Abstract
Objective
Test the hypothesis that reductions in thin-ideal internalization and body dissatisfaction mediate the effects of a dissonance-based eating disorder prevention program on reductions in eating disorder symptoms over 1-year follow-up.
Method
Data were drawn from a randomized effectiveness trial in which 306 female high school students (M age = 15.7 SD = 1.1) with body image concerns were randomized to the 4-session dissonance-based prevention program or an educational brochure control condition, wherein school counselors and nurses were responsible for participant recruitment and intervention delivery.
Results
Dissonance participants showed greater reductions in thin-ideal internalization, body dissatisfaction, and eating disorder symptoms; change in thin-ideal internalization predicted change in body dissatisfaction and symptoms; change in body dissatisfaction predicted change in symptoms; and all indirect effects were significant. Change in thin-ideal internalization fully mediated the effects of intervention condition on change in body dissatisfaction and partially mediated the effects on symptoms; change in body dissatisfaction partially mediated the effect of intervention condition on change in symptoms.
Conclusions
Findings provided support for the intervention theory of this eating disorder prevention program over longer-term follow-up, extending the evidence base for this effective intervention.
Keywords: eating disorders, body dissatisfaction, prevention, mediation
Because eating disorders are marked by functional impairment and increased risk for numerous health problems (Stice, Marti, Shaw, & Jaconis, 2009a; Wilson, Becker, & Heffernan, 2003), it is vital to develop effective prevention programs. Marked support has emerged for a dissonance-based eating disorder prevention program, wherein young women critique the thin-ideal espoused for women, which theoretically produces cognitive dissonance that causes participants to reduce thin-ideal internalization. Reduced thin-ideal internalization in turn putatively reduces body dissatisfaction, weight control efforts, and negative affect, thereby reducing eating disorder symptoms. Efficacy trials show that this intervention has reduced eating disorder risk factors (thin-ideal internalization, body dissatisfaction, and negative affect), eating disorder symptoms, and risk for future onset of eating disorders relative to alternative interventions and assessment-only controls, with some effects persisting for 3-years (Becker, Smith, & Ciao, 2006; Mitchell, Mazzeo, Rausch, & Cooke, 2007; Parez, Becker, & Ramirez, 2010; Stice, Marti, Spoor, Presnell, & Shaw, 2008; Stice, Shaw, Burton, & Wade, 2006).
To date, only one controlled trial has tested the meditational processes hypothesized to produce intervention effects, which is important for testing the intervention theory of prevention programs. Stice, Presnell, Gau, and Shaw (2007) found that relative to an expressive writing control condition, the dissonance intervention produced greater reductions in thin ideal internalization as well as greater reductions in body dissatisfaction, self-reported dieting, negative affect, and eating disorder symptoms, that change in thin-ideal internalization correlated with change in the other outcomes, that intervention effects became weaker when change in thin-ideal internalization was controlled, and that dissonance participants were more likely to show meaningful change (.5 SD) in thin-ideal internalization before they showed an equivalent degree of change in the other outcomes. The fact that change in thin-ideal internalization partially mediated the effects of this intervention on change in eating disorder symptoms prompted Stice et al (2007) to suggest that body dissatisfaction may also play a role in mediating the effects of the intervention on symptom reduction. An uncontrolled trial provided evidence that changes in both thin-ideal internalization and body dissatisfaction partially mediated the effects of this intervention on reductions in eating disorder symptoms (Seidel, Presnell, & Rosenfield, 2009).
Although these two studies provided support for the meditational model for this prevention program, both focused on change during the intervention delivery phase. As the dissonance intervention produces effects on outcomes that persist over multiple years, it seems important to test whether change in the hypothesized mediators accounts for longer-term intervention effects. Thus, we tested whether reductions in thin-ideal internalization and body dissatisfaction mediated the effects of the dissonance prevention program on change in eating disorder symptoms through 1-year follow-up. Another unique aspect of the present report is that data were drawn from an effectiveness trial rather than an efficacy trial, which test whether interventions produce effects when delivered by endogenous providers (e.g., school counselors) who are not closely supervised under real world conditions with heterogeneous populations. The current trial found that when high school counselors and nurses recruited students and delivered the intervention, it produced significantly greater reductions in thin-ideal internalization, body dissatisfaction, dieting, and eating disorder symptoms, but not negative affect, through 1-year follow-up relative to educational brochure controls (Stice, Rohde, Gau, & Shaw, 2009b). The present meditational model posits that the intervention reduces thin-ideal internalization that results in improved body dissatisfaction and consequent reduction in eating disorder symptoms. Thus, we tested whether change in thin-ideal internalization partially mediates the effects of the intervention on change in body dissatisfaction and eating disorder symptoms and whether change in body dissatisfaction partially mediates the effects of the intervention on change in symptoms.
Methods
Participants were 306 adolescent girls (M age = 15.7, SD = 1.1) recruited from high schools via direct mailings, flyers, and leaflets inviting females with body image concerns to participate in a trial evaluating body acceptance interventions. The sample was 2% Asian, 2% Black, 9% Hispanic, 81% Caucasian, and 6% who specified other/mixed racial heritage, which was somewhat less ethnically diverse than the US (5% Asian, 13% Black, 80% Caucasian, 16% Hispanic). Informed written consent was obtained from participants and parents. Potential participants had to affirm that they had body image concerns during a phone screening. The sole exclusion criterion was that participants could not meet criteria for DSM-IV anorexia nervosa, bulimia nervosa, or binge eating disorder at pretest. Participants were randomized to the dissonance intervention (n = 139) or a psychoeducational brochure control condition (n = 167) via coin toss. The dissonance intervention consisted of 4 weekly 1-hour group sessions with 6-10 participants, typically co-facilitated by two school nurses or counselors. A scripted manual was used for the dissonance intervention. Details regarding research ethics approval, participant flow, session content, the educational brochures, facilitator training and supervision, and fidelity and competence ratings are provided elsewhere (Stice et al., 2009b).
Participants provided interview and survey data at pretest, posttest, 6-month follow-up, and 1-year follow-up. Female assessors, blinded to the condition of participants, attended 24 hours of training and annual training workshops. They had to demonstrate high inter-rater agreement (kappa [k] > .80) with supervisors using tape-recorded interviews before collecting data. Weekly consensus meetings were held to resolve diagnostic questions. Participants received $15 for completing each assessment, which were usually conducted at schools.
The Ideal-Body Stereotype Scale-Revised assessed thin-ideal internalization (Stice et al., 2006). This scale has shown internal consistency (α = .91), test-retest reliability (r = .80), predictive validity for bulimic symptom onset, and sensitivity to detecting intervention effects (Stice et al., 2006; α = .78 at T1). Items from the Satisfaction and Dissatisfaction with Body Parts Scale (Berscheid, Walster, & Bohrnstedt, 1973) assessed dissatisfaction with nine body parts that are often of concern to females. This scale has shown internal consistency (α = .94), 3-week test-retest reliability (r = .90), predictive validity for bulimic symptom onset, and sensitivity to detecting intervention effects (Stice et al., 2006; α = .91 at T1). The Eating Disorder Diagnostic Interview assessed DSM-IV eating disorder symptoms. Items assessing the symptoms in the past month were summed to form an overall eating disorder symptom composite for each assessment. A log base10 transformation was used to normalize this variable. This scale has shown internal consistency (α = .92), 1-week test-retest reliability (r = .90), sensitivity to detecting intervention effects, and predictive validity for future onset of depression in past studies (Stice et al., 2006). In the current trial this scale showed internal consistency (α = .84 at T1), inter-rater agreement (ICC r = .93), and test-retest reliability (ICC r = .95).
Latent growth curve (LCG) modeling was used to test the meditational hypotheses. LCG models have been employed in a mediation framework by modeling parallel change in mediator and outcome variables and with an independent variable that represents intervention condition (MacKinnon, 2008). Mediation is assessed as the indirect path from the intervention condition to the mediator growth factor to the outcome growth factor. All models were implemented using the Mplus (Muthén & Muthén, 2010) based on direct maximum likelihood estimation using all available data. We tested whether (1) the initial variable (i.e., dissonance intervention relative to brochure control) predicts the outcome (i.e., eating disorder symptoms; path c), (2) the initial variable predicts the mediator (either thin ideal internalization or body dissatisfaction; path a), (3) change in the mediator predicts change in the outcome (path b), and (4) the relation the initial variable and the outcome is zero when the mediator is included in the model (path c′) for full mediation and significantly reduced for partial mediation. Paths a, b, and c′, are estimated in a single model (see Fig. 1). We directly tested the indirect effect from the independent variable to the dependent variable through the mediator using bias corrected bootstrap estimates, which tests the null hypothesis that the relation between the independent and dependent variables is not dependent on the mediator (i.e., that the product of the a and b paths is 0).
Fig 1.
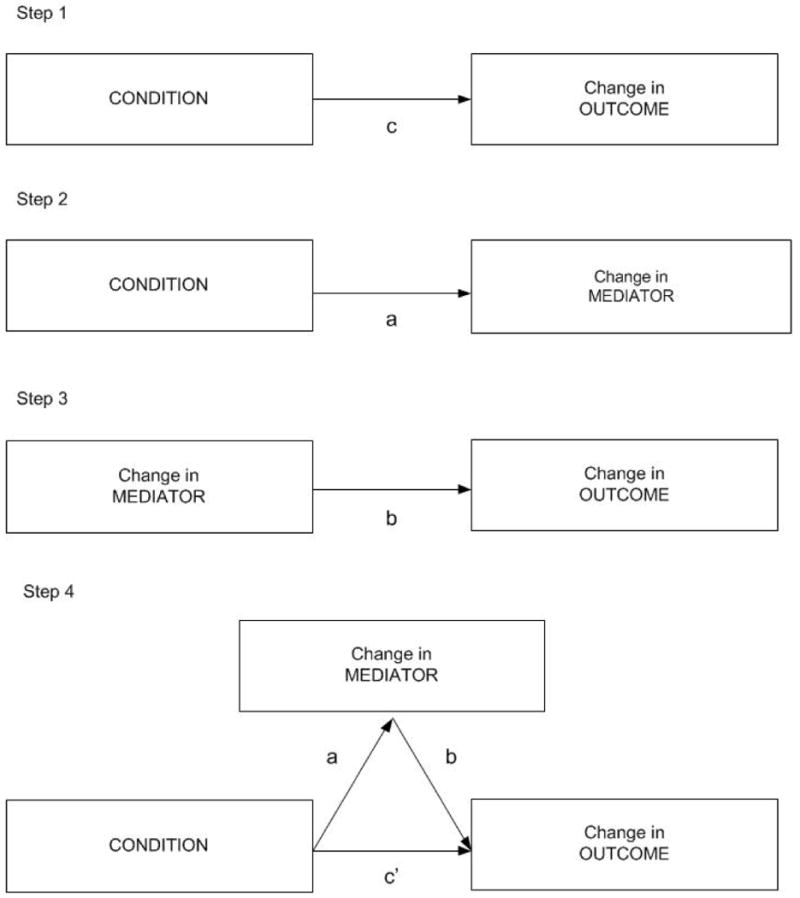
Schematic illustrating the criteria for testing mediation used in the present report.
We first examined group differences in variables at baseline to assess group equivalence and tested for univariate and multivariate normality. Next, the shapes of the growth patterns were examined to determine the best model of change. We considered models of static, linear, and quadratic change. The growth models were comprised of two factors that represent initial status and growth rate. Mediation in the growth models was assessed following MacKinnon (2008): after constructing the growth models, the growth factor of the mediator was regressed on initial status of the outcome and intervention condition. The condition coefficient in this equation represents the a path in the Baron and Kenny (1986) path model of mediation. The growth factor of the outcome was also regressed on the initial status of the mediator, the slope of the mediator, and condition. The coefficient for the slope of the mediator represents the b path in the Baron and Kenny (1986) path model, controlling for the effect of condition. Models controlled for baseline levels of variables that differed significantly across groups.
Results
Table 1 presents descriptive statistics for the mediators and outcome. As the variables failed to demonstrate multivariate normality using the Doornik-Hansen test (χ2 (24) = 150.52, p < .001), we used bias corrected bootstrapping to assess the statistical significance. Table 2 presents the mediators and outcome by intervention group and shows that there were significant differences between groups at baseline for thin-ideal internalization and body dissatisfaction. Thus, we controlled for baseline differences in these factors. Each variable showed a significant reduction from pretest to posttest that persisted for the duration of the follow-up, suggesting quadratic change over time. Thus, we set the factor loadings of the growth factor as [0 1 1 1], corresponding to baseline, posttest, 6-month follow-up, and 1-year follow-up, to reflect the non-linear change. Tucker-Lewis Index (TLI > .90), Confirmatory Fit Index (CFI > .90), and Root Mean Square Error of Approximation (RMSEA) (< .08) were used to assess model fit. When models did not show acceptable model fit, we examined modification indices to identify theoretically viable constraints to the models.1
Table 1.
Descriptive statistics for the original and transformed versions of the variables.
| Variable | Original variables | Log transformed variables | ||||
|---|---|---|---|---|---|---|
| Mean(SD) | Skewness | Kurtosis | Mean(SD) | Skewness | Kurtosis | |
| Baseline Thin-ideal internalization | 3.44 (0.53) | -0.81 | 2.01 | 1.22 (0.18) | -2.04 | 8.87 |
| 1 Month Post Thin-ideal internalization | 3.15 (0.63) | -0.90 | 0.73 | 1.12 (0.24) | -1.74 | 4.02 |
| 6 Months Post Thin-ideal internalization | 3.26 (0.58) | -0.94 | 1.34 | 1.16 (0.21) | -1.88 | 5.29 |
| 12 Months Post Thin-ideal internalization | 3.25 (0.59) | -0.78 | 1.67 | 1.16 (0.21) | -1.99 | 7.05 |
| Baseline Body dissatisfaction | 3.29 (0.81) | -0.14 | -0.06 | 1.16 (0.28) | -1.11 | 2.12 |
| 1 Month Post Body dissatisfaction | 3.06 (0.78) | 0.08 | 0.06 | 1.08 (0.28) | -0.86 | 1.36 |
| 6 Months Post Body dissatisfaction | 3.07 (0.75) | -0.09 | 0.20 | 1.09 (0.27) | -1.10 | 2.27 |
| 12 Months Post Body dissatisfaction | 3.06 (0.73) | 0.14 | 0.41 | 1.09 (0.26) | -0.86 | 1.75 |
| Baseline Eating pathology | 10.09 (11.94) | 2.73 | 8.94 | 1.83 (0.98) | 0.17 | -0.34 |
| 1 Month Post Eating pathology | 5.70 (7.18) | 3.68 | 19.46 | 1.28 (0.96) | 0.28 | -0.58 |
| 6 Months Post Eating pathology | 6.21 (8.86) | 4.34 | 28.79 | 1.31 (0.96) | 0.56 | -0.13 |
| 12 Months Post Eating pathology | 5.83 (7.20) | 3.18 | 12.38 | 1.32 (0.89) | 0.50 | -0.05 |
Table 2.
Descriptive statistics for control and intervention groups and mean differences.
| Variable | Control | Intervention | ||||||
|---|---|---|---|---|---|---|---|---|
| N | Mean | Standard Deviation | N | Mean | Standard Deviation | Significance* | Mean Difference | |
| Wave 1 TII | 169 | 3.51 | 0.46 | 135 | 3.35 | 0.59 | * | -0.15 |
| Wave 2 TII | 167 | 3.34 | 0.52 | 130 | 2.91 | 0.68 | *** | -0.44 |
| Wave 3 TII | 161 | 3.33 | 0.50 | 122 | 3.15 | 0.65 | ** | -0.18 |
| Wave 4 TII | 154 | 3.35 | 0.57 | 125 | 3.13 | 0.58 | ** | -0.21 |
| Wave 1 BD | 170 | 3.16 | 0.78 | 135 | 3.47 | 0.83 | *** | 0.31 |
| Wave 2 BD | 167 | 3.09 | 0.74 | 128 | 3.03 | 0.84 | -0.06 | |
| Wave 3 BD | 160 | 3.00 | 0.74 | 121 | 3.15 | 0.76 | 0.16 | |
| Wave 4 BD | 154 | 2.99 | 0.73 | 125 | 3.14 | 0.73 | 0.15 | |
| Wave 1 EDS | 171 | 1.74 | 0.95 | 135 | 1.94 | 1.02 | 0.19 | |
| Wave 2 EDS | 171 | 1.40 | 0.92 | 135 | 1.14 | 0.98 | * | -0.26 |
| Wave 3 EDS | 161 | 1.32 | 0.96 | 124 | 1.29 | 0.97 | -0.03 | |
| Wave 4 EDS | 157 | 1.39 | 0.87 | 125 | 1.24 | 0.92 | -0.15 | |
p < .05,
p < .01,
p < .001
Note: TII = thin-ideal internalization, BD = body dissatisfaction, EDS = eating disorder symptoms.
Model 1 tested whether change in thin-ideal internalization mediated the effects of the intervention on change in body dissatisfaction. This model (Fig. 2) showed an acceptable fit (TLI = .94; CFI = .96; RMSEA = .078). Condition significantly predicted the thin-ideal internalization growth factor (-0.14, 95% CI = -0.24, -0.05, standardized = -.28), indicating that dissonance participants showed greater reductions in thin-ideal internalization than controls (path a). The thin-ideal internalization growth factor correlated significantly with the body dissatisfaction growth factor (0.57, 95% CI = 0.37, 0.79, standardized = .33), indicating that greater reductions in thin-ideal internalization were associated with greater reductions in body dissatisfaction (path b). The direct effect of intervention condition on growth in body dissatisfaction was significant (-0.19, 95% CI = -0.30, -0.09, standardized = -.40) (path c). The direct path from intervention condition to growth iin body dissatisfaction was not significant (-0.02, 95% CI = -0.15, 0.10, standardized = -.03) (path c′) when controlling for change in thin-ideal internalization, in contrast to the c path, suggesting full mediation. The indirect path from intervention condition to growth in thin-ideal internalization to growth in body dissatisfaction was significant (-0.08, 95% CI = -0.16, -0.03, standardized = -.18), implying that larger decrease body dissatisfaction for intervention participants was mediated by reductions in thin-ideal internalization.
Fig 2.
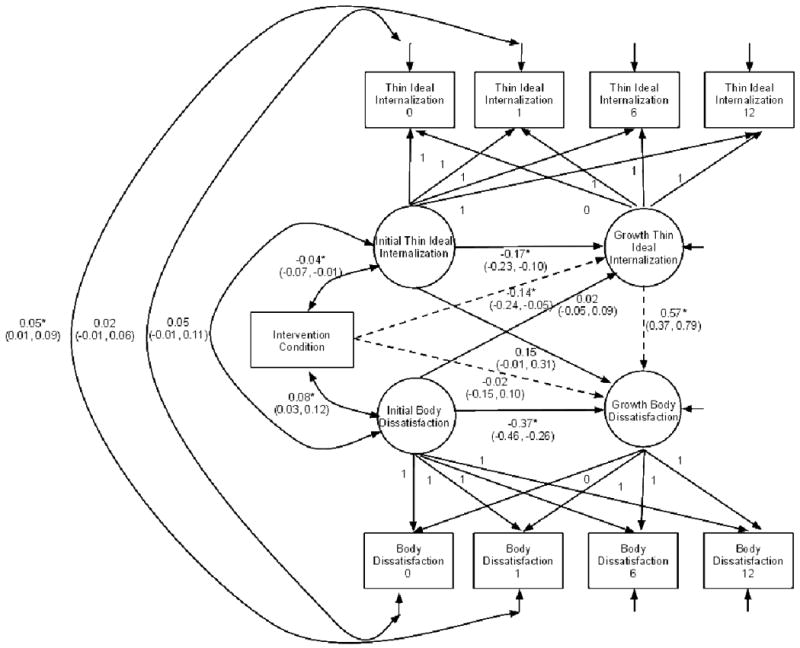
Latent growth curve model testing whether change in thin-ideal internalization mediates relation between intervention condition and change in body dissatisfaction.
Model 2 tested whether change in thin-ideal internalization mediated the effects of intervention condition on change in eating disorder symptoms. This model (Fig. 3) showed an acceptable fit (TLI =.94; CFI = .96; RMSEA = .074). Condition significantly predicted growth in thin-ideal internalization (-0.14, 95% CI = -0.24, -0.04, standardized = -.26) (path a). The thin-ideal internalization growth factor correlated significantly with the eating disorder symptoms growth factor (0.64, 95% CI = 0.19, 1.19, standardized = .53), indicating that greater reductions in the former variable correlated with greater reductions in the latter variable (path b). The direct effect of intervention condition on growth in eating disorder symptom was significant (-0.32, 95% CI = -0.48, -0.16, standardized = -.39) (path c). The direct path from intervention condition to growth iin eating disorder symptom remained significant (-0.29, 95% CI = -0.49, -0.08, standardized = -.44) (path c′) when controlling for growth in thin-ideal internalization. The indirect path from intervention condition to thin-ideal internalization to eating disorder symptoms was significant (-0.09, 95% CI = -0.11, -0.02, standardized = -.14, suggesting that larger decreases in symptoms for intervention participants was mediated by reductions in thin-ideal internalization.
Fig 3.
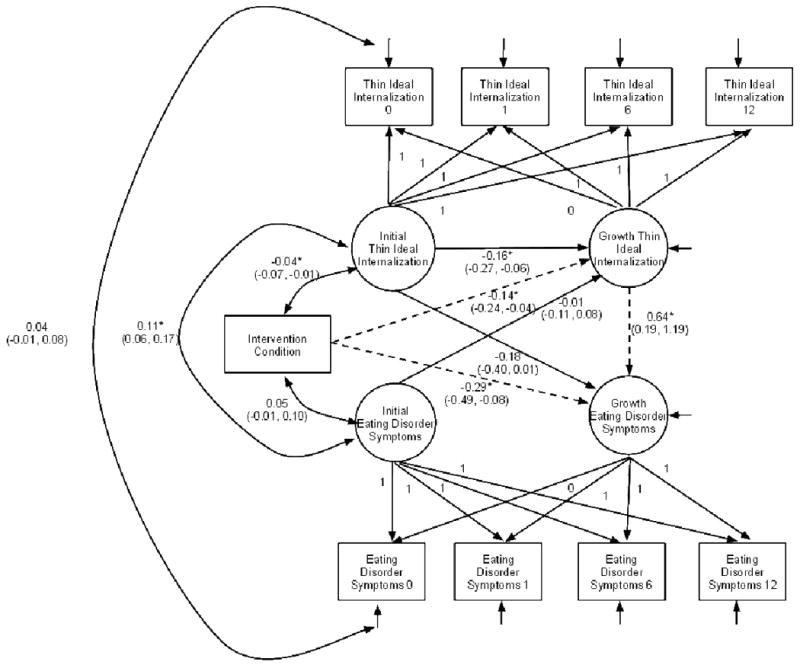
Latent growth curve model testing whether change in thin-ideal internalization mediates relation between intervention condition and change in eating disorder symptoms.
Model 3 tested whether change in body dissatisfaction mediated the effects of intervention condition on change in eating disorder symptoms. This model (Fig. 4) showed an acceptable fit (TLI =.97; CFI = .97; RMSEA = .067). Intervention condition significantly predicted growth in body dissatisfaction (-0.13, 95% CI = -0.23, -0.03, standardized = -.16), indicating that the intervention group showed greater reductions in body dissatisfaction (path a). The body dissatisfaction growth factor correlated significantly with the eating disorder symptoms growth factor (0.88, 95% CI = 0.66, 1.10, standardized = .84), indicating that reductions in the former correlated with reductions in the latter (path b). The direct effect of intervention condition on growth in eating disorder symptom was significant (-0.32, 95% CI = -0.48, -0.16, standardized = -.39) (path c). The direct path from intervention condition to growth in eating disorder symptoms was non-significant (-0.10, 95% CI = -0.29, -0.07, standardized = -.12) (path c′) controlling for growth in body dissatisfaction, indicating full mediation. The indirect path from intervention condition to body dissatisfaction to eating disorder symptoms was significant (-0.11, 95% CI = -0.21, -0.03, standardized = -.11), suggesting that larger decreases in symptoms for intervention participants was mediated by reductions in body dissatisfaction.
Fig 4.
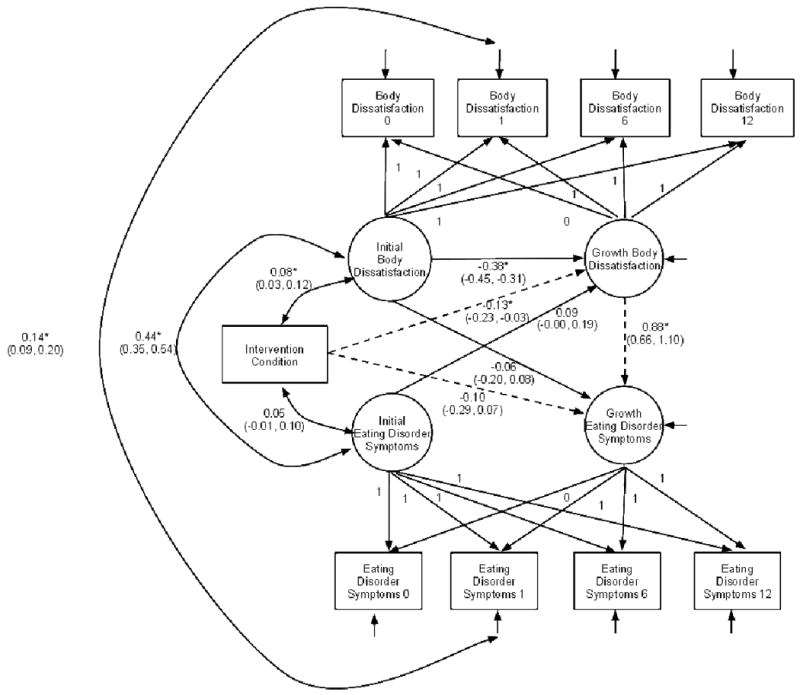
Latent growth curve model testing whether change in body dissatisfaction mediates relation between intervention condition and change in eating disorder symptoms.
Discussion
Results are consistent with the hypothesis that the dissonance intervention decreases eating disorder symptoms via reductions in thin-ideal internalization and body dissatisfaction; intervention condition predicted reductions in the thin-ideal internalization and body dissatisfaction, as well as eating disorder symptoms, change in both thin-ideal internalization and body dissatisfaction correlated with changes in eating disorder symptoms, intervention effects became significantly weaker when changes in the mediators was statistically controlled, and the indirect effects from intervention condition to change in the mediators to change in the outcome were significant. The direct effects were medium in magnitude and the indirect effects were small in magnitude. Results dovetail with findings from previous controlled (Stice et al., 2007) and uncontrolled (Seidel et al., 2009) trials that tested the meditational processes theorized to account for the effects of this prevention program during intervention delivery, suggesting results are generalizable. The current findings extend the results from these two past studies in that they provide evidence that change in thin-ideal internalization and body dissatisfaction mediates the effects of the intervention on long-term change in eating disorder symptoms.
Theoretically, voluntarily arguing against the thin-ideal results in cognitive dissonance that motivates participants to reduce their subscription to this unrealistic ideal, which results in improved body satisfaction, and consequent reductions in eating disorder symptoms. In support of this notion, participants assigned to high-dissonance versions of this intervention showed greater reductions in eating disorder symptoms than participants assigned to low-dissonance versions of this intervention (McMillan, Stice, & Rohde, in press). Collectively, these findings provide compelling support for the intervention theory for this prevention program.
Results suggested that change in thin-ideal internalization fully mediated the effect of the intervention on change in body dissatisfaction and that change in body dissatisfaction fully mediated the effect of the intervention on change in eating disorder symptoms, but that change in thin-ideal internalization only partially mediated the effect of intervention condition on change in eating disorder symptoms. This is of note because the two past trials also found that change in thin-ideal internalization only partially mediated the effects of the intervention effects on change in eating disorder symptoms (Seidel et al., 2009; Stice et al., 2007). The collective pattern of findings may suggest that change in both thin-ideal internalization and body dissatisfaction mediate the effects of the intervention on change in eating disorder symptoms. Although we attempted to directly estimate a dual mediation model, which included change in both thin-ideal internalization and body dissatisfaction, it failed to converge, apparently because of insufficient statistical power.2 However, an alternative explanation for the finding that change in thin-ideal internalization only partially mediated the effects of the intervention on change in eating disorder symptoms is that change in the outcome may lead to changes in the mediator (Seidel et al., 2009). Support for this notion of mutual influence between mediators and outcomes emerged in the uncontrolled trial conducted by Seidel et al. (2009). Post hoc analyses provided support for this reverse mediation model, suggesting that a reduction in eating disorder symptoms may lead to decreased thin-ideal internalization.3 In this context it is important to note that this test of mediation does not always provide support for the intervention theory (Stice et al., 2007).
With regard to study limitations, although our former mediation analysis directly tested whether change in thin-ideal internalization typically occurred before change in the outcomes (Stice et al., 2007), we were not able to address this question in the present study because it would have required more frequent assessments to accurately model the timing of change in the mediator relative to the outcomes. Further, the non-linear change in the outcomes over the longer follow-up period made it impossible to apply the procedure we developed to test whether change in the mediator typically occurs before parallel changes in the outcome (Stice et al., 2007). Second, the fact that we recruited participants for a trial of interventions designed to reduce body dissatisfaction may have biased the findings because body dissatisfaction was hypothesized to mediate intervention effects. Yet because this applies to participants in both conditions, it may not have influenced our test of differential effects across conditions. Third, as noted, we were underpowered to estimate the more complex dual mediation model, which would have provided a more comprehensive test of the hypothesized meditational processes.
Acknowledgments
This study was supported by a grant (MH70699) from the National Institutes of Health.
We thank project research assistants Cara Bohon, Krista Heim, Erica Marchand, and Janet Ng, Julie Pope, Alex Stanton, our undergraduate volunteers, the Eugene, Springfield, and Bethel School Districts, the school staff who recruited participants and facilitated the groups, and the participants who made this study possible.
Footnotes
In model 1, we allowed the baseline and posttest thin-ideal internalization and eating disorder symptom residuals to covary and allowed the posttest thin-ideal internalization intercept to be freely estimated. In model 2, we allowed the posttest thin-ideal internalization and eating disorder symptoms residuals to covary and allowed the posttest thin-ideal internalization intercept to be freely estimated. In model 3, we allowed the posttest body dissatisfaction and eating disorder symptoms residuals to covary.
There are several causes of model non-convergence, including negative variance, negative residuals, correlations greater than one, and linear dependencies between variables (Muthén & Muthén, 2010). Our sample was sufficiently powered for modeling two growth factors, but more complex models were dubious based on simulation work with a comparable number of parameters (2 factors, 10 observed variables, and 31 free parameters) that found that a sample size of 315 was required to achieve power of .80 for models with non-normal and missing data (Muthén & Muthén, 2002). Thus, it appears that we did not have sufficient power to estimate the more complex dual mediation model.
We tested a model in which eating disorder symptoms mediated the effects of the intervention on change in thin-ideal internalization. This model exhibited an acceptable fit (TLI = .94, CFI = .96, and RMSEA =.074). Path a, the eating disorder symptoms growth factor regressed on condition was significant (-0.38, 95% CI = -0.51, -0.21, standardized = -.38). Path b, the thin ideal internalization growth factor regressed on the eating disorder symptoms growth factor was significant (0.63, 95% CI = 0.44, 0.88, standardized = .63). Path c, the direct effect of intervention condition on the thin ideal internalization growth factor, was significant (-0.14, 95% CI = -0.22, -0.06, standardized = -.27). Path c′, the direct path from intervention condition to the thin ideal internalization growth factor when controlling for change in eating disorder symptoms was not significant (0.08, 95% CI = -0.05, 0.24, standardized = .08). The indirect path from intervention condition to the eating disorder symptoms growth factor to the in thin-ideal internalization growth factor was significant (-0.24, 95% CI = -0.40, -0.14, standardized = -.39).
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
Contributor Information
Eric Stice, Oregon Research Institute.
C. Nathan Marti, University of Texas at Austin.
Paul Rohde, Oregon Research Institute.
Heather Shaw, Oregon Research Institute.
References
- Becker CB, Smith LM, Ciao AC. Peer facilitated eating disorders prevention: A randomized effectiveness trial of cognitive dissonance and media advocacy. Journal of Counseling Psychology. 2006;53:550–555. [Google Scholar]
- Berscheid E, Walster E, Bohrnstedt G. The happy American body: A survey report. Psychology Today. 1973;7:119–131. [Google Scholar]
- MacKinnon DP. Multivariate Applications: Introduction to Statistical Mediation Analysis. New York: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- McMillan W, Stice E, Rohde P. High- and low-level dissonance-based eating disorder prevention programs with young women with body image concerns: An experimental trial. Journal of Consulting and Clinical Psychology. doi: 10.1037/a0022143. in press. [DOI] [PubMed] [Google Scholar]
- Mitchell KS, Mazzeo SE, Rausch SM, Cooke KL. Innovative interventions for disordered eating: Evaluating dissonance-based and yoga interventions. International Journal of Eating Disorders. 2007;40:120–128. doi: 10.1002/eat.20282. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide. 6th. Los Angeles: Muthén & Muthén; 2010. [Google Scholar]
- Muthén LK, Muthén BO. How to use a Monte Carlo study to decide on sample size and determine power. Structural Equation Modeling. 2002;9(4):599–620. [Google Scholar]
- Perez M, Becker CB, Ramirez A. Transportability of an empirically supported dissonance-based prevention program for eating disorders. Body Image. 2010;7:179–186. doi: 10.1016/j.bodyim.2010.02.006. [DOI] [PubMed] [Google Scholar]
- Seidel A, Presnell K, Rosenfield D. Mediators in the dissonance eating disorder prevention program. Behaviour Research and Therapy. 2009;47:645–653. doi: 10.1016/j.brat.2009.04.007. [DOI] [PubMed] [Google Scholar]
- Stice E, Marti CN, Shaw H, Jaconis M. An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. Journal of Abnormal Psychology. 2009;118:587–597. doi: 10.1037/a0016481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti N, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: Long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76:329–340. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Presnell K, Gau J, Shaw H. Testing mediators of intervention effects in randomized controlled trials: An evaluation of two eating disorder prevention programs. Journal of Consulting and Clinical Psychology. 2007;75:20–32. doi: 10.1037/0022-006X.75.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau J, Shaw H. An effectiveness trial of a dissonance-based eating disorder prevention program for high-risk adolescent girls. Journal of Consulting and Clinical Psychology. 2009;77:825–834. doi: 10.1037/a0016132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: A randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2006;74:263–275. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson GT, Becker CB, Heffernan K. Eating Disorders. In: Mash EJ, Barkley RA, editors. Child Psychopathology. 2nd. New York: Guilford; 2003. pp. 687–715. [Google Scholar]


