Abstract
Objective
Nurses (patient-advocates) and technicians (member of colonoscopy team) collected data on patient discomfort and evaluated various options of sedation or no sedation associated with the air and water methods for performing colonoscopy.
Method
Veterans participated in studies comparing air and water method colonoscopy. Options using minimal or on demand sedation were evaluated.
Results
Compared with the air method, the water method was associated with significantly lower pain scores, higher patient satisfaction ratings and shorter recovery times. On demand sedation was comparable to routine sedation when the water method was used. Patients prefer to be in control of when their medications would be administered during colonoscopy.
Conclusion
Evaluations by nurses (patient advocates) and technicians (member of colonoscopy team) with experience in assisting patients undergoing colonoscopy using the various options indicate the following. In settings without access to sedation, the water method is ideal for unsedated colonoscopy or extended flexible sigmoidoscopy for screening. Otherwise, the water method and on demand sedation is the most credible combination of options for patient care.
Key words: screening colonoscopy, colonoscopy pain, air method, water method, routine sedation, minimal sedation, on demand sedation, unsedated, extended flexible sigmoidoscopy
Nurses are patient advocates1. In the case of colonoscopy, nurses are known to be more accurate in assessing patient discomfort2. To ensure patient comfort we monitor pain scores during colonoscopy3–8. To evaluate patient satisfaction we query them about their overall experience and their willingness to repeat the procedure using the same technique with or without different options of sedation3–8. To determine the staff evaluation of the various options tried, we surveyed the nurses and the Gastroenterology technicians assisting the colonoscopy procedures9.
From the nurse perspective3–9, the benefits of not using sedation are as follows. There is no need for a sedation nurse. No sedation eliminates possible medication-related complications such as respiratory depression or significant cardiac rhythm changes10. There is rapid patient turn around due to minimized recovery time. The amnesic effects of sedation11 is obviated which facilitates discharge planning. There is less manpower demand because the overall service is more efficient.
Table 1 shows the mean pain scores at different colon segments in three separate studies carried out at the Sacramento VA Medical Center in the past several years, comparing the air and the water method. Pain score of 0 was no pain and 10 was most severe pain. The first study6 was performed by attending staff that employed minimal intravenous sedation (Fentanyl 25 mg/Versed 1 mg) + Benadryl 50 mg. Additional pain medications were given based on the monitoring procedures and pain scores. The second study7 was performed by supervised 2nd and 3rd year fellows using the same design as the first. The third study8 was performed by attending staff that employed the on demand sedation approach. In all three studies, the water method resulted in significantly lower mean pain scores particularly in the transverse and ascending colon during the insertion phase.
Table 1.
Air vs. water method - mean pain scores
| Study | Method | Number of patients | Rectum | Sigmoid | Descending colon | Transverse colon | Ascending colon | Cecum |
| 1 | Air | 28 | 0 | 1 | 2 | 4 | 4 | 2 |
| Water | 28 | 1 | 1 | 2 | 3* | 1* | 1 | |
| 2 | Air | 31 | 1 | 3 | 4 | 4 | 5 | 2 |
| Water | 31 | 0 | 1 | 2 | 3* | 3* | 2 | |
| 3 | Air | 50 | 0 | 1 | 2 | 3 | 3 | 2 |
| Water | 50 | 0 | 1 | 1 | 2* | 2* | 1 |
Data are mean pain scores. Pain score: 0 = none, 10 most severe.
vs. respective air method, p < 0.05, Student t test.
Study 1: Minimal sedation - Attending (5/08–7/08); Study 2: Minimal sedation - Trainees (11/08–2/09); Study 3: On demand sedation - Attending 4/09–11/09.
The advantages of on demand sedation include elimination of coercion. Patient can watch the procedure, ask questions about the findings and communicate with the endoscopist if they have not received sedation medications. The time for pre-medication is obviated. The procedure and recovery times are shortened if no sedation is given. The disadvantage is somewhat prolonged procedure time if sedation is given during colonoscopy.
Figure 1 compares patient satisfaction immediately after colonoscopy and 24 hours later. Rating scale used are 0 which stands for not satisfied and 10 for very satisfied. The bars depict the mean for the patients examined with the air method and the water method. The mean satisfaction scores were higher in the water group than the air group in all three studies. It also shows that the 3rd study which is the on demand group have a higher patient satisfaction rating over all.
Figure 1.
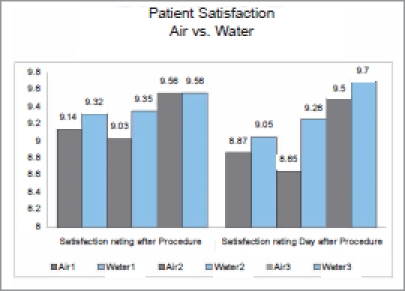
Patient satisfaction scores. Study 1: Minimal sedation - Attending (5/08–7/08); Study 2: Minimal sedation - Trainees (11/08–2/09); Study 3: On demand sedation - Attending 4/09–11/09. Data are mean pain scores. Pain score: 0 = none, 10 most severe.
Figure 2 shows the results of a phone survey of the 100 patients who participated in the on demand sedation study. The participants were asked if they preferred on demand sedation (patient controlled-sedation) during a colonoscopy. 82% answer yes and think it is a benefit to be in control of the use of drugs during the procedure. Out of the 82% or 82 patients who answered “YES”, 66 patients who preferred on demand sedation did not get sedation during colonoscopy procedure, 12 patients who also preferred on demand sedation requested medication during colonoscopy. These previously unpublished results indicate that patients prefer to be in control of their drugs and want to be given the option to choose even for those patients who requested sedation during colonoscopy.
Figure 2.
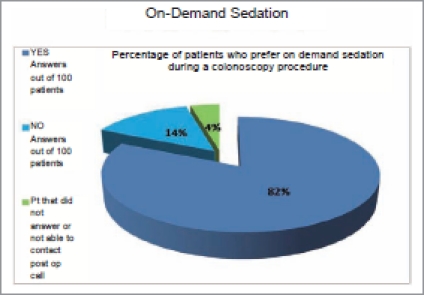
Percentage of patients who prefer on demand sedation
Table 2 shows the data of a survey we conducted amongst the nurses and technicians. Each was asked to rate the various combinations of air or water with each of the sedation options. They responded to 5 questions using a scale from 1 to 10 (10 being most positive). The 5 questions are shown in the second column. The individual scores were summed to give a total, the credibility score, shown in the bottom row. The data are shown as mean ± SD. Table 2 shows that for the unsedated patients, the water method was rated significantly higher. Table 3 shows staff evaluation regarding the option of on demand sedation during a colonoscopy procedure. The water method was rated significantly higher compared to the air group. Table 4 shows that even for the sedated patients the water method was rated significantly higher compared to the sedated air group which is the usual practice in colonoscopy procedures. When the results of the sedated (Table 4) and the sedation on demand (Table 3) patients examined by the water method were arranged side by side, the ratings were almost indistinguishable. The implication is that on demand sedation is just as good as routine sedation when the water method is employed.
Table 2.
Gastroenterology nurses and technicians survey — unsedated air vs. water colonoscopy
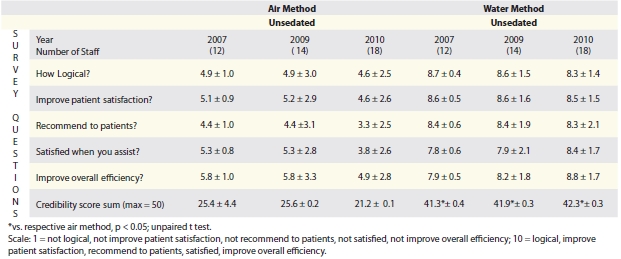 |
Table 3.
Gastroenterology nurses and technicians survey — on demand sedation air vs. water colonoscopy
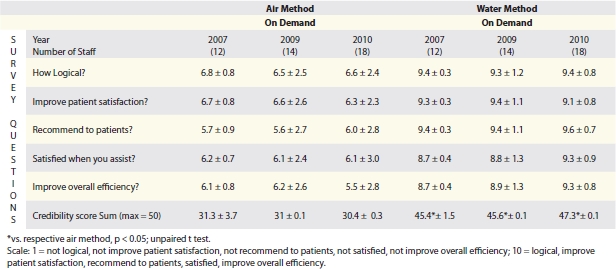 |
Table 4.
Gastroenterology nurses and technicians survey - sedated air vs. water colonoscopy
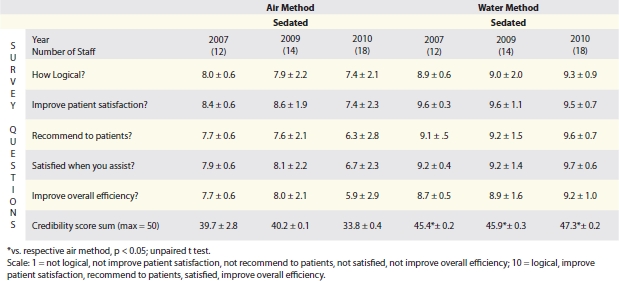 |
Figure 3 shows the mean on-site recovery times for the three studies. We have definitely observed a shorter recovery time whenever the water method was used, due to less time required for passing air, and less pain medications used.
Figure 3.
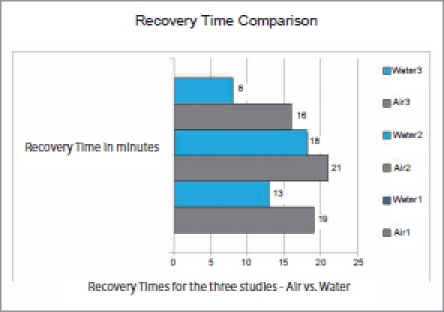
On-site recovery times
In summary in all 3 studies the water method is associated with significantly lower pain scores, higher patient satisfaction ratings and shorter recovery times. The water method is a better option than air method colonoscopy. On demand sedation is comparable to routine sedation when the water method is used. Patients prefer to be in control of when their medications would be administered during colonoscopy. We conclude that evaluations by nurses and technicians with experience in assisting patients undergoing colonoscopy using the various options indicate the water method combined with on demand sedation is the most acceptable or credible combination of options for patient care.
We have stopped performing routine screening flexible sigmoidoscopy in our institution but our physicians now offer patients scheduled unsedated colonoscopy12 - a form of extended flexible sigmoidoscopy13. The patient will undergo the screening procedure without medication until the cecum is reached or the procedure will stop if the patient encounters significant pain or discomfort. The extrapolation of our observations in this context of extended flexible sigmoidoscopy (e.g. in the inner city or rural settings where sedated colonoscopy is often unavailable) especially when the water method is used suggest that a good proportion of patients can complete the extended flexible sigmoidoscopy without medication and as a result a more complete screening procedure. Similar to giving patients the control over their medication needs, we observed that patient education which includes clear explanation, proper motivation and showing concern for the patients help to alleviate anxiety which is the key to a successful unsedated procedure.
Acknowledgement
The study is support in part by the C.W. Law Research Fund (JWL), Research support from the VANCHCS and VAGLAHS, and in part by an ACG Clinical Research Award (FWL). The authors acknowledge all the staff at the Sacramento VA Endoscopy unit for their participation in the questionnaire surveys.
Abbreviations
- IRB
Institution Review Board
- SD
standard deviation
- VAMC
Veterans Affairs Medical Center
Footnotes
Previously published online: www.landesbioscience.com/journals/jig
The authors have no conflict of interests to disclose relevant to this study.
Presented at the Colorectal Cancer Screening Symposium - New Approaches and Patient Perspective, March 20, 2010, Sacramento VAMC, Mather, CA.
References
- 1.Beyea SC. Patient advocacy--nurses keeping patients safe. AORN J. 2005;81:1046–1047. doi: 10.1016/s0001-2092(06)60471-7. [DOI] [PubMed] [Google Scholar]
- 2.Ramakrishnan S, Yiannakou JY, Ellis WR, Bain IM. Assessment of patient pain at colonoscopy: are nurses better than endoscopists? J R Soc Med. 2004;97:432–433. doi: 10.1258/jrsm.97.9.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leung JW, Mann S, Leung FW. Option for screening colonoscopy without sedation — a pilot study in United States veterans. Alimen Pharmacol Ther. 2007;26:627–631. doi: 10.1111/j.1365-2036.2007.03404.x. [DOI] [PubMed] [Google Scholar]
- 4.Leung FW, Mann SK, Salera R, Toomsen L, Cabrera H, Prather D, et al. Options for screening colonoscopy without sedation — sequel to a pilot study in United States veterans. Gastrointest Endosc. 2008;67:712–717. doi: 10.1016/j.gie.2007.10.028. [DOI] [PubMed] [Google Scholar]
- 5.Leung JW, Salera R, Toomsen L, Mann S, Leung FW. Pilot feasibility study of the method of water infusion without air insufflation in sedated colonoscopy. Dig Dis Sci. 2009;54:1997–2001. doi: 10.1007/s10620-008-0576-4. [DOI] [PubMed] [Google Scholar]
- 6.Leung JW, Mann SK, Siao-Salera R, Ransibrahmanakul K, Lim B, Cabrera H, et al. A randomized, controlled comparison of warm water infusion in lieu of air insufflation versus air insufflation for aiding colonoscopy insertion in sedated patients undergoing colorectal cancer screening and surveillance. Gastrointest Endosc. 2009;70:505–510. doi: 10.1016/j.gie.2008.12.253. [DOI] [PubMed] [Google Scholar]
- 7.Ransibrahmanakul K, Leung JW, Mann SK, Siao-Salera R, Lim BS, Hasyagar C, et al. Comparative effectiveness of water vs. air methods in minimal sedation colonoscopy performed by supervised trainees in the US -- a RCT. Am J Clin Med. 2010;7:113–118. [Google Scholar]
- 8.Leung JW, Mann SK, Siao-Salera RM, Ransibrahmanakul K, Lim BS, Canete W, et al. A randomized, controlled trial to confirm the beneficial effects of the water method on U.S. veterans undergoing colonoscopy with the option of on-demand sedation. Gastrointest Endosc. 2011;73:103–110. doi: 10.1016/j.gie.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 9.Siao-Salera R, Cabrera H, Leung JW, Prather D, Toomsen L, Mann SK, et al. Nurses who assist in colonoscopy on-demand sedation and a novel technique of water infusion without air insufflation evaluate the combination as a credible option for patient care. Am J Gastroenterol. 2007;102:S249–S271. [Google Scholar]
- 10.Ko CW, Riffle S, Michaels L, Morris C, Holub J, Shapiro JA, et al. Serious Complications within 30 days of screening and surveillance colonoscopy are uncommon. Clin Gastroenterol Hepatol. 2010;8:166–173. doi: 10.1016/j.cgh.2009.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hayes A, Buffum M. Educating patients after conscious sedation for gastrointestinal procedures. Gastroenterol Nurs. 2001;24:54–57. doi: 10.1097/00001610-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Leung FW, Harker JO, Jackson G, Okamoto KE, Behbahani OM, Jamgotchian NJ, et al. A proof-of-principle, prospective, randomized, controlled trial demonstrating improved outcomes in scheduled unsedated colonoscopy by the water method. Gastrointest Endosc. 2010;72:693–700. doi: 10.1016/j.gie.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 13.Lee JG, Lum D, Urayama S, Mann S, Saavedra S, Vigil H, et al. Extended flexible sigmoidoscopy performed by colonoscopists for colorectal cancer screening: a pilot study. Aliment Pharmacol Ther. 2006;23:945–951. doi: 10.1111/j.1365-2036.2006.02838.x. [DOI] [PubMed] [Google Scholar]


