Based Nursing. 2004;1:20–37. doi: 10.1111/j.1741-6787.2004.04013.x. [DOI] [PubMed] [Google Scholar]
- Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2nd edn. Thousand Oaks: SAGE; 1994. [Google Scholar]
- Morse JM. Qualitative and quantitative research: strategies for sampling. In: Chinn P, editor. Nursing Research: Methodological Issues. Rockville, MD: Aspen; 1987. pp. 181–193. [Google Scholar]
- Morse JM. Preventing Patient Falls. Thousand Oaks: Sage Publications; 1997. [Google Scholar]
- Nunnally JC, Bernstein IH. Psychometric Theory. 3rd edn. New York: McGraw Hill Book Company, Inc; 1994. [Google Scholar]
- Oliver D, Britton M, Seed P, Martin FC, Hopper AH. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies. BMJ. 1997;315:1049–1053. doi: 10.1136/bmj.315.7115.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver D, Daly F, Martin F, McMurdo M. Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age and Ageing. 2004;33:122–130. doi: 10.1093/ageing/afh017. [DOI] [PubMed] [Google Scholar]
- Oliver D, Connelly JB, Victor CR, Shaw FE, Whitehead A, Genc Y, Vanoli A, Martin FC, Gosney MA. Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta-analyses. BMJ. 2007;334:82–87. doi: 10.1136/bmj.39049.706493.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd P, Miller NH, Kaufman J, Kraemer HC, Bandura A, Greenwald G, Debusk RF. Nurse management for hypertension. A systems approach. American Journal of Hypertension. 2004;17(10):921–927. doi: 10.1016/j.amjhyper.2004.06.006. [DOI] [PubMed] [Google Scholar]
- Schwendimann R, Buhler H, De GS, Milisen K. Falls and consequent injuries in hospitalized patients: effects of an interdisciplinary falls prevention program. BMC Health Services Research. 2006;6:69. doi: 10.1186/1472-6963-6-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squillace MR, Remsberg RE, Harris-Kojetin LD, Bercovitz A, Rosenoff E, Han B. The national nursing assistant survey: improving the evidence base for policy initiatives to strengthen the certified assistant workforce. The Gerontologist. 2009;49:185–197. doi: 10.1093/geront/gnp024. [DOI] [PubMed] [Google Scholar]
- Stajkovic AD, Luthans F. Self-efficacy and work-related performance: a meta-analysis. Psychological Bulletin. 1998;124:240–261. [Google Scholar]
- Steffen AM, McKibbin C, Zeiss A, Gallagher-Thompson D, Bandura A. The revised scale for caregiving self-efficacy: reliability and validity studies. The Journals of Gerontology: Psychological Sciences. 2002;57B:P74–P86. doi: 10.1093/geronb/57.1.p74. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. Journal of Gerontology: Psychological Sciences. 1990;45:P239–P243. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, HRSA, BuHP, & Division of Nursing. The Registered Nurse Population: Findings from the 2004 National Sample Survey of Registered Nurses. Rockville, MD: Health Resources and Services Administration; 2004. [Google Scholar]
- U.S. Department of Health and Human Services, HRSA, BuHP, & Division of Nursing. The Registered Nurse Population: Findings from the 2008 National Sample Survey of Registered Nurses. Rockville, MD: Health Resources and Services Administration; 2010. [Google Scholar]
- Vassallo M, Amersey RA, Sharma JC, Allen SC. Falls on integrated medical wards. Gerontology. 2000;46:158–162. doi: 10.1159/000022152. [DOI] [PubMed] [Google Scholar]
- Walshe A, Rosen H. A study of patient falls from bed. Journal of Nursing Administration. 1979;9(5):31–35. [PubMed] [Google Scholar]
- Waltz CF, Strickland OL, Lenz ER. Measurement in Nursing and Health Research. 3rd edn. Philadelphia: F.A. Davis Company; 2005. [Google Scholar]
- Wyatt JC. When to use web-based surveys. Journal of the American Medical Informatics Association. 2000;7:426–429. doi: 10.1136/jamia.2000.0070426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyatt J, Altman D. Prognostic models: clinically useful or quickly forgotten? British Medical Journal. 1995;311:1539–1541. [Google Scholar]
- Zecevic AA, Salmoni AW, Speechley M, Vandervoort AA. Defining a fall and reasons for falling: comparisons among the views of seniors, health care providers, and the research literature. The Gerontologist. 2006;43:367–376. doi: 10.1093/geront/46.3.367. [DOI] [PubMed] [Google Scholar]