Abstract
Background
Most environmental non-tuberculous mycobacteria have been demonstrated to invade amoebal trophozoites and cysts, but such relationships are largely unknown for members of the Mycobacterium tuberculosis complex. An environmental source has been proposed for the animal Mycobacterium bovis and the human Mycobacterium canettii.
Methodology/Principal Findings
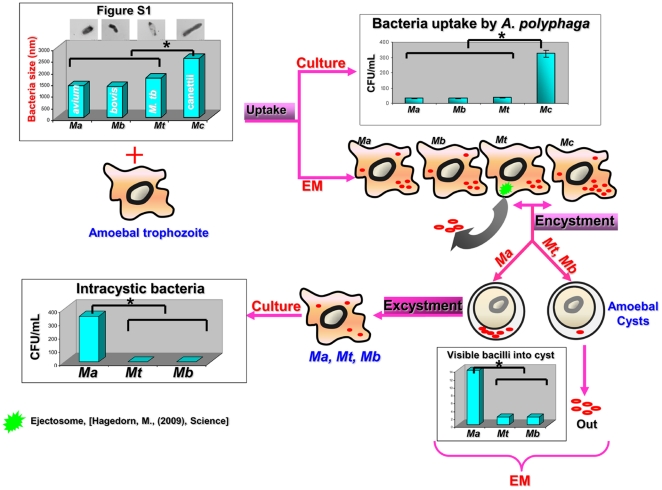
Using optic and electron microscopy and co-culture methods, we observed that 89±0.6% of M. canettii, 12.4±0.3% of M. tuberculosis, 11.7±2% of M. bovis and 11.2±0.5% of Mycobacterium avium control organisms were phagocytized by Acanthamoeba polyphaga, a ratio significantly higher for M. canettii (P = 0.03), correlating with the significantly larger size of M. canetti organisms (P = 0.035). The percentage of intraamoebal mycobacteria surviving into cytoplasmic vacuoles was 32±2% for M. canettii, 26±1% for M. tuberculosis, 28±2% for M. bovis and 36±2% for M. avium (P = 0.57). M. tuberculosis, M. bovis and M. avium mycobacteria were further entrapped within the double wall of <1% amoebal cysts, but no M. canettii organisms were observed in amoebal cysts. The number of intracystic mycobacteria was significantly (P = 10−6) higher for M. avium than for the M. tuberculosis complex, and sub-culturing intracystic mycobacteria yielded significantly more (P = 0.02) M. avium organisms (34×104 CFU/mL) than M. tuberculosis (42×101 CFU/mL) and M. bovis (35×101 CFU/mL) in the presence of a washing fluid free of mycobacteria. Mycobacteria survived in the cysts for up to 18 days and cysts protected M. tuberculosis organisms against mycobactericidal 5 mg/mL streptomycin and 2.5% glutaraldehyde.
Conclusions/Significance
These data indicate that M. tuberculosis complex organisms are amoeba-resistant organisms, as previously demonstrated for non-tuberculous, environmental mycobacteria. Intercystic survival of tuberculous mycobacteria, except for M. canettii, protect them against biocides and could play a role in their life cycle.
Introduction
Non-tuberculous mycobacteria, responsible for community-acquired and focal health-care associated infections following surgery and intervention procedures, emerged over the last decade. In France, Mycobacterium xenopi has been responsible for a large outbreak of rachis infections following vertebral disk surgery, as well as for cases of arthritis following joint surgery [1]. Likewise, Mycobacterium abscessus and Mycobacterium chelonae have been responsible for several outbreaks of surgical site infection following abdominoplasty and liposuction [2]. Also, an outbreak of Mycobacterium fortuitum furunculosis has been reported following shaving of the legs with a razor and a footbath in a nail salon [3]. Recently, large outbreaks of post-surgical infections caused by Mycobacterium bolettii and Mycobacterium massiliense involved several thousand patients in several hospitals in Brazil [4], [5].
In the aforementioned situations, infection was traced to improperly used water contaminated by non-tuberculous mycobacteria, illustrating that water was an important yet underestimated source for non-tuberculous mycobacteria. Indeed, the vast majority of non-tuberculous mycobacteria have been shown to be environmental organisms residing in soil and water [6]. It has been observed that such non-tuberculous mycobacteria could be recovered from water samples also colonized by free-living amoeba, such as a hospital water supply colonized by M. xenopi and a drinking water plant colonized by several species of non-tuberculous mycobacteria [7]. Additionally, non-tuberculous mycobacteria have been observed to reside within the cytoplasm of amoebal trophozoites, resulting in their characterization as amoeba-resistant organisms [8]. In amoeba, non-tuberculous mycobacteria could be eventually entrapped in the amoebal cyst, being uniquely located in the exocyst layer of the cyst wall [9]. These observations supported a model of a free-living amoebal cyst acting as a “Trojan horse” that protects embedded non-tuberculous, environmental mycobacteria against unfavorable conditions.
In contrast, the Mycobacterium tuberculosis complex (MTC) is uniquely comprised of seven closely related, host-associated organisms responsible for tuberculosis in mammals and humans with direct host-to-host transmission [10], [11]. MTC organisms have no known natural environmental stage, despite the fact that experimental data indicate that M. tuberculosis [12] and Mycobacterium bovis [13] could survive for hours to days in the amoebal trophozoites. These pioneering works did not firmly explore whether these MTC organisms could be further entrapped in the amoebal cyst, somewhat limiting interpretation of the data.
To gain further insight into the relationships between MTC organisms and free-living amoeba, we have quantified the relationships between representative organisms of the M. canettii, M. tuberculosis and M. bovis tuberculous species with the trophozoites and cysts of the free-living amoeba Acanthamoeba polyphaga.
Materials and Methods
Mycobacterium strains
M. tuberculosis H37Rv CIP103471, M. canettii CIP140010059T, M. bovis CIP671203 and a clinical isolate of M. avium subsp. hominissuis (herein referred to as M. avium) were subcultured on Middlebrook 7H10 agar (Becton Dickinson, Le Pont de Claix, France) for 21 days at 37°C in a 5% CO2 atmosphere. The in vitro susceptibility of these four organisms to 10 µg/mL streptomycin was determined by incubation on Middlebrook 7H9 and growth monitoring using the MGIT 960 apparatus (Becton Dickinson, Le-Pont-de-Claix, France). The susceptibility of M. avium and M. tuberculosis to glutaraldehyde was further tested by incubating M. avium and M. tuberculosis mycobacteria with 2.5% glutaraldehyde for 1 hour at room temperature, after which the cells were washed twice with phosphate buffered saline (PBS) and subcultured on Middlebrook 7H10 agar (Becton Dickinson) for 5 weeks at 37°C in a 5% CO2 atmosphere. Prior to infection, cells were harvested and dispersed by expelling the suspension 10 times through a sterile 25 gauge needle attached to a 1-mL syringe. The inoculum was adjusted to 106 mycobacteria/ml in PBS. A. polyphaga Link-AP1 strain [14], amoeba were suspended twice in Page's modified Neff's Amoeba Saline (PAS) to obtain 5×105 cells/mL, and 1 mL of such suspension was distributed into each well of a 12-well microplate (Corning, New York, USA) and inoculated with 100 µL of a 106 mycobacteria/mL suspension (Multiplicity of infection (MOI) = 1/1) of either M. tuberculosis H37Rv, M. canettii, M. bovis or M. avium. The microplate was centrifuged at 1,000× g for 30 min and then incubated at 32°C under a humidified 5% CO2 atmosphere. The microplate was examined daily for 3 days for cytopathic effect. The presence of intra-amoebal organisms was determined by shaking, 10-min centrifugation at 200× g and observation using a light microscope after Ziehl-Neelsen staining. All experiments were done in triplicate.
Encystment and excystment of infected amoeba
In 25-cm2 culture flasks (Corning, New York, USA), 10 mL of amoebal suspension infected for 24 hours was incubated with 10 µg/mL of streptomycin for 2 hours at room temperature to kill any remaining extra-amoebal and adherent mycobacteria. After treatment and washing, the trophozoites were rinsed with encystment buffer (0.1 M KCl, 0.02 M Tris, 8 mM MgSO4, 0.4 mM CaCl2 and 1 mM NaHCO3) and centrifuged at 1,000× g for 10 min, and the pellet was resuspended in 10 mL of fresh encystment buffer and incubated for three days at 32°C. Encystment of the amoeba was examined by light microscopy. After 3 days, amoebal cysts were pelleted by centrifugation at 1,000× g for 10 min. Some of the cysts were treated with 5 mg/mL of streptomycin for 48 hrs, and the remaining cysts were treated with 2.5% glutaraldehyde for 1 hour [15]. Treated cysts were washed three times with PAS. Some cysts were processed for electron microscopy (see below); the remainder was incubated for 7 days in PYG medium at 33°C. Intra-amoebal mycobacteria were released by lysing the monolayer with 1 mL of 0. 5% sodium dodecyl sulphate, followed by two successive passages through a 27-gauge needle [16]. The presence of viable mycobacteria was documented by detecting colonies on Middlebrook 7H10 agar inoculated with 100 µL of the cell lysate and incubated at 37°C for 21 days for MTC organisms and 15 days for M. avium.
Ultrastructural studies
The size of the Mycobacterium organisms was determined by transmission electron microscopy observation of 21 organisms for each species to determine the median and standard deviation of cell length. Amoebal monolayers previously infected by MTC organisms were fixed in 2% glutaraldehyde and 0.1 M cacodylate buffer overnight, then in 2% glutaraldehyde and 0.33% acroleine in 0.07 M cacodylate buffer for 1 hour. After washing in 0.2 M cacodylate buffer, the preparation was fixed in 1% osmium tetraoxide with 0.1 M potassium ferrycyanure for 1 hour and dehydrated in an ascending series of ethanol concentrations, up to 100% ethanol. The samples were then successively incubated (for 45 min) in a 3∶1, 2∶2, 1∶3 (vol/vol) ethanol-Epon suspension, then in 100% Epon overnight with continuous shaking before being embedded in an Epon 812 resin (Fluka, St Quentin Fallavier, France) incubated for 3 days at 60°C. Ultrathin sections (70 nm) were cut from the blocks using an ultracut microtome (Reichert-Leica, Marseille, France) before being deposited on Formvar-coated copper grids (Sigma-Aldrich, Taufkirchen, Germany). Ultrathin sections were stained for 10 min. with 5% uranyl acetate and lead citrate before being examined using a transmission electron microscope (Morgani 268D; Philips, Eindhoven, the Netherlands).
Measure of intraamoebal uptake and survival of mycobacteria
To measure the uptake of mycobacteria by A. polyphaga trophozoites, mycobacteria and amoeba were co-incubated at 37°C for 24 h prior to three washes with PAS. Washed trophozoites were then incubated in fresh medium containing 10 µg/mL of streptomycin for 2 hours to kill extracellular mycobacteria. The trophozoites were then washed three times with PAS and incubated at 37°C in fresh PAS. Intra-amoebal mycobacteria were released by lysing the monolayer with 1 ml of 0.5% sodium dodecyl sulphate, followed by two successive passages through a 27-gauge needle, and the lysates were plated as serial dilutions in complete Middlebrook 7H9 medium on Middlebrook 7H10 agar. Plates were incubated at 37°C for 21 days, and colony-forming units (CFUs) were counted. The intra-amoebal survival curves of M. tuberculosis, M. canettii, and M. bovis were determined after plating intra-amoebal mycobacteria after 0, 12, 24, 48, and 72 hours of infection.
Statistical analyses
Data are expressed as means ± standard deviation; unpaired Student's t-test and one-way ANOVA test were used, and a P value<0.05 was considered significant.
Results
Uptake and survival of mycobacteria in trophozoites
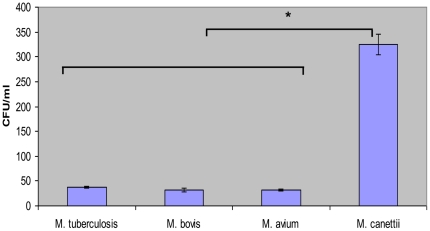
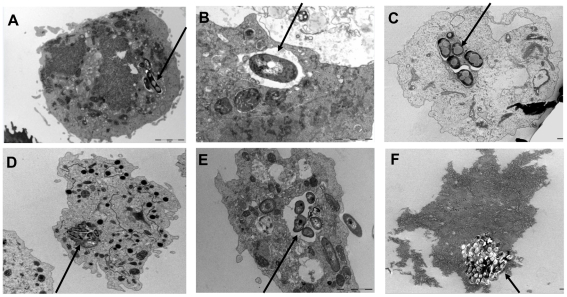
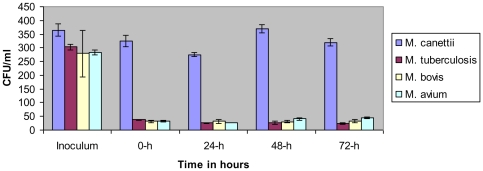
We observed that the length of mycobacterial cells used in this study was 2.56±0.5 µm for M. canettii organisms, 1.7±0.3 µm for M. tuberculosis organisms, 1.33±0.3 µm for M. bovis organisms, and 1.37±0.3 µm for M. avium organisms (Fig. S1); the length of M. canettii organisms was significantly larger than that of the three other mycobacteria (P = 0.035, one-way ANOVA). The four organisms were killed by 10 µg/mL streptomycin and M. avium and M. tuberculosis were killed also by 2.5% glutaraldehyde. Acid-fast stained A. polyphaga trophozoites exhibited intra-amoebal mycobacteria, regardless of the Mycobacterium species being studied. The proportion of inoculated mycobacteria phagocytozed by trophozoites was significantly higher (P = 0.03) for M. canettii organisms (89±0.6%) than for M. tuberculosis (12.4±0.3%), M. bovis (11.7±2%) and the M. avium control (11.2±0.5%) (Fig. 1). Phagocytosis yielded an insignificant difference in the percentage of infected amoeba, varying between 26±1% for M. tuberculosis, 28±2% for M. bovis, 32±2% for M. canettii and 36±2% for M. avium; the number of mycobacteria per trophozoite varied from 1 to 4 for M. tuberculosis, 1 to 6 for M. bovis and M. avium and from 1 to 10 for M. canettii (Fig. 2). Electron microscopy revealed that mycobacteria were residing inside one or several vacuoles without notable modification of the surrounding cytoplasm; vacuoles containing only one organism exhibited a close apposition of the vacuole membrane all over the mycobacterial cell surface (Fig. 2B). In some vacuoles, electron microscopy revealed morphological features that were compatible with mycobacterial division. Growth curves were not significantly different between the four species being studied, with the only observations being a small decrease in the number of CFUs at 24 h and minute variations in the number of CFUs from 24 h to 72 h (Fig. 3).
Figure 1. Uptake of mycobacteria by A. polyphaga trophozoites.
Cells were exposed to mycobacteria for 24 h. “*” denotes a statistically significant difference.
Figure 2. M. tuberculosis complex mycobacteria are internalized into amoeba.
Transmission electron-microscopy observation of M. tuberculosis H37Rv (A and B), M. bovis (C), M. avium (D) and M. canettii (E and F) in A. polyphaga trophozoites.
Figure 3. Survival of mycobacteria within A. polyphaga trophozoites at 33°C.
Time zero represents 24 h after infection, immediately after treatment with streptomycin. Each bar represents the mean of duplicate wells, and error bars show the standard error of the mean. “*” denotes a statistically significant difference.
Survival of mycobacteria in cysts
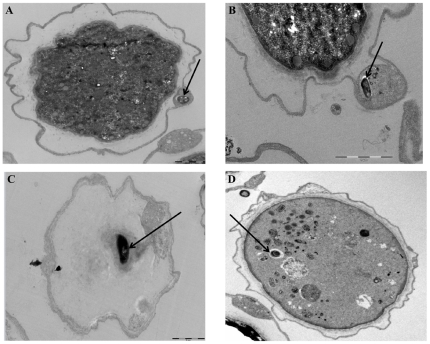
Light microscopy failed to reveal visible mycobacteria in A. polyphaga cysts three days after the induction of encystment, whereas electron microscopy observation of 300 such cysts showed M. tuberculosis, M. bovis, and M. avium organisms visible inside the A. polyphaga cysts (Fig. 4). As for these three species, we found <1% of cysts harboring mycobacteria visible in the space between the inner and outer wall of the cyst (Fig. 4A). M. bovis organisms were also observed on the inner side of the outer wall and in the cytoplasm of the cyst (Fig. 4C), as was the case for a few M. avium mycobacteria (Fig. 4D). The average number of mycobacteria per cyst was significantly higher (P = 10−6) for M. avium (5 bacilli/cyst) than for M. tuberculosis and M. bovis (1 bacillus/cyst). Further electron microscopy observation of up to 500 cysts failed to reveal any M. canettii organisms inside the A. polyphaga cysts. We further observed that a 48-hour exposure of the mycobacteria-infected cysts to 10 µg/ml streptomycin, used to kill extra-cystic mycobacteria, did not affect their excystment capacity, as new trophozoites emerged after a 7-day incubation in PYG medium at 33°C as determined by light microscopy. These cysts yielded significantly more (P = 0.02) M. avium organisms (34×104 CFU/mL) than M. tuberculosis (42×101 CFU/mL) and M. bovis (35×101 CFU/mL) in the presence of a washing fluid free of mycobacteria (Fig. 5). After the cysts were exposed to 2.5% glutaraldehyde, sub-culturing intracystic mycobacteria released 18×103 CFUs for M. avium and 220 CFUs for M. tuberculosis. A non-quantitative subculture further demonstrated that M. avium, M. tuberculosis and M. bovis organisms survived in the cysts of A. polyphaga for up to 18 days.
Figure 4. M. tuberculosis and M. bovis, but not M. canettii mycobacteria are included into amoebal cysts.
Transmission electron-microscopy observation of A. polyphaga cysts containing M. tuberculosis H37Rv (A and B) within a double cell wall, M. bovis (C) and M. avium subsp. hominissuis (D) in the cytoplasm.
Figure 5. Difference in the mechanism of interaction between MTC and M. avium.
Comparison of the size of mycobacteria by electron microscopy. M. bovis (A), M. avium (B), M. tuberculosis (C) and M. canettii (D). “*” denotes significant difference when comparing the size of M. canettii and that of the other species. Ma- Mycobacterium avium. Mb- Mycobacterium bovis. Mt- Mycobacterium tuberculosis. Mc- Mycobacterium canettii.
Discussion
In this study, M. avium, used as a control organism to certify the validity of the experimental protocol, yielded results identical to those previously published showing that M. avium survived in A. polyphaga trophozoites and cysts, therefore validating our data obtained using MTC organisms [9]. We further observed a few M. avium organisms in the cytoplasm of A. polyphaga cysts, thus adding to published observations that this organism can exist between the inner and outer cyst walls [9], [17]. We ensured that the positive observations we made did not merely result from contamination, as we thoroughly washed inoculated amoeba and treated cysts with either 5 mg/mL streptomycin or 2.5% glutaraldehyde, a concentration that we controlled to be mycobactericidal for the MTC reference strains that were examined. The negative controls examined in successive phases of the study remained negative, further indicating the authenticity of our data.
Our observation that M. tuberculosis and M. bovis organisms were engulfed by A. polyphaga trophozoites agreed with previous observations made when co-culturing M. tuberculosis organisms with the free-living amoeba Dictyostelium discodium [12] and when co-culturing M. bovis organisms with Acanthamoeba castellanii [13]. Our observation that M. canettii organisms could also be ingested by amoebal trophozoites has not been previously studied; additionally, the ratio of phagocytosed M. canettii organisms was significantly higher than the phagocytosed ratio of other mycobacteria. Interestingly, M. canettii organisms were significantly larger than the two other MTC mycobacteria being studied, a previously unreported observation. The size of particles has been shown to determine the efficiency of phagocytosis by free-living amoeba, with a 0.5 µm minimum size for inert latex particles to be ingested by Acantamoeba amoeba [18]. M. canettii organisms exhibit other unique phenotypic traits, including the smoothest colonies, which could also influence amoebal phagocytosis [19], [20]. We propose that the size of mycobacterial cells is one of the determinants of their efficient ingestion by free-living amoeba.
All MTC organisms further survived in vacuoles, as previously demonstrated for M. bovis organisms in A. castellanii hosts for 14 days [13]; we presented data indicating that survival in the amoebal trophozoite is a common property for MTC members, which should be regarded as amoeba-resistant organisms [7]. Following phagocytosis, a significantly higher number of M. canettii organisms survived in the amoeba trophozoite. Such intra-amoebal survival is consistent with the theory that amoeba-resistant organisms evolved mechanisms allowing them to also penetrate and survive in macrophages, classifying them as pathogens [8]. Whereas M. tuberculosis and M. bovis organisms have been previously demonstrated to survive in the vacuoles of macrophages, a pivotal phenotype in the pathology of tuberculosis [21], [22], such survival has not been yet reported for M. canettii. Data presented in this study suggest that M. canettii would be also an organism surviving in macrophages in line with the observation that this organism is a very rare agent of human tuberculosis after its first isolation from a 20-year-old French patient [23]. Recognizing MTC organisms as amoeba-resistant organisms agrees with their closest genomic proximity with Mycobacterium marinum, a waterborne species also capable of survival within D. discodium and A. polyphaga [16], [24], [25]. The current evolutionary model of mycobacteria proposes that the most recent common ancestor (MRCA) for M. tuberculosis and M. marinum was a common generalist environmental Mycobacterium species [26]. Recent genome analysis of the environmental Mycobacterium indicus pranii enforced a scenario in which the MRCA was an aquatic species that gave rise to waterborne M. marinum and Mycobacterium ulcerans on one branch, the Mycobacterium avium complex on a second branch and the MTC on a third branch [27]. Mycobacterium pinnepidii, an MTC organism responsible for tuberculosis in seals, indeed retained an aquatic habitat [28], [29]. In this scenario, intra-amoebal life of MRCA may have selected traits in MTC organisms that endowed them with resistance to macrophages. Such intra-amoebal survival could be exploited for laboratory diagnosis of tuberculosis from contaminated specimens; amoeba are able to allow for the survival of host-adapted organisms while destroying contaminant organisms, as previously reported for the initial recovery of the non-tuberculous Mycobacterium massiliense from human sputum [30]. Indeed, we have been able to isolate M. tuberculosis organisms from various contaminated clinical specimens using A. polyphaga as a cleaning scavenger (D. Raoult, unpublished data).
We further observed that a few M. tuberculosis and M. bovis organisms were entrapped in the amoebal cyst, more precisely located between the two external layers of the amoebal cyst, a property previously reported as a hallmark of mycobacteria among amoeba-resisting organisms [9]. However, extensive electron microscope observation failed to reveal any M. cannetii organisms in cysts and only an average number of 1 M. tuberculosis and M. bovis bacillus per infected cyst. This was in significant contrast with M. avium, which yielded an average of 5 visible bacilli per infected cyst, resulting in the fact that M. avium yielded 2 logs more viable mycobacteria than MTC organisms after the excystment of infected cysts. These data extend a previous preliminary study in which the ratio of encystment (approximately 50%) was not driven by the experimental conditions and in which M. bovis organisms were not observed in cysts [13]. Therefore, later experiments did not provide clear-cut evidence for the survival of M. bovis organisms in amoebal cysts. Combining morphological and cultural data indicates that, in contrast to M. avium, the majority of MTC organisms bypass the amoebal cyst after they are phagocytosed into the amoebal trophozoite. These data agree with the previous demonstration that M. tuberculosis organisms, but not M. avium organisms, were ejected from the amoeba Dictyostelium trophozoite by using an actin-based ejectosome [12]. MTC organisms may rely on their unique cellulase equipment, which are sugar cleaving enzymes capable of hydrolysing cellulose, a major component of the amoebal cyst cell wall [31], [32], to bypass amoebal cysts; the MTC organisms which still resided into the amoebal cyst, did resist glutaraldehyde, a biocide used to decontaminate medical devices, after entrapment in the amoebal cyst.
In conclusion, MTC should be regarded as amoeba-resistance organisms with the amoebal cyst protecting them against biocides except for M. canettii. These data may have implications for understanding the natural cycle of some MTC organisms.
Supporting Information
Comparison of the size of mycobacteria by electron microscopy. M. bovis (A), M. avium (B), M. tuberculosis (C) and M. canettii (D). There was a significant difference when comparing the size of M. canettii and that of the other species, (P = 0. 035), as assessed by unpaired Student's t test and one way ANOVA.
(TIF)
Acknowledgments
The authors acknowledge Audrey Borg and Bernard Campagna for assistance in the preparation of specimens for electron microscopy.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: The authors have no support or funding to report.
References
- 1.Astagneau P, Desplaces N, Vincent V, Chicheportiche V, Botherel A, et al. Mycobacterium xenopi spinal infections after discovertebral surgery: investigation and screening of a large outbreak. Lancet. 2001;358:747–751. doi: 10.1016/s0140-6736(01)05843-3. [DOI] [PubMed] [Google Scholar]
- 2.Furuya EY, Paez A, Srinivasan A, Cooksey R, Augenbraun M, et al. Outbreak of Mycobacterium abscessus wound infections among “lipotourists” from the United States who underwent abdominoplasty in the Dominican Republic. Clin Infect Dis. 2008;46:1181–1188. doi: 10.1086/529191. [DOI] [PubMed] [Google Scholar]
- 3.Winthrop KL, Abrams M, Yakrus M, Schwartz I, Ely J, et al. An outbreak of mycobacterial furunculosis associated with footbaths at a nail salon. N Engl J Med. 2002;346:1366–1371. doi: 10.1056/NEJMoa012643. [DOI] [PubMed] [Google Scholar]
- 4.Duarte RS, Lourenço MC, Fonseca Lde S, Leão SC, Amorim Ede L, et al. Epidemic of postsurgical infections caused by Mycobacterium massiliense. J Clin Microbiol. 2009;47:2149–2155. doi: 10.1128/JCM.00027-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Viana-Niero C, Lima KV, Lopes ML, Rabello MC, Marsola LR, et al. Molecular characterization of Mycobacterium massiliense and Mycobacterium bolletii in isolates collected from outbreaks of infections after laparoscopic surgeries and cosmetic procedures. J Clin Microbiol. 2008;46:850–855. doi: 10.1128/JCM.02052-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chilima BZ, Clark IM, Floyd S, Fine PE, Hirsch PR. Distribution of environmental mycobacteria in Karonga District, northern Malawi. Appl Environ Microbiol. 2006;72:2343–2350. doi: 10.1128/AEM.72.4.2343-2350.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomas V, Herrera-Rimann K, Blanc DS, Greub G. Biodiversity of amoebae and amoeba-resisting bacteria in a hospital water network. Appl Environ Microbiol. 2006;72:2428–2438. doi: 10.1128/AEM.72.4.2428-2438.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Greub G, Raoult D. Microorganisms resistant to free-living amoebae. Clin Microbiol Rev. 2004;17:413–433. doi: 10.1128/CMR.17.2.413-433.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ben Salah I, Drancourt M. Surviving within the amoebal exocyst: the Mycobacterium avium complex paradigm. BMC Microbiol. 2010;10:99. doi: 10.1186/1471-2180-10-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vincent V, Gutierrez MC. Mycobacterium: laboratory characteristics of slowly growing mycobacteria. In: Murray PR, Baron EJ, Jorgensen JH, Landry ML, Pfaller MA, editors. Manual of Clinical Microbiology (9th Edition) Washington DC: ASM Press; 2007. pp. 573–588. [Google Scholar]
- 11.Alexander KA, Laver PN, Michel AL, Williams M, van Helden PD, et al. Novel Mycobacterium tuberculosis complex pathogen, M. mungi. Emerg Infect Dis. 2010;16:1296–1299. doi: 10.3201/eid1608.100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hagedorn M, Rohde KH, Russell DG, Soldati T. Infection by tubercular mycobacteria is spread by nonlytic ejection from their amoeba hosts. Science. 2009;323:1729–1733. doi: 10.1126/science.1169381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taylor SJ, Ahonen LJ, de Leij FA, Dale JW. Infection of Acanthamoeba castellanii with Mycobacterium bovis and M. bovis BCG and survival of M. bovis within the amoebae. Appl Environ Microbiol. 2003;69:4316–4319. doi: 10.1128/AEM.69.7.4316-4319.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.La Scola B, Mezi L, Weiller PJ, Raoult D. Isolation of Legionella anisa using an amoebic coculture procedure. J Clin Microbiol. 2001;39:365–366. doi: 10.1128/JCM.39.1.365-366.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Greub G, Raoult D. Biocides currently used for bronchoscope decontamination are poorly effective against free-living amoebae. Infect control Hosp Epidemiol. 2003;24:784–786. doi: 10.1086/502137. [DOI] [PubMed] [Google Scholar]
- 16.Adekambi T, Ben Salah I, Khlif M, Raoult D, Drancourt M. Survival of environmental mycobacteria in Acanthamoeba polyphaga. Appl Environ Microbiol. 2006;72:5974–5981. doi: 10.1128/AEM.03075-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steinert M, Birkness K, White E, Fields B, Quinn F. Mycobacterium avium bacilli grow saprozoically in coculture with Acanthamoeba polyphaga and survive within cyst walls. Appl Environ Microbiol. 1998;64:2256–2261. doi: 10.1128/aem.64.6.2256-2261.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raoult D, Boyer M. Amoebae as genitors and reservoirs of giant viruses. Intervirology. 2010;53:321–329. doi: 10.1159/000312917. [DOI] [PubMed] [Google Scholar]
- 19.Fabre M, Hauck Y, Soler C, Koeck JL, van IJ, et al. Molecular characteristics of “Mycobacterium canettii” the smooth Mycobacterium tuberculosis bacilli. Infect Genet Evol. 2010;10:1165–1173. doi: 10.1016/j.meegid.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 20.Koeck JL, Fabre M, Simon F, Daffé M, Garnotel E, et al. Clinical characteristics of the smooth tubercle bacilli ‘Mycobacterium canettii’ infection suggest the existence of an environmental reservoir. Clin Microbiol Infect. 2010;10 doi: 10.1111/j.1469-0691.2010.03347.x. doi: 10.1111/j.1469-0691.2010.03347.x [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.de Chastellier C. The many niches and strategies used by pathogenic mycobacteria for survival within host macrophages. Immunobiology. 2009;214:526–542. doi: 10.1016/j.imbio.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 22.McDonough KA, Kress Y, Bloom BR. Pathogenesis of tuberculosis: interaction of Mycobacterium tuberculosis with macrophages. Infect Immun. 1993;61:2763–2773. doi: 10.1128/iai.61.7.2763-2773.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Canetti G. [Infection caused by atypical mycobacteria and antituberculous immunity]. Lille Med. 1970;15:280–282. [PubMed] [Google Scholar]
- 24.Hagedorn M, Soldati T. Flotillin and RacH modulate the intracellular immunity of Dictyostelium to Mycobacterium marinum infection. Cell Microbiol. 2007;9:2716–2733. doi: 10.1111/j.1462-5822.2007.00993.x. [DOI] [PubMed] [Google Scholar]
- 25.Solomon JM, Leung GS, Isberg RR. Intracellular replication of Mycobacterium marinum within Dictyostelium discoideum: efficient replication in the absence of host coronin. Infect Immun. 2003;71:3578–3586. doi: 10.1128/IAI.71.6.3578-3586.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stinear TP, Seemann T, Harrison PF, Jenkin GA, Davies JK, et al. Insights from the complete genome sequence of Mycobacterium marinum on the evolution of Mycobacterium tuberculosis. Genome Res. 2008;18:729–741. doi: 10.1101/gr.075069.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ahmed N, Saini V, Raghuvanshi S, Khurana JP, Tyagi AK, et al. Molecular analysis of a leprosy immunotherapeutic bacillus provides insights into Mycobacterium evolution. PLoS One. 2007;2:e968. doi: 10.1371/journal.pone.0000968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ahmed N, Alam M, Abdul MA, Asad RS, Cataldi A, et al. Genome sequence based, comparative analysis of the fluorescent amplified fragment length polymorphisms (FAFLP) of tubercle bacilli from seals provides molecular evidence for a new species within the Mycobacterium tuberculosis complex. Infect Genet Evol. 2003;2:193–199. doi: 10.1016/s1567-1348(02)00100-4. [DOI] [PubMed] [Google Scholar]
- 29.Cousins DV, Bastida R, Cataldi A, Quse V, Redrobe S, et al. Tuberculosis in seals caused by a novel member of the Mycobacterium tuberculosis complex: Mycobacterium pinnipedii sp. nov. Int J Syst Evol Microbiol. 2003;53:1305–1314. doi: 10.1099/ijs.0.02401-0. [DOI] [PubMed] [Google Scholar]
- 30.Adekambi T, Reynaud-Gaubert M, Greub G, Gevaudan MJ, La SB, et al. Amoebal coculture of “Mycobacterium massiliense” sp. nov. from the sputum of a patient with hemoptoic pneumonia. J Clin Microbiol. 2004;42:5493–5501. doi: 10.1128/JCM.42.12.5493-5501.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mba Medie F, Ben Salah I, Drancourt M, Henrissat B. Paradoxical conservation of a set of three cellulose-targeting genes in Mycobacterium tuberculosis complex organisms. Microbiology. 2010;156:1468–1475. doi: 10.1099/mic.0.037812-0. [DOI] [PubMed] [Google Scholar]
- 32.Mba Medie F, Vincentelli R, Drancourt M, Henrissat B. Mycobacterium tuberculosis Rv1090 and Rv1987 encode functional beta-glucan-targeting proteins. Protein Expr Purif. 2011;75:172–176. doi: 10.1016/j.pep.2010.08.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Comparison of the size of mycobacteria by electron microscopy. M. bovis (A), M. avium (B), M. tuberculosis (C) and M. canettii (D). There was a significant difference when comparing the size of M. canettii and that of the other species, (P = 0. 035), as assessed by unpaired Student's t test and one way ANOVA.
(TIF)