Abstract
OBJECTIVE:
This study aimed to investigate whether previous exercise training could prevent or attenuate acute cardiac alterations after myocardial infarction.
METHODS:
Female rats were submitted to swim training (1 h/day; 5 days/week) or allowed to remain sedentary for 8 weeks. Afterwards, they were randomly assigned to left coronary artery occlusion or sham surgery. After this procedure, the rats remained sedentary for one week until euthanasia. Cardiac structural and functional analyses were performed using Doppler echocardiography. The rats that had a moderate or large infarct size were included in the evaluations. The data (mean ± SEM) were analyzed using a two-way ANOVA model followed by Tukey's post-hoc test.
RESULTS:
After the surgery, no significant difference between the exercise and sedentary groups was observed in the left ventricular infarct sizes (34.58±3.04 vs. 37.59±3.07). In another group of rats evaluated with Evans blue 1 h after myocardial infarction, no siginificant difference in the area at risk was observed between the exercised and sedentary rats (49.73±1.52 vs. 45.48±3.49). The changes in the left ventricular fractional areas for the exercised and sedentary myocardial infarction groups (36±2% and 39±3%, respectively) were smaller than those for the exercise sham surgery (ES, 67±1%) and sedentary sham surgery (SS, 69±2%) groups. The E/A was higher in the sedentary myocardial infarction (4.4±0.3) and exercised myocardial infarction (5.5±0.3) rats than in the SS (2.4±0.1) and ES (2.2±0.1) rats.
CONCLUSION:
Previous swim training of female rats does not attenuate systolic and diastolic function alterations after myocardial infarction induced by left coronary artery occlusion, suggesting that cardioprotection cannot be provided by exercise training in this experimental model.
Keywords: Physical Exercise, Myocardial Infarction, Remodeling, Ventricular Function, Echocardiography
INTRODUCTION
In recent decades, medical and lifestyle therapies, including weight management, physical activity, tobacco cessation, and diet modification, have contributed to the secondary prevention of cardiovascular diseases. Physical exercise (Ex) plays a key role in preserving and promoting health, and it has currently become an important topic in cardiovascular disease control.1-4 Indeed, the incidence of myocardial infarction (MI) is significantly lower in physically active subjects.5 Furthermore, the survival rate of heart attack patients is higher for active individuals than for sedentary ones.5
Previous studies have shown that endurance exercise provides myocardial protection against both ischemia-reperfusion (I-R) injury6-9 and MI in rats.10-12 Ex has been shown to reduce cardiac injury and enhance myocardial recovery from an I-R insult by improving the recovery of left ventricular pressures,6,7 preserving coronary blood flow and reducing oxidative stress in cardiomyocytes.9 Exercise reduces or attenuates cardiac remodeling after an MI13,14 and incrementally improves functional cardiac parameters both in situ14 and in vitro.15
Although the exact molecular and biochemical mechanisms responsible for this protection are not fully understood, it has been postulated that these exercise-induced changes in the myocardium may result from increases in myocardial antioxidant defenses and/or cardiac levels of heat shock protein (HSP).6-8 Experimental MI studies have shown that Ex improves myocardial contractility parameters and autonomic function, increases the gene expression of proteins related to calcium homeostasis, and reduces inflammation in cardiac cells.3,6,16-18
Previous studies on the protective effects of physical exercise in acute MIs were performed using male rats and a coronary occlusion model,10-12 but it is still unclear whether this approach is also valid for female rats. In this study, we evaluated whether previous exercise training can also prevent or attenuate structural and functional cardiac alterations after myocardial infarction in female rats.
MATERIAL AND METHODS
Animals
Forty-two female Wistar rats (∼270 g) were used. The care and use of the animals followed the Principles of Laboratory Animal Care by the National Institutes of Health (National Institutes of Health Publication No., 96-23, Revised 1996) and was approved by the Ethics Committee of the Federal University of São Paulo (protocol number 0341/08).
The rats were distributed into four groups: sedentary sham (SS, n = 13); exercised sham (ES, n = 10); sedentary myocardial infarction (SMI, n = 11); and exercised myocardial infarction (EMI, n = 8). The rats were distributed among plastic cages (5 rats/cage) under a 12-12 h dark–light cycle at 22–23°C and 54–55% air humidity with free access to water and rodent pellet chow (Nuvilab CR1, manufactured by Nuvital, Curitiba, Brazil).
Experimental Protocol
The rats were first submitted to 8 weeks of exercise training or allowed to remain sedentary. Twenty-four hours after the last swimming session, the rats were anesthetized for myocardial infarction induction or sham surgery. Doppler echocardiography was performed under anesthesia at 7 days post-MI to measure the myocardial infarction size MIS, end-diastolic and end-systolic LV areas, fractional area change, peak E and A velocities, and the E/A ratio.
Exercise training protocol
The exercise training was performed in a swimming pool (132 cm in diameter and 80 cm deep) filled with tap water warmed to 32–34°C by a feedback-controlled electric heating coil. The water was maintained in continuous turbulence to provide continuous exercise. To allow adaptation, the swimming was limited to 10 min on the first day and increased by 10 min each day. The rats were eventually subjected to 60 min/day of swimming, 5 days/week for 8 weeks as described by Bocalini et al. (2010).19 In each exercise session, 8 to 10 rats were placed together in the swimming pool. During the exercise period, the age-matched sedentary control group was exposed to similar room noise and handling, but they remained in their cages.
Induction of MI and evaluation of the area at risk
The rats were first submitted to 8 wks of exercise training or allowed to remain sedentary. Twenty-four hours after the last swimming session, the rats were anesthetized for myocardial infarction induction or sham surgery.
An experimental MI was induced as previously described by Antonio et al. (2009)20 Briefly, the rats were anesthetized with ketamine (100 mg/kg, i.p., Dopalen, VetBrand) and xylazine (10 mg/kg, i.p., Anasedan, VetBrand), intubated orotracheally and artificially ventilated (Hugo Basile Rodent Ventilator 683; Harvard Apparatus, Millis, MA, USA). The heart was exteriorized through a left thoracotomy, and the left anterior descending coronary artery was occluded with a 6–0 polypropylene suture. Following the coronary occlusion, the heart was repositioned, the thorax was closed and the orotracheal tube was removed. In the sham-infarcted rats, the same surgical procedures were performed without the coronary ligation.
In another group of animals, an MI was induced under the same anesthesia used previously, and 1 mL of 10% Evans blue dye was injected slowly through a polyethylene tube (PE-50, Clay Adams) inserted into the aorta21 to label the left ventricular tissue that was not subjected to regional ischemia. The dye was passed through the heart for 10 s to ensure uniform tissue distribution. Afterwards, the heart was removed from the perfusion apparatus and a midline transverse section of the heart was performed. Both of the surfaces of each transverse section were photographed. The areas at risk and not at risk were determined using the IMAGE TOOL 3.0 software (UTHSCSA, San Antonio, TX, USA). The total area at risk was expressed as a percentage of the left ventricle.
Doppler echocardiogram
After ketamine- (100 mg/kg i.p., Dopalen, VetBrands) and xylazine-induced (10 mg/kg, i.p., Anasedan, VetBrands) anesthesia, the doppler echocardiography was performed by a single examiner using an HP Sonos 5500 transducer (Philips Medical System, Andover, MA) with 2 cm depth at 12 mHz, as in a previous report.20
Briefly, the 2-dimensional and M-mode images from the parasternal longitudinal, transverse and apical views were obtained and recorded on a 0.5-inch videotape, and the imaging analysis and measurements were performed offline. The MIS was estimated on the basis of the subjective identification of akinesis or dyskinesis. In each echocardiographic transverse plane (basal, mid, and apical), the arc corresponding to the segments with the MI and the total perimeter of the endocardial border (PE) were measured 3 times during end-diastole. The myocardial infarction size was calculated by MIS (%) = MI/PE X 100.
The final MIS of each rat was calculated as the mean of 3 estimates for the MIS. The end-diastolic and end-systolic LV areas, fractional area change, peak E and A velocities, and the E/A ratio were determined according to the American Society of Echocardiography standards.
Statistical analysis
The data were expressed as means ± SEM. A two-way ANOVA model followed by Tukey's post-hoc test was used for comparisons among the groups. The statistical analyses were performed using the Prism software (version 4.0, San Diego, CA, USA). The significance level was set at p < 0.05.
RESULTS
In the MI groups, 25 rats underwent coronary occlusion, 19 survived and 6 died (24%); 5 of these rats were in the sedentary group and one was in the exercised group. The MIS, end-diastolic and end-systolic LV areas, fractional area change, peak E and A velocities, and E/A ratio were measured in the 19 survivors.
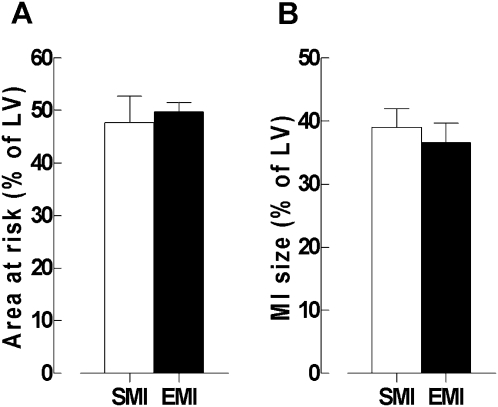
Seven days after surgery, the Doppler echocardiography did not show any significant differences in the MIS between the SMI (39.20±2.85) and EMI (34.59±3.04) groups (Figure 1b). To ensure that the prior exercise did not affect the infarct size, another group of rats that underwent the same protocol had their risk areas assessed using a simpler method. The measurement of the risk area by planimetry also showed no significant difference in the MIS between the SMI (45.48±3.49) and EMI (49.73±1.52) groups (Figures 1a and 2).
Figure 1.
The values are expressed as the mean ± SEM of the sedentary-infarcted (SMI) and exercise-infarcted (EMI) groups. Panel A: The area at risk, as measured by the Evans blue staining. Panel B: The infarct size (% of the left ventricle), as measured by echocardiography (Student's T-test).
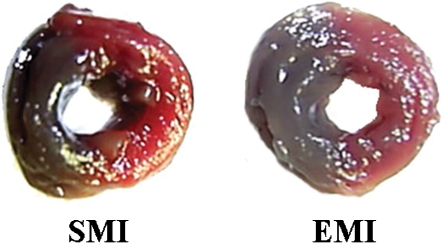
Figure 2.
Images of the midline transverse section of the heart showing the left ventricular staining by the Evans blue dye at one hour after the induction of infarction in the sedentary (SMI) and exercise (EMI) groups. The risk areas are stained red, and viable, perfused myocardium is stained blue.
At the end of the protocol, no significant difference was observed in the body weight (SS, 262±5; SMI, 266±5; ES, 247±4; EMI, 258±10 g). No significant differences were found in the heart rates (SS, 220±5; SMI, 210±8; ES, 207±7; EMI, 234±10) or isovolumic relaxation times in seconds (SS, 0,028±0,001; SMI, 0,038±0,002; ES, 0,031±0,001; EMI, 0,035±0,001), which indicates that the deficit in relaxation was similar among the groups. In the MI rats, the aortic ejection times in seconds (SS, 0,076±0,001; SMI, 0,068±0,003; ES, 0,077±0,002; EMI, 0,069±0,003) and cardiac masses (as assessed by the LV diameters during diastole and systole) were significantly increased (Table 1); however, no differences were observed between the sedentary and exercised rats before the sham surgery.
Table 1.
The structural echocardiography parameters.
| SS (n = 15) | SMI (n = 13) | ES (n = 11) | EMI (n = 8) | |
| Ao (cm) | 0,33±0,009a | 0,33±0,007a | 0,33±0,009a | 0,34±0,007a |
| LVSD (cm) | 0,451±0,017a | 0,683±0,025b | 0,460±0,017a | 0,714±0,019b |
| LVDD (cm) | 0,731±0,017a | 0,844±0,017b | 0,751±0,017a | 0,881±0,011b |
| TAWs (cm) | 0,24±0,011a | 0,13±0,008b | 0,24±0,008a | 016±0,006b |
| TAWd (cm) | 012±0,006a | 010±0,005a | 012±0,004a | 010±0,007a |
| TPWs (cm) | 024±0,011a | 013±0,008b | 024±0,008a | 012±0,006b |
| TPWd (cm) | 0,12±0,004a | 0,13±0,008a | 014±0,007a | 0,13±0,005a |
The values expressed as mean ± SEM. Ao = diameter of the aorta; LVSD = left ventricular systolic diameter; LVDD = left ventricular diastolic diameter; TAWs = left ventricular anterior wall thickness during systole; TAWd = left ventricular anterior wall thickness during diastole; TPWs = posterior wall thickness during systole; TPWd = posterior wall thickness during diastole, as assessed by echocardiography in the sedentary sham (SS), sedentary infarcted (SMI), exercised sham (ES) and exercised infarcted (EMI) groups at one week after the MI.
The different letters represent statistically significant differences (P<0.05) in a two-way ANOVA model followed by Tukey's post-hoc test.
Because the anterior wall thickness during systole is considered a measure of remodeling and chamber dilation, we also evaluated this variable during the relaxation phase. Nevertheless, there was no statistically significant difference between the EMI and SMI groups, which shows that prior exercise did not produce beneficial structural alterations (Table 1).
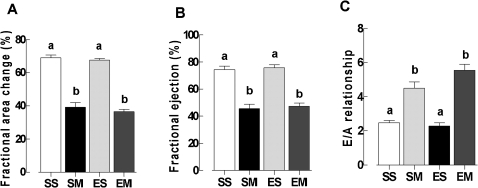
The systolic functional parameters were similar between the EMI and SMI rats at one week after MI surgery, indicating that prior exercise did not improve cardiac output in these animals. This finding is likely explained by the infarct sizes in the EMI group, which were roughly equal to those of the sedentary group. Both the fractional area change and the fractional ejection did not differ significantly between the infarcted groups (Figures 3a and 3b).
Figure 3.
The echocardiographic values are expressed as the mean ± SEM for the sedentary sham (SS), sedentary infarcted (SMI), exercised sham (ES) and exercised infarcted (EMI) groups. Panel A: The fractional area change. Panel B: The fractional ejection. Panel C: The E/A relationship. The different letters represent statistical significant differences (P<0.05) in a two-way ANOVA model followed by Tukey's post-hoc test.
The measures of diastolic function and atrial filling (E wave, A wave and E/A ratio) were not significantly different among groups (Figure 3c).
DISCUSSION
Our results demonstrated that exercise training performed prior to coronary occlusion surgery did not confer cardioprotection, as evaluated by Doppler echocardiography. The echocardiographic measures have already been validated by previous studies and were considered acceptable for measuring heart parameters.22,23 A previous study in our laboratory has demonstrated that in infarct size measurements assessed by echocardiography a week after coronary occlusion, the necrotic heart medial area is related to the infarct size as measured by tetrazolium staining.24
The lack of cardioprotection in the exercised group was most likely explained by the training having no significant effect on the infarct size. As a result, the measurements obtained after surgery were similar to those of the sedentary group with myocardial infarction. Most studies have focused on the effect of exercise training on cardiac alterations in the chronic phase (4 wks weeks after MI) and have shown beneficial remodeling results.14,15,25 Our data was obtained in the acute phase of infarction and after one week of detraining, and no physiological hypertrophy was observed in the ES group.
Many ischemia and reperfusion studies using isolated hearts have shown that exercise training prior to surgery decreases infarct size.26,27 Brown et al. (2007) performed a review of these studies to demonstrate how exercise training prior to surgical procedures affects transitory ischemia by decreasing the infarct size. By contrast, our study did not show that previous exercise training attenuates the infarct size, possibly because permanent coronary artery occlusion may produce greater damage to the heart tissue than transitory ischemia. A few recent studies have demonstrated that exercise training permanently decreases the infarct size in rats in vivo.11,12
One difference between the Freimann et al. (2005) study and the current study is the gender of the rats used. We used female rats, whereas Freeman et al. used males. It is known that there are differences relating to infarction and development between the genders.29,30
The majority of the data examining exercise-acquired tolerance to ischemic injury in rats comes from male animals. The reason for this predominance is that the pathological mechanisms in males, in contrast to those in females, are not influenced by fluctuations in hormonal activity.31 Exercise training before infarction surgery improves mortality and infarct healing in mice of both genders.32 Other physical training benefits include improved cardiac function, attenuated calcium homeostasis dysfunction and improved autonomic function.15,22,33 Nevertheless, it has not been shown that previous exercise training in this experimental model improves infarct healing in female rats. It is still unclear whether hormonal differences between the genders affect cardiac function after myocardial infarction in rats previously submitted to exercise. Therefore, the molecular mechanisms that may explain the differences between the findings of the present study on female rats and those of other studies on male rats require further investigation.
There are other studies that have shown no cardioprotection in exercised female rats, in contrast to the results for male rats and for female rats lacking ovaries. Among the many possible mechanisms for this divergence are the estrogen inhibition of HSP70 protein expression, the attenuation of end-diastolic pressure and protein normalization related to calcium homeostasis.34,35
Some of the echocardiographic measurements of hypertrophy were not different between the exercised and sedentary rats. Furthermore, the exercised sham surgery group did not have any hypertrophy after the one-week detraining period.36
Myocardial infarction has many consequences in its acute phase (including cardiac hypertrophy, cavity dilation, cicatrization and thickening in the infracted region, gene expression alterations, inflammatory changes, oxidative stress and cellular death) that result in cardiac remodeling, which leads to a change in the shape and function of the myocardium.18,37,38
Other contractile functional parameters, such as the fractional area change and ejection fraction, are decreased in ischemia and reperfusion studies. Our study, however, did not identify differences between the exercised and sedentary groups in these parameters.
In contrast to previous post-infarction healing14 and ischemia and reperfusion studies,28 ventricular relaxation in our study was impaired in both the exercised and sedentary groups after the infarction.
Therefore, exercise training in our female rats prior to myocardial infarction did not reduce the infarct size and was did not provide cardioprotection. Consequently, the systolic and diastolic function remained impaired one week after the infarction.
REFERENCES
- 1.Shepard RJ, Balady GR. Exercise as cardiovascular therapy. Cir. 1999;99:963–72. doi: 10.1161/01.cir.99.7.963. [DOI] [PubMed] [Google Scholar]
- 2.Scott WA. Maximizing performance and the prevention of injuries in competitive athletes. Curr Sports Med Rep. 2002;1:184–90. doi: 10.1249/00149619-200206000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Wisloff U, Ellingsen O, Kemi OJ. High-Intensity interval training to maximize cardiac benefits of exercise training. Exer Sport Sci Rev. 2009;37:139–46. doi: 10.1097/JES.0b013e3181aa65fc. 10.1097/JES.0b013e3181aa65fc [DOI] [PubMed] [Google Scholar]
- 4.Hall SL, Lorec T. Secondary prevention of coronary artery disease. Am Fam Physician. 2010;81:289–96. [PubMed] [Google Scholar]
- 5.Hull SS, Vanoli PB, Adamson RL, Foreman RD, Shwartz PJ. Exercise training confers anticipatory protection form sudden death during acute myocardial ischemia. Circ. 1994;89:548–52. doi: 10.1161/01.cir.89.2.548. [DOI] [PubMed] [Google Scholar]
- 6.Powers SK, Demirel HA, Vincent HK, Coombes JS, Naito H, Hamilton KL, et al. Exercise training improves myocardial tolerance to in vivo ischemia-reperfusion in the rat. Am J Physiol Regul Integr Comp Physiol. 1998;275:R1468–R1477. doi: 10.1152/ajpregu.1998.275.5.R1468. [DOI] [PubMed] [Google Scholar]
- 7.Demirel HA, Powers SK, Zergeroglu MA, Shanely RA, Hamilton K, Coombes J, et al. Short-term exercise improves myocardial tolerance to in vivo ischemia-reperfusion in the rat. J Appl Physiol. 2001;91:2205–12. doi: 10.1152/jappl.2001.91.5.2205. [DOI] [PubMed] [Google Scholar]
- 8.Hamilton KL, Powers SK, Sugiura T, Kim S, Lennon S, Tumer N, et al. Short-term exercise training cam improve myocardial tolerance to I/R elevation in heat shock proteins. Am J Physiol Heart Circ Physiol. 2001;281:H1346–H1352. doi: 10.1152/ajpheart.2001.281.3.H1346. [DOI] [PubMed] [Google Scholar]
- 9.Brown DA, Moore RL. Perspectives in innate and acquired cardioprotection: cardioprotection acquired through exercise. J Appl Physiol. 2007;103:1894–9. doi: 10.1152/japplphysiol.00464.2007. 10.1152/japplphysiol.00464.2007 [DOI] [PubMed] [Google Scholar]
- 10.McElroy CL, Gissen SA, Fishbein MC. Exercise induced reduction in myocardial infarct size after coronary artery occlusion in the rat. Circ. 1978;57:958–62. doi: 10.1161/01.cir.57.5.958. [DOI] [PubMed] [Google Scholar]
- 11.Freimann S, Scheinowitz M, Yekutieli D, Feinberg MS, Eldar M, Kessler-Icekson G. Prior Exercise training improves the outcome of acute myocardial infarction in the rat. J Am Coll Cardiol. 2005;45:931–8. doi: 10.1016/j.jacc.2004.11.052. 10.1016/j.jacc.2004.11.052 [DOI] [PubMed] [Google Scholar]
- 12.Dayan A, Feinberg MS, Holbova R, Deshet N, Scheinowitz M. Swimming exercise training prior to acute myocardial infarction attenuates left ventricular remodeling and improves left ventricular function in rats. Ann Clin Lab Sci. 2005;35:73–8. [PubMed] [Google Scholar]
- 13.Orestein TL, Parker TG, Butany JW, Goodman JM, Dawood F, Wen WH, et al. Favorable left ventricular remodeling following large myocardial infarction by exercise training: effect on ventricular mofphology and gene expression. J Clin Invest. 1995;96:858–66. doi: 10.1172/JCI118132. 10.1172/JCI118132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Portes LA, Saraiva RM, Santos AA, Tucci PJ. Swimming training attenuates remodeling, contractile dysfunction and congestive heart failure in rats with moderate and large myocardial infarctions. Clin Exp Pharmacol Physiol. 2008;36:394–9. doi: 10.1111/j.1440-1681.2008.05070.x. 10.1111/j.1440-1681.2008.05070.x [DOI] [PubMed] [Google Scholar]
- 15.Zhang LQ, Zhang XQ, Musch TI, Moore RL, Cheung JY. Sprint training restore normal contratility in postinfarction rat myocytes. J Appl Physiol. 2000;89:1099–105. doi: 10.1152/jappl.2000.89.3.1099. [DOI] [PubMed] [Google Scholar]
- 16.Ignarro LJ, Balestrieri ML, Napoli C. Nutrition, physical activity, and cardiovascular disease: An update. Cardiovasc Res. 2007;73:326–40. doi: 10.1016/j.cardiores.2006.06.030. 10.1016/j.cardiores.2006.06.030 [DOI] [PubMed] [Google Scholar]
- 17.Marini M, Lapalombella R, Margonato V, Ronchi R, Samaja M, Scapin C, et al. Mild Exercise training, cardioprotection and stress genes profile. Eur J Appl Physiol. 2007;99:503–10. doi: 10.1007/s00421-006-0369-4. 10.1007/s00421-006-0369-4 [DOI] [PubMed] [Google Scholar]
- 18.Frantz S, Bauersachs J, Ertl G. Post-infarct remodeling: contribution of would healing and inflammation. Cardiovasc Res. 2009;81:474–81. doi: 10.1093/cvr/cvn292. 10.1093/cvr/cvn292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bocalini DS, Carvalho EV, Sousa AFM, Levy RF, Tucci PJ. Exercise training-induced enhancement in myocardial mechanics is lost after 2 weeks of detraining in rats. Eur J Appl Physiol. 2010;109:909–14. doi: 10.1007/s00421-010-1406-x. 10.1007/s00421-010-1406-x [DOI] [PubMed] [Google Scholar]
- 20.Antonio EL, Santos AA, Araujo SRR, Bocalini DS, Dos Santos L, Fenelon G, et al. Left ventricle radio-frequency ablation in the rat: A new model of heart failure due to myocardial infarction homogeneous in size and low in mortality. J Card Fail. 2009;15:540–8. doi: 10.1016/j.cardfail.2009.01.007. 10.1016/j.cardfail.2009.01.007 [DOI] [PubMed] [Google Scholar]
- 21.Fliss H, Gattinger D. Apoptosis in ischemia and reperfusion rat myocardium. Circ Res. 1996;79:949–56. doi: 10.1161/01.res.79.5.949. [DOI] [PubMed] [Google Scholar]
- 22.Reffelmann T, Kloner RA. Transthoracic echocardiography in rats. Evalution of commonly used indices of left ventricular dimensions, contractile performance, and hypertrophy in a genetic model of hypertrophic heart failure (SHHF-Mcc-facp-Rats) in comparison with Wistar rats during aging. Basic Res Cardiol. 2003;98:275–84. doi: 10.1007/s00395-003-0401-3. [DOI] [PubMed] [Google Scholar]
- 23.Nozawa E, Kanashiro RM, Murad N, Carvalho AC, Cravo SL, Campos O, et al. Performance of two-dimensional Doppler chocardiography for the assessment of infarct size and left ventricular function in rats. Braz J Med Biol Res. 2006;39:687–95. doi: 10.1590/s0100-879x2006000500016. 10.1590/S0100-879X2006000500016 [DOI] [PubMed] [Google Scholar]
- 24.dos Santos L, Mello AF, Antonio EL, Tucci PJ. Determination of myocardial infarction size in rats by echocardiography and tetrazolium staining: correlation, agreements, and simplifications. Braz J Med Biol Res. 2008;41:199–201. doi: 10.1590/s0100-879x2008005000007. 10.1590/S0100-879X2008005000007 [DOI] [PubMed] [Google Scholar]
- 25.Wisloff U, Loennech JP, Curri S, Smith GL, Ellingsen O. Aerobic exercise reduced cardiomyocyte hypertrophy and increases contratility, Ca2+ sensitivity and SERCA-2 in rat after myocardial infarction. Cardiovasc Res. 2002;54:162–74. doi: 10.1016/s0008-6363(01)00565-x. 10.1016/S0008-6363(01)00565-X [DOI] [PubMed] [Google Scholar]
- 26.Bowles DK, Farrar RP, Starnes JW. Exercise training improves cardiac function after ischemia in the isolated, working rat heart. Am J Physiol. 1992;263:H804–809. doi: 10.1152/ajpheart.1992.263.3.H804. [DOI] [PubMed] [Google Scholar]
- 27.Yamashita N, Baxter GF, Yellon DM. Exercise directly enhances myocardial tolerance to ischaemia-reperfusion injury in the rat through a protein kinase C mediated mechanism. Heart. 2001;85:331–6. doi: 10.1136/heart.85.3.331. 10.1136/heart.85.3.331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown DA, Moore RL. Perspectives in innate and acquired cardioprotection: cardioprotection acquired through exercise. J Appl Physiol. 2007;103:1894–9. doi: 10.1152/japplphysiol.00464.2007. 10.1152/japplphysiol.00464.2007 [DOI] [PubMed] [Google Scholar]
- 29.Litwin SE, Katz SE, Litwin CM, Morgan JP, Douglas PS. Gender differences in postinfarction left ventricular remodeling. Cardiol. 1999;91:173–83. doi: 10.1159/000006906. 10.1159/000006906 [DOI] [PubMed] [Google Scholar]
- 30.Ostadal B, Netuka I, Maly J, Besik J, Ostadalova I. Gender differences in cardiac ischemic injury and protection - experimental aspects. Exp Biol Med. 2009;234:1011–9. doi: 10.3181/0812-MR-362. 10.3181/0812-MR-362 [DOI] [PubMed] [Google Scholar]
- 31.Leinwand LA. Sex is a potent modifier of the cardiovascular system. J Clin Invest. 2003;112:302–7. doi: 10.1172/JCI19429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.De Waard MC, Duncker DJ. Prior exercise improves survival, infarct healing, and left ventricular function after myocardial infarction. J Appl Physiol. 2008;107:928–36. doi: 10.1152/japplphysiol.91281.2008. 10.1152/japplphysiol.91281.2008 [DOI] [PubMed] [Google Scholar]
- 33.Medeiros A, Rolim NPL, Oliveira RSF, Rosa KT, Mattos KC, Casarini DE, et al. Exercise training delays cardiac dysfunction and prevents calcium handling abnormalities in sympathetic hyperactivity-induced heart failure mice. J Appl Physiol. 2008;104:103–9. doi: 10.1152/japplphysiol.00493.2007. 10.1152/japplphysiol.00493.2007 [DOI] [PubMed] [Google Scholar]
- 34.Parro Z, Haist JV, Karmazyn M, Noble EG. Exercise improves postischemic cardiac function in males but not in females: consequences of a novel sex specific heat shock protein 70 response. Circ Res. 2002;90:911–7. doi: 10.1161/01.res.0000016963.43856.b1. 10.1161/01.RES.0000016963.43856.B1 [DOI] [PubMed] [Google Scholar]
- 35.Bupha-Intr T, Laosiripisan J, Wattanapermpool J. Moderate intensity of regular exercise improves cardiac SR Ca 2+ uptake activity in ovariectomized rats. J Appl Physiol. 2009;107:1105–12. doi: 10.1152/japplphysiol.00407.2009. 10.1152/japplphysiol.00407.2009 [DOI] [PubMed] [Google Scholar]
- 36.Haram PM, Adams V, Kemi JO, Brubakk AO, Hambrecht R, Ellingsen O, et al. Time-course of endothelial adaptation following acute and regular exercise. Eur J Cardiovasc Prev Rehab. 2006;13:585–91. doi: 10.1097/01.hjr.0000198920.57685.76. 10.1097/01.hjr.0000198920.57685.76 [DOI] [PubMed] [Google Scholar]
- 37.Fedak PWM, Verma S, Weisei RD, Skrtic M, Li R. Cardiac remodeling and failure from molecules to man (Part I) Cardiovasc Pathol. 2005;14:1–11. doi: 10.1016/j.carpath.2004.12.002. 10.1016/j.carpath.2004.12.002 [DOI] [PubMed] [Google Scholar]
- 38.Holmes JW, Borg TK, Cowell JW. Structure and mechanics of healing myocardial infarcts. Annu Rev Biomed Eng. 2005;7:223–53. doi: 10.1146/annurev.bioeng.7.060804.100453. 10.1146/annurev.bioeng.7.060804.100453 [DOI] [PubMed] [Google Scholar]