Abstract
The efficacy of extracts and essential oils from Allium tuberosum, Coriandrum sativum, Cymbopogon martini, Cymbopogon winterianus, and Santolina chamaecyparissus was evaluated against Candida spp. isolates from the oral cavity of patients with periodontal disease. The most active oil was fractionated and tested against C. albicans biofilm formation. The oils were obtained by water-distillation and the extracts were prepared with macerated dried plant material. The Minimal Inhibitory Concentration—MIC was determined by the microdilution method. Chemical characterization of oil constituents was performed using Gas Chromatography and Mass Spectrometry (GC-MS). C. sativum activity oil upon cell and biofilm morphology was evaluated by Scanning Electron Microscopy (SEM). The best activities against planktonic Candida spp. were observed for the essential oil and the grouped F8–10 fractions from C. sativum. The crude oil also affected the biofilm formation in C. albicans causing a decrease in the biofilm growth. Chemical analysis of the F8–10 fractions detected as major active compounds, 2-hexen-1-ol, 3-hexen-1-ol and cyclodecane. Standards of these compounds tested grouped provided a stronger activity than the oil suggesting a synergistic action from the major oil constituents. The activity of C. sativum oil demonstrates its potential for a new natural antifungal formulation.
1. Introduction
During the last two decades, the yeasts of the genus Candida have received notable attention in medical literature. Colombo and Guimarães [1] emphasized the increase of nosocomial infections caused by Candida spp. In the beginning of the 80s, Candida spp. were the seventh most frequent pathogen associated with hospital-acquired infections in the United States of America. At the end of the 80s, this agent represented the fifth most frequent pathogen and presently, according to the author, accounts for 8% of the cases of hospital-acquired infections and is considered the fourth main isolated pathogen present in diagnostic tests.
The frequency of commensal Candida species isolated in the oral cavity of clinically healthy individuals varies from 40 to 60% [2]. Several factors predispose to the development of candidiasis, such as endocrine disorders, pregnancy, iron deficiency, immune disorders, and xerostomy [3]. The occurrence of oral candidosis can be related to the host and to the yeast itself. The most cited causes related to the host are diabetes mellitus (DM), loss of teeth, changes in dietary habits, oral hygiene, systemic diseases, hormonal changes, immunosuppression, radiation, and chemotherapy [4]. Among the factors related to the yeast (also called virulence factors), adhesion phenomenon, mycelium formation, phenotypic variability, production of extracellular enzymes (protease and phospholipase), and toxins [4–6] can be observed. Furthermore, the hability of the Candida species to grow as a biofilm can increase the resistance to drugs, blocking or preventing the access of antifungals to the more internal biofilm structure [7].
Candidosis is considered the most common fungal infection of the human oral cavity, and C. albicans is the main species related although nonalbicans species such as C. tropicalis, C. parapsilosis, C. krusei, C. glabrata, and C. dubliniensis, are becoming common among certain groups of patients [3, 8–10]. The occurrence of severe periodontitis has also been associated with the isolation of species of Candida spp. from periodontal lesions [11–14]. The yeast, through the access to tissues, produces metabolites that lead to inflammation.
The widespread use of azole antifungals for the treatment of oral candidosis, especially after the AIDS era, seems to have been the predominant factor for the increase in frequency of non-Candida albicans species, especially those naturally more resistant to this class of antifungal agents, such as C. glabrata and C. krusei [15]. Data from some studies suggest that prolonged or intermittent treatment with antifungal agents modifies C. albicans prevalence, increasing the frequency of other Candida species [16, 17].
The resistance of human pathogens to multiple drugs is well known today and indicates the need to search for antimicrobial substances from new sources, including plants used in folk medicine, which present a great variety of compounds with therapeutic properties. The use of plants as a source of drugs is prevalent in developing countries as an alternative to health problems and is well established in some cultures and traditions, especially in Asia, Latin America, and Africa [18]. Many native plants in these regions have not yet been studied and can be researched for antimicrobial action, in contrast to European native plants that have already been exhaustively studied [19]. According to Duarte & Figueira [19], the information available on medicinal plants active against C. albicans has not, until recently, resulted in effective formulations for human or animal use, except for some patents concerning material derived from the plant families Allium [20], Radix gentianae [21], and five extracts studied by Lee et al. [22].
In Brazil, despite the existing rich flora and biodiversity, data from only approximately 44 species and 22 families with positive activities are available, including native and exotic plants [19]. The aim of this study was to evaluate the antimicrobial activity of extracts, essential oils, and fractions from medicinal plants belonging to the CPMA-Medicinal and Aromatic Plant Collection at CPQBA/UNICAMP, against planktonic cells of Candida spp. from CBS collection and isolates from patients with periodontal disease. The most active oil, from Coriandrum sativum L, was tested against C. albicans biofilm formation.
2. Materials and Methods
2.1. Samples
For the development of this research, Candida spp. reference strains obtained from Netherlands Collection—CBS (C. albicans CBS 562, C. dubliniensis CBS 7987, C. krusei CBS 573, C. tropicalis CBS 94, and C. parapsilosis CBS 604) and clinical isolates from volunteers of the Dentistry Faculty of Piracicaba-FOP/UNICAMP, São Paulo-Brazil as C. albicans (3A5, 13A5, 41M2, and 50M2), C. dubliniensis 26A2, 26A3, and 26A4), C. krusei (56M3, 56M4, and 56M5), C. tropicalis (53M6, 52M7, and 53M8), and C. parapsilosis (45M2, 45M4, and 45M5) were used. The isolates were collected from oral mucosa and were identified on chromogenic medium CHROMagar-Candida and by morphological and biochemical tests. The codes of the clinical isolates correspond to the number of the volunteers and the place of origin (A from periodontal pocket and M from mucosa). Subsequently, the yeasts were stored at −70°C in YPD medium with 15% glycerol and maintained at the mycology collection of the Department of Microbiology and Immunology from FOP/UNICAMP. This research was performed under the authorization of the Research Ethics Committee (008/2003).
2.2. Medicinal Plants
The plants studied as Allium tuberosum Rottl. ex Spreng, Coriandrum sativum L, Cymbopogon martinii (Roxb.) J. F. Watson, C. winterianus Jowitt, and Santolina chamaecyparissus were grown in the experimental field of the Research Center for Chemistry, Biology and Agriculture (CPQBA), University of Campinas, São Paulo, Brazil. The plants were collected from November 2001 to November 2002, during the morning after dewpoint. Voucher specimens were deposited at the University of Campinas Herbarium (UEC) and identified by Dr. Washington Marcondes Ferreira Neto (curator), or at the herbarium at the CPQBA.
2.3. Essential Oil Extraction
The essential oils were obtained from 100 g of aerial fresh plant parts by water distillation using a Clevenger-type system for 3 h. The aqueous phase was extracted three times with 50 mL of dichloromethane. The pooled organic phases were dried with sodium sulphate and filtered, and the solvent was evaporated until dryness. Oil samples were stored at −25°C in sealed glass vials [23].
2.4. Extracts Preparation
Dried plant material (10 g) was macerated with 150 mL of hexane or dichloromethane, as indicated, and submitted to shaking at 200 rpm at room temperature for 3 h. Subsequently, the extracts were filtered, and the plant residues were re-extracted with fresh 70% ethanol. The pooled filtrates were concentrated under vacuum and stored at 4°C until further use [23].
2.5. Essential Oil Fractionation
The essential oil that presented best activity was fractioned in a dry column prepared with silica gel 60 Merck (0,063–0,200 mm). A cellulose bag (3 cm diameter) was used for support. The essential oil was put directly into the packed column and eluted. The mobile phase utilized in each column was defined after essential oil analysis using TLC (thin layer chromatography), in different eluents. After elution, the column was fractioned into three parts, and the fractions were transferred individually to the appropriate vials, solubilized in ethyl acetate, and analyzed by TLC. Similar fractions were grouped and filtered using vacuum and the silica residues extracted with ethyl acetate [23].
2.6. Activity Assay-Minimal Inhibitory Concentration (MIC) Test
Yeasts were grown overnight at 36°C in Sabouraud Dextrose Agar (Merck) plates. Inocula for the assays were prepared by diluting scraped cell mass into 0.85% NaCl solution, adjusted to McFarland scale 0.5, and confirmed by spectrophotometric reading at 580 nm. Cell suspensions were finally diluted to 104 UFC mL−1 in RPMI-1640 medium (Difco) for assays. MIC tests were carried out according to CLSI [24], using tissue culture test plate (96 wells), containing 100 μL RPMI-1640 medium. The stock solutions of the essential oil or crude extracts obtained from medicinal plants were diluted and transferred into the first well, and serial dilutions were performed to obtain concentrations ranging from 1 to 0.03 mg mL−1. Nystatin and Fluconazol (Merck) were used as antimycotic control reference ranging from 1 to 0.03 mg mL−1. The yeast inoculum was added to all wells, and plates were incubated at 36°C for 48 h. MIC was defined as the lowest concentration of oil or extract that inhibited visible growth, as indicated by the RPMI-1640 medium color change (pink to yellow).
2.7. C. albicans Biofilm Induction
Standardized C. albicans cells (1.0 × 106 cells/mL in RPMI 1640 medium) were introduced into wells of 96 well tissue culture plates (TPP) containing RPMI-1640 medium with 2% sucrose and were incubated for 1.5 h at 37°C. After the 1.5 h initial adhesion, the medium was aspirated, and nonadhered cells were removed and washed with sterile distilled water. RPMI 1640 medium was added to the adhered cells in the wells. The plates were incubated for 24 h at 37°C [25].
2.8. Activity of the Essential Oil and Fractions from C. sativum on the Biofilm Formation in C. albicans
To evaluate the antimicrobial activity of C. sativum essential oil on C. albicans biofilm formation, the samples were applied at regular intervals during 24 h at two different concentrations, corresponding to the MIC previously found for the planktonic cells, and 1 mg/mL. The applications were carried out before planktonic cells adhesion (T 0), after preadhesion (T 3 h) and after 6 h, 12 h, 18 h, 24 h, and 48 h. The plates were read at the following interval after application. The controls fluconazole (fungistatic)—0064 mg/mL and nystatin (fungicidal)—1 mg/mL were also included in the tests. The tests were performed in three independent experiments, each in triplicate [25].
2.9. Biofilm Quantification
The biofilm developed in each well was washed twice with 200 μL of distilled water and then dried for 45 min. In each well, 110 μL of 0.4% crystal violet were added for 45 min. After this procedure, the wells were washed four times with distilled water and immediately discolored with 350 μL of 95% ethanol. Elapsed 45 minutes after the last procedure, 100 μL of discolored solution was transferred to a well of a new plate and the crystal violet measured at 595 nm in an ELISA reader (SpectraMax 340 tunable MICROPLATES Reader, Molecular Devices Ltda). The amount of biofilm formed was measured, subtracting the absorbance from the absorbance values of the control wells [26].
2.10. Scanning Electron Microscopy (SEM)
In order to evaluate C. albicans integrity cells using SEM, the biofilms were first developed in Lab-Tek chambered coverglass (Nunc), as described above, and treated with C. sativum essential oil and standard drugs. The samples were fixed in glutaraldehyde 0.15 M 2.5% (v/v) PBS for one hour at room temperature. After this procedure, the chambered coverglasses were treated with 1% osmium trioxide for one hour and washed three times with 3 mL of distilled water. The chambered coverglasses were then hydrated with an ethanol series (50% to 100%), dried to a critical point and coated with gold in the metalizer, and then observed using a scanning electron microscope [27].
2.11. Gas Chromatography and Mass Spectrometry Analyses (GC-MS)
The identification of volatile constituents was performed using a Hewlett-Packard 6890 gas chromatograph, equipped with an HP-5975 mass selective detector and HP-5 capillary column (25 m × 0.25 mm × 0.25 μm diameter). GC and GC-MS were performed using split/splitless injection, with the injector set at 220°C, column set at 60°C, with a heating ramp of 3°C min−1 and a final temperature of 240°C, and the MS and FID detector set at 250°C. Helium was used as a carrier gas at 1 mL min−1. The GC-MS electron ionization system was set at 70 eV. A sample of the essential oil was solubilized in ethyl acetate for the analyses. Retention indices (RIs) were determined by coinjection of hydrocarbon standards. The oil components were identified by comparison with data from the literature, the profiles, the Nist 05 library, and by co-injection of authentic standards, when available [28].
2.12. Statistical Analysis
All statistical tests were performed with one-way ANOVA, and P value of <.05 was considered statically significant. The statistical test was run using STATISTICA v.5.0 (Stasoft, USA) system software, and graphics were carried out using SIGMAPLOT v.10.0. System software (SPSS Inc.). Different treatments were compared at all times during the biofilm assay.
3. Results
3.1. Oil and Extracts Yields
Oil and extracts yields were expressed in relation to dry weight of the plant material (% w/w). Larger quantities of essential oil were obtained from C. martinii (1.36%) and C. winterianus (1.88%) followed by S. chamaecyparissus (0.15%), C. sativum (0.08%), and A. tuberosum (0.11%). Compared to essential oils, extract yields were higher and ranged from 1,33% (C. sativum) to 18.5% (A. tuberosum). The intermediate yields were 7.33% (C. martini), 10.14% (S. chamaecyparissus), and 14.68% (C. winterianus).
According to the activity results, the C. sativum essential oil was fractioned in a dry column and the fractions grouped according to the equivalence of the bands presented in thin layer chromatography (TLC) analysis. The grouped F 8–10 fractions presented the highest yield (155.20 mg/g) followed by F7 fraction (120.40 mg/g), F5 fraction (25.90 mg/g), F6 (22.60 mg/g), and F3-4 grouped fraction (8.74 m/g).
3.2. Essential Oil and Extract Activity against Planktonic Candida spp
Minimum inhibitory concentration (MIC) of the essential oils (EOs), dichloromethanic extracts (DEs), and hexanic extract (HE) were tested against Candida spp. planktonic cells, as indicated in Table 1. In general, the oils and extracts presented a good action against planktonic Candida spp. and clinical isolates; however, the oil and the hexanic extract from C. sativum were capable of inhibiting all strains at MIC values between 0.015–0.500 mg/mL and 0.007–1.000 mg/mL.
Table 1.
Anti-Candida activity (MIC-mg/mL) of the essential oils, the dichloromethane (DE) and hexane (HE) extracts from the medicinal species studied.
| Candida spp. | A. tuberosum | C. sativum | C. martinii | C. winterianus | S. chamaecyparissus | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| EO | DE | EO | HE | EO | DE | EO | DE | EO | DE | |
| Culture collection | ||||||||||
| C. albicans CBS 562 | 0.500 | 0.500 | 0.015 | 0.125 | 0.063 | 0.250 | 1.000 | 0.125 | 1.000 | 0.250 |
| C. krusei CBS 573 | >1.0 | >1.0 | 0.015 | 0.125 | 0.063 | 0.125 | 0.063 | 0.063 | 0.500 | 0.500 |
| C. parapsilosis CBS 604 | 0.015 | 0.015 | 0.125 | 0.031 | 0.125 | 0.063 | 1.000 | 0.125 | 1.000 | 1.000 |
| C. dubliniensis CBS 7987 | 1.000 | >1.0 | 0.007 | 0.031 | 0.125 | 0.250 | 0.500 | 0.125 | 0.063 | 0.063 |
| C. tropicalis CBS 94 | >1.0 | >1.0 | 0.125 | 0.500 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
|
| ||||||||||
| Clinical isolatesa | ||||||||||
| C. albicans 3 A5 | 0.500 | >1.0 | 0.015 | 1.000 | 0.250 | 1.000 | 1.000 | 1.000 | 1.000 | >1.0 |
| C. albicans 13 A5 | 0.500 | >1.0 | 0.031 | 1.000 | 0.063 | 1.000 | 0.500 | 1.000 | 1.000 | >1.0 |
| C. albicans 41 M2 | 0.500 | >1.0 | 0.031 | 1.000 | 0.063 | 1.000 | 1.000 | 1.000 | 1.000 | >1.0 |
| C. albicans 50 M2 | 0.500 | >1.0 | 0.063 | 1.000 | 0.250 | 1.000 | 0.500 | 1.000 | 1.000 | >1.0 |
| C. krusei 56 M3 | 0.007 | >1.0 | 0.007 | 0.031 | 0.007 | 0.063 | 0.031 | 0.002 | 0.125 | 0.063 |
| C. krusei 56 M4 | 1.000 | >1.0 | 0.007 | 0.015 | 0.007 | 0.007 | 0.007 | 0.007 | 0.007 | 0.500 |
| C. krusei 56 M6 | 1.000 | >1.0 | 0.007 | 0.002 | 0.007 | 0.007 | 0.007 | 0.007 | 0.007 | 0.015 |
| C. parapsilosis 45 M2 | 0.015 | >1.0 | 0.007 | 0.063 | 0.031 | 0.063 | 0.250 | 0.250 | 0.500 | 0.125 |
| C. parapsilosis 45 M4 | 0.015 | >1.0 | 0.007 | 0.125 | 0.015 | 0.031 | 0.063 | 0.063 | 0.250 | 0.125 |
| C. parapsilosis 45 M5 | 0.015 | >1.0 | 0.015 | 0.007 | 0.250 | 1.000 | 1.000 | 0.063 | 1.000 | 1.000 |
| C. dubliniensis 26 A2 | 1.000 | >1.0 | 0.063 | 0.250 | 0.250 | 0.500 | 1.000 | 0.500 | 0.500 | 0.500 |
| C. dubliniensis 26 A3 | 1.000 | >1.0 | 0.031 | 0.250 | 0.250 | 0.500 | 1.000 | 0.250 | 0.250 | 0.500 |
| C. dubliniensis 26 A4 | >1.0 | >1.0 | 0.500 | 0.250 | 1.000 | 0.250 | 1.000 | 0.250 | 0.500 | 1.000 |
| C. tropicalis 53 M6 | >1.0 | >1.0 | 0.125 | 0.500 | >1.0 | >1.0 | >1.0 | >1.0 | 1.000 | 1.000 |
| C. tropicalis 53 M7 | >1.0 | >1.0 | 0.063 | 0.250 | 0.250 | 0.250 | 1.000 | 1.000 | >1.0 | >1.0 |
| C. tropicalis 53 M8 | >1.0 | >1.0 | 0.031 | 0.250 | >1.0 | >1.0 | >1.0 | >1.0 | >1.0 | >1.0 |
aThe codes correspond to the number of the volunteers and the place of sample origin; (A)-periodontal pocket; (M) oral mucosa.
The activity of the fractions of C. sativum essential oil was also tested against the planktonic cells of Candida spp., presenting in general strong activity, except for fraction 5 (Table 2). The lowest activity was observed for grouped F 8–10 MIC value, the most polar fraction found by TLC analysis. In order to compare the results of inhibition obtained from the medicinal plants, two commercially available antifungal agents were chosen: nystatin (polienic fungicide) and fluconazole (azole fungistatic).
Table 2.
Anti-Candida activity (MIC-mg/mL) of crude essential oil (EO) and C. sativum fractions (F).
| Candida spp. | EO | F 3–F 4 | F 5 | F 6 | F 7 | F 8–F 10 |
|---|---|---|---|---|---|---|
| Culture collection | ||||||
|
| ||||||
| C. albicans CBS 562 | 0.015 | 0.063 | >1.0 | 0.500 | 0.125 | 0.015 |
| C. krusei CBS 57 | 0.015 | 0.500 | 0.500 | 0.250 | 0.125 | 0.063 |
| C. parapsilosis CBS 604 | 0.125 | 0.500 | >1.0 | 0.250 | 0.250 | 0.063 |
| C. dubliniensis CBS 7987 | 0.007 | 0.125 | >1.0 | 0.063 | 0.063 | 0.031 |
| C. tropicalis CBS 94 | 0.125 | 0.500 | >1.0 | 1.000 | 0.063 | 0.063 |
|
| ||||||
| Clinical isolatesa | ||||||
| C. albicans 13 A5 | 0.031 | 0.125 | >1.0 | 0.500 | 0.250 | 0.063 |
| C. krusei 56 M3 | 0.007 | 0.250 | 0.250 | 0.250 | 0.125 | 0.063 |
| C. parapsilosis 45 M4 | 0.007 | 0.500 | >1.0 | 0.250 | 0.250 | 0.063 |
| C. dubliniensis 26 A3 | 0.031 | 0.250 | >1.0 | 0.250 | 0.125 | 0.063 |
| C. tropicalis 53 M7 | 0.063 | >1.0 | >1.0 | 1.000 | 0.250 | 0.125 |
aThe codes correspond to the number of the volunteers and the place of sample origin; (A)-periodontal pocket; (M) oral mucosa.
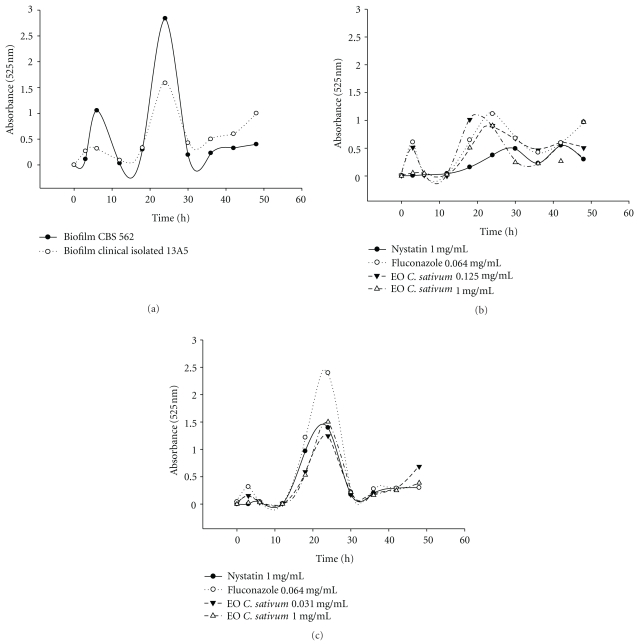
3.3. C. sativum Essential Oil Activity against C. albicans Biofilm
Figure 1(a) shows the kinetic biofilm development for C. albicans CBS 562 and clinical isolate 13A5. The action of nystatin, fluconazole, and C. sativum essential oil upon biofilm growth was presented in Figures 1(b) and 1(c). The crude essential oil from C. sativum and drugs was applied at regular intervals during biofilm cultivation. The results shown in Figures 1(b) and 1(c) indicate a clear effect of the oil on biofilm formation, characterized due to an increase in the lag phase and a decrease in the biofilm growth. Similar effects were observed for nistatin, though inferior to fluconazole (P ≤ .05).
Figure 1.
Biofilm kinetic development: (a) Control, without treatment; (b) action of nystatin, fluconazole and C. sativum essential oil in the biofilm kinetic development for C. albicans CBS 562; (c) action of nystatin, fluconazole and C. sativum essential oil in the biofilm kinetic development for C. albicans clinical isolate 13A5.
The statistical analysis demonstrated a significative difference (P ≤ .05) after 48 h of treatment (Figures 1(b), 1(c)). Considering the results obtained for C. albicans CBS 562, the best treatments were nystatin (1 mg/mL) and essential oil (0.125 mg/mL). For the clinical isolate 13A5, the effect on the biofilm was statistically identical as that for nystatin (1 mg/mL), fluconazole (0.0641 mg/mL), and essential oil (1 mg/mL), though inferior for the essential oil at 0.125 mg/mL.
3.4. Chemical Characterization of Oil Constituents
The chemical composition of the essential oil and grouped F 8–10 fractions from C. sativum is shown in Table 3. The evaluation was performed by gas chromatography coupled to mass spectrometry (GC-MS). The oil analysis indicated the presence of volatile derivatives of alcohols and aldehydes, such as decene, decanal, decenol, decenal, decanol, dodecanal, dodecanol, tetradecenal, tetradecanol, tridecanol, hexenol, and cyclodecane. Fraction F 8–10 was enriched with 3-hexen-1-ol (16.08%), 2-hexen-1-ol (14.52%), and 1-decanol (44.16%). Further experiments were carried out aiming to evaluate the action of the isolated components (Sigma-Aldrich standards) against C. albicans planktonic cells (Table 4).
Table 3.
Identified compounds, retention time (Rt), retention Index (RI), and relative percentage (%) in crude oil and C. sativum essential oil fractions F 8–10.
| Rt (min) | RI | Compounds | % Relative | |
|---|---|---|---|---|
| Crude oil | F 8–10 | |||
| 3.54 | — | 3-hexen-1-ol <E> | — | 0.44 |
| 3.63 | — | 3-hexen-1-ol <Z> | 1.24 | 16.08 |
| 3.78 | — | 2-hexen-1-ol <Z> | 0.77 | 14.52 |
| 5.19 | 933 | α-pinene | 0.15 | — |
| 10.23 | 1101 | Undecane | 0.33 | — |
| 10.40 | 1106 | Nonanal | 0.28 | — |
| 13.02 | 1172 | Nonanol | 0.19 | — |
| 14.49 | 1209 | Decanal | 10.97 | — |
| 16.73 | 1262 | 2-decenal <E> | 2.74 | — |
| 17.12 | 1272 | 2-decen-1-ol <E> | 4.11 | — |
| 17.32 | 1277 | 1-decanol | 15.30 | 44.16 |
| 18.65 | 1309 | Undecanal | 2.20 | — |
| 20.96 | 1364 | 2-undecenal <E> | 1.01 | — |
| 21.25 | 1371 | 2-undecenol <E> | 1.21 | 1.71 |
| 21.38 | 1375 | Undecanol | 1.96 | 3.62 |
| 22.89 | 1411 | dodecanal | 7.53 | — |
| 25.19 | 1469 | 2-dodecenal | 8.16 | — |
| 25.45 | 1475 | 2-dodecenol | 11.26 | 13.04 |
| 25.52 | 1477 | Cyclododecane | 2.54 | 4.43 |
| 26.89 | 1512 | Tridecanal | 1.00 | — |
| 29.11 | 1570 | 2-tridecenal <E> | 1.44 | — |
| 29.28 | 1574 | 2-tridecenol <E> | 0.86 | — |
| 29.56 | 1581 | Caryophyllene oxide | 0.47 | — |
| 30.78 | 1614 | Tetradecanal | 1.26 | — |
| 33.01 | 1674 | 2-tetradecenol <E> | 13.58 | — |
| 36.58 | 1775 | 2-pentadecenol | 3.10 | — |
| 40.03 | 1879 | 2-hexadecenol | 0.80 | — |
| 47.73 | — | Phytol | 3.06 | — |
| — | — | nonidentified compounds | 2.52 | 2.01 |
Table 4.
Anti-Candida activity (MIC-mg/mL) of the C. sativum essential oil (OE), fractions F 8–10 and from the major compounds present in F 8–10.
| Candida spp. | EO | Fractions F 8–10 | 2 -hexen-ol cis | 2-hexen-ol trans | 3-hexen-ol cis | 3-hexen-ol trans | 1-decanol | Majority compounds mixture |
|---|---|---|---|---|---|---|---|---|
| C. albicans CBS 562 | 0.015 | 0.015 | 0.063 | 0.031 | 0.500 | 0.063 | 0.031 | 0.0005 |
| C. albicans 13 A | 0.031 | 0.063 | 0.063 | 0.007 | 0.125 | 0.031 | 0.015 | 0.0005 |
3.5. Scanning Electron Microscopy
The action of C. sativum crude oil and grouped F 8–10 fractions upon C. albicans cells and biofilm morphology, evaluated by scanning electron microscopy (SEM), is presented in Figures 2(a)–2(c) and demonstrates that the plant materials caused an amendment in cell structure.
Figure 2.
Scanning electron microscopy (SEM) of the C. albicans biofilm: (a) without treatment; (b) treated with C. sativum crude essential oil; (c) treated with grouped fractions F 8–10.
4. Discussion
The activity of natural products upon microorganisms has been recently confirmed by literature. Plant materials such as extracts, essential oils, and isolated compounds have demonstrated inhibition against bacteria [29], yeast [30], and filamentous fungi [31]. Most studies, however, focus on planktonic cells; nevertheless, the fact that several microorganisms are capable of growing as a biofilm, leading to a greater resistance to drugs, indicates the need for further activity studies with these natural products regarding biofilm mechanism formation. In the present study, essential oils and extracts from 5 different medicinal species, with previously known antimicrobial activity [30, 32, 33], were evaluated against Candida spp. planktonic cells and C. albicans biofilm.
As there is no consensus regarding the acceptable inhibition level for natural products when compared with standard antibiotics, we have considered the definition proposed by Duarte et al. [30], being strong activity-MIC up to 0.5 mg/mL; moderate activity-MIC between 0.51 and 1.0 mg/mL, and weak activity-MIC above 1.1 mg/mL. Thus, the results obtained in the present work show a broad action of oils and extracts, with a greater activity for essential oils than for extracts, capable of inhibiting the different Candida spp. CBS and clinical isolates with moderate to strong activity. When the plant materials were compared with fluconazole and nystatin activity, the plant materials were similar or better than the aforementioned drugs in some cases.
Considering the susceptibility of CBS standard strains and the clinical isolates, the strains from CBS collection were, in general, more sensitive to essential oils. Among the different species investigated, clinical isolates from C. dubliniensis and C. tropicalis were the most resistant species (moderate to weak activities—MIC ≥ 1.0 mg/mL), except in the case of the essential oil from C. sativum.
The oil from C. sativum, a plant used as a very common condiment in Brazilian Northeast food, was capable of inhibiting all Candida spp. CBS and clinical isolates in the initial assays. The fractionation of the oil emphasized F 8–10 fraction activity; however, the application in planktonic cells did not incur in the best activities, indicating the potential use of this plant in the form of crude oil. F 8–10 fractions presented as main constituents 2-hexen-ol, 3-hexen-ol, and 1-decanol, and when tested alone or grouped showed a synergistic action from the compounds, as the mixture presented the lowest MIC values.
The crude essential oil from C. sativum applied at regular intervals affected biofilm development and caused a delay in the lag phase and a decrease in the biofilm growth (Figures 1(b) and 1(c)) when compared to the control assay (Figure 1(a)). The response of C. albicans CBS 562 and clinical isolate 13A5 to treatments was different, as this last presented a higher growth in the presence of the drugs and essential oil. The statistical analysis demonstrated a significative difference (P ≤ .05) after 48 h of treatment, showing a similar action for nystatin and C. sativum essential oil. The activity of the materials tested in the present study was confirmed through SEM analysis and demonstrated cell deformation, presenting a withered appearance.
5. Conclusion
In conclusion, the results of the present study indicate the potential use of themedicinal species for oral candidosis prevention or treatment and emphasize the action of the crude C. sativum essential oil, which demonstrates a strong activity against Candida spp. planktonic cells and C. albicans biofilm.
Acknowledgments
The authors thank FAPESP (São Paulo Research Foundation) and Capes (Brazilian Funding Agency) for the financial support.
References
- 1.Colombo AL, Guimarães T. Epidemiologia das infecções hematogênicas por Candida spp. Revista da Sociedade Brasileira de Medicina Tropical. 2003;36(5):599–607. doi: 10.1590/s0037-86822003000500010. [DOI] [PubMed] [Google Scholar]
- 2.Arendorf TM, Walker DM. The prevalence and intra-oral distribution of Candida albicans in man. Archives of Oral Biology. 1980;25(1):1–10. doi: 10.1016/0003-9969(80)90147-8. [DOI] [PubMed] [Google Scholar]
- 3.Samaranayake LP, MacFarlane TW. The effect of dietary carbohydrates on the in-vitro adhesion of Candida albicans to epithelial cells. Journal of Medical Microbiology. 1982;15(4):511–517. doi: 10.1099/00222615-15-4-511. [DOI] [PubMed] [Google Scholar]
- 4.Paula CR. Candidíases. In: Zaitz C, Campbell I, Marques AS, editors. Compêndio de Micologia Médica. Vol. 434. São Paulo, Brazil: MEDSI; 1998. [Google Scholar]
- 5.Vidotto V, Koga-Ito CY, Milano R, Fianchino B, Pontón J. Correlation between germ tube production, phospholipase activity and serotype distribution in Candida albicans. Revista Iberoamericana de Micologia. 1999;16(4):208–210. [PubMed] [Google Scholar]
- 6.Menezes EA, Augusto KL, Freire CCF, Cunha FA, Montenegro RM, Montenegro RM. Frequency and enzymatic activity of Candida spp. oral cavity of diabetic patients of the service of endocrinology of a hospital of Fortaleza-CE. Jornal Brasileiro de Patologia e Medicina Laboratorial. 2007;43(4):241–244. [Google Scholar]
- 7.Kuhn DM, George T, Chandra J, Mukherjee PK, Ghannoum MA. Antifungal susceptibility of Candida biofilms: unique efficacy of amphotericin B lipid formulations and echinocandins. Antimicrobial Agents and Chemotherapy. 2002;46(6):1773–1780. doi: 10.1128/AAC.46.6.1773-1780.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pfaller MA. Epidemiology of candidiasis. Journal of Hospital Infection. 1995;30:329–338. doi: 10.1016/0195-6701(95)90036-5. [DOI] [PubMed] [Google Scholar]
- 9.Xu J, Boyd CM, Livingston E, Meyer W, Madden JF, Mitchell TG. Species and genotypic diversities and similarities of pathogenic yeasts colonizing women. Journal of Clinical Microbiology. 1999;37(12):3835–3843. doi: 10.1128/jcm.37.12.3835-3843.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Repentigny L, Lewandowski D, Jolicoeur P. Immunopathogenesis of oropharyngeal candidiasis in human immunodeficiency virus infection. Clinical Microbiology Reviews. 2004;17(4):729–759. doi: 10.1128/CMR.17.4.729-759.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peterson DE, Minah GE, Overholser CD, et al. Microbiology of acute periodontal infection in myelosuppressed cancer patients. Journal of Clinical Oncology. 1987;5(9):1461–1468. doi: 10.1200/JCO.1987.5.9.1461. [DOI] [PubMed] [Google Scholar]
- 12.Slots J, Rams TE, Listgarten MA. Yeasts, enteric rods and pseudomonads in the subgingival flora of severe adult periodontitis. Oral Microbiology and Immunology. 1988;3(2):47–52. doi: 10.1111/j.1399-302x.1988.tb00080.x. [DOI] [PubMed] [Google Scholar]
- 13.Reichart PA. Oral manifestations in HIV infection: fungal and bacterial infections, Kaposi’s sarcoma. Medical Microbiology and Immunology. 2003;192(3):165–169. doi: 10.1007/s00430-002-0175-5. [DOI] [PubMed] [Google Scholar]
- 14.Boniotto M, Hazbón MH, Jordan WJ, et al. Novel hairpin-shaped primer assay to study the association of the -44 single-nucleotide polymorphism of the DEFB1 gene with early-onset periodontal disease. Clinical and Diagnostic Laboratory Immunology. 2004;11(4):766–769. doi: 10.1128/CDLI.11.4.766-769.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dronda F, Alonso-Sanz M, Laguna F, et al. Mixed oropharyngeal Candidiasis due to Candida albicans and non-albicans Candida strains in HIV-infected patients. European Journal of Clinical Microbiology and Infectious Diseases. 1996;15(6):446–452. doi: 10.1007/BF01691310. [DOI] [PubMed] [Google Scholar]
- 16.Persons DA, Laughlin M, Tanner D, Perfect J, Gockerman JP, Hathorn JW. Fluconazole and Candida krusei fungemia. New England Journal of Medicine. 1991;325(18):p. 1315. [PubMed] [Google Scholar]
- 17.Millon L, Manteaux A, Reboux G, et al. Fluconazole-resistant recurrent oral candidiasis in human immunodeficiency virus-positive patients: persistence of Candida albicans strains with the same genotype. Journal of Clinical Microbiology. 1994;32(4):1115–1118. doi: 10.1128/jcm.32.4.1115-1118.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shale TL, Stirk WA, Van Staden J. Screening of medicinal plants used in Lesotho for anti-bacterial and anti-inflammatory activity. Journal of Ethnopharmacology. 1999;67(3):347–354. doi: 10.1016/s0378-8741(99)00035-5. [DOI] [PubMed] [Google Scholar]
- 19.Duarte MCT, Figueira GM. Anti-Candida activity of extracts and essential oils from native and exotic medicinal plants in Brazil. In: Carpinella MC, Rai M, editors. Novel Therapeutic Agents from Plants. Science Publisher; 2009. pp. 123–166. [Google Scholar]
- 20.Plummer N. New antimicrobial compositions which colonise the small intestine—contain non-pathogenic microorganisms and Allium plant material; for treating gastrointestinal and urogenital disease. US Patent no. EP554319-A, 1992.
- 21.Chen Y. Method of treating Candida and Cryptococcus fungal infections by administering gentian. US Patent no. 5837254 A, 1996.
- 22.Lee SE, Hwang HJ, Ha JS, Jeong HS, Kim JH. Screening of medicinal plant extracts for antioxidant activity. Life Sciences. 2003;73(2):167–179. doi: 10.1016/s0024-3205(03)00259-5. [DOI] [PubMed] [Google Scholar]
- 23.Gorelov VE, Aksel’rod LS, Migalinskaya LN. An investigation of the hydraulics and effectiveness of fractionation columns with sieve packing. Chemical and Petroleum Engineering. 1971;7(3):211–214. [Google Scholar]
- 24.Clinical and Laboratorial Standards Institute, norma M27-A2. Método de referência para testes de diluição em caldo para determinação da sensibilidade de leveduras à terapia antifúngica. 2nd edition, 2002.
- 25.Niu C, Gilbert ES. Colorimetric method for identifying plant essential oil components that affect biofilm formation and structure. Applied and Environmental Microbiology. 2004;70(12):6951–6956. doi: 10.1128/AEM.70.12.6951-6956.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Djordjevic D, Wiedmann M, McLandsborough LA. Microtiter plate assay for assessment of Listeria monocytogenes biofilm formation. Applied and Environmental Microbiology. 2002;68(6):2950–2958. doi: 10.1128/AEM.68.6.2950-2958.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hawser SP, Douglas LJ. Biofilm formation by Candida species on the surface of catheter materials in vitro. Infection and Immunity. 1994;62(3):915–921. doi: 10.1128/iai.62.3.915-921.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Adams RP. Identification of Essential Oils Components by Gas Chromatography/Mass Spectrometry. 4th edition. Ill, USA: Allured Publishing Corporation; 2007. [Google Scholar]
- 29.Erturk O. Antibacterial and antifungal activity of ethanolic extracts from eleven spice plants. Biologia. 2006;61(3):275–278. [Google Scholar]
- 30.Duarte MCT, Figueira GM, Sartoratto A, Rehder VLG, Delarmelina C. Anti-Candida activity of Brazilian medicinal plants. Journal of Ethnopharmacology. 2005;97(2):305–311. doi: 10.1016/j.jep.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 31.Fukai T, Yonekawa M, Hou AJ, Nomura T, Sun HD, Uno J. Antifungal agents from the roots of Cudrania cochinchinensis against Candida, Cryptococcus, and Aspergillus species. Journal of Natural Products. 2003;66(8):1118–1120. doi: 10.1021/np030024u. [DOI] [PubMed] [Google Scholar]
- 32.Lo Cantore P, Iacobellis NS, De Marco A, Capasso F, Senatore F. Antibacterial activity of Coriandrum sativum L. and Foeniculum vulgare Miller var. vulgare (Miller) essential oils. Journal of Agricultural and Food Chemistry. 2004;52(26):7862–7866. doi: 10.1021/jf0493122. [DOI] [PubMed] [Google Scholar]
- 33.Proença A. Plantas Aromáticas em Portugal—Caracterização e Utilizações. Lisboa, Portugal: Fundação Calouste Gulbenkian, Serviço de Educação e Bolsas; 2007. [Google Scholar]