Abstract
Usedated colonoscopy is routinely available in many parts of the world. In the US, only educated professionals appear to be knowledgeable enough to request the unsedated option. Colonoscopists have also been willing to perform unsedated colonoscopy when a patient presents without an escort after undergoing bowel purge preparation. While the actual side-effects of sedation are minimal, the escort requirement and time burden of sedation are barriers to the uptake of screening colonoscopy in the US. The recent trend of deep sedation with propofol for screening colonoscopy increases the efficiency of the colonoscopists at significant costs (e.g. anesthetist reimbursement). The options of as needed and on demand sedation permit patients to complete colonoscopy without sedation. The latter appears to be potentially less coercive. Nurses with experience in the unsedated options recognize the benefit of the quick turn-around of the examination room and shortened occupancy of the recovery area. Discharge planning can be optimized due to absence of amnesia. Patients completing unsedated colonoscopy have given their endorsement of the options. Pain and discomfort continue to limit the success rate of cecal intubation to about 80%. A recently described water method (warm water infusion in lieu of air insufflation combined with removal of all residual colonic air by suction and residual feces by water exchange) has the potential of decreasing procedural discomfort and enhancing cecal intubation in unsedated colonoscopy. The availability of the novel water method assures colonoscopists that high success rate of cecal intubation can be achieved in the unsedated patients.
Key words: colonoscopy, unsedated, sedationless, water method
Unsedated colonoscopy is available on a routine basis in many parts of the world.1 This paper will discuss the components of patient time burden of sedation,2 tabulate the extent and significance of sedation-related complications3 and review how various options without routine sedation impact these events in the context of colorectal cancer screening and surveillance. In the end we shall address the question in the title of this manuscript if there is a place for sedationless (unsedated) colonoscopy.
An interesting historical note is that colonoscopy was initially developed as an unsedated procedure and procedural difficulty led to the introduction of sedation.4–6 Clearly in less skilled hands sedation did enhance cecal intubation.7 In the US, the standard practice of sedation in diagnostic examination and therapeutic procedures was extended to screening colonoscopy.8
A recent report in the primary care literature, however, suggested that sedation may be a barrier to colonoscopy screening.9 The need for transportation was reported by 14% of the patients as a reason for non-adherence to recommended screening colonoscopy. The need to take time off work after sedation was also an important negative incentive. On the provider side, some rural practitioners have less access to sedation.
The time burden of screening and surveillance colonoscopy was evaluated in detail in 110 patients at one university endoscopy center.2 89% of patients underwent PEG bowel preparation; and all received sedation, a combination of midazolam and fentanyl. Each subject completed a detailed diary of the time for all the events beginning with the start of bowel preparation and ending with being able to resume normal activities. The mean age of the cohort was 62 years; 57% were female, 85% were white; and 90% were insured. A total of 39.5 hours were spent for colonoscopy. After colonoscopy, the time to resume normal activities was 15.8 hrs. 57% lose ≥1 day of work.
Recently, Dr. Ko at the University of Washington published a report on complications after screening or surveillance colonoscopy in the U.S. based on patients in the Clinical Outcomes Research Initiative database.3 Of 21,375 patient reports, sedation-related complications during colonoscopy were described in 12.9/1000 patients (1.3%). The most common immediate complication was respiratory depression occurring in 7.5/1000. Immediate cardiovascular complications such as hypotension and bradycardia occurred in 4.9/1000. These were self-limited but some patients (2.9/1000) did require medications (e.g. atropine, flumazenil, naloxone) for rescue. Five patients were hospitalized for observation (abdominal pain, prolonged sedation)
Over the years, unsedated colonoscopy has acquired a negative image.10–12 Clinicians and investigators willing to provide the option have coined a number of terms to lessen the negative impact: sedation-free,13–16 medication-free17 and sedationless18,19 colonoscopy. A comparison of sedated and unsedated colonoscopy is shown in Table 1.
Table 1.
Comparison of sedated and unsedated colonoscopy
| Attributes of Scheduled Options | Sedated | Unsedated |
| Availability | Usual in US | Not usual in US |
| Risks: hypotension, hypoxia, etc. | Very small | None |
| Success rate | ∼ 90% | 80 to 90% |
| Purge preparation | Yes | Yes |
| Escort | Mandatory | Not required |
| Drive a car after colonoscopy | No | Yes |
| Discomfort reduced by medication | Highly likely | No |
| Remember discomfort | No | Yes |
| Remember discussion | No | Yes |
| Need monitoring after colonoscopy | Yes | No |
| Activity restriction after colonoscopy | Yes | No |
| May require repeat with sedation | NA | Incomplete |
Adapted from reference 43: Leung FW. Promoting informed choice of unsedated colonoscopy - patient-centered care for a subgroup of U.S. veterans. Dig Dis Sci 2008;53(11):2955–9.
At a recent conference on new approaches to colorectal cancer screening held at the Sacramento Veterans Affairs Medical Center in California, the following framework was presented to set the stage for discussions of the various options of colonoscopy without routine sedation (Table 2).29 The options can be scheduled or unscheduled. The only unscheduled one is unsedated colonoscopy offered to patients who drink the purge solution and arrives without an escort and do not mind having the colonoscopy done without sedation. In VA21 and community22 practice settings this option has been provided to 1–2% of colonoscopy patients. Scheduled options include deep sedation, conscious sedation and unsedated colonoscopy.
Table 2.
Options of colonoscopy with and without routine sedation
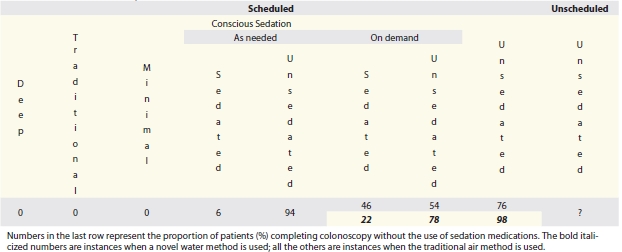 |
There is a definite growing trend to embrace deep sedation with propofol which can increase the colonoscopists' productivity by at least 2/3.23 If an anesthesiologist is involved, however, the cost for the colonoscopy can go up. The scheduled, unsedated option is usually requested by the patients who are educated professionals (e.g. a busy endoscopist who wants to return to work after colonoscopy). In one University practice setting, this group constituted 7% of all comers.24 The vast majority of Americans undergoing colonoscopy receive traditional sedation (combination of a narcotic pain medication for pain control and a benzodiazepine which promotes amnesia of any real discomfort). The practice of minimal sedation has been proposed.25,26 Patients receive less than the full amount at the outset and receive additional medications if they experience discomfort.
Conscious sedation can also be divided into as needed or on demand sedation. Sedation as needed24 is controlled by the colonoscopist and on demand sedation27,28 by the patients. As needed or on demand sedation starts out without pre-medications. Sedation as needed is based on the discomfort reported by the patient or degree of difficulty of the examination as assessed by the endoscopist. There is at least one report that suggested that endoscopists are not as accurate as the patients or nurses in assessing colonoscopy pain29 and this option therefore carries a risk of coercion, patients may have to put up with more pain than they need to. On demand sedation would be based on the discomfort experienced by the patient and patients are instructed to request additional medications if they feel they need them. This option is probably less likely to be coercive as the patient is supposed to have control over the timing of medications. In both instances, completion without sedation obviates sedation complications and the time burden associated with recovery — both on-site and at home.28
The numbers at the bottom row of Table 2 depicts the proportion of patients who can complete without sedation based on the various options and the techniques used. When sedation as needed was described, only 6% required sedation.24 When on demand sedation was described a higher proportion completed without sedation when a water method was used compared with when the air method was used for inserting the colonoscope.28 In scheduled unsedated patients, the water method offered a significantly higher success rate than the traditional air method.30,31
Nurses who have worked with these options32 considered the following as benefits of not using routine sedation. There is no need for nurse monitoring. The rapid turn around of the unsedated patient minimizes recovery time. The amnesic effects of sedation33 are obviated, and discharge planning is facilitated. Because of less manpower demand the service is more efficient.
Last year, Ms Laura Johannes, published an article in the Wall Street Journal after she herself had an unsedated colonoscopy (under the option of on demand sedation). She felt no pain and her article ‘Take a Deep Breath…’ Some doctors are pushing sedation-free colon exams. Really” has provided a patients' perspective.34 At the recent CRC symposium she described her readers' experience with unsedated colonoscopy: 89% reported little or no pain at all.35
A grave concern in the U.S. regarding unsedated colonoscopy is the belief that the procedure is painful.10–12 Indeed, worldwide the success rate of unsedated colonoscopy have been reported to be 67%36, 76%30,37, 78%31,38, 81%39,40, 82%41 and 83%.41 A novel method of water infusion in lieu of air insufflation significantly improved the success rate of cecal intubation to 97% in an observational study.30 The significant impact was confirmed in a subsequent randomized controlled trial with a cecal intubation rate of 98%.31 Colonoscopists interested in providing their patients with any of the unsedated option are encouraged to consider evaluating the water method30,31 in their practice.
A description of the water method is included for the consideration of interested colleagues. The maneuvers can be summarized as warm water infusion in lieu of air insufflation combined with suction removal of all residual colonic air and residual feces by water exchange. Because insufflated air could lengthen the colon and exaggerate angulations at the flexures making insertion in the unsedated patient more difficult, the air pump was turned off before insertion of the colonoscope into the rectum to avoid accidental insufflation of air. Further minimization of angulations at the flexures (e.g. sigmoid, splenic and hepatic) was achieved by suction removal of all residual air. Warm water was infused in lieu of air insufflation as the “principal modality” to decrease the discomfort of colonoscope insertion. Warm to touch tap water or water at body temperature (37°C maintained by a water bath) was used because data in one publication support its effect in minimizing colonic spasms. The warm water was infused through the biopsy channel using a peristaltic pump via a tube fitted with a blunt needle adaptor. Removal of angulations by suction of residual air collapsed the colon around the colonoscope, increasing the chance that the tip of the colonoscope would be pointing in the direction of the “future” lumen. The role of water infusion was to assist in identification of the lumen for advancement of the colonoscope. The tip of the colonoscope was oriented towards the “slit-like lumen” ahead. The infused water opened the lumen if the orientation was correct. Incorrect orientation would not lead to opening of the lumen ahead, and water infusion was stopped. The tip of the colonoscope was pulled away from the mucosa and redirected. The colonoscope was advanced by a series of to and fro, back and forth, or repeated insertion and withdrawal motions of the shaft of the colonoscope with a torque in the direction of the expected lumen, and intermittent water infusion. Since air could not be used to find the lumen, suspended residual feces obscuring the view was suctioned and replaced by clean water until the colonic lumen was visualized again. To avoid suction of the mucosa, the sequence of events for this maneuver was to start the water infusion first, followed by application of suction. The volume of water needed to clear the view was kept to a minimum, but not restricted. To ensure adequate visualization during the insertion phase a range of volumes [200 ml (clean colon) to 2,000 ml (dirty colon)] were necessary. The turbulence set up by the simultaneous infusion and suction in the collapsed lumen dislodged the residual fecal matter from the surrounding mucosa in close proximity to the tip of the colonoscope. This maneuver appeared to make removal of the residual fecal matter “easier” than by washing with a single water jet in a dilated air filled colon. Most of the infused water in fact was aspirated into the suction bottle instead of remaining in the colon. Over-distension could be obviated. If advancement failed, the patient would change position or the assistant would provide abdominal compression to facilitate passage of the colonoscope, as usual. If the advancement was uninterrupted, no abdominal pressure or change in patient position was employed. Cecal intubation was suggested by appropriate movement of the endoscopic image on the monitor screen when the right lower quadrant was palpated, or ∼90 cm of the colonoscope was in the colon in the short configuration, or the appendix orifice under water was visualized. The cecum was then distended by air to confirm visualization of the ileocecal valve and the appendix orifice (cecal intubation).27,28,30,31
In conclusion, the answer to the question “Is there a place for sedationless colonoscopy?” is “yes”, when it is integrated into the various options to minimize patient burden in screening and surveillance colonoscopy. The availability of the novel water method should assure colonoscopists that high success rate of cecal intubation can be achieved in the unsedated patients.
Acknowledgements
This study was supported in part by ACG Research Award (FWL 2009), VA Clinical Merit Medical Research Funds and the ASGE Career Development Award (FWL 1985).
Abbreviations
- ACG
American College of Gastroenterology
- ASGE
American Society for Gastrointestinal Endoscopy
- CRC
colorectal cancer
- NA
not applicable
- PEG
polyethylene glycol
- US
United States
- VA
Veterans Affairs
Footnotes
Previously published online: www.landesbioscience.com/journals/jig
Disclosure
The author is a member of the medical advisory board of Invendo Medical.
References
- 1.Leung FW, Aljebreen AM, Brocchi E, Chang EB, Liao W, Mizukami T, et al. Sedation risk-free colonoscopy for minimizing the burden of colorectal cancer screening. World J Gastrointest Endosc. 2010;2:81–89. doi: 10.4253/wjge.v2.i3.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jonas DE, Russell LB, Sandler RS, Chou J, Pignone M. Patient time requirements for screening colonoscopy. Am J Gastroenterol. 2007;102:2401–2410. doi: 10.1111/j.1572-0241.2007.01387.x. [DOI] [PubMed] [Google Scholar]
- 3.Ko CW, Riffle S, Michaels L, Morris C, Holub J, Shapiro JA, et al. Serious complications within 30 days of screening and surveillance colonoscopy are uncommon. Clin Gastro Hepatol. 2010;8:166–173. doi: 10.1016/j.cgh.2009.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolff WI, Shinya H. Colonofiberoscopy. JAMA. 1971;217:1509–1512. [PubMed] [Google Scholar]
- 5.Williams C, Teague RH. Colonoscopy. Gut. 1973;14:990–1003. doi: 10.1136/gut.14.12.990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waye JD. Colonoscopy. Surg Clin North Am. 1972;52:1013–1024. doi: 10.1016/s0039-6109(16)39799-7. [DOI] [PubMed] [Google Scholar]
- 7.Rodney WM, Dabov G, Orientale E, Reeves WP. Sedation associated with a more complete colonoscopy. J Fam Pract. 1993;36:394–400. [PubMed] [Google Scholar]
- 8.Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. New Engl J Med. 2000;343:162–168. doi: 10.1056/NEJM200007203430301. [DOI] [PubMed] [Google Scholar]
- 9.Denberg TD, Melhado TV, Coombes JM, Beaty BL, Berman K, Byers TE, et al. Predictors of nonadherence to screening colonoscopy. J Gen Intern Med. 2005;20:989–995. doi: 10.1111/j.1525-1497.2005.00164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leo RA. Unsedated endoscopy: you don't get a medal for it! South Med J. 2004;97:797–798. doi: 10.1097/01.SMJ.0000136287.03289.3D. [DOI] [PubMed] [Google Scholar]
- 11.Madan A, Minocha A. Who is willing to undergo endoscopy without sedation: patients, nurses, or the physicians? South Med J. 2004;97:800–805. doi: 10.1097/01.SMJ.0000129794.97798.A5. [DOI] [PubMed] [Google Scholar]
- 12.Levenson D. Health quality organization criticizes colonoscopies given without pain medication. Rep Med Guidel Outcomes Res. 2001;12:9–10. 12. [PubMed] [Google Scholar]
- 13.Takahashi Y, Tanaka H, Kinjo M, Sakumoto K. Sedation-free colonoscopy. Dis Colon Rectum. 2005;48:855–859. doi: 10.1007/s10350-004-0860-0. [DOI] [PubMed] [Google Scholar]
- 14.Takahashi Y, Tanaka H, Kinjo M, Sakumoto K. Prospective evaluation of factors predicting difficulty and pain during sedation-free colonoscopy. Dis Colon Rectum. 2005;48:1295–1300. doi: 10.1007/s10350-004-0940-1. [DOI] [PubMed] [Google Scholar]
- 15.Park CH, Lee WS, Joo YE, Kim HS, Choi SK, Rew JS, et al. Sedation-free colonoscopy using an upper endoscope is tolerable and effective in patients with low body mass index: a prospective randomized study. Am J Gastroenterol. 2006;101:2504–2510. doi: 10.1111/j.1572-0241.2006.00790.x. [DOI] [PubMed] [Google Scholar]
- 16.Fennerty B. Sedation-Free Colonoscopy: Why Isn't It the Standard? Journal Watch Editors. 2009. Feb 18th, 2010 Jan 11. Available from: http://blogs.jwatch.org/gastroenterology/index.php/sedationfree-colonoscopy-why-isnt-it-the-standard/2009/02/18.
- 17.Ylinen ER, Vehviläinen-Julkunen K, Pietilä AM, Hannila ML, Heikkinen M. Medication-free colonoscopy — factors related to pain and its assessment. J Adv Nurs. 2009;65:2597–2607. doi: 10.1111/j.1365-2648.2009.05119.x. [DOI] [PubMed] [Google Scholar]
- 18.Rösch T. A Prospective pilot study to assess technical performance of a new single use colonoscope with inverted sleeve technology. Digestive Disease Week. 2007 Abstract W1344. [Google Scholar]
- 19.Röch T, Adler A, Pohl H, Wettschureck E, Koch M, Wiedenmann B, et al. A motor-driven single-use colonoscope controlled with a hand-held device: a feasibility study in volunteers. Gastrointest Endosc. 2008;67:1139–1146. doi: 10.1016/j.gie.2007.10.065. [DOI] [PubMed] [Google Scholar]
- 20.Leung FW. Patients' perspective - written testimonials from physician-patients and oral accounts presented by patients in person. J Interv Gastroenterol. 2011;1:45–46. doi: 10.4161/jig.1.1.14605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nelson DB, McQuaid KR, Bond JH, Lieberman DA, Weiss DG, Johnston TK. Procedural success and complications of large-scale screening colonoscopy. Gastrointest Endosc. 2002;55:307–314. doi: 10.1067/mge.2002.121883. [DOI] [PubMed] [Google Scholar]
- 22.Aslinia F, Uradomo L, Steele A, Greenwald BD, Raufman JP. Quality assessment of colonoscopic cecal intubation: an analysis of 6 years of continuous practice at a University Hospital. Am J Gastroenterol. 2006;101:721–731. doi: 10.1111/j.1572-0241.2006.00494.x. [DOI] [PubMed] [Google Scholar]
- 23.Vargo JJ, Bramley T, Meyer K, Nightengale B. Practice efficiency and economics: the case for rapid recovery sedation agents for colonoscopy in a screening population. J Clin Gastroenterol. 2007;41:591–598. doi: 10.1097/01.mcg.0000225634.52780.0e. [DOI] [PubMed] [Google Scholar]
- 24.Rex DK, Imperiale TF, Portish V. Patients willing to try colonoscopy without sedation: associated clinical factors and results of a randomized controlled trial. Gastrointest Endosc. 1999;49:554–559. doi: 10.1016/s0016-5107(99)70381-0. [DOI] [PubMed] [Google Scholar]
- 25.Leung CW, Kaltenbach T, Soetikno R, Wu KK, Leung FW, Friedland S. Water immersion versus standard colonoscopy insertion technique: randomized trial shows promise for minimal sedation. Endosc. 2010;42:557–563. doi: 10.1055/s-0029-1244231. [DOI] [PubMed] [Google Scholar]
- 26.Leung JW, Mann SK, Siao-Salera R, Ransibrahmanakul K, Lim B, Cabrera H, et al. A randomized, controlled comparison of warm water infusion in lieu of air insufflation versus air insufflation for aiding colonoscopy insertion in sedated patients undergoing colorectal cancer screening and surveillance. Gastrointest Endosc. 2009;70:505–510. doi: 10.1016/j.gie.2008.12.253. [DOI] [PubMed] [Google Scholar]
- 27.Leung JW, Mann S, Leung FW. Option for screening colonoscopy without sedation — a pilot study in United States veterans. Alimen Pharmacol Ther. 2007;26:627–631. doi: 10.1111/j.1365-2036.2007.03404.x. [DOI] [PubMed] [Google Scholar]
- 28.Leung JW, Mann SK, Siao-Salera RM, Ransibrahmanakul K, Lim BS, Canete W, et al. A randomized, controlled trial to confirm the beneficial effects of the water method on U.S. veterans undergoing colonoscopy with the option of on-demand sedation. Gastrointest Endosc. 2011;73:103–110. doi: 10.1016/j.gie.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 29.Ramakrishnan S, Yiannakou JY, Ellis WR, Bain IM. Assessment of patient pain at colonoscopy: are nurses better than endoscopists? J R Soc Med. 2004;97:432–433. doi: 10.1258/jrsm.97.9.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leung FW, Aharonian HS, Leung JW, Guth PH, Jackson G. Impact of a novel water method on scheduled unsedated colonoscopy in U.S. veterans. Gastrointest Endosc. 2009;69:546–550. doi: 10.1016/j.gie.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 31.Leung FW, Harker JO, Jackson G, Okamoto KE, Behbahani OM, Jamgotchian NJ, et al. A proof-of-principle, prospective, randomized, controlled trial demonstrating improved outcomes in scheduled unsedated colonoscopy by the water method. Gastrointest Endosc. 2010;72:693–700. doi: 10.1016/j.gie.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 32.Siao-Salera R, Leung JW, Mann SK, Canete W, Gutierrez R, Galzote CR, et al. Options of sedation or no sedation for colonoscopy - the perspective of the GI nurses and technicians. J Interv Gastroenterol. 2011;1:37–41. doi: 10.4161/jig.1.1.14601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hayes A, Buffum M. Educating patients after conscious sedation for gastrointestinal procedures. Gastroenterol Nurs. 2001;24:54–57. doi: 10.1097/00001610-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Johannes L. Take a deep breath — some doctors are pushing sedation-free colon exams. The Wall Street Journal. 2009. Feb 2, [2010 Jan 11]. Available from: http://online.wsj.com/article/SB123445383000677755.html.
- 35.Johannes L. The patient's perspective — patients should be made aware of the options of sedation or no sedation and have a choice in screening colonoscopy. J Interv Gastroenterol. 2011;1:42–44. doi: 10.4161/jig.1.1.14604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aljebreen AM. The completeness rate of colonoscopy in a cohort of unsedated patients. Saudi J Gastroenterol. 2004;10:150–154. [PubMed] [Google Scholar]
- 37.Radaelli F, Meucci G, Sgroi G, Minoli G. Italian Association of Hospital Gastroenterologists (AIGO). Technical performance of colonoscopy: the key role of sedation/analgesia and other quality indicators. Am J Gastroenterol. 2008;103:1122–1130. doi: 10.1111/j.1572-0241.2007.01778.x. [DOI] [PubMed] [Google Scholar]
- 38.Seow-Choen F, Leong AF, Tsang C. Selective sedation for colonoscopy. Gastrointest Endosc. 1994;40:661–664. [PubMed] [Google Scholar]
- 39.Petrini J, Egan J, Hahn W. Unsedated colonoscopy: patient characteristics and satisfaction in a community-based endoscopy unit. Gastrointest Endosc. 2009;69:567–572. doi: 10.1016/j.gie.2008.10.027. [DOI] [PubMed] [Google Scholar]
- 40.Leung FW, Aharonian HS, Guth PH, Chu SK, Nguyen BD, Simpson P. Involvement of trainees in routine unsedated colonoscopy - review of pilot experience. Gastrointest Endosc. 2008;67:718–722. doi: 10.1016/j.gie.2007.11.040. [DOI] [PubMed] [Google Scholar]
- 41.Thiis-Evensen E, Hoff GS, Sauar J, Vatn MH. Patient tolerance of colonoscopy without sedation during screening examination for colorectal polyps. Gastrointest Endosc. 2000;52:606–610. doi: 10.1067/mge.2000.109804. [DOI] [PubMed] [Google Scholar]
- 42.Bayupurnama P, Nurdjanah S. The success rate of unsedated colonoscopy examination in adult. Internet J Gastroenterol. 2010;Volume 9(Number 2) [Google Scholar]
- 43.Leung FW. Promoting informed choice of unsedated colonoscopy - patient-centered care for a subgroup of U.S. veterans. Dig Dis Sci. 2008;53:2955–2959. doi: 10.1007/s10620-008-0253-7. [DOI] [PubMed] [Google Scholar]


