Abstract
Background and aims:
Our aim was to evaluate the utility of endoscopic obliterative therapy with Histoacryl for gastric varices and to investigate the incidence of serious complications.
Methods:
Endoscopic obliterative therapy with Histoacryl was performed on 129 gastric variceal patients. Sixty-five patients had cardiofornical varices, and 64 had fundal varices. Forty-five of 129 patients were emergency cases and the other 84 patients were prophylactic cases. Endoscopic therapy was performed under fluoroscopy using 70% Histoacryl (Histoacryl diluted with 5% Lipiodol).
Results:
Endoscopic hemostasis of gastric varices was successful in 45/45 (100%) emergency cases. The recurrence rate of gastric varices was 17/120 (14.2%) among patients whose variceal eradication was achieved. Additional treatment was successfully performed in all recurrent cases. The incidence of serious complications was 4/129 (3.1%), including two cases of splenic infarction, one case of pulmonary embolism, and one case of an inflammatory tumor of pancreatic tail. The two patients with splenic infarction improved with conservative medical treatment. The patient with pulmonary embolism showed no respiratory symptoms, and died of liver failure. The patient with the pancreatic tumor, which was diagnosed as an inflammatory tumor, was treated surgically.
Conclusions:
Endoscopic obliterative therapy with Histoacryl is a useful and relatively safe method for treatment of bleeding gastric varices. Nonetheless, careful attention must be paid to avoid potentially serious complications.
Keywords: cyanoacrylate, endoscopic obliterative therapy, gastric varices, Histoacryl
Introduction
Endoscopic treatments for bleeding esophageal varices, including endoscopic injection sclerotherapy and endoscopic variceal ligation, are accepted worldwide today. Bleeding gastric varices can also be treated successfully by injection of cyanoacrylate.
N-butyl-2-cyanoacrylate (Histoacryl, B.Braun Dexon GmbH Spangenberg, Germany) is a tissue glue monomer that polymerizes and solidifies instantly upon contact with blood. Soehendra et al were the first to report the usefulness of Histoacryl in the treatment of bleeding gastric varices,1 which have a high mortality rate. Endoscopic obliterative therapy with Histoacryl, although useful for treating bleeding gastric varices,2–6 has drawbacks that include embolic and septic complications.
In this study, we report on the therapeutic effects and serious complications encountered with endoscopic obliterative therapy using Histoacryl.
Methods
Patients
One hundred twenty-nine patients with gastric varices and portal hypertension who underwent endoscopic obliteration therapy with Histoacryl were evaluated retrospectively (76 men and 53 women; age range, 30–81 years; mean, 61.5 years). Among these patients, 45 were emergency cases and the other 84 were prophylactic cases; 55 patients were classified as Child-Pugh class A, 30 as class B, and 44 as class C. The pathology underlying portal hypertension was liver cirrhosis (LC) in 84 patients, cirrhosis associated with hepatocellular carcinoma (HCC) in 31 patients, primary biliary cirrhosis in four patients, idiopathic portal hypertension in five patients, and other diseases in five patients. LC was confirmed by a combination of clinical, biochemical, and ultrasound criteria, and HCC was diagnosed using imaging and biopsy. Etiologies of cirrhosis in the 115 cases included 22 with hepatitis B surface antigen (HBsAg) positivity, 67 with hepatitis C virus (HCV) positivity, 21 with alcoholic liver disease, and 5 unknown. The study was performed according to the tenets of the Declaration of Helsinki, and was approved by the Ethics Committee at Sapporo Kosei Hospital. Written informed consent was obtained from all patients prior to the procedure.
Endoscopic findings
Endoscopic findings were evaluated according to the general rules for recording endoscopic findings of esophago-gastric varices established by the Japanese Research Society on Portal Hypertension.7 The variceal form was classified as small and straight (F1), enlarged and tortuous (F2), or large and coil-shaped (F3). Variceal location was classified as cardiac (Lg-c, located adjacent to the cardiac orifice), fundal (Lg-f, located far from the cardiac orifice), or cardiac and fundal (Lg-cf, located between the cardiac orifice and the fornix). The red color sign (RC) referred to dilated, small vessels or telangiectasia on the variceal surface. Among the 129 patients, 94 had F2 type and 35 had F3 type varices. Locations of varices were Lg-f in 64 patients and Lg-cf in 65. Fourteen patients among the 129 had RC-positive varices, whereas 25 showed erosion of the variceal surface. Sixteen of the 129 patients were also afflicted with esophageal varices. Using computed tomography (CT), gastric varices were detected in all 129 patients and gastro-renal shunt as vessels flowing out of the gastric varices were detected in 107 of the 129 patients (83.0%).
Methods
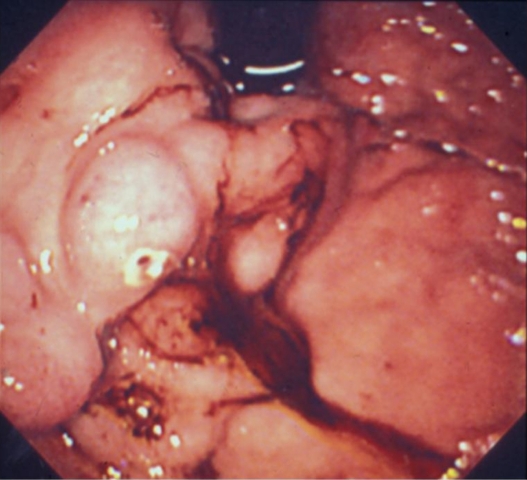
In 45 emergency cases, endoscopic examination was performed after stabilizing the general condition of the patients. When spurting or oozing bleeding, a red or white plug, or tiny erosion was observed (gastric varices) during emergency endoscopic examination (Figure 1a), endoscopic obliteration therapy using Histoacryl for hemostasis was performed immediately. Prophylactic endoscopic obliteration therapy using Histoacryl was performed on the remaining 84 patients due to a high risk of bleeding. Risk of bleeding was determined by the presence of varices that enlarged in a short time, showed red color sign or erosion on their surface or showed high gastric blood flow velocity and thin gastric wall thickness to submucosal gastric varices using endoscopic color Doppler ultrasonography.
Figure 1a.
Image of a white plug observed on gastric varices during emergency endoscopic examination.
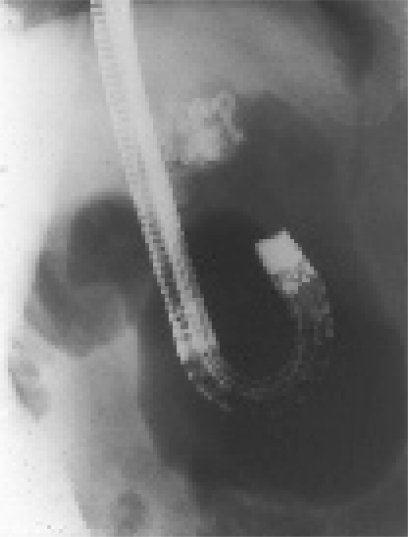
For endoscopic obliterative therapy for gastric varices, we used Histoacryl diluted to a final concentration of 70% in 5% Lipiodol (Guerbert, Roissy, France). Lipiodol prevents the tissue adhesive from polymerizing too quickly and also allows for radiographic monitoring. Obliterative therapy was performed repeatedly with a 23-gauge needle until gastric varices disappeared. Fluoroscopic observation with an infusion of 70% Histoacryl (avoiding flow into systemic circulation) was performed to determine the extent of the varices (Figure 1b). Gastric variceal recurrence was defined by red color sign on variceal surface or variceal bleeding.
Figure 1b.
Image of fluoroscopic observation with infusion of 70% Histoacryl to determine the extent of the varices.
Results
Using endoscopy, ten of 45 emergency cases showed active bleeding from gastric varices, whereas a fibrin plug or erosion of the variceal surface was detected in the other 35 patients. Endoscopic hemostasis was successful in 45/45 (100%) in emergency cases.
Eradication of gastric varices was achieved in 120 of 129 (93.0%) patients. Among these patients, the number of endoscopic treatments required for variceal eradication varied from one to six (two patients with one session, 63 with 2 sessions, 51 with 3 sessions, and 4 with four to six sessions). Total amount of Histoacryl ranged 1.5–8.0 mL; mean, 3.2 mL) in these 129 cases.
Varices reoccurred in 17 of the 120 patients (14.2%) in whom eradication was achieved, including 9/45 (20.0%) emergency cases and 8/75 (10.7%) prophylactic cases. Additional treatment was performed successfully in most cases.
The rate of serious complications related to the procedure was 4/129 (3.1%), and included one case of pulmonary embolism, one case of an inflammatory tumor of the pancreatic tail, and two cases of splenic infarction. Total amount of Histoacryl was 2.5–8.0 mL (mean 4.3 mL) in these 4 cases. Using CT, gastric varices and gastro-renal shunt were detected in these 4 patients.
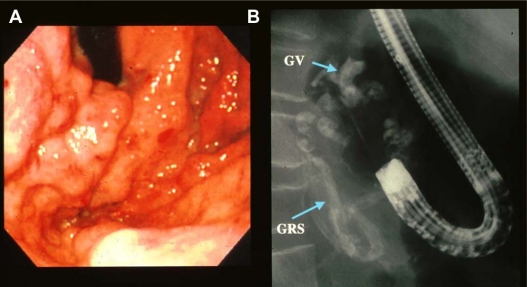
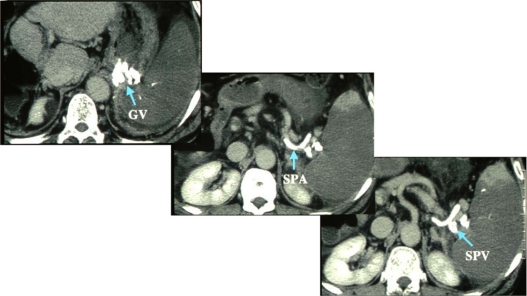
Both patients (F3, Lg-cf varices, see Figure 2a) with splenic infarction experienced persistent pain in their left upper quadrant immediately after injection, and developed a fever of 38 °C within five hours. We performed obliterative therapy using 70% Histoacryl under fluoroscopy (three times with a 2.5 mL total volume of Histoacryl (Figure 2b) in one case, and two times with a 2.5 mL volume in the other case). CT demonstrated large infarctions (70% in one case, and 90% in the other case, see Figure 2c) in the spleen. During hospitalization, white cell and platelet counts rose to two to three times above normal levels within 14 days. Fever and abdominal pains subsided gradually to full recovery with only conservative medical treatment and antibiotics in these 2 cases.
Figure 2.
A) Endoscopic image that reveals F3, Lg-cf varices with erosion. B) Image of endoscopic obliterative therapy under fluoroscopy using 70% Histoacryl in this patient.
Abbreviations: GV, gastric varices; GRS, gastro-renal shunt.
Figure 2c.
Five days after obliterative therapy, CT images demonstrate large infarctions encompassing 90% of the spleen.
Abbreviations: GV, gastric varices; SPA, splenic artery; SPV, splenic vein.
The patient (F3, Lg-cf varices) who developed a pulmonary embolism underwent four sessions endoscopic obliterative therapy under fluoroscopy, receiving a total of 8.0 mL Histoacryl due to varices of large size. Five hours later, the patient developed a fever of 38 °C and chest radiographs showed unusual nodular radiopaque pulmonary emboli along the pulmonary vessels. This patient showed no respiratory symptoms and died of liver failure with HBsAg positive liver cirrhosis.
Two years after endoscopic obliterative therapy using 70% Histoacryl, one patient developed an inflammatory tumor of the pancreatic tail, which we noted as a possible complication of the therapy. Endoscopic therapy was performed during two sessions using the total amount of Histoacryl being 4.0 mL.
Following CT and endoscopic ultrasonography (EUS), we performed surgery on the patient. Histopathological examination of the resected tumor revealed an encapsuled abscess formation with foreign body reaction and necrotic tissue surrounding the abscess. There were no Histoacryl deposits in the tumor.
Discussion
Endoscopic obliterative therapy with Histoacryl is useful for emergency control of acute gastric variceal bleeding. Histoacryl polymerizes immediately on contact with blood, resulting in rapid hemostasis. It is now the first-choice treatment worldwide for obliteration of bleeding gastric varices.2–6 The results of this study confirm that endoscopic injection of Histoacryl is highly effective for the treatment of gastric varices.
Common complications of the procedure include fever and chest pain due to an inflammatory response.8,9 Major complications of the procedure include ulceration and recurrent bleeding, although more serious complications, including embolization to the brain,10 portal vein,11 lung,12–17 and spleen17,18 have also been reported. Other complications include bacteremia,19 abscesses,20,21 and development of visceral fistula.22
Acute and chronic inflammatory changes with Histoacryl include perivascular inflammation and vessel wall necrosis with a foreign body reaction. Perigastric abscesses may be induced by perivascular inflammation with infection.20,21 Risk factors for extravariceal embolization with Histoacryl treatment include a large injection volume, dilution of radiolucent Histoacryl with radiopaque Lipiodol, speed of injection, and the presence of shunts.16,23,24 In our study, complications related to the procedure occurred in four (3.1%) patients, including two cases of splenic infarction, one case of pulmonary embolism, and one case of inflammatory tumor of the pancreatic tail.
Previously, Hwang et al evaluated the incidence of pulmonary embolism following N-butyl-2-cyanoacrylate endoscopic treatment for bleeding gastric varices and concluded that radiographically evident pulmonary embolisms were uncommon, but were more likely to occur in patients receiving a higher volume of liquid acrylate.16 Splenic infarction can occur when splenic vasculature is compromised by exposure to injected tissue adhesive agent,18 and may be complicated by splenic vein occlusion.25 Such infrequent cases of splenic infarction have been shown to be responsive to splenic artery embolization.26,27 Inflammatory tumor of pancreas is a novel complication of endoscopic obliterative therapy with Histoacryl. Prior to surgery, we were unable to diagnose the inflammatory tumor accurately, as CT, EUS, and angiographic findings all contributed to a preoperative diagnosis of advanced pancreatic cancer with splenic vein occlusion.
To prevent Histoacryl from solidifying too quickly, dilution with Lipiodol is necessary. In the cases described here, we used Histoacryl at a concentration of 70% in Lipiodol. Nonetheless, it should be noted that two of the risk factors for extravariceal embolization with Histoacryl treatment include a large injection volume, and dilution of radiolucent Histoacryl with radiopaque Lipiodol. Larger volumes of Histoacryl used for treating varices of higher blood volumes increase the chance of leakage, and by prolonging polymerization, overdilution with Lipiodol can increase the risk of embolizaion. To avoid embolic complications as much as possible, we recommend that endoscopists aim to use the smallest volume of Histoacryl necessary for obliteration, and to use Histoacryl in the most concentrated form practicable.
In conclusions, our results demonstrate the high efficacy and relative safety of Histoacryl used in treating gastric varices, but that careful attention must be paid to avoid potentially serious complications.
Footnotes
Disclosure
No conflicts of interest were declared in relation to this paper.
References
- 1.Soehendra N, Nam VC, Grimm H, Kempeneers I. Endoscopic obliteration of large esophagogastric varices with bucrylate. Endoscopy. 1986;18:25–26. doi: 10.1055/s-2007-1013014. [DOI] [PubMed] [Google Scholar]
- 2.Ogawa K, Ishikawa S, Naritaka Y, et al. Clinical evaluation of endoscopic injection sclerotherapy using n-butyl-2-cyanoacrylate for gastric variceal bleeding. J Gastroenterol Hepatol. 1999;14:245–250. doi: 10.1046/j.1440-1746.1999.01842.x. [DOI] [PubMed] [Google Scholar]
- 3.Huang YH, Yeh HZ, Chen GH, et al. Endoscopic treatment of bleeding gastric varices by N-butyl-2-cyanoacrylate (Histoacryl) injection: long-term efficacy and safety. Gastrointest Endosc. 2000;52:160–167. doi: 10.1067/mge.2000.104976. [DOI] [PubMed] [Google Scholar]
- 4.Dhiman RK, Chawla Y, Taneja S, Briswas R, Sharma TR, Dilawari JB. Endoscopic sclerotherapy of gastric variceal bleeding with N-butyl-2-cyanoacrylate. J Clin Gastroenterol. 2002;35:222–227. doi: 10.1097/00004836-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Akahoshi T, Hashizume M, Shimabukuro R, et al. Long-term results of endoscopic Histoacryl injection sclerotherapy for gastric variceal bleeding: a 10-year experience. Surgery. 2002;131:S176–S181. doi: 10.1067/msy.2002.119501. [DOI] [PubMed] [Google Scholar]
- 6.Fry LC, Neumann H, Olano C, Malfertheiner P, Monkemuller K. Efficacy, complications and clinical outcomes of endoscopic sclerotherapy with N-butyl-2-cyanoacrylate for bleeding gastric varices. Dig Dis. 2008;26:300–303. doi: 10.1159/000177012. [DOI] [PubMed] [Google Scholar]
- 7.Idezuki Y. General rules for recording endoscopic findings of esophagogastric varices. World J Surg. 1995;19:420–423. doi: 10.1007/BF00299178. [DOI] [PubMed] [Google Scholar]
- 8.Feretis C, Tabakopoulos D, Benakis P, Xenofontos M, Golematis B. Endoscopic hemostasis of esophageal and gastric variceal bleeding with Histoacryl. Endoscopy. 1990;22:282–284. doi: 10.1055/s-2007-1012872. [DOI] [PubMed] [Google Scholar]
- 9.Naga M, Foda A. An unusual complication of Histoacryl injection. Endoscopy. 1997;29:140. doi: 10.1055/s-2007-1004099. [DOI] [PubMed] [Google Scholar]
- 10.See A, Florent C, Lamy P, Levy VG, Bouvry M. Cerebrovascular accidents after endoscopic obturation of esophageal varices with isobutyl-2-cyanoacrylate in 2 patients. Gastroenterol Clin Biol. 1986;10:604–607. [PubMed] [Google Scholar]
- 11.Moustafa I, Omar MM, Nouh A. Endoscopic control of gastric variceal bleeding with butyl cyanoacrylate. Endoscopy. 1993;25:A11. [PubMed] [Google Scholar]
- 12.Thakeb F, Salama Z, Salama H, et al. The value of combined use of N-butyl-2-cyanoacrylate and ethanolamine oleate in the management of bleeding esophagogastric varices. Endoscopy. 1995;27:358–364. doi: 10.1055/s-2007-1005714. [DOI] [PubMed] [Google Scholar]
- 13.Takasugi JE, Shaw C. Inadvertent bucrylate pulmonary embolization: a case report. J Thorac Imag. 1989;4:71–73. doi: 10.1097/00005382-198910000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Moustafa I, Omar MM, Nouh A. Endoscopic control of gastric variceal bleeding with butyl cyanoacrylate in patients with schistosomiasis. J Egypt Soc Parasitol. 1997;27:405–410. [PubMed] [Google Scholar]
- 15.Roesh W, Rexroth G. Pulmonary, cerebral and coronary emboli during bucrylate injection of bleeding fundic varices. Endoscopy. 1998;30:S89–S90. doi: 10.1055/s-2007-1001406. [DOI] [PubMed] [Google Scholar]
- 16.Hwang SS, Kim HH, Park SH, et al. N-butyl-2-cyanoacrylate pulmonary embolism after endoscopic injection sclerotherapy for gastric variceal bleeding. J Comput Assist Tomogr. 2001;25:16–22. doi: 10.1097/00004728-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Tan YM, Goh KL, Kamarulzaman A, et al. Multiple systemic embolisms with septicemia after gastric variceal obliteration with cyanoacrylate. Gastrointest Endosc. 2002;55:276–278. doi: 10.1067/mge.2001.118651. [DOI] [PubMed] [Google Scholar]
- 18.Cheng PN, Sheu BS, Chen CY, Chang TT, Lin XZ. Splenic infarction after histoacryl injection for bleeding gastric varices. Gastrointest Endosc. 1998;48:426–427. doi: 10.1016/s0016-5107(98)70018-5. [DOI] [PubMed] [Google Scholar]
- 19.Chen WC, Hou MC, Lin HC, et al. Bacteremia after endoscopic injection of N-butyl-2-cyanoacrylate for gastric variceal bleeding. Gastrointest Endosc. 2001;54:214–218. doi: 10.1067/mge.2001.116566. [DOI] [PubMed] [Google Scholar]
- 20.Nishida K, Noda T, Kawazoe S, Takahashi K, Namoto M, Yoshizaki M. Perigastric abscess after endoscopic injection sclerotherapy (EIS) using Histoacryl for bleeding from gastric varices. Endosc Dig. 1997;9:1276–1281. [in Japanese with an English abstract]. [Google Scholar]
- 21.Verger P, Blais J, Gruau M, Haffaf Y. Retrogastric abscess secondary to gastric varices obturation with cyanoacrylate. Gastroenterol Clin Biol. 1998;22:248–249. [PubMed] [Google Scholar]
- 22.Battaglia G, Morbin T, Patarnello E, Merkel C, Corona MC, Ancona E. Visceral fistula as a complication of endoscopic treatment of esophageal and gastric varices using isobutyl-2-cyanoacrylate: report of two cases. Gastrointest Endosc. 2000;52:267–270. doi: 10.1067/mge.2000.105080. [DOI] [PubMed] [Google Scholar]
- 23.Seewald S, Sriram PV, Naga M, et al. Cyanoacrylate glue in gastric variceal bleeding. Endoscopy. 2002;34:926–932. doi: 10.1055/s-2002-35312. [DOI] [PubMed] [Google Scholar]
- 24.Kok K, Bond RP, Duncan IC, et al. Distal embolization and local vessel wall ulceration after gastric variceal obliteration with N-butyl-2-cyanoacrylate: a case report and review of the literature. Endoscopy. 2004;36:442–446. doi: 10.1055/s-2004-814323. [DOI] [PubMed] [Google Scholar]
- 25.Kurt M, Onal IK, Ibis M, Tas A, Ozderin YO, Okten RS. Splenic infarction: rare complication of N-butyl-2-cyanoacrylate injection for gastric varices. Dig Endosc. 2010;22:74–75. doi: 10.1111/j.1443-1661.2009.00922.x. [DOI] [PubMed] [Google Scholar]
- 26.Yu LK, Hsu CW, Tseng JH, Liu NJ, Sheen IS. Splenic infarction complicated by splenic artery occlusion after N-butyl-2-cyanoacrylate injection for gastric varices: case report. Gastrointest Endosc. 2005;61:343–345. doi: 10.1016/s0016-5107(04)02583-0. [DOI] [PubMed] [Google Scholar]
- 27.Martins Santos MM, Correia LP, Rodrigues RA, Lenz Tolentino LH, Ferrari AP, Della Libera E. Splenic artery embolization and infarction after cyanoacrylate injection for esophageal varices. Gastrointest Endosc. 2007;65:1088–1090. doi: 10.1016/j.gie.2006.10.008. [DOI] [PubMed] [Google Scholar]