Abstract
Aims
The objective of this study was to establish the extent of alcohol use disorders (AUDs) among drivers at risk for alcohol-related crashes. The prevalence of drivers with AUDs on U.S. roads on weekend evenings when alcohol-related crashes are most frequent is unknown. This study will inform laws and programs designed to reduce alcohol-involved crashes.
Design
Interviews using a 15-item AUD questionnaire with a stratified random sample of noncommercial drivers at 60 primary sampling locations in the 48 contiguous states on Fridays and Saturdays between 10 PM and 3 AM from July to November 2007.
Setting
Off-road locations into which a police officer directed a random selection of motorist passing the site.
Participants
4614 drivers of noncommercial vehicles.
Measurements
AUDs, including heavy drinking, alcohol abuse, and alcohol dependence.
Findings
Of the participating drivers, 73.7% were current drinkers (reported drinking in the last year). Among those drinkers, 14% were classifiable either as dependent drinkers or as abusive drinkers based on self-reports of drinking. Another 10% of the drivers were classified as heavy drinkers. Nearly half of the drivers in the survey who had BACs at or higher than the 0.08 grams per deciliter legal limit fell into one of those three AUD categories.
Conclusions
Survey data suggest that the majority of high-BAC drivers on U.S. roads show no clinical signs of an alcohol use disorder, but they are categorized as heavy drinkers. This suggests that environmental programs directed at reducing heavy drinking and brief behavioral interventions aimed at reducing episodes of excessive consumption have promise for reducing alcohol-related crashes.
Keywords: alcohol use disorders, drinking and driving, binge drinking, alcohol dependence, alcohol abuse, alcohol measurement, heavy drinking
INTRODUCTION
Crash Involvement of Drivers with Alcohol Use Disorders
Each year in the United States, 1.4 million motorists are arrested for driving while impaired (DWI). Approximately a third of the arrests involve drivers with a previous offense. Substantial research literature indicates that from a third to a half of the first DWI offenders can be classified as having a drinking problem [1, 2]. Estimates of alcohol use disorders (AUDs) run considerably higher for multiple DWI offenders, from 60 to 84% [3, 4]. Simpson, Mayhew, and Beirness [5] suggested that individuals who persist in driving at very high BACs are “hardcore” drinking drivers who are responsible for most serious alcohol-related crashes.
An alternative to the emphasis on hardcore drinking drivers is that the much larger number of normative drinkers, who despite being at a lower risk of crash involvement than the hardcore drinkers, account for most of the impaired-driving crashes. Hedlund and Fell [6] and Jones and Lacey [7], although noting the overrepresentation of repeat offenders in fatal crashes, pointed out that they still accounted for less than 10% of the total crashes. Baker and Chen [8] analyzed data from the 1993 National Mortality Followback Survey (NMFS), coupled with data from the Fatality Analysis Reporting System (FARS), in which the relatives and close associates were queried about drinking problems of fatally injured drivers. They concluded that only 25% of the drivers killed in single-vehicle crashes (where the driver is presumed responsible) were problem drinkers. Voas et al. [9], using data from the National Epidemiologic Survey of Alcohol-Related Conditions (NESARC) and the FARS, found that dependent (13.5%), abusive (4.5%), and binge drinkers (25.3%) comprised slightly less than half of the drinking drivers in fatal crashes, leaving 56% who could be classified as “normative” drinkers.
Lack of Data Fuels the Debate
These two alternative views of the drinking-and-driving problem are represented in an ongoing debate about policy issues. At stake are decisions regarding the allocation of increasingly scarce resources, either to specific deterrence programs designed to reduce recidivism among the relatively small number of convicted drinking drivers or to general deterrence programs aimed at the much larger number of normative or nondrinking drivers who have not been identified through an arrest for DWI. This issue is significant for national policy because, if the major segment of the impaired-driving problem involves individuals with clinical signs of alcohol abuse or dependence, program emphasis should be placed on efforts to identify and treat drivers with AUDs. The hardcore drinker concept supports more severe sentences for high-BAC drivers and repeat offenders [10]. Alternatively, the approach focusing on the very large number of normative drinkers emphasizes general deterrence through controls on alcohol sales and service [11], drinking-age laws [12] and enhanced impaired-driving enforcement programs [13, 14]. Largely, the lack of progress in this debate is caused by the limited data on drivers in crashes and the complete absence of data on the prevalence of AUDs among non-crash-involved drivers on the highways. This study was designed to produce data on the prevalence of AUDs among drivers on weekend evenings when alcohol consumption and impaired driving have been found to be the highest.
Aims
Although a large number of studies have assessed the AUD status of individuals convicted of DWI [1], and a more limited number of studies have assessed crash-involved drivers [7, 8, 15], with one small exception of the 6-state pilot project for this study [16], there have been no studies on the exposure of problem drinkers to crash involvement based on their prevalence on the road. The 2007 National Roadside Survey (NRS)[17], the fourth in a series of nationally representative surveys of weekend nighttime drivers conducted every decade, provided an opportunity to study AUD drivers by adding a brief 15-item questionnaire to the standard interview and breath test conducted in those surveys. This report covers the AUD prevalence information gained from that effort.
METHODS
The 2007 National Roadside Survey Procedures
A full description of the 2007 NRS procedures is provided in a report issued by the National Highway Traffic Safety Administration (NHTSA) [17]. As in the three previous NRS studies [18,19] the sampling system was based on the National Automotive Sampling System (NASS). The 60 primary sampling units that constitute the General Estimates System (GES), which is used to provide annual estimates of the number of crashes in the 48 contiguous United States, were selected as the sampling sites for the 2007 survey [17]. Surveys were conducted on Fridays and Saturdays during two periods, 10 PM to midnight and 1 AM to 3 AM, in off-road sites into which police officers directed the selected drivers. Each site contained three to five survey bays demarcated by traffic cones. The procedures for the survey were approved by the Pacific Institute for Research and Evaluation’s Institutional Review Board and are described in detail in the report on the 2007 survey procedures [17].
Administration of the AUD Survey
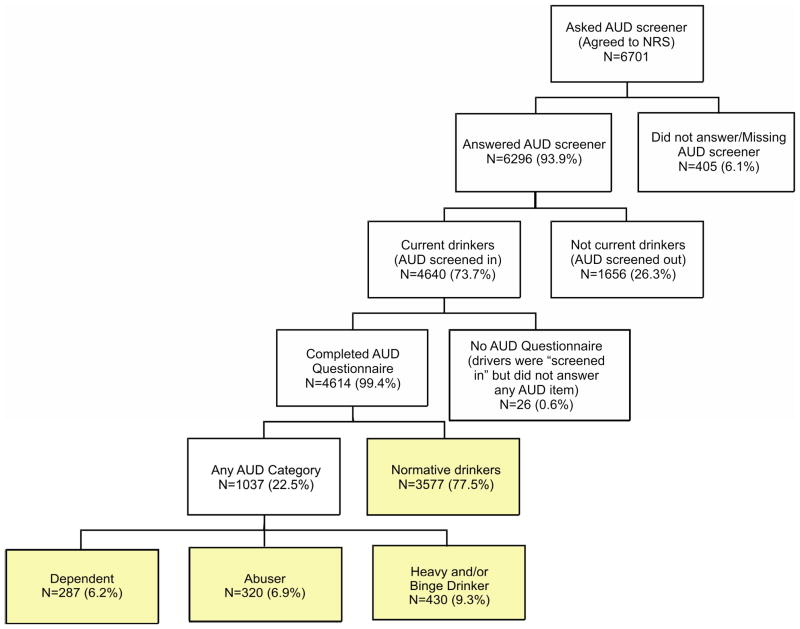
Figure 1 shows the stages of participation by the drivers at the survey sites that led to the final number of AUD respondents who provided usable data. Of the 8384 nighttime drivers who entered the survey sites and agreed to participate in the 2007 NRS study, 6701 (79.9%) completed the traditional survey questionnaire and were offered a $10 incentive to provide an oral fluid sample and an additional $5 incentive to complete the 15-item AUD questionnaire while the oral fluid sample was being collected. Of the 6701 respondents asked to complete the AUD questionnaire, 6296 (93.9%) accepted and were screened for participation in the AUD study, which was limited to participants who reported consuming alcohol in the past year. In response to item 1 of the AUD questionnaire, about 26% of the respondents reported that they had not had a drink in the past year (eg, were not current drinkers) and therefore were not asked to complete the rest of the AUD. This left 4640 current drinkers, 26 (.6%) of whom failed to complete the questionnaire, leaving 4614 or 99.4% who provided useable data. Of those, approximately 1 in 4 provided evidence of an AUD.
Figure 1.
Development of AUD analysis groups, nighttime
The response rate for the AUD portion of the program was very high. We suspect that given drivers’ participation in the protocol up to the point of the AUD survey, the additional items represented a very low response burden. A discussion of the 20% of nonresponders to the overall NRS program is included in the discussion section.
DWI Diagnostic Measures
Although the accuracy of the procedures used in diagnosing AUDs in the DWI population is limited [20, 21], there are several valuable scales that have been studied to date, including the Michigan Alcoholism Screening Test (MAST) and the Alcohol Use Disorders Identification Test (AUDIT). Conley [22] evaluated the construct validity of these instruments. Both exhibited acceptable internal consistency and correlated moderately well with each other (r=0.62). Although the MAST correlated more strongly (r=0.60) than the AUDIT (r=0.43) with Diagnostic and Statistical Manual of Mental Disorder Fourth Edition (DSM-IV) diagnoses, its utility with the broad driving population contacted in roadside surveys was questionable because the relatively severe dependent behaviors it covers might produce more refusals and might be too lengthy to be feasible as a rapid roadside assessment tool.
The AUDIT
The 10-item AUDIT has a brief three-item consumption scale (AUDIT-C) that has a correlation of 0.80 with the entire scale [23, 24]. This high correlation with the entire AUDIT scale renders the AUDIT-C ideal as a brief measure of heavy alcohol consumption. The AUDIT consumption subscale shows the best metric qualities as a measure for heavy drinking with high construct and criterion validity [22, 24, 25] and test-retest reliability [26]. However, additional measures beyond the AUDIT are required to fully explore dependence and abuse.
The AUDADIS
The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS) from the National Longitudinal Alcohol Estimate System (NLAES) is viewed as an appropriate tool for measuring alcohol abuse and dependence [27, 28]. The AUDADIS is a comprehensive, fully structured diagnostic tool developed for use in the NLAES survey, a large population-based study in the United States of AUDs and co-occurring health conditions [29]. Diagnoses from the AUDADIS are produced by algorithms that generate International Classification of Disease-Tenth version (ICD-10) and DSM-IV AUDs. The metric properties of the AUDADIS have been studied in great detail across cultures [30, 31] and settings [32,33]. The abuse scale has good validity, namely concordance rates with DSM-IV abuse of 0.5 [34]. The dependence scale of the AUDADIS also has high metric properties. The test-retest reliability (Kappa=0.68) exceeds clinical standards for a measurement instrument [34, 35, 36]. As a measure of validity, the AUDADIS has a correlation of 0.61 with the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) and a correlation of 0.69 with the Diagnostic Interview Schedule (DIS). These good reliability coefficients also provide additional support for the validity of the dependence syndrome and somewhat less so for the abuse syndrome.
The 2007 NRS Alcohol Use Disorder Measures
To assess AUDs, a 15-item version of the standard AUDADIS diagnostic instrument was constructed. From this questionnaire, three AUD measures covering dependence, abuse, and heavy drinking (AUDIT-C) were available. In addition, a current drinker category of respondents not falling into one of those three typologies was used as a measure of “normative” drinkers. Each of these is described in the following paragraphs.
Heavy drinkers
The first three items of the survey, shown in Table 1a, were scored as a unit to measure heavy drinking. They were derived from the AUDIT consumption subscale, also known as the AUDIT-C [22, 24, 26]. As shown in Table 1a, each of the three items is scored on a scale from 0 to 4, making the highest possible score for all three items equal 12. The standard scoring system (which was used in this study) specifies that a score of 6 or more is the criterion for heavy drinking for men and a score of 5 or more is the criterion for women.
Table 1.
15-item version of the standard AUDADIS diagnostic instrument used in 2007 NRS*
| a. AUDIT-C consumption items for measuring heavy drinking questions
| |||||
| 1. | In the past year, how often did you have a drink containing alcohol? | ||||
| never(0) | monthly or less(1) | 2–4 times/month(2) | 2–3 times/week(3) | 4 or more times/week(4) | |
|
| |||||
| 2. | In the past year, how many drinks containing alcohol did you have on a typical day when you were drinking? | ||||
| 1 or 2(0) | 2–4(1) | 5 or 6(2) | 7–9(3) | 10 or more (4) | |
|
| |||||
| 3. | In the past year, how often did you have six (five for a woman) or more drinks on one occasion? | ||||
| never(0) | less than monthly(1) | monthly(2) | weekly(3) | daily/almost daily(4) | |
|
| |||||
| b. AUDADIS alcohol abuse questions*
| |||||
| 4. | Did your drinking often interfere with taking care of your home or family or cause you problems at work or school? | ||||
| 5. | Did you more than once get into a situation while drinking or after drinking that increased your chances of getting hurt—like driving a car or other vehicle or using heavy machinery—after having had too much to drink? | ||||
| 6. | Did you get arrested, held at a police station or have legal problems because of your drinking? | ||||
| 7. | Did you continue to drink even though it was causing you trouble with your family of friends? | ||||
|
| |||||
| c. AUDADIS dependence questions*
| |||||
| 8. | Have you found that you have to drink more than you once did to get the effect you want? | ||||
| 9. | Did you find that your usual number of drinks had less effect on you than it once did? | ||||
| 10. | Did you more than once want to try to stop or cut down on your drinking, but you couldn’t do it? | ||||
| 11. | Did you end up drinking more or drinking for a longer period than you intended? | ||||
| 12. | Did you give up or cut down on activities that were important to you or gave you pleasure in order to drink? | ||||
| 13. | When the effects of alcohol were wearing off, did you experience some of the bad aftereffects of drinking—like trouble sleeping, feeling nervous, restless, anxious, sweating or shaking, or did you have seizures or sense things that weren’t really there? | ||||
| 14. | Did you spend a lot of time drinking or getting over the bad aftereffects of drinking? | ||||
| 15. | Did you continue to drink even though it was causing you to feel depressed or anxious or causing a health problem or making one worse? | ||||
All items prefaced with “In the last year.”
Abusive Drinkers
Items 4 through 7 on the survey (Table 1b) were derived from the AUDADIS [27,28]. The AUDADIS is constructed to have one item per DSM-IV symptom. A positive response to one or more of these items was the criterion for alcohol abuse in this study.
Dependent drinkers
Items 8 through 15 (Table 1c) were also taken from the AUDADIS. Items 8 and 9 both relate to the domain of tolerance and were scored as a single item. Items 10 through 15 each represent one DSM-IV diagnostic symptom of dependence. A total of seven diagnostic symptoms are therefore represented across the eight items. Three “yes” responses to any of the symptoms (items 8 and 9 counting as one item) were the criteria for alcohol dependence. If responses to four or more of the items were not provided, the case was scored as missing unless the three other available responses were “yes.”
Standard practice, implemented in this study, recognizes a hierarchical relationship between dependence and abuse such that individuals who qualify for both the dependence and abuse categories are classified as dependent and are not included in the abuse classification. Similarly, respondents falling into the heavy drinker category who also qualified as dependent or abusive were counted in the higher categories and not included in the heavy drinking category. Thus, the respondents assigned to each AUD category were independent based on the hierarchy: Dependent Drinkers>Abusive Drinkers>Heavy Drinkers.
Preliminary test of the AUD measures
An evaluation of the AUD measures was included as part of the preliminary field test program for the 2007 NRS [16]. The objective was (a) to demonstrate that weekend nighttime drivers interviewed at the roadside would agree to respond to the AUD questions and (b) to compare roadside responses with those responses collected in followup telephone interviews with the same respondents. The correlation between the roadside and telephone survey AUD dependence measure was .80; however, the abuse measure was much lower due to the tendency of the respondents to be more willing to admit to impaired driving (item 5) on the abuse scale in telephone followup compared to at the roadside. However, when that item was removed, the abuse scores for the roadside and telephone surveys correlated to .80.
Normative drinkers
Respondents who qualified as current year drinkers but who did not provide a response to the AUD survey that placed them in one of the three drinker categories were classified as normative drinkers. They served as a comparison group for the other drinking categories.
Demographic Characteristics of the Sample
Demographic data were collected as part of the traditional NRS study at the beginning of the survey procedure [17]. Gender was observed and recorded by the interviewer. The participant then responded to a series of questions covering the other demographic measures: age, employment, education, race, and ethnicity (Table 2).
Table 2.
Demographic characteristics of drivers by drinking category (percentages weighted)
| Characteristic | Dependent (%) | Abusive (%) | Heavy (%) | Normative (%) |
|---|---|---|---|---|
| n=335 | n=318 | n=499 | n=3503 | |
| Total (n=4655) | 7.19 | 6.83 | 10.72 | 75.26 |
| Gender | ||||
| Men (n=2936) | 68.9 | 67.22 | 67.18 | 61.81 |
| Women (n=1706) | 31.1 | 32.78 | 32.82 | 38.19 |
| Age | ||||
| <21 years (n=615) | 24.22 | 22.25 | 20.14 | 10.40 |
| 21–34 years (n=2175) | 60.23 | 45.67 | 52.16 | 44.93 |
| 35–44 years (n=863) | 5.63 | 18.62 | 16.19 | 20.18 |
| ≥ 45 years (n=989) | 9.91 | 13.46 | 11.52 | 24.49 |
| Ethnicity/race | ||||
| White or Caucasian (n=2285) | 58.46 | 57.89 | 62.00 | 45.89 |
| Black or African American (n=785) | 11.91 | 8.09 | 11.73 | 18.99 |
| Hispanic (n=1030) | 18.33 | 24.87 | 20.19 | 22.66 |
| Other (n=531) | 11.30 | 9.15 | 6.08 | 12.45 |
| Education | ||||
| Did not graduate high school/no GED (n=318) | 9.60 | 9.33 | 8.09 | 6.19 |
| High school graduate or GED (n=970) | 19.61 | 11.82 | 27.22 | 20.93 |
| Some college/college grad/some post-grad/post- grad degree (n=3355) | 70.79 | 78.85 | 64.70 | 72.88 |
| Employment | ||||
| Employed/self-employed (n=3816) | 71.67 | 79.05 | 82.97 | 83.36 |
| Student (n=402) | 21.39 | 13.05 | 12.70 | 6.45 |
| Unemployed/retired/homemaker/on disability/other (n=426) | 6.94 | 7.90 | 4.33 | 10.18 |
BAC Data
BAC was also collected as part of the traditional NRS procedure using an Intoxilizer SD-400 ™ handheld breath-test device [17]. For this study, the data were categorized into two levels: BAC <0.08 grams per deciliter (g/dL) and BAC ≥0.08 g/dL. A very high BAC is traditionally assessed at BAC ≥0.15 g/dL; however, only 37 drivers in the total sample tested at this level. We therefore used a threshold consistent with impaired driving and per se limits for drinking and driving and did not conduct separate analyses of the very high-BAC drivers.
Data Analysis
We examined the distribution of AUD categories, demographic characteristics, and BAC categories among weekend nighttime drivers. Data were analyzed using SAS statistical software (Version 9.1; SAS Institute, Cary, North Carolina). Logistic regression models were used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) for the highest BAC group for individual demographic characteristics. The high-BAC group, ≥ 0.08 g/dL, was used as the dependent variable. The model was adjusted for the independent variables: gender, age, ethnicity/race, employment status, and educational attainment. Proportions were weighted (1) to reflect the relative size of the driving population across geographic units and (2) to obtain population estimates using the weighting schematic for NRS data described by Lacey and colleagues in 2009 [17]. All data reported in Tables 2 through 4 and in the subsequent text are based on these weighted data.
Table 4.
Logistic regression results for analysis the AUD and moderating variables relationships to drivers with BACs>+0.08
| Total n= 4670 (current drinkers only; n’s weighted) | Odds ratio for BAC ≥0.08 | 95% confidence interval for OR | |
|---|---|---|---|
| Characteristics | |||
| Women (n=1720) | 0.50 | 0.32 | 0.76 |
| Reference: Men (n=2950) | |||
| Age Group | |||
| 21–34 years (n=2180) | 6.08 | 2.41 | 15.36 |
| 35–44 years (n=870) | 5.19 | 1.89 | 14.26 |
| 45+ years (n=998) | 5.85 | 2.12 | 16.10 |
| Reference: <21 years (n=623) | |||
| Race/Ethnicity | |||
| Other(n= 542) | 1.28 | 0.79 | 2.08 |
| Black or African American (n=786) | 1.09 | 0.69 | 1.72 |
| Hispanic (n=1037) | 1.01 | 0.55 | 1.86 |
| Reference: White or Caucasian (n= 2293) | |||
| Education Level | |||
| Did not graduate HS (n= 318) | 1.13 | 0.56 | 2.27 |
| Some college/College degree (n= 3369) | 0.62 | 0.42 | 0.94 |
| Reference: High School graduate (n= 984) | |||
| Employment status | |||
| Student (n= 401) | 1.93 | 0.99 | 3.79 |
| Unemployed/Retired/Homemaker/On disability/Other (n= 425) | 1.32 | 0.70 | 2.49 |
| Reference: Employed/self-employed (n=3844) | |||
| AUD Category | |||
| Dependent (n= 334) | 1.46 | 0.73 | 2.95 |
| Abuse (n= 318) | 1.40 | 0.66 | 2.96 |
| Heavy (n= 498) | 4.74 | 3.15 | 7.11 |
| Reference: Normative (n= 3502) | |||
RESULTS
Prevalence of AUD Drivers
Among all current drinkers, 7.2% could be categorized as dependent drinkers, 6.8% as abusive drinkers, and 10.0% as heavy drinkers, leaving 75.4% of the current drinkers who were classifiable as normative drinkers. Table 3 provides a comparison of the percentage of each AUD class in the total population of current drinkers to their distribution among drivers with BAC 0.08 g/dL. These percentages are weighted based on the 2007 sampling plan to provide national estimates [17]. Whereas 1 in 4 of all current drinkers could be classified as having an AUD, nearly half of the drivers with illegal BACs had an AUD, and one-third of all illegal BAC drivers were heavy drinkers.
Table 3.
Percentage of AUD, heavy, and normative drinkers among all current drinkers compared to participants with 0.08 g/dL or greater BACs (percentages weighted)
| Current Drinkers with any BAC (n=4684) | Current Drinkers with BAC ≥0.08 (n=133) | P (α=0.05) | |
|---|---|---|---|
|
Type of Drinker
| |||
| Dependent (n=335)a | 7.15 | 7.20 | 0.98 |
| Abusive (n=318) | 6.81 | 6.03 | 0.72 |
|
| |||
| Heavy (n=499) | 10.01 | 32.54 | <0.01 |
| Normative (n=3503) | 75.39 | 54.24 | <0.01 |
Dependent drinkers who also met abuse criteria were only classified as dependent, consistent with DSM criteria.
Relationship of AUD Categories to Driver BACs
Table 4 provides the results of the regression analysis relating AUD status to the BAC measured at the roadside. Listed are the five covariates entered into the analysis—gender, age, race/ethnicity, educational attainment, and employment status—with the AUD status measure. Two of the covariates, gender and age, demonstrate the expected relationship to a 0.08 g/dL BAC, with women and underage drivers less likely to be at that illegal level. Race/ethnicity and employment status were not significantly related to having a 0.08 g/dL BAC. Relative to normative drinkers, dependent and abusive drinkers were almost one and a half times as likely to have a 0.08 g/dL or greater BAC, while heavy drinkers were almost five times more likely to be at an illegal BAC. Drivers with at least some college were 60% less likely than persons with only a high school education to have a 0.08 g/dL or greater BAC.
DISCUSSION
Of the 2007 NRS participants who were screened for current year alcohol consumption, 75.5% (weighted) indicated that they had consumed alcohol in the last 12 months. This is substantially higher than the 55.1% 12-month prevalence in the 2007 National Household Survey on Drug Use and Health (NSDUH [29]). An important new finding in this study is that 14% (weighted) of all current drinkers among weekend nighttime drivers can be classified as either dependent or abusive, compared to 11.4% of respondents in the NSDUH. This verifies that individuals for whom there is evidence of an inability to control their drinking are on our highways in substantial numbers at high-risk driving times. An additional 10% (weighted) of the current drinkers reported heavy drinking, which was significantly associated with reaching an illegal BAC limit, even more so than being an abuser or dependent drinker. Developmentally, heavy drinkers may be sub-syndromic (that is not yet meeting clinical criteria for an AUD) and they continue to drink and drive in high numbers. On the other hand, clinically distinct abuse and dependence cases may be further along in the pathological continuum of alcohol-related problems (eg, joblessness, loss of a driver’s license) and are therefore less likely than heavy drinkers to be on the roadways due to these disorder-related circumstances. This hypothesis is partially supported by the overrepresentation of abuse and dependence cases in the non-employed categories compared to heavy drinkers, despite similar proportions of abuse and dependence cases in the current and high-BAC drinking categories.
Given the potential significance of these findings based on the unique 2007 NRS, it is important to keep in mind the limitations of this study. The sampling plan was based on the NASS used to estimate national crash statistics. Although this is a strength for the relevance of the data to national injury reduction, the data represent drivers at risk for crash involvement, not necessarily all U.S. drivers. Although drivers were selected at random, the 20% of the drivers entering the site who refused to participate in the survey may have affected the results because, typically, drivers in roadside surveys who refuse to participate have slightly higher BACs [19]. However, an attempt was made to convert a random sample of those drivers who initially refused to participate by offering a $100 incentive to complete the survey. Fifty percent of the drivers offered the incentive accepted and an analysis of their BACs demonstrated that they did not differ from the participants who initially agreed to the survey ([17], p. 12). Similarly, passive alcohol measures that detect alcohol in the air in front of the driver’s face were taken on all drivers regardless of participation in the NRS study to identify those drivers in potential need of assistance. There were also no statistically significant differences in passive alcohol measures between those who did and did not agree to participate. We therefore expect the possible underestimate of high-BAC or AUD drivers in our sample to be minimal.
Despite these limitations, this is the first national study to estimate the prevalence of AUDs among a sample of drivers at the roadside. This work is a first step in assessing the extent to which problem drinkers are represented on the roadways during the peak periods for alcohol-involved crashes, namely weekend nights. Although the proportion of drivers with a 0.08 g/dL or greater BAC were highest among the heavy drinkers, compared to abusive or dependent drinkers, this research converges with prior research that heavy episodic drinkers account for the largest proportion of DWI offenders. This study suggests that heavy drinkers also account for the largest proportion of high-BAC drivers on the roadways on weekend evenings. The largest proportion of high-BAC drivers were “normative” drinkers not falling into any problem-drinking category; normative drinkers represent the largest proportion of all drinkers, regardless of BAC at the roadside. What is most interesting about this finding is that the proportionate difference between high-BAC drivers and all other drivers is most pronounced for normative and heavy drinkers. There is a 28% reduction in the prevalence of normative drinkers in the high-BAC group compared to all current drinkers; yet, there is a more than threefold increase in the prevalence of heavy drinking in the high-BAC group compared to all current drinkers. There is no significant difference in the proportion of abusive or dependent drinkers among the current drinkers versus the high-BAC drinkers, making heavy drinkers the only drinkers overrepresented in the high-BAC group.
We sought to provide empirical estimates of alcohol use disorders in a national sample of living, non-crash-involved drivers and to determine which drivers are most at risk for high-BAC driving and possible alcohol-involved crashes. The findings provide a cross-sectional view of drinking and driving and further support the claim that heavy drinkers, and not those with clinically distinct alcohol abuse and dependence, are more likely to drive with high BACs. These data provide empirical support for further environmental interventions and general deterrence methods aimed at normative and heavy drinkers, versus targeted approaches aimed at clinically significant cases, such as those meeting abuse and dependence criteria.
Acknowledgments
This work was funded by the National Highway Traffic Safety Administration (Contract No. DTNH22-06-C-00040) and the National Institute on Alcohol Abuse and Alcoholism (Grant Nos. K05 AA14260, R01 AA0016407, and R21 AA015543).
Footnotes
Conflict of Interest: None.
Contributor Information
C Debra Furr-Holden, Email: dholden@jhsph.edu.
Robert B. Voas, Email: voas@pire.org.
John Lacey, Email: lacey@pire.org.
Eduardo Romano, Email: romano@pire.org.
Kristina Jones, Email: kjones@pire.org.
References
- 1.Cavaiola A, Wuth C. Assessment and treatment of the DWI offender. Binghamton, NY: The Haworth Press, Inc; 2002. [Google Scholar]
- 2.Wieczorek WF, Miller BA, Nochajski TH. The problem-drinker driver project. Research note 89-6. Albany, New York: New York State Divison of Alcoholism and Alcohol abuse; 1989. Bar versus home drinkers: different subgroups of problem-drinker drivers; pp. 1–2. [Google Scholar]
- 3.Wieczorek WF, Miller BA, Nochajski TH. Problem-Drinking Driver Project Research Note. Vol. 90. Buffalo, NY: Research Institute on Addictions; 1990. Alcohol diagnoses among DWI offenders; p. 6. [Google Scholar]
- 4.Perrine MW. Who are the drinking drivers? The spectrum of drinking drivers revisited. Alcohol Health Res World. 1990;14(1):26–35. [Google Scholar]
- 5.Simpson HM, Mayhew DR, Beirness DJ. Dealing with the hard core drinking driver. Ottawa, Canada: Traffic Injury Research Foundation; 1996. [Google Scholar]
- 6.Hedlund J, Fell J. Persistent drinking drivers in the U.S. 39th Annual Proceedings of the Association for the Advancement of Automotive Medicine; October 16–18, 1995; Chicago, IL. Des Plaines, IL: Association for the Advancement of Automotive Medicine; 1995. pp. 1–12. [Google Scholar]
- 7.Jones RK, Lacey JH. State of knowledge of alcohol impaired driving: Research on repeat DWI offenders. Washington, DC: National Highway Traffic Safety Administration; 2000. Report No.: DOT HS 809 027. [Google Scholar]
- 8.Baker SP, Chen LH. Determination of characteristics of fatally injured drivers. Washington, DC: National Highway Traffic Safety Administration & Johns Hopkins School of Public Health, Center for Injury Research and Policy; 2001. Report No.: DOT HS 809 380. [Google Scholar]
- 9.Voas R, Romano E, Tippetts AS, Furr-Holden CDM. Drinking status and fatal crashes: Which drinkers contribute most to the problem. 29th Annual Scientific Meeting of the Research Society on Alcoholism; 2006 June 24–28; Baltimore, Maryland: Research Society on Alcoholism; 2006. p. 1. [Google Scholar]
- 10.Robertson RD, Simpson HM. DWI system improvements for dealing with hard core drinking drivers: Adjudication & Sanctioning. Ottawa, Ontario, Canada: Traffic Injury Research Foundation; 2002. Dec, [Google Scholar]
- 11.Holder H. Drinking, alcohol availability and injuries: A systems model of complex relationships. In: Giesbrecht N, editor. Drinking and causalities: Accidents, poisonings, violence in an international perspective. London: Associated Book Publishers; 1988. pp. 138–148. [Google Scholar]
- 12.Fell JC, Fisher DA, Voas RB, Blackman K, Tippetts AS. The relationship of 16 underage drinking laws to reductions in underage drinking drivers in fatal crashes in the United States. 51st Annual Proceedings of the Association for the Advancement of Automotive Medicine; October 15–16, 2007; Chicago, IL. 2007. pp. 537–557. [PMC free article] [PubMed] [Google Scholar]
- 13.Fell JC, Voas RB. Reducing illegal blood alcohol limits for driving: Effects on traffic safety. In: Verster JC, Pandi-Perumal SR, Ramaekers JG, de Gier JJ, editors. Drugs, Driving and Traffic Safety. Basel, Switzerland: Birkhauser Verlag AG; 2009. pp. 415–437. [Google Scholar]
- 14.Voas RB, Holder HD, Gruenewald PJ. The effect of drinking and driving interventions on alcohol-involved traffic crashes within a comprehensive community trial. Addiction. 1997;92(Supplement 2):S221–S236. [PubMed] [Google Scholar]
- 15.Waller JA, Turkel HW. Alcoholism and traffic deaths. N Eng J Med. 1966;275:532–536. doi: 10.1056/NEJM196609082751005. [DOI] [PubMed] [Google Scholar]
- 16.Furr-Holden D, Voas RB, Lacey J, Kelley-Baker T, Romano E, Smart M. Toward national estimates of alcohol use disorders among drivers: Results from the National Roadside Survey Pilot Program. Traffic Inj Prev. 2009;10(5):403–409. doi: 10.1080/15389580903131498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lacey JH, Kelley-Baker T, Furr-Holden D, Voas RB, Moore C, Brainard K, et al. 2007 National Roadside Survey of Alcohol and Drug Use by Drivers: Methodology. Washington, DC: National Highway Traffic Safety Administration; 2009. Dec, Report No.: DOT HS 811 237. [Google Scholar]
- 18.Lestina DC, Greene M, Voas RB, Wells J. Sampling procedures and survey methodologies for the 1996 survey with comparisons to earlier National Roadside Surveys. Eval Rev. 1999;23(1):28–46. doi: 10.1177/0193841X9902300102. [DOI] [PubMed] [Google Scholar]
- 19.Voas RB, Wells J, Lestina D, Williams A, Greene M. Drinking and driving in the United States: The 1996 National Roadside Survey. Accid Anal Prev. 1998;30(2):267–275. doi: 10.1016/s0001-4575(97)00066-3. [DOI] [PubMed] [Google Scholar]
- 20.Allen JP. Assessment in alcoholism treatment: An overview. In: Allen JP, Wilson V, editors. Assessing alcohol problems: A guide for researchers and clinicians. 2. Washington, DC: National Institute on Alcohol Abuse and Alcoholism; 2003. pp. 1–12. [Google Scholar]
- 21.Lacey JH, Stewart JR, Council FM. Techniques for predicting high-risk drivers for alcohol countermeasures Volume I: Technical report. Washington, DC: U.S. Department of Transportation; 1979. May, Report No.: DOT HS 804–851. [Google Scholar]
- 22.Conley TB. Construct validity of the MAST and AUDIT with multiple offender drunk drivers. J Subst Abuse Treat. 2001;20(4):287–295. doi: 10.1016/s0740-5472(01)00159-3. [DOI] [PubMed] [Google Scholar]
- 23.Allen JP, Litten RZ, Fertig JB, Babor T. A review of research on the Alcohol Use Disorders Identification Test (AUDIT) Alcohol Clin Exp Res. 1997;21:613–619. [PubMed] [Google Scholar]
- 24.Chung T, Colby SM, Barnett NP, Monti PM. Alcohol use disorders identification test: Factor structure in an adolescent emergency department sample. Alcohol Clin Exp Res. 2002;26(2):223–231. [PubMed] [Google Scholar]
- 25.Meneses-Gaya C, Zuardi AW, Loureiro SR, Hallak JE, Trzesniak C, de Azevedo Marques JM, et al. Is the full version of the AUDIT really necessary? Study of the validity and internal construct of its abbreviated versions. Alcohol Clin Exp Res. 2010;34(8):1417–1424. doi: 10.1111/j.1530-0277.2010.01225.x. [DOI] [PubMed] [Google Scholar]
- 26.Babor TF, de la Fuente JR, Saunders J, Grant M. The Alcohol Use Disorders Identification Test: Guidelines for use in primary health care. Geneva: World Health Organization; 1992. [Google Scholar]
- 27.Cottler LB, Grant BF, Blaine J, Mavreas V, Pull C, Hasin D, et al. Concordance of DSM-IV alcohol and drug use disorder criteria and diagnoses as measured by AUDADIS-ADR, CIDI and SCAN. Drug Alcohol Depend. 1997;47(3):195–205. doi: 10.1016/s0376-8716(97)00090-2. [DOI] [PubMed] [Google Scholar]
- 28.Pull CB, Saunders JB, Mavreas V, Cottler LB, Grant BF, Hasin DS, et al. Concordance between ICD-10 alcohol and drug use disorder criteria and diagnoses as measured by the AUDADIS-ADR, CIDI and SCAN: Results of a cross-national study. Drug Alcohol Depend. 1997;47(3):207–216. doi: 10.1016/s0376-8716(97)00091-4. [DOI] [PubMed] [Google Scholar]
- 29.Substance Abuse and Mental Health Services Administration. Report No.: NSDUH Series H-34, DHHS Publication No. SMA 08–4343. Rockville, MD: Office of Applied Studies; 2008. Results from the 2007 National Survey on Drug Use and Health: National Findings. [Google Scholar]
- 30.Canino G, Bravo M, Ramirez R, Febo VE, Rubio-Stipec M, Fernandez RL, et al. Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): Reliability and concordance with clinical diagnoses in a Hispanic population. J Stud Alcohol. 1999;60(6):790–799. doi: 10.15288/jsa.1999.60.790. [DOI] [PubMed] [Google Scholar]
- 31.Vrasti R, Grant BF, Chatterji S, Ustun BT, Mager D, Olteanu I, et al. Reliability of the Romanian version of the alcohol module of the WHO Alcohol Use Disorder and Associated Disabilities: Interview Schedule - Alcohol/Drug- Revised. Eur Addiction Res. 1998;4(4):144–149. doi: 10.1159/000018947. [DOI] [PubMed] [Google Scholar]
- 32.Volk RJ, Steinbauer JR, Cantor SB, Holzer CE., III Alcohol Use and Disorders Identification Test (AUDIT) as screen for at-risk drinking in primary care patients of different racial/ethnic backgrounds. Addiction. 1997;92(2):197–206. [PubMed] [Google Scholar]
- 33.Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. Alcohol use disorder and associated disabilities interview schedule (AUDADIS): Reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend. 1997;44(2,3):133–141. doi: 10.1016/s0376-8716(97)01332-x. [DOI] [PubMed] [Google Scholar]
- 34.Üstün B, Compton W, Mager D, Babor T, Baiyewu O, Chatterji S, et al. WHO study on the reliability and validity of the alcohol and drug use disorder instruments: Overview of methods and results. Drug Alcohol Depend. 1997;47(3):161–169. doi: 10.1016/s0376-8716(97)00087-2. [DOI] [PubMed] [Google Scholar]
- 35.Grant BF, Harford TC. Comorbidity between DSM-IV alcohol use disorders and major depression: Results of a national survey. Drug Alcohol Depend. 1995;39(3):197–206. doi: 10.1016/0376-8716(95)01160-4. [DOI] [PubMed] [Google Scholar]
- 36.Grant JE, Kushner MG, Kim SW. Pathological gambling and alcohol use disorder. Alcohol Res Health. 2002;26(2):143–150. [Google Scholar]