Abstract
Background:
Antibiotic overuse in respiratory illness is common and is associated with drug resistance and hospital-acquired infection. Biomarkers that can identify bacterial infections may reduce antibiotic prescription. We aimed to compare the usefulness of the biomarkers procalcitonin and C-reactive protein (CRP) in patients with pneumonia or exacerbations of asthma or COPD.
Methods:
Patients with a diagnosis of community-acquired pneumonia or exacerbation of asthma or COPD were recruited during the winter months of 2006 to 2008. Demographics, clinical data, and blood samples were collected. Procalcitonin and CRP concentrations were measured from available sera.
Results:
Sixty-two patients with pneumonia, 96 with asthma, and 161 with COPD were studied. Serum procalcitonin and CRP concentrations were strongly correlated (Spearman rank correlation coefficient [rs] = 0.56, P < .001). Patients with pneumonia had increased procalcitonin and CRP levels (median [interquartile range] 1.27 ng/mL [2.36], 191 mg/L [159]) compared with those with asthma (0.03 ng/mL [0.04], 9 mg/L [21]) and COPD (0.05 ng/mL [0.06], 16 mg/L [34]). The area under the receiver operating characteristic curve (95% CI) for distinguishing between patients with pneumonia (antibiotics required) and exacerbations of asthma (antibiotics not required), for procalcitonin and CRP was 0.93 (0.88-0.98) and 0.96 (0.93-1.00). A CRP value > 48 mg/L had a sensitivity of 91% (95% CI, 80%-97%) and specificity of 93% (95% CI, 86%-98%) for identifying patients with pneumonia.
Conclusions:
Procalcitonin and CRP levels can both independently distinguish pneumonia from exacerbations of asthma. CRP levels could be used to guide antibiotic therapy and reduce antibiotic overuse in hospitalized patients with acute respiratory illness.
Overuse of antibiotics is common and accelerates the development of drug resistance and hospital-acquired infections.1 The widespread use of antibiotics over recent years has driven the increase in many drug-resistant bacteria, including that of methicillin-resistant Staphylococcus aureus and penicillin-resistant Streptococcus pneumoniae.2 Reliance on empirical broad-spectrum antibiotics in hospitals has led to the emergence and proliferation of the ribotype 027 Clostridium difficile strain.3,4 Reducing antibiotic prescription rates can reverse this trend,5 so strategies that achieve reductions in antibiotic use in hospitalized patients are urgently required.
Community-acquired pneumonia and acute exacerbations of asthma and COPD represent a large proportion of health-care use6‐8 and antibiotic prescription, with around 50% of all antibiotics in primary care being prescribed for acute respiratory infections.9 Patients hospitalized with community-acquired pneumonia have a mortality rate of up to 15%,10 so rapid clinical assessment and treatment with empirical antibiotics is appropriate.8 Viral infection causes the vast majority of exacerbations of asthma and is also an important cause of COPD exacerbations.11,12 Although current treatment guidelines for asthma exacerbations do not recommend antimicrobials,13,14 they are often prescribed.15 Large systematic reviews of studies suggest that antibiotics are not useful in mild to moderate exacerbations of COPD,16‐18 although in severe exacerbations there are reductions in rates of mechanical ventilation, short-term mortality, and readmission rates,19 with which their use must be balanced against the risk of developing severe side effects such as C difficile infection.
Recent strategies to reduce antibiotic overuse have included the development of biomarker-directed treatment algorithms wherein antibiotics are given or withheld depending on the level of biomarkers measured in the blood. Procalcitonin-guided therapy has been effective in reducing antibiotic use by approximately 50% in hospitalized patients presenting with acute lower respiratory tract infection symptoms (including patients with community-acquired pneumonia, exacerbations of COPD, and exacerbations of asthma)20,21 and by up to 40% in a selected group of patients with exacerbation of COPD.22 In a study of procalcitonin-guided antibiotic therapy for hospitalized patients with community-acquired pneumonia, 15% of patients had antibiotics withheld on admission and overall antibiotic exposure was reduced in the order of 50%.23 In all of these randomized controlled studies there was no increase in adverse events among patients who had antibiotics withheld.
Measurement of C-reactive protein (CRP) is inexpensive and widely available. CRP levels are elevated in patients with community-acquired pneumonia compared with healthy control subjects.24 Persistently elevated levels following treatment are associated with complications and treatment failure,24‐28 whereas a decline in concentration is associated with recovery.29 A previous systematic review of trials examining the diagnostic accuracy of CRP in radiologically confirmed pneumonia failed to demonstrate sufficient sensitivity or specificity to be clinically useful; however, the reviewers acknowledged that the methodologic quality of the included studies was too weak to draw definitive conclusions.30 We hypothesized that the biomarkers CRP and procalcitonin have clinical usefulness in distinguishing between community-acquired pneumonia (for which antibiotic therapy is indicated) from exacerbations of asthma (for which antibiotic therapy is not indicated) in hospitalized patients. The cut-offs derived from the receiver operator characteristic curves were used to propose when antibiotic therapy should/should not be given and to determine the potential reduction in antibiotic therapy prescription in patients with exacerbation of asthma and COPD.
Materials and Methods
Patients and Study Design
This was a prospective observational diagnostic accuracy study in patients recruited during the winter months of 2006 to 2008 in two hospitals with acute medical admission units within the University Hospitals of Leicester NHS Trust, England. Patients were adults aged 18 to 93 years who were hospitalized with an International Classification of Diseases, Tenth Revision discharge code31 diagnosis of community-acquired pneumonia, or an exacerbation of asthma or COPD, who participated in a study of rapid near-patient and molecular diagnostic tests in acute respiratory illness. Patients with pneumonia were defined as those with clinical signs and symptoms suggestive of lower respiratory infection and consolidation on plain chest radiograph. Patients with an acute exacerbation of asthma or COPD were defined as those with an appropriate past medical history and acute respiratory symptoms without consolidation on chest radiograph or an alternative diagnosis. The study was approved by the Leicestershire, Northamptonshire, and Rutland Ethics Committee, and all patients gave informed written consent (05/Q2502/76).
Measurements
At entry into the study, demographic and clinical data were recorded. Data regarding antibiotic usage before and during the hospital admission, length of hospital stay, and clinical markers of severity using the modified Early Warning Score32 and the pneumonia assessment tool CURB-65 (confusion, urea > 7 mmol/L, respiratory rate > 30 breaths/min, BP systolic < 90 and diastolic < 60, age > 65 years)33 score as appropriate on admission were collected from case notes. All patients had a plain chest radiograph that was reviewed on admission by the admitting physician and subsequently reported by a consultant radiologist. All patients had venous blood collected at study entry, and qualitative detection of S pneumoniae urinary antigen using the Binax assay. Where available, sputum for microbial culture was processed to identify potential pathogenic microorganisms (S pneumoniae, Moraxella catarrhalis, Haemophilus influenzae, and S aureus) by routine techniques.34 Procalcitonin and CRP assays were performed by personnel who were blind to the diagnosis. Unblinding was performed after data lock.
Procalcitonin
Procalcitonin was measured in duplicate from 50 μL of serum using a time-resolved amplified cryptate emission technology assay (Kryptor TRACE PCT; Brahms AG; Cambridge, England). The lower limit of detection is 0.02 ng/mL and concentrations below this limit of detection were assigned as zero. The assay functional sensitivity was 0.06 ng/mL, and the intraassay coefficient at a sample concentration of 0.2 ng/mL was 10%. Threshold values of 0.1 and 0.25 ng/mL were used as these have been validated in previous trials to guide antibiotic therapy (procalcitonin < 0.1, bacterial infection very unlikely, antibiotic use strongly discouraged; procalcitonin < 0.25, bacterial infection unlikely, antibiotic use discouraged; procalcitonin > 0.25 bacterial infection likely, antibiotic use suggested).20‐23
C-Reactive Protein
CRP was measured from 25 μL of serum using an automated clinical analyzer (Abbott Architect ci8200; Abbott Laboratories; Abbott Park, Illinois), which has a lower limit of detection of 5 mg/L. The intraassay and interassay variability was < 10%. CRP was measured in all patients as part of routine clinical care.
Statistical Analysis
Statistical analyses were performed using PRISM, version 4 (GraphPad Software Inc; La Jolla, California) and SPSS, version 16 (SPSS, Inc; Chicago, Illinois). Parametric data were expressed as mean and SE of the mean, and nonparametric data were described as median and interquartile range. One-way analysis of variance and the Kruskal-Wallis test were used for across- and between-group comparisons for parametric and nonparametric data, respectively; post hoc analysis was performed using Tukey or Dunn comparison tests. Correlations were assessed by Pearson correlation coefficient (r) and Spearman rank correlation coefficient (rs) for parametric and nonparametric data. The Clopper-Pearson method was used to calculate CIs for proportions. To determine the diagnostic accuracy of the biomarkers, receiver operating characteristic curves and area under the curve with 95% CIs for patients with asthma exacerbation (antibiotics not required) vs pneumonia (definite antibiotics required) were plotted. The Youden index was used to identify the optimal cut-off point on the receiver operator characteristic curve with equal weighting of sensitivity and specificity35 and to determine the potential reduction in antibiotic therapy in hospitalized patients. A P value < .05 was taken as the threshold for statistical significance.
Results
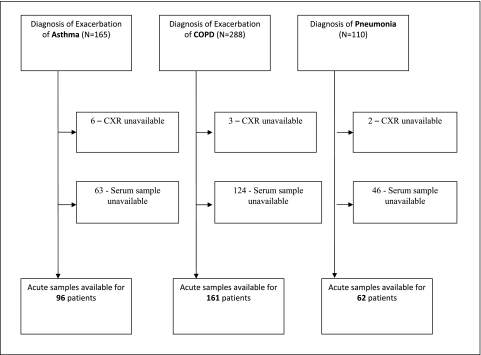
We studied 319 patients: 62 with pneumonia, 96 with acute exacerbation of asthma, and 161 with exacerbation of COPD (Fig 1, Table 1). Sputum culture for a potential pathogenic microorganism was detected in 29% and 44% of patients with pneumonia and COPD on admission. Urinary pneumococcal antigen was positive in 29% of patients with pneumonia.
Figure 1.
Trial profile for patients enrolled in the study. CXR = chest radiograph.
Table 1.
—Demographic and Clinical Data From Patients Admitted With Pneumonia, Exacerbation of Asthma, or Exacerbation of COPD
| Variable | Pneumonia | Asthma Exacerbation | COPD Exacerbation | P Value |
| No. | 62 | 96 | 161 | … |
| Male, % | 63 | 37 | 48 | .001 |
| Age,a y | 63 (24-93) | 41 (18-84) | 69 (39-93) | < .001 |
| Antibiotics given, % | 100 | 57 | 76 | < .001 |
| IV antibiotics given, % | 74 | 10 | 18 | < .001 |
| Antibiotics prior to admission, % | 25 | 35 | 35 | .34 |
| Streptococcus pneumoniae urinary antigen positive, % | 29 | 2 | 5 | < .001 |
| Length of stay,a d | 6 (1-40) | 3 (1-19) | 5 (1-31) | < .001 |
| Temperature,b °C | 37.1 (1.1) | 36.8 (0.9) | 36.6 (0.8) | < .001 |
| Respiratory rate,b | 22 (7) | 22 (7) | 23 (6) | .95 |
| Systolic BP, mm Hg | 120 (3) | 132 (2) | 134 (2) | < .001 |
| Pulse rate, beats/min | 98 (2) | 100 (2) | 95 (1) | .08 |
| Modified early warning scorea | 3 (0-7) | 3 (0-7) | 2 (0-8) | .06 |
| Blood leukocytes,b × 09 cells/L | 14.1 (7.5) | 10.8 (4.3) | 10.1 (4.9) | < .001 |
| Blood neutrophils,b × 109 cells/L | 12.4 (7.2) | 7.7 (4.4) | 7.5 (4.7) | < .001 |
| CRP,b mg/L | 191 (159) | 9 (21) | 16 (34) | < .001 |
| Procalcitonin,b ng/mL | 1.27 (2.36) | 0.03 (0.04) | 0.05 (0.06) | < .001 |
Data presented as mean (SE of mean), unless stated. CRP = C-reactive protein.
Mean (range).
Median (interquartile range).
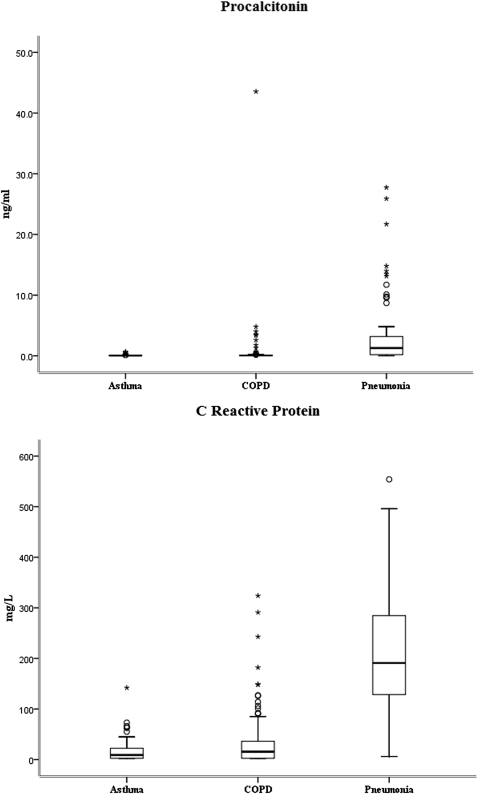
Patients with pneumonia had higher procalcitonin and CRP levels than those with COPD (P < .0001) or asthma (P < .0001) (Fig 2). The concentration of procalcitonin was below the limit of detection in 24%, 6%, and 2% of patients with asthma, COPD, and pneumonia, respectively. The median CURB-65 score was 1 (interquartile range 1). All of the patients with pneumonia received antibiotic therapy, whereas 57% and 76% of patients with asthma and COPD, respectively, received antibiotics while hospitalized.
Figure 2.
Box and whisker plots for patients admitted with exacerbation of asthma, COPD, and pneumonia for the biomarkers procalcitonin and C-reactive protein. The horizontal bar represents the median; the box length represents the interquartile range. Outliers are identified by ○ (1.5 × the interquartile range) and * (3 × the interquartile range).
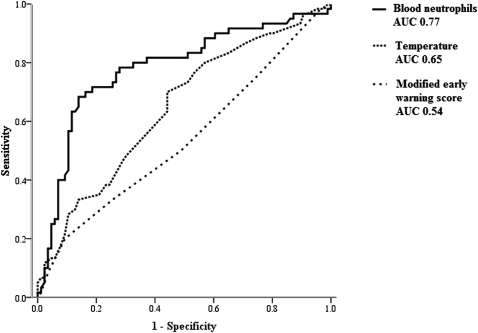
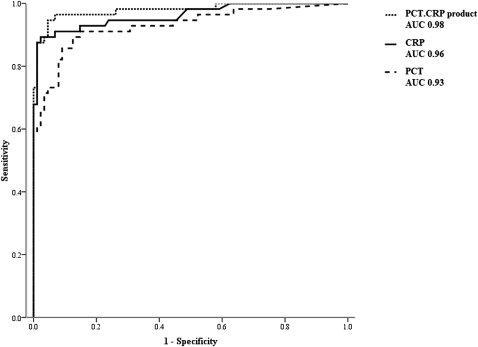
Procalcitonin and CRP levels were strongly correlated (rs = 0.56, P < .0001). The area under the receiver operator characteristic curve (95% CI) for the clinical parameters of peripheral neutrophil counts, temperature on admission, and modified early warning score32 for distinguishing between patients with pneumonia (antibiotics required) and exacerbations of asthma (antibiotics not required) were 0.77 (0.69-0.85), 0.65 (0.56-0.74), and 0.54 (0.44-0.63), respectively (Fig 3). The area under the receiver operator characteristic curve (95% CI) for procalcitonin and CRP was 0.93 (0.88-0.98) and 0.96 (0.93-1.00), whereas the product of procalcitonin and CRP (PCT × CRP) yielded a value of 0.98 (0.96-1.00) (Fig 4).
Figure 3.
Receiver operator characteristic curve distinguishing between patients with pneumonia (antibiotics required) and exacerbations of asthma (antibiotics not required) for peripheral neutrophils, temperature, and modified early warning score. AUC = area under the receiver operator characteristic curve.
Figure 4.
Receiver operator characteristic curve for distinguishing between patients with pneumonia (antibiotics required) and exacerbations of asthma (antibiotics not required) for PCT.CRP, PCT, and CRP. CRP = C-reactive protein; PCT = procalcitonin; PCT.CRP = procalcitonin C-reactive protein product. See Figure 3 for expansion of the other abbrevation.
Using the receiver operator characteristic curve to identify the optimum CRP threshold value, a level of > 48 mg/L had a sensitivity of 91% (95% CI, 80%-97%) and specificity of 93% (95% CI, 86%-98%) for identifying patients with pneumonia. The optimal threshold value calculated for procalcitonin was 0.08 ng/mL, of which a level greater than this had a sensitivity of 89% (95% CI, 78%-95%) and specificity of 78% (95% CI, 72%-82%) for identifying patients with pneumonia.
Thirty-three percent of all patients received antibiotics prior to admission. The area under the receiver operator characteristic curve (95% CI) was not different between the patients who did or did not receive prior antibiotics for CRP (0.96 [0.92-1.00] vs 0.94 [0.89-0.99] or procalcitonin (0.96 [0.89-1.00] vs 0.92 [0.83-1.00]).
The proportion of patients who would have received antibiotics if biomarker-directed therapy was used, using the threshold values for procalcitonin of 0.1 and 0.25 ng/mL and for CRP of 10, 30, and 48 mg/L, is shown in Table 2. Using a procalcitonin threshold value of > 0.25 ng/mL to guide antibiotic therapy, antibiotic use would be reduced from 57% to 4% in patients with exacerbation of asthma (ie, a reduction in antibiotic usage of 93%; 95% CI, 88%-98%), from 76% to 7% in patients with exacerbation of COPD (ie, a reduction of 91%; 95% CI, 87%-95%) and from 100% to 73% in those with pneumonia (ie, a reduction of 27%; 95% CI 17%-40%). Using a CRP threshold value of > 48 mg/L to guide antibiotic therapy, antibiotic use would be reduced from 57% to 7% (ie, a reduction of 88%; 95% CI, 76%-95%) in patients with asthma, from 76% to 18% (ie, a reduction of 76%; 95% CI, 65%-85%) in patients with exacerbation of COPD, and from 100% to 91% (ie, a reduction of 9%; 95% CI, 2%-18%) in patients with pneumonia.
Table 2.
—Proportion of Patients Receiving Antibiotic Therapy on Admission and Proportion Who Would Have Received Antibiotic Therapy if Biomarker-Directed Therapy Were Used With the Relevant Threshold Values for PCT and CRP
| Proportions Who Would Have Been Treated if Biomarker-Directed Therapy Were Used |
||||||
| PCT, ng/mL |
CRP, mg/L |
|||||
| Diagnosis | Proportions Actually Treated | 0.1 Threshold Value | 0.25 Threshold Value | 10 Threshold Value | 30 Threshold Value | 48 Threshold Value |
| Asthma, % | 57 | 9 | 4 | 43 | 15 | 7 |
| (95% CI) | (46-67) | (4-16) | (1-11) | (33-54) | (9-24) | (2-14) |
| COPD, % | 76 | 24 | 7 | 59 | 32 | 21 |
| (95% CI) | (68-82) | (17-31) | (4-13) | (51-67) | (25-40) | (15-28) |
| Pneumonia,% | 100 | 82 | 73 | 95 | 91 | 91 |
| (95% CI) | (96-100) | (70-91) | (60-83) | (85-99) | (80-97) | (80-97) |
PCT = procalcitonin. See Table 1 for expansion of other abbreviation.
Discussion
We have shown that the biomarkers procalcitonin and CRP are correlated and elevated in patients with pneumonia compared with patients with exacerbations of asthma and COPD, suggesting that they can usefully guide antibiotic usage. We have shown that both procalcitonin and CRP are more reliable in distinguishing between acute respiratory illnesses than the peripheral neutrophil count and clinical severity score. In this large study of common respiratory disease presentations we observed a high antibiotic prescription rate in patients with asthma contrary to recommendations and a high level of antibiotic use in exacerbations of COPD.13,14
Our findings support the view that biomarker-directed antibiotic therapy would lead to a marked reduction in antibiotic use in patients with exacerbations of asthma and COPD. There is a clinical need to reduce unnecessary antibiotic use in both primary and secondary care. Biomarker-directed therapy aims to reduce bacterial drug resistance and the high morbidity and mortality associated with hospital-acquired infections.1,2 Clinical trials that have used procalcitonin to guide antibiotic therapy for patients with symptoms suggestive of a lower respiratory tract infection, including patients with COPD, have shown that a biomarker-driven algorithm can cut antibiotic prescribing significantly and that this can be achieved without any increase in adverse events or treatment failures.20‐22
Our study also highlights the usefulness of CRP and procalcitonin in differentiating pneumonia from COPD and asthma. Although a recent study of the usefulness of biomarkers in predicting bacteremia in patients with community-acquired pneumonia suggested a superior efficacy of procalcitonin compared with CRP,36 it has been shown that CRP compared with procalcitonin is a better predictor of treatment responses in exacerbations of COPD.19 Furthermore, our findings concur with those of other recent studies showing that CRP can distinguish patients with pneumonia from exacerbation of COPD and heart failure.37,38
Our observations suggest that CRP could be used to guide antibiotic prescription in patients hospitalized with acute lower respiratory tract symptoms, which is similar to findings observed in a large cohort of patients with lower respiratory tract symptoms in primary care39 and interestingly has similar accuracy to studies looking at infected and noninfected patients.40,41 The threshold levels generated in our study to guide antibiotic therapy could lead to safe reductions in antibiotic usage among patients hospitalized with exacerbations of airways disease. Using the threshold level for CRP of > 48 mg/L to guide antibiotic therapy in acute respiratory illness, a small proportion of patients with pneumonia would not have been treated. However, withholding antibiotics from those patients with low levels of biomarkers was not associated with adverse outcomes.23
One possible limitation of this study is the use of the International Classification of Diseases, Tenth Revision classification of disease coding31 to define diagnosis and enrollment. Although coding can be inaccurate, we used additional clinical and radiographic evidence to improve diagnostic accuracy and confidence that our clinical groups represent those encountered in clinical practice. A further limitation is the lack of etiologic data to distinguish patients with a viral or bacterial cause for the lower respiratory tract illness. However, it is known that bacteria are detected in less than one-half of pneumonias,42 whereas isolation of viruses does not exclude bacterial coinfection and the need for antibiotics. By applying a clinical diagnosis to our cohort and using blinded comparisons, we evaluated procalcitonin and CRP under realistic clinical practice conditions. Our study was cross-sectional in nature so we cannot discount the possibility of subsequent clinical deterioration and delayed onset of pneumonia during admission, although it is notable that this phenomenon was not observed in the procalcitonin studies.20‐22 Furthermore, approximately 30% of our patients received antibiotics prior to admission that could potentially affect the levels of biomarkers measured. Interestingly, we found that this did not affect the usefulness of CRP, and marginally affected levels of procalcitonin, although preadmission antibiotic therapy has been shown not to affect the effectiveness or safety of biomarker-directed therapy.20‐23
In conclusion, there is an urgent need to reduce antibiotic prescription in patients hospitalized with acute respiratory illness. Our study demonstrates that CRP has at least equal accuracy for the detection of pneumonia and could be used in a similar way to procalcitonin to guide antibiotic therapy in hospitalized patients with lower respiratory tract infection, although this would require further evaluation in large prospective interventional randomized control studies.
Acknowledgments
Author contributions: All authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Dr Bafadhel: contributed to the data analysis, design of the study, and the writing of all sections of the manuscript, and approved the final version of the manuscript.
Dr Clark: contributed to collecting data, design of the study, data analysis, and the writing of all sections of the manuscript, and approved the final version of the manuscript.
Ms Reid: contributed to performing analysis of patient samples and approved the final version of the manuscript.
Ms Medina: contributed to collecting data, analysis of patient samples, and design of the study, and approved the final version of the manuscript.
Ms Batham: contributed to collecting data and design of the study, and approved the final version of the manuscript.
Dr Barer: contributed to design of the study and the writing of the manuscript, and approved the final version of the manuscript.
Dr Nicholson: contributed to data collection, study design, data analysis, and the writing of the manuscript, and approved the final version of the manuscript.
Dr Brightling: contributed to the study design, data analysis, and writing of the manuscript, and approved the final version of the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: Dr Brightling has received consultancy fees from Medimmune, Astrazeneca, GlaxoSmithKline, and Roche, and research grants from Astrazeneca, Medimmune, and GlaxoSmithKline. Dr Nicholson has received gifted vaccines from Novartis, GlaxoSmithKline, and Baxter; received consultancy fees from Merck, Novartis, GlaxoSmithKline and Sanofi Pasteur; and spoken at meetings sponsored by Berna Biotech, Esteves, Novartis and Roche. Ms Reid is employed by Brahms, England. Drs Bafadhel, Clark, and Barer, and Mss Medina and Batham, have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article. The views and opinions expressed in this article are those of the authors and do not necessarily reflect those of the Health Technology Assessment programme (HTA), National Institute for Health Research (NIHR), National Health Service (NHS), or the Department of Health (DoH).
Other contributions: Brahms AG, England, supplied the Kryptor TRACE bioanalyser on an unconditional loan for purpose of measuring procalcitonin. All study design, analysis and manuscript preparation was carried out independently of Brahms AG, England. We thank all the clinical staff of UHL involved in the care of the patients in this study.
Abbreviations
- CRP
C-reactive protein
Footnotes
Drs Bafadhel and Clark contributed equally to this article.
Funding/Support: This study was funded by a Health Technology Assessment grant [03/39/18] (Dr Nicholson) and Wellcome Senior Clinical Fellowship [03/91/68] (Dr Brightling).
References
- 1.Bauer MP, van Dissel JT, Kuijper EJ. Clostridium difficile: controversies and approaches to management. Curr Opin Infect Dis. 2009;22(6):517–524. doi: 10.1097/QCO.0b013e32833229ce. [DOI] [PubMed] [Google Scholar]
- 2.Hawkey PM, Jones AM. The changing epidemiology of resistance. J Antimicrob Chemother. 2009;64(suppl 1):i3–i10. doi: 10.1093/jac/dkp256. [DOI] [PubMed] [Google Scholar]
- 3.Dubberke ER, Wertheimer AI. Review of current literature on the economic burden of Clostridium difficile infection. Infect Control Hosp Epidemiol. 2009;30(1):57–66. doi: 10.1086/592981. [DOI] [PubMed] [Google Scholar]
- 4.Steinman MA, Gonzales R, Linder JA, Landefeld CS. Changing use of antibiotics in community-based outpatient practice, 1991-1999. Ann Intern Med. 2003;138(7):525–533. doi: 10.7326/0003-4819-138-7-200304010-00008. [DOI] [PubMed] [Google Scholar]
- 5.Frank MO, Batteiger BE, Sorensen SJ, et al. Decrease in expenditures and selected nosocomial infections following implementation of an antimicrobial-prescribing improvement program. Clin Perform Qual Health Care. 1997;5(4):180–188. [PubMed] [Google Scholar]
- 6.Braman SS. The global burden of asthma. Chest. 2006;130(1) suppl:4S–12S. doi: 10.1378/chest.130.1_suppl.4S. [DOI] [PubMed] [Google Scholar]
- 7.Rabe KF, Hurd S, Anzueto A, et al. Global Initiative for Chronic Obstructive Lung Disease Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176(6):532–555. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 8.Lim WS, Baudouin SV, George RC, et al. Pneumonia Guidelines Committee of the BTS Standards of Care Committee BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64(suppl 3):iii1–iii55. doi: 10.1136/thx.2009.121434. [DOI] [PubMed] [Google Scholar]
- 9.Roumie CL, Halasa NB, Grijalva CG, et al. Trends in antibiotic prescribing for adults in the United States—1995 to 2002. J Gen Intern Med. 2005;20(8):697–702. doi: 10.1111/j.1525-1497.2005.0148.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim WS, Macfarlane JT, Boswell TC, et al. Study of community acquired pneumonia aetiology (SCAPA) in adults admitted to hospital: implications for management guidelines. Thorax. 2001;56(4):296–301. doi: 10.1136/thorax.56.4.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sykes A, Johnston SL. Etiology of asthma exacerbations. J Allergy Clin Immunol. 2008;122(4):685–688. doi: 10.1016/j.jaci.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 12.Papi A, Bellettato CM, Braccioni F, et al. Infections and airway inflammation in chronic obstructive pulmonary disease severe exacerbations. Am J Respir Crit Care Med. 2006;173(10):1114–1121. doi: 10.1164/rccm.200506-859OC. [DOI] [PubMed] [Google Scholar]
- 13.British Thoracic Society Scottish Intercollegiate Guidelines Network British Guideline on the Management of Asthma. Thorax. 2008;63(suppl 4):iv1–iv121. doi: 10.1136/thx.2008.097741. [DOI] [PubMed] [Google Scholar]
- 14.Graham VA, Milton AF, Knowles GK, Davies RJ. Routine antibiotics in hospital management of acute asthma. Lancet. 1982;1(8269):418–420. doi: 10.1016/s0140-6736(82)91619-1. [DOI] [PubMed] [Google Scholar]
- 15.Glauber JH, Fuhlbrigge AL, Finkelstein JA, Homer CJ, Weiss ST. Relationship between asthma medication and antibiotic use. Chest. 2001;120(5):1485–1492. doi: 10.1378/chest.120.5.1485. [DOI] [PubMed] [Google Scholar]
- 16.Sethi S. Bacteria in exacerbations of chronic obstructive pulmonary disease: phenomenon or epiphenomenon? Proc Am Thorac Soc. 2004;1(2):109–114. doi: 10.1513/pats.2306029. [DOI] [PubMed] [Google Scholar]
- 17.Puhan MA, Vollenweider D, Latshang T, Steurer J, Steurer-Stey C. Exacerbations of chronic obstructive pulmonary disease: when are antibiotics indicated? A systematic review. Respir Res. 2007;8:30–41. doi: 10.1186/1465-9921-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ram FS, Rodriguez-Roisin R, Granados-Navarrete A, Garcia-Aymerich J, Barnes NC. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2006;(2):CD004403. doi: 10.1002/14651858.CD004403.pub2. [DOI] [PubMed] [Google Scholar]
- 19.Rothberg MB, Pekow PS, Lahti M, Brody O, Skiest DJ, Lindenauer PK. Antibiotic therapy and treatment failure in patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. JAMA. 2010;303(20):2035–2042. doi: 10.1001/jama.2010.672. [DOI] [PubMed] [Google Scholar]
- 20.Christ-Crain M, Jaccard-Stolz D, Bingisser R, et al. Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blinded intervention trial. Lancet. 2004;363(9409):600–607. doi: 10.1016/S0140-6736(04)15591-8. [DOI] [PubMed] [Google Scholar]
- 21.Schuetz P, Christ-Crain M, Thomann R, et al. ProHOSP Study Group Effect of procalcitonin-based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections: the ProHOSP randomized controlled trial. JAMA. 2009;302(10):1059–1066. doi: 10.1001/jama.2009.1297. [DOI] [PubMed] [Google Scholar]
- 22.Stolz D, Christ-Crain M, Bingisser R, et al. Antibiotic treatment of exacerbations of COPD: a randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest. 2007;131(1):9–19. doi: 10.1378/chest.06-1500. [DOI] [PubMed] [Google Scholar]
- 23.Christ-Crain M, Stolz D, Bingisser R, et al. Procalcitonin guidance of antibiotic therapy in community-acquired pneumonia: a randomized trial. Am J Respir Crit Care Med. 2006;174(1):84–93. doi: 10.1164/rccm.200512-1922OC. [DOI] [PubMed] [Google Scholar]
- 24.Almirall J, Bolíbar I, Toran P, et al. Community-Acquired Pneumonia Maresme Study Group Contribution of C-reactive protein to the diagnosis and assessment of severity of community-acquired pneumonia. Chest. 2004;125(4):1335–1342. doi: 10.1378/chest.125.4.1335. [DOI] [PubMed] [Google Scholar]
- 25.Menéndez R, Martinez R, Reyes S, et al. Stability in community-acquired pneumonia: one step forward with markers? Thorax. 2009;64(11):987–992. doi: 10.1136/thx.2009.118612. [DOI] [PubMed] [Google Scholar]
- 26.Menéndez R, Martínez R, Reyes S, et al. Biomarkers improve mortality prediction by prognostic scales in community-acquired pneumonia. Thorax. 2009;64(7):587–591. doi: 10.1136/thx.2008.105312. [DOI] [PubMed] [Google Scholar]
- 27.Smith RP, Lipworth BJ, Cree IA, Spiers EM, Winter JH. C-reactive protein. A clinical marker in community-acquired pneumonia. Chest. 1995;108(5):1288–1291. doi: 10.1378/chest.108.5.1288. [DOI] [PubMed] [Google Scholar]
- 28.Coelho L, Póvoa P, Almeida E, et al. Usefulness of C-reactive protein in monitoring the severe community-acquired pneumonia clinical course. Crit Care. 2007;11(4):R92–R100. doi: 10.1186/cc6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hansson LO, Hedlund JU, Ortqvist AB. Sequential changes of inflammatory and nutritional markers in patients with community-acquired pneumonia. Scand J Clin Lab Invest. 1997;57(2):111–118. doi: 10.1080/00365519709056378. [DOI] [PubMed] [Google Scholar]
- 30.van der Meer V, Neven AK, van den Broek PJ, Assendelft WJ. Diagnostic value of C reactive protein in infections of the lower respiratory tract: systematic review. BMJ. 2005;331(7507):26–31. doi: 10.1136/bmj.38483.478183.EB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brämer GR. International statistical classification of diseases and related health problems. Tenth revision. World Health Stat Q. 1988;41(1):32–36. [PubMed] [Google Scholar]
- 32.Subbe CP, Kruger M, Rutherford P, Gemmel L. Validation of a modified Early Warning Score in medical admissions. QJM. 2001;94(10):521–526. doi: 10.1093/qjmed/94.10.521. [DOI] [PubMed] [Google Scholar]
- 33.Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58(5):377–382. doi: 10.1136/thorax.58.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Health Protection Agency . London, England: Department for Evaluations, Standards and Training, Health Protection Agency; 2009. Investigation of Bronchoalveolar Lavage, Sputum and Associated Specimens. National Standard Method BSOP 57. Issue 2.3. [Google Scholar]
- 35.Akobeng AK. Understanding diagnostic tests 3: Receiver operating characteristic curves. Acta Paediatr. 2007;96(5):644–647. doi: 10.1111/j.1651-2227.2006.00178.x. [DOI] [PubMed] [Google Scholar]
- 36.Müller F, Christ-Crain M, Bregenzer T, Krause M, Zimmerli W, Mueller B, et al. Procalcitonin levels predict bacteremia in patients with community-acquired pneumonia: a prospective cohort trial. Chest. 2010;138(1):121–129. doi: 10.1378/chest.09-2920. [DOI] [PubMed] [Google Scholar]
- 37.Joffe E, Justo D, Mashav N, et al. C-reactive protein to distinguish pneumonia from acute decompensated heart failure. Clin Biochem. 2009;42(16-17):1628–1634. doi: 10.1016/j.clinbiochem.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 38.Justo D, Lachmi S, Saar N, et al. C-reactive protein velocity following antibiotics in patients with chronic obstructive pulmonary disease exacerbation and community acquired pneumonia. Eur J Intern Med. 2009;20(5):518–521. doi: 10.1016/j.ejim.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 39.Cals JW, Butler CC, Hopstaken RM, Hood K, Dinant GJ. Effect of point of care testing for C reactive protein and training in communication skills on antibiotic use in lower respiratory tract infections: cluster randomised trial. BMJ. 2009;338:1112–1116. doi: 10.1136/bmj.b1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Póvoa P, Coelho L, Almeida E, et al. C-reactive protein as a marker of infection in critically ill patients. Clin Microbiol Infect. 2005;11(2):101–108. doi: 10.1111/j.1469-0691.2004.01044.x. [DOI] [PubMed] [Google Scholar]
- 41.Chan YL, Tseng CP, Tsay PK, Chang SS, Chiu TF, Chen JC. Procalcitonin as a marker of bacterial infection in the emergency department: an observational study. Crit Care. 2004;8(1):R12–R20. doi: 10.1186/cc2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Holm A, Nexoe J, Bistrup LA, et al. Aetiology and prediction of pneumonia in lower respiratory tract infection in primary care. Br J Gen Pract. 2007;57(540):547–554. [PMC free article] [PubMed] [Google Scholar]