Abstract
Purpose
Men with high-risk features (extraprostatic extension or high Gleason grade) face a high risk of prostate cancer recurrence after radical prostatectomy. Clinical trials of adjuvant systemic therapy for such patients have been limited.
Patients and Methods
The SWOG (Southwest Oncology Group) S9921 study randomly assigned 983 men with high-risk features at prostatectomy to receive adjuvant therapy with androgen deprivation (ADT) alone or in combination with mitoxantrone chemotherapy. ADT consisted of goserelin and bicalutamide for 2 years.
Results
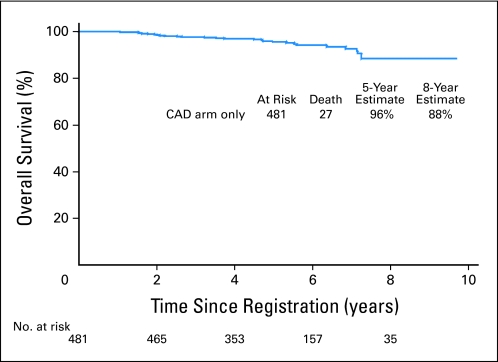
Although the final primary treatment comparison results are not ready for publication, this article reports results in the ADT-alone control arm with a median follow-up of 4.4 years. For these 481 men, the estimated 5-year biochemical failure-free survival is 92.5% (95% CI, 90 to 95), and 5-year overall survival is 95.9% (95% CI, 93.9 to 97.9).
Conclusion
The results of this trial, taken in context, make a compelling argument for counseling all high-risk patients with prostate cancer about adjuvant ADT. This article discusses the challenges in the design and implementation of clinical trials to take the next step forward in adjuvant therapy for prostate cancer because of the excellent survival achieved with currently available therapies and highlights the need for better molecular markers to personalize care.
INTRODUCTION
Prostate cancer affects 186,000 men annually in the United States and accounts for more than 28,000 deaths.1 Most men diagnosed in the prostate-specific antigen (PSA) era have favorable disease characteristics that are amenable to cure with surgery or radiation. However, the subset of men with high-grade (Gleason score ≥ 8) or extraprostatic disease (T3/T4 or lymph node involvement) have a risk of treatment failure as high as 70% with surgery alone.2–5 This has fostered interest in adjuvant therapy with androgen deprivation as well as chemotherapy.
Systemic therapy has a limited role in localized prostate cancer, although adjuvant androgen deprivation therapy (ADT) has yielded significant improvement in disease-free survival for men with high-risk features treated with definitive radiation6,7and a significant overall survival advantage for men with Gleason scores of 8 or higher.6 For surgical patients, a survival advantage with adjuvant ADT was reported in a small trial of lymph node–positive (D1) patients.8 Unlike breast cancer, for which validated tissue markers predict benefit from hormone therapy, essentially all prostate adenocarcinomas express the androgen receptor, and more than 90% of men respond to ADT. Molecular predictive markers have not yet been validated in prostate cancer to identify men who would experience more or less benefit, although duration of response has varied widely.9,10 Adjuvant therapy in prostate cancer has thus been investigated for all patients, without the advantage of targeting a molecularly enriched population. Although chemotherapy is now an accepted perioperative adjunct in several common solid tumor types, few data exist to guide our use of adjuvant chemotherapy in prostate cancer. Unlike other malignancies, prostate cancer has two distinct disease states (ie, castration sensitive and castration resistant) with distinct biologies. To date, chemotherapy has proven beneficial only in castration-resistant prostate cancer, with less efficacy in early-stage or castration-sensitive disease.11
In this landscape, a national multidisciplinary group of investigators was convened to address the merit of adjuvant systemic therapy for men with high-risk localized prostate cancer after radical prostatectomy. After discussions among cooperative group and National Cancer Institute representatives, several adjuvant trials were planned. SWOG designed the S9921 study to compare androgen deprivation alone and with mitoxantrone as adjuvant therapy for men with high-risk prostate cancer after prostatectomy.
PATIENTS AND METHODS
SWOG S9921 was designed to investigate whether the addition of mitoxantrone chemotherapy to ADT using zoladex plus bicalutamide would improve survival after prostatectomy, compared with ADT alone. The control arm of androgen deprivation rather than observation was determined on the basis of several factors: the results of ECOG (Eastern Cooperative Oncology Group) 3886, in which immediate postoperative ADT yielded a substantial improvement in survival compared with delayed treatment for patients with prostate cancer with nodal involvement; data from trials documenting a benefit from ADT adjunctive to radiation8,12; and the fact that a phase III trial evaluating adjuvant ADT versus observation was planned by ECOG, such that the standard of care by the time of study completion was projected as likely to include ADT. Two years of ADT were chosen in consideration for quality of life. Combined blockade was chosen because of superiority of ADT with an antiandrogen over castration alone, noted in earlier SWOG trials.13,14
At the time of study design, mitoxantrone was the only chemotherapy approved for castration-resistant prostate cancer.15 In other solid tumors, especially breast cancer, the impact of chemotherapy agents was amplified by applying it in the adjuvant setting.16 A subgroup analysis of a small randomized trial found that in men with locally advanced prostate cancer, mitoxantrone achieved a prolonged median survival of 80 months, compared with 36 months with ADT alone.17 Hence, S9921 included mitoxantrone 12 mg/m2 every 21 days for six cycles with 2 years of combined androgen blockade as the experimental arm.
The primary end point of the trial was overall survival. Patients in the control arm were expected to have a median survival of 10 years as a result of at least one high-risk feature: Gleason score of 8 or higher; preoperative PSA of 15 ng/mL or greater; stage T3b, T4, or N1 disease; or Gleason score of 7 with either preoperative PSA greater than 10 ng/mL or a positive margin. Eligibility required normal cardiac function, postoperative PSA nadir of 0.2 ng/mL or less, and no more than 4 months of ADT before enrollment.
PSA was monitored every 3 months for 5 years, then every 6 months until 10 years after completion of study therapy. Testosterone was measured every 6 months until recovery to normal range. Relapse was defined as three consecutive PSA levels greater than 0.2 ng/mL or one value more than 0.2 ng/mL and initiation of radiation. Relapse-free survival was defined from date of random assignment to first elevated PSA. Death without relapse is censored. Survival was defined from random assignment to date of death as a result of any cause. Men were censored at their last known contact date. The primary objective of the study was a 30% improvement in median survival with the addition of mitoxantrone, translating into a reduction in the death hazard rate by 23%. Published series of recurrence rates in similar high-risk populations are summarized in Table 1. Assuming exponential survival, 9.5 years of accrual, and an additional 4 years of follow-up, this study design has 0.92 statistical power to detect a 30% improvement in median survival with 680 patients per arm, using a one-sided test with .05 significance level.
Table 1.
Selected Large Series Examining Rate of Biochemical Recurrence After Radical Prostatectomy According to Pathologic Stage or Grade
| Study | Population | Adjuvant Treatment | No. | RFS | OS |
|---|---|---|---|---|---|
| Carver et al2 | T3 | neoADT, 36% | 176 | 5 year, 48% | 5 year, 94% |
| (19% LN positive) | 10 year, 85% | ||||
| (disease specific) | |||||
| Petrovich et al3* | T3N0 | None | 199 | 5 year, 60% | NR |
| Roehl et al4 | T3 | XRT, 6% | 887 | 10 year, 15% | 10 year, 83% |
| Gleason score, 8-10 | 237 | 10 year, 32% | (97% disease specific) | ||
| Nguyen et al5 | Gleason score, 8-10 | None | 135 | 5 year, 42% | NR |
Abbreviations: RFS, recurrence-free survival; OS, overall survival; LN, lymph node; neoADT, neoadjuvant androgen deprivation therapy; NR, not reported; XRT, external radiation therapy.
RFS in this study combined biochemical with clinical recurrence.
RESULTS
Preliminary Results of SWOG S9921
Although the primary treatment comparison data are not yet mature, this report was authorized by the data safety monitoring committee because it felt that the information would be useful to investigators designing clinical trials and to clinical oncologists treating these patients. This report summarizes the events and survival for the S9921 control arm only.
Accrual to S9921 commenced in February 2000, with 983 patients randomly assigned (487 in the mitoxantrone plus ADT arm and 496 in the ADT-alone arm) before January 2007. The protocol and informed consent document were approved by the National Cancer Institute Cancer Therapy Evaluation Program and the institutional review boards of participating sites. Written informed consent was obtained from all patients before enrollment. Accrual was permanently stopped when the data safety monitoring committee prohibited use of mitoxantrone after three cases of acute myeloid leukemia in the mitoxantrone arm, the details of which have been reported.18 There were no cases of leukemia in the ADT-alone arm.
The baseline and demographic characteristics of the 481 eligible men assigned to receive ADT alone are summarized in Table 2. The median PSA of 7.8 ng/mL and highest value of 12.3 ng/mL are relatively low, considering 61% of patients had stage T3 disease or higher, and 16% were node positive. There were 10 major treatment violations in the ADT arm; eight men received no protocol therapy, and two received chemotherapy. The median time to testosterone recovery was 11.7 months after completion of androgen blockade (95% CI, 11.3 to 11.9). The 6- and 18-month recovery rates were 16% and 89%, respectively.
Table 2.
Baseline Demographic Characteristics of Men in S9921ADT-Alone Treatment Arm (n = 481)
| Characteristic | No. | % |
|---|---|---|
| Age, years | ||
| Median | 60.7 | |
| Range | 40-82 | |
| Presurgical PSA | ||
| Median | 7.8 | |
| Range | 5.1-12.3 | |
| Race | ||
| Non-Hispanic white | 399 | 83 |
| Black | 66 | 14 |
| Hispanic | 25 | 5 |
| Asian/Pacific Islander | 9 | 2 |
| Native American | 2 | 0.5 |
| Unknown | 5 | 1 |
| Stage | ||
| Organ confined | 110 | 23 |
| ≥ T3 but N0 | 292 | 61 |
| N1 | 79 | 16 |
| Gleason score | ||
| < 7 | 9 | 2 |
| 7 | 215 | 45 |
| 8-10 | 257 | 53 |
| Radiation therapy planned | ||
| Yes | 130 | 27 |
| No | 351 | 73 |
| Positive surgical margin | ||
| Yes | 316 | 66 |
| No | 165 | 34 |
Abbreviations: ADT, androgen deprivation therapy; PSA, prostate-specific antigen.
Toxicity was modest, as would be expected from zoladex and bicalutamide. There were 135 grade 3 events, including abdominal pain (two), anxiety (three), arthralgias (two), cardiovascular events (ischemia and arrhythmia), gynecomastia, hypertension (eight), hot flashes (nine), memory loss (two), muscle weakness/myalgias (four), rash (one), transaminitis (four), and urinary changes including incontinence (12). No unexpected adverse events were noted in the ADT-alone arm, and only 30 of 481 men discontinued protocol therapy early because of toxicities.
Survival and Freedom From Biochemical Failure in the Control Arm
The statistical design for S9921 assumed a median survival of 10 years; however, the low number of deaths with the current follow-up triggered this report. Assuming exponential survival, 5-year survival is predicted to be 71%, and 8-year survival is expected to be 57%. There have been only 27 deaths (13 as a result of prostate cancer) among 481 men in the ADT-alone arm, or a 96% survival at 5 years and 88% survival at 8 years with a median follow-up of 4.4 years (Fig 1). The PSA recurrence-free survival at 5 years is 92.5%. These numbers hold across risk subgroups (Table 3). Because adjuvant radiation is known to affect recurrence in men with extracapsular disease, positive margins, and seminal vesicle involvement,19,20 an analysis was conducted to assess whether freedom from biochemical failure was affected by radiation. The data are limited by collection only of intention to receive radiation at study entry, without confirmation of receipt or doses. Twenty-seven percent of patients randomly assigned to the control arm were stratified as planning to receive adjuvant radiation. The biochemical failure and overall survival results are not changed when those intending to receive radiation were excluded from the analysis, with 5-year freedom from biochemical failure estimated at 92.7%, compared with 92.5% for the whole group, and this holds across risk subgroups (Table 4).
Fig 1.
Survival of patients in the chemical androgen deprivation (CAD) –alone arm of the SWOG (Southwest Oncology Group) S9921 study.
Table 3.
Biochemical FFR and OS for Patients Receiving 2 Years of Combined Androgen Blockade in S9921 Control Arm
| Risk Group | No. | 5-Year FFR |
5-Year OS |
||
|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | ||
| All patients in ADT arm | 481 | 92.5 | 90.0 to 95.0 | 95.9 | 93.9 to 97.9 |
| High (node positive) | 79 | 83.2 | 73.8 to 92.6 | 92.3 | 85.6 to 99.0 |
| Intermediate (Gleason score ≥ 8 or stage T3b) | 277 | 92.2 | 88.7 to 95.7 | 96.8 | 94.6 to 99.0 |
| Low (Gleason score 7 with positive margins or PSA > 10) | 125 | 99.1 | 97.3 to 100 | 95.9 | 91.8 to 100 |
Abbreviations: FFR, freedom from relapse; OS, overall survival; ADT, androgen deprivation therapy; PSA, prostate-specific antigen.
Table 4.
Biochemical FFR and OS for Risk Groups With Removal of Patients Anticipating Receipt of Adjuvant RT
| Risk Group (no planned RT) | No. | 5-Year FFR Estimate |
5-Year OS Estimate |
||
|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | ||
| All eligible patients | 351 | 92.7 | 89.8 to 95.6 | 95.4 | 93.0 to 97.8 |
| High (node positive) | 64 | 87.4 | 78.6 to 96.2 | 92.4 | 85.1 to 99.7 |
| Intermediate (Gleason score ≥ 8 or stage T3b) | 199 | 91.8 | 87.7 to 95.9 | 96.7 | 94.0 to 99.4 |
| Low (Gleason score 7 with positive margins or PSA > 10) | 88 | 98.7 | 96.2 to 100 | 94.5 | 89.0 to 100 |
Abbreviations: FFR, freedom from relapse; OS, overall survival; RT, radiation therapy; PSA, prostate-specific antigen.
DISCUSSION
Adjuvant systemic therapy has not been well studied in prostate cancer. Except for the ECOG study in node-positive disease, there have been no prospective studies of postoperative ADT in the PSA era. In the ECOG study, 47 node-positive patients with prostate cancer received adjuvant androgen ablation, with a significant improvement in survival.8 Although not designed specifically to address the role of adjuvant androgen ablation, but rather the role of adjuvant chemotherapy, the control arm of S9921 now represents the largest prospective cohort of that treatment and shows that the combination of radical prostatectomy and combined androgen blockade is associated with favorable disease-free and overall survival. The only other multi-institutional prospective data are from the bicalutamide study group. Although antiandrogens as monotherapy are not considered to be as effective as the luteinizing hormone-releasing hormone agonists in patients with locally advanced prostate cancer, bicalutmide monotherapy reduced progression, although full outcomes (ie, 5-year biochemical failure-free survival) have not been elucidated.21 Because of the paucity of prospective data, the control arm of S9921 is one of the most important sources of information on the adjuvant use of androgen ablation.
Apart from the possible selection bias inherent in a trial randomly assigning patients to receive chemotherapy, another potential explanation for the better-than-expected results in S9921 is that stage migration has occurred since the advent of widespread PSA testing, resulting in reduced prostate cancer–specific mortality.22–24 In addition, there may have been an upgrading of Gleason scores, such that the Gleason score of 6 of yesterday may be classified as 7 today, altering its predictive value for recurrence.25,26 These trends could have contributed to the low rate of cancer recurrence in this study. The use of adjuvant radiation may also have influenced recurrence rate, because it has been shown to improve relapse-free and metastasis-free survival for men with positive surgical margins, extracapsular extension, and seminal vesicle involvement.19,20 However, at the time of random assignment, only 27% of study patients intended to receive radiation. The majority of men with positive surgical margins and stage T3/T4 disease did not receive immediate radiation, and despite this, relapse-free survival is excellent. We separately evaluated the group not intending to receive adjuvant radiation, and the outcomes remained unchanged. A third possible contributor to the excellent survival in S9921 was the availability of effective salvage therapies, the increasing use of docetaxel for metastatic castration-resistant disease, and novel therapies such as abiraterone and sipuleucel-T. Nevertheless, 2 years of adjuvant ADT is likely a significant contributor to improved outcomes after radical prostatectomy even for patients with these adverse pathologic features. Importantly, this trial does not address the question of whether immediate ADT after radical prostatectomy is superior to starting ADT at the time of biochemical or clinical recurrence.
When evaluating overall benefit, potential harms caused by adjuvant therapy must be assessed. Data from the Surveillance, Epidemiology and End Results and Medicare databases indicate that ADT is associated with an increased risk of diabetes (hazard ratio, 1.44; 95% CI, 1.34 to 1.55), with questionable effects on cardiac morbidity.27,28 Age may influence cardiac effects, and the role of therapy duration is unclear, because 31 (6.4%) of 483 men who received 6 months of ADT with radiation suffered cardiac mortality, compared with 25 (5.1%) of 487 who received 3 years.28 Because all men in S9921 received ADT, we cannot determine excess cardiovascular morbidity related to androgen deprivation in this trial. Furthermore, only men with normal cardiac function were enrolled because of potential cardiotoxicity from mitoxantrone therapy, and as such, the cardiac event rate is not generalizable to all patients with prostate cancer. Nevertheless, cardiac morbidity during the study was reassuringly low, with only one ischemic event in the casodex plus zoladex arm, compared with five events among patients who also received mitoxantrone. In extended follow-up, there were three deaths attributed to cardiac causes for mitoxantrone-treated patients, and two were considered cardiac among men who had been treated in the control arm. Although 89% of men recovered normal testosterone levels after 18 months, the fact that some men remain hypogonadal after 2 years of adjuvant ADT is an important piece of information in counseling patients. The potential for long-term cardiac risk must be considered before using adjuvant ADT outside of a clinical trial, especially because a significant percentage of men in this population may be cured with surgery alone.
Despite the aforementioned limitations, the results of S9921 have some application in current clinical practice. The survival advantage from immediate ADT in ECOG 3886, the favorable disease-free and overall survival as well as toxicity in the control arm of S9921, and the superior outcomes for men with high-risk or locally advanced prostate cancer receiving ADT with radiation make a compelling argument for counseling men with high-risk prostate cancer after radical prostatectomy about the merits of adjuvant androgen deprivation. On the basis of previous adjuvant studies, men with stage T3 or margin-positive prostate cancer should be offered adjuvant radiation, but the results of S9921 suggest there may be a role for androgen deprivation in this setting as well, because excellent outcomes were seen despite a minority of eligible men receiving adjuvant radiation. For men with relative contraindications to radiation, adjuvant ADT certainly represents a reasonable choice.
The excellent disease-specific outcomes after surgery, even for what is currently regarded as high-risk disease, clearly highlight the limitations in our ability to predict the true risk of death. In fact, most of the risk criteria that are presently employed are related to PSA relapse and not risk of death. Clearly, PSA relapse is not equal to risk of death, because the majority of men with biochemical recurrence do not die as a result of prostate cancer even after 15 years.29 Overall survival, therefore, remains the gold standard and was the primary end point for S9921, although its evaluation requires significantly greater resources.
Although excellent outcomes were observed in men receiving adjuvant ADT, the increasing recognition of potentially significant toxicity makes testing de-escalation of treatment an appealing candidate for the next step forward. To evaluate noninferiority of a novel treatment arm, such as shorter course of ADT, compared with the control arm from S9921, an enormous sample size would be required based on the low event rate observed. For example, if there were no difference in survival between men treated with 2 years or 1 year of ADT, and we specified that the lower threshold of survival considered not inferior to the control would be 10% below that seen in S9921, nearly 20,000 patients would be required for random assignment to have 90% statistical power. More exciting questions, such as the role of emerging third-generation androgen deprivation agents or adding immune therapy, will be similarly difficult to answer. Even if a study were designed to test for superiority of a new agent, with a large treatment effect anticipated (for instance, 33% improvement in survival) based on the 88% survival at 8 years from S9921, a trial in the range of 3,000 to 3,500 randomly assigned patients would still be required, extending over 15 to 20 years for completion. If the anticipated treatment effect were more modest, for instance, a 25% improvement in survival, the sample size would increase to more than 5,000 men.
To reduce the number of patients necessary to answer such questions, the next adjuvant prostate cancer trial will need to define an even higher-risk population, which will be difficult until more reliable, perhaps molecular, predictors of outcome become validated. An alternative would be to leave the adjuvant realm and select only patients who do not nadir appropriately after definitive local therapy and/or those who experience biochemical recurrence. This would enrich the population for events, although even this group of patients has had heterogeneous outcomes. This design would spare some men from adjuvant androgen deprivation who would achieve a cure with surgery alone (with or without adjuvant radiation therapy). Among those experiencing biochemical recurrence, well-documented parameters define populations at highest risk of disease progression: Gleason score of 8 or higher, short time from surgery to recurrence, and rapid PSA doubling time.29 Changing the trial population from strictly adjuvant to biochemical recurrence would create an opportunity to use an alternative and more rapidly assessable end point, such as PSA nadir during treatment or PSA progression at 7 months. These novel end points have been shown to yield strong predictive value for survival in the metastatic setting, although their applicability to men with biochemical recurrence has not yet been defined.30,31 Progression-free and overall survival would still be end points of interest, but this alternative end point analysis could accelerate screening of new agents in the phase II setting. One drawback to such a design is that these results would not necessarily be generalizable to men who desire additional treatment after prostatectomy because of high risk of disease recurrence, despite achieving an adequate PSA nadir.
In conclusion, within the context of PSA-driven stage migration, 2 years of adjuvant androgen deprivation after radical prostatectomy resulted in an extremely low rate of disease recurrence and prostate cancer–specific death for high-risk patients in S9921. Added to the experience with ADT adjuvant to prostatectomy in lymph node–positive patients and adjunctive to definitive radiation in intermediate and high-risk disease, these data support the consideration of ADT in patients with high-risk prostate cancer after prostatectomy. Designing a trial to take the next step forward in the development of adjuvant therapy for high-risk localized prostate cancer is challenging because of the excellent survival achieved with currently available therapies.
Footnotes
Supported in part by Public Health Service Cooperative Agreement Grants No. CA32102, CA38926, CA27057, CA42777, CA58882, CA20319, CA14028, CA68183, CA46368, CA46282, CA37981, CA22433, CA58686, CA128567, CA04919, CA95860, CA76447, CA46441 CA35192, CA46136, CA11083, CA35178, CA76132, CA63844, CA46113, CA45808, CA86780, CA12644, CA35431, CA35119, CA16385, CA45450, CA67575, CA74647, CA35128, CA45560, CA58723, CA35176, CA58658, CA63848, CA35281, CA35262, CA021115, and CA031946 from the National Cancer Institute, Bethesda, MD, and in part by Astra-Zeneca and OSI Pharmaceuticals.
Presented in part at the 45th Annual Meeting of the American Society of Clinical Oncology, May 29-June 2, 2009, Orlando, FL, and the 2010 Annual Meeting of the American Urological Association, May 29-June 3, 2010, San Francisco, CA.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
Clinical trial information can be found for the following: NCT00004124.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Although all authors completed the disclosure declaration, the following author(s) indicated a financial or other interest that is relevant to the subject matter under consideration in this article. Certain relationships marked with a “U” are those for which no compensation was received; those relationships marked with a “C” were compensated. For a detailed description of the disclosure categories, or for more information about ASCO's conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors.
Employment or Leadership Position: None Consultant or Advisory Role: None Stock Ownership: None Honoraria: E. David Crawford, AstraZeneca; Ian Thompson, Ferring Pharmaceuticals Research Funding: None Expert Testimony: None Other Remuneration: None
AUTHOR CONTRIBUTIONS
Conception and design: Thomas W. Flaig, Catherine M. Tangen, Maha H.A. Hussain, Gregory P. Swanson, David P. Wood Jr, Nancy A. Dawson, E. David Crawford, Ian M. Thompson
Administrative support: Nicholas J. Vogelzang, Ian M. Thompson
Provision of study materials or patients: Maha H.A. Hussain, Gregory P. Swanson, Nancy A. Dawson, Naomi B. Haas, E. David Crawford, Nicholas J. Vogelzang, L. Michael Glode
Collection and assembly of data: Catherine M. Tangen, Wael A. Sakr, E. David Crawford, L. Michael Glode
Data analysis and interpretation: Tanya B. Dorff, Thomas W. Flaig, Catherine M. Tangen, Maha H.A. Hussain, David P. Wood Jr, Naomi B. Haas, Nicholas J. Vogelzang, Ian M. Thompson, L. Michael Glode
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2009. CA Cancer J Clin. 2009;59:225–249. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- 2.Carver BS, Bianco FJ, Jr, Scardino PT, et al. Long-term outcome following radical prostatectomy in men with clinical stage T3 prostate cancer. J Urol. 2006;176:564–568. doi: 10.1016/j.juro.2006.03.093. [DOI] [PubMed] [Google Scholar]
- 3.Petrovich Z, Lieskovsky G, Stein JP, et al. Comparison of surgery alone with surgery and adjuvant radiotherapy for pT3N0 prostate cancer. BJU Int. 2002;89:604–611. doi: 10.1046/j.1464-410x.2002.02698.x. [DOI] [PubMed] [Google Scholar]
- 4.Roehl KA, Han M, Ramos CG, et al. Cancer progression and survival rates following anatomical radical retropubic prostatectomy in 3,478 consecutive patients: Long-term results. J Urol. 2004;172:910–914. doi: 10.1097/01.ju.0000134888.22332.bb. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen CT, Reuther AM, Stephenson AJ, et al. The specific definition of high risk prostate cancer has minimal impact on biochemical relapse-free survival. J Urol. 2009;181:75–80. doi: 10.1016/j.juro.2008.09.027. [DOI] [PubMed] [Google Scholar]
- 6.Pilepich MV, Caplan R, Byhardt RW, et al. Phase III trial of androgen suppression using goserelin in unfavorable-prognosis carcinoma of the prostate treated with definitive radiotherapy: Report of Radiation Therapy Oncology Group Protocol 85-31. J Clin Oncol. 1997;15:1013–1021. doi: 10.1200/JCO.1997.15.3.1013. [DOI] [PubMed] [Google Scholar]
- 7.Roach M, 3rd, Bae K, Speight J, et al. Short-term neoadjuvant androgen deprivation therapy and external-beam radiotherapy for locally advanced prostate cancer: Long-term results of RTOG 8610. J Clin Oncol. 2008;26:585–591. doi: 10.1200/JCO.2007.13.9881. [DOI] [PubMed] [Google Scholar]
- 8.Messing EM, Manola J, Yao J, et al. Immediate versus deferred androgren deprivation treatment in patients with node-positive prostate cancer after radical prostatectomy and pelvic lymphadenectomy. Lancet Oncol. 2006;7:472–479. doi: 10.1016/S1470-2045(06)70700-8. [DOI] [PubMed] [Google Scholar]
- 9.Ravdin PM, Green S, Dorr TM, et al. Prognostic significance of progesterone receptor levels in estrogen receptor-positive patients with metastatic breast cancer treated with tamoxifen: Results of a prospective Southwest Oncology Group Study. J Clin Oncol. 1992;10:1284–1291. doi: 10.1200/JCO.1992.10.8.1284. [DOI] [PubMed] [Google Scholar]
- 10.Scher HI, Buchanan G, Gerald W, et al. Targeting the androgen receptor: Improving outcomes for castration-resistant prostate cancer. Endocr Relat Cancer. 2004;11:459–476. doi: 10.1677/erc.1.00525. [DOI] [PubMed] [Google Scholar]
- 11.Magi-Galluzzi C, Zhou M, Reuther AM, et al. Neoadjuvant docetaxel treatment for locally advanced prostate cancer. Cancer. 2007;110:1248–1254. doi: 10.1002/cncr.22897. [DOI] [PubMed] [Google Scholar]
- 12.Bolla M, Gonzalez D, Warde P, et al. Improved survival in patients with locally advanced prostate cancer treated with radiotherapy and goserelin. N Engl J Med. 1997;337:295–300. doi: 10.1056/NEJM199707313370502. [DOI] [PubMed] [Google Scholar]
- 13.Crawford ED, Eisenberger MA, McLeod DG, et al. A controlled trial of leuprolide with and without flutamide in prostatic carcinoma. N Engl J Med. 1989;321:419–424. doi: 10.1056/NEJM198908173210702. [DOI] [PubMed] [Google Scholar]
- 14.Eisenberger MA, Blumenstein BA, Crawford ED, et al. Bilateral orchiectomy with or without flutamide for metastatic prostate cancer. N Engl J Med. 1998;339:1036–1042. doi: 10.1056/NEJM199810083391504. [DOI] [PubMed] [Google Scholar]
- 15.Tannock IF, Osoba D, Stockler MR, et al. Chemotherapy with mitoxantrone plus prednisone or prednisone alone for symptomatic hormone-resistant prostate cancer: A Canadian randomized trial with palliative end points. J Clin Oncol. 1996;14:1756–1764. doi: 10.1200/JCO.1996.14.6.1756. [DOI] [PubMed] [Google Scholar]
- 16.Clarke M, Collins R, Darby S, et al. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: An overview of the randomised trials. Lancet. 2005;365:1687–1717. doi: 10.1016/S0140-6736(05)66544-0. [DOI] [PubMed] [Google Scholar]
- 17.Wang J, Halford S, Rigg A, et al. Adjuvant mitoxantrone chemotherapy in advanced prostate cancer. BJU Int. 2000;86:675–680. doi: 10.1046/j.1464-410x.2000.00894.x. [DOI] [PubMed] [Google Scholar]
- 18.Flaig TW, Tangen CM, Hussain MH, et al. Randomization reveals unexpected acute leukemias in Southwest Oncology Group prostate cancer trial. J Clin Oncol. 2008;26:1532–1536. doi: 10.1200/JCO.2007.13.4197. [DOI] [PubMed] [Google Scholar]
- 19.Bolla M, van Poppel H, Collette L, et al. Postoperative radiotherapy after radical prostatectomy: A randomised controlled trial (EORTC trial 22911) Lancet. 2005;366:572–578. doi: 10.1016/S0140-6736(05)67101-2. [DOI] [PubMed] [Google Scholar]
- 20.Thompson IM, Tangen CM, Paradelo J, et al. Adjuvant radiotherapy for pathological T3N0M0 prostate cancer significantly reduces risk of metastases and improves survival: Long-term followup of a randomized clinical trial. J Urol. 2009;181:956–962. doi: 10.1016/j.juro.2008.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iversen P, Johansson JE, Lodding P, et al. Bicalutamide (150 mg) versus placebo as immediate therapy alone or as adjuvant to therapy with curative intent for early nonmetastatic prostate cancer: 5.3-year median followup from the Scandinavian Prostate Cancer Group Study Number 6. J Urol. 2004;172:1871–1876. doi: 10.1097/01.ju.0000139719.99825.54. [DOI] [PubMed] [Google Scholar]
- 22.Jhaveri FM, Klein EA, Kupelian PA, et al. Declining rates of extracapsular extension after radical prostatectomy: Evidence for continued stage migration. J Clin Oncol. 1999;17:3167–3172. doi: 10.1200/JCO.1999.17.10.3167. [DOI] [PubMed] [Google Scholar]
- 23.Stephenson RA, Stanford JL. Population-based prostate cancer trends in the United States: Patterns of change in the era of prostate-specific antigen. World J Urol. 1997;15:331–335. doi: 10.1007/BF01300179. [DOI] [PubMed] [Google Scholar]
- 24.Galper SL, Chen MH, Catalona WJ, et al. Evidence to support a continued stage migration and decrease in prostate cancer specific mortality. J Urol. 2006;175:907–912. doi: 10.1016/S0022-5347(05)00419-2. [DOI] [PubMed] [Google Scholar]
- 25.Smith EB, Frierson HF, Jr, Mills SE, et al. Gleason scores of prostate biopsy and radical prostatectomy specimens over the past 10 years: Is there evidence for systematic upgrading? Cancer. 2002;94:2282–2287. doi: 10.1002/cncr.10457. [DOI] [PubMed] [Google Scholar]
- 26.Tsivian M, Sun L, Mouraviev V, et al. Changes in Gleason score grading and their effect in predicting outcome after radical prostatectomy. J Urol. 2009;74:1090–1093. doi: 10.1016/j.urology.2009.03.043. [DOI] [PubMed] [Google Scholar]
- 27.Keating NL, O'Malley AJ, Smith MR. Diabetes and cardiovascular disease during androgen deprivation for prostate cancer. J Clin Oncol. 2006;24:4448–4456. doi: 10.1200/JCO.2006.06.2497. [DOI] [PubMed] [Google Scholar]
- 28.D'Amico AV, Denham JW, Crook J, et al. Influence of androgen suppression therapy for prostate cancer on the frequency and timing of fatal myocardial infarctions. J Clin Oncol. 2007;25:2420–2425. doi: 10.1200/JCO.2006.09.3369. [DOI] [PubMed] [Google Scholar]
- 29.Freedland SJ, Humphreys EB, Mangold LA, et al. Risk of prostate cancer-specific mortality following biochemical recurrence after radical prostatectomy. JAMA. 2005;294:433–439. doi: 10.1001/jama.294.4.433. [DOI] [PubMed] [Google Scholar]
- 30.Hussain M, Tangen CM, Higano C, et al. Absolute prostate-specific antigen value after androgen deprivaiton is a strong independent predictor of survival in new metastatic prostate cancer: Data from Southwest Oncology Group Trial 9346 (INT-0162) J Clin Oncol. 2006;24:3984–3990. doi: 10.1200/JCO.2006.06.4246. [DOI] [PubMed] [Google Scholar]
- 31.Hussain M, Goldman B, Tangen C, et al. Prostate-specific antigen progression predicts overall survival in patients with metastatic prostate cancer: Data from Southwest Oncology Group trials 9346 (Intergroup Study 0162) and 9916. J Clin Oncol. 2009;27:2450–2456. doi: 10.1200/JCO.2008.19.9810. [DOI] [PMC free article] [PubMed] [Google Scholar]