Abstract
Objectives. We used qualitative and quantitative data collection methods to identify the health concerns of African American residents in an urban community and analyzed the extent to which there were consistencies across methods in the concerns identified.
Methods. We completed 9 focus groups with 51 residents, 27 key informant interviews, and 201 community health surveys with a random sample of community residents to identify the health issues participants considered of greatest importance. We then compared the issues identified through these methods.
Results. Focus group participants and key informants gave priority to cancer and cardiovascular diseases, but most respondents in the community health survey indicated that sexually transmitted diseases, substance abuse, and obesity were conditions in need of intervention. How respondents ranked their concerns varied in the qualitative versus the quantitative methods.
Conclusions. Using qualitative and quantitative approaches simultaneously is useful in determining community health concerns. Although quantitative approaches yield concrete evidence of community needs, qualitative approaches provide a context for how these issues can be addressed. Researchers should develop creative ways to address multiple issues that arise when using a mixed-methods approach.
Community-based participatory research is a collaborative process in which academic and community investigators work together to develop, implement, and evaluate interventions to improve the health of community residents.1–4 As part of these partnerships, formative research that includes focus groups and key informant interviews may be conducted to identify the health priorities and concerns of community residents and to obtain guidance from stakeholders on how these issues should be addressed and how to develop interventions.5,6 Although this information is critical to the implementation of intervention strategies, the generalizability of data obtained from these methods may be limited because individuals may self-select for participation in focus groups, and key informants are often identified using nonrandom methods. Thus, it may be important to use quantitative methods such as population-based random surveys along with qualitative approaches to ensure that the health priorities and concerns identified during the formative phase of academic–community partnerships are most representative of the community. However, limited empirical data exist on the congruence of data obtained using different methods.
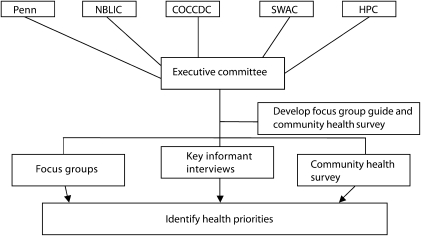
In 2005, members of 4 community-based organizations in Philadelphia, Pennsylvania, and researchers and staff at the University of Pennsylvania ( Figure 1) established the West Philadelphia Consortium to Address Disparities with funding from the National Center on Minority Health and Health Disparities.7 The purpose of our academic–community partnership is to conduct collaborative research to address disparities in chronic diseases that disproportionately affect African Americans in terms of morbidity and mortality using a community-based participatory framework. In keeping with the principles of community-based participatory research, the leaders of each community partner are listed as coinvestigators (R. R., V. B., E. D., J. P.) in the research alongside the academic-based coinvestigators. Moreover, each community partner receives its share of the funding directly. The organizations involved have all worked with academic investigators previously and realized that they share similar interests and could work together in a mutually beneficial way.
FIGURE 1.
Overview of mixed-methods approach: West Philadelphia Consortium to Address Disparities, Philadelphia, PA, 2006–2007.
Note. COCCDC = Christ of Calvary Community Development Corporation; HPC = Health Promotion Council of Southeastern Pennsylvania; NBLIC = National Black Leadership Initiative on Cancer; Penn = University of Pennsylvania; SWAC = Southwest Action Coalition.
We used a mixed-methods8 approach that consisted of focus groups, key informant interviews, and a fixed choice community health survey (CHS) with a random sample of residents to identify the health concerns of African American residents in the West Philadelphia community to determine the focus for pilot interventions that the partnership would develop and implement. We describe analyses that were undertaken to determine the extent to which there was consistency in the concerns residents identified using qualitative and quantitative methods, and we offer suggestions for managing inconsistencies that may arise when using a mixed-methods approach.
METHODS
Participants in this study were adult African American men and women. To be eligible to participate in focus groups and the CHS, individuals had to be at least 21 years of age and reside in West Philadelphia. Most key informant interviews were also with adult African American community residents. However, some of the key informants were from another racial or ethnic background and did not reside in the community, but were included because they had significant experience working in the community (e.g., health outreach workers, clergy).
Procedures
During regularly scheduled monthly meetings, community and academic partners determined the questions to ask community members about their health concerns. On the basis of feedback from community and academic partners, the study's principal investigator (C. H. H.) drafted the focus group and key informant discussion guides as well as the CHS. We then sent each of these drafts to each community partner via e-mail for review and input. All partners reviewed the edited survey and guides during a regular meeting and agreed on the final versions.
We recruited focus group participants into the study through self-referrals from newspaper advertisements that described the study as an opportunity for African American men and women to identify health issues that were important to them and other members of their community. We directed interested individuals to call a study telephone line for additional information. During this initial telephone call, we completed a screening interview to determine eligibility. At the end of the interview, we invited eligible individuals to participate in a focus group. We mailed logistical information about the focus groups to individuals who accepted the invitation. We conducted focus groups from April 2006 through October 2006. These consisted of 10 to 15 participants per group, and each session was about 1.5 to 2 hours long.
The project manager (B. W.), an African American woman, moderated the focus groups using a semistructured discussion guide. The members of the partnership jointly designed the discussion guide to understand how residents conceptualized health and to identify the conditions in their community that they believed were the most important to address. Specifically, we asked participants, “What do you believe are the most important health issues that need to be addressed in your community?” We also asked participants to describe community resources for health and to identify barriers to improving health outcomes in their community.
At the end of this general discussion, we used a modified form of the nominal group technique9,10 to reach consensus about which health issues were most important to address from an individual and community perspective. Specifically, we asked each participant to describe 4 to 5 health issues most important to them personally and an additional 4 to 5 health issues needing to be addressed in their community. We recorded each respondent's answers as they described them. We tallied the answers and listed the 3 conditions with the highest number of marks on a board as the most important. We also recorded the health conditions that the respondents described as being most important during this process in an Excel 2007 (Microsoft Corp., Redmond, WA) spreadsheet. We audiotaped and transcribed verbatim each focus group and gave participants a $20 gift certificate.
A community member of the consortium conducted key informant interviews from June 2006 through October 2006. We selected a purposive sample of key informants that members of the executive council had identified and recruited. We used a semistructured interview guide that was similar in content to the one we had used in the focus groups to conduct interviews with key informants. Specifically, we asked key informants to discuss the most important health issues that needed to be addressed in the community. Key informant interviews lasted between 1 and 2 hours and we audiotaped them. We also gave participants in the interviews a $20 gift certificate.
We completed the CHS with a random sample of African American residents of West Philadelphia from October through December 2006. The CHS was a semistructured interview that took approximately 20 to 30 minutes to complete. During the CHS, we also asked respondents 1 open-ended question: “If you could improve one health issue in your community, what would it be?” We recorded responses to this question verbatim. After this question, we asked respondents to indicate how concerned (1 = not at all concerned, 2 = a little concerned, 3 = somewhat concerned, 4 = very concerned) they were about diseases such as cancer, mental illness, diabetes, and substance abuse.
We determined the list of conditions included in this item on the basis of the leading health indicators and diseases for which the prevalence or mortality is greater among African Americans (e.g., obesity, cancer). We also asked respondents to indicate how likely it was that they would develop specific forms of cancer (e.g., breast, cervical, colon, prostate, lung) and cardiovascular conditions (e.g., heart disease, stroke, congestive heart failure), how life threatening these conditions were to them, and how much control they had over developing these diseases.
We adapted these items from those used in previous research.11,12 We also evaluated health behaviors (e.g., fruit and vegetable consumption, physical activity for exercise), access to health care services (e.g., location of usual source of care), and use of health care services (e.g., blood pressure screening) using items that we adapted from the Behavioral Risk Factor Surveillance System Survey.13 We also asked respondents to provide information about their socioeconomic background (e.g., income, marital status, education level) and medical history (e.g., diagnosis of high blood pressure, cancer). For this report, we analyzed responses to items in the CHS that asked respondents to identify a health issue in their community that they would improve, and we evaluated concerns about specific conditions because they were those most appropriate for comparing the concerns that participants identified in focus groups and key informant interviews.
The Center for Survey Research at the University of Virginia generated the sample for the CHS. Center for Survey Research staff generated a random-digit dial sample of telephone numbers in the 4 zip codes for West Philadelphia. To enhance response rates, we matched the random-digit dial sample against the telephone directory of listed numbers. We mailed introductory letters with information about the survey to households identified in this list. The contact rate for the survey was 67% (American Association for Public Opinion Research [AAPOR] contact rate 3), the cooperation rate was 43% (AAPOR cooperation rate 4), and the response rate was 24% (AAPOR response rate 4).14 Once we reached an eligible household, we selected respondents for participation in the survey using the “last or next birthday” method.15 We mailed individuals who completed the survey a $25 gift certificate.
Data Analysis
We used grounded theory16,17 to code the qualitative data and elicit key themes. We used the constant comparative method to compare themes across groups and key informants and to determine relationships among them. Trained research assistants coded and analyzed focus group and key informant transcripts using N6, 2006 version (QSR International, Melbourne, Australia) for analyzing qualitative data. For the quantitative CHS, we first generated descriptive statistics to characterize respondents in terms of socioeconomic background. We then generated a list of the conditions that respondents identified when we asked them whether there was one that needed to be improved. In the small number of cases in which respondents identified more than 1 condition, we included the first 1 recorded in our list. We then generated frequencies to characterize the number of individuals who identified each type of condition. We also generated frequencies to describe the extent to which participants were concerned about these conditions that they identified a priori.
Sample Characteristics
We completed 9 focus groups with 51 African American West Philadelphia residents and 27 key informant interviews; 201 residents completed the CHS. As shown in Table 1, there was some variation in the samples from these activities. For example, although focus group participants and key informants were fairly evenly split with regard to gender, the majority of participants in the CHS were women (71%). In addition, more of the key informants we interviewed had some college education or were college graduates and were more likely to be employed compared with participants in the focus group and CHS. Most participants in all 3 study activities were not married, and the mean age was approximately 50 years.
TABLE 1.
Sample Characteristics (n = 279): West Philadelphia Consortium to Address Disparities, Philadelphia, PA, 2006–2007
| Variable | Focus Groups, No. (%) or Mean (SD; range) | Key Informant Interviews, No. (%) or Mean (SD; range) | CHS, No. (%) or Mean (SD; range) |
| Gender | |||
| Men | 26 (51) | 13 (48) | 59 (29) |
| Women | 25 (49) | 14 (52) | 142 (71) |
| Marital status | |||
| Not married | 37 (77) | 13 (54) | 145 (74) |
| Married | 11 (23) | 11 (46) | 52 (26) |
| Education level | |||
| ≥ some college | 22 (46) | 25 (93) | 112 (58) |
| ≤ high school | 26 (54) | 2 (7) | 85 (42) |
| Employment status | |||
| Not employed | 25 (52) | 4 (15) | 86 (44) |
| Employed | 23 (48) | 22 (85) | 109 (56) |
| Income level | |||
| < $20 000 (< $15 000 in CHS) | 26 (60) | 2 (9) | 36 (25) |
| ≥ $20 000 (≥ $15 000 in CHS) | 17 (40) | 21 (91) | 107 (75) |
| Age, y | 50 (11.25; 23–72) | 51 (11.29; 32–74) | 51 (15.54; 21–65) |
Note. CHS = community health survey.
RESULTS
We asked focus group participants and key informants to identify the most important health issues that need to be addressed in their community. We used key informant interviews to get at a range of issues and, within the focus group discussions, we used the nominal group technique to arrive at consensus on the issues that emerged. Further, we analyzed the focus group and key informant interview data separately. However, despite differences in education and employment factors between key informants and focus group participants, there was tremendous overlap in the responses from these 2 groups; therefore, we report the analyses of these methods as concerns identified using qualitative methods.
Health Concerns Identified Using Qualitative Methods
The majority of both key informants and focus group participants identified chronic diseases, such as cancer and cardiovascular diseases, because of their personal health history and those of family, friends, and community members:
I have a couple of friends with breast cancer and prostate cancer, and a friend who died a couple of years ago, she had cancer. (Focus group participant)
Well a good friend of mine, he died of cancer. And my father, he had different cancers. And um, I see it throughout the community and how it [can] ravage your body, and the changes it take ’em through. I notice it's a horrible way to go. (Focus group participant)
My family has a history of cancer. I've had 2 mastectomies. I've had breast cancer twice. (Key informant)
High blood pressure, stroke, cancer, diabetes—either the individual has contracted one or maybe more of these diseases personally or someone in their family has been affected by it. Certainly, somebody that each member of the community knows has this issue. (Key informant)
I picked high blood pressure and diabetes ’cause they affect people in my family. People I know [are] always talking about blood pressure and diabetes. (Focus group participant)
In addition to identifying chronic illnesses, participants also identified risk factors such as obesity and being overweight, as well as environmental factors that contribute to the excess burden of disease among African Americans as conditions that need to be addressed:
The issue of nutrition I think is primary in the health issues I see in West Philadelphia. (Key informant)
First comes the weight and with the weight comes the diabetes, the high blood pressure. Now these things are not only from diet, but these things come from weight. (Focus group participant)
I gained 35, 50 pounds. My pressure shot through the roof. As I started gaining this weight, my pressure went up. (Focus group participant)
I think [we need] awareness on how to eliminate the possibility of cancer and cardiovascular problems by monitoring your diet and exercise. (Key informant)
Everyone needs to have a safe living environment … if you're living on the street, if you're living in a shelter, you're not necessarily living in the best living environment, which can impact your health. (Key informant)
Over the past 25–30 years, they started injecting the beef with hormones and these things are really impacting our health. (Focus group participant)
Just like they flood our communities with all these ads for cigarettes and all the ads for the fast food stuff, but if I tell someone about a health fair that's been going on for 2 hours, they know nothing about it. (Focus group participant)
[It's important to] eliminate some of these environmental hazards and educate people around environmental issues. (Key informant)
Participants also stated that interventions should focus on increasing access to information about these issues through education programs delivered to individuals:
Well, they have that thing called the wellness center. We need more centers like that that's designed to reach out to the community and bring you in and to assist with your medical problems slightly free of charge. (Focus group participant)
But having access to programs that benefit the residents and even having the folk that are affected by the problems to help design the programs … folk that are affected by the problem need to be a part of the solution. (Key informant)
Violence and sexually transmitted diseases (STDs), particularly HIV/AIDS, also emerged as health concerns, but to a much lesser degree than those reported.
Health Concerns Identified Using Quantitative Methods
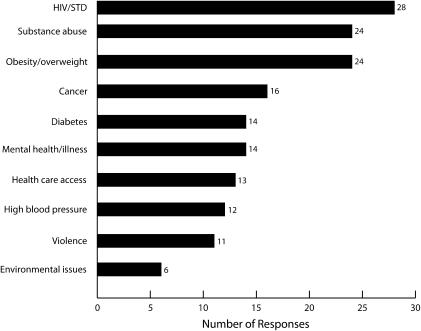
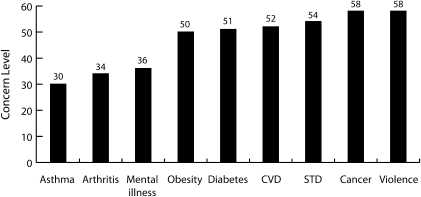
Overall, 94% of respondents in the CHS identified a health condition that they believed needed to be improved; 29 different conditions were identified. The top 10 conditions are shown in Figure 2. Of these conditions, most respondents (n = 28) identified STDs, primarily HIV/AIDS, and the fewest respondents (n = 6) identified environmental issues (e.g., pollution, neighborhood cleanliness). The same number of respondents identified several conditions. For instance, 24 respondents identified obesity as the condition that most needed to be improved, and 24 other respondents identified substance abuse as a priority. Figure 3 shows responses to concerns about specific conditions that were identified a priori. Participants were most concerned about cancer, violence, and STDs and were least concerned about asthma and arthritis.
FIGURE 2.
Health conditions from community health survey: West Philadelphia Consortium to Address Disparities, Philadelphia, PA, 2006–2007.
Note. STD = sexually transmitted disease.
FIGURE 3.
Descriptive information on health concerns from community health survey: West Philadelphia Consortium to Address Disparities, Philadelphia, PA, 2006–2007.
Note. CVD = cardiovascular disease; STD = sexually transmitted disease. Respondents were asked: “How concerned are you about . . .?” Respondents were not asked to rate their concern on a scale from 1-100. The scale was, “Not at all concerned,” “A little concerned,” “Somewhat concerned,” and “Very concerned.”
Community Forum
Upon completion of data analysis, we invited key informants and focus group participants to a community forum at which we shared our findings and asked for input about the accuracy of the results and the extent to which they felt the results were representative of members of the West Philadelphia community. We also sought their input about the best ways to address the concerns identified through the mixed methods. Thirty-eight research participants attended the event.
DISCUSSION
As part of developing an academic–community partnership to improve health outcomes among African American residents in an urban community, we used a mixed-methods approach to identify the health issues that were of greatest importance. We found that community residents were concerned about some health conditions, but there was variation in the priority they gave to these conditions in our qualitative and quantitative samples. The areas of greatest concern that focus group participants and key informants identified had a similar but different focus from those identified by CHS participants. For example, focus group participants and key informants gave priority to cancer and cardiovascular disease, but most respondents in the CHS indicated that STDs, substance abuse, and obesity were conditions in need of intervention. A smaller but substantial number of respondents in the CHS identified cancer and mental health. A possible reason for this variation is that different people were enrolled in the focus groups, key informant interviews, and the CHS.
Limitations
Many researchers use either quantitative or qualitative data collection methods to determine the health priorities of community members; however, there are limitations to using only 1 approach. For example, although a strength of using qualitative data collected through focus groups and key informant interviews is that it provides a context within which to frame priorities, selection bias may limit the generalizability of the results. Community members who participate in key informant interviews are typically selected for their stakeholder status within the community. This status may not be indicative of their awareness of community priorities as a whole but rather of the segment of the community with which they typically interact. Similarly, those who participate in focus groups may not be representative of the community and may also be inclined to follow the group dynamic with respect to views about health concerns.
Random, population-based surveys may address these limitations but are subject to low response rates, and selection factors may also reduce the generalizability of these data. Data collected quantitatively through random surveys may also leave out key contextual factors regarding why priorities exist, and ways to address them that may be couched in the experiences, knowledge, and beliefs of community members may be omitted using this type of approach.18 For example, investigators may be able to determine that community members have little knowledge about a particular health concern using quantitative approaches but may not be able to assess the core beliefs from which their concerns originate through this method. Additionally, identification of the most appropriate delivery method(s) for getting information to the study population as part of structured surveys may not be possible. Successful program development and implementation should incorporate all these components to identify the health conditions that are of greatest concern so that relevant and needed interventions are developed.
As an unintended consequence of using multiple methods to identify the health concerns of community residents, different issues may emerge. If multiple issues are identified, the partnership will have to make potentially difficult choices about which issues to address, especially when resources to develop interventions are limited. We faced this situation and spent a considerable amount of time reaching consensus about the focus for the intervention because we had allocated resources to support only 2 pilot interventions. We reconciled the differences in priorities that the qualitative and quantitative data suggested through a structured process that included submission of concepts for pilot projects from community and academic members of the partnership and group discussion about the merits of each concept, for example, whether it would address a community health priority and what the possible strengths and weaknesses of the study design would be.
Although the concepts that were submitted addressed the health concerns community residents identified in all 3 methods, we realized that the model of supporting 2 pilot interventions on the basis of the concepts that individual members of the partnership submitted was counterproductive for facilitating active collaboration. That is, we wanted to develop and implement pilot interventions that would maximize the participation of all consortium members. Therefore, we held a series of meetings to identify the overarching themes reflected in the pilot concepts. As a result of these meetings, we identified 2 broad research areas (e.g., changing the availability of and access to foods and providing education for health promotion and disease prevention). We ultimately developed and implemented an intervention that provided education about risk factors for cancer and cardiovascular disease (e.g., obesity) and ways to reduce exposure to these factors.7 The effects of this intervention on fruit and vegetable intake and physical activity are now being evaluated in a randomized trial funded by the National Center on Minority Health and Health Disparities. An additional issue we faced was that more concerns were identified than we had resources to address in the short term.
Community-based research is a long-term endeavor, and the data obtained from both the quantitative and qualitative methods provide critical information that community and academic members of our partnership can use to develop relevant intervention strategies. For instance, because health care access was identified as an issue in the CHS and was an underlying theme in the focus groups and key informant interviews, we developed a community-based navigator program for cancer control recently funded by the National Cancer Institute.
Conclusions
Obtaining input from community stakeholders is a critical component of community-based participatory research that is necessary for obtaining guidance to develop interventions.1–3 Although we found that different concerns may emerge when using both qualitative and quantitative approaches, both approaches were useful in determining health concerns of community residents and developing creative intervention approaches for addressing those concerns. For community–academic partnerships, it is important to plan strategies for reaching consensus on how to address these variations in a way that is amenable to all partners and beneficial to the participating community. Although there may be some variation in the extent to which different issues are prioritized, data from multiple sources can be used as the basis for developing plans for how to improve health outcomes.
Acknowledgments
The National Center on Minority Health and Health Disparities (grant R24MD001594), the National Cancer Institute (grant R01CA132656), and the National Center for Research Resources (grant RR024133) supported this research.
We give special thanks to interviewers at the Center for Survey Research at the University of Virginia who used the random-digit dial technique to complete our community health surveys.
Human Participant Protection
Institutional review board no. 8 at the University of Pennsylvania approved this research.
We obtained written informed consent from the focus group and key informant interview participants and verbal consent from the CHS survey participants.
References
- 1.Viswanathan M, Ammerman A, Eng E, et al. Community-based participatory research: assessing the evidence. Evid Rep Technol Assess (Summ). 2004;99:1–8 [PMC free article] [PubMed] [Google Scholar]
- 2.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202 [DOI] [PubMed] [Google Scholar]
- 3.Israel BA, Schulz AJ, Parker EA, Becker AB. Community-based participatory research: policy recommendations for promoting a partnership approach in health research. Educ Health (Abingdon). 2001;14(2):182–197 [DOI] [PubMed] [Google Scholar]
- 4.Jones L, Wells K. Strategies for academic and clinician engagement in community-participatory partnered research. JAMA. 2007;297(4):407–410 [DOI] [PubMed] [Google Scholar]
- 5.MacQueen KM, McLellan E, Metzger DS, et al. What is community? An evidence-based definition for participatory research. Am J Public Health. 2001;91(12):1929–1938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levy SR, Anderson EE, Issel LM, et al. Using multilevel, multisource needs assessment data for planning community interventions. Health Promot Pract. 2004;5(1):59–68 [DOI] [PubMed] [Google Scholar]
- 7.Halbert CH, Kumanyika S, Bowman M, et al. Participation rates and representativeness of African Americans recruited to a health promotion program. Health Educ Res. 2010;25(1)6–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Creswell JW, Plano Clark VL, Gutmann ML, Hanson WE. Advanced mixed methods research designs. : Tashakkori A, Teddlie C, Handbook of Mixed Methods in Social and Behavioral Research. Thousand Oaks, CA: Sage; 2003:209–240 [Google Scholar]
- 9.Dobbie A, Rhodes M, Tysinger JW, Freeman J. Using a modified nominal group technique as a curriculum evaluation tool. Fam Med. 2004;36(6):402–406 [PubMed] [Google Scholar]
- 10.Levine DA, Saag KG, Casebeer LL, et al. Using a modified nominal group technique to elicit director of nursing input for an osteoporosis intervention. J Am Med Dir Assoc. 2006;7(7):420–425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hughes C, Lerman C, Lustbader E. Ethnic differences in risk perception among women at increased risk for breast cancer. Breast Cancer Res Treat. 1996;40(1):25–35 [DOI] [PubMed] [Google Scholar]
- 12.National Cancer Institute Health Information National Trends Survey. Available at: http://hints.cancer.gov/hints. Accessed October 10, 2006
- 13.Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, GA: US Department of Health and Human Services; 2006 [Google Scholar]
- 14.American Association for Public Opinion Research Standard definitions. Final dispositions of case codes and outcomes for surveys. Available at: http://www.aapor.org/Standard_Definitions/1818.htm. Accessed June 4, 2010
- 15.Salmon CT, Nichols JS. The next-birthday method of respondent selection. Public Opin Q. 1983;47:270–276 [Google Scholar]
- 16.Charmaz K. Grounded theory: objectivist and constructivist methods. : Denzin NK, Lincoln YS, Handbook of Qualitative Research. Thousand Oaks, CA: Sage; 2000:509–535 [Google Scholar]
- 17.Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago: Aldine; 1967 [Google Scholar]
- 18.Farquhar SA, Parker EA, Schulz AJ, Israel BA. Application of qualitative methods in program planning for health promotion interventions. Health Promot Pract. 2006;7(2):234–242 [DOI] [PubMed] [Google Scholar]