Abstract
Objective
Depression is associated with poor social problem-solving, and psychotherapies that focus on problem-solving skills are efficacious in treating depression. We examined the associations between treatment, social problem solving, and depression in a randomized clinical trial testing the efficacy of psychotherapy augmentation for chronically depressed patients who failed to fully respond to an initial trial of pharmacotherapy (Kocsis et al., 2009).
Method
Participants with chronic depression (n = 491) received Cognitive Behavioral Analysis System of Psychotherapy (CBASP), which emphasizes interpersonal problem-solving, plus medication; Brief Supportive Psychotherapy (BSP) plus medication; or medication alone for 12 weeks.
Results
CBASP plus pharmacotherapy was associated with significantly greater improvement in social problem solving than BSP plus pharmacotherapy, and a trend for greater improvement in problem solving than pharmacotherapy alone. In addition, change in social problem solving predicted subsequent change in depressive symptoms over time. However, the magnitude of the associations between changes in social problem solving and subsequent depressive symptoms did not differ across treatment conditions.
Conclusions
It does not appear that improved social problem solving is a mechanism that uniquely distinguishes CBASP from other treatment approaches.
Keywords: depression, social problem solving, psychotherapy, chronic
Numerous studies have documented associations between social problem solving and depressive disorders and symptoms. Depressed individuals often exhibit a negative orientation toward problems in living (e.g., appraising a problem as a threat, doubting one’s own problem-solving ability) and deficits in specific problem-solving skills on self-report inventories and performance-based measures (Dixon et al., 1993; Haaga et al., 1995; Kant et al., 1997; Marx et al., 1992; Nezu et al., 1986; Reinecke et al., 2001).
Hypothesizing that ineffective problem solving plays a role in the etiology and maintenance of depression, several investigators have developed treatments for depression that specifically target social problem solving (D’Zurilla & Nezu, 2007; Mynors-Wallis et al., 1995). The efficacy of social problem-solving therapies has been examined in several dozen clinical trials, generally with favorable results (e.g., Areán, et al., 2010; Barrett et al., 2001; Mynors-Wallis et al., 1995, 2000; Nezu, 1986; Nezu & Perri, 1989; Williams et al., 2000). In two recent meta-analyses, social problem-solving therapies for depression had a moderate effect size (Bell & D’Zurilla, 2009; Cuipers et al., 2007).
The presumptive mechanism through which problem-solving therapies alleviate depression involves their effects on social problem solving. Indeed, several studies have reported that problem-solving therapies produce greater change in social problem solving than comparator treatments and being on a wait-list (Alexopoulos et al., 2003; Nezu, 1986; Nezu et al., 1989; Nezu et al., 2003; Sahler et al., 2002; also see Areán et al. [1993], who found no significant treatment condition by time interaction, but reported that only problem-solving therapy was associated with significant gains in social problem solving ). Three of these studies also attempted to test mediation more explicitly. In a sample of distressed cancer patients, Nezu et al. (2003) reported that change in social problem solving correlated with change in symptoms. In geriatric patients with major depressive disorder (MDD) and deficits in executive functioning, Alexopoulos et al. (2003) found a significant interaction between the effects of treatment condition and improvement in social problem solving on change in depression, which they interpreted as evidence of mediation. Finally, using path models in a sample of mothers of children with recently diagnosed cancer, Sahler et al. (2002) reported that change in social problem solving partially mediated the association between problem-solving skills training and change in negative affect. Unfortunately, in all of these studies data on social problem solving and symptoms were only available at pre- and post-intervention. Hence, it was not possible to determine whether change in social problem solving preceded, followed, or occurred contemporaneously with change in symptoms. Thus, although the extant literature suggests that social problem solving may mediate the antidepressant effects of problem-solving therapies, the specialized nature of the samples and the limited numbers of assessment points do not permit firm conclusions.
The present paper, from the Research Evaluating the Value of Augmenting Medication with Psychotherapy (REVAMP) trial (Kocsis et al., 2009), examines whether the Cognitive Behavioral Analysis System of Psychotherapy (CBASP; McCullough, 2000), an approach that targets interpersonal problem solving in chronic depression, influences depressive symptoms via its effects on social problem solving. This study extends previous investigations by assessing social problem solving and depressive symptoms biweekly throughout treatment, and using time-lagged analyses within a mixed models framework to test whether changes in problem solving predict subsequent depression over time. In addition, we examine whether the associations over time between social problem solving and subsequent depressive symptoms are greater for patients receiving CBASP plus medication than patients receiving Brief Supportive Psychotherapy (BSP) plus medication and patients receiving medication alone.
The larger REVAMP trial tested the efficacy of a stepped treatment strategy in which CBASP or BSP was added to pharmacotherapy switch or augmentation in chronically depressed patients who failed to fully respond to an initial trial of medication. As chronic depression is characterized by poor coping and social adjustment (Klein & Leader, 1996; McCullough et al., 1990; Miller et al., 1998), a problem-solving intervention may have particular relevance for this population (McCullough, 2000). As described elsewhere (Kocsis et al., 2009), the three treatment conditions (CBASP plus pharmacotherapy, BSP plus pharmacotherapy, and pharmacotherapy alone) produced similar change in depressive symptoms. Hence, although our analyses explore whether the treatment conditions influence depressive symptoms through different mechanisms, they differ from traditional tests of mediation; rather than determining whether change in social problem solving accounts for differential treatment effects, we examine whether the magnitude of the associations over time between social problem solving and subsequent depressive symptoms differ between treatment conditions. We address three specific questions: (a) do CBASP plus pharmacotherapy produce greater change in social problem solving than BSP plus pharmacotherapy and pharmacotherapy alone; (b) is social problem solving associated with subsequent depression over time; and (c) is this association stronger for CBASP than for each of the two comparison treatments conditions?
Method
Design
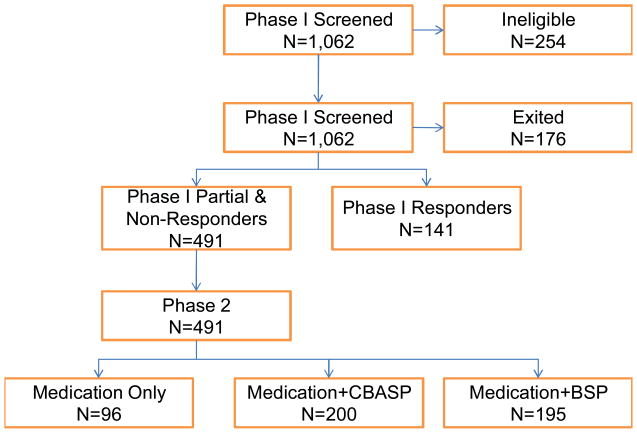
REVAMP consisted of two 12-week phases. During phase 1, patients were assigned to receive an antidepressant medication according to a pharmacotherapy algorithm, and their response was evaluated. Patients achieving less than full remission were randomized into phase 2. Full remission was defined by concomitantly meeting the following three conditions: a) ≥ 60% reduction in Hamilton Scale for Depression [HAM-D] score, b) a 24-item HAM-D total score less than 8, and c) no longer meeting DSM-IV criteria for MDD for 2 consecutive visits during weeks 6 through 12. Phase 2 participants all received the next-step treatment in the pharmacotherapy algorithm and were randomly assigned to one of three treatment cells in a 2:2:1 ratio: to have CBASP or BSP added to their pharmacotherapy or to receive medication alone. The 12-week duration for phase 2 mirrored the length of treatment in a previous chronic depression study by our group (Keller et al., 2000; Schatzberg et al., 2005) and the STAR*D study (Thase et al., 2007).
Participants
Patients were recruited at eight sites through outreach to clinicians and advertising. All patients met criteria for a current episode of MDD as defined by the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV; American Psychiatric Association, 1994) and assessed with the Structured Clinical Interview for DSM-IV Axis-I Disorders, Patient Edition (SCID-P; First et al., 1996). The MDD episode had to have a minimum duration of at least four weeks and the patient had to have experienced depressive symptoms for more than two years without remission. Thus, participants met criteria for double depression (current MDD episode with antecedent dysthymic disorder), chronic MDD, or recurrent MDD with incomplete recovery between episodes. Interviews were conducted by experienced raters who had been certified in the SCID by an expert rater at another site based on a videotaped interview.
Patients were between 18 and 75 years old, had scores of at least 20 on the 24-item Hamilton Rating Scale for Depression (HAM-D; Guy, 1976) at baseline, were fluent in English, and provided signed informed consent. Exclusion criteria were pregnancy; current diagnosis of any psychotic disorder; history of bipolar disorder; dementia; current principal diagnosis of posttraumatic stress disorder, anorexia, bulimia nervosa, or obsessive-compulsive disorder; antisocial, schizotypal, or severe borderline personality disorder; and current alcohol or other substance-related dependence disorder (except nicotine dependence) requiring detoxification. Patients with substance abuse disorders were permitted to enroll if they agreed to participate in Alcoholics Anonymous or chemical dependence counseling and to implement a sobriety plan in conjunction with study treatment. Also excluded were patients previously treated with CBASP, those who had already failed at least four of the treatment steps in the pharmacotherapy algorithm, those unwilling to terminate other forms of psychiatric treatment, and those had serious unstable or terminal medical illness that might compromise study participation.
Pharmacotherapy
The pharmacotherapy algorithm (see Kocsis et al., 2009) was based on empirically derived algorithms such as the Texas Medication Algorithm Project and the STAR*D study (Crismon et al., 1999; Fava et al., 2003). The sequence began with two selective serotonin reuptake inhibitors (SSRIs), sertraline hydrochloride and escitalopram oxalate. Bupropion hydrochloride was prescribed for patients who reported no response to two adequate SSRI trials or to augment treatment in those who responded only partially to an SSRI. Patients who had not benefited from these medications were offered additional options, including venlafaxine hydrochloride, mirtazapine, and lithium carbonate augmentation.
The protocol specified minimum and maximum doses, speed of dosage escalation, and trial lengths after each change. Patients were evaluated every two weeks. To minimize attrition, a patient intolerant to a medication during the first four weeks of Phase 1 could be moved to the next level of the sequence. No other psychotropic medications were permitted other than zolpidem tartrate and zaleplon for insomnia. Pharmacotherapists followed the manual by Fawcett et al. (1987) from the National Institute of Mental Health Treatment of Depression Collaborative Research Program (NIMH TDCRP; Elkin et al., 1989), with minimal psychotherapeutic intervention. During the randomized phase of the study, sessions were audiotaped and reviewed for adherence to guidelines. Bimonthly supervision by senior pharmacotherapists helped to ensure adherence. Patients were given packets of pills containing their daily dose for the interval between visits. At each visit, pharmacotherapists asked patients about treatment adherence and to return unused pills.
Cognitive Behavioral Analysis System of Psychotherapy
CBASP is a manualized, time-limited, cognitive-behavioral psychotherapy developed specifically to treat chronic depression (McCullough, 2000, 2001). Its goals are to help patients change their patterns of coping, improve their interpersonal skills, understand the consequences of their thoughts and behavior, and interact more effectively with others. The core procedure in CBASP involves training patients to apply a structured interpersonal problem-solving algorithm, referred to as situational analysis (SA). In SA, patients identify a recent distressing interpersonal situation and examine it with the therapist. The process consists of three phases: elicitation, remediation, and generalization. In the elicitation phase, patients describe: (a) the specific situation, (b) their thoughts during the situation, (c) their behavior, (d) the outcome of the encounter, (e) the outcome they would have desired, and (f) whether the desired outcome was achieved. In the remediation phase, patients work with therapists to identify alternative thoughts, behaviors, and/or desired outcomes during the situation to increase the probability of achieving a realistic and attainable desired outcome. Among the many problem-solving strategies that might be employed in this phase include several designed either to formulate a more realistic desired outcome or goal, or devise more effective means of achieving the goal including: (1) assisting the patient to identify a behaviorally specific desired outcome, in cases where this is not clear; (2) examining how achievable the desired outcome is and reformulating the goal when it is unrealistic or unattainable; (3) helping the patient to prioritize a single desired outcome in cases where multiple goals are presented; (4) examining the extent to which the individual’s thoughts are consistent with, and likely to increase the probability of achieving, the desired outcome, and generating alternative ways of thinking about the problem that might increase the chances of attaining the individual’s goal; (5) examining whether the individual’s behaviors are consistent with, and likely to maximize the probability of achieving, the desired outcome, and generating alternative behaviors that may be more successful; and (6) using role plays to expand on and rehearse alternate behavioral strategies that may increase the probability of achieving the desired outcome. In the generalization phase, patients and therapists review what has been learned and explore how the patient’s new understanding and skills can be applied to similar situations in the past and future.
SA was introduced during the third session. Patients were assigned the task of self-monitoring distressing interpersonal situations between sessions using the Coping Style Questionnaire (McCullough, 2000, 2001). Patients brought this material into each session and it became the focus of SAs.
CBASP sessions were held twice weekly during weeks 1–4 and weekly during weeks 5–12. Up to four more sessions could be added during weeks 5–8 if the patient needed additional time to master SA, for a total of 16–20 sessions. Therapists and supervisors were trained and certified in CBASP by James P. McCullough, Jr. who developed the therapy. Therapists were required to have at least two years of clinical experience after completing a Ph.D. in Psychology or psychiatric residency, or five years of experience after completing a Masters in Social Work degree. Therapists met with site supervisors weekly. Therapy sessions were videotaped, and McCullough and the site supervisors monitored the integrity of the therapists’ adherence to protocol using a CBASP Therapist Adherence Rating Scale that ensures that CBASP specific behaviors are administered competently and behaviors foreign to CBASP are not used.
Brief Supportive Psychotherapy
As defined in an unpublished treatment manual (Markowitz & Sacks, 2002), BSP emphasizes the nonspecific or “common” factors assumed to be important ingredients across psychotherapies (Frank, 1971; Rogers, 1951), including reflective listening, empathy, evoking affect, therapeutic optimism, and acknowledgment of patients’ assets. Specific interpersonal, cognitive, behavioral, and psychodynamic interventions, and especially situational analyses, were strictly proscribed. Paralleling the CBASP condition, 16–20 BSP sessions were scheduled during the 12 weeks of treatment. The BSP therapists’ professional degrees, amount of clinical experience, training, and supervision were comparable to those of the CBASP therapists. The certification and training procedures were led by JCM (see Markowitz, Manber & Rosen, 2008).
Adherence Monitoring
During the randomized phase of the study, all treatments (including pharmacotherapy) were monitored to ensure therapist adherence to protocol. All psychotherapy sessions were videotaped and all pharmacotherapy sessions were audiotaped. For each psychotherapy therapist-patient dyad, one or two tapes were randomly selected—one early (sessions 2–6) and onefrom later in treatment (session 8 or later)—and rated in their entirety using the Collaborative Study Psychotherapy Rating Scale from the NIMH TDCRP (Elkin et al., 1989) and the Therapist Adherence Rating Scale. Adherence ratings were conducted at the Cornell site by two trained raters with established reliability.
Randomization
Randomization was done centrally at the data coordinating center and was stratified by site, phase 1 response status (ie, no response or partial response), and medication history (failure to respond to < 3 adequate medication trials, including the trials during phase 1 of this study, versus failure to respond to ≥ 3 adequate medication trials). A randomization allocation ratio of 2:2:1 (CBASP plus medication:BSP plus medication:Medication alone) was used.
Measures
Social Problem Solving
Patients completed the Social Problem Solving Inventory-Revised (SPSI-R) (D’Zurilla, Nezu, & Maydeu-Olivares, 2002) on a biweekly basis beginning in the second week after randomization, prior to commencing work on SA in the CBASP condition. The SPSI-R is a 52-item self-report measure of social problem solving based on the classic model developed by D’Zurilla and Goldfried (1971) and expanded and refined by D’Zurilla and Nezu (1982, 2007). According to this model, two major processes determine real-world problem-solving outcomes: problem orientation, a motivational process involving a set of relatively stable cognitive schemas that reflect a general awareness of everyday problems and the individual’s own problem solving-ability; and problem solving proper. Problem solving proper involves the rational application of four major problem-solving skills: problem definition and formulation; generation of alternative solutions; decision making; and solution implementation and verification.
The SPSI-R assesses five factor-analytically derived dimensions: positive problem orientation; negative problem orientation; rational problem solving (including subscales for each of the four major problem-solving skills listed above); impulsivity/carelessness style; and avoidance style. The SPSI-R has excellent psychometric properties, including high internal consistency and test-retest stability, and good convergent and discriminant validity (D’Zurilla & Nezu, 1990; D’Zurilla et al., 2002; D’Zurilla & Maydeu-Olivares, 1995). For example, the SPSI-R is significantly related to independent global judgments of problem-solving competence in the real world, as well as to other problem solving inventories. In addition, it is distinguishable from related constructs such as intelligence, experiential coping, optimism, pessimism, and positive and negative trait affectivity (D’Zurilla & Maydeu-Olivares, 1995).
Although McCullough’s model and D’Zurilla’s models were developed relatively independently, there is considerable convergence between them. In the course of completing the SA procedure, CBASP addresses the four problem-solving skills that comprise problem-solving proper in D’Zurilla’s model. The elicitation stage of SA is designed to identify and define problematic interpersonal situations, which then become the basis for further analysis (problem identification and formulation). The remediation phase of SA emphasizes the generation of alternative approaches and strategies with a higher probability of achieving the desired goal and/or the generation of alternative goals that may be more realistic and attainable (generation of alternative solutions). In the remediation phase, patients also work on the decision-making process, as they must learn to select an outcome that is both desirable and potentially achievable, and determine which cognitions and behaviors are most likely to achieve that goal (decision-making). Between-session homework assignments are designed to give patients opportunities to implement their new problem-solving skills in real-world contexts, and these attempts are reviewed in the next session (solution implementation and verification). Finally, CBASP addresses avoidant and impulsive/careless problem-solving styles by requiring patients to apply the SA approach to problematic situations both between and within sessions, and examining the situations and their problem-solving efforts in a very specific and concrete manner. While CBASP does not directly address problem orientations, D’Zurilla and Nezu (2007) have argued that the most powerful influence on improvement in problem orientation is likely to be successful problem-solving performance (CBASP’s primary target), rather than cognitive restructuring or other procedures that focus directly on problem orientation.
Depressive symptoms
Independent evaluators assessed depressive symptoms every two weeks using the 24-item HAM-D (Guy, 1976). We chose the 24-item version of the HAM-D because it contains cognitive items characteristic of chronically depressed patients and has been used in all previous major chronic depression studies. Evaluations were performed by experienced raters who were certified on an annual basis by independently rating videotapes of criterion evaluations. Raters were unaware of patients’ treatment condition. Raters’ and clinicians’ offices were physically separated at each site, and raters instructed patients at the beginning of each assessment session not to mention psychotherapy or their psychotherapist during the interviews.
Data Analysis
The randomized treatment groups were compared on baseline demographic and clinical variables. Analyses of variance or Kruskal-Wallis tests were used to compare the groups on continuous or ordinal variables. We used χ2 tests for categorical variables. Similar analyses compared dropouts and completers on baseline demographic and clinical variables. Each statistical test in this report had a 2-tailed alpha level of .05. The general data analytic strategy for efficacy used mixed effects linear regression models because they are flexible enough to account for different numbers of observations per subject. Furthermore, this modeling procedure can account for the changing symptomatic state of subjects over the course of the trial. The models included 2 random effects (intercept and slope) and fixed effects for treatment, site, time, and response status at the end of phase 1 of the study (non-remission or partial remission). To examine interactions, cross-product terms for treatment X time were added to the model and improvement in model fit was compared using the log-likelihood ratio test. The first set of models focused on the effects of treatment condition on social problem solving over time. The second set of models examined whether the associations between problem solving and subsequent depressive symptoms over time differed between treatment conditions. In these models, SPSI-R scores were lagged two weeks behind HAM-D scores. That is, SPSI-R scores at week 2 predicted HAM-D scores at week 4; SPSI-R scores at week 4 predicted HAM-D scores at week 6; and so on through SPSI-R scores at week 10 predicting HAM-D scores at week 12.
Results
Eight hundred and eight patients enrolled in phase 1. Phase 1was completed by 632 (78.2%) patients, 491 (77.7 %) of whom failed to remit and entered phase 2. Table 1 provides the clinical and demographic characteristics of the 491 participants enrolled in phase 2 by randomization group. The only statistically significant difference among the groups randomized to the three treatment conditions was a slightly higher percentage of whites randomized to psychotherapy plus medication versus medication alone.
Table 1.
Descriptive characteristics of sample
| Variable | CBASP | BSP | Meds only | Test statistic (df) |
|---|---|---|---|---|
| Sex, No. (%) | ||||
| Male | 85 (44.3) | 78 (41.7) | 47 (52.2) | χ2(2)=2.00 |
| Female | 107 (55.7) | 109 (58.3) | 43 (47.8) | |
| Race, No. (%) | ||||
| White | 175 (91.1)a | 167 (89.3)a | 76 (84.4)b | χ2(4)= 13.34* |
| Black | 11 (5.7) | 9 (4.8) | 1 (1.1) | |
| Other | 6 (3.1) | 11 (5.9) | 13 (14.4) | |
| Hispanic ethnicity, No. (%) | ||||
| Yes | 14 (7.3) | 14 (7.5) | 7 (7.8) | χ2(2)=0.01 |
| No | 178 (92.7) | 173 (92.5) | 83 (92.2) | |
| Employment Status, No. (%) | ||||
| Employed | 117 (60.9) | 118 (63.4) | 53 (58.9) | χ2(4)=2.49 |
| Unemployed | 61 (31.8) | 54 (29.0) | 33 (36.7) | |
| Retired | 14 (7.3) | 14 (7.5) | 4 (4.4) | |
| Education, No. (%) | ||||
| <High School | 3 (1.6)a | 3 (1.6)b | 0 (0.0)b | χ2(4)=10.09* |
| High school graduate | 51 (26.6) | 74 (39.6) | 37 (41.1) | |
| >=High School | 138 (71.9) | 110 (58.8) | 53 (58.9) | |
| Marital Status, No. (%) | ||||
| Married | 70 (36.5) | 86 (46.0) | 39 (43.3) | χ2(6)=8.98 |
| Never | 68 (35.4) | 49(26.2) | 31 (34.4) | |
| Divorced | 48 (25) | 48 (25.7) | 16 (17.8) | |
| Recurrence, No. (%) | ||||
| Yes | 132 (68.8) | 123 (65.8) | 54 (60.0) | χ2(2)=1.85 |
| No | 60 (31.3) | 64 (34.2) | 36 (40.0) | |
| Attempted Suicide, No. (%) | ||||
| Yes | 18 (9.8) | 19 (10.9) | 12 (13.6) | χ2(2)=0.75 |
| No | 166 (90.2) | 156 (89.1) | 76 (86.4) | |
| Age, years Mean (SD) | 45.3 (11.8) | 46.6 (11.5) | 43.4 (13.3) | F(2,475)=2.91+ |
| Age at initial onset of MDD, years Mean(SD) | 27.0 (13.2) | 26.3 (13.8) | 25.5 (12.1) | F(2,457)=0.62 |
| Length of index episode of MDD, months Mean(SD) | 90.7(120.0) | 91.8(113.0) | 94.2(110.0) | F(2,471)=0.01 |
| Duration of MDD, years Mean(SD) | 14.0 (13.7) | 20.1 (18.1) | 17.3 (12.0) | F(2,457)=1.31 |
| No. of episodes of MDD | 2.5 (2.3) | 2.4 (2.1) | 2.8 (6.5) | F(2,412)=0.26 |
Note: CBASP = Cognitive Behavioral Analysis System of Psychotherapy plus medication; BSP = Brief Supportive Psychotherapy plus medication; Meds = Medication. Different superscripts indicate that groups differ at p< .05 in pairwise comparisons.
p < .10;
p< .05.
Patients assigned to BSP attended a mean (SD) of 13.1(7.0) therapy sessions, and patients assigned to CBASP attended 12.5 (6.6) sessions. The mean (SD) numbers of pharmacotherapy visits were 5.4 (1.4), 5.3 (1.5), and 5.2 (1.5) in the CBASP, BSP, and medication only groups, respectively.
Adherence ratings were conducted on 84 BSP, 68 CBASP, and 52 pharmacotherapy sessions. Only one CBASP session, and no BSP and pharmacotherapy sessions, were rated as having inadequate adherence to protocol.
Effects of treatment on social problem solving
Table 2 presents HAM-D and SPSI-R total scores at each assessment as a function of treatment condition. First, we compared the effects of the three treatment conditions on social problem solving. There were significant differences among the three treatment conditions on the trajectories of social problem solving for the total SPSI-R score and all subscale scores except Negative Problem Orientation (see Table 3). For the total SPSI-R score, patients receiving CBASP plus medication showed significantly greater improvement in social problem solving over time than patients receiving BSP plus medication (coefficient = 0.0999; SE = 0.0294; z = 3.39, p < .001), and a trend for greater improvement than patients receiving medication alone (coefficient = 0.0614; SE = 0.0362; z = 1.69, p = .09). Patients receiving BSP plus medication and patients receiving medication alone did not differ on change in social problem solving over time (coefficient = 0.0385; SE = 0.0365; z = 1.06, p = .29). Methods for calculating effect sizes for mixed models are not well-developed, hence we computed Cohen’s d for the pairwise comparisons between groups on change from baseline total SPSI-R score and the last observation carried forward. The effects for the comparisons between CBASP plus medication and the two comparison conditions were medium in size (.34 and .29, for BSP plus medication and medication alone, respectively). The magnitude of the difference between the BSP plus medication and medication alone was small (d = .03).
Table 2.
Means and Standard Deviations for HAM-D and SPSI-R total and five subscales as function of treatment condition and week of treatment.
| Arm | Week 2 | Week 4 | Week 6 | Week 8 | Week 10 | Week 12 |
|---|---|---|---|---|---|---|
| CBASP | ||||||
| HAM-D | 16.94 (8.92) | 14.85 (8.57) | 15.08 (8.26) | 14.94 (9.38) | 12.77 (8.45) | |
| SPSI-total | 10.66 (3.21) | 11.12 (3.32) | 11.27 (3.40) | 11.57 (3.59) | 11.81 (3.53) | 12.29 (3.49) |
| SPSI-AS | 11.39 (6.48) | 11.19 (6.70) | 11.02 (6.66) | 10.39 (6.74) | 10.56 (6.83) | 9.91 (6.56) |
| SPSI-ICS | 11.79 (7.81) | 11.11 (7.75) | 11.52 (8.20) | 11.04 (8.12) | 10.14 (7.17) | 10.42 (7.24) |
| SPSI-NPO | 18.02 (8.71) | 16.76 (8.98) | 15.82 (9.05) | 15.03 (9.60) | 14.19 (9.68) | 13.87 (9.70) |
| SPSI-PPO | 8.25 (4.05) | 8.50 (4.14) | 8.98 (4.22) | 9.60 (4.24) | 9.55 (4.49) | 10.17 (4.70) |
| SPSI-RPS | 33.31 (16.27) | 34.82 (16.34) | 35.36 (16.22) | 36.15 (16.91) | 37.64 (17.26) | 40.39 (17.66) |
| BSP | ||||||
| HAM-D | 17.24 (8.04) | 16.28 (8.70) | 14.42 (8.65) | 13.18 (8.36) | 11.29 (8.30) | |
| SPSI-total | 11.52 (3.08) | 11.64 (3.23) | 11.70 (3.39) | 11.63 (3.43) | 11.81 (3.49) | 12.11 (3.41) |
| SPSI-AS | 10.17 (6.10) | 9.95 (6.35) | 10.02 (6.51) | 10.27 (6.43) | 9.98 (6.80) | 9.49 (6.59) |
| SPSI-ICS | 10.02 (6.63) | 9.84 (7.05) | 10.06 (6.90) | 10.04 (6.96) | 10.14 (7.86) | 9.64 (6.71) |
| SPSI-NPO | 16.47 (9.03) | 15.40 (8.92) | 14.81 (9.32) | 14.66 (9.41) | 14.08 (9.50) | 13.24 (9.17) |
| SPSI-PPO | 9.01 (3.83) | 8.94 (4.06) | 9.36 (4.29) | 8.74 (4.22) | 9.14 (4.11) | 9.72 (4.40) |
| SPSI-RPS | 36.27 (15.94) | 35.09 (15.49) | 36.40 (16.46) | 35.20 (17.24) | 35.89 (17.35) | 36.88 (17.90) |
| Medication only | ||||||
| HAM-D | 15.27 (9.46) | 13.74 (7.97) | 13.71 (8.54) | 13.66 (8.52) | 12.28 (8.44) | |
| SPSI-total | 11.29 (2.92) | 11.32 (3.25) | 11.66 (3.28) | 11.51 (3.16) | 12.15 (3.14) | 12.22 (3.45) |
| SPSI-AS | 10.53 (5.52) | 10.28 (6.52) | 9.92 (6.45) | 9.83 (6.53) | 9.23 (6.31) | 8.62 (7.00) |
| SPSI-ICS | 10.04 (6.04) | 10.01 (7.14) | 9.67 (7.20) | 9.65 (7.39) | 8.70 (7.49) | 9.47 (7.70) |
| SPSI-NPO | 16.17 (8.96) | 15.37 (9.23) | 14.73 (9.79) | 14.71 (9.83) | 13.37 (9.79) | 13.39 (10.24) |
| SPSI-PPO | 8.17 (4.03) | 7.93 (4.11) | 8.75 (4.43) | 8.76 (4.33) | 8.96 (3.80) | 9.14 (4.19) |
| SPSI-RPS | 35.22 (14.81) | 35.28 (16.15) | 35.87 (17.11) | 35.60 (15.45) | 37.24 (15.30) | 37.15 (15.77) |
Note. HAM-D = Hamilton Rating Scale for Depression; SPSI-R = Social Problem Solving Inventory-Revised; AS = Avoidance Style; ICS = Impulsivity/Carelessness Style; NPO = Negative Problem Orientation; PPO = Positive Problem Orientation; RPS = Rational Problem Solving; CBASP = Cognitive Behavioral Analysis System of Psychotherapy; BSP = Brief Supportive Psychotherapy
Table 3.
Models testing effects of treatment on social problem solving over time
| Variable | N | Nobs | −2LLdiff | df | p-value |
|---|---|---|---|---|---|
| SPSI-total | 474 | 2339 | 11.45 | 2 | 0.003 |
| SPSI-AS | 478 | 2514 | 7.45 | 2 | 0.02 |
| SPSI-ICS | 476 | 2482 | 7.14 | 2 | 0.02 |
| SPSI-NPO | 478 | 2489 | 4.53 | 2 | 0.10 |
| SPSI-PPO | 478 | 2522 | 11.60 | 2 | 0.003 |
| SPSI-RPS | 476 | 2463 | 14.60 | 2 | 0.0007 |
Note. SPSI = Social Problem Solving Inventory-Revised; AS = Avoidance Style; ICS = Impulsivity/Carelessness Style; NPO = Negative Problem Orientation; PPO = Positive Problem Orientation; RPS = Rational Problem Solving.
Turning to the SPSI-R subscales, patients receiving CBASP plus medication exhibited significantly greater increases in rational problem solving than patients receiving BSP plus medication and patients receiving medication alone (coefficient = .4993; SE = .1340; z = 3.73, p < .001, and coefficient = .1052; SE = .0457; z = 2.30, p = .02, respectively). Patients receiving CBASP plus medication also exhibited significantly greater increases in positive problem orientation than patients receiving BSP plus medication and patients receiving medication alone (coefficient = .1201; SE = .0369; z = 3.25, p = .001, and coefficient = .1052; SE = .0457; z = 2.30, p = .02, respectively). However, patients receiving BSP plus medication did not differ from those receiving medication alone on change in rational problem solving and positive problem orientation (coefficient = −.0964; SE = .1673; z = −0.58, p = .56, and coefficient = −.0149; SE = .0459; z = −0.32, p = .75, respectively).
Interestingly, patients receiving BSP plus medication exhibited significantly less change in avoidant problem solving over time than patients receiving CBASP plus medication and patients receiving medication alone (coefficient = −.1236; SE = .0492; z = −2.51, p = .01, and coefficient = −.1248; SE = .0614; z = −2.03, p = .04, respectively). Patients receiving BSP plus medication also exhibited significantly less change in impulsivity/carelessness over time than patients receiving CBASP plus medication, with a similar trend compared to patients receiving medication alone (coefficient = −.1537; SE = .0593; z = −2.59, p < .01, and coefficient = −.1255; SE = .0737; z = −1.70, p = .09, respectively). In contrast, patients receiving CBASP plus medication did not differ from those receiving medication alone on levels of avoidant and impulsivity/careless problem solving over time (coefficient = .0012; SE = .0611; z = 0.02, p = .98, and coefficient = −.0282; SE = .0733; z = −0.38, p = .70, respectively).
Does social problem solving predict subsequent depressive symptoms over time?
As treatment did not significantly influence the trajectory of scores on the negative problem orientation subscale, this subscale was excluded from further analyses. We next estimated main effects only models to examine the association over time between social problem solving and subsequent depressive symptoms. In the model for total SPSI-R scores, there were significant effects for a) time, indicating that HAM-D scores decreased over time (coefficient = −.4804; SE = .0477; z = −10.07, p < .001); b) phase 1 response status (coefficient = −6.7573; SE = .6379; z = −10.59, p < .001), indicating a greater decline in HAM-D scores among patients who entered the randomized phase as non-responders rather than partial responders; and c) total SPSI-R score (coefficient = −.3136; SE = .0707; z = −4.44, p < .001), indicating that as social problem solving increased over time, depressive symptoms at the next visit declined. The effects of site and treatment condition on HAM-D scores over time were not significant.
The main effects only models for the subscales were generally consistent with the main effects only model for the total SPSI-R. In the main effects only models for the subscales, time and phase 1 remission status significantly predicted the trajectory of HAM-D scores, whereas site and treatment condition did not. Positive problem orientation predicted a reduction in depressive symptoms (coefficient = −.1320; SE = .0493; z = −2.68, p = .007), while impulsive/careless and avoidant styles were associated with greater depressive symptoms over time (coefficient = .0800; SE = .0302; z = 2.65, p = .008 and coefficient = .1466; SE = .0344; z = 4.26, p < .001, respectively). Rational problem solving did not predict the trajectory of depressive symptoms over time.
Does treatment condition influence the associations between social problem solving and subsequent depressive symptoms over time?
In order to determine whether the temporal associations between social problem solving and subsequent depressive symptoms differed as a function of treatment condition, we ran five models adding the main effect of treatment and the corresponding treatment by SPSI-R interaction term to the main effects models described above for the total SPSI-R scale and the negative problem orientation, avoidant style, and impulsivity/carelessness style subscales. As shown in Table 4, adding the interaction term did not significantly improve the fit of any of the five models, indicating that the association between social problem solving and subsequent depressive symptoms over time did not differ between treatment conditions.
Table 4.
Models testing interaction of treatment and social problem solving on depression over time
| Variable | N | Nobs | −2LLdiff | df | p-value |
|---|---|---|---|---|---|
| SPSI-total | 459 | 1843 | 0.13 | 2 | 0.94 |
| SPSI-AS | 462 | 1974 | 1.48 | 2 | 0.79 |
| SPSI-ICS | 462 | 1946 | 0.29 | 2 | 0.87 |
| SPSI-PPO | 462 | 1983 | 0.26 | 2 | 0.88 |
| SPSI-RPS | 462 | 1940 | 1.79 | 2 | 0.41 |
Note. SPSI = Social Problem Solving Inventory-Revised; AS = Avoidance Style; ICS = Impulsivity/Carelessness Style; NPO = Negative Problem Orientation; PPO = Positive Problem Orientation; RPS = Rational Problem Solving.
We re-analyzed these data using cumulative change in social problem solving between first assessment and time t to predict change in lagged HAM-D scores from time t to time t + 1. The models including treatment X social problem solving interaction terms for the total SPSI-R and subscales again failed to provide a significant increment in fit when compared to the corresponding main effects only model.
Discussion
We addressed three questions in this study: (a) does CBASP plus pharmacotherapy produce greater change in social problem solving than BSP plus pharmacotherapy and pharmacotherapy alone; (b) is social problem solving associated with subsequent reductions in depressive symptoms; and (c) is this association stronger for CBASP than for the two comparison treatments conditions? We found that patients who received CBASP plus pharmacotherapy exhibited significantly, greater gains in social problem solving than patients who received BSP plus pharmacotherapy. In addition, there was a trend for patients in the CBASP condition to exhibit greater improvement in social problem solving than patients receiving medication alone. Examining specific forms of social problem solving, patients receiving CBASP plus medication exhibited significantly greater increases in rational problem solving and positive problem orientation than patients in either of the other two conditions. In addition, patients receiving BSP plus medication exhibited significantly less change in avoidant problem solving than patients in the other two conditions, and significantly less change in impulsive problem solving than patients receiving CBASP plus medication.
The differences in change in social problem solving tended to be greatest between the two psychotherapy augmentation conditions, with the pharmacotherapy alone condition occupying an intermediate position. This raises the possibility that BSP may have hindered some aspects of problem solving, perhaps by reinforcing emotion-focused coping strategies. However, this should not be overinterpreted, as BSP plus pharmacotherapy did not differ from pharmacotherapy alone on change in the total SPSI-R.
The present findings are consistent with prior studies that found problem-solving therapy was associated with greater improvement in social problem solving than comparison conditions, such as supportive therapy and being on a waiting-list (Alexopoulos et al., 2003; Nezu, 1986; Nezu et al., 1989; Nezu et al., 2003; Sahler et al., 2002). Importantly, this study extended past work by examining a more severe and chronic sample than most previous studies.
We also found that gains in social problem solving predicted subsequent reductions in depressive symptoms over time. Several other studies reported an association between change in social problem solving and change in depression (Alexopoulos et al., 2003; Nezu et al., 2003; Sahler et al., 2002). However, unlike the present study, these studies assessed both variables only at baseline and follow-up, hence the direction of the association could not be determined.
As CBASP plus medication predicted greater change in social problem solving and gains in social problem solving predicted declines in depression over time, one might expect that patients in the CBASP condition would have better outcomes than patients in the comparison conditions. However, as reported in our previous article (Kocsis et al., 2009) and confirmed in the analyses in the present paper, the three treatment conditions did not differ on depression outcomes. This pattern of findings suggests that different treatments influence depressive symptoms through different processes. If so, and social problem solving plays a greater role in alleviating depression in CBASP than other treatment approaches, then one might expect that change in social problem solving would be closely linked to change in depressive symptoms over time in the CBASP condition. Contrary to our hypotheses, however, the interaction of treatment condition with the association between social problem solving and lagged depression scores did not approach significance. Instead, the magnitude of the relation between change in social problem solving and subsequent depression was similar regardless of whether or not patients received CBASP.
Taken together, this pattern of findings suggests that while CBASP plus medication may produce greater gains in social problem solving than BSP plus medication and, at a trend level, pharmacotherapy alone, and that better social problem solving is associated with subsequent improvements in depressive symptoms, this mechanism may be common across treatments. That is, to the extent that any treatment positively influences social problem solving, a decline in depressive symptoms is likely to follow. However, it important to consider that possibility that problem solving does play a somewhat greater role in producing change in CBASP, but that despite our large sample, we did not have sufficient power to detect this effect. A more thorough dismantling of the specific aspects of CBASP that enhance problem solving and consideration of the ways in which the intervention might be augmented to strengthen its effect may be useful, given that problem solving appears to be an important, and teachable, aspect of coping. Alternatively, although there is considerable convergence between the processes targeted in CBASP and the constructs assessed by the SPSI-R, it is conceivable that a problem-solving measure that was specifically designed for CBASP might have greater sensitivity.
This study had a number of strengths, including a large, carefully characterized sample and multiple assessments of social problem solving and depressive symptoms over time. However, several limitations should be considered. First, CBASP is an integrative treatment. Although training in interpersonal problem solving is a central component, CBASP also addresses long-standing maladaptive interpersonal patterns, dysfunctional cognitions, social skills deficits, and problems in the therapeutic relationship (McCullough, 2000). Hence, it is conceivable that the results would differ for treatments that focus more narrowly on social problem solving. Second, treatment was limited to 16–20 sessions over 12 weeks. Although this was more intensive than most problem-solving therapies (D’Zurilla & Nezu, 1999; Mynors-Wallis et al., 1995), the patients in this sample were considerable more severe and chronic than in most previous problem-solving trials. Hence, a longer duration of treatment might be needed to isolate specific therapeutic mechanisms for this population. Third, all patients in the CBASP condition received concomitant pharmacotherapy and had previously experienced at least one unsuccessful medication trial. This may have adversely influenced some patients’ motivation to fully engage with CBASP and situational analysis, attenuating its effects on social problem solving. Fourth, assessments were conducted biweekly, and we examined only a two-week lag between social problem solving and depressive symptoms. It is possible that the effects of social problem solving on depressive symptoms unfold over much shorter or longer intervals, reducing the sensitivity of our analyses. Fifth, we used a self-report inventory to assess social problem solving. Although the SPSI-R is the most widely used and best-validated social problem-solving measure, other approaches, such as performance-based measures or experience sampling methods, might conceivably yield different results. Finally, patients were treated at academic centers, hence may not be entirely representative of chronically depressed patients in treated in community settings.
In conclusion, in a large, randomized clinical trial of chronically depressed patients, we found that CBASP in conjunction with medication produced significantly greater improvement in social problem solving than BSP plus medication, and a similar trend compared to pharmacotherapy alone. In addition, change in social problem solving predicted subsequent change in depressive symptoms over time. However, the magnitude of the associations between changes in social problem solving and subsequent depressive symptoms did not differ between treatment conditions. Hence, these findings fail to support the hypothesis that improved social problem solving, as measured by the SPSI-R, is a mechanism that uniquely distinguishes CBASP, despite its emphasis on addressing social problem-solving deficits, from other treatment approaches.
APPENDIX.
REVAMP Consort Chart
Acknowledgments
The study was supported by National Institute of Mental Health grants U01 MH62475; U01 MH61587; U01 MH62546; U01 MH61562; U01 MH63481; U01 MH62465; U01 MH61590; U01 MH61504; and U01 MH62491. Trial Registration is: clinicaltrials.gov Identifier: NCT00057551.
Footnotes
Thomas D’Zurilla is a recipient of royalties in relation to the SPSI-R. John Markowitz receives royalties from National Psychiatric Press, Basic Books and Oxford Press. John Markowitz also receives and Editorial stipend from Elsevier Press. Andrew Leon is on the Safety Monitoring Boards for Pfizer, Astra Zenica, Sunovion and is a consultant for NIMH, MedAvante, and Roche. James Kocsis has a research contract from Forest Pharmaceuticals, manufacturer of Lexapro.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
Contributor Information
Daniel N. Klein, Department of Psychology, Stony Brook University
Andrew C. Leon, Department of Psychiatry, Weill-Cornell Medical College
Chunshan Li, Department of Psychiatry, Weill-Cornell Medical College.
Thomas J. D’Zurilla, Department of Psychology, Stony Brook University
Sarah R. Black, Department of Psychology, Stony Brook University
Dina Vivian, Department of Psychology, Stony Brook University.
Frank Dowling, Department of Psychiatry, Stony Brook University.
Bruce A. Arnow, Department of Psychiatry, Stanford University School of Medicine
Rachel Manber, Department of Psychiatry, Stanford University School of Medicine.
John C. Markowitz, Department of Psychiatry, Columbia University College of Physicians and Surgeons
James H. Kocsis, Department of Psychiatry, Weill-Cornell Medical College
References
- Alexopoulos GS, Raue P, Areán P. Problem-solving therapy versus supportive therapy in geriatric major depression with executive dysfunction. American Journal of Geriatric Psychiatry. 2003;11:46–52. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Areán PA, Perri MG, Nezu AM, Schein RL, Christopher F, Joseph TX. Comparative effectiveness of social problem-solving therapy and reminiscence therapy as treatments for depression in older adults. Journal of Consulting and Clinical Psychology. 1993;61:1003–1010. doi: 10.1037//0022-006x.61.6.1003. [DOI] [PubMed] [Google Scholar]
- Areán PA, Raue P, Mackin S, Kanellopoulos D, McCulloch C, Alexopoulos GS. Problem-solving therapy and supportive therapy in older adults with major depression and executive dysfunction. American Journal of Psychiatry. doi: 10.1176/appi.ajp.2010.09091327. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett JE, Williams JW, Jr, Oxman TE, Frank E, Katon W, Sullivan M, et al. Treatment of dysthymia and minor depression in primary care: A randomized trial in patients aged 18–59 years. Journal of Family Practice. 2001;50:405–412. [PubMed] [Google Scholar]
- Bell AC, D’Zurilla TJ. Problem-solving therapy for depression: A meta-analysis. Clinical Psychology Review. 2009;29:348–353. doi: 10.1016/j.cpr.2009.02.003. [DOI] [PubMed] [Google Scholar]
- Crismon ML, Trivedi MH, Pigott TA, Rush AJ, Hirschfeld RMA, Kahn DA, et al. The Texas Medication Algorithm Project: Report of the Texas Consensus Conference Panel on Medication Treatment of Major Depressive Disorder. Journal of Clinical Psychiatry. 1999;60:142–156. [PubMed] [Google Scholar]
- Cuijpers P, van Straten A, Warmerdam L. Problem solving therapies for depression: A meta-analysis. European Psychiatry. 2007;22:9–15. doi: 10.1016/j.eurpsy.2006.11.001. [DOI] [PubMed] [Google Scholar]
- D’Zurilla TJ, Goldfried MR. Problem solving and behavior modification. Journal of Abnormal Psychology. 1971;78:107–126. doi: 10.1037/h0031360. [DOI] [PubMed] [Google Scholar]
- D’Zurilla TJ, Maydeu-Olivares A. Conceptual and methodological issues in social problem-solving assessment. Behavior Therapy. 1995;26:409–432. [Google Scholar]
- D’Zurilla TJ, Nezu AM. Social problem solving in adults. In: Kendal PC, editor. Advances in cognitive-behavioral research and therapy. Vol. 1. New York: Academic Press; 1982. [Google Scholar]
- D’Zurilla TJ, Nezu AM. Development and preliminary evaluation of the Social Problem-Solving Inventory. Psychological Assessment. 1990;2:156–163. [Google Scholar]
- D’Zurilla TJ, Nezu AM. Problem-solving therapy: A social competence approach to clinical intervention. 3. Ann Arbor, Michigan: Springer Publishing; 2007. [Google Scholar]
- D’Zurilla TJ, Nezu AM. Problem-solving therapy: A positive approach to clinical intervention. 3. Ann Arbor, Michigan: Spring Publishing; 2007. [Google Scholar]
- D’Zurilla TJ, Nezu AM, Maydeu-Olivares A. Manual for the Social Problem-Solving Inventory – Revised. North Tonawanda, NY: Multi-Health Systems; 2002. [Google Scholar]
- Dixon WA, Heppner PP, Burnett JW, Anderson WP, Wood PK. Distinguishing among antecedents, concomitants, and consequences of problem-solving appraisal and depressive symptoms. Journal of Counseling Psychology. 1993;40:357–364. [Google Scholar]
- Elkin I, Shea MT, Watkins JT, Imber SD, Sotsky SM, Collins JF, et al. National Institute of Mental Health Treatment of Depression Collaborative Research Program: General effectiveness of treatments. Archives of General Psychiatry. 1989;46:971–983. doi: 10.1001/archpsyc.1989.01810110013002. [DOI] [PubMed] [Google Scholar]
- Fava M, Rush AJ, Trivedi MH, Nierenberg AA, Thase ME, Sackeim HA, et al. Background and rationale for the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study. Psychiatric Clinics of North America. 2003;26:457–494. doi: 10.1016/s0193-953x(02)00107-7. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Epstein P, Fiester SJ, Elkin I, Autry JH. NIMH Treatment of Depression Collaborative Research Program. Clinical management – imipramine/placebo administration manual. Psychopharmacological Bulletin. 1987;23:309–324. [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis I Disorders — Patient Edition (SCID-I/P, Version 2.0) Biometrics Research Department, New York State Psychiatric Institute; New York: 1996. [Google Scholar]
- Frank JD. Eleventh Emil A. Gutheil memorial conference: Therapeutic factors in psychotherapy. American Journal of Psychotherapy. 1971;25:350–361. doi: 10.1176/appi.psychotherapy.1971.25.3.350. [DOI] [PubMed] [Google Scholar]
- Guy W. ECDEU assessment manual for psychopharmacology. Washington, DC: Department of Health, Education, and Welfare; 1976. Publication No. (ADM) 76–338. [Google Scholar]
- Haaga DAF, Fine JA, Terrill DR, Stewart BL, Beck AT. Social problem-solving deficits, dependency, and depressive symptoms. Cognitive Therapy and Research. 1995;19:147–158. [Google Scholar]
- Kant GL, D’Zurilla TJ, Maydeu-Olivares A. Social problem solving as a mediator of stress-related depression and anxiety in middle-aged and elderly community residents. Cognitive Therapy and Research. 1997;21:73–96. [Google Scholar]
- Keller MB, McCullough JP, Klein DN, Arnow B, Dunner DL, Gelenberg AJ, et al. A comparison of nefazodone, the cognitive behavioral analysis system of psychotherapy, and their combination for the treatment of chronic depression. New England Journal of Medicine. 2000;342:1462–1470. doi: 10.1056/NEJM200005183422001. [DOI] [PubMed] [Google Scholar]
- Kocsis JH, Gelenberg AJ, Rothbaum BO, Klein DN, Trivedi MH, Manber R, et al. Cognitive behavioral analysis system of psychotherapy and brief supportive psychotherapy for augmentation of antidepressant nonresponse in chronic depression: The REVAMP trial. Archives of General Psychiatry. 2009;66:1178–1188. doi: 10.1001/archgenpsychiatry.2009.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leader JB, Klein DN. Social adjustment in dysthymia, double depression and episodic major depression. Journal of Affective Disorders. 1996;37:91–101. doi: 10.1016/0165-0327(95)00076-3. [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Manber R, Rosen P. Therapists’ responses to training in brief supportive psychotherapy. American Journal of Psychotherapy. 2008;62:67–81. doi: 10.1176/appi.psychotherapy.2008.62.1.67. [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Sacks M. Manual for Brief Supportive Psychotherapy for Chronic Depression. Department of Psychiatry, Cornell University Medical College; New York, New York: 2002. Unpublished manuscript. [Google Scholar]
- Marx EM, Williams JM, Claridge GC. Depression and social problem solving. Journal of Abnormal Psychology. 1992;101:78–86. doi: 10.1037//0021-843x.101.1.78. [DOI] [PubMed] [Google Scholar]
- McCullough JP. Treatment for Chronic Depression: Cognitive Behavioral Analysis System of Psychotherapy. New York: Guilford Press; 2000. [DOI] [PubMed] [Google Scholar]
- McCullough JP. Training Manual for Diagnosing and Treating Chronic Depression: Cognitive Behavioral Analysis System of Psychotherapy. New York, NY: Guilford Press; 2001. [Google Scholar]
- McCullough JP, Braith JA, Chapman RC, Kasnetz MD, Carr KF, Cones JH, et al. Comparison of dysthymic major and nonmajor depressives. Journal of Nervous and Mental Disorders. 1990;178:596–597. doi: 10.1097/00005053-199009000-00008. [DOI] [PubMed] [Google Scholar]
- Miller IW, Keitner GI, Schatzberg AF, Klein DN, Thase ME, Rush AJ, et al. The treatment of chronic depression, part 3: Psychosocial functioning before and after treatment with sertraline or imipramine. Journal of Clinical Psychiatry. 1998;59:608–619. doi: 10.4088/jcp.v59n1108. [DOI] [PubMed] [Google Scholar]
- Mynors-Wallis LM, Gath DH, Lloyd-Thomas AR, Tomlinson D. Randomised controlled trial comparing problem solving treatment with amitriptyline and placebo for major depression in primary care. British Medical Journal. 1995;310:441–445. doi: 10.1136/bmj.310.6977.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mynors-Wallis LM, Gath DH, Day A, Baker F. Randomised controlled trial of problem solving treatment, antidepressant medication, and combined treatment for major depression in primary care. British Medical Journal. 2000;320:26–30. doi: 10.1136/bmj.320.7226.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nezu AM. Efficacy of a social problem-solving therapy approach for unipolar depression. Journal of Consulting and Clinical Psychology. 1986;54:196–202. doi: 10.1037//0022-006x.54.2.196. [DOI] [PubMed] [Google Scholar]
- Nezu AM, Nezu CM, Nezu VA. Depression, general distress, and causal attributions among university students. Journal of Abnormal Psychology. 1986;95:184–186. doi: 10.1037//0021-843x.95.2.184. [DOI] [PubMed] [Google Scholar]
- Nezu AM, Nezu CM, Perri MG. Problem-solving therapy for depression: Theory, research, and clinical guidelines. Oxford, England: John Wiley & Sons; 1989. [Google Scholar]
- Nezu AM, Perri MG. Social problem-solving therapy for unipolar depression: An initial dismantling investigation. Journal of Consulting and Clinical Psychology. 1989;57:408–413. [PubMed] [Google Scholar]
- Nezu AM, Nezu CM, Felgoise SH, McClure KS, Houts PS. Project Genesis: Assessing the efficacy of problem-solving therapy for distressed adult cancer patients. Journal of Consulting and Clinical Psychology. 2003;71:1036–1048. doi: 10.1037/0022-006X.71.6.1036. [DOI] [PubMed] [Google Scholar]
- Reinecke MA, DuBois DL, Schultz TM. Social problem solving, mood, and suicidality among inpatient adolescents. Cognitive Therapy and Research. 2001;25:743–756. [Google Scholar]
- Rogers CR. Client-centered therapy. Boston, MA: Houghton Mifflin; 1951. [Google Scholar]
- Sahler OJ, Varni JW, Fairclough DL, Butler RW, Noll RB, Dolgin MJ, et al. Problem-solving skills training for mothers of children with newly diagnosed cancer: A randomized trial. Journal of Developmental and Behavioral Pediatrics. 2002;23:77–86. doi: 10.1097/00004703-200204000-00003. [DOI] [PubMed] [Google Scholar]
- Schatzberg AF, Rush AJ, Arnow BA, Banks P, Blalock JA, Borian FE, et al. Chronic depression: Medication (nefazodone) or psychotherapy (CBASP) is effective when the other is not. Archives of General Psychiatry. 2005;62:513–520. doi: 10.1001/archpsyc.62.5.513. [DOI] [PubMed] [Google Scholar]
- Thase ME, Friedman ES, Biggs MM, Wisniewski SR, Trivedi MH, Luther JF, et al. Cognitive therapy versus medication in augmentation and switch strategies as second-step treatments: A STAR*D report. American Journal of Psychiatry. 2007;164:739–752. doi: 10.1176/ajp.2007.164.5.739. [DOI] [PubMed] [Google Scholar]
- Williams JW, Jr, Barrett J, Oxman T, Frank E, Katon W, Sullivan M, et al. Treatment of dysthymia and minor depression in primary care: A randomized controlled trial in older adults. Journal of the American Medical Association. 2000;284:1519–1526. doi: 10.1001/jama.284.12.1519. [DOI] [PubMed] [Google Scholar]