Abstract
A 35-year-old female presented with scaly annular and pigmented lesions all over the body of 2 years duration. Her clinical features, histopathology, immunofluorescence findings and positive ANA and anti-Ro antibodies were suggestive of subacute cutaneous lupus erythematosus-lichen planus. We report this case because of its clinical rarity.
Keywords: Subacute cutaneous lupus erythematosus, lichen planus, overlap syndrome
Introduction
Lupus eythematosus-lichen planus (LE-LP) overlap syndrome is an uncommon disorder with about 50 cases being reported in literature.[1] There is an overlap of clinical, histopathological, and immunofluoresecnce findings, which help in distinguishing the disorder. Most of the cases reported were LE-LP overlap and the association of subacute cutaneous lupus erythematosus (SCLE) with LP has been reported only once in literature.[2]
Case Report
A 35-year-old female presented with multiple scaly pigmented plaques on the trunk and limbs of 2 years duration. The lesions initially started as scaly annular plaques on the lower limbs, which became ulcerated, crusted and healed with pigmentation and gradually spread to involve other parts of the body. There were no associated systemic complaints. There was no history of viral infection or drug intake prior to onset of lesions. On examination, multiple hyperpigmented and annular polycyclic plaques were present on the trunk and both limbs. Few erosive and crusted plaques were seen in the forearms and lower legs [Figure 1]. Oral cavity showed palatal erosions with hyperpigmentation [Figure 2]. Genitalia, palms, soles, and nails were normal.
Figure 1.

Erosive and crusted plaques in the forearms
Figure 2.

Oral cavity showing palatal erosions with hyperpigmentation
Her complete blood count, liver and renal function tests were normal. ANA and Anti- Ro antibodies were positive. Lupus anticoagulant, anti cardiolipin antibody, VDRL, and HIV ELISA were negative. Histopathology revealed epidermis with hyperkeratosis, follicular plugging and basal vacuolar damage. Few civatte bodies were seen in the epidermis and superficial dermis [Figure 3]. The superficial dermis was edematous and showed mucin deposits with perivascular lymhocytic infiltrate and melanophages. Direct immunofluorescence showed linear deposits of fibrinogen at the basement membrane zone. With the history and investigations, a diagnosis of SCLE-LP overlap syndrome was made. She was administered oral steroids and hydroxychloroquine and the lesions subsided.
Figure 3.
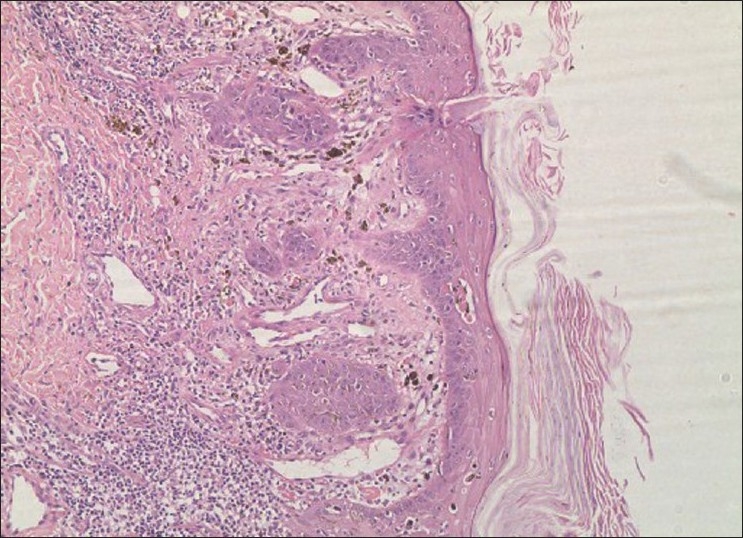
Hyperkeratosis with basal cell degeneration, colloid bodies, and pigmentary incontinence (H and E, 10×)
Discussion
SCLE is a nonscarring nonatrophy-producing photosensitive dermatoses characterized by papulosquamous or annular lesions. SCLE occurs in genetically predisposed individuals, most often in patients with HLA-B8 and HLA-DR3. It is strongly associated with anti-Ro (SS-A) antibodies. The reaction is believed to be related to ultraviolet (UV) light modulation of autoantigens, epidermal cytokines and adhesion molecules, with resultant keratinocyte apoptosis. It can also be induced by drugs such as hydrochlorthiazide and terbinafine and complement (C2) deficiency.
The association of LE with LP has been documented, most of them being systemic lupus erythematosus.[1] A genetic, autoimmune, viral, or drug etiology has been postulated as a cause of LE or LP, and it has also been considered as a spectrum of same disease caused by a viral infection in a genetically predisposed host[3]
The association of SCLE with LP is very rare with only a single case has been reported by Grabbe et al.2They concluded that clinically and historically, SCLE-like lesions appeared to progress into LP-like lesions, supporting the concept of a common autoimmune pathophysiology in these disorders. In our case, the lesions started as scaly annular plaques and ultimately healed with pigmentation similar to the case reported by Grabbe et al. The presence of pigmented plaques, oral pigmentation and positive immunofluorescence findings were suggestive of lichen planus, whereas the presence of scaly annular plaques, palatal erosions, histopathology findings and ANA and Anti-Ro positivity were suggestive of SCLE. Inaloz et al.1reported a case of LE-LP overlap with positive immunofluorescence findings for LP and negative for LE as seen in our case.
We report this case because of its rare association
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Inaloz HS, Chowdhury MM, Motley RJ. Lupus erythematosus/lichen planus overlap syndrome with scarring alopecia. J Eur Acad Dermatol Venereol. 2001;15:171–4. doi: 10.1046/j.1468-3083.2001.00223.x. [DOI] [PubMed] [Google Scholar]
- 2.Grabbe S, Kolde G. Coexisting lichen planus and subacute cutaneous lupus erythematosus. Clin Exp Dermatol. 1995;20:249–54. doi: 10.1111/j.1365-2230.1995.tb01315.x. [DOI] [PubMed] [Google Scholar]
- 3.Shahzadi N, Khurshid K, Suhail Pal S. Lichen planus/lupus erythematosus overlap with hypothyroidism: a case report. J Pak Assoc Derma. 2008;18:238–40. [Google Scholar]


