Abstract
Toxoplasmosis is one of the more common parasitic zoonoses world-wide. Its causative agent, Toxoplasma gondii, is a facultatively heteroxenous, polyxenous protozoon that has developed several potential routes of transmission within and between different host species. If first contracted during pregnancy, T. gondii may be transmitted vertically by tachyzoites that are passed to the foetus via the placenta. Horizontal transmission of T. gondii may involve three life-cycle stages, i.e. ingesting infectious oocysts from the environment or ingesting tissue cysts or tachyzoites which are contained in meat or primary offal (viscera) of many different animals. Transmission may also occur via tachyzoites contained in blood products, tissue transplants, or unpasteurised milk. However, it is not known which of these routes is more important epidemiologically. In the past, the consumption of raw or undercooked meat, in particular of pigs and sheep, has been regarded as a major route of transmission to humans. However, recent studies showed that the prevalence of T. gondii in meat-producing animals decreased considerably over the past 20 years in areas with intensive farm management. For example, in several countries of the European Union prevalences of T. gondii in fattening pigs are now <1%. Considering these data it is unlikely that pork is still a major source of infection for humans in these countries. However, it is likely that the major routes of transmission are different in human populations with differences in culture and eating habits. In the Americas, recent outbreaks of acute toxoplasmosis in humans have been associated with oocyst contamination of the environment. Therefore, future epidemiological studies on T. gondii infections should consider the role of oocysts as potential sources of infection for humans, and methods to monitor these are currently being developed. This review presents recent epidemiological data on T. gondii, hypotheses on the major routes of transmission to humans in different populations, and preventive measures that may reduce the risk of contracting a primary infection during pregnancy.
1. Introduction
The tissue cyst-forming coccidium Toxoplasma gondii is one of the more polyxenous parasites known to date. It has a facultatively heteroxenous life cycle and can probably infect all warm-blooded animals (mammals and birds) and humans. T. gondii is prevalent in most areas of the world and is of veterinary and medical importance, because it may cause abortion or congenital disease in its intermediate hosts. Because of its great importance as a causative agent of a zoonosis T. gondii has been studied most intensively among the coccidia. To date, more than 15 000 original research articles, more than 500 reviews, and several books and book chapters have been published on this parasite (Table 1). However, there are still many aspects of its biology, natural life cycle, and the epidemiology of T. gondii infections of which we know relatively little.
Table 1.
Entries on T. gondii or toxoplasmosis in different publication databases
| Search termsa | ParasiteCDb | VETCDc | PubMedd |
|---|---|---|---|
| Toxoplasm* | 10 753 | 6615 | 12 605 |
| AND human* | 8546 | 3915 | 9086 |
| AND animal* | 10 567 | 6611 | 6186 |
| AND (zoonosis OR zoonoses) | 553 | 604 | 253 |
| AND (congenital OR pregnancy) | 1400 | 377 | 3051 |
| AND (immunocompromised OR immunosuppression) | 1027 | 168 | 525 |
| AND AIDS | 882 | 49 | 1754 |
| AND (prevalence OR seroprevalence) | 1585 | 942 | 2275 |
| AND epidemiology | 1305 | 777 | 2141 |
| AND transmission | 707 | 473 | 859 |
| AND (source* OR route*) AND infection | 200 | 160 | 212 |
| AND (tachyzoite* OR endozoite*) | 980 | 791 | 782 |
| AND (tissue cyst* OR bradyzoite* OR cystozoite*) | 454 | 404 | 231 |
| AND (oocyst* OR sporozoite*) | 687 | 662 | 407 |
| AND (therapy OR treatment) | 2670 | 1040 | 3725 |
| AND control | 1632 | 894 | 1498 |
| AND ((prevention OR preventive) NOT control) | 252 | 120 | 120 |
| AND (risk factor*) | 99 | 36 | 36 |
| AND (economy OR economic impact) | 15 | 15 | 46 |
Boolean operators (in capitals) and truncations (*) were as shown. In PubMed phrase searching with double quotes was used to search for entries on ‘tissue cyst*’, ‘risk factor*’ and ‘economic impact’.
ParasiteCD, 1973–2000/04 (CAB International); searches were carried out using the search and retrieval software WinSPIRS, version 2.0 (Silver-Platter International, N.V.).
VETCD, 1973–2000/05 (CAB International); searches were carried out using the search and retrieval software WinSPIRS, version 2.0 (SilverPlatter International, N.V.).
PubMed, 1966–2000/07; searches were carried out using the advanced search options of the new PubMed system of the National Center for Biotechnology Information (NCBI) at the National Library of Medicine (NLM), USA.
Asexual stages of toxoplasma-like parasites were first observed at the turn of the century in tissues of birds and mammals [1]. The first comprehensive description of T. gondii merozoites (i.e. tachyzoites or endozoites) in the spleen, liver, and blood of gondis, a species of North African rodents, was given in 1908 by Nicolle and Manceaux [2]. They introduced the genus Toxoplasma [3], and T. gondii became the type species of the genus. During the first half of this century, several species of Toxoplasma were named mainly in accordance with the host species in which they were detected [1,4,5]. It was not until the late 1930s that biological and immunological comparisons provided evidence that various isolates of animal and human origin were identical with T. gondii [6]. However, even then only asexual stages (merozoites and tissue cysts) of T. gondii were known and its classification was uncertain [5,7].
Evidence for the coccidian nature of T. gondii came first from EM studies carried out in the 1960s. These studies revealed ultrastructural similarities between extraintestinal merozoites of T. gondii and intestinal merozoites of Eimeria species, and thus indicated a coccidian-like life cycle for T. gondii [4,5,8]. The heteroxenous life cycle of T. gondii was elucidated in the late 1960s after it had been found that the faeces of cats may contain an infectious stage of T. gondii which induces infection when ingested by intermediate hosts [9]. This stage was eventually identified as an isosporan-type oocyst previously described as part of the Isospora bigemina complex [4,5,10]. In 1970, knowledge of the coccidian life cycle of T. gondii was completed by the discovery of sexual stages in the small intestine of cats [1,4,5,11–14].
Thus, knowledge on the life cycle of T. gondii was completed more than 60 years after the first description of its asexual stages in intermediate hosts. It was finally revealed that T. gondii is a tissue cyst-forming coccidium with a heteroxenous life cycle in which an asexual phase of development in various tissues of herbivorous or omnivorous intermediate hosts is linked to a sexual phase of development in the intestine of carnivorous definitive hosts. Since then, several other protozoa that had been assigned to the genus Toxoplasma during the first half of this century, have either been synonymised with T. gondii, have been reclassified into other coccidian genera, or their descriptions superseded [1,4,5,15]. Over the past 3 decades, T. gondii has been generally considered as the only valid species of the genus Toxoplasma [5,11,16–22]. More recently, molecular epidemiological studies have provided evidence that there are at least two clonal lineages within T. gondii, one comprising strains that are virulent in mice and another comprising strains that are avirulent in mice [23,24]. This finding has raised debate on whether or not the different lineages within T. gondii are indicative of ongoing speciation [23–29], and a recent hypothesis suggested that vertical transmission of T. gondii in the mouse-virulent lineage may have a greater epidemiological importance than has been believed so far [23,24].
In the course of evolution, T. gondii has developed a broad range of potential routes of transmission. However, the elucidation of these routes during the past 3 decades has not elucidated which of these routes is more important epidemiologically. For example, many studies have focussed on congenital toxoplasmosis in humans which is a result of vertical transmission of the parasite during pregnancy. By contrast, we know little about the relative importance of horizontal transmission of T. gondii between different host species, of the major reservoirs of the parasite in nature, or of the epidemiological impact of the different sources causing infection or disease in humans. Likewise, many studies have been carried out on the asexual stages of T. gondii, in particular on the tachyzoite, while much fewer studies have considered the sexual stages or their infectious product, i.e. the sporozoites within the oocyst. Moreover, only few studies have been aimed at identifying risk factors that may be associated with acquiring an infection with T. gondii postnatally (Table 1).
This review focuses on probable routes of transmission of T. gondii from animals to humans. We review recent outbreaks of toxoplasmosis in humans and discuss the sources of infection that have been associated with them. We also review epidemiological data on T. gondii that have been recorded over the last decade and discuss strategies for prevention or control of T. gondii infections in humans. However, because of the large number of scientific papers that are being published on T. gondii every year it is not possible to cover all aspects of this zoonosis in this review. Therefore, we refer to the comprehensive reviews of Dubey and Towle [30], Dubey and Beattie [11], Jackson and Hutchison [12], Remington and Desmonts [31], Ho-Yen and Joss [32], Dubey [13], Remington et al. [33], and Ambroise-Thomas and Petersen [34] for more detailed information and for data recorded on this parasite prior to the 1990s.
2. Life cycle of Toxoplasma gondii
T. gondii is a ubiquitous parasite that occurs in most areas of the world. It is capable of infecting an unusually wide range of hosts and many different host cells [7,11,35]. The life cycle of T. gondii is facultatively heteroxenous (Fig. 1). Intermediate hosts are probably all warm-blooded animals including most livestock, and humans. Definitive hosts are members of the family Felidae, for example domestic cats [11–13,22,36].
Fig. 1.

Life cycle of T. gondii. Development in the intermediate host is illustrated below the horizontal bar, development in the definitive host is illustrated above the horizontal bar. The infectious stages, i.e. tachyzoites, bradyzoites contained in tissue cysts, and sporozoites contained in sporulated oocysts, have been shaded (modified from Ref. [245]).
In intermediate hosts, T. gondii undergoes two phases of asexual development. In the first phase, tachyzoites (or endozoites) multiply rapidly by repeated endodyogeny in many different types of host cells. Tachyzoites of the last generation initiate the second phase of development which results in the formation of tissue cysts. Within the tissue cyst, bradyzoites (or cystozoites) multiply slowly by endodyogeny [11–13,20,35]. Tissue cysts have a high affinity for neural and muscular tissues. They are located predominantly in the central nervous system (CNS), the eye as well as skeletal and cardiac muscles. However, to a lesser extent they may also be found in visceral organs, such as lungs, liver, and kidneys [13,14,35]. Tissue cysts are the terminal life-cycle stage in the intermediate host and are immediately infectious. In some intermediate host species, they may persist for the life of the host. The mechanism of this persistence is unknown. However, many investigators believe that tissue cysts break down periodically, with bradyzoites transforming to tachyzoites that reinvade host cells and again transform to bradyzoites within new tissue cysts [14,20,22,31,35,37,38]. If ingested by a definitive host, the bradyzoites initiate another asexual phase of proliferation which consists of initial multiplication by endodyogeny followed by repeated endopolygeny in epithelial cells of the small intestine. The terminal stages of this asexual multiplication initiate the sexual phase of the life cycle. Gamogony and oocyst formation also take place in the epithelium of the small intestine. Unsporulated oocysts are released into the intestinal lumen and passed into the environment with the faeces. Sporogony occurs outside the host and leads to the development of infectious oocysts which contain two sporocysts, each containing four sporozoites [11–13,20,35].
There are three infectious stages in the life cycle of T. gondii, i.e. tachyzoites, bradyzoites contained in tissue cysts, and sporozoites contained in sporulated oocysts (Fig. 1). All three stages are infectious for both intermediate and definitive hosts which may acquire a T. gondii infection mainly via one of the following routes (Fig. 2): (A) horizontally by oral ingestion of infectious oocysts from the environment, (B) horizontally by oral ingestion of tissue cysts contained in raw or undercooked meat or primary offal (viscera) of intermediate hosts, or (C) vertically by transplacental transmission of tachyzoites [11–13,20,31,35,39]. In addition, in several hosts tachyzoites may also be transmitted in the milk from the mother to the offspring [11–13,20,23,31].
Fig. 2.
Major routes of transmission of T. gondii.
Thus, T. gondii may be transmitted from definitive to intermediate hosts, from intermediate to definitive hosts, as well as between definitive and between intermediate hosts (Figs. 1 and 2). It is currently not known which of the various routes of transmission is more important epidemiologically. However, the prevalence of T. gondii infections is not confined to the presence of a certain host species. Its life cycle may continue indefinitely by transmission of tissue cysts between intermediate hosts (even in the absence of definitive hosts) and also by transmission of oocysts between definitive hosts (even in the absence of intermediate hosts).
3. Zoonotic importance of Toxoplasma gondii
3.1. Prevalence of T: gondii infections in humans
Toxoplasmosis is one of the more common parasitic zoonoses world-wide. Disease in humans caused by T. gondii was first recognised in the late 1930s (Table 2). In 1939, Sabin [6] first proved that Toxoplasma isolates from humans and those previously obtained from animals belonged to the same species. In 1948, the introduction of the methylene blue dye test by Sabin and Feldman [40] enabled seroepidemiological studies in humans as well as a broad range of animal species which provided evidence for a wide distribution and high prevalence of T. gondii in many areas of the world. Since then, it has been estimated that up to one third of the world human population has been exposed to the parasite [1,12,14,41]. However, seroprevalence estimates for human populations vary greatly among different countries, among different geographical areas within one country, and among different ethnic groups living in the same area. Thus, over the past 3 decades antibodies to T. gondii have been detected in from 0 to 100% of individuals in various adult human populations [11,12,31,42,43].
Table 2.
History of T. gondii and its emergence as a human pathogen
| Year | Event | Reference |
|---|---|---|
| 1900 | Description of toxoplasma-like parasites in Java sparrows | [246,247] |
| 1908 | First description of toxoplasma-like tissue cysts in humans (as sarcosporidiosis) | [248] |
| 1908 | Description of T. gondii merozoites in gondi (first named Leishmania gondii) | [2] |
| 1909 | Introduction of the genus Toxoplasma (type species: T. gondii) | [3] |
| 1923 | First recorded case of toxoplasmosis in an 11- month-old infant with congenital hydrocephalus and microphthalmia (recognised retrospectively) | [203,204,249] |
| 1928 | First description of the tissue cyst as a persistent stage in intermediate hosts | [205] |
| 1937 | First recorded case of fatal disseminated toxoplasmosis in an adult (22-year-old) human | [250] |
| 1937–39 | Recognition of T. gondii as a causative agent of encephalomyelitis in human neonates | [206–208] |
| 1939 | Description of classic triad of symptoms of congenital toxoplasmosis in humans (retinochoroiditis, hydrocephalus, encephalitis followed by cerebral calcification) | [208] |
| 1939 | Identity of isolates from humans and animals based on biological and immunological similarities | [6] |
| 1940–41 | Recognition of T. gondii as a causative agent of acute, acquired disease in adult humans | [250,251] |
| 1941–42 | Comprehensive description of toxoplasmic encephalitis in children with acquired toxoplasmosis | [252,253] |
| 1942 | Vertical transmission recognised in humans | [209] |
| 1948 | Methylene blue dye test introduced for detection of antibodies to T. gondii (gold standard for T. gondii-specific serology in humans) | [40] |
| 1951–52 | Recognition of T. gondii as a causative agent of lymphadenopathy in humans | [254,255] |
| 1952 | Description of T. gondii as a causative agent of retinochoroiditis in humans | [71] |
| 1952 | Description of classic tetrad of symptoms of congenital toxoplasmosis in humans (retinochoroiditis, cerebral calcification, hydrocephalus or microcephalus, and psychomotor disturbances) | [256] |
| 1953–54 | First recorded case of toxoplasmic encephalitis in a patient with Hodgkin’s disease | [257] |
| 1954–56 | Hypothesis that horizontal transmission to humans may occur via tissue cysts in undercooked meat (pork) | [258,259] |
| 1959 | Serological evidence of T. gondii infections in vegetarians | [260] |
| 1960 | Discovery that tissue cysts are resistant to proteolytic enzymes | [127,261] |
| 1960 | Description of major sequelae of congenital toxoplasmosis in humans | [262] |
| 1965 | Recognition of the coccidian nature of T. gondii based on the ultrastructure of extraintestinal merozoites | [263,264] |
| 1965 | Epidemiological evidence that horizontal transmission to humans occurs via undercooked meat | [265] |
| 1965 | Hypothesis that an infectious stage of T. gondii is passed into the environment via the faeces of cats | [9] |
| 1968 | Recognition of T. gondii as a complication in patients with malignancies | [266] |
| 1969 | Identification of the oocyst of T. gondii | [267–273] |
| 1970 | Description of the sexual phase of the life cycle in the small intestine of cats | [270,274– 277] |
| 1969–72 | Recognition of the epidemiological role of cats in the spread of T. gondii in different geographical areas | [171,172] |
| 1981–82 | First recorded cases of CNS toxoplasmosis in AIDS patients | [278] |
| 1984 | Recognition of T. gondii as an opportunistic pathogen in AIDS patients | [102] |
| 1995–99 | Largest recorded outbreak of acute toxoplasmosis in humans (100 individuals aged 6–83 years) associated with oocysts in municipal drinking water | [69,191,279] |
When comparing seroprevalence data for infections with T. gondii it should be taken into account that the different serological methods used to obtain these data are not standardised. The Sabin–Feldman dye test, which is still considered as the ‘gold standard’ for detection of antibodies to T. gondii in humans, is labour-intensive and has the disadvantage that it requires a continuous supply of live parasites. Therefore, most epidemiological studies on T. gondii infections now use different tests for antibody detection. A broad range of serological tests have been developed to detect antibodies to T. gondii in humans and animals [11,31,44]. These tests vary in sensitivity, specificity, and predictive values. As a consequence, no two tests produce the same results in all cases, even when carried out in the same laboratory [45–54]. In addition, prevalence rates vary over time and with the age of the individuals included in the study [55–68].
Therefore, the data reviewed here do not reflect nationwide prevalences and may differ from the true prevalence of infection in the various populations. However, they are comparable if they are interpreted as estimates reflecting the different levels of prevalence among similar populations, i.e. populations that are comparable with respect to age, cultural habits, environmental factors, or other factors that may have an impact on the epidemiology of T. gondii infections (see Section 4). For example, in the 1990s seroprevalences in Central European countries, such as Austria, Belgium, France, Germany, and Switzerland, have been estimated to range between 37 and 58% in women of child-bearing age with no obstetric history (Table 3). Comparable seroprevalences have been observed in similar populations in Croatia, Poland, Slovenia, Australia, and Northern Africa. Seroprevalences are higher in several Latin-American countries, including Argentina, Brazil, Cuba, Jamaica, and Venezuela (51–72%), and in West African countries on the Gulf of Guinea, i.e. Benin, Cameroon, Congo, Gabon, and Togo (54–77%). Lower seroprevalences have been reported for women of childbearing age in Southeast Asia, China, and Korea (4–39%). Seroprevalences are also low in areas with a cold climate, such as the Scandinavian countries (11–28%). However, there is no doubt that overall T. gondii infections are highly prevalent in adult human populations throughout the world (Table 3).
Table 3.
Seroprevalences of T. gondii infection in women of childbearing age (1990–2000)
| Country | Year of samplinga | BOHb | Seroprevalence (%)c | Number of samples tested (n) | Methodd | Reference |
|---|---|---|---|---|---|---|
| Argentina | 1992–94 | No | 59 | 3049 | IFAT | [280] |
| Australia | 1986–89 | No | 35 | 10207 | DAT | [137] |
| Austria | 1981–91 | No | 43 | 167041 | SFDT | [196] |
| 1993–94 | No | 50 | 8596 | e | [281] | |
| 1994–95 | No | 37 | 2413 | e | [282] | |
| 1995–96 | No | 43 | 18227 | e | [281] | |
| 1997 | No | 42 | 4601 | e | [281] | |
| Bangladesh | 1991 | Yes | 16 | 302 | LAT | [283] |
| 1994–95 | No | 11 | 617 | LAT | [284] | |
| < 1998 | No | 38 | 286 | ELISA | [285] | |
| Belgium | 1979–90 | No | 56 | 11286 | IFAT | [286] |
| 1990 | No | 50 | 784 | MEIA | [287] | |
| Benin | 1993 | No | 54 | 211 | ELISA | [288] |
| Brazil | 1997 | No | 72 | 185 | ELISA | [289] |
| Cameroon | 1989–90 | No | 77 | 192 | ELISA | [290] |
| China | < 1995 | No | 39 | 1211 | ELISA | [291] |
| 1996 | No | 4 | 557 | IHAT | [292] | |
| Colombia | 1991–92 | No | 60 | 937 | IFAT | [67] |
| Congo | 1986–90 | No | 60 | 2897 | IHAT | [293] |
| Croatia | 1989–93 | No | 46 | 2778 | ELISA | [294] |
| Cuba | 1990–91 | No | 71 | 362 | ELISA | [295] |
| 1990–91 | No | 71 | 5537 | ELISA | [296] | |
| < 1993 | No | 51 | 3196 | – | [297] | |
| Czech Republic | 1984–86 | No | 35 | 3392 | SFDT | [298] |
| 1984–86 | No | 25 | 3392 | CFT | [298] | |
| < 1999 | No | 29* | 191 | CFT | [299] | |
| Denmark | 1990 | No | 27 | 5402 | ELISA | [300] |
| 1992–96 | No | 28 | 89873 | ELISA | [232] | |
| Egypt | < 1990 | Yes | 72 | 200 | SFDT | [301] |
| < 1990 | Yes | 59 | 200 | IFAT | [301] | |
| < 1991 | Yes | 28 | 72 | IFAT | [302] | |
| < 1993 | Yes | 65 | 100 | ELISA | [303] | |
| < 1995 | Yes | 42* | 62 | ELISA | [304] | |
| < 1990 | No | 38 | 100 | SFDT | [301] | |
| < 1990 | No | 32 | 100 | IFAT | [301] | |
| < 1991 | No | 12 | 34 | IFAT | [302] | |
| < 1992 | No | 31 | 70 | IFAT | [305] | |
| < 1993 | No | 27 | 600 | IHAT | [306] | |
| < 1993 | No | 6 | 100 | ELISA | [303] | |
| 1992–93 | No | 43 | 150 | IHAT | [307] | |
| Ethiopia | < 1994 | No | 20 | 94 | ELISA | [308] |
| Finland | 1988–89 | No | 20 | 16733 | e | [309] |
| France | 1993–94 | No | 58 | 987 | – | [310] |
| 1995 | No | 54 | 13459 | – | [65] | |
| Gabon | 1995–97 | No | 71 | 767 | LAT | [311] |
| Germany | 1987–90 | No | 73 | 4355 | ELISA | [62] |
| 1989–90 | No | 42 | 2104 | DAT | [312] | |
| < 1992 | No | 39 | 5670 | ISAGA | [313] | |
| Greece | 1991–95 | No | 30 | 1242 | ELISA | [314] |
| < 1996 | No | 37 | 914 | ELISA | [315] | |
| India | 1986–91 | Yes | 8 | 2075 | IFAT | [316] |
| 1990 | Yes | 22 | 100 | IHAT | [317] | |
| < 1997 | Yes | 8 | 540 | LAT | [318] | |
| Iraq | 1994–95 | Yes | 19 | 81 | IHAT | [319] |
| 1994–95 | No | 6 | 119 | IHAT | [319] | |
| Israel | 1988–89 | No | 21 | 213 | IFAT | [320] |
| Italy | < 1990 | No | 73 | 691 | DAT | [321] |
| 1987–91 | No | 49 | 19432 | ELISA | [322] | |
| 1992–93 | No | 60 | 1800 | ISAGA | [323] | |
| 1993 | No | 40 | 3518 | – | [324] | |
| 1993–94 | No | 18 | 2295 | ELFA | [325] | |
| 1992–97 | No | 23 | 9029 | ELISA | [326] | |
| Jamaica | 1986 | No | 57 | 1604 | ELISA | [327] |
| Korea | 1990 | No | 7 | 618 | IFAT | [328] |
| 1990 | No | 7 | 618 | ELISA | [328] | |
| 1993–94 | No | 4 | 899 | ELISA | [329] | |
| 1993–94 | No | < 1 | 899 | LAT | [329] | |
| Libya | < 1991 | No | 47 | 369 | IHAT | [330] |
| Madagascar | 1992 | No | 84 | 599 | ELISA | [331] |
| Mexico | < 1995 | Yes | 35 | 350 | ELISA | [332] |
| Nepal | 1995–96 | No | 55 | 345 | LAT | [333] |
| 1995–96 | No | 55 | 345 | ELISA | [333] | |
| Nigeria | < 1990 | No | 40 | 834 | DAT | [334] |
| < 1990 | No | 39 | 834 | IFAT | [334] | |
| < 1992 | No | 78 | 352 | SFDT | [335] | |
| Norway | 1992–93 | No | 11 | 35940 | ELISA | [336] |
| Pakistan | < 1996 | Yes | 17 | 240 | IFAT | [337] |
| < 1997 | Yes | 33 | 105 | ELISA | [338] | |
| Papua New Guinea | 1989–90 | No | 18 | 197 | DAT | [339] |
| Poland | 1991–92 | No | 59 | 3734 | DAT | [340] |
| Saudi Arabia | < 1991 | Yes | 100 | 219 | IHAT | [341] |
| < 1991 | No | 32 | 921 | IHAT | [342] | |
| Senegal | < 1990 | No | 33 | 60 | LAT | [343] |
| 1993 | No | 40 | 353 | ELISA | [344] | |
| 1993 | No | 40 | 720 | IFAT | [345] | |
| Slovenia | 1989–91 | No | 51 | 3959 | SFDT | [346] |
| Spain | < 1991 | No | 39 | 1221 | DAT | [347] |
| 1991–93 | No | 13 | 299 | IFAT | [348] | |
| 1991–93 | No | 30 | 6454 | ELISA | [349] | |
| 1994–95 | No | 42 | 109 | ELISA | [350] | |
| Sweden | 1992–93 | No | 14 | 3094 | DAT | [351] |
| Switzerland | 1990–91 | No | 46 | 9059 | ELISA | [352] |
| Tanzania | 1989–91 | No | 35 | 549 | SFDT | [353] |
| Thailand | < 1991 | No | 13 | 690 | LAT | [354] |
| 1996 | No | 13 | 1181 | SFDT | [355] | |
| Togo | < 1991 | No | 75 | 620 | ELISA | [356] |
| Trinidad | 1991–92 | No | 43 | 300 | ELISA | [357] |
| Tunisia | 1988–91 | No | 64 | 3288 | IFAT | [358] |
| 1991–93 | No | 57 | 809 | IFAT | [359] | |
| 1994–96 | No | 43 | 2231 | ELISA | [360] | |
| Turkey | < 1993 | Yes | 47 | 1160 | IFAT | [361] |
| < 1993 | Yes | 47 | 1146 | ELISA | [361] | |
| < 1995 | Yes | 77 | 314 | IHAT | [362] | |
| < 1995 | Yes | 35 | 100 | IFAT | [363] | |
| < 1996 | Yes | 82* | 140 | ELISA | [364] | |
| < 1996 | Yes | 38 | 954 | ELISA | [365] | |
| < 1997 | Yes | 63 | 314 | ELISA | [366] | |
| < 1993 | No | 27 | 187 | ELISA | [367] | |
| < 1993 | No | 19 | 187 | SFDT | [367] | |
| 1991–95 | No | 55 | 2287 | ELISA | [368] | |
| 1992–95 | No | 40 | 996 | ELISA | [369] | |
| < 1995 | No | 62 | 100 | IFAT | [363] | |
| < 1995 | No | 47 | 152 | IHAT | [362] | |
| < 1995 | No | 32 | 150 | – | [370] | |
| 1995–96 | No | 43 | 258 | – | [371] | |
| < 1996 | No | 81 | 72 | ELISA | [364] | |
| < 1996 | No | 80* | 420 | ELISA | [372] | |
| < 1996 | No | 71* | 420 | IHAT | [372] | |
| < 1996 | No | 34 | 324 | – | [373] | |
| < 1998 | No | 61 | 326 | ELISA | [374] | |
| < 1999 | No | 85 | 86 | IFAT | [375] | |
| United Arab Emirates | < 1997 | No | 23 | 1503 | ELISA | [376] |
| United Kingdom | ||||||
| Sheffield | 1989–92 | No | 10 | 1621 | LAT | [377] |
| East England | 1992 | No | 8 | 13000 | ELISA | [378] |
| Wales | < 1992 | No | 22 | 192 | SFDT | [335] |
| Venezuela | 1976–92 | No | 54 | 7696 | IHAT | [379] |
| Yugoslavia | 1988–91 | No | 77 | 1157 | SFDT | [380] |
Years of sampling are listed as published in the references. In cases where this information was not available, the year listed here is the year when the study was published, as indicated by ‘<’. Data from the 1980s are included if the study was published in the 1990s and if no recent data were available for the area.
BOH, women with bad obstetric history.
Seroprevalences marked with ‘*’ were calculated from the published data.
CFT, complement fixation test; DAT, direct agglutination test; ELISA, enzyme-linked immunosorbent assay; ELFA, enzyme-linked fluorescent assay; IFAT, indirect immunofluorescent antibody test; IHAT, indirect haemagglutination test; ISAGA, immunosorbent agglutination assay; LAT, latex agglutination test; MEIA, microparticle capture enzyme immunoassay; SFDT, Sabin–Feldman dye test; –, not reported.
Data were derived from screening programs using various diagnostic methods.
3.2. Postnatally acquired toxoplasmosis in immunocompetent humans
While infection with T. gondii in humans is very common, clinical disease is largely confined to risk groups (see Sections 3.3 and 3.4). Most cases of T. gondii infections in immunocompetent humans are asymptomatic. Occasionally, various mild symptoms may be observed of which lymphadenopathy is the most significant clinical manifestation [11,69,70]. Severe manifestations, such as encephalitis, sepsis syndrome/shock, myocarditis, or hepatitis may occur, but are very rare in immunocompetent humans [70].
Since the early 1950s, infection with T. gondii has also been recognised as an important cause of retinochoroiditis [71]. However, ocular toxoplasmosis has long been regarded as a result of a prenatal infection with T. gondii, which manifests later in life [70,72,73]. While retinochoroidital lesions in infants with congenital toxoplasmosis are well recognised (see Section 3.3), it has been controversial whether similar ocular lesions in older children or adults result from a recently acquired, primary infection or from recurrences of prenatal infection [70,72,74–78]. However, there are now several recorded cases in which the development of ocular symptoms, such as retinitis and retinochoroiditis, was convincingly associated with acquired toxoplasmosis in humans [69,76,79–87].
While most of the earlier studies on acquired toxoplasmic retinochoroiditis have been based on sporadic cases [77,79,84,87], some recent studies have examined the outcome of multiple cases following outbreaks of acute toxoplasmosis in adults due to various sources (see Sections 4.2.4 and 4.3.3). In those outbreaks, in which a possible source of infection was revealed and dated by epidemiological investigation, the period between primary infection and onset of ocular symptoms ranged from 1 month to 3.5 years, while the age range of the patients was much wider, i.e. 10–57 years [79,81,82,86]. In the world’s largest recorded outbreak of acquired toxoplasmosis in humans (100 cases, see Section 4.3.3), 20 patients with equal gender distribution and a mean age of 54 years (range 15–83 years) presented with retinal lesions within less than 1 year after the outbreak [69,87]. In addition, a population-based household survey in a rural area in southern Brazil suggested that an exceptionally high prevalence of familial ocular toxoplasmosis in that area, which is more than 30 times higher than estimates for the same condition elsewhere, has an acquired aetiology [88,89]. These findings were supported by a recent study in France on 49 patients with acquired toxoplasmosis of whom 44 also developed ocular symptoms [76]. As a screening programme for congenital toxoplasmosis is compulsory in France since 1978, a prenatal infection with T. gondii could be ruled out in several of those cases based on the documented immune status of the mother. Thus, it has now become clear that ocular toxoplasmosis may be both a result of a prenatal infection or an infection that was acquired postnatally.
3.3. Congenital toxoplasmosis
In immunocompetent hosts, infection with T. gondii usually results in life-long immunity against toxoplasmosis. Therefore, if a primary T. gondii infection is acquired 4–6 months before conception or earlier, protective immunity will usually prevent vertical transmission to the foetus on subsequent exposures. The exception is seen in immunocompromised women with systemic lupus erythematosus (SLE) or acquired immunodeficiency syndrome (AIDS) where previously infected, seropositive individuals have transmitted T. gondii congenitally [90].
However, if first contracted during pregnancy, T. gondii may also be transmitted to the foetus in immunocompetent women. The mechanism of vertical transmission is not yet understood. A probable scenario is that temporary parasitaemia in a primarily infected pregnant woman may result in invasion of the placenta by tachyzoites which then multiply within cells of the placenta. Eventually, some of these may cross the placenta and enter the foetal circulation or foetal tissues [31,91]. Congenital toxoplasmosis may cause abortion, neonatal death, or foetal abnormalities with detrimental consequences for the foetus [31,33,42,92]. It may also significantly reduce the quality of life in children who survive a prenatal infection [11,93–95].
Over the past 3 decades, the incidence of prenatal infection with T. gondii has been estimated to vary from 1 to 100 per 10 000 births in different countries [11,12,31,42,93,94]. The risk of intrauterine infection of the foetus, the risk of manifestation of congenital toxoplasmosis, and the severity of the disease depend on the time of maternal infection during pregnancy, the immunological competence of the mother during parasitaemia, the number and virulence of the parasites transmitted to the foetus, and the age of the foetus at the time of transmission. If not treated, the risk of intrauterine infection of the foetus increases during pregnancy, i.e. from about 14% after primary maternal infection in the first trimester to about 59% after primary maternal infection in the last trimester [31,42]. Because of this, the incidence of prenatal infection with T. gondii varies from the incidence of primary maternal infection during pregnancy. Incidence rates also vary depending on the method of estimation. Estimates may be derived directly from surveys at birth or during infancy, or indirectly from prospective surveys of acquired T. gondii infection during pregnancy [31]. Recent estimates based on serological studies suggested incidences of primary maternal infection during pregnancy to range from about 1 to 310 per 10 000 pregnancies in different populations in Europe, Asia, Australia, and the Americas (Table 4). These rates are dependent on the prevalence of infection in the population under study and are slightly higher (6–410 per 10 000) if only susceptible women are taken into account, i.e. those women who have not developed immunity before conception (Table 4). Incidences of prenatal infection with T. gondii in the same or similar populations have been estimated to range from about 1 to 120 per 10 000 births (Table 5).
Table 4.
Incidence of T. gondii infection in women of childbearing age (1990–2000)
| Country | Year of samplinga | Incidence per 1000 pregnanciesb | Incidence per 1000 susceptible mothersb | Number of pregnant women tested (n)b | Prevalence (%) | Reference |
|---|---|---|---|---|---|---|
| Argentina | 1992 | 7 | – | – | 40 | [381] |
| Australia | 1986–89 | 1.08* | 1.6 | 10207 | 35 | [137] |
| Austria | 1989–91 | 0.08 | – | – | 37 | [196] |
| Colombia | 1991–92 | 3.75–15 | 10–40 | 937 | 60 | [67] |
| Czech Republic | 1982–94 | 2.2 | 3.70* | 50023 | 40 | [382] |
| Denmark | 1990 | 0.44* | 0.61 | 5402 | 27 | [299] |
| 1992–96 | 1.5 | 2.1 | 89873 | 28 | [232] | |
| Finland | 1988–89 | 1.49* | 2.4 | 16733 | 20 | [308,383] |
| Germany | 1987–90 | 2.53 | 9.28* | 4355 | 73 | [62] |
| 1990 | 4.9–6.1 | – | 126733* | – | [384] | |
| Greece | < 1996 | 6 | – | 914 | 37 | [314] |
| Israel | 1988–89 | 14 | 20* | 213 | 21 | [319] |
| Norway | 1992–94 | 1.31* | 1.47 | 35940 | 11 | [385] |
| Slovenia | 1991–94 | 4.73* | 7.5 | 8254 | 37 | [386] |
| Spain | < 1996 | 0.56 | 1.3 | 3580 | 57 | [387] |
| Sweden | 1992–93 | 1.29* | 1.51* | 3094 | 14 | [350] |
| United Arab Emirates | < 1997 | 31 | 41* | 1503 | 23 | [375] |
| United Kingdom | 1989–92 | 0.62* | 0.68* | 1621 | 10 | [376] |
| 1992 | 3.97* | 4–6 | 13328 | 8 | [377] |
Years of sampling are listed as published in the references. In cases where this information was not available, the year listed here is the year when the study was published, as indicated by ‘<’. Data from the 1980s are included if the study was published in the 1990s and if no recent data were available for the area.
Figures marked with ‘*’ were calculated from the published data. –, not reported.
Table 5.
Incidence of prenatal infection with T. gondii in human neonates (1990–2000)
| Country | Year of samplinga | Incidence per 1000 birthsb | Incidence per 1000 births to non-immune mothersb | Number of samples tested (n)b | Prevalence of infection in mothers (%) | Reference |
|---|---|---|---|---|---|---|
| Australia | 1986–89 | 0.16* | 0.23 | 18908 | 32 | [137] |
| Austria | 1991 | < 0.10 | – | – | 37 | [196] |
| Denmark | 1992–96 | 0.30 | 0.42 | 89873 | 28 | [232] |
| Germany | 1990 | 1.1 | – | 126733* | – | [384] |
| Guatemala | 1987 | 10.9 | 20* | 550 | 44 | [388] |
| Norway | 1992–94 | 0.31* | 0.34* | 35940 | 11 | [385] |
| Poland | 1996–98 | 0.55 | 1.33 | 27516 | 59 | [199] |
| Switzerland | 1986–90 | 0.73 | – | 15000 | – | [389] |
| 1991–94 | 0.33 | – | 15000 | – | [389] | |
| United Arab Emirates | < 1997 | 12 | 16 | 1503 | 23 | [375] |
| United Kingdom | 1992 | 0.3–1.6 | – | 13328 | 8 | [377] |
| USA | 1986–91 | 0.08* | – | 530000 | – | [233] |
| 1986–92 | 0.08* | – | 635000 | – | [201] |
Years of sampling are listed as published in the references. In cases where this information was not available, the year listed here is the year when the study was published, as indicated by ‘<’. Data from the 1980s are included if the study was published in the 1990s and if no recent data were available for the area.
Figures marked with ‘*’ were calculated from the published data. –, not reported.
While the risk of intrauterine infection of the foetus increases during pregnancy, the effects on the foetus are more severe if transmission occurs at an early stage of pregnancy [31,42,96,97]. The most significant manifestation in the foetus is encephalomyelitis which may have severe consequences. About 10% of prenatal infections result in abortion or neonatal death [31,42]. Another 10–23% of prenatally infected newborns show clinical signs of toxoplasmosis at birth [31,42,93,98]. Signs of the classic triad of toxoplasmosis (retinochoroiditis, intracranial calcifications, and hydrocephalus) manifest in up to 10% of these newborns, while the other newborns show a variety of symptoms, ranging from central nervous symptoms to non-specific symptoms of acute infection (retinochoroiditis, convulsions, splenomegaly, hepatomegaly, fever, anaemia, jaundice, lymphadenopathy etc.). About 12–16% of these newborns die from the disease. The surviving infants suffer from progressive mental retardation or other neurological deficiencies which often require special education and residential care [11,31,93,94].
However, if transmission occurs at a late stage of pregnancy the effects on the foetus are less severe, with most infants infected during the third trimester being asymptomatic at birth. In total, in about 67–80% of prenatally infected infants the infection is subclinical and can only be diagnosed using serological and other laboratory methods. Although these infants appear healthy at birth, they may develop clinical symptoms and deficiencies later in life. These deficiencies predominantly affect the eyes (retinochoroiditis, strabismus, blindness), the CNS (psychomotorical or other neurological deficiencies, convulsions, mental retardation), or the ear (deafness) [31,42,95]. It has been estimated that about one third of prenatally infected children will develop visual impairment later in life [11,99,100].
3.4. Toxoplasmosis in immunocompromised humans
In immunocompromised humans a previously acquired latent infection can lead to reactivated toxoplasmosis with encephalitis. Toxoplasmic encephalitis and disseminated toxoplasmosis have been observed in patients with immunodeficiencies due to various causes, such as Hodgkin’s disease or immunosuppressive therapy because of other malignancies. Disseminated toxoplasmosis may also complicate transplantation of organs or bone marrow. This may result either from transplantation of an organ from a T. gondii-infected donor to a susceptible recipient or from reactivation of a latent T. gondii infection in the recipient due to immunosuppressive treatment [12,73,101].
T. gondii is also an important opportunistic pathogen in AIDS patients. World-wide, T. gondii causes severe encephalitis in up to 40% of AIDS patients, and 10–30% of AIDS patients infected with T. gondii succumb to the disease [73,101–104]. However, with highly active antiretroviral therapy (HAART) and immune reconstitution the incidence of CNS toxoplasmosis in AIDS patients is now declining in many countries, and reactivation of a latent infection can also be prevented by prophylaxis with trimethoprim-sulfamethoxyzole (TMX-Sulfa).
In addition to reactivated toxoplasmosis immunocompromised patients are at risk from severe disease following primary infection, which frequently presents as pulmonary disease or diffuse encephalitis [73].
4. How do humans acquire an infection with Toxoplasma gondii?
With incidences of prenatal infections ranging from 1 to 120 per 10 000 births (Table 5), and seroprevalences in women of childbearing age ranging from 4 to 85% (Table 3), only a small percentage of infections with T. gondii in adult human populations are acquired vertically. This raises the question of how humans acquire the infection postnatally. Not all possible routes of infection are important epidemiologically, and sources of infection may vary greatly among different ethnic groups and geographical locations. Therefore, knowledge on the more probable routes of horizontal transmission to humans and on the most likely sources of infection in a given population is a pre-requisite for the development of effective strategies for prevention of infection in risk groups, such as non-immune pregnant women and immunocompromised patients, in particular those with AIDS.
4.1. Tachyzoites
Tachyzoites play the major role in vertical transmission of T. gondii (see Section 3.3). By contrast, they are very sensitive to environmental conditions and are usually killed rapidly outside the host. Therefore, it is generally believed that horizontal transmissions of T. gondii infections via tachyzoites are not important epidemiologically. However, they may occur infrequently.
In recent years, it has been found that transplantation of heart, kidney, liver, and bone marrow may be complicated by T. gondii infections (see Section 3.4). In these cases either tachyzoites or tissue cysts may be involved [11,101]. Tachyzoites of T. gondii have also been transmitted via blood products, in particular those containing the white cell fraction, and by accidental injection in the laboratory [11,20,31,73,105]. However, parasitaemia usually occurs for only a short period of time after primary infection. Therefore, it has been suggested that there is only a low risk of acquiring an infection with T. gondii via ordinary blood transfusion [11].
Tachyzoites of T. gondii have been found in the milk of several intermediate hosts, including sheep, goats, and cows [11–13,20,23,31], but thus far, acute toxoplasmosis in humans has been associated only with consumption of unpasteurised goat’s milk [82,106–108]. Tachyzoites are sensitive to proteolytic enzymes and usually are destroyed by gastric digestion. However, a recent study showed that tachyzoites may occasionally survive for a short period of time (up to 2 h) in acid pepsin solutions, and that oral application of high doses of tachyzoites may cause an infection in mice and cats [109]. It has also been suggested that tachyzoites may enter the host by penetration of mucosal tissue and thereby gain access to the host’s circulation or lymphatic system before reaching the stomach [23,82,106]. This may also explain a recent report of toxoplasmosis in a breast-fed infant whose mother acquired a primary infection with T. gondii [110]. However, tachyzoites are sensitive to temperature and, thus, it is interesting to note that in a family of goat owners T. gondii was transmitted to two children who frequently consumed unpasteurised goat’s milk while their parents who only had small amounts of goat’s milk in tea or coffee remained seronegative [20,108]. Tachyzoites are killed by pasteurisation and heating. Therefore, it is advisable that milk, in particular goat’s milk, should be pasteurised or boiled before human consumption. This is particularly important for its use in infants who have a lower concentration of proteolytic enzymes in the digestive tube and who are more susceptible to toxoplasmosis than adults. A recent study assessing risk factors associated with primary T. gondii infections in women of childbearing age suggested that in Poland drinking milk may be a potential risk factor for horizontal transmission to humans [111]. In the past, it has often been thought that the risk of acquiring an infection with T. gondii by drinking cow’s milk, if any, is minimal [11,12,14,39], but it cannot be excluded that any type of milk is a potential source of infection if consumed raw. Likewise, it has been suggested that the high seroprevalence of T. gondii (67%) in pastoral camels in Sudan may be of public health significance for nomads who consume cameline milk raw [112].
In addition to blood and milk, tachyzoites have been detected in other body fluids, including saliva, sputum, urine, tears, and semen [11,20,31], but there is currently no evidence of horizontal transmission of T. gondii to humans via any of these routes. An early study reported that T. gondii tachyzoites may be isolated from raw chicken eggs laid by hens with experimentally induced infection [113]. However, commercially raised poultry is virtually free of T. gondii infection (see Section 4.2.1). In addition, tachyzoites are highly susceptible to both heating and salt concentration and, thus, any type of cooking would kill tachyzoites in eggs.
In general, it is believed that the majority of horizontal transmissions to humans are caused by ingestion of one of the two persistent stages of T. gondii, i.e. tissue cysts in infected meat or offals (viscera) and oocysts in food or water contaminated with feline faeces [11,13,114–116].
4.2. Tissue cysts
4.2.1. Importance and prevalence of infections with Toxoplasma gondii in meat-producing animals
Tissue cysts of T. gondii contained in meat of livestock are an important source of infection for humans (Fig. 2). Tissue cysts may develop as early as 6–7 days after infection of intermediate hosts by both oocysts or other tissue cysts [35]. They probably persist for the life of the host (see Section 2). However, the number of tissue cysts that may develop inside a certain host and the locations parasitised vary with the intermediate host species [35,114,116–118]. In meat-producing animals, tissue cysts of T. gondii are most frequently observed in tissues of infected pigs, sheep, and goats, and less frequently in infected poultry, rabbits, dogs, and horses (Fig. 3). Tissue cysts are found only rarely in beef or buffalo meat, although antibodies in up to 92% of cattle and up to 20% of buffaloes are evidence of past exposure to the parasite (Table 6).
Fig. 3.
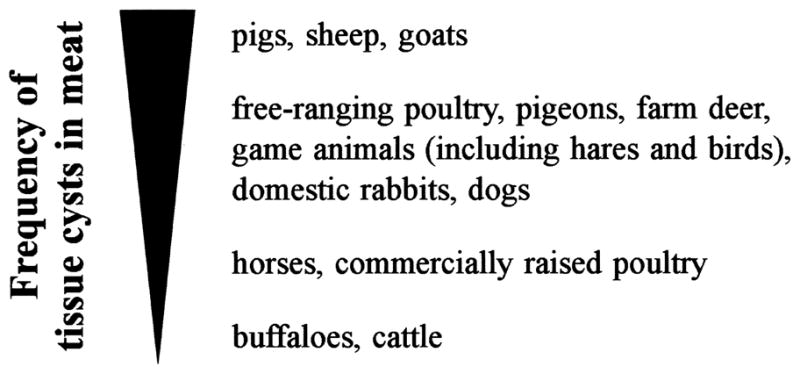
Relative importance of meat-producing and game animals in the transmission of T. gondii to humans, adapted from the Report on the WHO Workshop on Public Health Aspects on Toxoplasmosis, Meeting of the Working Groups ‘Husbandry, Household and Environment’ and ‘Food Hygiene’, Bilthoven, The Netherlands, 23rd-24th October, 1989 and from Refs. [116–118].
Table 6.
Seroprevalences of T. gondii infection in cattle and buffaloes (1990–2000)
| Country | Year of samplinga | Seroprevalence (%)b | Number of samples tested (n)b | Methodc | Reference |
|---|---|---|---|---|---|
| Cattle | |||||
| Argentina | < 1990 | 39 | 249 | IHAT | [390] |
| Bangladesh | < 1993 | 16 | 205 | LAT | [391] |
| Brazil | < 1994 | 32 | 334 | IFAT | [392] |
| 1996 | 1 | 194 | LAT | [393] | |
| < 1999 | 26 | 400 | IFAT | [394] | |
| China | < 1990 | 4 | 90 | IHAT | [151] |
| < 1991 | 1 | 208 | IHAT | [395] | |
| Costa Rica | 1991 | 34 | 601 | IFAT | [396] |
| Czech Republic | 1979–90 | 4 | 1926 | SFDT | [397] |
| 1979–90 | 2 | 1238 | CFT | [397] | |
| 1981–90 | 22 | 218 | SFDT | [397] | |
| 1981–90 | 3 | 176 | CFT | [397] | |
| Djibouti | < 1994 | 3 | 499 | IHAT | [398] |
| Egypt | < 1990 | 21 | 19 | IHAT | [399] |
| < 1997 | 49 | 39 | IHAT | [400] | |
| < 1997 | 49 | 39 | IFAT | [400] | |
| France | < 1997 | 69 | 364 | IFAT | [401] |
| Greece | < 1992 | 40 | 1890 | CFT | [402] |
| India | < 1991 | 43 | 102 | DAT | [403] |
| < 1992 | 9 | 32 | LAT | [404] | |
| Iran | 1984–88 | 15 | 142 | LAT | [405] |
| < 1996 | 0 | 2000 | LAT | [406] | |
| < 1996 | 0 | 2000 | IHAT | [406] | |
| Iraq | 1989–90 | 48 | 204 | CFT | [407] |
| Israel | 1985–90 | 15 | 172 | IFAT | [408] |
| Italy | < 1993 | 92 | 255 | DAT | [409] |
| Malaysia | < 1990 | 0 | 132 | IHAT | [410] |
| Mexico | 1990–91 | 28 | 300 | SFDT | [411] |
| < 1993 | 12 | 397 | ELISA | [412] | |
| Netherlands | < 1995 | 13–43** | 6976* | ELISA | [122] |
| Norway | 1989 | 5 | 1053 | ELISA | [145] |
| Pakistan | 1993 | 25 | 100 | LAT | [413] |
| Portugal | 1988–90 | 43 | 60 | DAT | [414] |
| Reunion | 1987 | 54 | 780 | ELISA | [415] |
| Saudi Arabia | < 2000 | 2 | 60 | IHAT | [416] |
| Spain | < 1991 | 41 | 304 | MAT | [417] |
| < 1991 | 40 | 304 | IFAT | [417] | |
| Switzerland | 1994 | 14 | 148 | ELISA | [418] |
| Thailand | 1996–97 | 3 | 119 | LAT | [419] |
| Trinidad | < 1996 | 27 | 55 | DAT | [420] |
| Turkey | < 1994 | 9 | 272 | IHAT | [421] |
| < 1995 | 4 | 280 | ELISA | [422] | |
| < 1995 | 5 | 280 | IHAT | [422] | |
| < 1997 | 63* | 203* | SFDT | [423] | |
| 1997–98 | 66 | 106 | SFDT | [424] | |
| Vietnam | 1995 | 11 | 200 | DAT | [425] |
| Buffaloes | |||||
| Brazil | 1996 | 4 | 104 | LAT | [393] |
| China | < 1990 | 0 | 83 | IHAT | [151] |
| Egypt | < 1990 | 20 | 15 | IHAT | [399] |
| < 1998 | 0 | 75 | DAT | [426] | |
| India | < 1992 | 10 | 48 | LAT | [404] |
| Iran | 1995–96 | 9 | 385 | IFAT | [427] |
| Vietnam | 1995 | 3 | 200 | DAT | [425] |
Years of sampling are listed as published in the references. In cases where this information was not available, the year listed here is the year when the study was published, as indicated by ‘<’. Data from the 1980s are included if the study was published in the 1990s and if no recent data were available for the area.
Figures marked with ‘*’ were calculated from the published data. Seroprevalences marked with ‘**’ varied with the herd examined.
CFT, complement fixation test; DAT, direct agglutination test; ELISA, enzyme-linked immunosorbent assay; IFAT, indirect immunofluorescent antibody test; IHAT, indirect haemagglutination test; LAT, latex agglutination test; MAT, modified agglutination test; SFDT, Sabin–Feldman dye test.
In Europe and in the USA, pork has generally been considered to be a major source of T. gondii infection in humans [115–117,119]. This hypothesis is based on the fact that tissue cysts have been found in most commercial cuts of pork [120,121], and on estimates for prevalences of T. gondii infection in pigs that were made in the 1970s or 1980s [11]. However, depending on the method used to obtain such estimates, these data vary greatly among different countries and among different farms within the same country. In most countries epidemiological data on infections with T. gondii in livestock are not regularly monitored. Recent studies on fattening pigs raised on farms using intensive management in the Netherlands, Austria, and Germany demonstrated that the prevalence of T. gondii infection in pigs has decreased significantly, (i.e. to <1%) over the last decade with changes in pig production and management (Table 7) [114,118,122]. Seroprevalences of T. gondii infection in fattening pigs raised on farms using intensive management have now been found to be <10% in many countries (Table 8). In addition, in several countries of the European Union seroprevalences in older pigs, such as sows, which are usually kept on farms with more extensive management and, consequently, are more frequently exposed to the environment than fattening pigs, also decreased distinctly (Table 7).
Table 7.
Changes in seroprevalences of T. gondii infection in fattening pigs and sows between 1960 and 2000 in selected European countries now using intensive farm management
| Country | Year of samplinga | Seroprevalence (%)b | Number of samples tested (n) | Methodc | Reference |
|---|---|---|---|---|---|
| Fattening pigs | |||||
| Austria | < 1975 | 32 | 100 | SFDT | [428] |
| 1982 | 12 | 2238 | IFAT | [429] | |
| < 1990 | 4 | 2755 | CFT | [430] | |
| 1992 | < 1 | 2300 | IFAT | [429] | |
| Germany | 1962–64 | 12–97** | 500 | SFDT | [431] |
| 1974 | 9 | 1366 | SFDT | [432] | |
| 1980 | 16 | 834 | IFAT, IHAT | [433] | |
| 1993–95 | < 1 | 60 | ELISA | [434] | |
| Netherlands | < 1969 | 54 | 50 | SFDT | [435] |
| < 1982 | 0 | 196 | ELISA | [436] | |
| < 1991 | 2 | 23348 | ELISA | [437] | |
| < 1995 | < 2 | 994 | ELISA | [122] | |
| Sows | |||||
| Austria | < 1990 | 3 | 1162 | CFT | [430] |
| 1992 | 4 | 46 | IFAT | [429] | |
| Germany | < 1982 | 32 | 95 | IFAT, IHAT | [433] |
| 1993–95 | 8 | 90 | ELISA | [434] | |
| 1997–99 | 18 | . 2000 | ELISA | [438] | |
| Netherlands | < 1969 | 86 | 50 | SFDT | [435] |
| < 1982 | 11 | 36 | ELISA | [436] | |
| < 1995 | 31 | 1009 | ELISA | [122] | |
Years of sampling are listed as published in the references. In cases where this information was not available, the year listed here is the year when the study was published, as indicated by ‘<’.
Seroprevalences marked with ‘**’ varied with the cut-off titre used in the SFDT.
CFT, complement fixation test; ELISA, enzyme-linked immunosorbent assay; IFAT, indirect immunofluorescent antibody test; IHAT, indirect haemagglutination test; SFDT, Sabin–Feldman dye test.
Table 8.
Seroprevalences of T. gondii infection in pigs (1990–2000)
| Country | Year of samplinga | Seroprevalence (%)b | Number of samples tested (n)b | Methodc | Reference |
|---|---|---|---|---|---|
| Fattening/slaughter pigs | |||||
| Argentina | < 1998 | 43 | 388 | IHAT | [439] |
| < 1998 | 43 | 388 | IFAT | [439] | |
| Austria | < 1990 | 4 | 2755 | CFT | [430] |
| 1992 | < 1 | 2300 | IFAT | [429] | |
| Brazil | < 1992 | 90 | 198 | IFAT | [440] |
| < 1997 | 7–54** | 792* | IFAT | [441] | |
| < 1998 | 9–61** | 792* | ELISA | [442] | |
| Canada | 1990 | 9 | 1443 | MAT | [443] |
| 1991–92 | 9* | 2800 | LAT | [444] | |
| Chile | 1984 | 30 | 1474 | IHAT | [445] |
| 1984 | 28 | 1474 | SFDT | [445] | |
| Czech Republic | 1979–90 | 6 | 2616 | SFDT | [446] |
| 1979–90 | < 1 | 1179 | CFT | [446] | |
| 1981–90 | 32 | 287 | SFDT | [447] | |
| 1981–90 | 11 | 215 | CFT | [447] | |
| 1988–90 | 35 | 57 | SFDT | [446] | |
| 1988–90 | 14 | 57 | CFT | [446] | |
| Finland | 1984 | 3 | 1847 | ELISA | [448] |
| Germany | 1993–95 | 0 | 60 | ELISA | [434] |
| Italy | < 1991 | 64 | 90 | IFAT | [449] |
| Japan | 1992–93 | 3 | 423 | LAT | [450] |
| Mexico | < 1993 | 9 | 1203 | ELISA | [412] |
| Netherlands | < 1991 | 2 | 23348 | ELISA | [437] |
| < 1995 | 2 | 994 | ELISA | [122] | |
| Norway | 1993–94 | 3 | 1605 | ELISA | [145] |
| Poland | < 1991 | 36 | 925 | ELISA | [147] |
| Portugal | 1988–90 | 5 | 300 | DAT | [414] |
| Trinidad | 1992–95 | 6 | 55 | CAT | [420] |
| USA | |||||
| Illinois | 1992 | 3 | 1885 | MAT | [451] |
| Illinois | 1992–93 | 21 | 4252 | MAT | [452] |
| Iowa | < 1990 | 5 | 2029 | ELISA | [453] |
| Iowa | < 1995 | 22 | 1000 | MAT | [454] |
| N Carolina | 1994–95 | < 1* | 2312 | MAT | [455] |
| N Carolina | < 1998 | 1 | 3990 | MAT | [456] |
| Tennessee | 1991–92 | 3 | 437 | MAT | [455] |
| Zimbabwe | < 1992 | 1 | 211 | LAT | [457] |
| < 1992 | 0 | 211 | ELISA | [457] | |
| 1995 | 9 | 97 | MAT | [458] | |
| Sows | |||||
| Austria | < 1990 | 3 | 1162 | CFT | [430] |
| 1992 | 4 | 46 | IFAT | [429] | |
| Germany | 1993–95 | 8 | 90 | ELISA | [434] |
| 1997–99 | 18 | . 2000 | ELISA | [438] | |
| Japan | 1992–93 | 13 | 141 | LAT | [450] |
| Netherlands | < 1995 | 31 | 1009 | ELISA | [122] |
| USA | |||||
| 17 states | 1990 | 20 | 3479 | MAT | [455] |
| Illinois | 1992 | 21 | 5080 | MAT | [451] |
| Illinois | 1992–93 | 15 | 2617 | MAT | [452] |
| Iowa | < 1990 | 10 | 587 | ELISA | [453] |
| Iowa | < 1992 | 14 | 273 | MAT | [459] |
| Tennessee | 1991–92 | 29* | 3841 | MAT | [460] |
| Zimbabwe | < 1992 | 10 | 100 | ELISA | [457] |
| Not classified | |||||
| Brazil | < 1990 | 38 | 1131 | IFAT | [461] |
| < 1995 | 100 | 200 | IHAT | [462] | |
| < 1999 | 24 | 267 | IFAT | [394] | |
| China | < 1990 | 10 | 816 | IHAT | [151] |
| < 1991 | 20 | 525 | IHAT | [395] | |
| Costa Rica | 1991 | 44 | 496 | IFAT | [396] |
| Czech Republic | 1981–90 | 31 | 230 | SFDT | [446] |
| 1981–90 | 10 | 158 | CFT | [446] | |
| Ghana | 1997–98 | 39 | 641 | ELISA | [463] |
| Malaysia | < 1990 | 16 | 122 | IHAT | [410] |
| Poland | < 1991 | 36 | 925 | ELISA | [147] |
| Taiwan | 1978–88 | 28 | 3880 | LAT | [464] |
| USA | |||||
| Hawaii | < 1992 | 49 | 509 | DAT | [465] |
| New England | < 1999 | 47 | 1897 | MAT | [466] |
Years of sampling are listed as published in the references. In cases where this information was not available, the year listed here is the year when the study was published, as indicated by ‘<’. Data from the 1980s are included if the study was published in the 1990s and if no recent data were available for the area.
Figures marked with ‘*’ were calculated from the published data. Seroprevalences marked with ‘**’ varied with the herd examined.
CAT, card agglutination test; CFT, complement fixation test; DAT, direct agglutination test; ELISA, enzyme-linked immunosorbent assay; IFAT, indirect immunofluorescent antibody test; IHAT, indirect haemagglutination test; LAT, latex agglutination test; MAT, modified agglutination test; SFDT, Sabin– Feldman dye test.
These data show that it is possible to significantly reduce the risk of T. gondii infection in livestock using intensive farm management with adequate measures of hygiene, confinement, and prevention. These measures include: (A) to keep meat-producing animals indoors throughout their life-time, (B) to keep the sheds free of rodents, birds, and insects, (C) to feed meat-producing animals on sterilised food, and (D) to control access to sheds and feed stores, i.e. no pet animals should be allowed inside them [117]. Using such preventive measures, it is economically possible to produce pigs and poultry free of T. gondii infection (Tables 7–9), although this has been achieved in only a few countries, i.e. in the Netherlands, Denmark, and the former German Democratic Republic [117,122].
Table 9.
Seroprevalences of T. gondii infection in domestic and wild fowl (1990–2000)
| Country | Year of samplinga | Seroprevalence (%)b | Number of samples tested (n)b | Methodc | Reference |
|---|---|---|---|---|---|
| Chickens | |||||
| Brazil | < 2000 | 10 | 155 | IFAT | [467] |
| China | < 1995 | 3* | 109 | – | [468] |
| Czech Republic | 1981–90 | 1–5** | 4458* | SFDT | [469] |
| India | < 1998 | 40 | 185 | MAT | [470] |
| Iran | < 1990 | 33* | 101 | IHAT | [471] |
| Japan | 1995 | 6* | 50 | LAT | [472] |
| Malaysia | < 1990 | 17 | 48 | IHAT | [410] |
| Pakistan | 1993 | 0 | 64 | LAT | [413] |
| Turkey | 1995–96 | 2 | 140 | SFDT | [473] |
| Ducks | |||||
| China | < 1995 | 4* | 82 | – | [468] |
| Czech Republic | 1981–90 | 2 | 297 | SFDT | [469] |
| Iran | < 1990 | 0 | 8 | IHAT | [471] |
| Turkey | 1995–96 | 0 | 55 | SFDT | [473] |
| Geese | |||||
| Czech Republic | 1981–90 | 16 | 32 | SFDT | [469] |
| Iran | < 1990 | 50* | 8 | IHAT | [471] |
| Turkey | 1995–96 | 4 | 45 | SFDT | [473] |
| Pigeons | |||||
| Iran | < 1990 | 33* | 12 | IHAT | [471] |
| Turkey | 1996–97 | 0 | 60 | SFDT | [474] |
| USA (New Jersey) | 1986–87 | 6* | 34 | MAT | [152] |
| Turkeys | |||||
| Iran | < 1990 | 24* | 25 | IHAT | [471] |
| Turkey | 1995–96 | 0 | 60 | SFDT | [473] |
| Wild turkeys | |||||
| USA (Alabama) | < 1994 | 71 | 17 | MAT | [475] |
| USA (West Virginia) | 1993 | 10 | 130 | – | [153] |
Years of sampling are listed as published in the references. In cases where this information was not available, the year listed here is the year when the study was published, as indicated by ‘<’. Data from the 1980s are included if the study was published in the 1990s and if no recent data were available for the area.
Figures marked with ‘*’ were calculated from the published data. Seroprevalences marked with ‘**’ varied with the herd examined.
IFAT, indirect immunofluorescent antibody test; IHAT, indirect haemagglutination test; LAT, latex agglutination test; MAT, modified agglutination test; SFDT, Sabin–Feldman dye test; –, not reported.
By contrast, production of free-ranging livestock will inevitably be associated with T. gondii infection. Animals kept on pastures with an increased pressure of infection due to contamination of the environment with oocysts (see Section 4.3.2), such as sheep and goats, show high seroprevalences in many areas of the world, i.e. up to 92 and 75%, respectively, (Tables 10 and 11). This is of particular importance, because tissue cysts have been found in many edible parts of sheep [123,124], and small ruminants are important in both milk and meat production throughout the world (see Sections 4.1 and 4.2.4).
Table 10.
Seroprevalences of T. gondii infection in sheep (1990–2000)
| Country | Year of samplinga | Seroprevalence (%)b | Number of samples tested (n)b | Methodc | Reference |
|---|---|---|---|---|---|
| Lambs | |||||
| Zimbabwe | < 1992 | 6 | 107 | IFAT | [457] |
| < 1992 | 3 | 107 | ELISA | [457] | |
| Slaughter sheep | |||||
| Djibouti | < 1994 | 10 | 486 | IHAT | [398] |
| Egypt | < 1990 | 29 | 17 | IHAT | [399] |
| Indonesia | < 1998 | 60 | 123 | IHAT | [476] |
| Iran | 1984–88 | 14 | 138 | LAT | [405] |
| Norway | 1993 | 18 | 2070 | ELISA | [145] |
| 1993 | 16 | 1940 | ELISA | [146] | |
| Pakistan | 1993 | 3 | 40 | LAT | [413] |
| Saudi Arabia | < 1997 | 39 | 100 | IHAT | [477] |
| Trinidad | < 1996 | 36 | 14 | CAT | [420] |
| Turkey | 1993–94 | 37 | 712 | SFDT | [478] |
| USA (North East) | < 1990 | 59 | 654 | ELISA | [479] |
| Farmed sheep | |||||
| Austria | < 1991 | 72 | 531 | CFT | [480] |
| < 1996 | 66 | 4079 | IFAT | [114] | |
| Bangladesh | < 1993 | 64 | 56 | LAT | [481] |
| Brazil | < 1999 | 52 | 228 | IFAT | [394] |
| Cameroon | < 1994 | 32 | 211 | LAT | [482] |
| Canada | 1988 | 58 | 3872 | ELISA | [483] |
| Chile | < 1999 | 28 | 408 | IFAT | [484] |
| < 1999 | 12 | 408 | IHAT | [484] | |
| China | < 1991 | 7 | 202 | IHAT | [395] |
| Croatia | < 1994 | 4 | 95 | DAT | [485] |
| Czech Republic | 1982–89 | 55 | 886 | SFDT | [486] |
| 1982–89 | 40 | 484 | CFT | [486] | |
| 1986–90 | 46–74** | 661* | SFDT | [486] | |
| 1986–90 | 13–23** | 650* | CFT | [486] | |
| France | < 1997 | 92 | 642 | IFAT | [401] |
| Germany | 1993–95 | 33 | 1122 | ELISA | [434] |
| < 1997 | 21 | 151 | IFAT | [487] | |
| Greece (Crete) | < 1995 | 23 | 8700 | ELISA | [488] |
| India | < 1993 | 23 | 88 | DAT | [489] |
| Ireland | < 1990 | 56 | 837 | IHAT | [490] |
| Israel | 1985–90 | 25 | 372 | IFAT | [408] |
| Jordan | 1989–90 | 21 | 176 | LAT | [491] |
| < 1993 | 21 | 559 | LAT | [492] | |
| Malaysia | < 1990 | 23 | 106 | IHAT | [410] |
| Mexico | < 1990 | 30 | 495 | IFAT | [493] |
| Niger | < 1991 | 14 | 70 | LAT | [494] |
| Nigeria | < 1993 | 12 | 206 | LAT | [495] |
| Slovakia | 1988–91 | 10 | 1939 | CFT | [496] |
| Spain | < 1991 | 40 | 550 | DAT | [497] |
| < 1991 | 35 | 550 | IFAT | [497] | |
| 1992–93 | 12 | 541 | MAT | [498] | |
| < 1996 | 38 | 3212 | DAT | [499] | |
| < 1996 | 35 | 2306 | MAT | [500] | |
| < 1996 | 34 | 2306 | IFAT | [500] | |
| Suriname | 1994 | 67 | 106 | MAT | [501] |
| Sweden | < 1992 | 19 | 704 | ELISA | [502] |
| Turkey | 1990–92 | 26 | 259 | IHAT | [422] |
| 1990–92 | 22 | 259 | ELISA | [422] | |
| < 1992 | 23–31** | 295* | IHAT | [503] | |
| < 1997 | 89 | 62 | SFDT | [504] | |
| < 1997 | 40 | 531 | SFDT | [505] | |
| 1997–98 | 34 | 154 | SFDT | [424] | |
| United Kingdom | 1990 | 29 | 202 | LAT | [506] |
| Uruguay | 1991 | 14–29** | 573* | LAT | [507] |
| 1992 | 28 | 422 | DAT | [508] | |
| 1992–94 | 39 | 1613 | DAT | [509] | |
| Zimbabwe | < 1992 | 9 | 109 | ELISA | [457] |
| Unclassified | |||||
| Bangladesh | < 1993 | 18 | 17 | LAT | [391] |
| Benin | < 1996 | 0 | 21 | IHAT | [510] |
| Brazil | < 1995 | 48 | 370 | IFAT | [511] |
| 1996 | 19 | 240 | IFAT | [393] | |
| Burkina Faso | < 1996 | 23 | 65 | IHAT | [510] |
| China | < 1996 | 29 | 56 | IHAT | [512] |
| Côte d’Ivore | < 1996 | 68 | 62 | IHAT | [510] |
| Djibouti | < 1996 | 13 | 183 | IHAT | [510] |
| Ethiopia | < 1996 | 26 | 94 | IHAT | [510] |
| Ghana | 1997–98 | 33 | 732 | ELISA | [513] |
| Iran | < 1996 | 25 | 1102 | IHAT | [406] |
| < 1996 | 24 | 2209 | LAT | [406] | |
| Mexico | 1988 | 38 | 702 | IFAT | [514] |
| Niger | < 1996 | 20 | 77 | IHAT | [510] |
| Saudi Arabia | < 2000 | 3 | 150 | IHAT | [416] |
| Senegal | < 1993 | 55 | 190 | ELISA | [515] |
| < 1993 | 46 | 190 | IFAT | [515] | |
| < 1996 | 12 | 52 | IHAT | [510] | |
| Turkey | 1994 | 72 | 414 | IFAT | [516] |
| 1994 | 69 | 414 | SFDT | [516] | |
| 1994 | 37 | 414 | LAT | [516] | |
| 1994–95 | 15 | 1050 | LAT | [517] | |
Years of sampling are listed as published in the references. In cases where this information was not available, the year listed here is the year when the study was published, as indicated by ‘<’. Data from the 1980s are included if the study was published in the 1990s and if no recent data were available for the area.
Figures marked with ‘*’ were calculated from the published data. Seroprevalences marked with ‘**’ varied with the herd examined.
CAT, card agglutination test; CFT, complement fixation test; DAT, direct agglutination test; ELISA, enzyme-linked immunosorbent assay; IFAT, indirect immunofluorescent antibody test; IHAT, indirect haemagglutination test; LAT, latex agglutination test; MAT, modified agglutination test; SFDT, Sabin– Feldman dye test.
Table 11.
Seroprevalences of T. gondii infection in goats (1990–2000)
| Country | Year of samplinga | Seroprevalence (%)b | Number of samples tested (n)b | Methodc | Reference |
|---|---|---|---|---|---|
| Kids | |||||
| Jordan | 1989–90 | 19 | 69 | LAT | [491] |
| Slaughter goats | |||||
| Bangladesh | 1994–95 | 13 | 528 | LAT | [518] |
| Djibouti | < 1994 | 6 | 554 | IHAT | [398] |
| < 1996 | 21 | 176 | IHAT | [510] | |
| Egypt | < 1990 | 29 | 14 | IHAT | [399] |
| Indonesia | < 1998 | 40 | 38 | IHAT | [476] |
| Iran | 1984–88 | 13 | 130 | LAT | [405] |
| Pakistan | 1993 | 0 | 58 | LAT | [413] |
| Saudi Arabia | < 1997 | 28 | 100 | IHAT | [477] |
| Zimbabwe | < 1992 | 5 | 156 | ELISA | [457] |
| Farmed goats | |||||
| Austria | < 1996 | 69 | 687 | IFAT | [114] |
| Bangladesh | < 1993 | 54 | 33 | LAT | [481] |
| < 1993 | 12 | 306 | LAT | [391] | |
| Botswana | 1994–96 | 10 | 345 | IHAT | [519] |
| Brazil | 1993 | 16 | 202 | IFAT | [520] |
| < 1994 | 31 | 153 | IFAT | [521] | |
| Croatia | 1992 | 4–14** | 179* | MAT | [522] |
| Czech Republic | 1981–90 | 61 | 54 | SFDT | [486] |
| 1981–90 | 21 | 54 | CFT | [486] | |
| Djibouti | < 1996 | 31 | 35 | IHAT | [510] |
| Ethiopia | < 1996 | 20 | 133 | IHAT | [510] |
| Germany | 1993–95 | 42 | 69 | ELISA | [434] |
| < 1997 | 19 | 829 | IFAT | [487] | |
| Greece (Crete) | < 1995 | 14 | 2320 | ELISA | [488] |
| Jordan | < 1993 | 17 | 305 | LAT | [492] |
| Malaysia | 1991–92 | 35 | 400 | MAT | [523] |
| < 1996 | 18 | 107 | IHAT | [410] | |
| Mexico | < 1993 | 3 | 707 | ELISA | [412] |
| New Zealand | < 1991 | 35 | 185 | IFAT | [524] |
| < 1991 | 32 | 185 | LAT | [524] | |
| Netherlands | < 1998 | 47 | 189 | DAT | [525] |
| Nigeria | < 1993 | 5 | 248 | LAT | [495] |
| Reunion | 1987 | 75 | 395 | ELISA | [415] |
| Senegal | < 1996 | 4 | 144 | IHAT | [510] |
| Spain (Grand Canary Island) | < 1995 | 63 | 1052 | ELISA | [526] |
| Turkey | 1990–92 | 15 | 66 | IHAT | [422] |
| 1990–92 | 12 | 66 | ELISA | [422] | |
| < 1997 | 63 | 38 | SFDT | [504] | |
| 1997 | 44 | 98 | SFDT | [527] | |
| USA | < 1990 | 65 | 99 | MAT | [528] |
| < 1990 | 55 | 99 | IHAT | [528] | |
| Venezuela | < 1998 | 6 | 438 | IHAT | [529] |
| Unclassified | |||||
| Brazil | 1996 | 29 | 439 | LAT | [393] |
| China | < 1996 | 26 | 1028 | IHAT | [512] |
| Czech Republic | 1994 | 20 | 247 | CFT | [530] |
| 1994–96 | 30* | 202 | CFT | [531] | |
| 1996 | 60–66** | 159* | IFAT | [531] | |
| 1994–97 | 45* | 203 | CFT | [531] | |
| Egypt | < 1997 | 51 | 78 | IFAT | [400] |
| < 1997 | 49 | 78 | IHAT | [400] | |
| France | < 1997 | 0–77** | 765 | ELISA | [532] |
| Ghana | 1997–98 | 27 | 526 | ELISA | [513] |
| India | < 1993 | 68 | 95 | DAT | [489] |
| Iran | < 1993 | 20 | 530 | LAT | [406] |
| Mexico | < 1990 | 44 | 211 | IFAT | [493] |
| Saudi Arabia | < 2000 | 4 | 56 | IHAT | [416] |
| Sri Lanka | 1989 | 22 | 139 | MAT | [533] |
| Turkey | 1996 | 54 | 68 | SFDT | [534] |
| Uganda | 1996 | 31 | 784 | ELISA | [535] |
| USA | 1982–84 | 22 | 1000 | MAT | [536] |
Years of sampling are listed as published in the references. In cases where this information was not available, the year listed here is the year when the study was published, as indicated by ‘<’. Data from the 1980s are included if the study was published in the 1990s and if no recent data were available for the area.
Figures marked with ‘*’ were calculated from the published data. Seroprevalences marked with ‘**’ varied with the herd examined.
CFT, complement fixation test; DAT, direct agglutination test; ELISA, enzyme-linked immunosorbent assay; IFAT, indirect immunofluorescent antibody test; IHAT, indirect haemagglutination test; LAT, latex agglutination test; MAT, modified agglutination test; SFDT, Sabin–Feldman dye test.
Seroprevalences are distinctly lower and more varying in horses, rabbits, and poultry (Tables 9, 12 and 13). This may reflect epidemiological factors such as different types of confinement, hygiene of stables, and different types of feed. By contrast, seroprevalences are usually high in dogs, indicating their continuous exposure to a natural environment and the cumulative effect of age (Table 14).
Table 12.
Seroprevalences of T. gondii infection in horses (1990–2000)
| Country | Year of samplinga | Seroprevalence (%)b | Number of samples tested (n) | Methodc | Reference |
|---|---|---|---|---|---|
| Argentina | < 1990 | 20 | 20 | IHAT | [390] |
| 1986–98 | 13 | 76 | IFAT | [537] | |
| Brazil | 1994–96 | 32 | 561 | IFAT | [538] |
| < 1997 | 8* | 430 | SFDT | [539] | |
| < 1999 | 16 | 101 | MAT | [540] | |
| < 1999 | 12 | 173 | IFAT | [394] | |
| China | < 1991 | 2 | 132 | IHAT | [395] |
| Czech Republic | 1987 | 8 | 2886 | SFDT | [541] |
| Sweden | 1986–87 | < 1 | 219 | ELISA | [542] |
| Turkey | 1995 | 2 | 103 | SFDT | [543] |
| < 1997 | 8* | 60 | SFDT | [544] | |
| < 1998 | 8 | 194 | SFDT | [545] | |
| < 1998 | 6 | 194 | LAT | [545] | |
| < 1998 | 2 | 50 | SFDT | [546] | |
| USA | 1998 | 16 | 339 | SFDT | [547] |
| 1998 | 7 | 1788 | MAT | [547] |
Years of sampling are listed as published in the references. In cases where this information was not available, the year listed here is the year when the study was published, as indicated by ‘<’. Data from the 1980s are included if the study was published in the 1990s and if no recent data were available for the area.
Seroprevalences marked with ‘*’ were calculated from the published data.
ELISA, enzyme-linked immunosorbent assay; IFAT, indirect immunofluorescent antibody test; IHAT, indirect haemagglutination test; LAT, latex agglutination test; MAT, modified agglutination test; SFDT, Sabin–Feldman dye test.
Table 13.
Seroprevalences of T. gondii infection in rabbits (1990–2000)
| Country | Year of samplinga | Seroprevalence (%) | Number of samples tested (n) | Methodb | Reference |
|---|---|---|---|---|---|
| Chile | < 1990 | 13 | 143 | IHAT | [548] |
| China | < 1990 | 8 | 12 | IHAT | [151] |
| Czech Republic | 1981–86 | 53 | 366 | SFDT | [549] |
| Egypt | < 1991 | 20 | 100 | CIA | [550] |
| France | < 1990 | 6 | 187 | IFAT | [551] |
Years of sampling are listed as published in the references. In cases where this information was not available, the year listed here is the year when the study was published, as indicated by ‘<’. Data from the 1980s are included if the study was published in the 1990s and if no recent data were available for the area.
CIA, carbon immunoassay; IFAT, indirect immunofluorescent antibody test; IHAT, indirect haemagglutination test; SFDT, Sabin–Feldman dye test.
Table 14.
Seroprevalences of T. gondii infection in dogs (1990–2000)
| Country | Year of samplinga | Seroprevalence (%)b | Number of samples tested (n)b | Methodc | Reference |
|---|---|---|---|---|---|
| Argentina | 1988–94 | 60 | 232 | IFAT | [552] |
| Brazil | 1988–90 | 47 | 243 | IFAT | [553] |
| 1994 | 53 | 218 | IHAT | [554] | |
| < 1998 | 63 | 276 | ELISA | [555] | |
| < 1998 | 55 | 327 | IFAT | [556] | |
| < 1998 | 46 | 276 | IFAT | [555] | |
| < 1999 | 84 | 189 | IFAT | [557] | |
| Chile | < 1991 | 12 | 178 | IHAT | [558] |
| China | < 1997 | 5 | 101 | ELISA | [559] |
| Czech Republic | 1982–84 | 33–39** | 1393* | SFDT | [560] |
| 1982–84 | 12–15** | 1393* | CFT | [560] | |
| France | < 1998 | 39 | 3580 | IFAT | [561] |
| Iran | < 1993 | 31 | 100 | SFDT | [562] |
| Israel | < 1996 | 36 | 220 | IFAT | [563] |
| Italy | 1996 | 17 | 104 | IFAT | [564] |
| Pakistan | < 1992 | 17* | 12 | LAT | [565] |
| Spain | < 1997 | 47 | 97 | IFAT | [566] |
| Sweden | < 1994 | 30 | 398 | DAT | [567] |
| Taiwan | 1995–96 | 25 | 289 | LAT | [568] |
| 1995–96 | 8 | 658 | ELISA | [569] | |
| < 1998 | 20 | 105 | LAT | [570] | |
| 1997 | 20 | 51 | LAT | [571] | |
| Turkey | < 1996 | 85 | 52 | IFAT | [572] |
| < 1996 | 79 | 52 | SFDT | [572] | |
| < 1996 | 69 | 70 | SFDT | [573] | |
| < 1996 | 48 | 52 | LAT | [572] | |
| < 1997 | 72 | 50 | SFDT | [574] | |
| < 1997 | 46 | 50 | LAT | [574] | |
| < 1998 | 75* | 53 | SFDT | [575] | |
| USA (Kansas) | < 1990 | 25 | 229 | DAT | [576] |
Years of sampling are listed as published in the references. In cases where this information was not available, the year listed here is the year when the study was published, as indicated by ‘<’. Data from the 1980s are included if the study was published in the 1990s and if no recent data were available for the area.
Figures marked with ‘*’ were calculated from the published data. Seroprevalences marked with ‘**’ varied with the herd examined.
CFT, complement fixation test; DAT, direct agglutination test; ELISA, enzyme-linked immunosorbent assay; IFAT, indirect immunofluorescent antibody test; IHAT, indirect haemagglutination test; LAT, latex agglutination test; SFDT, Sabin–Feldman dye test.
4.2.2. Prevalence of infections with Toxoplasma gondii in game and wild animals
Tissue cysts of T. gondii in venison and other meat of wild animals, including hares, wild boars, deer and other cervids, kangaroos, and bears are another potential source of infection for humans. Hunters and their families may also become infected during evisceration and handling of game [39]. Thus, in addition to the frequent consumption of caribou meat (see Section 4.2.4), a recent outbreak of congenital toxoplasmosis in Inuits was associated with skinning of animals (wolf, fox, and marten) for fur by women during pregnancy [125]. These cases also show that toxoplasmosis in humans may occur in arctic regions, although T. gondii infections are less frequent in regions with a cold climate than in regions with a warm and humid climate (see Section 3.1). In addition to higher environmental pressure of infection, there is a cumulative effect of age in many wild animals which results in very high prevalences of infection. Some recent data on T. gondii infections in wild mammals and birds are contained in Tables 9 and 15.
Table 15.
Seroprevalences of T. gondii infection in game and wild animals (1990–2000)
| Country | Year of samplinga | Seroprevalence (%)b | Number of samples tested (n)b | Methodc | Reference |
|---|---|---|---|---|---|
| Wild boars | |||||
| Austria | 1990–93 | 19 | 269 | IFAT | [577] |
| Czech Republic | 1981–90 | 15 | 124 | SFDT | [154] |
| Germany | 1993–94 | 25 | 130 | IFAT | [578] |
| 1997 | 21 | 81 | IFAT | [579] | |
| 1997 | 19 | 81 | ELISA | [579] | |
| 1997 | 15 | 81 | SFDT | [579] | |
| Japan | < 1999 | 6 | 108 | LAT | [580] |
| USA | |||||
| South Carolina | 1993 | 37 | 149 | MAT | [581] |
| Tennessee | 1990 | 31 | 108 | MAT | [581] |
| Zimbabwe | < 1999 | 0 | 3 | MAT | [458] |
| Deer | |||||
| Brazil | 1990 | 27 | 66 | IHAT | [582] |
| 1995 | 12 | 41 | IFAT | [582] | |
| 1995 | 12 | 41 | ELISA | [582] | |
| Czech Republic | 1981–90 | 14–100** | 401 | SFDT | [154] |
| USA | |||||
| Alabama | < 1991 | 44 | 16 | DAT | [583] |
| California | 1987–91 | 7 | 276 | LAT | [584] |
| Kansas | 1989–93 | 44 | 106 | MAT | [585] |
| Minnesota | 1990–93 | 30 | 1367 | MAT | [586] |
| Ohio | 1996–98 | 44 | 147 | MAT | [587] |
| Pennsylvania | 1991 | 60 | 593 | MAT | [588] |
| Moose | |||||
| Canada | < 1990 | 15 | 125 | IHAT | [589] |
| Reindeer | |||||
| Finland | 1993–96 | 0–25** | 900* | DAT | [590] |
| Norway | 1993–94 | < 1 | 1677* | DAT | [590] |
| Gazelles and antelopes | |||||
| Saudi Arabia | 1990–91 | 0–6** | 608* | IHAT | [591] |
| Zimbabwe | < 1999 | 12–37** | 86* | MAT | [458] |
| Bears | |||||
| USA | |||||
| Alaska | 1988–91 | 15–18** | 520 | LAT | [592] |
| Florida | 1993–95 | 56 | 66 | LAT | [593] |
| N Carolina | 1996–97 | 84 | 143 | MAT | [594] |
| Pennsylvania | 1989–92 | 80 | 665 | DAT | [595] |
| Pennsylvania | 1992 | 80 | 322 | MAT | [596] |
| Pennsylvania | 1993 | 79 | 28 | MAT | [597] |
| Pennsylvania | 1993 | 75* | 28 | DAT | [597] |
| Pennsylvania | 1993 | 32* | 28 | LAT | [597] |
| Pennsylvania | 1993 | 21* | 28 | IHAT | [597] |
Years of sampling are listed as published in the references. In cases where this information was not available, the year listed here is the year when the study was published, as indicated by ‘<’.
Figures marked with ‘*’ were calculated from the published data. Seroprevalences marked with ‘**’ varied with the geographical area or the species examined.
DAT, direct agglutination test; ELISA, enzyme-linked immunosorbent assay; IFAT, indirect immunofluorescent antibody test; IHAT, indirect haemag-glutination test; LAT, latex agglutination test; MAT, modified agglutination test; SFDT, Sabin–Feldman dye test.
Some wild animals, such as Australian native marsupials, have evolved in the absence of T. gondii until cats were introduced to their environment only a few hundred years ago. As a consequence, these animals are highly susceptible to the parasite. Although seroprevalences of T. gondii infection in marsupials are usually lower than in mammals, kangaroo meat in particular has recently been recognised as a potential source of infection for humans, because it is very lean with little fat and, thus, is usually consumed rare or undercooked [126].
4.2.3. Survival of tissue cysts of Toxoplasma gondii in food for humans
Bradyzoites of T. gondii are more resistant to digestive enzymes, (i.e. pepsin and trypsin) than tachyzoites (see Section 4.1) [35,109,127]. Therefore, ingestion of viable tissue cysts by a non-immune host will usually result in an infection with T. gondii. Although tissue cysts are less resistant to environmental conditions than oocysts (see Section 4.3.2), they are relatively resistant to changes in temperature and remain infectious in refrigerated (1–4°C) carcasses or minced meat for up to 3 weeks [123,128], i.e. probably as long as the meat remains suitable for human consumption [116]. Tissue cysts also survive freezing at temperatures between −1 and −8°C for longer than a week [129]. Most tissue cysts are killed at temperatures of −12°C or lower [129,130], but occasionally some tissue cysts may survive deep-freezing [116]. It has also been suggested that some strains of T. gondii may be resistant to freezing [130].
By contrast, tissue cysts in meat are killed by heating to 67°C [116,128]. Survival of tissue cysts at lower temperatures depends on the duration of cooking. For example, under laboratory conditions tissue cysts remained viable at 60°C for about 4 min and at 50°C for about 10 min [128]. It is important to note that cooking for a prolonged period of time may be necessary under household conditions to achieve the temperatures that are required to kill all tissue cysts of T. gondii in all parts of the meat. Some tissue cysts will remain infectious if cooking procedures are used in which the meat is heated unevenly, for example microwave cooking [124].
Some studies suggested that tissue cysts are killed by commercial procedures of curing with salt, sucrose, or low temperature smoking [124,132]. Therefore, it has previously been suggested that processed meat is an unlikely source of infection for humans [114,119]. However, the survival time of tissue cysts varies greatly with the concentration of the salt solution and the temperature of storage [132]. Under laboratory conditions, tissue cysts were killed in 6% NaCl solution at all temperatures examined (4–20°C), but survived in aqueous solutions with lower concentration of salt for several weeks [132]. It has also been shown that salting does not necessarily kill tissue cysts in home-made pork sausages [133,134]. In one study, T. gondii tissue cysts were killed by 3% table salt after 3–7 days [133]. This is much later than the usual storage time for pork sausages and, thus, salting alone is probably not sufficient to prevent transmission to humans via tissue cysts.
Tissue cysts are killed by gamma irradiation at a dose of 1.0 kGy which has been approved by authorities in the USA [116,130]. However, irradiation of meat has only been approved in a few countries, it is only feasible in industrialised countries, and is opposed to by consumers in many regions of the world.
4.2.4. Food-borne outbreaks of toxoplasmosis in humans, risk factors, and preventive measures that reduce the risk of food-borne infection with Toxoplasma gondii
Recent outbreaks of acute toxoplasmosis in humans in various regions of the world demonstrate that the sources of infection vary greatly in different human populations with differences in culture and eating habits. In Canada, an outbreak of congenital toxoplasmosis in a settlement of Inuits in northern Quebec was associated with frequent consumption of caribou meat, in addition to skinning of fur animals (see Section 4.2.2), while seropositivity in pregnant women living in the same settlement was associated with consumption of dried seal meat, seal liver, and raw caribou meat [125,135]. In Australia, an outbreak of acute and congenital toxoplasmosis was associated with rare kangaroo meat and undercooked lamb satay which were consumed during a cocktail party in Queensland [136]. Consumption of raw mutton at a party has also been reported as a source of acute toxoplasmosis in humans in Brazil [85]. It is also important to consider that, in addition to meat, tissue cysts of T. gondii may form in visceral organs (see Section 2). Thus, an outbreak of acute toxoplasmosis in humans occurred after consumption of raw spleen and liver of a wild boar, and a second outbreak after consumption of raw liver of a domestic pig, in Korea where raw liver is believed to have special nutritional value [86]. In the latter cases, either tachyzoites or tissue cysts may have been involved.
While these reports highlight that the risk of acquiring an infection with T. gondii via meat or other edible parts of animals varies with cultural and eating habits in different human populations, data derived from outbreaks of acute toxoplasmosis are usually linked to an occasional point source of infection and, thus, do not necessarily reflect the major, epidemiologically important sources of infection for the whole population. For example, kangaroo meat has only recently become commercially available for human consumption in Australia [126], yet 35% of women of child-bearing age in Western Australia show serological evidence of previous exposure to T. gondii [137]. It has to be kept in mind that most infections with T. gondii in immunocompetent humans are asymptomatic and, thus, will not be recorded unless systematic screening programs for T. gondii infections are carried out in the population under study (see Section 5).
Only recently, comprehensive case-control studies have been aimed at identifying the different sources of infection with T. gondii in different human populations. In several studies associated with the European Research Network on Congenital Toxoplasmosis [138], a large number of women were screened for seroconversion during pregnancy [139–142]. A European multicentre study including selected cities in Belgium, Denmark, Italy, Norway, Switzerland, and the UK identified the consumption of undercooked lamb, beef, or game, contact with soil, and travel outside Europe and North America as strong risk factors for acquiring an infection with T. gondii, with 30–63% of infections in the various regions being attributed to consumption of undercooked or cured meat products [142]. Likewise, consumption of raw pork and tasting of raw meat during meal preparation were the principle risk factors for acquiring a T. gondii infection in a similar population in Poland [111]. Frequent consumption of meat or consumption of undercooked meat have also been associated with seroconversion or seropositivity for T. gondii in case-control studies on healthy adults in France, Yugoslavia, and the USA [141,143,144].
However, while consumption of raw or undercooked meat was consistently identified as a risk factor in all of these studies, the relative importance of the risk factor and the type of meat associated with it varied among different countries [142]. For example, in France consumption of undercooked beef was a stronger risk factor than consumption of undercooked lamb [141], in Norway consumption of undercooked lamb was a stronger risk factor than consumption of undercooked pork [140], whereas in Poland consumption of undercooked pork was the principle risk factor identified in the study [111]. These findings may reflect differences in eating habits of consumers or different prevalences of infection in meat-producing animals in these regions. Thus, in Norway up to 18% of sheep, but only 3% of slaughter pigs are infected with T. gondii [145,146], whereas 36% of slaughter pigs are infected in Poland [147].
To prevent food-borne horizontal transmission of T. gondii to humans, meat and other edible parts of animals should not be consumed raw or undercooked, i.e. they should be cooked thoroughly (67°C) before consumption. Although freezing alone is not a reliable means of rendering all tissue cysts non-infectious (see Section 4.2.3), deep-freezing meat (−12°C or lower) before cooking can reduce the risk of infection. In addition, meat should not be tasted during seasoning or cooking [111,142], which is of particular importance for non-immune pregnant women (see Sections 3.3 and 5.1). It is also essential that preventive measures to reduce the risk of horizontal transmission of T. gondii to humans via tissue cysts include a high standard of kitchen hygiene. Thus, in a case-control study in Norway, washing kitchen knives infrequently after preparation of raw meat was independently associated with an increased risk of primary infection during pregnancy [140]. Both tissue cysts and tachyzoites are killed by water [127] and, thus, hands and all kitchen utensils used for the preparation of uncooked meat or other food from animals should be cleaned thoroughly with hot water and soap [116].
4.3. Oocysts
4.3.1. Importance of cats in the epidemiology of infections with Toxoplasma gondii
Infections with T. gondii in cats are usually asymptomatic, and vertical transmissions occur only infrequently [11,36,148]. However, latent infections with T. gondii are common in domestic cats and wild felines throughout the world [11,36]. At least 17 species of wild felines have been reported to shed oocysts of T. gondii, i.e. European and African wild cats, Pallas cat, bobcat, leopard cat, Amur leopard cat, iriomote cat, ocelot, Geoffroy’s cat, Pampas cat, jaguarundi, cougar, leopard, jaguar, tiger, lion, and cheetah [149], and there is serological evidence of T. gondii infection in servals [150]. In domestic cats, antibodies to T. gondii may be detected in up to 74% of adult cat populations, depending on the type of feeding and whether cats are kept indoors or outdoors (Table 16). Seroprevalences are usually higher in stray or feral cats than in cats living in an urban or suburban environment. However, between 9 and 46% of pet cats in Europe, South America, and the USA show serological evidence of past exposure to the parasite, while seroprevalences of T. gondii infections in Asia have been estimated to range between 6 and 9% (Table 16).
Table 16.
Seroprevalences of T. gondii infection in cats (1990–2000)
| Country | Year of samplinga | Seroprevalence (%)b | Number of samples tested (n)b | Methodc | Reference |
|---|---|---|---|---|---|
| Pet cats | |||||
| Argentina | 1993 | 20 | 169 | IHAT | [598] |
| Brazil | 1996–97 | 18 | 248 | IFAT | [599] |
| Chile | < 1992 | 40 | 65 | IHAT | [600] |
| France | < 1997 | 43 | 519 | IFAT | [401] |
| < 1998 | 43 | 506 | IFAT | [561] | |
| Germany | 1989–90 | 46 | 231 | IFAT | [601] |
| 1989–90 | 31–47** | 218* | ELISA | [602] | |
| 1989–90 | 34–51** | 218* | IFAT | [602] | |
| 1992–94 | 34–61** | 465* | ELISA | [603] | |
| Italy | 1996 | 9 | 113 | IFAT | [564] |
| Japan | 1994–95 | 9 | 471 | LAT | [604] |
| < 1998 | 6 | 800 | LAT | [605] | |
| Mexico | < 1999 | 71 | 24 | ELISA | [606] |
| Singapore | < 1992 | 7 | 15 | LAT | [607] |
| Sweden | 1986–87 | 42 | 241 | ELISA | [542] |
| Taiwan | < 1990 | 8 | 117 | ELISA | [608] |
| Turkey | 1994 | 43 | 65 | SFDT | [609] |
| USA (Oklahoma) | 1987–88 | 22 | 618 | LAT | [610] |
| Stray or feral cats | |||||
| Australia | < 1997 | 50 | 18 | LAT | [611] |
| < 1999 | 40 | 103 | ELISA | [612] | |
| Bangladesh | 1995 | 33 | 24 | LAT | [282] |
| Brazil | < 1999 | 73 | 173 | IFAT | [557] |
| Germany | 1989–90 | 66 | 61 | IFAT | [601] |
| 1989–90 | 58 | 88 | ELISA | [602] | |
| 1989–90 | 56 | 88 | IFAT | [602] | |
| 1992–94 | 59 | 112 | ELISA | [603] | |
| 1998 | 66 | 259 | ELISA | [613] | |
| Italy | < 1997 | 33 | 490 | ELISA | [614] |
| < 1997 | 33 | 490 | DAT | [614] | |
| Japan | 1990–91 | 19 | 231 | LAT | [615] |
| Korea | < 1999 | 13 | 198 | ELISA | [131] |
| Singapore | < 1992 | 31 | 706 | LAT | [607] |
| United Kingdom (Oxfordshire) | < 1996 | 62 | 45 | IHAT | [616] |
| USA | |||||
| Illinois | 1992–93 | 68 | 391 | MAT | [452] |
| Iowa | < 1992 | 42 | 74 | MAT | [459] |
| Turkey | < 1995 | 70 | 53 | IHAT | [617] |
| Not classified | |||||
| Argentina | 1988–94 | 61 | 145 | IFAT | [552] |
| < 1997 | 35 | 55 | IFAT | [618] | |
| Austria | < 1996 | 48 | 456 | IFAT | [114] |
| Czech Republic | 1995–97 | 59 | 390 | IFAT | [619] |
| Japan | 1989–91 | 11 | 726 | LAT | [620] |
| Panama | 1990–92 | 32–61** | 141* | DAT | [155] |
| Poland | 1992–96 | 71 | 357 | DAT | [621] |
| Slovenia | < 1997 | 70 | 54 | IFAT | [622] |
| < 1997 | 59 | 54 | ELISA | [622] | |
| < 1997 | 57 | 54 | DAT | [622] | |
| Turkey | < 1998 | 56 | 36 | SFDT | [623] |
| < 1998 | 38 | 24 | SFDT | [624] | |
| United Kingdom (Scotland) | < 1993 | 19* | 158 | – | [625] |
| USA | < 1992 | 74 | 124 | ELISA | [626] |
Years of sampling are listed as published in the references. In cases where this information was not available, the year listed here is the year when the study was published, as indicated by ‘<’. Data from the 1980s are included if the study was published in the 1990s and if no recent data were available for the area.
Figures marked with ‘*’ were calculated from the published data. Seroprevalences marked with ‘**’ varied with the type of keeping or the year of examination.
DAT, direct agglutination test; ELISA, enzyme-linked immunosorbent assay; IFAT, indirect immunofluorescent antibody test; IHAT, indirect haemag-glutination test; LAT, latex agglutination test; MAT, modified agglutination test; SFDT, Sabin–Feldman dye test; –, not reported.
Domestic cats and other feline species may become infected with T. gondii either by ingesting infectious oocysts from the environment or by ingesting tissue cysts from intermediate hosts. For example, cats may ingest tissue cysts when feeding on food scraps containing meat or viscera of livestock or game animals. Cats that are allowed to hunt may become infected by feeding on carcasses of small mammals or birds infected with T. gondii (Fig. 2). Depending on the host species, the geographical area, and the season of the year, up to 73% of small rodents and up to 71% of wild birds may be infected with T. gondii (Table 9) [12,151–164].
After primary infection of cats with tissue cysts of T. gondii, the bradyzoites immediately initiate a phase of asexual proliferation which consists of numerous cycles of endopolygeny in the small intestine. The terminal stages of this proliferation initiate the sexual phase of reproduction which results in the formation of oocysts (see Section 2, Fig. 1). Almost all cats that have been infected primarily with tissue cysts shed oocysts after a prepatent period of 3–10 days, with patency lasting for up to 20 days [12,22,36,165]. By contrast, after primary infection with oocysts of T. gondii, the sporozoites first initiate a phase of asexual multiplication, which is similar to the development in intermediate hosts, in extraintestinal tissues (see Section 2, Fig. 1). In the course of this development, some parasites migrate to intestinal tissues and initiate a sexual phase of reproduction. About one third of cats that have been infected primarily with oocysts shed other oocysts after a prolonged prepatent period of 18–49 days for up to 10 days [166,167]. Cats may also become infected by ingesting large numbers (≥1000) of tachyzoites (see Section 4.1) which may result in shedding of oocysts after 15–19 days for up to 7 days [109].
Cats usually only shed large numbers of oocysts after a primary infection with T. gondii. It has previously been believed that shedding of oocysts after reinfection or reshedding of oocysts in the absence of reinfection with T. gondii is rare. However, recent studies showed that this immunity does not persist for the life of the cat. A second shedding of oocysts could be induced in cats that were challenged with T. gondii about 6 years after primary infection [168,169]. In addition, in some cases short-term reshedding of oocysts has been observed without reinfection of the cat. It is currently not known which factors induce a reshedding of oocysts under natural conditions. Experimentally, reshedding of oocysts may be induced by superinfection with other coccidia, for example Isospora species, as well as after immuno-suppression, for example due to application of high doses of corticosteroids [11,12,36,119,149,170].
The domestic cat is the only domestic animal that is used as a definitive host by T. gondii, and thus appears to play a key role in the epidemiology of T. gondii infections. After primary infection with T. gondii cats that are kept inside houses may shed large numbers of oocysts into the household, thereby putting their owners at risk of infection. Stray cats or cats that are roaming on farms may contaminate the environment with oocysts which may infect livestock that will later be slaughtered for human consumption (Fig. 2). However, oocysts shed by cats are unsporulated and, thus, are not immediately infectious (see Section 4.3.2, Fig. 1). Therefore, direct contact with cats usually does not result in an infection with T. gondii. Cat-ownership and keeping of cats inside houses or flats does not necessarily provide a risk of contracting a T. gondii infection, if preventive measures are effective and cat faeces are removed daily from the household (see Section 4.3.3).
4.3.2. Importance and survival of oocysts of Toxoplasma gondii in the environment
By contrast, sporulated oocysts contained in the environment are a potential source of infection for humans and other intermediate hosts. The epidemiological importance of oocysts is highlighted by the fact that, despite the worldwide distribution of T. gondii, infections with this parasite are virtually absent on small islands and atolls which have never been inhabited by cats [171,172]. Contamination of the environment with oocysts of T. gondii may be due to infected domestic cats or wild felines. After primary infection with tissue cysts or oocysts of T. gondii, a single cat may shed more than 100 million oocysts into the environment [12,22,167,173]. Under environmental conditions with sufficient aeration, humidity, and warm temperature oocysts sporulate and become infectious within 1–5 days [12,20,36], while sporulation may be delayed under microaerophilic conditions [22]. Depending on the strain of T. gondii, ingestion of as few as 10 sporulated oocysts may cause an infection in intermediate hosts, such as pigs [174], and ingestion of 100 or more sporulated oocysts may result in a patent infection in felines [167], thereby further contributing to the contamination of the environment with oocysts.
Sporulated oocysts of T. gondii are very resistant to environmental conditions. They survive short periods of cold and dehydration, and remain infectious in moist soil or sand for up to 18 months [22,165]. Under laboratory conditions, sporulated oocysts survived storage at 4°C for up to 54 months and freezing at −10°C for 106 days [175]. However, they were killed within 1–2 min by heating to 55–60°C [175]. Sporulated oocysts also are highly impermeable and, therefore, are also very resistant to disinfectants [11,20,22,36,130].
Oocysts are distributed in the environment through wind, rain, and surface water, or harvested feeds. Hay, straw, and grain which had been contaminated with cat faeces have been identified as sources of infection for livestock [11,176]. In addition, oocysts may be spread via earthworms, coprophagous invertebrates, or manure [11,177]. In the gut of cockroaches, which may act as transport hosts of T. gondii, oocysts remain infectious for up to 19 days [178]. Humans may become infected via contact with contaminated soil, for example through gardening (see Section 4.3.3). Oocysts of T. gondii have been isolated from samples of soil in various areas of the world [22,36,165]. It has also been suggested that the fur of dogs that have come in contact with cat faeces may be a vector for transmission of oocysts to humans [155].
4.3.3. Oocyst-transmitted outbreaks of toxoplasmosis in humans, risk factors, and preventive measures that reduce the risk of oocyst-transmitted infection with Toxoplasma gondii
There are several preventive measures that may reduce the risk of horizontal transmission of T. gondii infections to humans via oocysts. In order to advise appropriate measures for prevention of oocyst shedding by pet cats, cat owners belonging to risk groups, i.e. non-immune pregnant women and immunocompromised patients (see Sections 3.3 and 3.4), should have their cat examined with respect to infection with T. gondii. In this context, examination of faeces is not an appropriate procedure as most cats will shed the majority of oocysts during only 1–2 days, while the whole period of patency may last for up to 20 days (see Section 4.3.1). On those days on which only few oocysts are shed and in cases of reshedding, koproscopic methods may provide a negative result although faeces are still infectious for intermediate hosts as shown in bioassays. Therefore, examination of faeces is only meaningful for the cat owner if the result is positive, i.e. if toxoplasma-like oocysts have been detected in the faeces of the cat.
In epidemiological situations it is more advisable to examine the cat serologically for T. gondii-specific antibodies to find out the immune status of the cat [148]. A serologically negative result suggests that the cat has not yet been exposed to T. gondii and is still susceptible to infection in the future. In such cases cats should be fed on dry, canned, or cooked food and should be prevented from hunting to prevent a primary infection with T. gondii. In addition, the environment of the cat should be controlled with respect to potential intermediate hosts, such as mice and rats, as well as transport hosts, such as cockroaches and other invertebrates. A serologically positive result suggests that the cat already has been infected with T. gondii in the past. The majority of cats with detectable levels of IgG antibodies to T. gondii are likely to be immune and, thus, will not shed oocysts in the near future. Cats that have been infected via tissue cysts usually seroconvert (IgG) between 2 and 5 weeks post-infection, which is after the period of patency (see Section 4.3.1) [150,169,173,179–183]. However, in some cats that have been infected by ingestion of oocysts, IgG antibodies are already detectable during the prolonged period of prepatency [167]. Thus, while detection of IgG antibodies in the serum of cats is indicative of immunity in most cases, it does not exclude that in some rare cases shedding of oocysts may still occur. In addition, some previously infected cats may reshed oocysts over short periods of time (see Section 4.3.1), and consequently immuno-suppressive treatment of cats owned by individuals belonging to risk groups should be avoided. It may also be advisable that immunocompromised individuals should not keep a cat in their household.
In all cases, faeces of pet cats should be removed daily from the household. Cat litter boxes and all items that may have come in contact with cat faeces should be cleaned thoroughly with hot water (>70°) and detergents wearing gloves, but preferably not by immunocompromised individuals or pregnant women. In a case-control study on primary maternal infection in Norway, cleaning the cat litter box was identified as a strong risk factor [140]. However, with the appropriate preventive measures the risk of acquiring an infection with T. gondii from a pet cat can be highly controlled by its owner. Accordingly, in the same case-control study in Norway as well as in a European multi-centre case-control study on primary T. gondii infections in humans, neither direct daily contact with cats nor living in a household or neighborhood with cats were associated with T. gondii infection [140,142].
On the other hand, while consumption of undercooked meat was identified as the principle risk factor in several recent case-control studies on T. gondii infections in humans (see Section 4.2.4) [111,139,140,142,144], this finding does not explain the high rate of seropositivity (24–47%) in some populations of vegetarians [144,184]. However, a few risk factors identified in those studies point to the importance of oocysts in the transmission of T. gondii infections to humans. For example, contact with soil was identified as a strong risk factor in the European multi-centre case-control study, and 6–17% of primary infections in humans were attributed to this factor [142], while in the case-control study in Norway, eating unwashed raw vegetables or fruits was associated with an increased risk of primary infection during pregnancy [140]. Thus, it is advisable that pregnant women and immunocompromised individuals should wash or cook vegetables and fruits, which may be contaminated with cat faeces, before consumption. These individuals should also wear gloves when working in gardens. In addition, T. gondii oocysts in sand pits used as childrens’ playgrounds may be a source of infection. Geophagia was strongly associated with an outbreak of acute toxoplasmosis in six of 11 preschool-aged children of an extended family who played in the same sandy yard of their grandmother’s house, which was also visited by cats [185]. Where ever possible, measures should be taken to prevent cats from defecating into childrens’ playgrounds.
At least another three well-documented outbreaks of acute toxoplasmosis in humans have been associated with contamination of the environment by oocysts. In 1977, an outbreak of acute toxoplasmosis in 37 of 86 patrons of a riding stable in Atlanta, USA, was linked to inhalation of aerolized oocysts which were shed by cats in the stable [81,186–188]. Another outbreak of toxoplasmosis in 35 of 98 military trainees was linked to ingestion of oocyst-contaminated water during training in a jungle environment in Panama [189,190]. However, the largest and best documented outbreak of acute toxoplasmosis in humans to date occurred in 110 individuals in Vancouver, Canada, in 1995. Comprehensive, retrospective epidemiological studies provided strong evidence that this outbreak was caused by contamination of municipal drinking water with oocysts [69,191–194]. It has been suggested that both domestic cats and wild felines (cougars) may have been the source of this outbreak by shedding T. gondii oocysts into the environment of a reservoir that was the source of the municipal water system, which used unfiltered chloraminated surface water [69,193,195].
5. Strategies for surveillance and control of toxoplasmosis in humans
Preventive measures such as the ones described above (see Sections 4.2.4 and 4.3.3) can significantly reduce the risk of acquiring an infection with T. gondii, but cannot always prevent the infection. Therefore, because of the great impact that T. gondii has on the quality of human life several authorities, including the World Health Organisation, have advised strategies for surveillance and control of toxoplasmosis in humans. Such strategies are particularly important for risk groups and are directed at prevention of symptomatic congenital toxoplasmosis and long-term sequelae in children with prenatal T. gondii infection, and at prevention of fatal disease in immunocompromised patients.
In some European countries and some states of the USA, screening programmes have been launched that are aimed at either early detection of primary maternal infection with T. gondii during pregnancies or at detection of prenatal infection in neonates at birth. However, these programmes are not standardised and vary greatly among different countries. Such variation is largely due to controversy that exists on whether treatment of the mother during pregnancy is effective in reducing the risk of vertical transmission to the foetus, in reducing the risk of symptomatic congenital toxoplasmosis in the neonate, or in preventing long-term sequelae in the child. Consequently, there is debate on the cost-effectiveness of such programmes.
In Austria and France, prenatal screening programmes are mandatory and were already established in 1975 and 1978, respectively, [68,196,197]. More recently, prenatal screening has been initiated in parts of Italy (Campania region) [198], whereas Denmark, Poland (Poznan region), and parts of the USA (Massachusetts and New Hampshire) have established neonatal screening programmes [199–202]. While the establishment of these programmes has not clarified the debate about their costs and benefits in public health, they have significantly improved our knowledge on congenital toxoplasmosis as well as on many aspects of the management of, and outcome for, children with prenatal T. gondii infection. In addition, they have provided invaluable data on the epidemiology of infections with this parasite in humans.
5.1. Congenital toxoplasmosis
In 1923, Janků first described tissue cysts of T. gondii in the retina of an 11-month-old infant with congenital hydrocephalus and microphthalmia [203,204]. This was later recognised as the first recorded case of congenital toxoplasmosis in humans [205]. In the late 1930s, studies by Wolf and Cowen [206–208] led to the recognition of T. gondii as a causative agent of encephalomyelitis in human neonates. In the early 1940s, it was recognised that this disease had a congenital origin and, thus, resulted from vertical transmission of the parasite from the mother to her child [209]. The major symptoms of congenital toxoplasmosis in neonates and infants were described during the 1940s and early 1950s, but it was not before the 1960s that prenatal infection with T. gondii was also recognised as a cause of major sequelae later in life (Table 2).
Prenatal infection with T. gondii occurs in from about 1 to 120 per 10 000 live births depending on the geographic location and the population studied (Table 5). This rate can be modelled as a function of the seroconversion rate of the population at risk, e.g. women of childbearing age [210,211]. Thus, a seroconversion rate of 3% per year would suggest that 15% of women between the ages of 20 and 30 would seroconvert with an expected prenatal infection rate of about 46 per 10 000 live births.
Transmission of T. gondii to the foetus in an infected mother has an excellent correlation with isolation of the organism from the placenta. This transmission occurs during the initial acquisition of the infection by immunologically naive pregnant women. There is some debate if chronic infection can increase the rate of spontaneous abortion in subsequent pregnancies, but congenital toxoplasmosis is not a risk in subsequent pregnancies. There are only rare reports of transmission occurring in pregnancies of women who were seropositive at the time of conception [90,212]. The majority of these reports involve women who are immunocompromised with either steroid use and SLE or infection with human immunodeficiency virus (HIV) in the presence of a low CD4 count (less than 300) [90]. It is believed that reactivation of latent infection, (e.g. circulating tachyzoites) in an immunocompromised woman results in a seeding of the placenta and subsequent transmission to the foetus despite the seropositive status of the mother. In a study of 112 placentas from immunocompetent women who were seropositive for T. gondii before pregnancy, no organisms could be found in the placenta [33]. In another study of 177 pregnancies that were terminated, women were separated into two categories; 62 women who acquired infection before or soon after conception and 115 women who acquired infection during pregnancy [213]. Of the women who acquired infection during pregnancy 10 out of 115 had organisms in the placenta, while no organisms were found in the placenta of the 62 women who acquired infection before or at conception. These data confirm that vertical transmission of T. gondii may occur if infection is acquired during pregnancy and that immunity acquired before pregnancy, as reflected by maternal IgG seropositivity, is protective for the foetus.
Vertical transmission of T. gondii during pregnancy is a function of when primary maternal infection occurs during the 40-week gestation period. The later maternal infection is acquired during pregnancy, the more frequently parasites are transmitted to the foetus. In the last few weeks of gestation the transmission rate rises to greater than 90%, while in the first 6 weeks after conception the rate is under 2% [213– 215]. An average transmission rate for each trimester in which seroconversion occurs is 14% for the first trimester, 30% for the second trimester, and 59% for the third trimester. In prospective surveys of women who seroconvert during pregnancy the average incidence of prenatal infection in this population is 30% of the maternal seroconversion rate, (e.g. if the rate of maternal seroconversion is three per 1000 pregnancies the incidence of prenatal infection will be one per 1000 pregnancies). While the transmission rate rises during gestation, the risk of symptomatic congenital toxoplasmosis and the severity of the disease are inversely related to the week of gestation in which transmission occurs. Thus, the highest frequency of severe abnormalities at birth is seen in children whose mother acquired a primary infection with T. gondii between the 10th and 24th week of gestation [215]. Several studies have demonstrated that treatment of pregnant women who show evidence of recently acquired infection with T. gondii can decrease the severity of congenital toxoplasmosis in their children. In a study of 542 pregnancies in which spiramycin was given to women who seroconverted during pregnancy (388 women given treatment and 154 without treatment) the percentage of children without prenatal infection increased from 39 to 77%, and the percentage of children with severe congenital disease or intrauterine death decreased from 11 to 3% [214]. If transmission to the foetus can be documented in utero (by polymerase chain reaction (PCR) or other techniques [33]) the administration of pyrimethamine and sulfadiazine to the mother can treat the infection in utero and further decrease the severity of symptoms in infected children [216,217].
It should be appreciated that children who have been prenatally infected but are asymptomatic at birth will develop manifestations of this infection such as retinochoroiditis later in life [218]. Treatment of prenatally infected children in a recent clinical trial suggests that early treatment of children diagnosed with prenatal T. gondii infection can decrease these late manifestations and improve outcome for these children [219].
Prevention of congenital toxoplasmosis can thus be accomplished by preventing infection in seronegative pregnant women or by treatment of those women who acquire a primary infection with T. gondii, as reflected in maternal seroconversion, during pregnancy. In some cases, education programmes aimed at reducing the risk of primary maternal infection during pregnancy also have been successful in decreasing maternal seroconversion rates [220]. For example, a study at Saint Antoine Hospital demonstrated a decrease of the maternal seroconversion rate from 3.7 to 1.1% [221]. In these programs, women were informed about the epidemiology of T. gondii infections as well as preventive measures, such as the need to cook meat thoroughly, to wash hands after handling raw meat, to wash kitchen utensils that have come in contact with raw meat, to wash fruits and vegetables before consumption, to avoid contact with items contaminated with cat faeces, to use gloves if cleaning a cat litter box cannot be avoided, to remove any cat faeces from such litter boxes on a daily basis, and to clean all litter boxes with hot water between litter changes (see Sections 4.2.4 and 4.3.3).
Serological screening of pregnant women is an effective strategy to prevent prenatal infections with T. gondii in their children. The rate of maternal seroconversion in a given population will determine the cost-effectiveness of such a screening strategy. For example, a seroconversion rate of 7.5% per year would indicate only 20% of women would be at risk of seroconversion during the childbearing years, while a seroconversion rate of 1% per year would indicate 80% of the women would be at risk of seroconversion during the childbearing years; yet in both cases the overall rate of prenatal infections for those populations would be 27 per 10 000 live births. Thus, to identify these 27 cases, only 20% of the women would need repeated screening if the seroconversion rate was 7.5% per year vs. 80% of the women in the other scenario. Nonetheless cost-benefit analysis suggests that even in areas with low incidence of T. gondii infections screening for primary maternal infections during pregnancy is economically worthwhile [222]. An effective screening strategy would involve serological examination of pregnant women for presence or absence of antibodies (IgG and IgM) to T. gondii at the time of presentation and in each subsequent trimester. Seroconversion should be followed up with confirmatory tests as well as determination by amniocentesis and PCR if transmission to the foetus has occurred. This has been extensively reviewed by Remington and co-authors [33]. Women who seroconvert during pregnancy should be treated with spiramycin, and if transmission to the foetus is documented, they should be treated with pyrimethamine and sulfadiazine. Once born, all children of mothers who seroconverted during pregnancy should be evaluated for congenital toxoplasmosis and treated if infection is still evident [214,217– 219,223–231].
An alternative strategy for the identification of prenatal infections with T. gondii is serological screening of neonates [58,199,201,232–234]. The most common technique in neonatal screening has been to use dried blood collected on filter paper in serological tests for IgM antibodies to T. gondii [199,201,232–234,], although neonatal screening utilising cord blood has also been effective [58]. Dried blood on filter paper is utilised for phenylketonuria (PKU) screening programmes in many countries and techniques have been published for the elution of antibodies from such samples [235]. As programmes that utilise such PKU samples for T. gondii serology can piggyback onto pre-existing collection systems for screening for genetic disorders, such neonatal screening programmes are cost-effective even in areas with a low incidence of prenatal infections with T. gondii [201,232]. The majority of neonatal screening programmes use IgM capture enzyme-linked immunosorbent assay (ELISA) techniques for screening, which have a sensitivity of only 70–90% (with some reports on sensitivities as low as 40% [236]). Thus, neonatal screening for only IgM antibodies to T. gondii will only identify a subset of the children with prenatal infection. To some extent this may explain the lower observed than expected prevalence of prenatal infections with T. gondii, compared to historical data, seen in such screening programmes [201,233]. Nonetheless, the experience with most of these programmes is that neonatal screening identifies prenatally infected children that would otherwise have gone undiagnosed and untreated. False-positive IgM serology occurs in about 0.19 per 1000 pregnancies. Therefore, the evaluation of a positive IgM result in a neonate should include serological tests for IgG and IgM antibodies to T. gondii in both the mother and the neonate. In some cases serial serological testing, serological tests for IgA antibodies to T. gondii, or immunoblots may be needed to clarify if congenital transmission has occurred [33,237]. Treatment of children identified with prenatal T. gondii infections has been demonstrated to decrease adverse sequelae [214,217– 219,223–231]. Therefore, neonatal screening programmes for T. gondii infection should result in a net health care cost savings.
5.2. Immunocompromised patients
The other human population in which T. gondii causes severe disease is in immunocompromised patients where reactivation of latent infection causes symptomatic disease [238]. In heart transplantation, seronegative recipients are at high risk of toxoplasmosis, and primary prophylaxis with pyrimethamine and sulfadiazine for 6 weeks (at full treatment dosages) has been demonstrated to prevent this infection [239,240].
T. gondii has been an important opportunistic pathogen in AIDS patients, where the development of toxoplasmic encephalitis was reported to occur in up to 40% of seropositive patients during the course of their HIV infection (see Section 3.4). This infection has declined in the era of HAART due to the improved immune status of HIV infected patients, and CNS toxoplasmosis is now rarely seen in patients with CD4 counts over 200 [238]. Once CNS toxoplasmosis has been diagnosed in an AIDS patient, treatment should be continued indefinitely as stopping treatment is associated with a high relapse rate. Primary prevention of reactivated toxoplasmosis in HIV patients who are serologically positive for T. gondii has been successful with trimethoprim-sulfamethoxazole, dapsone-pyrimethamine, or fansidar (administered to prevent Pneumocystis carinii pneumonia) [241–243]. In HIV infected patients who are serologically negative for T. gondii, preventive measures as described in Section 4.2.4 and 4.3.3 are prudent as a primary infection with T. gondii in the setting of AIDS can result in pneumonia or other severe symptoms (see Section 3.4).
6. Conclusions
Because of the great importance of T. gondii as a causative agent of a zoonosis, public health organisations, such as the World Health Organisation, have repeatedly advised the collection of accurate epidemiological data on this parasite. Such data are essential to elucidate the relative importance of the various sources of infection for humans, to control disease, and to prevent reduction in quality of human life caused by this parasite. However, only few countries of the world regularly monitor toxoplasmosis in humans, and even less countries monitor T. gondii infection in animals.
Although it is now 3 decades ago that the heteroxenous life cycle of T. gondii was elucidated, we still know very little about the relative epidemiological importance of the various routes of horizontal transmission to humans. Because tachyzoites only survive for a short period of time outside the host, it has been generally accepted that postnatal infections in humans are acquired by ingesting one of the two persistent stages of T. gondii, i.e. tissue cysts contained in meat or viscera of many animals and oocysts shed into the environment by domestic cats of wild felines. However, their relative importance in the epidemiology of T. gondii infections remains obscure. On one hand, consumption of undercooked meat has been identified as the principle risk factor in several recent case-control studies on primary infection of T. gondii or seropositivity in humans, on the other hand up to 47% of strict vegetarians have been shown to possess antibodies to T. gondii [184].
It is likely that the major sources of T. gondii infections are different in human populations with differences in culture and eating habits. However, it is also important to take into account that epidemiology is in a state of flux, in particular in the case of a versatile parasite, such as T. gondii. There are many factors that have an impact on the epidemiology of T. gondii infections, such as the type of management and production of livestock, hygienic standards of abattoirs, food processing and technology, the density of cats or wild felines in the environment, environmental conditions that have an influence on the sporulation of oocysts in the environment, (i.e. temperature, humidity, wind), geographical location (with respect to latitude) as well as the different habits of human consumers, to name just a few.
Because of the versatility of T. gondii and its complex epidemiology, it is not possible to advise strategies for control or prevention of disease that are effective worldwide or are effective for all ethnic groups in one location. In recent case-control studies on pregnant women in six European countries, travel outside Europe was identified as a risk factor for acquiring a primary infection with T. gondii [140,142]. This finding points to the fact that people change their habits when entering different environments, and thus become at risk from sources of infection, if only temporarily, that are not important epidemiologically in their home situation. In addition, changes in the habits of consumers may have an impact on potential sources of infection with T. gondii. For example, very recently meat from kangaroos and other marsupials, which are highly susceptible to T. gondii, has become available to consumers outside Australia, for example in Europe. Because this meat is very lean it is usually served undercooked in restaurants, and thus has the potential of a new source of infection for European consumers. Examples such as these highlight the fact that the epidemiology of T. gondii infections in human populations may change when individuals change their eating habits or develop preferences for new food types.
Several recent studies have raised the hypothesis that water-borne transmission of oocysts to humans may have a greater epidemiological importance than has been believed previously. While the risk of acquiring an infection with T. gondii via oocysts that are shed by pet cats into the household of their owners may be significantly reduced by preventive measures, it is currently unknown whether measures for quality control of drinking water are sufficient for preventing its contamination with infectious oocysts of T. gondii from the environment. As a consequence, the Vancouver outbreak of toxoplasmosis in humans (see Section 4.3.3) has now initiated research on the oocyst stage of the parasite, and methods are being developed to facilitate their detection in drinking water [244]. It is desirable that future epidemiological studies on T. gondii should consider the role of oocysts as potential sources of infection for humans and there is a need for methods to monitor these in the environment.
Acknowledgments
ARH was supported by a scholarship of the Karl-Enigk-Stiftung, and LMW by National Institutes of Health grant AI37488.
References
- 1.Ashburn D. History and general epidemiology. In: Ho-Yen DO, Joss AWL, editors. Human toxoplasmosis. Oxford: Oxford University Press; 1992. pp. 1–25. [Google Scholar]
- 2.Nicolle C, Manceaux L. Sur une infection à corps de Leishman (ou organismes voisins) du gondi. C R Hebd Séances Acad Sci. 1908;147:763–6. [Google Scholar]
- 3.Nicolle C, Manceaux L. Sur un protozoaire nouveau du gondi. C R Hebd Séances Acad Sci. 1909;148:369–72. [Google Scholar]
- 4.Levine ND. Taxonomy of Toxoplasma. J Protozool. 1977;24:36–41. doi: 10.1111/j.1550-7408.1977.tb05278.x. [DOI] [PubMed] [Google Scholar]
- 5.Tenter AM, Johnson AM. Phylogeny of the tissue cyst-forming coccidia. Adv Parasitol. 1997;39:69–139. doi: 10.1016/s0065-308x(08)60045-7. [DOI] [PubMed] [Google Scholar]
- 6.Sabin AB. Biological and immunological identity of Toxoplasma of animal and human origin. Proc Soc Exp Biol. 1939;41:75–80. [Google Scholar]
- 7.Levine ND. Sarcocystis, Toxoplasma and related protozoa. Vol. 12. Minneapolis: Burgess Publishing Company; 1961. Protozoan Parasites of domestic animals and of man; pp. 317–46. [Google Scholar]
- 8.Scholtyseck E, Mehlhorn H. Elektronenmikroskopische Befunde ändern das System der Einzeller. Naturwiss Rundsch. 1973;26:420–7. [Google Scholar]
- 9.Hutchison WM. Experimental transmission of Toxoplasma gondii. Nature. 1965;206:961–2. doi: 10.1038/206961a0. [DOI] [PubMed] [Google Scholar]
- 10.Levine ND, Baker JR. The Isospora - Toxoplasma - Sarcocystis confusion. Parasitol Today. 1987;3:101–5. [Google Scholar]
- 11.Dubey JP, Beattie CP. Toxoplasmosis of animals and man. Boca Raton, FL: CRC Press; 1988. [Google Scholar]
- 12.Jackson MH, Hutchison WM. The prevalence and source of Toxoplasma infection in the environment. Adv Parasitol. 1989;28:55–105. doi: 10.1016/s0065-308x(08)60331-0. [DOI] [PubMed] [Google Scholar]
- 13.Dubey JP. Toxoplasma, Neospora, Sarcocystis, and other tissue cyst-forming coccidia of humans and animals. In: Kreier JP, editor. Parasitic protozoa. 2. Vol. 6. 1993. pp. 1–158. [Google Scholar]
- 14.Dubey JP. Toxoplasmosis, sarcocystosis, isosporosis, and cyclosporosis. In: Palmer SR, Soulsby EJL, Simpson DJH, editors. Zoonoses. Oxford: Oxford University Press; 1998. pp. 579–97. [Google Scholar]
- 15.Levine ND. The protozoan phylum apicomplexa. II. Boca Raton, FL: CRC Press; 1988. [Google Scholar]
- 16.Frenkel JK. Besnoitia wallacei of cats and rodents: with a reclassification of other cyst-forming isosporoid coccidia. J Parasitol. 1977;63:611–28. [PubMed] [Google Scholar]
- 17.Smith DD. The Sarcocystidae: Sarcocystis, Frenkelia, Toxoplasma, Besnoitia, Hammondia, and Cystoisospora. J Protozool. 1981;28:262–6. [Google Scholar]
- 18.Euzéby J. Apicomplexa, 1: Coccidioses (Sensu Lato). Collection Fondation Marcel Merieux: 1987. 1987. Protozoologie médicale comparée, vol 2: Myxozoa -Microspora - Ascetospora. [Google Scholar]
- 19.Current WL, Upton SJ, Long PL. Taxonomy and life cycles. In: Long PL, editor. Coccidiosis of man and domestic animals. Boca Raton, FL: CRC Press; 1990. pp. 1–16. [Google Scholar]
- 20.Evans R. Life cycle and animal infection. In: Ho-Yen DO, Joss AWL, editors. Human toxoplasmosis. Oxford: Oxford University Press; 1992. pp. 26–55. [Google Scholar]
- 21.Literák I, Rychlík I, Svobodová V, Pospíšil Z. Restriction fragment length polymorphism and virulence of Czech Toxoplasma gondii strains. Int J Parasitol. 1998;28:1367–74. doi: 10.1016/s0020-7519(98)00090-3. [DOI] [PubMed] [Google Scholar]
- 22.Frenkel JK. Biology of Toxoplasma gondii. In: Ambroise-Thomas P, Peterse E, editors. Congenital toxoplasmosis: scientific background, clinical management and control. Paris: Springer-Verlag; 2000. pp. 9–25. [Google Scholar]
- 23.Johnson AM. Speculation on possible life cycles for the clonal lineages in the genus Toxoplasma. Parasitol Today. 1997;13:393–7. doi: 10.1016/s0169-4758(97)01129-0. [DOI] [PubMed] [Google Scholar]
- 24.Johnson AM. Is there more than one species in the genus Toxoplasma? Tokai J Exp Clin Med. 1999;23:383–9. [PubMed] [Google Scholar]
- 25.Boothroyd JC. Population biology of Toxoplasma: clonality, virulence, and speciation (or not) Infect Agents Dis. 1993;2:100–2. [PubMed] [Google Scholar]
- 26.Boothroyd JC, Sibley LD. Population biology of Toxoplasma gondii. Res Immunol. 1993;144:14–6. doi: 10.1016/s0923-2494(05)80090-2. [DOI] [PubMed] [Google Scholar]
- 27.Tibayrenc M. Entamoeba, Giardia and Toxoplasma: clones or cryptic species? Parasitol Today. 1993;9:102–5. doi: 10.1016/0169-4758(93)90217-4. [DOI] [PubMed] [Google Scholar]
- 28.Howe DK, Sibley LD. Toxoplasma gondii comprises three clonal lineages: correlation of parasite genotype with human disease. J Infect Dis. 1995;172:1561–6. doi: 10.1093/infdis/172.6.1561. [DOI] [PubMed] [Google Scholar]
- 29.Frenkel JK, Ambroise-Thomas P. Genomic drift of Toxoplasma gondii. Parasitol Res. 1997;83:1–5. doi: 10.1007/s004360050197. [DOI] [PubMed] [Google Scholar]
- 30.Dubey JP, Towle A. Toxoplasmosis in sheep: a review and annotated bibliography. Slough: CAB International; 1986. [Google Scholar]
- 31.Remington JS, Desmonts G. Toxoplasmosis. In: Remington JS, Klein JO, editors. Infectious diseases of the fetus and newborn infant. 3. Philadelphia: WB Saunders; 1990. pp. 89–195. [Google Scholar]
- 32.Ho-Yen DO, Joss AWL. Human toxoplasmosis. Oxford: Oxford University Press; 1992. [Google Scholar]
- 33.Remington JS, McLeod R, Desmonts G. Toxoplasmosis. In: Remington JS, Klein JO, editors. Infectious diseases of the fetus and newborn infant. 4. Philadelphia: WB Saunders; 1995. pp. 140–267. [Google Scholar]
- 34.Ambroise-Thomas P, Petersen E. Congenital toxoplasmosis: scientific background, clinical management and control. Paris: Springer-Verlag; 2000. [Google Scholar]
- 35.Dubey JP, Lindsay DS, Speer CA. Structures of Toxoplasma gondii tachyzoites, bradyzoites, and sporozoites and biology and development of tissue cysts. Clin Microbiol Rev. 1998;11:267–99. doi: 10.1128/cmr.11.2.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dubey JP. Toxoplasmosis in cats. Feline Pract. 1986;16:12–45. [Google Scholar]
- 37.Weiss LM, Udem SA, Tanowitz HB, Wittner M. Western blot analysis of the antibody response of patients with AIDS and toxoplasma encephalitis: antigenic diversity among Toxoplasma strains. J Infect Dis. 1988;157:7–13. doi: 10.1093/infdis/157.1.7. [DOI] [PubMed] [Google Scholar]
- 38.Dubey JP. Advances in the life cycle of Toxoplasma gondii. Int J Parasitol. 1998;28:1019–24. doi: 10.1016/s0020-7519(98)00023-x. [DOI] [PubMed] [Google Scholar]
- 39.Dubey JP. Toxoplasmosis: an overview. Southeast Asian J Trop Med Public Health. 1991;22:88–92. [PubMed] [Google Scholar]
- 40.Sabin AB, Feldman HA. Dyes as microchemical indicators of a new immunity phenomenon affecting a protozoon parasite (Toxoplasma) Science. 1948;108:660–3. doi: 10.1126/science.108.2815.660. [DOI] [PubMed] [Google Scholar]
- 41.Gross U. Toxoplasma gondii. Berlin: Springer-Verlag; 1996. [Google Scholar]
- 42.Chatterton JMW. Pregnancy. In: Ho-Yen DO, Joss AWL, editors. Human toxoplasmosis. Oxford: Oxford University Press; 1992. pp. 144–83. [Google Scholar]
- 43.Zuber P, Jacquier P. Épidémiologie de la toxoplasmose: situation au niveau mondial. Schweiz Med Wochenschr. 1995;125(Suppl 65):19S–22S. [PubMed] [Google Scholar]
- 44.Joss AWL. Diagnosis. In: Ho-Yen DO, Joss AWL, editors. Human toxoplasmosis. Oxford: Oxford University Press; 1992. pp. 79–118. [Google Scholar]
- 45.Fleck DG. Annotation: diagnosis of toxoplasmosis. J Clin Pathol. 1989;42:191–3. doi: 10.1136/jcp.42.2.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Johnson J, Duffy K, New L, Holliman RE, Chessum BS, Fleck DG. Direct agglutination test and other assays for measuring antibodies to Toxoplasma gondii. J Clin Pathol. 1989;42:536–41. doi: 10.1136/jcp.42.5.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Joss AWL, Skinner LJ, Chatterton JMW, Cubie HA, Pryde JFD, Campbell JD. Toxoplasmosis: effectiveness of enzyme immunoassay screening. Med Lab Sci. 1989;46:107–12. [PubMed] [Google Scholar]
- 48.Wilson M, Ware DA, Juranek DD. Serologic aspects of toxoplasmosis. J Am Vet Med Assoc. 1990;196:277–81. [PubMed] [Google Scholar]
- 49.Van Enk RA, James KK, Thompson KD. Evaluation of three commercial enzyme immunoassays for Toxoplasma and cytomegalovirus antibodies. Am J Clin Pathol. 1991;95:428–34. doi: 10.1093/ajcp/95.3.428. [DOI] [PubMed] [Google Scholar]
- 50.Valtaud E, Lacroix C, Rodier MH, Toullat G, Jacquemin JL. Étude critique d’une technique ELISA et d’un test d’agglutination directe haute sensibilité pour le dépistage des IgG antitoxoplasmiques. Ann Biol Clin. 1991;49:397–400. [PubMed] [Google Scholar]
- 51.Derouin F, Garin YJF, Buffard C, et al. Étude multicentrique de la sérologie toxoplasmique par différents réactifs ELISA commercialisés. Bull World Health Organ. 1994;72:249–56. [PMC free article] [PubMed] [Google Scholar]
- 52.Decoster A, Lecolier B. Bicentric evaluation of Access Toxo immunoglobulin M (IgM) and IgG assays and IMx Toxo IgM and IgG assays and comparison with Platelia Toxo IgM and IgG assays. J Clin Microbiol. 1996;34:1606–9. doi: 10.1128/jcm.34.7.1606-1609.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Petithory JC, Ambroise-Thomas P, de Loye J, et al. Le sérodiagnostic de la toxoplasmose: étude comparative multicentrique d’une gamme étalon, par les différents tests actuels et avec expression des résultats en unités internationales. Bull World Health Organ. 1996;74:291–8. [PMC free article] [PubMed] [Google Scholar]
- 54.Petithory JC, Reiter-Owona I, Berthelot F, Milgram M, de Loye J, Petersen E. Performance of European laboratories testing serum samples for Toxoplasma gondii. Eur J Clin Microbiol Infect Dis. 1996;15:45–9. doi: 10.1007/BF01586184. [DOI] [PubMed] [Google Scholar]
- 55.Horion M, Thoumsin H, Senterre J, Lambotte R. 20 years of screening for toxoplasmosis in pregnant women: the Liege experience in 20,000 pregnancies. Rev Med Liege. 1990;45:492–7. [PubMed] [Google Scholar]
- 56.Bornand JE, Piguet JD. Infestation toxoplasmique: prévalence, risque d’infection congénitale et évolution à Genève de 1973 à 1987. Schweiz Med Wochenschr. 1991;121:21–9. [PubMed] [Google Scholar]
- 57.Forsgren M, Gille E, Ljungström I, Nokes DJ. Toxoplasma gondii antibodies in pregnant women in Stockholm in 1969. 1979, and 1987. Lancet. 1991;337:1413–4. doi: 10.1016/0140-6736(91)93095-q. [DOI] [PubMed] [Google Scholar]
- 58.Berger R, Stürchler D, Rudin C. Cord blood screening for congenital toxoplasmosis: detection and treatment of asymptomatic newborns in Basel, Switzerland. Scand J Infect Dis (Suppl) 1992;84:46–50. [PubMed] [Google Scholar]
- 59.Henri T, Jacques S, Rene L. Twenty-two years screening for toxoplasmosis in pregnancy: Liege - Belgium. Scand J Infect Dis (Suppl) 1992;84:46–50. [PubMed] [Google Scholar]
- 60.Walker J, Nokes DJ, Jennings R. Longitudinal study of Toxoplasma seroprevalence in South Yorkshire. Epidemiol Infect. 1992;108:99– 106. doi: 10.1017/s0950268800049542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ades AE, Nokes DJ. Modeling age- and time-specific incidence from seroprevalence: toxoplasmosis. Am J Epidemiol. 1993;137:1022–34. doi: 10.1093/oxfordjournals.aje.a116758. [DOI] [PubMed] [Google Scholar]
- 62.Krauße T, Straube W, Wiersbitzky S, Hitz V, Kewitsch A. Toxoplasmosescreening in der Schwangerschaft – ein Pilotprogramm im Nordosten Deutschlands. Geburtshilfe Frauenheilkd. 1993;53:613–8. doi: 10.1055/s-2007-1023597. [DOI] [PubMed] [Google Scholar]
- 63.Murga SN, Nguyen TD, Atchade PS, Bigaignon G. Séro-épidemiologie de la toxoplasmose dans la population belge. Bull Soc Franç Parasitol. 1993;11:181–8. [Google Scholar]
- 64.Nokes DJ, Forsgren M, Gille E, Ljungström I. Modelling Toxoplasma incidence from longitudinal seroprevalence in Stockholm. Sweden Parasitology. 1993;107:33–40. doi: 10.1017/s0031182000079373. [DOI] [PubMed] [Google Scholar]
- 65.Ancelle T, Goulet V, Tirard-Fleury V, et al. La toxoplasmose chez la femme enceinte en France en 1995: résultats d’une enquête nationale périnatale. Bull Épidémiol Hebd. 1996;51:227–9. [Google Scholar]
- 66.Jacquier P. Congenital toxoplasmosis in Switzerland: epidemiological data and medical and public health strategies. Mitt Österr Ges Tropenmed Parasitol. 1996;18:25–32. [Google Scholar]
- 67.Gomez-Marin JE, Montoya-de-Londono MT, Castano-Osorio JC. A maternal screening program for congenital toxoplasmosis in Quindio, Colombia and application of mathematical models to estimate incidences using age-stratified data. Am J Trop Med Hyg. 1997;57:180–6. doi: 10.4269/ajtmh.1997.57.180. [DOI] [PubMed] [Google Scholar]
- 68.Aspöck H. Prevention of congenital toxoplasmosis in Austria: experience of 25 years. In: Ambroise-Thomas P, Petersen E, editors. Congenital toxoplasmosis: scientific background, clinical management and control. Paris: Springer-Verlag; 2000. pp. 277–92. [Google Scholar]
- 69.Bowie WR, King AS, Werker DH, et al. Outbreak of toxoplasmosis associated with municipal drinking water. Lancet. 1997;350:173–7. doi: 10.1016/s0140-6736(96)11105-3. [DOI] [PubMed] [Google Scholar]
- 70.Ho-Yen DO. Clinical features. In: Ho-Yen DO, Joss AWL, editors. Human Toxoplasmosis. Oxford: Oxford University Press; 1992. pp. 56–78. [Google Scholar]
- 71.Wilder HC. Toxoplasma chorioretinitis in adults. AMA Arch Ophthalmol. 1952;48:127–36. doi: 10.1001/archopht.1952.00920010132001. [DOI] [PubMed] [Google Scholar]
- 72.Perkins ES. Ocular toxoplasmosis. Br J Ophthalmol. 1973;57:1–17. doi: 10.1136/bjo.57.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Luft BJ. Toxoplasma gondii. In: Walzer PD, Genta RM, editors. Parasitic infections in the compromised host. New York: Marcel Dekker; 1989. pp. 179–279. [Google Scholar]
- 74.Rothova A. Ocular involvement in toxoplasmosis. Br J Ophthalmol. 1993;77:371–7. doi: 10.1136/bjo.77.6.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nussenblatt RB, Belfort R. Ocular toxoplasmosis: an old disease revisited. J Am Med Assoc. 1994;271:304–7. doi: 10.1001/jama.271.4.304. [DOI] [PubMed] [Google Scholar]
- 76.Couvreur J, Thulliez P. Toxoplasmose acquise à localisation oculaire ou neurologique: 49 cas. Presse Med. 1996;25:438–42. [PubMed] [Google Scholar]
- 77.Montoya JG, Remington JS. Toxoplasmic chorioretinitis in the setting of acute acquired toxoplasmosis. Clin Infect Dis. 1996;23:277–82. doi: 10.1093/clinids/23.2.277. [DOI] [PubMed] [Google Scholar]
- 78.Stanford M, Gilbert R. Epidemiology of ocular Toxoplasma. In: Ambroise-Thomas P, Petersen E, editors. Congenital toxoplasmosis: scientific background, clinical management and control. Paris: Springer-Verlag; 2000. pp. 251–9. [Google Scholar]
- 79.Masur H, Jones TC, Lempert JA, Cherubini TD. Outbreak of toxoplasmosis in a family and documentation of acquired retinochoroiditis. Am J Med. 1978;64:396–402. doi: 10.1016/0002-9343(78)90218-8. [DOI] [PubMed] [Google Scholar]
- 80.Gump DW, Holden RA. Acquired chorioretinitis due to toxoplasmosis. Ann Intern Med. 1979;90:58–60. doi: 10.7326/0003-4819-90-1-58. [DOI] [PubMed] [Google Scholar]
- 81.Akstein RB, Wilson LA, Teutsch SM. Acquired toxoplasmosis. Ophthalmology. 1982;89:1299–302. doi: 10.1016/s0161-6420(82)34629-1. [DOI] [PubMed] [Google Scholar]
- 82.Sacks JJ, Roberto RR, Brooks NF. Toxoplasmosis infection associated with raw goat’s milk. J Am Med Assoc. 1982;248:1728–32. doi: 10.1001/jama.1982.03330140038029. [DOI] [PubMed] [Google Scholar]
- 83.Hausmann N, Richard G. Acquired ocular toxoplasmosis: a fluorescein angiography study. Ophthalmology. 1991;98:1647–51. doi: 10.1016/s0161-6420(91)32073-6. [DOI] [PubMed] [Google Scholar]
- 84.Ronday MJH, Luyendijk L, Baarsma GS, Bollemeijer JG, Van der Lelij A, Rothova A. Presumed acquired ocular toxoplasmosis. Arch Ophthalmol. 1995;113:1524–9. doi: 10.1001/archopht.1995.01100120054009. [DOI] [PubMed] [Google Scholar]
- 85.Bonametti AM, Passos J, do N, da Silva EMK, Bortoliero AL. Surto de toxoplasmose aguda transmitida através da ingestão de carne crua de gado ovino. Rev Soc Bras Med Trop. 1997;30:21–5. doi: 10.1590/s0037-86821997000100005. [DOI] [PubMed] [Google Scholar]
- 86.Choi WY, Nam HW, Kwak NH, et al. Foodborne outbreaks of human toxoplasmosis. J Infect Dis. 1997;175:1280–2. doi: 10.1086/593702. [DOI] [PubMed] [Google Scholar]
- 87.Burnett AJ, Shortt SG, Isaac-Renton J, King A, Werker D, Bowie WR. Multiple cases of acquired toxoplasmosis retinitis presenting in an outbreak. Ophthalmology. 1998;105:1032–7. doi: 10.1016/S0161-6420(98)96004-3. [DOI] [PubMed] [Google Scholar]
- 88.Silveira C, Belfort R, Burnier M, Nussenblatt R. Acquired toxoplasmic infection as the cause of toxoplasmic retinochoroiditis in families. Am J Ophthalmol. 1988;106:362–4. doi: 10.1016/0002-9394(88)90382-0. [DOI] [PubMed] [Google Scholar]
- 89.Glasner PD, Silveira C, Kruszon-Moran D, et al. An unusually high prevalence of ocular toxoplasmosis in southern Brazil. Am J Ophthalmol. 1992;114:136–44. doi: 10.1016/s0002-9394(14)73976-5. [DOI] [PubMed] [Google Scholar]
- 90.Wechsler B, Du LTH, Vignes B, Piette JC, Chomette G, Godeau P. Toxoplasmose et lupus revue de la littérature à propos de 4 observations. Ann Méd Interne. 1986;137:324–30. [PubMed] [Google Scholar]
- 91.Ebbesen P. Placenta physiology. In: Ambroise-Thomas P, Petersen E, editors. Congenital toxoplasmosis: scientific background, clinical management and control. Paris: Springer-Verlag; 2000. pp. 27–35. [Google Scholar]
- 92.Hayde M, Pollak A. Clinical picture: neonatal signs and symptoms. In: Ambroise-Thomas P, Petersen E, editors. Congenital toxoplasmosis: scientific background, clinical management and control. Paris: Springer-Verlag France; 2000. pp. 153–64. [Google Scholar]
- 93.Koskiniemi M, Lappalainen M, Hedman K. Toxoplasmosis needs evaluation: an overview and proposals. Am J Dis Child. 1989;143:724–8. doi: 10.1001/archpedi.1989.02150180106030. [DOI] [PubMed] [Google Scholar]
- 94.Roberts T, Murrell KD, Marks S. Economic losses caused by food-borne parasitic diseases. Parasitol Today. 1994;10:419–23. doi: 10.1016/0169-4758(94)90171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.McLeod R, Boyer K. Management of and outcome for the newborn infant with congenital toxoplasmosis. In: Ambroise-Thomas P, Petersen E, et al., editors. Congenital toxoplasmosis: scientific background, clinical management and control. Paris: Springer-Verlag; 2000. pp. 189–213. [Google Scholar]
- 96.Gilbert R. Epidemiology of infection in pregnant women. In: Ambroise-Thomas P, Petersen E, editors. Congenital toxoplasmosis: scientific background, clinical management and control. Paris: Springer-Verlag; 2000. pp. 237–49. [Google Scholar]
- 97.Jacquemard F. Clinical aspects of infection during pregnancy. In: Ambroise-Thomas P, Petersen E, editors. Congenital toxoplasmosis: scientific background, clinical management and control. Paris: Springer-Verlag; 2000. pp. 111–20. [Google Scholar]
- 98.Lebech M, Petersen E, et al. Reihenuntersuchung von Neugeborenen auf angeborene Toxoplasmose in Dänemark aufgrund mütterlicher Serumkonversion während der Schwangerschaft. Mitt Österr Ges Tropenmed Parasitol. 1996;18:33–40. [Google Scholar]
- 99.Brézin AP. Ophthalmology in the neonate with congenital toxoplasmosis. In: Ambroise-Thomas P, Petersen E, editors. Congenital toxoplasmosis: scientific background, clinical management and control. Paris: Springer-Verlag; 2000. pp. 165–77. [Google Scholar]
- 100.Rothova A. Recurrent ocular disease in congenital toxoplasmosis: clinical manifestations. In: Ambroise-Thomas P, Petersen E, editors. Congenital toxoplasmosis: scientific background, clinical management and control. Paris: Springer-Verlag; 2000. pp. 215–29. [Google Scholar]
- 101.Ho-Yen DO. Immunocompromised patients. In: Ho-Yen DO, Joss AWL, editors. Human toxoplasmosis. Oxford: Oxford University Press; 1992. pp. 184–203. [Google Scholar]
- 102.Luft BJ, Brooks RG, Conley FK, McCabe RE, Remington JS. Toxoplasmic encephalitis in patients with acquired immune deficiency syndrome. J Am Med Assoc. 1984;252:913–7. [PubMed] [Google Scholar]
- 103.Luft BJ, Remington JS. Toxoplasmic encephalitis in AIDS. Clin Infect Dis. 1992;15:211–22. doi: 10.1093/clinids/15.2.211. [DOI] [PubMed] [Google Scholar]
- 104.Ammassari A, Murri R, Cingolani A, de Luca A, Antinori A. AIDS-associated cerebral toxoplasmosis: an update on diagnosis and treatment. In: Gross U, editor. Toxoplasma gondii. Berlin: Springer-Verlag; 1996. pp. 209–22. [DOI] [PubMed] [Google Scholar]
- 105.Ho-Yen DO. Infection in the laboratory. In: Ho-Yen DO, Joss AWL, editors. Human Toxoplasmosis. Oxford: Oxford University Press; 1992. pp. 257–60. [Google Scholar]
- 106.Riemann HP, Meyer ME, Theis JH, Kelso G, Behymer DE. Toxoplasmosis in an infant fed unpasteurized goat milk. J Pediatr. 1975;87:573–6. doi: 10.1016/s0022-3476(75)80825-0. [DOI] [PubMed] [Google Scholar]
- 107.De Andrade Chiari C, Pereira Neves D. Toxoplasmose humana adquirida através da ingestão de leite de cabra. Mem Inst Oswaldo Cruz (Rio de Janeiro) 1984;79:337–40. doi: 10.1590/s0074-02761984000300007. [DOI] [PubMed] [Google Scholar]
- 108.Skinner LJ, Timperley AC, Wightman D, Chatterton JMW, Ho-Yen DO. Simultaneous diagnosis of toxoplasmosis in goats and goatowner’s family. Scand J Infect Dis. 1990;22:359–61. doi: 10.3109/00365549009027060. [DOI] [PubMed] [Google Scholar]
- 109.Dubey JP. Re-examination of resistance of Toxoplasma gondii tachyzoites and bradyzoites to pepsin and trypsin digestion. Parasitology. 1998;116:43–50. doi: 10.1017/s0031182097001935. [DOI] [PubMed] [Google Scholar]
- 110.Bonametti AM, Passos JN, da Silva EMK, Macedo ZS. Probable transmission of acute toxoplasmosis through breast feeding. J Trop Pediatr. 1997;43:116. doi: 10.1093/tropej/43.2.116. [DOI] [PubMed] [Google Scholar]
- 111.Paul M. Potential risk factors for Toxoplasma gondii infection in cases with recently acquired toxoplasmosis. Przegl Epidemiol. 1998;52:447–54. [PubMed] [Google Scholar]
- 112.Elamin EA, Elias S, Daugschies A, Rommel M. Prevalence of Toxoplasma gondii antibodies in pastoral camels(Camelus dromedarius) in the Butana plains, mid-Eastern Sudan. Vet Parasitol. 1992;43:171–5. doi: 10.1016/0304-4017(92)90158-6. [DOI] [PubMed] [Google Scholar]
- 113.Jacobs L, Melton ML. Toxoplasmosis in chickens. J Parasitol. 1966;52:1158–62. [PubMed] [Google Scholar]
- 114.Edelhofer R, Aspöck H. Infektionsquellen und Infektionswege aus der Sicht des Toxoplasmose-Screenings der Schwangeren in Öster-reich. Mitt Österr Ges Tropenmed Parasitol. 1996;18:59–70. [Google Scholar]
- 115.Janitschke K. Pränatale Übertragung der Toxoplasmen von der Mutter auf das Kind. Bundesgesundheitsbl - Gesundheitsforsch -Gesundheitsschutz. 1999;42:548–52. doi: 10.1007/s001030050153. [DOI] [PubMed] [Google Scholar]
- 116.Dubey JP. The scientific basis for prevention of Toxoplasma gondii infection: studies on tissue cyst survival, risk factors and hygiene measures. In: Ambroise-Thomas P, Petersen E, editors. Congenital toxoplasmosis: scientific background, clinical management and control. Paris: Springer-Verlag; 2000. pp. 271–5. [Google Scholar]
- 117.Shirley MW. COST 820 - Vaccines against animal coccidioses. 5.4. Working group 4, sarcocystiosis, toxoplasmosis, neosporosis. Luxembourg: Office for Official Publications of the European Communities; 1997. pp. 28–52. [Google Scholar]
- 118.Tenter AM, Seineke P, Simon K, et al. Aktuelle Studien zur Epidemiologie von Toxoplasma-infektionen. In: Conraths FJ, Greiner M, Kreienbrock L, Schnieder T, et al., editors. Neuere Methoden und Ergebnisse zur Epidemiologie von Parasitosen. DVG, Deutsche Veterinärmedizinische Gesellschaft e.V. Gießen: Offset Köhler KG. 1999. pp. 247–72. [Google Scholar]
- 119.Dubey JP. Toxoplasmosis. J Am Vet Med Assoc. 1994;205:1593–8. [PubMed] [Google Scholar]
- 120.Dubey JP, Murrell KD, Fayer R. Persistence of encysted Toxoplasma gondii in tissues of pigs fed oocysts. Am J Vet Res. 1984;45:1941–3. [PubMed] [Google Scholar]
- 121.Dubey JP, Murrell KD, Fayer R. Distribution of Toxoplasma gondii tissue cysts in commercial cuts of pork. J Am Vet Med Assoc. 1986;188:1035–7. [PubMed] [Google Scholar]
- 122.Van Knapen F, Kremers AFT, Franchimont JH, Narucka U. Prevalence of antibodies to Toxoplasma gondii in cattle and swine in the Netherlands: towards an integrated control of livestock production. Vet Q. 1995;17:87–91. doi: 10.1080/01652176.1995.9694539. [DOI] [PubMed] [Google Scholar]
- 123.Dubey JP, Kirkbride CA. Economic and public health considerations of congenital toxoplasmosis in lambs. J Am Vet Med Assoc. 1989;195:1715–6. [PubMed] [Google Scholar]
- 124.Lundén A, Uggla A. Infectivity of Toxoplasma gondii in mutton following curing, smoking, freezing or microwave cooking. Int J Food Microbiol. 1992;15:357–63. doi: 10.1016/0168-1605(92)90069-f. [DOI] [PubMed] [Google Scholar]
- 125.McDonald JC, Gyorkos TW, Alberton B, MacLean JD, Richer G, Juranek D. An outbreak of toxoplasmosis in pregnant women in northern Québec. J Infect Dis. 1990;161:769–74. doi: 10.1093/infdis/161.4.769. [DOI] [PubMed] [Google Scholar]
- 126.Johnson AM. Australian native marsupials as vectors of toxoplasmosis. New Goals for the 21st Century. Abstracts of the XIV th International Congress for Tropical Medicine and Malaria; Nagasaki, Japan. November 17–22, 1996; p. 132. [Google Scholar]
- 127.Jacobs L, Remington JS, Melton ML. The resistance of the encysted form of Toxoplasma gondii. J Parasitol. 1960;46:11–21. [PubMed] [Google Scholar]
- 128.Dubey JP, Kotula AW, Sharar A, Andrews CD, Lindsay DS. Effect of high temperature on infectivity of Toxoplasma gondii tissue cysts in pork. J Parasitol. 1990;76:201–4. [PubMed] [Google Scholar]
- 129.Kotula AW, Dubey JP, Sharar AK, Andrews CD, Shen SK, Lindsay DS. Effect of freezing on infectivity of Toxoplasma gondii tissue cysts in pork. J Food Prot. 1991;54:687–90. doi: 10.4315/0362-028X-54.9.687. [DOI] [PubMed] [Google Scholar]
- 130.Kuticic V, Wikerhauser T. Studies of the effect of various treatments on the viability of Toxoplasma gondii tissue cysts and oocysts. In: Gross U, editor. Toxoplasma gondii. Berlin: Springer-Verlag; 1996. pp. 261–5. [DOI] [PubMed] [Google Scholar]
- 131.Sohn WM, Nam HW. Western blot analysis of stray cat sera against Toxoplasma gondii and the diagnostic availability of monoclonal antibodies in sandwich-ELISA. Korean J Parasitol. 1999;37:249–56. doi: 10.3347/kjp.1999.37.4.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Dubey JP. Survival of Toxoplasma gondii tissue cysts in 0.85–6% NaCl solutions at 4–20°C. J Parasitol. 1997;83:946–9. [PubMed] [Google Scholar]
- 133.Jamra LM, Martins MC, Vieira M, de P. Acao do sal de cozinha sobre o Toxoplasma gondii. Rev Inst Med Trop Sao Paulo. 1991;33:359–63. [PubMed] [Google Scholar]
- 134.Navarro IT, Vidotto O, Giraldi N, Mitsuka R. Resistência do Toxoplasma gondii ao cloreto de sódio e aos condimentos em linguica de suínos. Bol Oficina Sanit Panam. 1992;112:138–43. [PubMed] [Google Scholar]
- 135.Pekeles GS, McDonald JC, Gyrokos TW, et al. An outbreak of congenital toxoplasmosis in Northern Quebec. Arctic Med Res. 1991;(Suppl):360–2. [PubMed] [Google Scholar]
- 136.Robson JMB, Wood RN, Sullivan JJ, Nicolaides NJ, Lewis BR. A probable foodborne outbreak of toxoplasmosis. Commun Dis Intell. 1995;19:517–22. [Google Scholar]
- 137.Walpole IR, Hodgen N, Bower C. Congenital toxoplasmosis: a large survey in Western Australia. Med J Aust. 1991;154:720–4. doi: 10.5694/j.1326-5377.1991.tb121307.x. [DOI] [PubMed] [Google Scholar]
- 138.Ambroise-Thomas P, Petersen E. Congenital toxoplasmosis: past, present and future. In: Ambroise-Thomas P, Petersen E, editors. Congenital toxoplasmosis: scientific background, clinical management and control. Paris: Springer-Verlag; 2000. pp. 1–7. [Google Scholar]
- 139.Buffolano W, Gilbert RE, Holland FJ, Fratta D, Palumbo F, Ades AE. Risk factors for recent Toxoplasma infection in pregnant women in Naples. Epidemiol Infect. 1996;116:347–51. doi: 10.1017/s0950268800052675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kapperud G, Jenum PA, Stray-Pedersen B, Melby KK, Eskild A, Eng J. Risk factors for Toxoplasma gondii infection in pregnancy: results of a prospective case-control study in Norway. Am J Epidemiol. 1996;144:405–12. doi: 10.1093/oxfordjournals.aje.a008942. [DOI] [PubMed] [Google Scholar]
- 141.Baril L, Ancelle T, Goulet V, Thulliez P, Tirard-Fleury V, Carme B. Risk factors for Toxoplasma infection in pregnancy: a case-control study in France. Scand J Infect Dis. 1999;31:305–9. doi: 10.1080/00365549950163626. [DOI] [PubMed] [Google Scholar]
- 142.Cook AJ, Gilbert RE, Buffolano W, et al. Sources of Toxoplasma infection in pregnant women: a European multicentre case-control study. Br Med J. 2000;15:142–7. doi: 10.1136/bmj.321.7254.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bobić B, Jevremović IJ, Šibalić D, Djurković-Djaković O. Risk factors for Toxoplasma infection in a reproductive age female population in the area of Belgrade, Yugoslavia. Eur J Epidemiol. 1998;14:605–10. doi: 10.1023/a:1007461225944. [DOI] [PubMed] [Google Scholar]
- 144.Roghmann MC, Faulkner CT, Lefkowitz A, Patton S, Zimmerman J, Morris JG. Decreased seroprevalence for Toxoplasma gondii in Seventh Day Adventists in Maryland. Am J Trop Med Hyg. 1999;60:790–2. doi: 10.4269/ajtmh.1999.60.790. [DOI] [PubMed] [Google Scholar]
- 145.Skjerve E, Tharaldsen J, Waldeland H, Kapperud G, Nesbakken T. Antibodies to Toxoplasma gondii in Norwegian slaughtered sheep, pigs and cattle. Bull Scand Soc Parasitol. 1996;6:11–7. [Google Scholar]
- 146.Skjerve E, Waldeland H, Nesbakken T, Kapperud G. Risk factors for the presence of antibodies to Toxoplasma gondii in Norwegian slaughter lambs. Prev Vet Med. 1998;35:219–27. doi: 10.1016/s0167-5877(98)00057-9. [DOI] [PubMed] [Google Scholar]
- 147.Bartoszcze M, Krupa K, Roszkowski J. ELISA for assessing Toxoplasma gondii antibodies in pigs. J Vet Med B. 1991;38:263–4. doi: 10.1111/j.1439-0450.1991.tb00869.x. [DOI] [PubMed] [Google Scholar]
- 148.Lappin MR. Feline toxoplasmosis: interpretation of diagnostic test results. Semin Vet Med Surg (Small Anim) 1996;11:154–60. doi: 10.1016/s1096-2867(96)80027-2. [DOI] [PubMed] [Google Scholar]
- 149.Lukešová D, Literák I. Shedding of Toxoplasma gondii oocysts by Felidae in zoos in the Czech Republic. Vet Parasitol. 1998;74:1–7. doi: 10.1016/s0304-4017(97)00155-6. [DOI] [PubMed] [Google Scholar]
- 150.Lappin MR, Jacobsen ER, Kollias GV, Powell CC, Stover J. Comparison of serologic assays for the diagnosis of toxoplasmosis in nondomestic felids. J Zoo Wildl Med. 1991;22:169–74. [Google Scholar]
- 151.Shen L, Zhichung L, Biaucheng Z, Huayuan Y. Prevalence of Toxoplasma gondii infection in man and animals in Guangdong. Peoples Republic of China. Vet Parasitol. 1990;34:357–60. doi: 10.1016/0304-4017(90)90082-m. [DOI] [PubMed] [Google Scholar]
- 152.Kirkpatrick CE, Colvin BA, Dubey JP. Toxoplasma gondii antibodies in common barn-owls (Tyto alba) and pigeons (Columba livia) in New Jersey. Vet Parasitol. 1990;36:177–80. doi: 10.1016/0304-4017(90)90108-n. [DOI] [PubMed] [Google Scholar]
- 153.Quist CF, Dubey JP, Luttrell MP, Davidson WR. Toxoplasmosis in wild turkeys: a case report and serologic survey. J Wildl Dis. 1995;31:255–8. doi: 10.7589/0090-3558-31.2.255. [DOI] [PubMed] [Google Scholar]
- 154.Hejlíček K, Literák I, Nezval J. Toxoplasmosis in wild mammals from the Czech Republic. J Wildl Dis. 1997;33:480–5. doi: 10.7589/0090-3558-33.3.480. [DOI] [PubMed] [Google Scholar]
- 155.Frenkel JK, Hassanein KM, Hassanein RS, Brown E, Thulliez P, Quintero-Nunez R. Transmission of Toxoplasma gondii in Panama City, Panama: a five-year prospective cohort study of children, cats, rodents, birds, and soil. Am J Trop Med Hyg. 1995;53:458–68. doi: 10.4269/ajtmh.1995.53.458. [DOI] [PubMed] [Google Scholar]
- 156.Berdyev AS, Shevkunova EA. On the distribution of toxoplasmosis among wild vertebrates in Turkmenia (according to serological data) Parazitologiya. 1988;22:378–83. [PubMed] [Google Scholar]
- 157.Dymon M, Ramisz A, Sokołowska B, Zemburowa K, Umiński J, Krupa K. Epizootie Toxoplasma gondii u zwierza¸t dziko żyja¸cych i hodowlanych. Wiad Parazytol. 1988;34:690–704. [PubMed] [Google Scholar]
- 158.Peach W, Fowler J, Hay J. Incidence of Toxoplasma infection in a population of European starlings Sturnus vulgaris from Central England. Ann Trop Med Parasitol. 1989;83:173–7. doi: 10.1080/00034983.1989.11812327. [DOI] [PubMed] [Google Scholar]
- 159.Literák I, Hejlíček K, Nezval J, Folk Č. Incidence of Toxoplasma gondii in populations of wild birds in the Czech Republic. Avian Pathol. 1992;21:659–65. doi: 10.1080/03079459208418887. [DOI] [PubMed] [Google Scholar]
- 160.Lindsay DS, Smith PC, Hoerr FJ, Blagburn BL. Prevalence of encysted Toxoplasma gondii in raptors from Alabama. J Parasitol. 1993;79:870–3. [PubMed] [Google Scholar]
- 161.Hejlíček K, Literák I, Nezval J. Toxoplazmoza lovne zvere. Zverina jako mozny zdroj toxoplazmove infekce. Veterinarstvi. 1994;44:518– 9. [Google Scholar]
- 162.Keshavarz-Valian H, Ebrahimi A. Prevalence of Toxoplasma gondii in birds of Kerman city by serological and parasitological methods. Iranian J Public Health. 1994;23:25–33. 61. [Google Scholar]
- 163.Literák I, Pinowski J, Anger M, Juřicová Z, Kyu-Hwang H, Romanowski J. Toxoplasma gondii antibodies in house sparrows (Passer domesticus) and tree sparrows (P. montanus) Avain Pathol. 1997;26:823–7. doi: 10.1080/03079459708419255. [DOI] [PubMed] [Google Scholar]
- 164.Devada K, Anandan R. Prevalence of Toxoplasma gondii in some common rodents and birds. Indian Vet J. 1998;75:581–2. [Google Scholar]
- 165.Boch J. Die Kokzidiose der Katze. Tierärztl Prax. 1984;12:383–90. [PubMed] [Google Scholar]
- 166.Freyre A, Dubey JP, Smith DD, Frenkel JK. Oocyst-induced Toxoplasma gondii infections in cats. J Parasitol. 1989;75:750–5. [PubMed] [Google Scholar]
- 167.Dubey JP. Infectivity and pathogenicity of Toxoplasma gondii oocysts for cats. J Parasitol. 1996;82:957–61. [PubMed] [Google Scholar]
- 168.Dubey JP. Duration of immunity to shedding of Toxoplasma gondii oocysts by cats. J Parasitol. 1995;81:410–5. [PubMed] [Google Scholar]
- 169.Dubey JP, Lappin MR, Thulliez P. Long-term antibody responses of cats fed Toxoplasma gondii tissue cysts. J Parasitol. 1995;81:887–93. [PubMed] [Google Scholar]
- 170.Rommel M, Schnieder T, Krause HD, Westerhoff J. Trials to suppress the formation of oocysts and cysts of Toxoplasma gondii in cats by medication of the feed with toltrazuril. Vet Med Rev. 1987;2:141–53. [Google Scholar]
- 171.Wallace GD. Serologic and epidemiologic observations on toxoplasmosis on three Pacific attols. Am J Epidemiol. 1969;90:103–11. doi: 10.1093/oxfordjournals.aje.a121054. [DOI] [PubMed] [Google Scholar]
- 172.Munday BL. Serological evidence of Toxoplasma infection in isolated groups of sheep. Res Vet Sci. 1972;13:100–2. [PubMed] [Google Scholar]
- 173.Omata Y, Oikawa H, Kanda M, Mikazuki K, Nakabayashi T, Suzuki N. Experimental feline toxoplasmosis: humoral immune responses of cats inoculated orally with Toxoplasma gondii cysts and oocysts. Jpn J Vet Sci. 1990;52:865–7. doi: 10.1292/jvms1939.52.865. [DOI] [PubMed] [Google Scholar]
- 174.Dubey JP, Lunney JK, Shen SK, Kwok OCH, Ashford DA, Thulliez P. Infectivity of low numbers of Toxoplasma gondii oocysts to pigs. J Parasitol. 1996;82:438–43. [PubMed] [Google Scholar]
- 175.Dubey JP. Toxoplasma gondii oocyst survival under defined temperatures. J Parasitol. 1998;84:862–5. [PubMed] [Google Scholar]
- 176.Buxton D. Ovine toxoplasmosis: a review. J R Soc Med. 1990;83:509–11. doi: 10.1177/014107689008300813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Hiepe T, Buchwalder R. Wirtschaftsdünger als Vektor für Parasiten -Ein Erfahrungsbericht. Dtsch Tierärztl Wochenschr. 1991;98:268–72. [PubMed] [Google Scholar]
- 178.Chinchilla M, Guerrero OM, Castro A, Sabah J. Cockroaches as transport hosts of the protozoan Toxoplasma gondii. Rev Biol Trop. 1994;42:329–31. [PubMed] [Google Scholar]
- 179.Dubey JP, Thulliez P. Serologic diagnosis of toxoplasmosis in cats fed Toxoplasma gondii tissue cysts. J Am Vet Med Assoc. 1989;194:1297–9. [PubMed] [Google Scholar]
- 180.Lappin MR, Greene CE, Prestwood AK, Dawe DL, Tarleton RL. Enzyme-linked immunosorbent assay for the detection of circulating antigens of Toxoplasma gondii in the serum of cats. Am J Vet Res. 1989;50:1586–90. [PubMed] [Google Scholar]
- 181.Lappin MR, Greene CE, Prestwood AK, Dawe DL, Tarleton RL. Diagnosis of recent Toxoplasma gondii infection in cats by use of an enzyme-linked immunosorbent assay for immunoglobulin M. Am J Vet Res. 1989;50:1580–5. [PubMed] [Google Scholar]
- 182.Lappin MR, Bush DJ, Reduker DW. Feline serum antibody responses to Toxoplasma gondii and characterization of target antigens. J Parasitol. 1994;80:73–80. [PubMed] [Google Scholar]
- 183.Burney DP, Lappin MR, Cooper C, Spilker MM. Detection of Toxoplasma gondii-specific IgA in the serum of cats. Am J Vet Res. 1995;56:769–73. [PubMed] [Google Scholar]
- 184.Hall SM, Pandit A, Golwilkar A, Williams TS. How do Jains get Toxoplasma infection? Lancet. 1999;354:486–7. doi: 10.1016/s0140-6736(99)02587-8. [DOI] [PubMed] [Google Scholar]
- 185.Stagno S, Dykes AC, Amos CS, Head RA, Juranek DD, Walls K. An outbreak of toxoplasmosis linked to cats. Pediatrics. 1980;65:706– 12. [PubMed] [Google Scholar]
- 186.Maddison SE, Slemenda SB, Teutsch SM, et al. Lymphocyte proliferative responsiveness in 31 patients after an outbreak of toxoplasmosis. Am J Trop Med Hyg. 1979;28:955–61. doi: 10.4269/ajtmh.1979.28.955. [DOI] [PubMed] [Google Scholar]
- 187.Teutsch SM, Juranek DD, Sulzer A, Dubey JP, Sikes RK. Epidemic toxoplasmosis associated with infected cats. N Engl J Med. 1979;300:695–9. doi: 10.1056/NEJM197903293001302. [DOI] [PubMed] [Google Scholar]
- 188.Dubey JP, Sharma SP, Juranek DD, Sulzer AJ, Teutsch SM. Characterization of Toxoplasma gondii isolates from an outbreak of toxoplasmosis in Atlanta. Georgia Am J Vet Res. 1981;42:1007–10. [PubMed] [Google Scholar]
- 189.Benenson MW, Takafuji ET, Lemon SM, Greenup RL, Sulzer AJ. Oocyst-transmitted toxoplasmosis associated with ingestion of contaminated water. N Engl J Med. 1982;307:666–9. doi: 10.1056/NEJM198209093071107. [DOI] [PubMed] [Google Scholar]
- 190.Sulzer AJ, Franco EL, Takafuji E, Benenson M, Walls KW, Greenup RL. An oocyst-transmitted outbreak of toxoplasmosis: patterns of immunoglobulin G and M over one year. Am J Trop Med Hyg. 1986;35:290–6. doi: 10.4269/ajtmh.1986.35.290. [DOI] [PubMed] [Google Scholar]
- 191.Bell A, Gill R, Isaac-Renton J, et al. Outbreak of toxoplasmosis associated with municipal drinking water – British Columbia. Can Commun Dis Rep. 1995;21:161–4. [PubMed] [Google Scholar]
- 192.Mullens A. ‘I think we have a problem in Victoria’: MDs respond quickly to toxoplasmosis outbreak in BC. Can Med Assoc J. 1996;154:1721–4. [PMC free article] [PubMed] [Google Scholar]
- 193.Aramini JJ, Stephen C, Dubey JP. Toxoplasma gondii in Vancouver Island cougars (Felis concolor vancouverensis): serology and oocyst shedding. J Parasitol. 1998;84:438–40. [PubMed] [Google Scholar]
- 194.Aramini JJ, Stephen C, Dubey JP, Engelstoft C, Schwantje H, Ribble CS. Potential contamination of drinking water with Toxoplasma gondii oocysts. Epidemiol Infect. 1999;122:305–15. doi: 10.1017/s0950268899002113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Stephen C, Haines D, Bollinger T, Atkinson K, Schwantje H. Serological evidence on Toxoplasma infection in cougars on Vancouver Island, British Columbia. Can Vet J. 1996;37:241. [PMC free article] [PubMed] [Google Scholar]
- 196.Aspöck H, Pollak A. Prevention of prenatal toxoplasmosis by serological screening of pregnant women in Austria. Scand J Infect Dis (Suppl) 1992;84:32–7. [PubMed] [Google Scholar]
- 197.Thulliez P. Screening programme for congenital toxoplasmosis in France. Scand J Infect Dis (Suppl) 1992;84:43–5. [PubMed] [Google Scholar]
- 198.Buffolano W, Sagliocca L, Fratta D, Tozzi A, Cardone A, Binkin N. Prenatal toxoplasmosis screening in Campania region, Italy. Ital J Gynaecol Obstet. 1994;3:70–4. [Google Scholar]
- 199.Paul M, Petersen E, Pawlowski ZS, Szczapa J. Neonatal screening for congenital toxoplasmosis in the Poznan region of Poland by analysis of Toxoplasma gondii-specific IgM antibodies eluted from filter paper blood spots. Pediatr Infect Dis J. 2000;19:30–6. doi: 10.1097/00006454-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 200.Lebech M, Petersen E. Neonatal screening for congenital toxoplasmosis in Denmark: presentation of the design of a prospective study. Scand J Infect Dis (Suppl) 1992;84:75–9. [PubMed] [Google Scholar]
- 201.Guerina NG, Hsu HW, Meissner HC, et al. Neonatal serologic screening and early treatment for congenital Toxoplasma gondii infection. N Engl J Med. 1994;330:1858–63. doi: 10.1056/NEJM199406303302604. [DOI] [PubMed] [Google Scholar]
- 202.Petersen E, Eaton RB. Neonatal screening for congenital infection with Toxoplasma gondii. In: Ambroise-Thomas P, Petersen E, editors. Congenital toxoplasmosis: scientific background, clinical management and control. Paris: Springer-Verlag; 2000. pp. 305–11. [Google Scholar]
- 203.Janků J. Pathogenesa a pathologická anatomie tak nazvaného vrozeného kolobomu žluté skvrny v oku normálně velikém a mikrophthal-mickéém s nálezem parazitu v sítnici. Čas Lék Česk. 1923;39–43:1021–7. 1054–9, 1081–5, 1111–5, 1138–44. [Google Scholar]
- 204.Janků J. Die Pathogenese und Pathologische Anatomie des sogen-annten angeborenen Koloboms des gelben Fleckes im normal großen sowie im mikrophthalmischen auge mit Parasitenbefund in der Netzhaut. Česk Parasitol. 1959;6:9–57. [Google Scholar]
- 205.Levaditi C, Schoen R, Sanchis Bayarri V. L’encéphalomyélite toxoplasmique chronique du lapin et de la souris. C R Séances Soc Biol Fil (Paris) 1928;99:37–40. [Google Scholar]
- 206.Wolf A, Cowen D. Granulomatous encephalomyelitis due to an Encephalitozoon (encephalitozoic encephalomyelitis): a new protozoan disease of man. Bull Neurol Inst NY. 1937;6:306–71. [Google Scholar]
- 207.Wolf A, Cowen D. Granulomatous encephalomyelitis due to a protozoan (Toxoplasma or Encephalitozoon). II. Identification of a case from the literature. Bull Neurol Inst NY. 1938;7:266–83. [Google Scholar]
- 208.Wolf A, Cowen D, Paige BH. Toxoplasmic encephalomyelitis. III. A new case of granulomatous encephalitis due to a protozoon. Am J Pathol. 1939;15:657–94. [PMC free article] [PubMed] [Google Scholar]
- 209.Paige BH, Cowen D, Wolf A. Toxoplasmic encephalomyelitis. V. Further observations of infantile toxoplasmosis: intrauterine inception of the disease; visceral manifestation. Am J Dis Child. 1942;63:474–514. [Google Scholar]
- 210.Frenkel JK. Toxoplasma in and around us. Bioscience. 1973;23:343– 52. [Google Scholar]
- 211.Frenkel JK. Breaking the transmission chain of Toxoplasma: a program for the prevention of human toxoplasmosis. Bull NY Acad Med. 1974;50:228–35. [PMC free article] [PubMed] [Google Scholar]
- 212.Desmonts G, Couvreur J, Thulliez P. Toxoplasmose congénitale: cinq cas de transmission a l’enfant d’une infection maternelle antérieure a la grosesse. Presse Med. 1990;19:1445–9. [PubMed] [Google Scholar]
- 213.Desmonts G, Daffos F, Forestier F, Capella-Pavlovsky M, Thulliez P, Chartier M. Prenatal diagnosis of congenital toxoplasmosis. Lancet. 1985;1(8427):500–4. doi: 10.1016/s0140-6736(85)92096-3. [DOI] [PubMed] [Google Scholar]
- 214.Desmonts G, Couvreur J. Congenital toxoplasmosis: a prospective study of the offspring of 542 women who acquired toxoplasmosis during pregnancy: pathophysiology of congenital disease. In: Thalhammer O, Baumgarten K, Pollak A, editors. Perinatal medicine: sixth European Congress; Stuttgart: Georg Thieme Verlag; 1979. pp. 51–60. [Google Scholar]
- 215.Desmonts G. Toxoplasmose acquise de la femme enceinte: estimation du risque de transmission du parasite et de toxoplasmose congénitale. Lyon Méd. 1982;248:115–23. [Google Scholar]
- 216.Daffos F, Forestier F, Capella-Pavlovsky M, et al. Prenatal management of 746 pregnancies at risk for congenital toxoplasmosis. N Engl J Med. 1988;318:271–5. doi: 10.1056/NEJM198802043180502. [DOI] [PubMed] [Google Scholar]
- 217.Couvreur J, Thulliez P, Daffos F, et al. In utero treatment of toxoplasmic fetopathy with the combination pyrimethamine-sulfadiazine. Fetal Diagn Ther. 1993;8:45–50. doi: 10.1159/000263746. [DOI] [PubMed] [Google Scholar]
- 218.Wilson CB. Treatment of congenital toxoplasmosis. Pediatr Infect Dis J. 1990;9:682–3. [PubMed] [Google Scholar]
- 219.McAuley J, Boyer KM, Patel D, et al. Early and longitudinal evaluations of treated infants and children and untreated historical patients with congenital toxoplasmosis: the Chicago Collaborative Treatment Trial [published erratum appears in Clin Infect Dis 1994;19:820] Clin Infect Dis. 1994;18:38–72. doi: 10.1093/clinids/18.1.38. [DOI] [PubMed] [Google Scholar]
- 220.Aspöck H, Flamm H, Picher O. Die Toxoplasmose-Überwachung während der Schwangerschaft – 10 Jahre Erfahrungen in Österreich. Mitt Österr Ges Tropenmed Parasitol. 1986;8:105–13. [Google Scholar]
- 221.Roux G, Desmonts G, Mulliez N, et al. Toxoplasmose et grossesse: bilan de deux ans de prophylaxie de la toxoplasmose congénitale a la maternité de l’hôpital Saint-Antoine (1973–1974) J Gynecol Obstet Biol Reprod (Paris) 1976;5:249–64. [PubMed] [Google Scholar]
- 222.Lappalainen M, Sintonen H, Koskiniemi M, et al. Cost-benefit analysis of screening for toxoplasmosis during pregnancy. Scand J Infect Dis. 1995;27:265–72. doi: 10.3109/00365549509019020. [DOI] [PubMed] [Google Scholar]
- 223.Couvreur J, Nottin N, Desmonts G. La toxoplasmose congénitale traitée: résultats cliniques et biologiques. Ann Pediatr (Paris) 1980;27:647–52. [PubMed] [Google Scholar]
- 224.Couvreur J, Desmonts C. Treatment of toxoplasmosis acquired during pregnancy with Spiramycin. Zentralbl Gynäkol. 1983;105:1104–7. [PubMed] [Google Scholar]
- 225.Couvreur J, Desmonts C. Die Behandlung der konnatalen Toxoplasmose. Zentralbl Gynäkol. 1983;105:1108–12. [PubMed] [Google Scholar]
- 226.Desmonts G, Couvreur J. Congenital toxoplasmosis: prospective study of the outcome of pregnancy in 542 women with toxoplasmosis acquired during pregnancy. Ann Pediatr (Paris) 1984;31:805–9. [PubMed] [Google Scholar]
- 227.Couvreur J, Desmonts G, Thulliez P. Prophylaxis of congenital toxoplasmosis: effects of spiramycin on placental infection. J Anti-microb Chemother. 1988;22:193–200. doi: 10.1093/jac/22.supplement_b.193. [DOI] [PubMed] [Google Scholar]
- 228.Couvreur J, Thulliez P, Daffos F, et al. Fetal toxoplasmosis: in utero treatment with pyrimethamine sulfamides. Arch Fr Pediatr. 1991;48:397–403. [PubMed] [Google Scholar]
- 229.Couvreur J. Congenital toxoplasmosis: epidemiology, physiopathology, evolution, diagnosis, prognosis, principles of the treatment, prevention. Rev Prat. 1992;42:243–6. [PubMed] [Google Scholar]
- 230.Hohlfeld P, Daffos F, Costa JM, Thulliez P, Forestier F, Vidaud M. Prenatal diagnosis of congenital toxoplasmosis with a polymerase-chain-reaction test on amniotic fluid. N Engl J Med. 1994;331:695–9. doi: 10.1056/NEJM199409153311102. [DOI] [PubMed] [Google Scholar]
- 231.Couvreur J. Le traitement in utero de la toxoplasmose congénitale par l’association pyrimethamine-sulfadiazine. Presse Med. 1991;20:1136. [PubMed] [Google Scholar]
- 232.Lebech M, Andersen O, Christensen NC, et al. Feasibility of neonatal screening for Toxoplasma infection in the absence of prenatal treatment. Lancet. 1999;353:1834–7. doi: 10.1016/s0140-6736(98)11281-3. [DOI] [PubMed] [Google Scholar]
- 233.Hsu HW, Grady GF, Maguire JH, Weiblen BJ, Hoff R. Newborn screening for congenital Toxoplasma infection: five years experience in Massachusetts, USA. Scand J Infect Dis (Suppl) 1992;84:59–64. [PubMed] [Google Scholar]
- 234.Petersen E, Eaton RB. Control of congenital infection with Toxoplasma gondii by neonatal screening based on detection of specific immunoglobulin M antibodies eluted from phenylketonuria filter-paper blood-spot samples. Acta Paediatr Suppl. 1999;88:36–9. doi: 10.1111/j.1651-2227.1999.tb01154.x. [DOI] [PubMed] [Google Scholar]
- 235.Lebech M, Petersen E. Detection by enzyme immunosorbent assay of Toxoplasma gondii IgG antibodies in dried blood spots on PKU-filter paper from newborns. Scand J Infect Dis. 1995;27:259–63. doi: 10.3109/00365549509019019. [DOI] [PubMed] [Google Scholar]
- 236.Naessens A, Jenum PA, Pollak A, et al. Diagnosis of congenital toxoplasmosis in the neonatal period: a multicenter evaluation. J Pediatr. 1999;135:714–9. doi: 10.1016/s0022-3476(99)70090-9. [DOI] [PubMed] [Google Scholar]
- 237.Robert-Gangneux F, Commere V, Tourte-Schaefer C, Dupouy-Camet J. Performance of a Western blot assay to compare mother and newborn anti-Toxoplasma antibodies for the early neonatal diagnosis of congenital toxoplasmosis. Eur J Clin Microbiol Infect Dis. 1999;18:648–54. doi: 10.1007/s100960050366. [DOI] [PubMed] [Google Scholar]
- 238.Montoya JG, Remington JS. Toxoplasmosis. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and Practice of Infectious Diseases. Philadelphia: Curchill Livingstone; 2000. pp. 2858–88. [Google Scholar]
- 239.Couvreur J, Tournier G, Sardet-Frismand A, Fauroux B. Transplantation cardiaque ou cardio-pulmonaire et toxoplasmose. Presse Med. 1992;21:1569–74. [PubMed] [Google Scholar]
- 240.Tanowitz HB, Weiss LM, Van Hoeven KH, Kellie S, Wittner M. Parasitic diseases of the heart II: toxoplasmosis and other protozoan and helminthic diseases. J Cardiovasc Pathol. 1992;1:97–106. doi: 10.1016/1054-8807(92)90013-E. [DOI] [PubMed] [Google Scholar]
- 241.Bozzette SA, Finkelstein DM, Spector SA, et al. A randomized trial of three antipneumocystis agents in patients with advanced human immunodeficiency virus infection: NIAID AIDS Clinical Trials Group. N Engl J Med. 1995;332:693–9. doi: 10.1056/NEJM199503163321101. [DOI] [PubMed] [Google Scholar]
- 242.Podzamczer D, Salazar A, Jimenez J, et al. Intermittent trimethoprim-sulfamethoxazole compared with dapsone-pyrimethamine for the simultaneous primary prophylaxis of Pneumocystis pneumonia and toxoplasmosis in patients infected with HIV. Ann Intern Med. 1995;122:755–61. doi: 10.7326/0003-4819-122-10-199505150-00004. [DOI] [PubMed] [Google Scholar]
- 243.Podzamczer D, Miró JM, Bolao F, et al. Twice-weekly maintenance therapy with sulfadiazine-pyrimethamine to prevent recurrent toxoplasmic encephalitis in patients with AIDS: Spanish Toxoplasmosis Study Group. Ann Intern Med. 1995;123:175–80. doi: 10.7326/0003-4819-123-3-199508010-00003. [DOI] [PubMed] [Google Scholar]
- 244.Isaac-Renton J, Bowie WR, King A, et al. Detection of Toxoplasma gondii oocysts in drinking water. Appl Environ Microbiol. 1998;64:2278–80. doi: 10.1128/aem.64.6.2278-2280.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Rommel M. Recent advances in the knowledge of the biology of the cyst-forming coccidia. Angew Parasitol. 1989;30:173–83. [PubMed] [Google Scholar]
- 246.Laveran M. Au sujet de l’hématozoaire endoglobulaire de Padda oryzivora. C R Séances Soc Biol Fil (Paris) 1900;52:19–20. [Google Scholar]
- 247.Marullaz M. Au sujet d’un toxoplasme des oiseaux. Bull Soc Pathol Exot. 1913;6:323–6. [Google Scholar]
- 248.Darling ST. Sarcosporidiosis: with report of a case in man. Proc Canal Zone Med Assoc. 1908;1:141–52. [Google Scholar]
- 249.Levaditi C. Au sujet de certaines protozooses héréditaires humaines à localisation oculaires et nerveuses. C R Séances Soc Biol Fil (Paris) 1928;98:297–9. [Google Scholar]
- 250.Pinkerton H, Weinman D. Toxoplasma infection in man. Arch Pathol. 1940;30:374–92. [Google Scholar]
- 251.Pinkerton H, Henderson RG. Adult toxoplasmosis: a previously unrecognized disease entity simulating the typhus-spotted fever group. J Am Med Assoc. 1941;116:807–14. [Google Scholar]
- 252.Sabin AB. Toxoplasmic encephalitis in children. J Am Med Assoc. 1941;116:801–7. [Google Scholar]
- 253.Sabin AB. Toxoplasmosis, a recently recognized disease in human beings. Adv Pediatr. 1942;1:1–56. [Google Scholar]
- 254.Gard S, Magnusson JH. A glandular form of toxoplasmosis in connection with pregnancy. Acta Med Scand. 1951;141:59–64. doi: 10.1111/j.0954-6820.1951.tb14195.x. [DOI] [PubMed] [Google Scholar]
- 255.Siim JC. Studies on acquired toxoplasmosis. II. Report of a case with pathological changes in lymph node removed at biopsy. Acta Pathol Microbiol Scand. 1952;30:104–8. [PubMed] [Google Scholar]
- 256.Sabin AB, Eichenwald H, Feldman HA, Jacobs L. Present status of clinical manifestations of toxoplasmosis in man: indications and provisions for routine serologic diagnosis. J Am Med Assoc. 1952;150:1063–9. doi: 10.1001/jama.1952.03680110003002. [DOI] [PubMed] [Google Scholar]
- 257.Frenkel JK, Nelson BM, Arias-Stella J. Immunosuppression and toxoplasmic encephalitis: clinical and experimental aspects. Hum Pathol. 1975;6:97–111. doi: 10.1016/s0046-8177(75)80111-0. [DOI] [PubMed] [Google Scholar]
- 258.Weinman D, Chandler AH. Toxoplasmosis in swine and rodents: reciprocal oral infection and potential human hazard. Proc Soc Exp Biol Med. 1954;87:211–6. doi: 10.3181/00379727-87-21337. [DOI] [PubMed] [Google Scholar]
- 259.Weinman D, Chandler AH. Toxoplasmosis in man and swine - an investigation of the possible relationship. J Am Med Assoc. 1956;161:229–32. doi: 10.1001/jama.1956.62970030012010. [DOI] [PubMed] [Google Scholar]
- 260.Rawal BD. Toxoplasmosis: a dye-test survey on sera from vegetarians and meat eaters in Bombay. Trans R Soc Trop Med Hyg. 1959;53:61–3. doi: 10.1016/0035-9203(59)90084-7. [DOI] [PubMed] [Google Scholar]
- 261.Jacobs L, Remington JS, Melton ML. A survey of meat samples from swine, cattle, and sheep for the presence of encysted Toxoplasma. J Parasitol. 1960;46:23–8. [PubMed] [Google Scholar]
- 262.Eichenwald HA. A study of congenital toxoplasmosis. In: Siim JC, editor. Human Toxoplasmosis. Copenhagen: Ejnar Munksgaard Forlag; 1960. pp. 41–9. [Google Scholar]
- 263.Scholtyseck E, Piekarski G. Elektronenmikroskopische Untersuchungen an Merozoiten von Eimerien (Eimeria perforans und E. stiedae) und Toxoplasma gondii: Zur systematischen Stellung von T. gondii. Z Parasitenkd. 1965;26:91–115. doi: 10.1007/BF00348725. [DOI] [PubMed] [Google Scholar]
- 264.Scholtyseck E, Mehlhorn H, Friedhoff K. The fine structure of the conoid of sporozoa and related organisms. Z Parasitenkol. 1970;34:68–94. [Google Scholar]
- 265.Desmonts G, Couvreur J, Alison F, Baudelot J, Gerbeaux J, Lelong M. Étude épidémiologique sur la toxoplasmose: de l’influence de la cuisson des viandes de boucherie sur la fréquence de l’infection humaine. Rev Fr Étud Clin Biol. 1965;10:952–8. [PubMed] [Google Scholar]
- 266.Vietzke WM, Gelderman AH, Grimley PM, Valsamis MP. Toxoplasmosis complicating malignancy: experience at the National Cancer Institute. Cancer. 1968;21:816–27. doi: 10.1002/1097-0142(196805)21:5<816::aid-cncr2820210506>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 267.Hutchison WM, Dunachie JF, Siim JC, Work K. Life cycle of Toxoplasma gondii. Br Med J. 1969;4:806. doi: 10.1136/bmj.4.5686.806-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Kühn D, Weiland G. Experimentelle Toxoplasma-infektionen bei der Katze. I. Wiederholte Übertragung von Toxoplasma gondii durch Kot von mit Nematoden infizierten Katzen. Berl Münch Tierärztl Wochenschr. 1969;82:401–4. [PubMed] [Google Scholar]
- 269.Siim JC, Hutchison WM, Work K. Transmission of Toxoplasma gondii: further studies on the morphology of the cystic form in cat faeces. Acta Pathol Microbiol Scand. 1969;77:756–7. [PubMed] [Google Scholar]
- 270.Dubey JP, Miller NL, Frenkel JK. The Toxoplasma gondii oocyst from cat feces. J Exp Med. 1970;132:636–62. doi: 10.1084/jem.132.4.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Overdulve JP. The identity of Toxoplasma Nicolle and Manceaux, 1909 with Isospora schneider, 1881. I and II. Proc K Ned Akad Wet C. 1970;73:129–51. [PubMed] [Google Scholar]
- 272.Sheffield HG, Melton ML. Toxoplasma gondii: the oocyst, sporozoite, and infection of cultured cells. Science. 1970;167:892–3. doi: 10.1126/science.167.3919.892. [DOI] [PubMed] [Google Scholar]
- 273.Witte HM, Piekarski G. Die Oocysten-Ausscheidung bei experimentell infizierten Katzen in Abhängigkeit vom Toxoplasma-Stamm. Z Parasitenkd. 1970;33:358–60. doi: 10.1007/BF00331472. [DOI] [PubMed] [Google Scholar]
- 274.Frenkel JK, Dubey JP, Miller NL. Toxoplasma gondii in cats: fecal stages identified as coccidian oocysts. Science. 1970;167:893–6. doi: 10.1126/science.167.3919.893. [DOI] [PubMed] [Google Scholar]
- 275.Hutchison WM, Dunachie JF, Siim JC, Work K. Coccidian-like nature of Toxoplasma gondii. Br Med J. 1970;1:142–4. doi: 10.1136/bmj.1.5689.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Weiland G, Kühn D. Experimentelle Toxoplasma-Infektionen bei der katze. II. Entwicklungsstadien des Parasiten im Darm. Berl Münch Tierärztl Wochenschr. 1970;83:128–32. [PubMed] [Google Scholar]
- 277.Hutchison WM, Dunachie JF, Work K, Siim JC. The life cycle of the coccidian parasite, Toxoplasma gondii, in the domestic cat. Trans R Soc Trop Med Hyg. 1971;65:380–99. doi: 10.1016/0035-9203(71)90018-6. [DOI] [PubMed] [Google Scholar]
- 278.Luft BJ, Conley F, Remington JS, et al. Outbreak of central-nervous-system toxoplasmosis in western Europe and North America. Lancet. 1983;1(8328):781–4. doi: 10.1016/s0140-6736(83)91847-0. [DOI] [PubMed] [Google Scholar]
- 279.Eng SB, Werker DH, King AS, et al. Computer-generated dot maps as an epidemiologic tool: investigating an outbreak of toxoplasmosis. Emerg Infect Dis. 1999;5:815–9. doi: 10.3201/eid0506.990613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Fuente MC, Bovone NS, Cabral GE. Profilaxis de la toxoplasmosis prenatal. Medicina (B Aires) 1997;57:155–60. [PubMed] [Google Scholar]
- 281.Moese JR, Vander-Moese A. Mother-child pass in Austria and primary toxoplasmosis infections in pregnant women. Cent Eur J Public Health. 1998;6:261–4. [PubMed] [Google Scholar]
- 282.Aspöck H. Österreichs Beitrag zur Toxoplasmose-Forschung und 20 Jahre Toxoplasmose-Überwachung der Schwangeren in Österreich. Mitt Österr Ges Tropenmed Parasitol. 1996;18:1–18. [Google Scholar]
- 283.Samad MA, Begum N, Shamsunahar Ahmed MU. Serological diagnosis of Toxoplasma gondii infection in women associated with gyneco-obstetric problems. Southeast Asian J Trop Med Public Health. 1993;24:102–6. [PubMed] [Google Scholar]
- 284.Samad MA, Islam MR, Dey BC, Alam MM. Effects of corticosteroids in stray cats with natural antibodies to Toxoplasma gondii. J Protozool Res. 1997;7:1–8. [Google Scholar]
- 285.Ashrafunnessa H, Khatun S, Nazrul Islam M, Huq T. Seroprevalence of Toxoplasma antibodies among the antenatal population in Bangladesh. J Obstet Gynaecol Res. 1998;24:115–9. doi: 10.1111/j.1447-0756.1998.tb00061.x. [DOI] [PubMed] [Google Scholar]
- 286.Foulon W, Naessens A, Derde MP. Evaluation of the possibilities for preventing congenital toxoplasmosis. Am J Perinatol. 1994;11:57–62. doi: 10.1055/s-2007-994537. [DOI] [PubMed] [Google Scholar]
- 287.Luyasu V, Robert A, Lissenko D, et al. A seroepidemiological study on toxoplasmosis. Acta Clin Belg. 1997;52:3–8. doi: 10.1080/17843286.1997.11718544. [DOI] [PubMed] [Google Scholar]
- 288.Rodier MH, Berthonneau J, Bourgoin A, et al. Seroprevalences of Toxoplasma, malaria, rubella, cytomegalovirus, HIV and treponemal infections among pregnant women in Cotonou, Republic of Benin. Acta Trop. 1995;59:271–7. doi: 10.1016/0001-706x(95)00087-u. [DOI] [PubMed] [Google Scholar]
- 289.Rey LC, Ramalho ILC. Seroprevalence of toxoplasmosis in Fortaleza, Ceara, Brazil. Rev Inst Med Trop Sao Paulo. 1999;41:171–4. doi: 10.1590/s0036-46651999000300007. [DOI] [PubMed] [Google Scholar]
- 290.Ndumbe PM, Andela A, Nkemnkeng-Asong J, Watonsi E, Nyambi P. Prevalence of infections affecting the child among pregnant women in Yaounde, Cameroon. Med Microbiol Immunol (Berl) 1992;181:127–30. doi: 10.1007/BF00202052. [DOI] [PubMed] [Google Scholar]
- 291.Sun RG, Liu ZL, Wang DC, et al. The prevalence of Toxoplasma infection among pregnant women and their newborn infants in Chengdu. Chung Hua Liu Hsing Ping Hsueh Tsa Chih. 1995;16:98– 100. [PubMed] [Google Scholar]
- 292.Hou JH, Pu RZ, Liu JY, et al. A study on IHA examination of Toxoplasma infection in pregnant and postpartum women in Lanzhou district. Endemic Dis Bull. 1997;12:78–79. [Google Scholar]
- 293.Makuwa M, Lecko M, Nsimba B, Bakouetela J, Lounana-Kouta J. Toxoplasmose et la femme enceinte au Congo. Bilan de 5 ans de dépistage (1986–1990) Méd Afr Noire. 1992;39:493–5. [Google Scholar]
- 294.Stojanovic D. Effect of toxoplasmosis on occurrence of spontaneous abortions and anomalies in neonates of the Timok region. Vojnosanit Pregl. 1998;55:151–9. [PubMed] [Google Scholar]
- 295.Martinez Sanchez R, Bacallao Gordo R, Alberti Amador E, Alfonso Berrio L. Prevalence of toxoplasmosis in pregnant women of the province of La Habana. Rev Inst Med Trop Sao Paulo. 1994;36:445– 50. [PubMed] [Google Scholar]
- 296.González-Morales T, Bacallo-Gallestey J, García-Santana CA, Molina-Garcia JR. Prevalencia de anticuerpos anti-Toxoplasma gondii en una población de mujeres embarazadas en Cuba. Gac Méd Méx. 1995;131:499–503. [PubMed] [Google Scholar]
- 297.Lopez R, Perez X, Guerra E, Herrera R, Acosta C. Toxoplasmosis entre mujeres embarazadas en ciudad de La Habana. Biomedica. 1993;13:173–8. [Google Scholar]
- 298.Hejlíček K, Literák I, Vostalová E, Křešnicka J. Protilátky proti Toxoplasma gondii u gravidních žen v okrese České Budějovice. Epidemiol Mikrobiol Imunol. 1999;48:102–5. [PubMed] [Google Scholar]
- 299.Flegr J, Havlíček J. Changes in the personality profile of young women with latent toxoplasmosis. Folia Parasitol (Praha) 1999;46:22–8. [PubMed] [Google Scholar]
- 300.Lebech M, Larsen SO, Petersen E. Prevalence, incidence and geographical distribution of Toxoplasma gondii antibodies in pregnant women in Denmark. Scand J Infect Dis. 1993;25:751–6. doi: 10.3109/00365549309008574. [DOI] [PubMed] [Google Scholar]
- 301.Eissa MH, Abdelsalam AM, Antonious SN, Abdelgafar AR, Morsy TA. Comparative study of the Sabin–Feldman dye test and the indirect haemagglutination test in serodiagnosis of toxoplasmosis. J Egypt Soc Parasitol. 1990;20:729–35. [PubMed] [Google Scholar]
- 302.El-Ridi AMS, Nada SMM, Aly AS, Ramadan ME, Hagar EG, Taha TA. Toxoplasmosis and pregnancy: an analytical study in Zagazig. Egypt J Egypt Soc Parasitol. 1991;21:81–5. [PubMed] [Google Scholar]
- 303.Hammouda NA, El-Gebaly WM, Sadaka SM. Seroprevalence of Toxoplasma and cytomegalovirus in complicated pregnancies. J Egypt Soc Parasitol. 1993;23:865–70. [PubMed] [Google Scholar]
- 304.Attia RA, El-Zayat MM, Rizk H, Motawea S. Toxoplasma IgG and IgM antibodies: a case control study. J Egypt Soc Parasitol. 1995;25:877–82. [PubMed] [Google Scholar]
- 305.Azab ME, Kamel AM, Makled KM, et al. Naturally occurring Toxoplasma antibodies in serum and milk of lactating women. J Egypt Soc Parasitol. 1992;22:561–8. [PubMed] [Google Scholar]
- 306.Azab ME, El-Shenawy SFS, El-Hady HM, Ahmad MM. Comparative study of three tests (indirect haemagglutination, direct agglutination, and indirect immunofluorescence) for detection of antibodies to Toxoplasma gondii in pregnant women. J Egypt Soc Parasitol. 1993;23:471–6. [PubMed] [Google Scholar]
- 307.El Nawawy A, Soliman AT, El Azzouni O, et al. Maternal and neonatal prevalence of Toxoplasma and cytomegalovirus (CMV) antibodies and hepatitis-B antigens in an Egyptian rural area. J Trop Pediatr. 1996;42:154–7. doi: 10.1093/tropej/42.3.154. [DOI] [PubMed] [Google Scholar]
- 308.Eshete H, Tessema S, Abebe S, Abebe A. Some notes on toxoplasmosis in pregnant women in Addis Ababa. Ethiop Med J. 1994;32:135–6. [PubMed] [Google Scholar]
- 309.Koskiniemi M, Lappalainen M, Koskela P, et al. The program for antenatal screening of toxoplasmosis in Finland: a prospective cohort study. Scand J Infect Dis (Suppl) 1992;84:70–4. [PubMed] [Google Scholar]
- 310.Carme B, Lenne E, Tirard V, Hayette MP, Gondry J. Étude épidémiologique de la toxoplasmose chez les femmes enceintes a Amiens (Picardie). Nécessite d’une enquête nationale. Méd Malad Inf. 1994;24:1271–3. [Google Scholar]
- 311.Nabias R, Ngouamizokou A, Migot-Nabias F, Mbou-Moutsimbi RA, Lansoud-Soukate J. Enquête sérologique sur la toxoplasmose chez les consultantes du centre de P.M.I. de Franceville (Gabon) Bull Soc Pathol Exot. 1998;91:318–20. [PubMed] [Google Scholar]
- 312.Roos T, Martius J, Gross U, Schrod L. Systematic serologic screening for toxoplasmosis in pregnancy. Obstet Gynecol. 1993;81:243– 50. [PubMed] [Google Scholar]
- 313.Beringer T. Istdie Toxoplasmose-Diagnostik im Rahmender Schwangerschaftsvorsorge sinnvoll? Geburtsh Frauenheilkd. 1992;52:740–1. doi: 10.1055/s-2007-1023804. [DOI] [PubMed] [Google Scholar]
- 314.Gatopoulou AT, Zorba CG, Giakoum GP, Panagiotopoulou AG, Athanasopoulos PK. Serological investigations of antibodies to Toxoplasma gondii in women of reproductive age living in Achaia, in the four-year period 1991–1995. Acta Microbiol Hell. 1997;42:513–21. [Google Scholar]
- 315.Lolis D, Koutsogiannis D, Papadopoulou C, Antoniades G. The risk of primary toxoplasmosis during pregnancy in Greece. Mediterr J Infect Parasit Dis. 1996;11:89–92. [Google Scholar]
- 316.Mittal V, Bhatia R, Singh VK, Sehgal S. Prevalence of toxoplasmosis in Indian women of childbearing age. Indian J Pathol Microbiol. 1995;30:143–5. [PubMed] [Google Scholar]
- 317.Malhotra VL, Bharadwaj Y, Lakshmy A, Kapur H, Prakash K. Comparison of enzyme-linked immunosorbent assay and indirect haemagglutination test in serologic diagnosis of toxoplasmosis. J Commun Dis. 1991;23:154–6. [PubMed] [Google Scholar]
- 318.Chakraborty P, Sinha S, Adhya S, Chakraborty G, Bhattacharya P. Toxoplasmosis in women of child bearing age and infant follow up after in-utero treatment. Indian J Pediatr. 1997;64:879–82. doi: 10.1007/BF02725516. [DOI] [PubMed] [Google Scholar]
- 319.Al Hamdani MM, Mahdi NK. Toxoplasmosis among women with habitual abortion. East Mediterr Health J. 1996;3:310–5. [Google Scholar]
- 320.Franklin DM, Dror Z, Nishri Z. The prevalence and incidence of Toxoplasma antibodies in pregnant women. Isr J Med Sci. 1993;29:285–6. [PubMed] [Google Scholar]
- 321.Cellesi S, Sansoni A, Mencarelli M, Zanchi A, Marsili C. Prevalenza degli anticorpi anti-Toxoplasma gondii in un campione di popolazione femminile della provincia di Siena. G Mal Infett Parassit. 1990;42:333–5. [Google Scholar]
- 322.Valcavi PP, Natali A, Soliani L, Montali S, Dettori G, Cheezi C. Prevalence of anti-Toxoplasma gondii antibodies in the population of the area of Parma (Italy) Eur J Epidemiol. 1995;11:333–7. doi: 10.1007/BF01719439. [DOI] [PubMed] [Google Scholar]
- 323.De Rosa M, Romeo R, Chisari M, Petraroli C, Morabito D, Bolignano G. Prevalenza di anticorpi antitoxoplasma in donne gravide. Ig Mod. 1994;102:403–7. [Google Scholar]
- 324.Buffolano W, Del Pezzo M, Avagliano G, Di Constanzo P. Prevalenza degli anticorpi anti-Toxoplasma nelle donne campane in et à fertile. Microbiol Med. 1993;8:189–91. [Google Scholar]
- 325.Leone F, Allori B, Antognoli A, et al. Toxoplasmosis in pregnancy: research on 2295 women in Rome and its province. Riv Eur Sci Med Farmacol. 1996;18:191–5. [PubMed] [Google Scholar]
- 326.Russo A, Pirruccello B, Brunetti F, Massari G, Passalacqua O, Reina MG. Screening degli anticorpi anti-Toxoplasma in donne en eta feconda. Ig Mod. 1999;111:559–65. [Google Scholar]
- 327.Prabhakar P, Bailey A, Smikle MF, McCaw-Binns A, Ashley D. Seroprevalence of Toxoplasma gondii, rubella virus, cytomegalovirus, herpes simplex virus (TORCH) and syphilis in Jamaican pregnant women. West Indian Med J. 1991;40:166–9. [PubMed] [Google Scholar]
- 328.Im KI, Yong TS, Shin HJ, Lee DH. Anti-Toxoplasma antibody titres in pregnant women. Yonsei Rep Trop Med. 1991;22:15–20. [Google Scholar]
- 329.Ryu JS, Min DY, Ahn MH, et al. Toxoplasma antibody titers by ELISA and indirect latex agglutination test in pregnant women. Korean J Parasitol. 1996;34:233–8. doi: 10.3347/kjp.1996.34.4.233. [DOI] [PubMed] [Google Scholar]
- 330.Kassem HH, Morsy TA. The prevalence of anti-Toxoplasma antibodies among pregnant women in Benghazi, (S.P.L.A.J. ) Libya J Egypt Soc Parasitol. 1991;21:69–74. [PubMed] [Google Scholar]
- 331.Lelong B, Rahelimino B, Candolfi E, et al. Prévalence de la toxoplasmose dans une population de femmes enceintes à Tananarive (Madagascar) Bull Soc Pathol Exot. 1995;88:46–9. [PubMed] [Google Scholar]
- 332.Galván Ramírez M, de la L, Soto Mancilla JL, Velasco Castrejón O, Pérez Medina R. Incidence of anti-Toxoplasma antibodies in women with high-risk pregnancy and habitual abortions. Rev Soc Bras Med Trop. 1995;28:333–7. doi: 10.1590/s0037-86821995000400005. [DOI] [PubMed] [Google Scholar]
- 333.Rai SK, Shibata H, Sumi K, et al. Toxoplasma antibody prevalence in Nepalese pregnant women and women with bad obstetric history. Southeast Asian J Trop Med Public Health. 1998;29:739–43. [PubMed] [Google Scholar]
- 334.Aganga AO, Umoh JU, Ekwempu CC, Kyewalabye EK. Niger J Parasitol. 9–11. 1990. Prevalence studies of human Toxoplasma infection in Zaria, Nigeria; pp. 159–64. [Google Scholar]
- 335.Onadeko MO, Joynson DHM, Payne RA. The prevalence of Toxoplasma infection among pregnant women in Ibadan, Nigeria. J Trop Med Hyg. 1992;95:143–5. [PubMed] [Google Scholar]
- 336.Jenum PA, Kapperud G, Stray-Pedersen B, Melby KK, Eskild A, Eng J. Prevalence of Toxoplasma gondii specific immunoglobulin G antibodies among pregnant women in Norway. Epidemiol Infect. 1998;120:87–92. doi: 10.1017/s0950268897008480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Pal RA, Qayyum M, Yaseen M. Seroprevalence of antibodies to Toxoplasma gondii, with particular reference to obstetric history of patients in Rawalpindi-Islamabad, Pakistan. J Pak Med Assoc. 1996;46:56–8. [PubMed] [Google Scholar]
- 338.Ahmed MU, Hafiz A. Toxoplasmosis and abortion: serological co-relation. J Coll Phys Surg Pak. 1997;7:156–9. [Google Scholar]
- 339.Klufio CA, Delamare O, Amoa AB, Kariwiga G. The prevalence of Toxoplasma antibodies in pregnant patients attending the Port Moresby General Hospital antenatal clinic: a seroepidemiological survey. P N G Med J. 1993;36:4–9. [PubMed] [Google Scholar]
- 340.Pawlowski Z, Mrozewicz B, Kacprzak E, et al. Toksoplazmoza wrodzona w województwie pozna skim. Ginekol Pol. 1994;65:409–12. [PubMed] [Google Scholar]
- 341.El-Sebai MM. Study on toxoplasmosis in Quasseem, Saudi Arabia. J Egypt Soc Parasitol. 1991;21:273–5. [PubMed] [Google Scholar]
- 342.El Hady HM. Toxoplasmosis among pregnant women in Abha, Saudi Arabia. J Egypt Soc Parasitol. 1991;21:811–5. [PubMed] [Google Scholar]
- 343.Dumas N, Le Guenno B, Digoutte JP, Seguela JP. Toxoplasmose en République du Sénégal sondage séro-épidémiologique. Bull Soc Pathol Exot. 1990;83:283–5. [PubMed] [Google Scholar]
- 344.Faye O, Leye A, Dieng Y, Richard-Lenoble D, Diallo S. La toxoplasmose a Dakar. Bull Soc Pathol Exot. 1998;91:249–50. [PubMed] [Google Scholar]
- 345.Diallo S, Ndir O, Dieng Y, et al. Séroprévalence de la toxoplasmose à Dakar (Sénégal) en 1993: étude chez des femmes en période de procréation. Santé. 1996;6:102–6. [PubMed] [Google Scholar]
- 346.Logar J, Novak-Antolič Ž, Zore A, Cerar V, Likar M. Incidence of congenital toxoplasmosis in the Republic of Slovenia. Scand J Infect Dis. 1992;24:105–8. doi: 10.3109/00365549209048408. [DOI] [PubMed] [Google Scholar]
- 347.Jaqueti J, Hernández-García R, Nicolás D, Martinez-Hernández D, Navarro-Gallar F, Garcia-Esteban RJ. Serology against Toxoplasma gondii in pregnant women. Development of prevalence rates in the course of 4 years. Rev Clin Esp. 1991;188:278–80. [PubMed] [Google Scholar]
- 348.Ribes-Bautista A, Saniger Herrera JM, Reche Navarro C, Segovia Martinez A, Peis-Redondo JI, Cruz-Rios MC. Estudio serologico de las infecciones de transmission vertical en las mujeres embarazadas controladas en tres centros de salud de Jaén. Rev Esp Salud Publica. 1996;70:313–8. [PubMed] [Google Scholar]
- 349.Gutiérrez J, Roldán C, Maroto MC. Seroprevalence of human toxoplasmosis. Microbios. 1996;85:73–5. [PubMed] [Google Scholar]
- 350.Menéndez MT, Cordero M, Viejo G, Miguel D, Malo de Molina A, Otero C. Marcadores serólogicos en población gestante de la Zona Básica de Salud de El Natahoya (Gijón). [The serum markers in the pregnant population of the basic health area of El Natahoyo] Aten Primaria. 1996;18:17–21. [PubMed] [Google Scholar]
- 351.Evengård B, Lilja G, Capraru T, et al. A retrospective study of seroconversion against Toxoplasma gondii during 3,000 pregnancies in Stockholm. Scand J Infect Dis. 1999;31:127–9. doi: 10.1080/003655499750006146. [DOI] [PubMed] [Google Scholar]
- 352.Jacquier P, Hohlfeld P, Vorkauf H, Zuber P. Épidémiologie de la toxoplasmose en Suisse: étude nationale de séroprévalence menée chez les femmes enceintes en 1990–1991. Schweiz Med Wochenschr. 1995;125(Suppl 65):29S–38S. [PubMed] [Google Scholar]
- 353.Doehring E, Reiter-Owona I, Bauer O, et al. Toxoplasma gondii antibodies in pregnant women and their newborns in Dar es Salaam, Tanzania. Am J Trop Med Hyg. 1995;52:546–8. doi: 10.4269/ajtmh.1995.52.546. [DOI] [PubMed] [Google Scholar]
- 354.Chintana T. Pattern of antibodies in toxoplasmosis of pregnant women and their children in Thailand. Southeast Asian J Trop Med Public Health. 1991;22(Suppl):107–10. [PubMed] [Google Scholar]
- 355.Chintana T, Sukthana Y, Bunyakai B, Lekkla A. Toxoplasma gondii antibody in pregnant women with and without HIV infection. Southeast Asian J Trop Med Public Health. 1998;29:383–6. [PubMed] [Google Scholar]
- 356.Deniau M, Tourte-Schaefer C, Agbo K, Dupouy-Camet J, Heyer C, Lapierre J. Évaluation des risques de toxoplasmose congénitale au Togo. Bull Soc Pathol Exot. 1991;84:664–72. [PubMed] [Google Scholar]
- 357.Orrett FA. Sero-prevalence of Toxoplasma antibodies among pregnant women in Trinidad. Med Sci Res. 1993;21:399–400. [Google Scholar]
- 358.Ben Ayed Nouira N, Hafsia S, Khaled S, et al. Incidence de la toxoplasmose pendant la grossesse et risque d’infection foetale. Tunis Méd. 1997;75:788–93. [PubMed] [Google Scholar]
- 359.Khemiri B, Mahjoub S, Hmid RB, et al. La séroprévalence de la toxoplasmose et de la rubéole parmi une population de femmes enceintes consultant au CMNRT: Service “A”. Tunis Méd. 1997;75:788–93. [PubMed] [Google Scholar]
- 360.Ndong-Obame T, Ayadi A. La toxoplasmose acquise et congénitale dans la région de Sfax (Tunisie) Bull Soc Franç Parasitol. 1997;15:141–7. [Google Scholar]
- 361.Tavmergen E, Oruc S, Tavmergen EN, Ak M, Capanoglu R. Infertilite olgularinda toksoplazmoz prevalansinin araştirilmasi. Turk J Infect. 1993;7:317–20. [Google Scholar]
- 362.Poyraz O, Ozcelik S, Sagyi G, Guler H. Investigation of Toxoplasma gondii antibodies in women of Sivas region by indirect hemagglutination method. Turk Parazitol Derg. 1995;19:195–9. [Google Scholar]
- 363.Tasci S. Dusuk yapan hastalarda Toxoplasma antikorlari dagiliminin indirekt floresan antikor teknigi ile araştirilmasi. Turk Parazitol Derg. 1995;19:32–8. [Google Scholar]
- 364.Ozcelik S, Poyraz O, Guler O, Saygi G. Investigation of Toxoplasma gondii IgG and IgM antibodies in cases of spontaneous abortion, stillbirth, abnormal birth. Turk Parazitol Derg. 1996;20:159–62. [Google Scholar]
- 365.Dogan N, Akgun Y. Dusuk, olu dogum, erken dogum oykulu dogurganlik yas grubu hastalarda TORCH etkenlerinin dagilimi. Turk Parazitol Derg. 1996;20:317–23. [Google Scholar]
- 366.Berktas M, Balci I, Yilmaz H, Bozkurt H. Cesitli obstetrik sorunlari bulunan kadin hastalarda Toxoplasma antikorlarinin araştirilmasi. Acta Parasitol Turc. 1997;21:360–2. [Google Scholar]
- 367.Gun H, Tanyuksel M, Haznedaroglu T, Erdal N, Gursoy HG. Sađlik meslek lisesi ogrencilerinde toksoplazmosis seropozitifliginin araştirilmasi. Turk Parazitol Derg. 1993;17:15–9. [Google Scholar]
- 368.Altintas N, Kuman HA, Akisu C, Aksoy U, Atambay M. Toxoplasmosis in last four years in Agean region, Turkey. J Egypt Soc Parasitol. 1997;27:439–43. [PubMed] [Google Scholar]
- 369.Durmaz R, Durmaz B, Tas I, Rafiq M. Seropositivity of toxoplasmosis among reproductive-age women in Malatya, Turkey. J Egypt Soc Parasitol. 1995;25:693–8. [PubMed] [Google Scholar]
- 370.Sasmaz E, Bahar IH, Cakir N, Yuce A, Okuyan M. Toksoplazmoz ve cinsel etkinlik. Turk J Infect. 1995;9:419–20. [Google Scholar]
- 371.Kaleli B, Kaleli I, Aktan E, Akal I, Aksit F. Gebelerde toksoplasma IgG ve IgM seropozitifligi. Acta Parasitol Turc. 1997;21:241–3. [Google Scholar]
- 372.Ozcelik S, Guler H, Saygi G, Poyraz O. Investigation of anti-Toxo-plasma gondii antibodies in women who kept pets or eat raw meat. Turk Parazitol Derg. 1996;20:155–8. [Google Scholar]
- 373.Kocabeyoglu O, Yergok YZ, Emekdas G, Kosan E, Birinci I, Diler M. Gebe kadinlarda Toxoplasma IgG ve IgM antikor prevalansi. Turk Parazitol Derg. 1996;20:149–53. [Google Scholar]
- 374.Bayhan G, Suay A, Atmaca S, Yayla M. Gebelerde Toksoplazma seropozitifligi. Acta Parasitol Turc. 1998;22:359–61. [Google Scholar]
- 375.Kara H, Ozcan K, Tanriverdi S, Koltas S. Anne kani, kord kani ve amniyon sivisinda Toxoplasma IgG ve IgM antikorlarinin gosterilmesi. Acta Parasitol Turc. 1999;23:115–8. [Google Scholar]
- 376.Dar FK, Alkarmi T, Uduman S, Abdulrazzaq Y, Grundsell H, Hughes P. Gestational and neonatal toxoplasmosis: regional seroprevalence in the United Arab Emirates. Eur J Epidemiol. 1997;13:567–71. doi: 10.1023/a:1007392703037. [DOI] [PubMed] [Google Scholar]
- 377.Zadik PM, Kudesia G, Siddons AD. Low incidence of primary infection with Toxoplasma among women in Sheffield: a seroconversion study. Br J Obstet Gynaecol. 1995;102:608–10. doi: 10.1111/j.1471-0528.1995.tb11397.x. [DOI] [PubMed] [Google Scholar]
- 378.Allain JP, Palmer CR, Pearson G. Epidemiological study of latent and recent infection by Toxoplasma gondii in pregnant women from a regional population in the U. K J Infect. 1998;36:189–96. doi: 10.1016/s0163-4453(98)80012-1. [DOI] [PubMed] [Google Scholar]
- 379.Soto UR, De Soto ST. Toxoplasmosis y embarazo. Kasmera. 1993;21:1–36. [Google Scholar]
- 380.Bobić B, Djurković-Djaković O, Šibalić D, et al. Epidemiological relationship between human Toxoplasma infection and cats in Belgrade. Acta Vet (Beograd) 1996;46:155–60. [Google Scholar]
- 381.Hirt J, Durlach RA. Toxoplasmosis prenatal. Infect Microbiol Clin. 1995;7:29–30. [Google Scholar]
- 382.Palička P, Slabá H, Zitek K. Active control of congenital toxoplasmosis in the population. Cent Eur J Public Health. 1998;6:265–8. [PubMed] [Google Scholar]
- 383.Lappalainen M, Koskela P, Hedman K, et al. Incidence of primary Toxoplasma infections during pregnancy in southern Finland: a prospective cohort study. Scand J Infect Dis. 1992;24:97–104. doi: 10.3109/00365549209048407. [DOI] [PubMed] [Google Scholar]
- 384.Hengst P. Screening for toxoplasmosis in pregnant women: presentation of a screening programme in the former ‘East’-Germany, and the present status in Germany. Scand J Infect Dis (Suppl) 1992;84:38–42. [PubMed] [Google Scholar]
- 385.Jenum PA, Stray-Pedersen B, Melby KK, et al. Incidence of Toxoplasma gondii infection in 35,940 pregnant women in Norway and pregnancy outcome for infected women. J Clin Microbiol. 1998;36:2900–6. doi: 10.1128/jcm.36.10.2900-2906.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Logar J, Novak-Antolič Ž, Zore A. Serological screening for toxoplasmosis in pregnancy in Slovenia. Scand J Infect Dis. 1995;27:163–4. doi: 10.3109/00365549509018999. [DOI] [PubMed] [Google Scholar]
- 387.Rodriguez JC, Alcantara MJ, Royo G. Toxoplasmosis in pregnancy: new diagnostic techniques. Enferm Infecc Microbiol Clin. 1996;14:145–9. [PubMed] [Google Scholar]
- 388.Sinibaldi J, De Ramirez I. Incidence of congenital toxoplasmosis in live Guatemalan newborns. Eur J Epidemiol. 1992;8:516–20. doi: 10.1007/BF00146369. [DOI] [PubMed] [Google Scholar]
- 389.Berger R, Merkel S, Rudin C. Toxoplasmose und Schwangerschaft – erkenntnisse aus einem Nabelschnurblut-Screening von 30000 Neugeborenen. Schweiz Med Wochenschr. 1995;125:1168–73. [PubMed] [Google Scholar]
- 390.Marder G, Serafini WD, Ulon SN. Prevalencia de anticuerpos toxoplasmicos en personas y animales domesticos y salvajes. Vet Argent. 1990;7:43–48. [Google Scholar]
- 391.Samad MA, Rahman KB, Halder AK. Seroprevalence of Toxoplasma gondii in domestic ruminants in Bangladesh. Vet Parasitol. 1993;47:157–9. doi: 10.1016/0304-4017(93)90186-q. [DOI] [PubMed] [Google Scholar]
- 392.Marana ERM, Navarro IT, Vidotto O, Freire RL, Lott R. Ocorrência de anticorpos anti-Toxoplasma gondii em bovinos de corte, abatidos em matadouros do Norte do Estado do Paraná-Brasil. Semina Ci Agr (Londrina) 1994;15:38–40. [Google Scholar]
- 393.Pita Gondim LF, Barbosa HV, Ribeiro Filho CHA, Saeki H. Serological survey of antibodies to Toxoplasma gondii in goats, sheep, cattle and water buffaloes in Bahia State, Brazil. Vet Parasitol. 1999;82:273–6. doi: 10.1016/s0304-4017(99)00033-3. [DOI] [PubMed] [Google Scholar]
- 394.Garcia JL, Navarro IT, Ogawa L, de Oliveira RC. Soroprevalência do Toxoplasma gondii, em suínos, bovinos, ovinos e eqüinos, e sua correlaçao com humanos, felinos e caninos, oriundos de propriedades rurais do norte do Paraná-Brasil. Ciênc Rural (Santa Maria) 1999;29:91–7. [Google Scholar]
- 395.Huang DS. An investigation of toxoplasmosis in domestic animals in Yunnan Province. Chin J Vet Sci Technol. 1991;21:25–6. [Google Scholar]
- 396.Arias ML, Reyes L, Chinchilla M, Linder E. Seroepidemiology of Toxoplasma gondii (Apicomplexa) in meat producing animals in Costa Rica. Rev Biol Trop. 1994;42:15–20. [PubMed] [Google Scholar]
- 397.Hejlíček K, Literák I. Occurrence of toxoplasmosis and its prevalence in cattle in the south Bohemian region. Acta Vet Brno. 1992;61:195–206. [Google Scholar]
- 398.Chantal J, Dorchies P, Legueno B. Enquête sur certaines zoonoses en République de Djibouti. I. Chez les ruminants à l’abattoir de Djibouti. Rev Méd Vét. 1994;145:633–40. [Google Scholar]
- 399.El Ridi AMS, Nada SMM, Aly AS, Habeeb SM, Aboul-Fattah MM. Serological studies on toxoplasmosis in Zagazig slaughterhouse. J Egypt Soc Parasitol. 1990;20:677–81. [PubMed] [Google Scholar]
- 400.Ibrahim BB, Salama MMI, Gawish NI, Haridy FM. Serological and histopathological studies on Toxoplasma gondii among the workers and the slaughtered animals in Tanta abattoir, Gharbia Governorate. J Egypt Soc Parasitol. 1997;27:273–8. [PubMed] [Google Scholar]
- 401.Cabannes A, Lucchese F, Hernandez JC, et al. Enquête séroépidémiologique sur Toxoplasma gondii chez les ovins, bovins et félins dans le département de la Gironde. Bull Soc Franç Parasitol. 1997;15:11–22. [Google Scholar]
- 402.Kritsepi-Konstantinou M. Serological survey of cattle for toxoplasmosis. Bull Hell Vet Med Soc. 1992;43:48–52. [Google Scholar]
- 403.Mathur K, Tomer VNS, Purohit AK. Study on the seroprevalence of toxoplasmosis, Q fever and brucellosis in cattle with history of abortion and associated ailments. Indian J Anim Health. 1991;30:137–40. [Google Scholar]
- 404.Hafeez M, Charyulu NS, Kumar EGTV, Hasina S. Studies on toxoplasmosis in Andhra Pradesh: detection of serum antibodies in cattle and buffaloes. Cheiron. 1992;20:132–3. [Google Scholar]
- 405.Hoghooghi-Rad N, Afraa M. Prevalence of toxoplasmosis in humans and domestic animals in Ahwaz, capital of Khoozestan Province, south-west Iran. J Trop Med Hyg. 1993;96:163–8. [PubMed] [Google Scholar]
- 406.Hashemi-Fesharki R. Seroprevalence of Toxoplasma gondii in cattle, sheep and goats in Iran. Vet Parasitol. 1996;61:1–3. doi: 10.1016/0304-4017(95)00818-7. [DOI] [PubMed] [Google Scholar]
- 407.Saleem AN, Fatohi FAM. Prevalence of Toxoplasma-like and brucella antibodies in cattle with clinical and gynecological disturbances in Mosul, Iraq. Iraqi J Vet Sci. 1993;6:48–52. [Google Scholar]
- 408.Shkap V, Pipano E, Marcus S, Rapoport E. The prevalence of Toxoplasma gondii antibodies in sheep and cattle in Israel. Isr J Vet Med. 1992;47:100–2. [Google Scholar]
- 409.Avezza F, Greppi G, Agosti M, Belloli A, Faverzani S. La toxoplasmosi bovina: risultati di una indagine siero-epidemiologica. Atti Soc Ital Buiatria. 1993;25:621–4. [Google Scholar]
- 410.Rajamanickam C, Cheah TS, Paramasvaran S. Antibodies to Toxoplasma gondii from domestic animals in Malaysia. Trop Anim Health Prod. 1990;22:61–2. doi: 10.1007/BF02243502. [DOI] [PubMed] [Google Scholar]
- 411.Martínez Gómez F, Ixta Rodríguez O, de los Angeles Cantún Coj H, Castillo Castillo M. Prevalencia de anticuerpos anti-Toxoplasma en bovinos del estado de Tabasco, México. Vet Méx. 1992;23:337–8. [Google Scholar]
- 412.García-Vázquez Z, Rosario-Cruz R, Diaz-Garcia G, Hernandez-Baumgarten O. Seroprevalence of Toxoplasma gondii infection in cattle, swine and goats in four Mexican states. Prev Vet Med. 1993;17:127–32. [Google Scholar]
- 413.Zaki M. Seroprevalence of Toxoplasma gondii in domestic animals in Pakistan. J Pak Med Assoc. 1995;45:4–5. [PubMed] [Google Scholar]
- 414.Fortier B, de Almeida E, Pinto I, Ajana F, Camus D. Prévalence de la toxoplasmose porcine et bovine a Porto. Méd Malad Inf. 1990;20:551–4. [Google Scholar]
- 415.Roger F, Prunaux O, Guignard A. La toxoplasmose bovine et caprine à l’Ile de Réunion: résultats d’une enquête sérologique. Rev Méd Vét. 1991;142:143–6. [Google Scholar]
- 416.El-Metenawy TM. Seroprevalence of Toxoplasma gondii antibodies among domesticated ruminants at Al-Qassim Region, Saudi Arabia. Dtsch Tierärztl Wochenschr. 2000;107:32–3. [PubMed] [Google Scholar]
- 417.Moreno T, Martinez-Gomez F, Becerra C. The seroprevalence of bovine toxoplasmosis in Cordoba, Spain. Ann Trop Med Parasitol. 1991;85:285–6. doi: 10.1080/00034983.1991.11812561. [DOI] [PubMed] [Google Scholar]
- 418.Busato A, Steiner L, Gottstein B, Gaillard C. Häufigkeiten und Ursachen von Kälberverlusten und Kälberkrankheiten in Mutterkuh-betrieben. III. Seroprävalenz ausgewählter Krankheiten und Prävalenz von Endoparasiten beim Absetzen. Dtsch Tierärztl Wochenschr. 1997;104:191–5. [PubMed] [Google Scholar]
- 419.Suteeraparp P, Pholpark S, Pholpark M, et al. Seroprevalence of antibodies to Neospora caninum and associated abortion in dairy cattle from central Thailand. Vet Parasitol. 1999;86:49–57. doi: 10.1016/s0304-4017(99)00130-2. [DOI] [PubMed] [Google Scholar]
- 420.Adesiyun AA, Cazabon EPI. Seroprevalences of brucellosis, Q-fever and toxoplasmosis in slaughter livestock in Trinidad. Rev Élev Méd Vét Pays Trop. 1996;49:28–30. [PubMed] [Google Scholar]
- 421.Kucukerden N. Elaziđ ve yöresi sigiirlarinda Toxoplasma gondii nin yaylisi üzerine araþtirmalar. Sađlik Bilimleri Derg. 1994;8:62. [Google Scholar]
- 422.Öz Ý, Özyer M, Çorak R. Adana yöresi siđir koyun ve keçilerinde ELISA ve IHA testleri ile toxoplasmosis’in yayginliđinin araþtirilmasi: a study on the prevalence of toxoplasmosis in cattle, sheep and goats in Adana region by using ELISA and IHA tests. Etlik Vet Mikrobiyol Derg. 1995;8:87–99. [Google Scholar]
- 423.Eren H, Babür C, Erdal N, Sert H. Ankara ve Aydin yöresi sigirlarinda Sabin–Feldman testi ile Toxoplasma gondii‘nin prevalansi. Turk Hij Deney Biyol Derg. 1997;54:31–4. [Google Scholar]
- 424.Ýnci A, Aydin N, Babür C, Çam Y, Akdođan C, Kuzan Þ. Kayseri yöresinde siđir ve koyunlarda toksoplazmozis ve brusellozis üzerine seroepidemiyolojik araştirmalar: seroepidemiological studies on toxoplasmosis and brucellosis in cattle and sheep around Kayseri. Pendik Vet Mikrobiyol Derg. 1999;30:41–6. [Google Scholar]
- 425.Huong LTT, Ljungström BL, Uggla A, Björkman C. Prevalence of antibodies to Neospora caninum and Toxoplasma gondii in cattle and water buffaloes in southern Vietnam. Vet Parasitol. 1998;75:53–7. doi: 10.1016/s0304-4017(97)00178-7. [DOI] [PubMed] [Google Scholar]
- 426.Dubey JP, Romand S, Hilali M, Kwok OCH, Thulliez P. Seroprevalence of antibodies to Neospora caninum and Toxoplasma gondii in water buffaloes (Bubalus bubalis) from Egypt. Int J Parasitol. 1998;28:527–9. doi: 10.1016/s0020-7519(97)00190-2. [DOI] [PubMed] [Google Scholar]
- 427.Navidpour S, Hoghooghirad N. Seroprevalence of anti-Toxoplasma gondii antibodies in buffaloes in Khoozestan province. Iran Vet Parasitol. 1998;77:191–4. doi: 10.1016/s0304-4017(97)00148-9. [DOI] [PubMed] [Google Scholar]
- 428.Salaheddin-Nassr S. Thesis, Dr vet med, Wein. 1975. Zum Auftreten von Toxoplasmaantikörpern im Blutserum verschiedener Haustierarten (Vergleichende Untersuchungen mit verschiedenen serologischen Methoden) [Google Scholar]
- 429.Edelhofer R. Prevalence of antibodies against Toxoplasma gondii in pigs in Austria - an evaluation of data from 1982 and 1992. Parasitol Res. 1994;80:642–4. doi: 10.1007/BF00932946. [DOI] [PubMed] [Google Scholar]
- 430.Quehenberger P, Schuller W, Awad-Masalmeh M. Untersuchung über das Vorkommen von komplementbindenden Antikörpern gegen Chlamydia psittaci und Toxoplasma gondii beim Schwein in den einzelnen Bundesländern Österreichs. Wien Tierärztl Monatsschr. 1990;77:285–90. [Google Scholar]
- 431.Boch J, Rommel M, Janitschke K. Beiträge zur Toxoplasmose des Schweines. II. Untersuchungen von Schlachtschweinen auf Toxoplasma-Infektionen. Berl Münch Tierärztl Wochenschr. 1964;77:244–7. [Google Scholar]
- 432.Schaal E, Kleikamp I. Untersuchungen über die Verbreitung der Toxoplasmose bei Schlachtschweinen in Westfalen. Berl Münch Tierärztl Wochenschr. 1976;89:341–4. [PubMed] [Google Scholar]
- 433.Boch J, Neurohr B. Vorkommen latenter Toxoplasma infektionen bei Schweinen in Süddeutschland und deren Nachweis mit IFAT und IHA. Tierärztl Umsch. 1982;37:820–6. [Google Scholar]
- 434.Seineke P. Thesis. Dr vet med; Hannover: 1996. Seroprävalenz von antikörpern gegen Toxoplasma gondii bei Schafen, Ziegen und Schweinen in Niedersachsen. [Google Scholar]
- 435.Cremers FXMM. De waarde van de Sabin–Feldmanreactie voor de diagnostiek van toxoplasmose bij het verken, rund en schaap. Tijdschr Diergeneeskd. 1969;94:695–8. [Google Scholar]
- 436.Van Knapen F, Franchimont JH, van der Lugt G. Prevalence of antibodies to Toxoplasma in farm animals in the Netherlands and its implication for meat inspection. Vet Q. 1982;4:101–5. doi: 10.1080/01652176.1982.9693848. [DOI] [PubMed] [Google Scholar]
- 437.Berends BR, Smeets JFM, Harbers AHM, Van Knapen F, Snijders JMA. Investigations with enzyme-linked immunosorbent assays for Trichinella spiralis and Toxoplasma gondii in the Dutch ‘Integrated quality control for finishing pigs’ research project. Vet Q. 1991;13:190–8. doi: 10.1080/01652176.1991.9694308. [DOI] [PubMed] [Google Scholar]
- 438.Damriyasa IM, Bauer C, Volmer R, et al. Survey on endo- and ectoparasite infections in sow farms in Southern Hessen, Germany. Proceedings of the 17th International Conference of the World Association for the Advancement of Veterinary Parasitology; 1999. [Google Scholar]
- 439.Fernández F, Ouviña G, Codoni C. Seroprevalencia toxoplasmotica en porcinos de consumo en la zone oeste del Gran Buenos Aires, Argentina. Vet Argent. 1998;15:269–71. [Google Scholar]
- 440.Guimarães AM, Ribeiro MFB, Lima JD, de Almeida TMB. Freqüência de anticorpos anti-Toxoplasma gondii em suínos da raça Piau. Arq Bras Med Vet Zootec. 1992;44:69–71. [Google Scholar]
- 441.Araujo FAP, Souza WJS. Antibody response against Toxoplasma gondii (Apicomplexa) measured by indirect fluorescent antibody technique in pigs naturally infected in the area of Great Erechim, RS, Brazil. Arq Fac Vet UFRGS (Porto Alegre) 1997;25:75–83. [Google Scholar]
- 442.Araujo FAP, Santos JR, Souza WJS. Detection of Toxoplasma gondii infection in naturally infected pigs by enzyme-linked immunosorbent assay (ELISA) in the area of Great Erechim, RS, Brazil. Arq Fac Vet UFRGS (Porto Alegre) 1998;26:57–65. [Google Scholar]
- 443.Smith HJ. Seroprevalence of anti-Toxoplasma IgG in Canadian swine. Can J Vet Res. 1991;55:380–1. [PMC free article] [PubMed] [Google Scholar]
- 444.Gajadhar AA, Aramini JJ, Tiffin G, Bisaillon JR. Prevalence of Toxoplasma gondii in Canadian market-age pigs. J Parasitol. 1998;84:759–63. [PubMed] [Google Scholar]
- 445.Tamayo R, Contreras M, del C, Méndez M, Castro M. Toxoplasmosis en cerdos beneficiados en las plantas faenadoras de Temuco y Valdivia, Chile. Arch Med Vet. 1990;22:95–9. [Google Scholar]
- 446.Hejlíček K, Literák I. Prevalence of toxoplasmosis in pigs in the region of South Bohemia. Acta Vet Brno. 1993;62:159–66. [Google Scholar]
- 447.Hejlíček K, Literák I. Zur Epizootiologie und Ökologie der Schweinetoxoplasmose. Wien Tierärztl Monatsschr. 1994;81:170–4. [Google Scholar]
- 448.Hirvelä-Koski V. The prevalence of Toxoplasma antibodies in swine sera in Finland. Acta Vet Scand. 1992;33:21–5. doi: 10.1186/BF03546932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 449.Genchi G, Polidori GA, Zaghini L, Lanfranchi P. Aspetti epidemiologici della toxoplasmosi nell’ allevamento intensivo del suino. Arch Vet Ital. 1991;42:105–11. [Google Scholar]
- 450.Asami S, Kawai S, Inoue M, Shimizu H, Kano S, Suzuki M. Prevalence of antibodies against Toxoplasma gondii in pigs in Gunma Prefecture. Jpn J Parasitol. 1995;44:28–31. [Google Scholar]
- 451.Weigel RM, Dubey JP, Siegel AM, et al. Prevalence of antibodies to Toxoplasma gondii in swine in Illinois in 1992. J Am Vet Med Assoc. 1995;206:1747–51. [PubMed] [Google Scholar]
- 452.Dubey JP, Weigel RM, Siegel AM, et al. Sources and reservoirs of Toxoplasma gondii infection on 47 swine farms in Illinois. J Parasitol. 1995;81:723–9. [PubMed] [Google Scholar]
- 453.Zimmerman JJ, Dreesen DW, Owen WJ, Beran GW. Prevalence of toxoplasmosis in swine from Iowa. J Am Vet Med Assoc. 1990;196:266–70. [PubMed] [Google Scholar]
- 454.Dubey JP, Thulliez P, Powell EC. Toxoplasma gondii in Iowa sows: comparison of antibody titers to isolation of T. gondii by bioassays in mice and cats. J Parasitol. 1995;81:48–53. [PubMed] [Google Scholar]
- 455.Patton S, Zimmerman J, Roberts T, et al. Seroprevalence of Toxoplasma gondii in hogs in the National Animal Health Monitoring System (NAHMS) J Eukaryot Microbiol. 1996;43:121S. doi: 10.1111/j.1550-7408.1996.tb05037.x. [DOI] [PubMed] [Google Scholar]
- 456.Davies PR, Morrow WEM, Deen J, Gamble HR, Patton S. Seroprevalence of Toxoplasma gondii and Trichinella spiralis in finishing swine raised in different production systems in North Carolina, USA. Prev Vet Med. 1998;36:67–76. doi: 10.1016/s0167-5877(98)00072-5. [DOI] [PubMed] [Google Scholar]
- 457.Pandey VS, Van Knapen F. The seroprevalence of toxoplasmosis in sheep, goats and pigs in Zimbabwe. Ann Trop Med Parasitol. 1992;86:313–5. doi: 10.1080/00034983.1992.11812671. [DOI] [PubMed] [Google Scholar]
- 458.Hove T, Dubey JP. Prevalence of Toxoplasma gondii antibodies in sera of domestic pigs and some wild game species from Zimbabwe. J Parasitol. 1999;85:372–3. [PubMed] [Google Scholar]
- 459.Smith KE, Zimmerman JJ, Patton S, Beran GW, Hill HT. The epidemiology of toxoplasmosis on Iowa swine farms with an emphasis on the roles of free-living mammals. Vet Parasitol. 1992;42:199–211. doi: 10.1016/0304-4017(92)90062-e. [DOI] [PubMed] [Google Scholar]
- 460.Assadi-Rad AM, New JC, Patton S. Risk factors associated with transmission of Toxoplasma gondii to sows kept in different management systems in Tennessee. Vet Parasitol. 1995;57:289–97. doi: 10.1016/0304-4017(94)00677-5. [DOI] [PubMed] [Google Scholar]
- 461.Vidotto O, Navarro IT, Giraldi N, Mitsuka R, Freire RL. Estudos epidemiológicos da toxoplasmose em suínos da região de Londrina – PR. Semina Londrina. 1990;11:53–9. [Google Scholar]
- 462.Grünspan ED, Moreira WS, Edelweiss MIA, et al. Imunoglobulinas antitoxoplásmicas e retinocorodite em suínos. Ciênc Rural (Santa Maria) 1995;25:261–4. [Google Scholar]
- 463.Arko-Mensah J, Bosompem KM, Canacoo EA, Wastling JM, Akanmori BD. The seroprevalence of toxoplasmosis in pigs in Ghana. Acta Trop. 2000;76:27–31. doi: 10.1016/s0001-706x(00)00085-1. [DOI] [PubMed] [Google Scholar]
- 464.Chang GN, Tsai SS, Kuo M, Dubey JP. Serological survey of swine toxoplasmosis in Taiwan. J Chin Soc Vet Sci. 1990;16:103–11. [Google Scholar]
- 465.Dubey JP, Gamble HR, Rodrigues AO, Thulliez P. Prevalence of antibodies to Toxoplasma gondii and Trichinella spiralis in 509 pigs from 31 farms in Oahu, Hawaii. Vet Parasitol. 1992;43:57–63. doi: 10.1016/0304-4017(92)90048-e. [DOI] [PubMed] [Google Scholar]
- 466.Gamble HR, Brady RC, Dubey JP. Prevalence of Toxoplasma gondii infection in domestic pigs in the New England states. Vet Parasitol. 1999;82:129–36. doi: 10.1016/s0304-4017(99)00004-7. [DOI] [PubMed] [Google Scholar]
- 467.Garcia JL, Navarro IT, Ogawa L, Marana ERM. Soroprevalência do Toxoplasma gondii em galinhas (Gallus gallus domesticus) de criações domésticas, oriundas de propriedades rurais do norte do Paraná, Brasil. Ciênc Rural (Santa Maria) 2000;30:123–7. [Google Scholar]
- 468.Yan AW, Yu XL, Long ZM, et al. [Investigation of Toxoplasma gondii in man and animals in the South Sea area of China] In: Xu RM, Zhang QE, et al., editors. Contributions to epidemiological survey in China. Vol. 1. Beijing: Military Medical Science Press; 1995. pp. 27–9. [Google Scholar]
- 469.Literák I, Hejlíček K. Incidence of Toxoplasma gondii in populations of domestic birds in the Czech Republic. Avian Pathol. 1993;22:275– 81. doi: 10.1080/03079459308418920. [DOI] [PubMed] [Google Scholar]
- 470.Devada K, Anandan R, Dubey JP. Serologic prevalence of Toxoplasma gondii in chickens in Madras, India. J Parasitol. 1998;84:621–2. [PubMed] [Google Scholar]
- 471.Ghorbani M, Gharavi MJ, Kahnamoui A. Serological and parasitological investigations on Toxoplasma infection in domestic fowls in Iran. Iranian J Public Health. 1990;19:9–17. [Google Scholar]
- 472.Matsuo K. Survei serologik antibodi Toxoplasma gondii dengan uji aglutinasi lateks pada ayam di propinsi lampung. J Ilmu Ternak Vet. 1996;2:73–5. [Google Scholar]
- 473.Ýnci A, Babär C, Dincer S, Erdal N. Turkiye’nin bazi illerinde evcil kanatlilarda Sabin–Feldman boya testi ile anti-Toxoplasma gondii antikorlarinin saptanmasi. Acta Parasitol Turc. 1998;22:420–3. [Google Scholar]
- 474.Babür C, Gicik Y, Ýnci A. Ankara’da guvercinlerde Sabin–Feldman boya testi ile anti-Toxoplasma gondii antikorlarinin araştirilmasi. Acta Parasitol Turc. 1998;22:308–10. [Google Scholar]
- 475.Lindsay DS, Smith PC, Blagburn BL. Prevalence and isolation of Toxoplasma gondii from wild turkeys in Alabama. J Helminthol Soc Wash. 1994;61:115–7. [Google Scholar]
- 476.Iskandar T. Pengisolasian Toxoplasma gondii dari otot diafragma seekor domba yang mengandung titer antibodi tinggi dan tanahtinja dari seekor kucing. J Ilmu Ternak Vet. 1998;3:111–6. [Google Scholar]
- 477.Amin AM, Morsy TA. Anti-Toxoplasma antibodies in butchers and slaughtered sheep and goats in Jeddah Municipal abattoir, Saudi Arabia. J Egypt Soc Parasitol. 1997;27:913–8. [PubMed] [Google Scholar]
- 478.Babür C, Karaer Z. Koyunlarda Toxoplasma gondii‘nin seroinsidensi ve izolasyonu üzerine arast\i\rmalar. Acta Parasitol Turc. 1997;21:293–9. [Google Scholar]
- 479.Malik MA, Dreesen DW, de la Cruz A. Toxoplasmosis in sheep in northeastern United States. J Am Vet Med Assoc. 1990;196:263–5. [PubMed] [Google Scholar]
- 480.Schweighardt H. Spezifische Abortursachen bei Rind und Schaf unter besonderer Berücksichtigung der mikrobiellen Erreger (Protozoen, Bakterien, Pilze) Wien Tierärztl Monatsschr. 1991;78:2–6. [Google Scholar]
- 481.Samad MA, Rahman KMB, Basher SA. Serological status to natural Toxoplasma gondii infection in mixed flocks of sheep and goats in Bangladesh. J Protozool Res. 1993;3:25–8. [Google Scholar]
- 482.Achu-Kwi MD, Ekue NF. Prevalence of Toxoplasma gondii antibodies in Djallonke sheep flocks in the Vina Division, Cameroon. Bull Anim Health Prod Afr. 1994;42:89–92. [Google Scholar]
- 483.Waltner-Toews D, Mondesire R, Menzies P. The seroprevalence of Toxoplasma gondii in Ontario sheep flocks. Can Vet J. 1991;32:734–7. [PMC free article] [PubMed] [Google Scholar]
- 484.Gorman T, Arancibia JP, Lorca M, Hird D, Alcaíno H. Seroprevalence of Toxoplasma gondii infection in sheep and alpacas (Llama pacos) in Chile. Prev Vet Med. 1999;40:143–9. doi: 10.1016/s0167-5877(99)00044-6. [DOI] [PubMed] [Google Scholar]
- 485.Rajković-Janje R, Marinculić A, Pauković Č, č Ž, Horvat J. Nalaz protutijela za protozoon Toxoplasma gondii u krvi ovaca u Republici Hrvatskoj. Vet Stanica. 1994;25:145–50. [Google Scholar]
- 486.Hejlíček K, Literák I. Incidence and prevalence of toxoplasmosis among sheep and goats in southern and western Bohemia. Acta Vet Brno. 1994;63:151–9. [Google Scholar]
- 487.Sting R, Nagel C, Steng G. Die Bedeutung infektiöser Abortursachen in Schafherden im nördlichen Baden-Württemberg unter besonderer Berücksichtigung von Chlamydia psittaci. Berl Münch Tierärztl Wochenschr. 1997;110:5–11. [PubMed] [Google Scholar]
- 488.Stefanakis A, Bizake A, Krambovitis E. Seroprevalence of toxoplasmosis in the sheep and goats of Crete, Greece. Bull Hell Vet Med Soc. 1995;46:243–9. [Google Scholar]
- 489.Dubey JP, Somvanshi R, Jithendran KP, Rao JR. High seroprevalence of Toxoplasma gondii in goats from Kumaon region of India. J Vet Parasitol. 1993;7:17–21. [Google Scholar]
- 490.O’Brien D, Geraghty V. A serological survey for toxoplasmosis in sheep in Ireland. Ir Vet J. 1990:43–6. [Google Scholar]
- 491.Aldomy FMM, Wilsmore AJ. Prevalence of Toxoplasma antibodies in small ruminants in Jordan. Pak Vet J. 1998;18:213–5. [Google Scholar]
- 492.Harps O. Thesis. Dr Vet Med; Hannover: 1993. Untersuchungen über die seroprävalenz von Toxoplasma-infektionen bei kleinen Wiederkäuern in Jordanien. [Google Scholar]
- 493.García-Vázquez Z, Rosario-Cruz R, Solorzano-Salgado M. Prevalence of antibodies against Toxoplasma gondii in sheep and goats in three states of Mexico. Prev Vet Med. 1990;10:25–9. [Google Scholar]
- 494.Weitzman GL, Stem EC, Gilfillan RS, Lindenmayer JM. Preliminary serological survey for bluetongue and toxoplasmosis in sheep in Niger. Trop Anim Health Prod. 1991;23:258. doi: 10.1007/BF02357112. [DOI] [PubMed] [Google Scholar]
- 495.Amin JD, Silsmore AJ. A Serological survey of some abortifacient diseases of sheep and goats in the Maiduguri area of Nigeria. Bull Anim Health Prod Afr. 1993;41:123–8. [Google Scholar]
- 496.Kovacova D. Serologicka prevalencia Toxoplasma gondii u oviec. Veterinarstvi. 1993;43:51–4. [Google Scholar]
- 497.Moreno T, Martinez-Gomez F, Hernandez-Rodriguez S, de Setefilla Martinez-Cruz M, Martinez-Moreno A. The seroprevalence of ovine toxoplasmosis in Cordoba, Spain. Ann Trop Med Parasitol. 1991;85:287–8. doi: 10.1080/00034983.1991.11812562. [DOI] [PubMed] [Google Scholar]
- 498.Mainar RC, de la Cruz C, Asensio A, Domínguez L, Vázquez-Boland JA. Prevalence of agglutinating antibodies to Toxoplasma gondii in small ruminants of the Madrid region, Spain, and identification of factors influencing seropositivity by multivariate analysis. Vet Res Commun. 1996;20:153–9. doi: 10.1007/BF00385636. [DOI] [PubMed] [Google Scholar]
- 499.Marca MC, Ramos JJ, Loste A, Fernández A, Hernández M. Prevalencia de toxoplasmosis ovina en la provincia of Zaragoza. Med Vet. 1996;13:503–6. [Google Scholar]
- 500.Marca MC, Ramos JJ, Loste A, Sáez T, Sanz MC. Comparison of indirect immunofluorescent antibody test and modified direct agglutination test methods for detection of Toxoplasma gondii antibodies in adult sheep in Spain. Vet Parasitol. 1996;67:99–103. doi: 10.1016/s0304-4017(96)01031-x. [DOI] [PubMed] [Google Scholar]
- 501.Bastiaensen P, Dorny P. Ovine toxoplasmosis in Suriname and its possible impact on human infection. Tropicultura. 1999;16–17:18–20. [Google Scholar]
- 502.Lundén A, Carlsson U, Näslund K. Toxoplasmosis and border disease in 54 Swedish sheep flocks: seroprevalence and incidence during one gestation period. Acta Vet Scand. 1992;33:175–84. doi: 10.1186/BF03547324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 503.Dumanli N, Güler S, Körođlu E, Orak S. Elaziđ yöresinde koyunlarda Toxoplasma gondii‘nin yayiliþi. Dođa Tr J Vet Anim Sci. 1991;16:10–8. [Google Scholar]
- 504.Babür C, Ýnci A, Karaer Z. Cankiri yöresinde koyun ve kecilerde Toxoplasma gondii seropozitifliginin Sabin–Feldman boya testi ile saptanmasi. Acta Parasitol Turc. 1997;21:409–12. [Google Scholar]
- 505.Altintas K, Gungor C, Zeybek H, Yarali C. Sabin–Feldman testi ile Ankara yöresi koyunlarinda Toxoplasma gondii prevalansinin saptanmasi. Turk Parazitol Derg. 1997;21:63–5. [Google Scholar]
- 506.Samad MA, Clarkson MJ. Seroconversion to natural Toxoplasma gondii infection during reproductive cycle and its effect on reproduction in sheep. Bangladesh Vet J. 1994;28:1–6. [Google Scholar]
- 507.Savio E, Nieto A. Ovine toxoplasmosis: seroconversion during pregnancy and lamb birth rate in Uruguayan sheep flocks. Vet Parasitol. 1995;60:241–7. doi: 10.1016/0304-4017(94)00764-8. [DOI] [PubMed] [Google Scholar]
- 508.Freyre A, Bonino J, Falcon J, et al. Prevalencia, incidencia, y perdidas por toxoplasmosis en siete majadas del Uruguay. Prod Ovina. 1994;7:57–69. [Google Scholar]
- 509.Freyre A, Bonino J, Falcon J, et al. Evaluacion de las perdidas economicas debidas a toxoplasmosis en ovinos en el Uruguay. Parasitol Día. 1996;20:100–8. [Google Scholar]
- 510.Deconinck P, Pangui LJ, Akakpo J, et al. Prévalence de la toxoplasmose chez les petits ruminants en Afrique tropicale: résultats d’une enquête séro-épidémiologique sur 1042 animaux. Rev Méd Vét. 1996;147:377–8. [Google Scholar]
- 511.Freire RL, Giraldi N, Vidotto O, Navarro IT. Levantamento soroepidemiológico da toxoplasmose em ovinos na região de Londrina, Paraná. Arq Bras Med Vet Zootec. 1995;47:609–12. [Google Scholar]
- 512.Zhang DL, Ma JW, Du CB, et al. Serological determination of toxoplasmosis in sheep and goats in some villages and towns of Tianzhu, Gansu. Chin J Vet Sci Technol. 1996;26:31. [Google Scholar]
- 513.Van der Puije WN, Bosompem KM, Canacoo EA, Wastling JM, Akanmori BD. The prevalence of anti-Toxoplasma gondii antibodies in Ghanan sheep and goats. Acta Trop. 2000;76:21–6. doi: 10.1016/s0001-706x(00)00084-x. [DOI] [PubMed] [Google Scholar]
- 514.Cruz-Vazquez CC, García-Vázquez Z, Rosario-Cruz R, Solorzano-Salgado M. Ovine toxoplasmosis in Huitzilac, Morelos, Mexico. Prev Vet Med. 1992;12:27–33. [Google Scholar]
- 515.Pangui LJ, Lahamdi A, Samb F. Utilisation de l’IFI et de l’ELISA dans une enquête sérologique de la toxoplasmose chez le mouton ‘de case’ à Dakar - Sénégal. Rec Méd Vét. 1993;169:45–6. [Google Scholar]
- 516.Babür C, Karaer Z, Çakmak A, Yarali C, Zeybek H. Ankara yöresinde Sabin–Feldman (SF), indirekt floresan antikor (IFA), latex aglutinasyon (LA) testleri ile koyun toxoplasmosis’inin prevalansi. Sađlik Bilimleri Derg. 1996;10:273–7. [Google Scholar]
- 517.Zeybek H, Yarali C, Nishikawa H, Nishikawa F, Dündar B. Ankara yöresi koyunlarinda Toxoplasma gondii‘nin prevalansinin saptanmasi. Etlik Vet Mikrobiyol Derg. 1995;8:80–6. [Google Scholar]
- 518.Samad MA, Dey BC, Chowdhury NS, Akhtar S, Khan MR. Sero-epidemiological studies on Toxoplasma gondii infection in man and animals in Bangladesh. Southeast Asian J Trop Med Public Health. 1997;28:339–43. [PubMed] [Google Scholar]
- 519.Binta MG, Mushi EZ, Raborokgwe M, Monyame RK, Ndebele TR. The prevalence in Botswana of antibodies to Toxoplasma gondii in goats with a history of abortion. Zimbabwe Vet J. 1998;29:47–50. [Google Scholar]
- 520.Serra-Freire da NM, Norberg AN, Gazeta YGS. Toxoplasmosis caprina no Rio de Janeiro, Brasil. Parasitol Día. 1994;18:77–81. [Google Scholar]
- 521.Sella MZ, Navarro IT, Vidotto O, Freire RL, Shida PN. Epidemiologia da toxoplasmose caprina: levantamento sorológico do Toxoplasma gondii em caprinos leiteiros na micro região de Londrina, Paraná, Brasil. Rev Bras Parasitol Vet. 1994;3:13–16. [Google Scholar]
- 522.Rajković-Janje R, Marinculić A, Jovanović-Bunta V, Živičnjak T. Seroepidemiological survey of toxoplasmosis in goats in the Republic of Croatia. Vet Arh. 1993;63:125–9. [Google Scholar]
- 523.Dorny P, Casman C, Sani R, Vercruysse J. Toxoplasmosis in goats: a sero-epidemiological study in Peninsular Malaysia. Ann Trop Med Parasitol. 1993;87:407–10. doi: 10.1080/00034983.1993.11812786. [DOI] [PubMed] [Google Scholar]
- 524.Opel U, Charleston WAG, Pomroy WE, Rommel M. A survey of the prevalence of Toxoplasma infection in goats in New Zealand and a comparison of the latex agglutination and indirect fluorescence tests. Vet Parasitol. 1991;40:181–6. doi: 10.1016/0304-4017(91)90098-g. [DOI] [PubMed] [Google Scholar]
- 525.Antonis AFG, van Knapen F, Dercksen DP, Jager PM. Toxoplasmose bij geiten in Nederland: een pilot-studie. Tijdschr Diergeneeskd. 1998;123:561–5. [PubMed] [Google Scholar]
- 526.Rodríguez-Ponce E, Molina JM, Hernández S. Seroprevalence of goat toxoplasmosis on Grand Canary Island (Spain) Prev Vet Med. 1995;24:229–34. [Google Scholar]
- 527.Babür C, Piskin FC, Biyikoglu G, Dundar B, Yarali C. Eskisehir Cifteler Harasi Ankara keçilerinde anti-Toxoplasma gondii antikorlarinin Sabin–Feldman Dye Test (SFDT) ile araştirilmasi. Acta Parasitol Turc. 1999;23:72–4. [Google Scholar]
- 528.Patton S, Johnson SS, Puckett K. Prevalence of Toxoplasma gondii antibodies in nine populations of dairy goats: compared titers using modified direct agglutination and indirect hemagglutination. J Parasitol. 1990;76:74–7. [PubMed] [Google Scholar]
- 529.Nieto SO, Meléndez RD. Seroprevalence of Toxoplasma gondii in goats from arid zones of Venezuela. J Parasitol. 1998;84:190–1. [PubMed] [Google Scholar]
- 530.Literák I, Skřivánek M, Skalka B, Celer V. Antibodies to some infections on large goat farms in the Czech Republic. Vet Med -Czech. 1995;40:133–6. [PubMed] [Google Scholar]
- 531.Šlosárková S, Literák I, Skřivánek M, Svobodová V, Suchý P, Herzig I. Toxoplasmosis and iodine deficiency in Angora goats. Vet Parasitol. 1999;81:89–97. doi: 10.1016/s0304-4017(98)00244-1. [DOI] [PubMed] [Google Scholar]
- 532.Chartier C, Beziaud E, Buzoni-Gatel D, et al. Enquête séro-épidémiologique sur les avortements infectieux des caprins en région Poitou-Charentes. Rev Méd Vét. 1997;148:489–96. [Google Scholar]
- 533.Dorny P, van Aken D. Prevalence of Toxoplasma gondii antibodies in goats in Sri Lanka. Ann Trop Med Parasitol. 1992;86:83–5. doi: 10.1080/00034983.1992.11812634. [DOI] [PubMed] [Google Scholar]
- 534.Yađci Þ, Babür C, Karaer Z, Çakmak A. Ankara yöresinde keçilerde toxoplasmosis: toxoplasmosis of goats in Ankara. Etlik Vet Mikrobiyol Derg. 1997;9:94–8. [Google Scholar]
- 535.Bisson A, Maley S, Rubaire-Akiiki CM, Wastling JM. The seroprevalence of antibodies to Toxoplasma gondii in domestic goats in Uganda. Acta Trop. 2000;76:33–8. doi: 10.1016/s0001-706x(00)00086-3. [DOI] [PubMed] [Google Scholar]
- 536.Dubey JP, Adams DS. Prevalence of Toxoplasma gondii antibodies in dairy goats from 1982 to 1984. J Am Vet Med Assoc. 1990;196:295–6. [PubMed] [Google Scholar]
- 537.Dubey JP, Venturini MC, Venturini L, McKinney J, Pecoraro M. Prevalence of antibodies to Sarcocystis neurona, Toxoplasma gondii, and Neospora caninum in horses from Argentina. Vet Parasitol. 1999;86:59–62. doi: 10.1016/s0304-4017(99)00127-2. [DOI] [PubMed] [Google Scholar]
- 538.Vidotto O, Kano FS, Freire RL, et al. Ocorrência de anticorpos anti-Toxoplasma gondii em eqüinos procedentes de quatro estados (SP, PR, MS e MT) abatidos em Apucarana, PR. Semina Londrina. 1997;18:9–13. [Google Scholar]
- 539.Gazeta GS, Dutra AEA, Norberg AN, et al. Freqüência de anticorpos anti-Toxoplasma gondii em soros de eqüinos no Estado do Rio de Janeiro, Brasil. Rev Bras Parasitol Vet. 1997;6:87–91. [Google Scholar]
- 540.Dubey JP, Kerber CE, Granstrom DE. Serologic prevalence of Sarcocystis neurona, Toxoplasma gondii, and Neospora caninum in horses in Brazil. J Am Vet Med Assoc. 1999;215:970–2. [PubMed] [Google Scholar]
- 541.Hejlíček K, Literák I. Prevalence of antibodies to Toxoplasma gondii in horses in the Czech Republic. Acta Parasitol. 1994;39:217–9. [Google Scholar]
- 542.Uggla A, Mattson S, Juntti N. Prevalence of antibodies to Toxoplasma gondii in cats, dogs and horses in Sweden. Acta Vet Scand. 1990;31:219–22. doi: 10.1186/BF03547564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 543.Ýnci A, Babür C, Karaer Z. Gemlik askeri harasi atlarinda anti-Toxoplasma gondii antikorlarinin Sabin–Feldman boya testi ile saptanmasi. Turk Parazitol Derg. 1996;20:417–9. [Google Scholar]
- 544.Babür C, Yađci Þ, Sert H, Yaman N, Ateþ C, Karaer ZTC. Sađlik bakanliđi Refik Saydam Hifzisihha merkez baþkanliđi serum üretim çiftliđi atlarinda toxoplasmosis’in serodiagnozu: Serodiagnose of toxoplasmosis in horses of Health Refik Saydam Hifzisihha Centre Serum Ranch. Etlik Vet Mikrobiyol. 1997;9:1–5. [Google Scholar]
- 545.Zeybek H, Dundar B, Altintas K, Gungor C. Tek tirnakli hayvanlarda toxoplasmosis’in seroprevalansi. Acta Parasitol Turc. 1998;22:424–7. [Google Scholar]
- 546.Babür C, Çakmak A, Biyikoglu G, Piskin FC. Ankara Ataturk Orman Çiftliđi Hayvanat Bahcesi vahsi hayvanlarini beslemek icin kesilen atlarda anti-Toxoplasma gondii antikorlarinin Sabin–Feldman boya testi ile saptanmasi. Acta Parasitol Turc. 1998;22:174–6. [Google Scholar]
- 547.Dubey JP, Thulliez P, Romand S, Kwok OCH, Shen SK, Gamble HR. Serologic prevalence of Toxoplasma gondii in horses slaughtered for food in North America. Vet Parasitol. 1999;86:235–8. doi: 10.1016/s0304-4017(99)00148-x. [DOI] [PubMed] [Google Scholar]
- 548.Alcaíno H, Herrera M, Gorman T. Helmintiasis e infeccion por Toxoplasma gondii en conejos silvestres (Oryctolagus cuniculus) de la zone precordillerana del Rio Renaico, Chile. Parasitol Día. 1990;14:86–90. [Google Scholar]
- 549.Hejlíček K, Literák I. Prevalence of toxoplasmosis in rabbits in South Bohemia. Acta Vet Brno. 1994;63:145–50. [Google Scholar]
- 550.Hilali M, Nassar AM, Ramada EI. Detection of encephalitozoonosis and toxoplasmosis among rabbits by carbon immunoassay. Vet Med J Giza. 1991;39:129–35. [Google Scholar]
- 551.Chalupský J, Vávra J, Gaudin JC, et al. Mise en évidence sérologique de la présence d’encephalitozoonose et de toxoplasmose chez le lapin de Garenne (Oryctolagus cuniculus) en France. Bull Soc Franç Parasitol. 1990;8:91–95. [Google Scholar]
- 552.Gury Dohmen FE. en perros y gatos de Buenos Aires. Rev Med Vet (B Aires) 1995;76:65–8. [Google Scholar]
- 553.Guimarães AM, Ribeiro MFB, Lima JD, Cury MC, Spiewak G. Freqüência de anticorpos anti-Toxoplasma gondii em caës de Belo Horizonte, Minas Gerais. Arq Bras Med Vet Zootec. 1992;44:67–8. [Google Scholar]
- 554.Cabral DD, Silva DAO, Mineo JR, Ferreira FA, Duran FP. Frequency of anti-Toxoplasma gondii antibodies in apparently healthy dogs of the city of Uberlandia-MG. Rev Bras Parasitol Vet. 1998;7:87–90. [Google Scholar]
- 555.Domingues LM, Machado RZ, Costa MT, Carvalho CS, Costa AJ, Malheiros EB. Canine toxoplasmosis: a comparative evaluation of the detection of anti-Toxoplasma gondii antibodies by the indirect immunoenzymatic assay (ELISA) and the indirect immunofluorescence reaction (IIF) Rev Bras Parasitol Vet. 1998;7:79–85. [Google Scholar]
- 556.Cabral DD, de Silva DA, Miranda EO, et al. Deteccao de anticorpos anti-Leishmania (Viannia) braziliensis e L. donovani, anti-Trypanosoma cruzi e anti-Toxoplasma gondii em caës da area rural do municipio de Uberlandia, MG, Brasil. Vet Noticias. 1998;4:15–9. [Google Scholar]
- 557.Garcia JL, Navarro IT, Ogawa L, de Oliveira RC. Soroepidemiologia da toxoplasmose em gatos e case de propriedades rurais do municipio de Jaguapita, Estado do Paraná, Brasil. Ciênc Rural (Santa Maria) 1999;29:99–104. [Google Scholar]
- 558.Gorman T, Garcia M, Lorca M. Infeccion por Toxoplasma gondii y Trichinella spiralis en perros de la comuna de San Bernardo, Santiago. Parasitol Día. 1991;15:49–51. [Google Scholar]
- 559.Pan H, Ma YH, Mo ZS, Taug XD, Sun Y. Investigation of serum antibodies against Toxoplasma gondii and Trichinella spriralis in service dogs in Southern China. Chin J Vet Sci Technol. 1997;27:16–7. [Google Scholar]
- 560.Hejlíček K, Literák I, Lhoták M. Prevalence of antibodies to Toxoplasma gondii in army dogs in the Czech Republic and Slovak Republic. Vet Med - Czech. 1995;40:137–40. [PubMed] [Google Scholar]
- 561.Cabannes A, Lucchese F, Pelse H, et al. La prévalence de la toxoplasmose chez les animaux familiers dans le sud-ouest da la France. Méd Malad Inf. 1998;28:647–51. [Google Scholar]
- 562.Shad-Del F, Sarvestani RG, Milani MS. Sero-prevalence of Toxoplasma infection in human and dog population in Shiraz. Iran J Appl Anim Res. 1993;3:83–9. [Google Scholar]
- 563.Baneth G, Shkap V, Savitsky I, Pipano E. The prevalence of antibodies to Toxoplasma gondii in dogs in Israel. Isr J Vet Med. 1996;51:31–3. [Google Scholar]
- 564.Bartoli M, Nacca A, Licciardi V, Veneziano V, Cringoli G. Anticorpi verso Toxoplasma gondii in cani e gatti della provincia di Benevento. Acta Med Vet. 1996;42:191–6. [Google Scholar]
- 565.Shaikh AA, Kondo K, Ahmed SS, Sano M. Sero-diagnostic investigations on human and dog sera for parasitic infections. Proc Parasitol. 1992;13:34–40. [Google Scholar]
- 566.Di Lorenzo C, Venturini C, Castellano C, Venturini L, Unzaga JM, Bacigalupe D. Detección de anticuerpos anti-Neospora caninum y anti-Toxoplasma gondii en perros de área urbana. Rev Med Vet (Buenos Aires) 1997;78:325–6. [Google Scholar]
- 567.Björkman C, Lundén A, Uggla A. Prevalence of antibodies to Neospora caninum and Toxoplasma gondii in Swedish dogs. Acta Vet Scand. 1994;35:445–7. doi: 10.1186/BF03548321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 568.Fan CK, Tsai YJ, Chung WC, Chang JS, Chao PH. Seroepidemiology of Toxoplasma gondii infection among dogs in Taipei. Taiwan Kaohsiung J Med Sci. 1998;14:387–91. [PubMed] [Google Scholar]
- 569.Lin DS. Seroprevalence to Toxoplasma gondii in privately-owned dogs in Taiwan. Prev Vet Med. 1998;35:21–7. doi: 10.1016/s0167-5877(97)00090-1. [DOI] [PubMed] [Google Scholar]
- 570.Fan CK, Su KE, Chung WC, Tsai YJ, Lu JL, Chao PH. Seroprevalence of Toxoplasma gondii infection among domestic dogs in aboriginal districts of Eastern Taiwan. J Chin Soc Vet Sci. 1998;24:283–7. [Google Scholar]
- 571.Fan CK, Su KE, Chung WC, et al. Seroprevalence of Toxoplasma gondii antibodies among Atayal aboriginal people and their hunting dogs in northeastern Taiwan. Jpn J Med Sci Biol. 1998;51:35–42. doi: 10.7883/yoken1952.51.35. [DOI] [PubMed] [Google Scholar]
- 572.Çakmak A, Karaer Z, Biyikoglu G, Babür C, Piskin FC. Ankara’da sokak köpeklerinde toxoplasmosisin seroprevalansi. Sađlik Bilimleri Derg. 1996;10:279–82. [Google Scholar]
- 573.Ýnci A, Babür C, Kalinbacak A. Gemlik askeri harasi köpeklerinde anti-Toxoplasma gondii antikorlarinin Sabin–Feldman boya testi ile araştirilmasi. Turk Parazitol Derg. 1996;20:413–6. [Google Scholar]
- 574.Babür C, Biyikoglu G, Piskin FC, Erdal N. Istanbul sokak köpeklerinde toksoplazmosis’in seroprevalani. Acta Parasitol Turc. 1997;21:413–6. [Google Scholar]
- 575.Atkas M, Babür C, Karaer Z, Dumanli N, Körođlu E. Elaziđ’da sokak köpeklerinde toxoplasmosisin seroprevalansi. Vet Bilimleri Derg. 1998;14:47–50. [Google Scholar]
- 576.Lindsay DS, Dubey JP, Upton SJ, Ridley RK. Serological prevalence of Neospora caninum and Toxoplasma gondii in dogs from Kansas. J Helminthol Soc Wash. 1990;57:86–8. [Google Scholar]
- 577.Edelhofer R, Prosl H, Kutzer E. Zur Trichinellose und Toxoplasmose der Wildschweine in Ostösterreich. Wien Tierärztl Monatsschr. 1996;83:225–9. [Google Scholar]
- 578.Lutz W. Serologischer Nachweis von Antikörpern gegen Toxoplasma gondii und Leptospira bei Schwarzwild. Z Jagdwiss. 1997;43:283–7. [Google Scholar]
- 579.Tackmann K. Seroprevalence of antibodies against Toxoplasma gondii in wild boars (Sus scrofa) In: Shirley M, editor. EUR 18476 – COST 820 Vaccines against animal coccidioses – annual report 1997. Luxemboug: Office for Official Publications of the European Communitites; 1999. p. 16. [Google Scholar]
- 580.Nogami S, Tabata A, Moritomo T, Hayashi Y. Prevalence of anti- Toxoplasma gondii antibody in wild boar, Sus scrofa riukiuanus, on Iriomote Island, Japan. Vet Res Commun. 1999;23:211–4. doi: 10.1023/a:1006292824574. [DOI] [PubMed] [Google Scholar]
- 581.Didderich V, New JC, Noblet GP, Patton S. Serologic survey of Toxoplasma gondii antibodies in free-ranging wild hogs (Sus scrofa) from the Great Smoky Mountains National Park and from sites in South Carolina. J Eukaryot Microbiol. 1996;43:122S. doi: 10.1111/j.1550-7408.1996.tb05038.x. [DOI] [PubMed] [Google Scholar]
- 582.Ferreira RA, Mineo JR, Duarte JM, Silva DAO, Patarroyo JH. Toxoplasmosis in naturally infected deer from Brazil. J Wildl Dis. 1997;33:896–9. doi: 10.7589/0090-3558-33.4.896. [DOI] [PubMed] [Google Scholar]
- 583.Lindsay DS, Blagburn BL, Dubey JP, Mason WH. Prevalence and isolation of Toxoplasma gondii from white-tailed deer in Alabama. J Parasitol. 1991;77:62–4. [PubMed] [Google Scholar]
- 584.Chomel BB, Carniciu ML, Kasten RW, Castelli PM, Work TM, Jessup DA. Antibody prevalence of eight ruminant infectious diseases in California mule and black-tailed deer (Odocoileus hemionus) J Wildl Dis. 1994;30:51–9. doi: 10.7589/0090-3558-30.1.51. [DOI] [PubMed] [Google Scholar]
- 585.Brillhart DB, Fox LB, Dubey JP, Upton SJ. Seroprevalence of Toxoplasma gondii in wild mammals in Kansas. J Helminthol Soc Wash. 1994;61:117–21. [Google Scholar]
- 586.Vanek JA, Dubey JP, Thulliez P, Riggs MR, Stromberg BE. Prevalence of Toxoplasma gondii antibodies in hunter-killed white-tailed deer (Odocoileus virginianus) in four regions of Minnesota. J Parasitol. 1996;82:41–4. [PubMed] [Google Scholar]
- 587.Crist SC, Stewart RL, Rinehart JP, Needham GR. Surveillance for Toxoplasma gondii in the white-tailed deer (Odocoileus virginianus) in Ohio. Ohio J Sci. 1999;99:34–7. [Google Scholar]
- 588.Humphreys JG, Stewart RL, Dubey JP. Prevalence of Toxoplasma gondii antibodies in sera of hunter-killed white-tailed deer in Pennsylvania. Am J Vet Res. 1995;56:172–3. [PubMed] [Google Scholar]
- 589.Siepierski SJ, Tanner CE, Embil JA. Prevalence of antibody to Toxoplasma gondii in the moose (Alces alces americana Clinton) of Nova Scotia, Canada. J Parasitol. 1990;76:136–8. [PubMed] [Google Scholar]
- 590.Oksanen A, Åsbakk K, Nieminen M, Norberg H, Näreaho A. Antibodies against Toxoplasma gondii in Fennoscandian reindeer – association with the degree of domestication. Parasitol Int. 1997;46:255– 61. [Google Scholar]
- 591.Mohammed OB, Hussein HS. Antibody prevalence of toxoplasmosis in Arabian gazelles and oryx in Saudi Arabia. J Wildl Dis. 1994;30:560–2. doi: 10.7589/0090-3558-30.4.560. [DOI] [PubMed] [Google Scholar]
- 592.Chomel BB, Zarnke RL, Kasten RW, Kass PH, Mendes E. Serologic survey of Toxoplasma gondii in grizzly bears (Ursus arctos) and black bears (Ursus americanus), from Alaska, 1988 to 1991. J Wildl Dis. 1995;31:472–9. doi: 10.7589/0090-3558-31.4.472. [DOI] [PubMed] [Google Scholar]
- 593.Dunbar MR, Cunningham MW, Roof JC. Seroprevalence of selected disease agents from free-ranging black bears in Florida. J Wildl Dis. 1998;34:612–9. doi: 10.7589/0090-3558-34.3.612. [DOI] [PubMed] [Google Scholar]
- 594.Nutter FB, Levine JF, Stoskopf MK, Gamble HR, Dubey JP. Sero-prevalence of Toxoplasma gondii and Trichinella spiralis in North Carolina black bears (Ursus americanus) J Parasitol. 1998;84:1048– 50. [PubMed] [Google Scholar]
- 595.Briscoe N, Humphreys JG, Dubey JP. Prevalence of Toxoplasma gondii infections in Pennsylvania black bears. Ursus americanus. J Wildl Dis. 1993;29:599–601. doi: 10.7589/0090-3558-29.4.599. [DOI] [PubMed] [Google Scholar]
- 596.Dubey JP, Briscoe N, Gamble R, Zarlenga D, Humphreys JG, Thulliez P. Characterization of Toxoplasma and Trichinella isolates from muscles of black bears in Pennsylvania. Am J Vet Res. 1994;55:815–9. [PubMed] [Google Scholar]
- 597.Dubey JP, Humphreys JG, Thulliez P. Prevalence of viable Toxoplasma gondii tissue cysts and antibodies to T. gondii by various serologic tests in black bears (Ursus americanus) from Pennsylvania. J Parasitol. 1995;81:109–12. [PubMed] [Google Scholar]
- 598.Fernández F, Ouviña G, Clot E, Fernandes Guido R, Codoni C. Prevalence of Toxoplasma gondii antibodies in cats in the western part of Great Buenos Aires, Argentina, 1993. Vet Parasitol. 1995;59:75–9. doi: 10.1016/0304-4017(94)00732-r. [DOI] [PubMed] [Google Scholar]
- 599.Lucas SRR, Hagiwara MK, de Souza Loureiro V, Ikesaki JYH, Birgel EH. Toxoplasma gondii infection in Brazilian domestic outpatient cats. Rev Inst Med Trop Sao Paulo. 1999;41:221–4. doi: 10.1590/S0036-46651999000400003. [DOI] [PubMed] [Google Scholar]
- 600.Alcaíno H, Gorman T, Larenas I. Fauna endoparasitaria del gato domestico en una zona urbana marginal de la Region Metropolitana de Chile. Parasitol Día. 1992;16:139–42. [Google Scholar]
- 601.Unbehauen I. Thesis. Dr vet med; Hannover: 1991. Untersuchungen über das Vorkommen von Darmparasiten bei Katzen im Raum Lübeck. [Google Scholar]
- 602.Tenter AM, Vietmeyer C, Johnson AM, Janitschke K, Rommel M, Lehmacher W. ELISAs based on recombinant antigens for seroepidemiological studies on Toxoplasma gondii infections in cats. Parasitology. 1994;109:29–36. doi: 10.1017/s0031182000077738. [DOI] [PubMed] [Google Scholar]
- 603.Simon KGM. Thesis. Dr vet med; Hannover: 1995. Evaluierung diagnostischer Tests zur Untersuchung von Infektionen mit Toxoplasma gondii bei Katzen und Schafen. [Google Scholar]
- 604.Maruyama S, Hiraga S, Yokoyama E, et al. Seroprevalence of Bartonella henselae and Toxoplasma gondii infections among pet cats in Kanagawa and Saitama Prefectures. J Vet Med Sci. 1998;60:997– 1000. doi: 10.1292/jvms.60.997. [DOI] [PubMed] [Google Scholar]
- 605.Nogami S, Moritomo T, Kamata H, et al. Seroprevalence against Toxoplasma gondii in domiciled cats in Japan. J Vet Med Sci. 1998;60:1001–4. doi: 10.1292/jvms.60.1001. [DOI] [PubMed] [Google Scholar]
- 606.Galván-Ramírez M, Sánchez-Vargas G, Vielma Sandoval M, Soto-Mancilla JL. Presence of anti-Toxoplasma antibodies in humans and their cats in the urban zone of Guadalajara. Rev Soc Bras Med Trop. 1999;32:483–8. doi: 10.1590/s0037-86821999000500003. [DOI] [PubMed] [Google Scholar]
- 607.Chong LH, Singh M, Chua SB, Fong WE. Feline toxoplasmosis in Singapore. Singapore Vet J. 1993;17:79–87. [Google Scholar]
- 608.Lin DS, Lai SS, Bowman DD, Jacobson RH, Barr MC, Giovengo SL. Feline immunodeficiency virus, feline leukaemia virus, Toxoplasma gondii, and intestinal parasitic infections in Taiwanese cats. Br Vet J. 1990;146:468–75. doi: 10.1016/0007-1935(90)90037-4. [DOI] [PubMed] [Google Scholar]
- 609.Ýnci A, Budak C, Dincer S. Ankara’da kedilerde Sabin–Feldman boya testi ile anti-Toxoplasma gondii antikorlarinin araştirilmasi. Turk Parazitol Derg. 1996;20:407–11. [Google Scholar]
- 610.Rodgers SJ, Baldwin CA. A serologic survey of Oklahoma cats for antibodies to feline immunodeficiency virus, coronavirus, and Toxoplasma gondii and for antigen to feline leukemia virus. J Vet Diagn Invest. 1990;2:180–3. doi: 10.1177/104063879000200305. [DOI] [PubMed] [Google Scholar]
- 611.Milstein TC, Goldsmid JM. Parasites of feral cats from southern Tasmania and their potential significance. Aust Vet J. 1997;75:218–9. doi: 10.1111/j.1751-0813.1997.tb10072.x. [DOI] [PubMed] [Google Scholar]
- 612.Sumner B, Ackland ML. Toxoplasma gondii antibody in domestic cats in Melbourne. Aust Vet J. 1999;77:447–9. doi: 10.1111/j.1751-0813.1999.tb12089.x. [DOI] [PubMed] [Google Scholar]
- 613.Hecking-Veltman J, Tenter AM, Daugschies A. Studien zur Parasitenfauna bei streunenden Katzen im Raum Mönchengladbach. Prakt Tierarzt. 2000 (in press) [Google Scholar]
- 614.D’Amore E, Falcone E, Busani L, Tollis M. A serological survey of feline immunodeficiency virus and Toxoplasma gondii in stray cats. Vet Res Commun. 1997;21:355–9. doi: 10.1023/a:1005864321370. [DOI] [PubMed] [Google Scholar]
- 615.Win KS, Matsamura T, Kumagai S, Uga S, Konishi E. Prevalence of antibody to Toxoplasma gondii in Hyogo prefecture, Japan: comparison at a 10-year interval. Kobe J Med Sci. 1997;43:159–68. [PubMed] [Google Scholar]
- 616.Yamaguchi N, MacDonald DW, Passanisi WC, Harbour DA, Hopper CD. Parasite prevalence in free-ranging farm cats. Felis silvestris catus. Epidemiol Infect. 1996;116:217–23. doi: 10.1017/s0950268800052468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 617.Poyraz O, Ozcelik S, Gunes T, Saygi G. Presence of anti-Toxoplasma gondii antibodies in the sera of cats. Turk Parazitol Derg. 1995;19:191–4. [Google Scholar]
- 618.Venturini MC, Castellano MC, Bacigalupe D, et al. Coinfeccion con Toxoplasma gondii y virus de la inmunodeficiencia felina (FIV) Parasitol Día. 1997;21:81–4. [Google Scholar]
- 619.Svobodová V, Knotek Z, Svoboda M. Prevalence of IgG and IgM antibodies specific to Toxoplasma gondii in cats. Vet Parasitol. 1998;80:173–6. doi: 10.1016/s0304-4017(98)00201-5. [DOI] [PubMed] [Google Scholar]
- 620.Furuya H, Nogami S, Inoue I, Takahashi D, Mizusawa H, Tohyama K. Seroepidemiological survey on Toxoplasma gondii infection in kittens. Jpn J Parasitol. 1993;42:388–91. [Google Scholar]
- 621.Wasiatycz G. Ekstensywność zarazenia kotów Toxoplasma gondii w Poznaniu i jego okolicy w aspekcie niebezpieczenstwa inwazji tego pierwotniaka dla czlowieka. Wiad Parazytol. 1998;44:693–704. [Google Scholar]
- 622.Krt B. Detection of antibodies to Toxoplasma gondii in cats in Slovenia. Zb Vet Fak Univ Ljubljana. 1997;34:141–9. [Google Scholar]
- 623.Babür C, Aktas M, Dumanli N, Altas MG. Elaziđ yöresinde kedilerde Sabin–Feldman boya testi ile anti-Toxoplasma gondii antikorlarinin araştirilmasi. Vet Bilimleri Derg. 1998;14:55–8. [Google Scholar]
- 624.Eren H, Babür C, Özlem MB, Durukan A, Ulutaş B. Aydin ili kedi ve köpeklerinde anti-Toxoplasma gondii antikorlarinin Sabin–Feldman boya testi ile araştirilmasi (1): the prevalence of Toxoplasma gondii in dogs and cats in Aydin by the Sabin–Feldman dye test. Bornova Vet Kontr Araşt Enst Md Derg. 1998;23:23–8. [Google Scholar]
- 625.Jackson MH, Hutchison WM. Unwanted cats – physical condition, Toxoplasma infection and ectoparasites. Br Vet J. 1993;149:295–7. doi: 10.1016/S0007-1935(05)80175-7. [DOI] [PubMed] [Google Scholar]
- 626.Lappin MR, Marks A, Greene CE, et al. Serologic prevalence of selected infectious diseases in cats with uveitis. J Am Vet Med Assoc. 1992;210:1005–9. [PubMed] [Google Scholar]



