Abstract
Context
Total hip arthroplasty (THA) is a common surgical procedure but little is known about longitudinal trends.
Objective
To examine demographics and outcomes of patients undergoing primary and revision THA between 1991 and 2008.
Design, Setting, and Participants
Observational cohort of 1,453,493 Medicare beneficiaries who underwent primary THA and 348,596 who underwent revision THA.
Outcomes
Changes in patient demographics and comorbidity; hospital length of stay (LOS); mortality; discharge disposition; and all-cause readmission rates.
Results
Between 1991 and 2008 the mean age for primary THA increased from 74.1 (95% CI, 74.0-74.1) years to 75.1 (95% CI, 75.1-75.2)(P=0.01) and 75.8 (95% CI, 75.7-75.9) to 77.3 (95% CI, 77.2-77.4) for revision THA (P<.001). The mean number of comorbid illnesses per patient increased from 1.0 (95% CI, 1.0-1.0) to 2.0 (95% CI, 2.0-2.0) for primary and 1.1 (95% CI, 1.1-1.1) to 2.3 (95% CI, 2.3-2.3) for revision THA (P<.001 for both). For primary THA, LOS decreased from 9.1 days (95% CI, 9.1-9.2) in 1991–1992 to 3.7 days (95% CI, 3.7-3.7) in 2007–2008 (P=0.002); unadjusted in-hospital and 30-day mortality decreased from 0.5% (95% CI, 0.5%-0.5%) to 0.2% (95% CI, 0.2%-0.2%)(P< 0.001) and 0.7% (95% CI, 0.7%-0.7%) to 0.4% respectively (95% CI, 0.4%-0.4%)(P< 0.001). The proportion of primary THA patients discharged home declined from 68.0% (95% CI, 67.8%-68.3%) to 48.2% (95% CI, 48.0%-48.4%)(P<.001); the proportion discharged to skilled care increased from 17.8% (95% CI, 17.6%-18.1%) to 34.3% (95% CI, 34.1%-34.5%) (P<.001); 30-day all-cause readmission increased from 5.9% (95% CI, 5.8%-6.1%) to 8.5% (95% CI, 8.4%-8.6%) (P<.001). For revision THA similar trends were observed in hospital LOS, in-hospital mortality, discharge disposition, and hospital readmission rates.
Conclusions
Among Medicare beneficiaries who underwent primary and revision hip arthroplasty between 1991 and 2008, there was a decrease in hospital LOS, but an increase in the rates of post-acute care and readmission.
BACKGROUND
Total hip arthroplasty (THA) is a safe and effective therapy for patients with advanced degenerative joint disease.1,2 In recent years there has been a dramatic increase in utilization of this procedure both in the United States (U.S) and abroad.3–6 There is a general assumption that increasing experience with THA has resulted in improvements in patient outcomes as has been observed in other procedures,7–9 but rigorous empirical data documenting such improvement are limited.10–14 This lack of data is striking given that an estimated 280,000 THA procedures are performed annually at a cost of more than $12 billion.5
The lack of rigorous evaluation of THA outcomes is somewhat surprising given ongoing efforts to regionalize surgical procedures to higher volume and higher quality hospitals.15–17 As a generally elective surgery, THA is precisely the type of procedure that should be amenable to regionalization. Moreover, the introduction of the Medicare prospective payment system (PPS) in 1983 provided hospitals with incentive to control costs.18,19 A particularly important cost-control mechanism has been through reducing hospital length-of-stay (LOS). However, there is growing concern that hospitals may be reducing LOS by discharging patients prematurely resulting in increased utilization of skilled-care facilities20,21 and increased patient readmissions thus eliminating much of the cost savings originally envisioned by the PPS.22,23
With this background, the objective of this study was to evaluate long term trends in the outcomes of Medicare beneficiaries undergoing primary and revision THA and explore whether reductions in hospital LOS might be associated with increases in discharge of patients to post-acute care settings and/or increases in readmission rates.
METHODS
Data
We used Medicare Provider Analysis and Review (MedPAR) Part A data files to identify fee-for-service beneficiaries who underwent primary or revision THA between 1991 and 2008. Patients were identified using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9CM) procedure codes (81.51 for primary and 8005, 8153, 0070, 0071, 0072, 0073for revision THA).24–27 The Part A files contain a range of data collected from discharge abstracts for all hospitalized fee-for-service Medicare enrollees including: patient demographics; ICD-9CM codes for primary and secondary diagnoses and procedures; admission source (e.g., emergency department or transfer from outside hospital); admission and discharge dates; discharge disposition (coded as 25 separate categories); death occurring up to three years after discharge; a unique patient identifier that allows for identification of patient readmissions; and each hospital’s unique six digit identification number. For purposes of this analysis patient race was categorized as white, black, other and missing. Comorbid illnesses present on the index admission were identified using algorithms described by Elixhauser et al.28,29 which consider 30 specific conditions and exclude comorbid conditions that may represent complications of care or that are related to the primary reason for hospitalization.
To perform our 18-year longitudinal study, we used two separate Medicare Part A data files obtained from the Centers for Medicare and Medicaid Services (CMS): one file extended from 1991 through 2005; and a second from 2006 through 2008. Each of these files contains an internally consistent unique patient identifier that allows for the tracking of individual patients across time within the file. However, because the unique patient identifiers differ across the two different data files, it was impossible to link individual patients across the two different files. Thus, for example, if a single patient were hospitalized in December, 2005 and readmitted again in January, 2006 the lack of a consistent unique identifier across the two files precluded us from determining whether a single patient were admitted and readmitted or whether two different patients were admitted (one in December, 2005 and another in January, 2006). From a practical standpoint, this had minimal impact on our results but did influence our methodological approach, as described below.
Our intention was to examine changes in outcomes of patients undergoing primary and revision THA procedures. As primary THA is most often an elective procedure while revision THA can be either an elective or more urgent procedure, we applied separate exclusion criteria to the primary and revision THA populations in accordance with prior studies.27,30,31 For primary THA we sequentially excluded patients with acute fractures (N=136,887), patients admitted through the emergency department (N=19,721), and patients admitted after transfer from another acute-care hospital (N=2,856); these exclusion criteria were developed to select a population of primary elective THA patients. Our revision THA population did not exclude these types of patients because revision THA is often an emergent or unscheduled procedure and thus exclusion of these populations would not make sense.
Outcomes of Interest
Our outcomes of interest included hospital length of stay (LOS), mortality (in-hospital, within 30-days and 90-days of admission), discharge disposition, and all-cause readmission within 30-days and 90-days of admission. Discharge disposition was stratified into six mutually exclusive categories: home; skilled care/intermediate care; transfer to another acute-care hospital; inpatient rehabilitation; dead; and other. We limited our 30-day readmission analysis to patients whose index hospitalization occurred prior to November 30, 2005 for procedures performed between 1991 and 2005, and prior to November 30, 2008 for procedures performed between 2006 and 2008 to allow for a full 30-day follow-up period. Similarly, our 90-day readmission analysis was limited to patients whose index hospitalization occurred prior to September 30, 2005 for procedures performed between 1991 and 2005 and prior to September 30, 2008 for procedures performed between 2006 and 2008. Patients with hospital LOS greater than one-year were excluded from the LOS analysis in accordance with other recent studies.22
Statistical Analysis
We examined the demographic characteristics and prevalence of key comorbid illnesses for patients who underwent THA during the study period; for simplicity, data are presented separately for each two-year period (e.g., 1991–92, 1993–94, etc). We used analysis of variance for comparisons of continuous variables and the Mantel-Hanzel chi-square test for categorical variables. All analyses were performed separately for primary and revision THA patients.
We compared rates of each of the outcomes described above for each of the two-year periods using similar statistical methods. We used graphical techniques to examine changes in LOS, mortality, discharge disposition, and readmission rates over the course of the study period. To account for the changing demographics of the primary and revision THA populations over time, we calculated risk-standardized mortality ratios (RSMR) that adjusted for age, sex (male, female), race (white, black, other, and unknown).32 Inclusion of patient demographics in calculating these rates is important given that prior studies have demonstrated differential complication and utilization rates for joint arthroplasty among different demographic groups.33–35 Again, all analyses were conducted separately for the primary and revision THA cohorts.
All p-values are 2-tailed, with p-values less than .05 deemed statistically significant. All statistical analyses were performed using SAS 9.2 (SAS Institute Inc., Cary, NC). This project was approved by the University of Iowa Institutional Review Board.
Sensitivity Analysis
To assess the robustness of our results, we performed a number of supplemental analyses. First, we repeated our analyses while restricting our analysis to the first primary or first revision hip arthroplasty procedure performed on each patient during a 12-month period; this eliminates patients who undergo “staged” bilateral arthroplasty procedures or complicated revisions. Second, we repeated our analyses after adding back the excluded populations described previously (e.g., fracture patients). Results of these analyses are available from the authors by request.
RESULTS
Our final study population included 1,453,493 elective primary total hip arthroplasty procedures and 348,596 revision hip arthroplasty procedures performed on Medicare beneficiaries between 1991 and 2008. For primary THA (Table 1) mean age increased from 74.1 (95% CI, 74.0-74.1) in 1991–1992 to 75.1 (95% CI, 75.1-75.2) in 2007–2008. The prevalence diabetes increased from 7.1% (95% CI, 7.0%-7.3%) to 15.5% (95% CI, 15.4%-15.7) and the prevalence of obesity increased from 2.2% (95% CI, 2.2%-2.3%) to 7.6% (95% CI, 7.5%-7.7%) (P< 0.001 for each).
Table 1.
Characteristics of medicare beneficiaries receiving primary THA between 1991 and 2008
| Characteristics | 1991–1992 | 1993–1994 | 1995–1996 | 1997–1998 | 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 |
|---|---|---|---|---|---|---|---|---|---|
| No. of hospitalizations | 124038 | 133287 | 146047 | 147317 | 145521 | 169429 | 189574 | 188335 | 209945 |
| Age, years, mean (SD) | 74.1 (6.0) | 74.1 (6.0) | 74.8 (6.1) | 75.1 (6.2) | 75.2 (6.2) | 75.3 (6.2) | 75.4 (6.2) | 75.6 (6.3) | 75.1 (6.5) |
| Sex, female, number, (%) | 79673 (64.2) | 85074 (63.8) | 93799 (64.2) | 94582 (64.2) | 93556 (64.3) | 109175 (64.4) | 121038 (63.8) | 118078 (62.7) | 130653 (62.2) |
| Race | |||||||||
| White, number, (%) | 113637 (91.6) | 123459 (92.6) | 137453 (94.1) | 138944 (94.3) | 137022 (94.2) | 159052 (93.9) | 177370 (93.6) | 176028 (93.5) | 195707 (93.2) |
| Black, number, (%) | 4573 (3.7) | 5001 (3.8) | 5668 (3.9) | 5683 (3.9) | 5806 (4.0) | 7032 (4.2) | 8064 (4.3) | 8287 (4.4) | 9729 (4.6) |
| Other, number, (%) | 1774 (1.4) | 1895 (1.4) | 1648 (1.1) | 2081 (1.4) | 2176 (1.5) | 2694 (1.6) | 3407 (1.8) | 3376 (1.8) | 3930 (1.9) |
| Missing, number, (%) | 4054 (3.3) | 2932 (2.2) | 1278 (0.9) | 609 (0.4) | 517 (0.4) | 651 (0.4) | 733 (0.4) | 644 (0.3) | 579 (0.3) |
| Comorbidity | |||||||||
| Diabetes, number, (%) | 8863 (7.1) | 10785 (8.1) | 13018 (8.9) | 14603 (9.9) | 15354 (10.6) | 19572 (11.6) | 24411 (12.9) | 27148 (14.4) | 32566 (15.5) |
| CHF, number, (%) | 3575 (2.9) | 4620 (3.5) | 5708 (3.9) | 6087 (4.1) | 6147 (4.2) | 7559 (4.5) | 8883 (4.7) | 8965 (4.8) | 8859 (4.2) |
| Obesity, number, (%) | 2774 (2.2) | 3631 (2.7) | 4599 (3.1) | 5165 (3.5) | 5440 (3.7) | 7444 (4.4) | 9622 (5.1) | 11387 (6.0) | 16007 (7.6) |
| Renal failure, number, (%) | 548 (0.4) | 657 (0.5) | 823 (0.6) | 829 (0.6) | 940 (0.6) | 1262 (0.7) | 1791 (0.9) | 4691 (2.5) | 8225 (3.9) |
| Number of comorbid conditions, mean (SD) | 1.0 (1.1) | 1.2 (1.2) | 1.3 (1.3) | 1.4 (1.3) | 1.5 (1.3) | 1.6 (1.3) | 1.8 (1.4) | 1.9 (1.4) | 2.0 (1.4) |
Other race includes Asian, Hispanic, North American Native, or other not specified.
P < 0.001 for all comparisons, except for age (P=0.01)
Trends were similar for revision THA (Table 2). In particular, mean age increased from 75.8 (95% CI, 75.7-75.9) in years 1991–1992 to 77.3 (95% CI, 77.2-77.4) in 2007–2008. The prevalence of diabetes increased from 7.2% (95% CI, 6.9%-7.4%) to 15.7% (95% CI, 15.3%-16.0%) and the prevalence of obesity increased from 1.4% (95% CI, 1.3%-1.5%) to 4.7% (95% CI, 4.5%-4.9%) (P< 0.001 for each).
Table 2.
Characteristics of medicare beneficiaries receiving revision THA between 1991 and 2008
| Characteristics | 1991–1992 | 1993–1994 | 1995–1996 | 1997–1998 | 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 |
|---|---|---|---|---|---|---|---|---|---|
| No. of hospitalizations | 31969 | 33772 | 36409 | 38703 | 38815 | 42972 | 42790 | 40488 | 42678 |
| Age, years, mean (SD) | 75.8 (6.9) | 75.9 (6.9) | 76.6 (6.9) | 76.9 (6.9) | 77.2 (6.9) | 77.2 (6.9) | 77.3 (6.9) | 77.5 (7.0) | 77.3 (7.2) |
| Sex, female, number, (%) | 20507 (64.1) | 21423 (63.4) | 23278 (63.9) | 24404 (63.1) | 24585 (63.3) | 26920 (62.6) | 26633 (62.2) | 25262 (62.4) | 26305 (61.6) |
| Race | |||||||||
| White, number, (%) | 29269 (91.6) | 31105 (92.1) | 33982 (93.3) | 36236 (93.6) | 36236 (93.4) | 39983 (93.0) | 39904 (93.3) | 37799 (93.4) | 39765 (93.2) |
| Black, number, (%) | 1333 (4.2) | 1481 (4.4) | 1689 (4.6) | 1786 (4.6) | 1770 (4.6) | 2099 (.9) | 1979 (4.6) | 1824 (4.5) | 1933 (4.5) |
| Other, number, (%) | 396 (1.2) | 417 (1.2) | 421 (1.2) | 515 (1.3) | 645 (1.7) | 749 (1.7) | 779 (1.8) | 787 (1.9) | 886 (2.1) |
| Missing, number, (%) | 971 (3.0) | 769 (2.3) | 317 (0.9) | 166 (0.4) | 164 (0.4) | 141 (0.3) | 128 (0.3) | 78 (0.2) | 94 (0.2) |
| Comorbidity | |||||||||
| Diabetes, number, (%) | 2290 (7.2) | 2819 (8.3) | 3589 (9.9) | 4166 (10.8) | 4470 (11.5) | 5391 (12.5) | 5841 (13.7) | 5926 (14.6) | 6685 (15.7) |
| CHF, number, (%) | 1679 (5.3) | 2299 (6.8) | 2824 (7.8) | 3083 (8.0) | 3303 (8.5) | 3878 (9.0) | 4207 (9.8) | 4187 (10.3) | 3880 (9.1) |
| Obesity, number, (%) | 448 (1.4) | 554 (1.6) | 813 (2.2) | 876 (2.3) | 967 (2.5) | 1255 (2.9) | 1413 (3.3) | 1588 (3.9) | 1588 (4.7) |
| Renal failure, number, (%) | 257 (0.8) | 321 (1.0) | 400 (1.1) | 455 (1.2) | 605 (1.6) | 744 (1.7) | 919 (2.1) | 1906 (4.7) | 2584 (6.1) |
| Number of comorbid conditions, mean (SD) | 1.1 (1.2) | 1.4 (1.3) | 1.6 (1.4) | 1.6 (1.4) | 1.8 (1.5) | 1.9 (1.5) | 2.1 (1.5) | 2.3 (1.5) | 2.3 (1.5) |
Other race includes Asian, Hispanic, North American Native, or other not specified.
P < 0.001 for all comparisons.
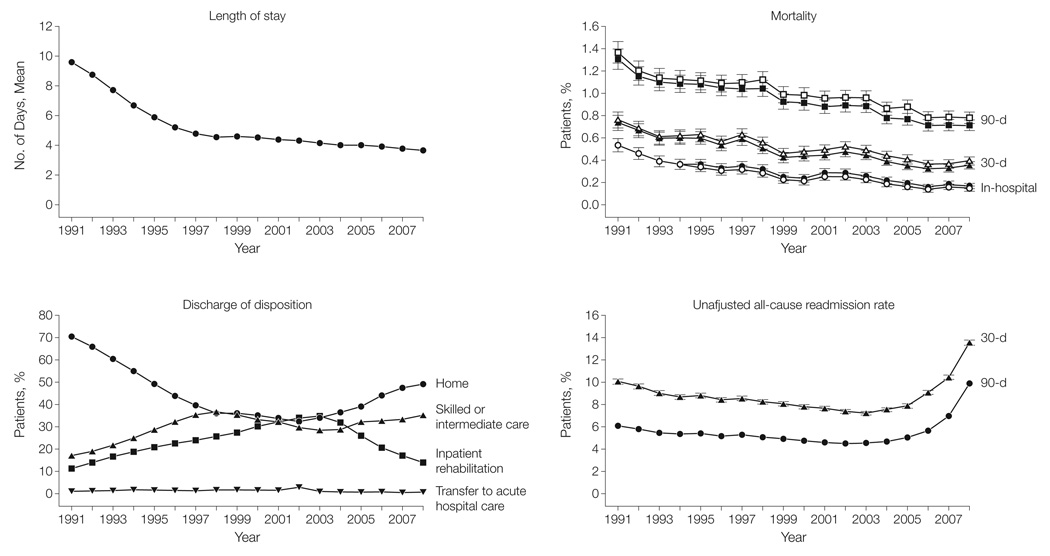
For primary THA mean hospital LOS declined from 9.1 days (95% CI, 9.1-9.2) in 1991–1992 to 3.7 days (95% CI, 3.7-3.7) in 2007–2008 (Table 3 and Figure 1), a 59.3% relative decrease (P< 0.001). In-hospital mortality after primary THA dropped from 0.5% (95% CI, 0.5%-0.5%) in 1991–1992 to 0.2% (95% CI, 0.2%-0.2%) in 2007–2008, a 60.0% relative reduction (P< 0.001). Likewise, 30-day mortality decreased from 0.7% (95% CI, 0.7%-0.7%) in 1991–1992 to 0.4% (95% CI, 0.4%-0.4%) in 2007–2008 (a relative reduction of 42.9%, P=0.004) and 90-day mortality declined from 1.2% (95% CI, 1.2%-1.3%) to 0.8%(95% CI, 0.7%-0.8%) (P<0.001). After adjustment for patient characteristics, risk-adjusted 30-day mortality over the study period declined from 0.7% (95% CI, 0.7%-0.8%) to 0.3% (95% CI, 0.3%-0.4%) and 90-day mortality dropped from 1.3% (95% CI, 1.2%-1.3%) to 0.7% (95% CI, 0.7%-0.7%) (P<0.001 for each).
Table 3.
Hospital LOS, discharge disposition, mortality, and readmission rates for primary THA
| 1991–1992 | 1993–1994 | 1995–1996 | 1997–1998 | 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 | |
|---|---|---|---|---|---|---|---|---|---|
| No. of hospitalizations | 124038 | 133287 | 146047 | 147317 | 145521 | 169429 | 189574 | 188335 | 209945 |
| LOS | |||||||||
| Mean | 9.1 (9.1,9.2) | 7.2 (7.2,7.2) | 5.5 (5.5,5.5) | 4.7 (4.7,4.7) | 4.5 (4.5,4.6) | 4.4 (4.4,4.4) | 4.1 (4.1,4.1) | 3.9 (3.9,4.0) | 3.7 (3.7,3.7) |
| Median (IQR) | 8 (7–10) | 7 (5–8) | 5 (4–6) | 4 (3–5) | 4 (3–5) | 4 (3–5) | 4 (3–4) | 3 (3–4) | 3 (3–4) |
| Mortality | |||||||||
| In-hospital, % | 0.5 (0.5,0.5) | 0.4 (0.3,0.4) | 0.3 (0.3,0.4) | 0.3 (0.3,0.4) | 0.2 (0.2,0.3) | 0.3 (0.3,0.3) | 0.2 (0.2,0.3) | 0.2 (0.2,0.2) | 0.2 (0.2,0.2) |
| 30-day, % | 0.7 (0.7,0.7) | 0.6 (0.6,0.6) | 0.6 (0.6,0.6) | 0.6 (0.6,0.6) | 0.5 (0.4,0.5) | 0.5 (0.5,0.5) | 0.5 (0.4,0.5) | 0.4 (0.4,0.4) | 0.4 (0.4,0.4) |
| 90-day, % | 1.2 (1.2,1.3) | 1.1 (1.0,1.1) | 1.1 (1.0,1.2) | 1.1 (1.1,1.2) | 1.0 (0.9,1.0) | 1.0 (0.9,1.0) | 0.9 (0.9,1.0) | 0.8 (0.8,0.9) | 0.8 (0.7,0.8) |
| Discharge disposition | |||||||||
| Home, % | 68.0 (67.8,68.3) | 57.5 (57.2,57.8) | 46.4 (46.1,46.6) | 37.8 (37.5,38.0) | 35.5 (35.3,35.7) | 33.0 (32.7,33.2) | 35.1 (34.9,35.3) | 41.5 (41.3,41.7) | 48.2 (48.0,48.5) |
| Skilled or intermediate care, % | 17.8 (17.6,18.1) | 23.2 (23.0 23.5) | 30.3 (30.1,30.6) | 36.0 (35.8,36.2) | 34.2 (34.0,34.5) | 30.9 (30.7,31.1) | 28.4 (28.2,28.6) | 32.4 (32.2,32.6) | 34.3 (34.1,34.5) |
| Transfer to other acute care hospital, % | 1.0 (0.9,1.0) | 1.2 (1.1,1.2) | 1.3 (1.2,1.3) | 1.2 (1.2,1.3) | 1.3 (1.3,1.4) | 1.9 (1.8,2.0) | 0.8 (0.7,0.8) | 0.6 (0.6,0.6) | 0.4 (0.4,0.5) |
| In-hospital death, % | 0.5 (0.5,0.5) | 0.4 (0.3,0.4) | 0.3 (0.3,0.4) | 0.3 (0.3,0.4) | 0.2 (0.2,0.3) | 0.3 (0.3,0.3) | 0.2 (0.2,0.3) | 0.2 (0.2,0.2) | 0.2 (0.2,0.2) |
| Inpatient rehabilitation, % | 12.6 (12.4,12.8) | 17.6 (17.4,17.8) | 21.6 (21.4,21.8) | 24.6 (24.4,24.9) | 28.6 (28.4,28.9) | 33.1 (32.9,33.3) | 33.4 (33.2,33.6) | 23.0 (23.2,22.8) | 15.0 (14.9,15.2) |
| Other, % | 0.0 (0.0,0.1) | 0.1 (0.1,0.1) | 0.1 (0.0,0.1) | 0.1 (0.0,0.1) | 0.1 (0.0,0.1) | 0.8 (0.8,0.9) | 2.0 (2.0,2.1) | 2.3 (2.3,2.4) | 1.9 (1.8,1.9) |
| All-cause readmission | |||||||||
| 30-day, % | 5.9 (5.8,6.1) | 5.4 (5.3,5.5) | 5.3 (5.2,5.4) | 5.2 (5.1,5.3) | 4.8 (4.7,4.9) | 4.6 (4.5,4.7) | 4.6 (4.5,4.7) | 5.4 (5.3,5.5) | 8.5 (8.4,8.6) |
| 90-day, % | 9.8 (9.7,10.0) | 8.8 (8.7,9.0) | 8.6 (8.5,8.8) | 8.4 (8.3,8.5) | 7.9 (7.8,8.1) | 7.5 (7.4,7.6) | 7.4 (7.3,7.5) | 8.6 (8.4,8.7) | 11.9 (11.7,12.0) |
Abbreviation: IQR, interquartile range.
Mean and % accompanied by (95% Confidence Intervals)
All-cause 30-day readmission limited to patients whose index hospitalization was before Nov 31th, 2005 between 1991 and 2005, and Nov 31th, 2008 between 2006 and 2008; 90-day readmission limited to patients whose index hospitalization was before Sep 30th, 2005 between 1991 and 2005, and Sep 30th, 2008 between 2006 and 2008.
P < 0.001 for all comparisons.
Figure 1.
The proportion of primary THA patients discharged home declined from 68.0% (95% CI, 67.8%-68.3%) in 1991–1992 to 48.2% (95% CI, 48.0%-48.5%) in 2007–2008 while the proportion of patients discharged to skilled or intermediate care increased from 17.8%% (95% CI, 17.6%-18.1%) to 34.3% (95% CI, 34.1%-34.5%) (P<.001 for both) (Table 3 and Figure 1). The 30-day all-cause readmission rate declined from 5.9% (95% CI, 5.8%-6.1%) in 1991–1992 to 4.6% (95% CI, 4.5%-4.7%) in 2001–2002 (P<.001) before increasing to 8.5% (95% CI, 8.4%-8.6%) in 2007–2008 (P<.001); results were similar for 90-day readmission rates.
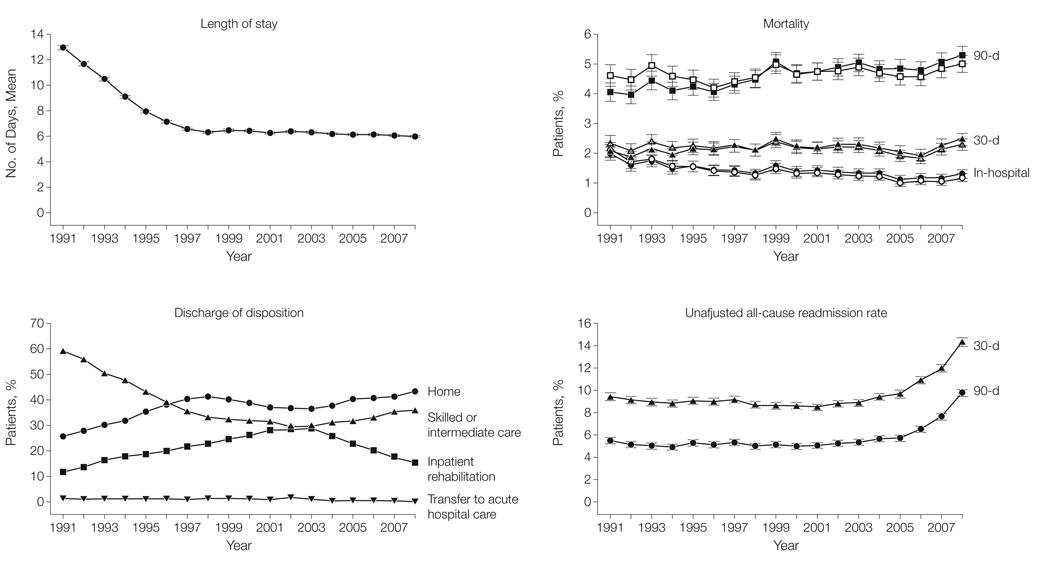
For revision THA mean hospital LOS declined from 12.3 days (95% CI, 12.2-12.4) in 1991–1992 to 6.0 days (95% CI, 6.0-6.1)in 2007–2008 (Table 4 and Figure 2), a 51.2% relative decrease (P< 0.001). Unadjusted in-hospital mortality after revision THA dropped from 1.8% (95% CI, 1.6%-1.9%) in 1991–1992 to 1.2% (95% CI, 1.1%-1.3%) in 2007–2008, a 33.3% relative reduction (P< 0.001). Alternatively during the study period unadjusted 30-day mortality increased from 2.0% (95% CI, 1.8%-2.1%) in 1991–1992 to 2.4% (95% CI, 2.2%-2.5%) in 2007–2008 (an 20.0% relative increase) (P=0.004) and 90-day mortality increased from 4.0% (95% CI, 3.8%-4.2%) to 5.2% (95% CI, 5.0%-5.4%) (a 30.0% relative increase) (P<0.001). However, after adjustment for patient characteristics, risk-adjusted 30-day mortality remained stable within a narrow range between 1.9% and 2.3% (P = 0.22) while adjusted 90-day mortality remained near 4.5% throughout the study period (P = 0.16).
Table 4.
Hospital LOS, discharge disposition, mortality, and readmission rates for revision THA
| 1991–1992 | 1993–1994 | 1995–1996 | 1997–1998 | 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 | |
|---|---|---|---|---|---|---|---|---|---|
| No. of hospitalizations | 31969 | 33772 | 36409 | 38703 | 38815 | 42972 | 42790 | 40488 | 42678 |
| LOS | |||||||||
| Mean | 12.3 (12.2, 12.4) | 9.8 (9.7,9.9) | 7.5 (7.5,7.6) | 6.4 (6.4,6.5) | 6.5 (6.4,6.5) | 6.3 (6.3,6.4) | 6.3 (6.2,6.3) | 6.1 (6.1,6.2) | 6.0 (6.0,6.1) |
| Median (IQR) | 9 (7–13) | 7 (6–11) | 6 (4–8) | 5 (4–7) | 5 (4–7) | 5 (4–7) | 5 (3–7) | 4 (3–7) | 4 (3–7) |
| Mortality | |||||||||
| In-hospital, % | 1.8 (1.6,1.9) | 1.6 (1.5,1.8) | 1.5 (1.4,1.6) | 1.4 (.2,1.5) | 1.5 (1.4,1.6) | 1.4 (1.3,1.5) | 1.3 (1.2,1.4) | 1.1 (1.0,1.3) | 1.2 (1.1,1.3) |
| 30-day, % | 2.0 (1.8,2.1) | 2.0 (1.9,2.2) | 2.1 (2.0,2.3) | 2.2 (2.0,2.3) | 2.4 (2.2,2.5) | 2.2 (2.1,2.4) | 2.2 (2.1,2.4) | 2.0 (1.9,2.1) | 2.4 (2.2,2.5) |
| 90-day, % | 4.0 (3.8,4.2) | 4.3 (4.0,4.5) | 4.2 (3.9,4.4) | 4.4 (4.2,4.6) | 4.9 (4.7,5.1) | 4.8 (4.6,5.0) | 4.9 (4.7,5.1) | 4.8 (4.6,5.0) | 5.2 (5.0,5.4) |
| Discharge disposition | |||||||||
| Home, % | 57.4 (56.8,57.9) | 48.9 (48.4,49.5) | 40.9 (40.4,41.4) | 34.2 (33.7,34.6) | 32.0 (31.6,32.5) | 30.7 (30.3,31.1) | 30.4 (30.0, 30.8) | 32.3 (31.8,32.7) | 35.4 (34.9,35.8) |
| Skilled or intermediate care, % | 26.7 (26.2,27.1) | 30.9 (30.4,31.4) | 36.8 (36.3,37.3) | 40.9 (40.4,41.3) | 39.4 (39.0,39.9) | 36.8 (36.4,37.3) | 36.9 (36.5,37.4) | 40.5 (40.0,41.0) | 42.4 (42.0,42.9) |
| Transfer to other acute care hospital, % | 1.4 (1.2,1.5) | 1.4 (1.3,1.6) | 1.4 (1.3,1.6) | 1.4 (1.3,1.5) | 1.6 (1.5,1.7) | 1.7 (1.6,1.8) | 1.1 (1.0,1.2) | 0.8 (0.7,0.9) | 0.6 (0.5,0.6) |
| In-hospital death, % | 1.8 (1.6,1.9) | 1.6 (1.5,1.8) | 1.5 (1.4,1.6) | 1.4 (.2,1.5) | 1.5 (1.4,1.6) | 1.4 (1.3,1.5) | 1.3 (1.2,1.4) | 1.1 (1.0,1.3) | 1.2 (1.1,1.3) |
| Inpatient rehabilitation, % | 12.7 (12.3,13.0) | 17.0 (16.6,17.4) | 19.3 (18.9,19.7) | 22.2 (21.8,22.6) | 25.4 (24.9,25.8) | 28.5 (28.1,28.9) | 27.3 (26.8,27.7) | 21.6 (21.2,22.0) | 16.5 (16.1,16.9) |
| Other, % | 0.1 (0.1,0.2() | 0.1 (0.0,0.1) | 0.1 (0.0,0.1) | 0.1 (0.0,0.1) | 0.1 (0.0,0.1) | 0.9 (0.8,1.0) | 3.0 (2.8,3.2) | 3.7 (3.5,3.9) | 3.9 (3.7,4.1) |
| All-cause readmission | |||||||||
| 30-day, % | 8.7 (8.3,9.0) | 8.0 (7.8,8.3) | 8.4 (8.2,8.7) | 8.4 (8.1,8.7) | 8.2 (7.9,8.5) | 8.4 (8.1,8.6) | 8.9 (8.7,9.2) | 9.9 (9.6,10.2) | 14.1 (13.8,14.5) |
| 90-day, % | 15.1 (14.7,15.5) | 14.4 (14.1,14.8) | 14.7 (14.3,15.0) | 14.5 (14.2,14.9) | 14.0 (13.6,14.3) | 14.0 (13.47,14.4) | 14.9 (14.5,15.2) | 16.9 (16.5,17.3) | 21.2 (20.8,21.6) |
Abbreviation: IQR, interquartile range.
Mean and % accompanied by (95% Confidence Intervals)
All-cause 30-day readmission limited to patients whose index hospitalization was before Nov 31th, 2005 between 1991 and 2005, and Nov 31th, 2008 between 2006 and 2008; 90-day readmission limited to patients whose index hospitalization was before Sep 30th, 2005 between 1991 and 2005, and Sep 30th, 2008 between 2006 and 2008.
P < 0.001 for all comparisons, except for 30-day mortality (P=0.004)
Figure 2.
The proportion of revision THA patients discharged home declined from 57.4% (95% CI, 56.8%-57.9%)in 1991–1992 to 35.4% (95% CI, 34.9%-35.8%) in 2007–2008 while the proportion of patients discharged to skilled or intermediate care increased from 26.7% (95% CI, 26.2%-27.1%) to 42.4% (95% CI, 42.0%-42.9%) (P<.001 for both) (Table 4 and Figure 2). The 30-day all-cause readmission rate decreased from 8.7% (95% CI, 8.3%-9.0%) in 1991–1992 to 8.2% (95% CI, 7.9%-8.5%) in 1999–2000 (P<.001) before increasing to 14.1% (95% CI, 13.8%-14.5%) in 2007–2008 (P<.001) with similar results for 90-day readmission rates.
DISCUSSION
In an analysis of Medicare administrative data from 1991–2008, we identified a number of interesting trends. We found that despite increasing patient complexity, both unadjusted and adjusted mortality for primary THA showed substantial improvement over time. Alternatively, for revision THA unadjusted mortality appeared to increase modestly but this increase was largely explained by increasing patient complexity. Most importantly, marked declines in hospital LOS for both primary and revision THA seemed to correspond with an increase in the proportion of patients who were discharged to post-acute care and an increase in patient readmissions.
A number of our findings warrant further discussion. First, our finding of increasing complexity of both primary and revision THA patients is important. While a number of studies have documented increasing complexity of patients in the cardiovascular disease literature,22,23,36 few studies have evaluated trends in patient complexity in orthopaedics and most have focused on knee arthroplasty.1,37–39 Our finding of an increase in the average age of both primary and revision THA patients suggests that at least some of the increase in patient complexity is real and is not simply an artifact of more aggressive coding practices (aka, upcoding).40
Our finding of increased patient complexity is particularly important when considering the changes in patient mortality that we observed. We found clinically and statistically significant reductions in primary THA mortality, albeit from very low baseline levels. Alternatively, the finding of an increase in revision THA mortality in unadjusted analyses was somewhat unexpected; the finding that this increase in mortality was no longer significant in adjusted analyses is reassuring. The absence of similar large-scale studies of the U.S. hip arthroplasty population with which to compare our results highlights the need for more rigorous study of THA outcomes.
Second, the marked decrease in hospital LOS for both primary and revision THA is interesting and has significant policy implications. The motivation for hospitals to reduce LOS under the Medicare prospective payment system has been well described previously,41,42 but the impact of declining LOS is much less clear. While Bueno et al. noted that reductions in LOS for Medicare beneficiaries hospitalized with congestive heart failure were accompanied by an increase in readmission rates,22 a prior study by Baker et al. found that reductions in LOS were not associated with an increase in readmissions.43 To the best of our knowledge no prior studies have evaluated the impact of reductions in LOS in regard to joint arthroplasty.
We found that the reduction in hospital LOS in both primary and revision THA patients was accompanied by a significant increase in the proportion of patients discharged to post-acute care facilities (i.e., nursing homes and rehabilitation centers) and a significant reduction in the proportion of patients discharged directly home. Moreover, we found that while the reduction in hospital LOS was not associated with an increase in readmission rates between 1992 and 1999, in more recent years readmission rates have risen markedly. Together these findings suggest that the old adage that there is no such thing as a free lunch may hold when it comes to hospital LOS; reductions in LOS accompanied by an increase in patient discharges to skilled care facilities and an increase in readmission rates. These findings reinforce the potential wisdom of moving to bundled payments and/or reimbursement for episodes of care as a way for incentivizing the “correct” LOS rather than perpetual reductions in LOS that seem to be occurring.
Our study has a number of limitations that warrant brief mention. First, our study was limited to fee-for-service Medicare beneficiaries and thus extrapolation to other populations should be done with caution. That said, more than 60% of all THA procedures are performed on Medicare enrollees, making this an appropriate data-set for studying THA. Second, our study relied upon administrative data and thus we were unable to evaluate a number of important arthroplasty outcomes including functional status and patient satisfaction.
In conclusion, mortality after primary THA has declined moderately over time and mortality after revision THA has remained stable despite substantial increases in patient complexity. There have also been marked reductions in hospital LOS and rising readmission rates.
ACKNOWLEDGEMENTS
Dr. Cram was supported by a K23 career development award (RR01997201) from the NCRR at the NIH and the Robert Wood Johnson Physician Faculty Scholars Program. This work is also funded by R01 HL085347-01A1 from NHLBI at the NIH (Cram) and R01 AG033202 (Li). The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Dr. Cram has received consulting fees from The Consumers Union (publisher of Consumer Reports Magazine) and Vanguard Health Inc. for advice he provided on quality improvement initiatives. Dr. Cram and Ms. Lu had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
None of the authors have any conflicts of interest.
REFERENCES
- 1.Khatod M, Inacio M, Paxton EW, et al. Knee replacement: epidemiology, outcomes, and trends in Southern California: 17,080 replacements from 1995 through 2004. Acta Orthop. 2008 Dec;79(6):812–819. doi: 10.1080/17453670810016902. [DOI] [PubMed] [Google Scholar]
- 2.Katz JN, Phillips CB, Baron JA, et al. Association of hospital and surgeon volume of total hip replacement with functional status and satisfaction three years following surgery. Arthritis & Rheumatism. 2003 Feb;48(2):560–568. doi: 10.1002/art.10754. [see comment] [DOI] [PubMed] [Google Scholar]
- 3.Merx H, Dreinhofer K, Schrader P, et al. International variation in hip replacement rates. Annals of the Rheumatic Diseases. 2003 Mar;62(3):222–226. doi: 10.1136/ard.62.3.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lohmander LS, Engesaeter LB, Herberts P, Ingvarsson T, Lucht U, Puolakka TJ. Standardized incidence rates of total hip replacement for primary hip osteoarthritis in the 5 Nordic countries: similarities and differences. Acta Orthop. 2006 Oct;77(5):733–740. doi: 10.1080/17453670610012917. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. U.S. Centers for Disease Control; 2009. Health, United States, 2009. [Google Scholar]
- 6.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. Journal of Bone and Joint Surgery. 2005 Jul;87(7):1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 7.Venkitachalam L, Kip KE, Selzer F, et al. Twenty-year evolution of percutaneous coronary intervention and its impact on clinical outcomes: a report from the National Heart, Lung, and Blood Institute-sponsored, multicenter 1985–1986 PTCA and 1997–2006 Dynamic Registries. Circ Cardiovasc Interv. 2009 Feb;2(1):6–13. doi: 10.1161/CIRCINTERVENTIONS.108.825323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryan J, Linde-Zwirble W, Engelhart L, Cooper L, Cohen DJ. Temporal changes in coronary revascularization procedures, outcomes, and costs in the bare-metal stent and drug-eluting stent eras: results from the US Medicare program. Circulation. 2009 Feb 24;119(7):952–961. doi: 10.1161/CIRCULATIONAHA.108.781138. [DOI] [PubMed] [Google Scholar]
- 9.Birkmeyer NJ, Marrin CA, Morton JR, et al. Decreasing mortality for aortic and mitral valve surgery in Northern New England. Northern New England Cardiovascular Disease Study Group. Annals of Thoracic Surgery. 2000 Aug;70(2):432–437. doi: 10.1016/s0003-4975(00)01456-9. [DOI] [PubMed] [Google Scholar]
- 10.Birrell F, Johnell O, Silman A. Projecting the need for hip replacement over the next three decades: influence of changing demography and threshold for surgery. Annals of the Rheumatic Diseases. 1999 Sep;58(9):569–572. doi: 10.1136/ard.58.9.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huo MH, Parvizi J, Bal BS, Mont MA. What's new in total hip arthroplasty. Journal of Bone and Joint Surgery. 2008 Sep;90(9):2043–2055. doi: 10.2106/JBJS.H.00741. [DOI] [PubMed] [Google Scholar]
- 12.Schrama JC, Espehaug B, Hallan G, et al. Risk of revision for infection in primary total hip and knee arthroplasty in patients with rheumatoid arthritis compared with osteoarthritis: a prospective, population-based study on 108,786 hip and knee joint arthroplasties from the Norwegian Arthroplasty Register. Arthritis Care Res (Hoboken) 2010 Apr;62(4):473–479. doi: 10.1002/acr.20036. [DOI] [PubMed] [Google Scholar]
- 13.Himanen AK, Belt E, Nevalainen J, Hamalainen M, Lehto MU. Survival of the AGC total knee arthroplasty is similar for arthrosis and rheumatoid arthritis. Finnish Arthroplasty Register report on 8,467 operations carried out between 1985 and 1999. Acta Orthop. 2005 Feb;76(1):85–88. doi: 10.1080/00016470510030373. [DOI] [PubMed] [Google Scholar]
- 14.Lie SA, Engesaeter LB, Havelin LI, Gjessing HK, Vollset SE. Mortality after total hip replacement: 0–10-year follow-up of 39,543 patients in the Norwegian Arthroplasty Register. Acta Orthopaedica Scandinavica. 2000 Feb;71(1):19–27. doi: 10.1080/00016470052943838. [DOI] [PubMed] [Google Scholar]
- 15.Ricciardi R, Virnig BA, Ogilvie JW, Jr, Dahlberg PS, Selker HP, Baxter NN. Volume-outcome relationship for coronary artery bypass grafting in an era of decreasing volume. Archives of Surgery. 2008 Apr;143(4):338–344. doi: 10.1001/archsurg.143.4.338. discussion 344. [DOI] [PubMed] [Google Scholar]
- 16.Ho V, Town RJ, Heslin MJ. Regionalization versus competition in complex cancer surgery. Health Econ Policy Law. 2007 Jan;2(Pt 1):51–71. doi: 10.1017/S1744133106006256. [DOI] [PubMed] [Google Scholar]
- 17.Birkmeyer JD, Siewers AE, Marth NJ, Goodman DC. Regionalization of high-risk surgery and implications for patient travel times. JAMA. 2003 Nov 26;290(20):2703–2708. doi: 10.1001/jama.290.20.2703. [DOI] [PubMed] [Google Scholar]
- 18.Zwanziger J, Melnick GA. The effects of hospital competition and the Medicare PPS program on hospital cost behavior in California. Journal of Health Economics. 1988;7(4):301–320. doi: 10.1016/0167-6296(88)90018-5. 1988/12// [DOI] [PubMed] [Google Scholar]
- 19.Sloan FA, Morrisey MA, Valvona J. Effects of the Medicare prospective payment system on hospital cost containment: an early appraisal. Milbank Quarterly. 1988;66(2):191–220. [PubMed] [Google Scholar]
- 20.Buntin MB, Colla CH, Escarce JJ. Effects of payment changes on trends in post-acute care. Health Services Research. 2009 Aug;44(4):1188–1210. doi: 10.1111/j.1475-6773.2009.00968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu K, Baseggio C, Wissoker D, Maxwell S, Haley J, Long S. Long-term care hospitals under Medicare: facility-level characteristics. Health Care Financing Review. 2001;23(2):1–18. [PMC free article] [PubMed] [Google Scholar]
- 22.Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010 Jun 2;303(21):2141–2147. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ross JS, Chen J, Lin Z, et al. Recent national trends in readmission rates after heart failure hospitalization. Circ Heart Fail. 2010 Jan;3(1):97–103. doi: 10.1161/CIRCHEARTFAILURE.109.885210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mitchell JB, Bubolz T, Paul JE, et al. Using Medicare claims for outcomes research. Medical Care. 1994 Jul;32(7 Suppl):JS38–51. [PubMed] [Google Scholar]
- 25.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. Journal of Bone & Joint Surgery - American Volume. Sep 2004;86-A(9):1909–1916. doi: 10.2106/00004623-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Losina E, Barrett J, Mahomed NN, Baron JA, Katz JN. Early failures of total hip replacement: effect of surgeon volume. Arthritis & Rheumatism. 2004 Apr;50(4):1338–1343. doi: 10.1002/art.20148. [DOI] [PubMed] [Google Scholar]
- 27.Katz JN, Losina E, Barrett J, et al. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. Journal of Bone & Joint Surgery - American Volume. 2001 Nov;83-A(11):1622–1629. doi: 10.2106/00004623-200111000-00002. [see comment] [DOI] [PubMed] [Google Scholar]
- 28.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical Care. 1998 Jan;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005 Nov;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 30.Hagen TP, Vaughan-Sarrazin MS, Cram P. Relation between hospital orthopaedic specialisation and outcomes in patients aged 65 and older: retrospective analysis of US Medicare data. BMJ. 2010;340:c165. doi: 10.1136/bmj.c165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cram P, Rosenthal GE, Vaughan-Sarrazin MS, Wolf B, Katz JN. A comparison of total hip and knee replacement in specialty and general hospitals. J Bone Joint Surg Am. 2007 Aug;89(8):1675–1684. doi: 10.2106/JBJS.F.00873. [DOI] [PubMed] [Google Scholar]
- 32.Shahian DM, Torchiana DF, Shemin RJ, Rawn JD, Normand SL. Massachusetts cardiac surgery report card: implications of statistical methodology. Ann Thorac Surg. 2005 Dec;80(6):2106–2113. doi: 10.1016/j.athoracsur.2005.06.078. [DOI] [PubMed] [Google Scholar]
- 33.Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003 Oct 2;349(14):1350–1359. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- 34.Escalante A, Barrett J, del Rincon I, Cornell JE, Phillips CB, Katz JN. Disparity in total hip replacement affecting Hispanic Medicare beneficiaries. Med Care. 2002 Jun;40(6):451–460. doi: 10.1097/00005650-200206000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Hausmann LR, Mor M, Hanusa BH, et al. The effect of patient race on total joint replacement recommendations and utilization in the orthopedic setting. J Gen Intern Med. 2010 Sep;25(9):982–988. doi: 10.1007/s11606-010-1399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krumholz HM, Wang Y, Chen J, et al. Reduction in acute myocardial infarction mortality in the United States: risk-standardized mortality rates from 1995–2006. JAMA. 2009 Aug 19;302(7):767–773. doi: 10.1001/jama.2009.1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jain NB, Higgins LD, Ozumba D, et al. Trends in epidemiology of knee arthroplasty in the United States, 1990–2000. Arthritis and Rheumatism. 2005 Dec;52(12):3928–3933. doi: 10.1002/art.21420. [DOI] [PubMed] [Google Scholar]
- 38.Robertsson O, Dunbar MJ, Knutson K, Lidgren L. Past incidence and future demand for knee arthroplasty in Sweden: a report from the Swedish Knee Arthroplasty Register regarding the effect of past and future population changes on the number of arthroplasties performed. Acta Orthopaedica Scandinavica. 2000 Aug;71(4):376–380. doi: 10.1080/000164700317393376. [DOI] [PubMed] [Google Scholar]
- 39.Mehrotra C, Remington PL, Naimi TS, Washington W, Miller R. Trends in total knee replacement surgeries and implications for public health, 1990–2000. Public Health Reports. 2005 May–Jun;120(3):278–282. doi: 10.1177/003335490512000310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Silverman E, Skinner J. Medicare upcoding and hospital ownership. J Health Econ. Mar 2004;23(2):369–389. doi: 10.1016/j.jhealeco.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 41.Davis C, Rhodes DJ. The impact of DRGs on the cost and quality of health care in the United States. Health Policy. 1988;9(2):117–131. doi: 10.1016/0168-8510(88)90029-2. [DOI] [PubMed] [Google Scholar]
- 42.Chulis GS. Assessing Medicare's prospective payment system for hospitals. Medical Care Review. 1991 Summer;48(2):167–206. doi: 10.1177/002570879104800203. [DOI] [PubMed] [Google Scholar]
- 43.Baker DW, Einstadter D, Husak SS, Cebul RD. Trends in postdischarge mortality and readmissions: has length of stay declined too far? Archives of Internal Medicine. 2004 Mar 8;164(5):538–544. doi: 10.1001/archinte.164.5.538. [DOI] [PubMed] [Google Scholar]