Abstract
Background
Despite the positive conclusions of several randomized controlled trials and the publication of national recommendations on colorectal cancer (crc) screening, uptake remained low. The inauguration of the National Colorectal Cancer Screening Network in 2007, the same year that the first screening program was announced in Canada, provided an opportunity for integrated knowledge translation to accelerate the processes of program implementation and screening uptake.
Aim
Two primary aims were identified. The first focused on means to monitor the effects of various implementation plans in delivering high-quality population-based crc screening. The second focused on identifying and addressing knowledge gaps that may impair screening participation.
Method
The methods used are described in the context of the knowledge-to-action cycle and demonstrate that the initiative itself dictates the point in the cycle at which to start.
Results
The identified need to monitor various implementation plans resulted in the shared development of a quality determinants document. All programs committed to designing data collection so that core components could be measured and compared; 6 operating programs have conducted the first data collection, which will allow for monitoring and for new knowledge creation as the process develops further. The knowledge gap identification project started with new knowledge creation, which identified a higher-than-expected willingness of Canadians to discuss crc screening with physicians, but a low level of understanding of screening as a wellness-related behaviour. Knowledge translation interventions have been developed with the stakeholders to address those gaps, and ongoing surveys to be carried out later in 2011 will help to gauge progress in the understanding and acceptance of crc screening by the population.
Conclusions
A national network that engaged all programs, policymakers, experts, and lay representatives successfully used knowledge translation principles to enhance the trajectory of crc screening in Canada.
Keywords: Knowledge translation, colorectal cancer, screening, screening programs
1. INTRODUCTION
The knowledge-to-action trajectory for colorectal cancer (crc) screening did not immediately have a steep upward slope in Canada. In 2001, the Canadian Preventive Services Task Force recommended the inclusion of crc screening in the routine health plans of Canadians 50–74 years of age 1. A year later, population-based recommendations for Canada were published, also advocating regular screening in the same target age group, using a fecal test at the entry level and colonoscopy as the diagnostic follow-up 2. Also recommended was that the screening be done within organized provincial screening programs.
In the first few years after publication of the recommendations, the uptake of crc screening remained quite low. In 2003, the Canadian Community Health Survey indicated that self-reported use of fecal occult blood tests in the preceding 2 years ranged from 4% to 14% among adults 50–74 years of age in the 4 provinces—Newfoundland and Labrador, Saskatchewan, British Columbia, Ontario—that included the associated questions in the survey 3. This low rate was only marginally better among people who regularly saw physicians. In fact, only about 20% of those who had seen their physician more than 4 times in the preceding year were up-to-date for screening 4. A survey in Alberta in 2004 reported that 14.3% of average-risk Albertans 50–74 years of age were up-to-date with crc screening when either endoscopy or fecal tests were considered 5. Further, despite the call in 2002 for organized provincial programs, progress was very slow. Five years later, little had changed. No provincial programs were announced until January 2007 6.
In April 2007, the Canadian Partnership Against Cancer (cpac) was inaugurated. This organization was charged with implementing a national cancer control strategy, the outline of which had been developed by a number of stakeholders over several years 7. One of the action groups that developed the strategy was the Screening Action Group; when cpac was formally announced, one of its first recommendations was to develop a National Colorectal Cancer Screening Network (nccsn). The primary goals of the network would be to accelerate the knowledge-to-action trajectory in crc screening in Canada and to facilitate implementation of organized crc screening programs across Canada.
The present article describes two of the knowledge translation (kt) initiatives undertaken in the first few years of the nccsn. The first initiative, developing the means to monitor various implementation plans, is an example of the action cycle component of the knowledge-to-action framework outlined by Graham and colleagues 8 and demonstrates how movement through the knowledge-to-action cycle can result in new knowledge creation. The second initiative, focusing on knowledge gaps that may impair screening participation, demonstrates the knowledge creation component and how it moved forward into the knowledge-to-action cycle. In describing these two interrelated initiatives, we hope to illustrate the value of tailoring kt initiatives depending on the phase of development of each initiative. We also intend to show how networks that involve the primary implementers of population-based programs can accelerate the knowledge-to-action trajectory and thereby maximize the impact of interventions on a target population.
2. IMPLEMENTATION
2.1. The NCCSN: Network Formulation
The development of the network provided an ideal platform for integrated kt, as described by Graham and Tetroe 9. In effect, the network was organized to involve policymakers, implementers, and content experts and, in so doing, to allow for rapid information exchange and knowledge transfer. In letters sent in the summer of 2007, nominees in each province were sought for the network. Deputy ministers of health were invited to identify the representative within their department who would be most involved in the consideration and potential development of crc screening programs. Provincial cancer agencies, or their equivalents, all of whom had facilitated the development of organized breast cancer screening programs in the 1990s, were invited to nominate a representative who would likely be involved in the development and implementation of a crc screening program. Finally, the Public Health Association of Canada, professional organizations, and key non-governmental organizations, including some crc advocacy groups, were invited to nominate representatives to the network.
The network met initially about 4 times annually, and within the first 6 months, the process led to the foregoing two issues (evaluation of various implementation strategies through measurement of quality determinants, and maximization of participation) being identified as priorities for the group. Thus, the stage was set from which kt could be built through the action plans concerning those issues.
2.2. Initiatives in Evaluation of Program Implementation
On the surface, it could appear that the knowledge creation required to implement crc screening was largely complete well before the first program was announced. Randomized controlled trials had been published 10–14, resulting in the national recommendations cited earlier 1,2. In fact, as plans for each program were developed and announced, all aligned themselves with the national recommendations (target age 50–74 years, fecal test as the entry-level test, colonoscopy as the preferred follow-up test).
However, as is often the case in health care, the optimal strategies for implementation of evidence-based practices are often unknown, and ideal mechanisms could vary across different contexts. Thus, it was not surprising that the modes of implementation varied from province to province (Table i). For example, some provinces used direct mailing of invitations and tests as the entry point; others based recruitment on family physician referral or introduced physician incentive programs to enhance recruitment. All programs used a fecal test as the entry-level test, but some programs used the guaiac-based tests on which the original randomized controlled trial results were based 10–14, and still others used fecal immunochemical tests, which are newer test methods that are more specific for human hemoglobin 15,16. Thus, there was interest in developing methods for assessing the impact that these various strategies—all of which were reasonable, given varying provincial contexts—would have on the eventual outcomes of crc screening. In other words, the programs found themselves in the knowledge-to-action realm of “select, tailor and implement evaluations,” and they were therefore interested in moving forward in the cycle to allow for an evaluation of outcomes, and from there to further program refinement. To that end, the participants agreed to pursue an agenda of uncovering the key quality determinants of crc screening programs, building those determinants into their data collection methods, and reporting on them to one another so as to rapidly transfer knowledge on ideal program approaches.
TABLE I.
Program components for test characteristics and recruitment, active colorectal cancer screening programs
| Province |
Entry level test |
Fecal test recruitment method |
|||||
|---|---|---|---|---|---|---|---|
| gfobt | fit | Physician | Self-referral through pharmacy | Mailed invitation letter | Mailed fecal test | Other | |
| British Columbia | ✓ | ✓ | ✓ | ✓ (trial/pilot) |
✓ (by contacting the call centre to register participation) |
||
| Alberta | ✓ | ✓ (in future) |
|||||
| Saskatchewan | ✓ | ✓ (primary method) |
✓ (3 weeks after letter) |
✓ (by calling the program) |
|||
| Manitoba | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ (distributed through the Manitoba Breast Screening Program) |
|
| Ontario | ✓ | ✓ (primary method) |
✓ | ✓ (pilot fall 2009) |
✓ (by calling Telehealth Ontario) |
||
| Prince Edward Is. | ✓ | ✓ | ✓ | ✓ | |||
| Nova Scotia | ✓ | ✓ | ✓ (2 weeks after letter) |
||||
gfobt = guaiac fecal occult blood test; fit = fecal immunochemical test.
The knowledge-to-action framework notes that, to ensure that the “research” data collected are relevant to the information needed for actual implementation, end-users of the knowledge should be included in determining the data to be collected 17. That approach was an integral part of the process. In addition to the policymakers and implementation leaders who were already network members, stakeholders representing expertise in laboratories, pathology, endoscopy, and oncology were included. Some international experts were included as well. The process was further informed by the participation of several nccsn members in the International Colorectal Cancer Screening Network, which was working toward identifying higher-level quality data points for future international comparisons 18.
The first priority was to develop a common set of quality determinants (concepts related to quality) and quality indicators (to allow for practical and reliable comparisons). In May 2008, the network, with the support of cpac, engaged stakeholders from across Canada in a process to identify those elements. Quality determinants were grouped under 4 main categories: crc screening programming, entry-level tests, colonoscopy, and pathology. At the end of the process, a preliminary list of quality determinants and indicators was completed for each group. A smaller working group of network members led further refinement. Subsequently, network consensus formed around 5 key quality determinants (participation, screening, diagnostic follow-up, case management, and program outcomes) and an initial set of 20 quality indicators. All are documented in Quality Determinants for Colorectal Cancer Screening in Canada 19.
To move into the phase of actual monitoring and potential evaluation, the working group reconvened in January 2010 and developed a work plan to outline detailed definitions for the indicators and to develop a process for the collection, analysis, and reporting of the aggregated data results. Definitions and calculations for each indicator were then carefully reviewed, detailing the possible effects of various program implementation patterns (an important part of these discussions and decisions), so that results over time could be adequately compared.
Based on the agreed-on definitions, reporting templates were drafted by the analytics division of cpac. Working group members tested the templates in their own jurisdictions in relation to the definitions and the aggregated data flow. Once all feedback was received and revisions were complete, a final set of templates was distributed to the provinces able to submit results for crc screens taking place between April 2008 and March 2009.
At the first call for data, 6 provinces were able to submit. Given the early stage of development of the programs at this point (only 1 program was fully implemented province-wide), this step toward pan-Canadian adoption and an ability to assess the effects of various implementation strategies and of rapid knowledge transfer on ideal program approaches was significant. The process is well documented, and planning has begun for the 2nd and 3rd reporting cycles. As programs continue to develop and evolve, future reports will be widely disseminated and used in a consideration of the impacts of various implementation strategies on the programs themselves.
2.3. Initiatives Encouraging Physician Referral for CRC Screening
In focused and localized Canadian surveys done just before the launch of the first crc screening programs, physicians identified potential barriers to the diffusion of crc screening. In general, physicians believed that patients would not comply with screening. In one province, 39.8% of primary care providers 20 and 36.8% of specialist groups 21 believed that patients would be unlikely to accept a recommendation for a fecal test. However, American surveys revealed that physicians were more pessimistic than patients. Although more than half the physicians indicated that embarrassment was a barrier to patient participation in screening, only 8.5% of the patients who were not active screeners actually cited embarrassment as a reason not to be screened 22. Clearly, there were potential gaps in physician beliefs about the willingness of their patients to respond to suggestions for screening and the self-reported patient likelihood to accept such recommendations.
At the time the programs launched, however, little national information was available on public attitudes or uptake of crc screening. The Canadian Community Health Survey, which provides data on breast and cervical screening uptake across Canada, did not include crc screening questions as core questions until 2008. Further, although that survey is an excellent source of information on self-reported screening practices, it does not explore the knowledge, attitudes, and behaviours that could either predispose to screening or act as barriers. Thus, the network developed a strategy to create the knowledge required to understand those issues in the Canadian context and then to address them with health care providers and the public. In this case, then, knowledge creation was key and would be required to drive the knowledge-to-action cycle.
To acquire the necessary information quickly, cpac issued a call for proposals for a telephone survey of the Canadian public in the target age group. As a result, a survey research organization (Angus Reid Public Opinion, a division of Vision Critical) and a hospital-based academic research unit (Applied Health Research Centre, St. Michael’s Hospital, Toronto, ON) worked together, in consultation with cpac, to design and execute the survey. The work was carried out with the understanding that the data would be available immediately to cpac and the network for application to their work, but that academic publication of more complex analyses by the research group would also be encouraged. The design used random-digit dialling, was conducted in English or French, and enrolled nearly 2500 Canadians 50–74 years of age.
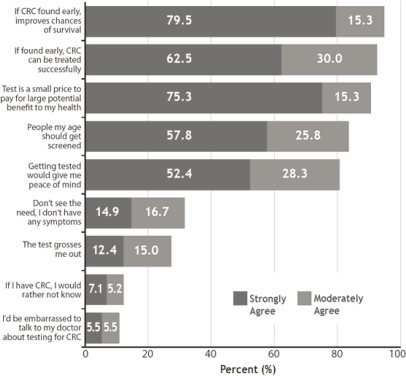
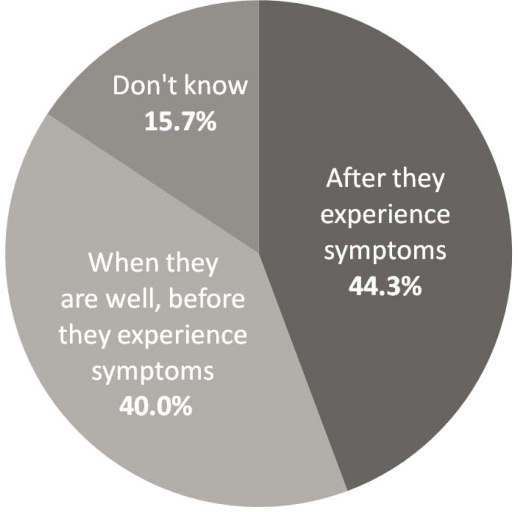
The results of the survey showed a number of areas for potential knowledge transfer and targeted action. First, more than 90% of the public 50–74 felt that crc screening was a small price to pay for a large potential health benefit (Figure 1). Only 11% felt that they would be too embarrassed to discuss crc screening with their doctor. The value of conversation with the health care provider was underlined by the finding that those who had had such a conversation were several times more likely to be up-to-date for screening than those who had not. However, one critical point was found when probing further on the meaning of screening: most participants thought that screening was important, but only 40% were aware that the core concept of screening is to be tested when asymptomatic, with the intention of intervening as early as possible (Figure 2).
FIGURE 1.
Percentage of Canadians 50–74 years of age agreeing (strongly or moderately) with statements about colorectal cancer (crc) 23.
FIGURE 2.
Perceptions among Canadians 50–74 years of age about the time at which screening first occurs 23.
Concurrent with the survey of the public, focus groups of physicians across Canada were convened to discuss potential barriers in fuller depth. The results of the surveys, together with interprovincial comparisons that were expected to be helpful in local jurisdictions, were presented to the network at their regular meetings.
With those data, a kt approach designed with the input of several network members set out to address the identified issues with primary care providers and specialists. The first and simplest strategy was to make physicians aware of the gap between professional and public comfort with crc screening—in other words, to let them know that their initiation of a conversation about screening would be valued by most patients and that it would sharply increase the likelihood that those patients would be screened. The second was to make physicians and the public aware of the value of a conversation about screening in motivating target-age individuals to be screened. Finally, tools were developed that could be used by practitioners to support crc recommendations to patients, to give further information on fecal testing in case office counselling time was not sufficient to do so, or if patient (or provider) embarrassment made the discussion of the mechanics of fecal testing uncomfortable.
The awareness gap had already been approached to some degree through publication of a commentary in the major family practice journal in Canada, pointing out some of the contrasts in physician and public perceptions 24.
Once the up-to-date and comprehensive Canadian survey data were available, several approaches were taken. Press releases, which received excellent national coverage, announced the first survey results. Short and accessible publications, which were reviewed by primary care providers before release, were developed, with key messages on crc screening highlighted. These were inserted in the mailing packages with the single largest-circulation general medical journal in Canada 25. The inserts, and more-detailed resources, were also placed on CancerView Canada, an online resource for cancer control professionals in Canada 26. Links to online tools were provided, including a brief animated video that outlined the steps of undergoing a fecal test, and physicians were encouraged to recommend those resources to patients who might wish more information than could be shared in a typical office visit.
A more general public awareness program was also undertaken with the intention of reaching the general public (including physicians), to raise further awareness of screening and to enlist people in encouraging others to be screened. This program, titled Colonversation 27, was launched in a media campaign that informed, entertained, and encouraged people to start that “awkward conversation.” The introduction used a phased approach, and the later stages are just now being implemented. Finally, all tools and data were shared with the provincial programs, who were free to use them in the development of their own approaches to public and physician awareness.
3. DISCUSSION
The development of the nccsn provides an ideal platform both for the development of new knowledge tailored to program needs and for effecting the knowledge-to-action cycle as rapidly as possible. The network includes policymakers and implementation leaders from every province, and there is some territorial representation as well (all territories were invited to participate). The inclusion of other professional groups, and the appropriate engagement of specific experts and researchers as partners in relevant areas of the work, is designed to create a milieu for truly integrated kt. The two examples cited earlier were, in fact, priorities identified by the network members themselves, and there was thus some assurance that the results of the initiatives would be salient to their needs and more likely to be applied.
The quality determinants work was particularly relevant to a program that was just being inaugurated, because all participants were able to design their provincial data collection and quality assurance programs a priori to obtain the information that they collectively agreed would be relevant in measuring all key aspects of program function. To drive the work forward, it was conceded that although core knowledge (that is, the efficacy of crc screening) had already been developed, all programs were in the early stages of implementing that knowledge and that this situation, in and of itself, created knowledge gaps that would need to be addressed. If the final result were to be the development of a quality determinants document, then that tool have lacked the means for its use. The collection and sharing of program data was the essential step in moving the groups through the knowledge-to-action cycle. And, in fact, early data have been collected, reinforcing the willingness to collaborate and learn from one another.
It will be 2 or 3 years before roll-out of the programs is far enough advanced in some jurisdictions to allow for a robust interpretation of results. When that stage of maturity is reached, the programs will be able to use the shared program data to provide relevant context for individual program evaluations and to move further along the knowledge-to-action cycle. In the meantime, in other initiatives, cpac is working with the Canadian Association of Gastroenterologists—a group that is addressing the definition of key elements of colonoscopy quality. Their definition could be adopted both within programs and, more generally, in the endoscopy community across Canada.
It is difficult to assess the direct impact of the awareness campaigns, because the network and the programs are not the only groups active in generating increased awareness. We have been able to monitor increased activity on the Colonversation and publications sites of CancerView Canada after the distribution of physician resources, but the recency of that distribution makes it unlikely that the effect on screening uptake is currently measurable. However, there was excellent media uptake of early announcements, and the Colonversation site is one of the most frequently visited on CancerView Canada. The 2009 publication of the 2008 Canadian Community Health Survey data showed that, overall, screening uptake had improved before the campaign’s launch, most dramatically in the 2 provinces that implemented programs first in 2007 28. By 2008, the percentage of people 50–74 years of age who were up to date for crc testing was nearly 40% in Canada overall, and more than 50% in Manitoba and Ontario. Those results imply that as a nation, we are moving through the “diffusion of innovation” curve 29, and that our next messages need to be directed not to the early adopters, but to the majority of Canadians. As a result, informational needs are likely to change, and the network will be involved in helping to assess those needs. A second awareness survey planned for 2011 will provide an update on Canadian awareness and attitudes to crc screening and will be valuable in helping to assess the effects of this and other awareness campaigns, and in shaping future public outreach. In addition, the gaps in public understanding that may be identified in the new survey could be used to reshape awareness activities and further research. Finally, the new survey will allow for a comparison of uptake and attitudes between provinces whose strategies have focused largely on health care provider referral and those that have used direct mailing as a primary strategy.
In Canada, health care is largely a provincial and territorial responsibility (the federal government provides services for some specific populations, but the provincial screening programs include those groups in their population-based planning). The reasons for an apparent 5-year gap between the publication of national population-based guidelines 2 and the announcement of the first provincial program is a matter for speculation only. That being said, the role of cpac is to accelerate uptake, and the nccsn was designed to maximize the potential for that uptake.
When the network began, 3 programs had been announced, and none were yet implemented. Three years later, all 10 provinces and 1 territory had announced programs, and many of those are in implementation or pilot phases. Despite the gap in time from the publication of guidelines to the first program announcement, this roll-out trajectory has been quite rapid, and it occurred much more quickly than the similar roll-out of breast cancer screening programs in Canada.
As part of the work of the nccsn, a 3-year review was carried out with network members. They continued to identify the quality determinants work and data sharing as priorities for the ongoing shared work. The collection of program data will, in and of itself, serve as knowledge generation that will be critical to further program development and will ensure that such development will occur within the context of delivering quality programs most likely to result in reduction in mortality from crc in Canada.
4. ACKNOWLEDGMENTS
The authors acknowledge the support of Kaileah McKellar and Lindsay Orr–Van Abbema in network support and collection of program information, and the contribution of the members of the nccsn and its quality determinants committee. In addition, the work of the survey team (Angus Reid Public Opinion, a division of Vision Critical, and the Applied Health Research Centre, St. Michael’s Hospital, Toronto, ON) is gratefully acknowledged. This work was supported by the cpac.
Footnotes
5. CONFLICT OF INTEREST DISCLOSURES
All of the authors are affiliated with the nccsn, but have no financial conflicts of interest to disclose.
6. REFERENCES
- 1.Canadian Task Force on Preventive Health Care Colorectal cancer screening. Recommendation statement from the Canadian Task Force on Preventive Health Care. CMAJ. 2001;165:206–8. [PMC free article] [PubMed] [Google Scholar]
- 2.National Committee on Colorectal Cancer Screening . Ottawa, ON: Public Health Agency of Canada; 2002. Technical Report for the National Committee on Colorectal Cancer Screening [Web page] [Available online at: www.phac-aspc.gc.ca/publicat/ncccs-cndcc/; cited February 23, 2011] [Google Scholar]
- 3.Canadian Cancer Society, National Cancer Institute of Canada . Canadian Cancer Statistics 2006. Toronto, ON: Canadian Cancer Society; 2006. Progress in cancer control: screening; pp. 71–85. [Available online at: www.cancer.ca/canadawide/about%20cancer/cancer%20statistics/~/media/CCS/Canada%20wide/Files%20List/English%20files%20heading/pdf%20not%20in%20publications%20section/Canadian%20Cancer%20Statistics%20-%202006%20-%20EN%20-%20PDF_935505792.ashx; cited February 23, 2011] [Google Scholar]
- 4.Zarychanski R, Chen Y, Bernstein CN, Herbert PC. Frequency of colorectal screening and the impact of family physicians on screening behaviour. CMAJ. 2007;177:593–7. doi: 10.1503/cmaj.070558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGregor SE, Hilsden RJ, Li FX, Bryant HE, Murray A. Low uptake of colorectal cancer screening 3 yr after release of national recommendations for screening. Am J Gastorenterol. 2007;102:1727–35. doi: 10.1111/j.1572-0241.2007.01217.x. [DOI] [PubMed] [Google Scholar]
- 6.Ministry of Health and Long-Term Care (mhltc) Toronto, ON: MHLTC; 2007. McGuinty Government Launches First Colorectal Cancer Screening Program of Its Kind in Canada [press release] [Available online at: www.health.gov.on.ca/english/media/news_releases/archives/nr_07/jan/nr_012307.html; cited February 23, 2011] [Google Scholar]
- 7.Canadian Partnership Against Cancer (cpac) Toronto, ON: CPAC; 2010. Partnership Makes the Difference: Impact Report 2010. [Available online at: www.partnershipagainstcancer.ca/wp-content/uploads/FINAL-Impact-Report-ENG-for-web1.pdf; cited February 23, 2011] [Google Scholar]
- 8.Graham ID, Logan J, Harrison MB, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof. 2006;26:13–24. doi: 10.1002/chp.47. [DOI] [PubMed] [Google Scholar]
- 9.Graham ID, Tetroe J. How to translate health research knowledge into effective healthcare action. Healthc Q. 2007;10:20–2. doi: 10.12927/hcq..18919. [DOI] [PubMed] [Google Scholar]
- 10.Mandel JS, Bond JH, Church TR, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. N Engl J Med. 1993;328:1365–71. doi: 10.1056/NEJM199305133281901. [Erratum in: N Engl J Med 1993;329:672] [DOI] [PubMed] [Google Scholar]
- 11.Kewenter J, Brevinge H, Engaras B, Haglind E, Ahren C. Follow-up after screening for colorectal neoplasms with fecal occult blood testing in a controlled trial. Dis Colon Rectum. 1994;37:115–19. doi: 10.1007/BF02047531. [DOI] [PubMed] [Google Scholar]
- 12.Hardcastle JD, Chamberlain JO, Robinson MH, et al. Randomised controlled trial of faecal-occult-blood-screening for colorectal cancer. Lancet. 1996;348:1472–7. doi: 10.1016/S0140-6736(96)03386-7. [DOI] [PubMed] [Google Scholar]
- 13.Kronborg O, Fenger C, Olsen J, Jorgensen OD, Sondergaard O. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet. 1996;348:1467–71. doi: 10.1016/S0140-6736(96)03430-7. [DOI] [PubMed] [Google Scholar]
- 14.Mandel JS, Church TR, Ederer F, Bond JH. Colorectal cancer mortality: effectiveness of biennial screening for fecal occult blood. J Natl Cancer Inst. 1999;91:434–7. doi: 10.1093/jnci/91.5.434. [DOI] [PubMed] [Google Scholar]
- 15.Park DI, Ryu S, Kim YH, et al. Comparison of guaiac-based and quantitative immunochemical fecal occult blood testing in a population at average risk undergoing colorectal cancer screening. Am J Gastroenterol. 2010;105:2017–25. doi: 10.1038/ajg.2010.179. [DOI] [PubMed] [Google Scholar]
- 16.Duffy MJ, van Rossum LG, van Turenhout ST, et al. Use of faecal markers in screening for colorectal neoplasia: a European group on tumour markers position paper. Int J Cancer. 2011;128:3–11. doi: 10.1002/ijc.25654. [DOI] [PubMed] [Google Scholar]
- 17.Straus SE, Tetroe J, Graham I. Defining knowledge translation. CMAJ. 2009;181:165–8. doi: 10.1503/cmaj.081229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Atkin WS, Benson VS, Green J, et al. Improving colorectal cancer screening outcomes: proceedings of the second meeting of the International Colorectal Cancer Screening Network, a global quality initiative. J Med Screen. 2010;17:152–7. doi: 10.1258/jms.2010.010002. [DOI] [PubMed] [Google Scholar]
- 19.Canadian Partnership Against Cancer (cpac) Quality Determinants for Colorectal Cancer Screening in Canada. Toronto, ON: CPAC; 2009. [Available online at: www.partnershipagainstcancer.ca/wp-content/uploads/QD_for_CRC_Screening_in_Canada_2009-10-05_v16.pdf; cited February 23, 2011] [Google Scholar]
- 20.McGregor SE, Hilsden RJ, Murray A, Bryant HE. Colorectal cancer screening: practices and opinions of primary care physicians. Prev Med. 2004;39:279–85. doi: 10.1016/j.ypmed.2004.03.037. [DOI] [PubMed] [Google Scholar]
- 21.Hilsden RJ, McGregor E, Murray A, Khoja S, Bryant H. Colorectal cancer screening practices and attitudes of gastroenterologist, internists, and surgeons. Can J Surg. 2006;48:434–40. [PMC free article] [PubMed] [Google Scholar]
- 22.Klabunde CN, Vernon SW, Nadel MR, Breen N, Seeff L, Brown ML. Barriers to colorectal screening: a comparison of reports from primary care physicians and average risk adults. Med Care. 2005;43:939–44. doi: 10.1097/01.mlr.0000173599.67470.ba. [DOI] [PubMed] [Google Scholar]
- 23.Canadian Partnership Against Cancer (cpac) Cancer Control Spotlight: Colorectal Cancer Screening. Toronto, ON: CPAC; 2010. [Available online at: www.cancerview.ca/idc/groups/public/documents/webcontent/rl_cancer_1crcscreen.pdf; cited February 23, 2011] [Google Scholar]
- 24.Bryant H, McGregor SE. Perception versus reality: overcoming barriers to colorectal cancer screening. Can Fam Physician. 2008;54:495–7. [PMC free article] [PubMed] [Google Scholar]
- 25.Canadian Partnership Against Cancer (cpac) Cancer Control Snapshot: Colorectal Cancer Screening in Canada. Toronto, ON: CPAC; 2010. [Available online at: www.cancerview.ca/idc/groups/public/documents/webcontent/rl_crc_snapshot_one_en.pdf; cited February 23, 2011] [Google Scholar]
- 26.CancerViewCanada . Toronto, ON: CancerViewCanada; CancerView Canada link [Web page] n.d. [Available online at: www.cancerview.ca/portal/server.pt/community/home/448; cited February 23, 2011] [Google Scholar]
- 27.CancerViewCanada . Toronto, ON: CancerViewCanada; Colonversation home page [Web page] n.d. [Available online at: www.cancerview.ca/portal/server.pt/community/colonversation/492/colonversation; cited February 23, 2011] [Google Scholar]
- 28.Wilkins K, Shields M. Colorectal cancer testing in Canada—2008. Health Rep. 2009;20:21–30. [PubMed] [Google Scholar]
- 29.Green LW, Ottoson JM, Garcia C, Hiatt RA. Diffusion theory and knowledge dissemination, utilization, and integration in public health. Annu Rev Public Health. 2009;30:151–74. doi: 10.1146/annurev.publhealth.031308.100049. [DOI] [PubMed] [Google Scholar]