Abstract
Non-islet cell tumour hypoglycaemia is a rare paraneoplastic phenomenon where there is spontaneous hypoglycaemia due to secretion of insulin-like growth factor-2 (IGF-2) from large mesenchymal or epithelial tumours. A 67-year-old man presented to the accident and emergency department with a 6-week history of confusion and collapse. Investigations confirmed that he was having recurrent hypoglycaemic attacks. He had been diagnosed with a pelvic solitary fibrous tumour 1 year previously. Further tests demonstrated a high circulating level of IGF-2, which was being secreted by the tumour, confirming a diagnosis of non-islet cell tumour hypoglycaemia. The episodes of hypoglycaemia have resolved following treatment with glucocorticoids. He is currently awaiting radiotherapy.
Background
Non-islet cell tumour hypoglycaemia (NICTH) is a rare with a few hundred case reports around the world. One-half of patients with such tumours present with hypoglycaemia before the tumour is diagnosed, but in the other half symptoms of hypoglycaemia present first and lead to the diagnosis of the tumours.1 2 Treatment is based mainly on individual anecdotal reports,2 3 rather than randomised control trials although there is on-going research regarding pathogenesis. There may be a degree of underdiagnosis of NICTH, especially in patients with disseminated malignancy.
Case presentation
A 67-year-old man presented with an episode of collapse and a history of recurrent confusion. There had been multiple episodes during the previous 6 weeks, when he had been disorientated and noted by friends to have slurred speech, usually first thing in the morning.
The year before he had been diagnosed with a benign pelvic solitary fibrous tumour, when he presented with right lower limb swelling and urinary retention. He had been referred to a tertiary centre for tumour embolisation, with a view to subsequently performing surgery, but the patient defaulted from follow-up and did not have surgery. His syncopal episodes started a few months after tumour embolisation.
There was no other medical history or significant family history and the patient was not on any medication. There was no history of drug or alcohol abuse. Abdominal examination demonstrated a large, hard, non-tender mass, arising out of the pelvis. A warm, swollen and dusky-coloured left leg was also observed. Examination of other systems was unremarkable.
Investigations
Laboratory blood glucose testing confirmed hypoglycaemia, with day and night values dropping below 2.0 mmol/l. During spontaneous hypoglycaemia blood was taken to measure levels of insulin, C-peptide, pro-insulin and insulin-like growth factors 1 and 2 (IGF-1, IGF-2).Results were:
-
▶
Insulin – < 22 pmol/l (0–60)
-
▶
Pro-insulin – 1.3 pmol/l (0–7)
-
▶
C-peptide – 35 pmol/l (174 – 960)
-
▶
IGF-1 – 10.2 nmol/l (5–22.5)
-
▶
IGF-2 – 177.4 nmol/l
-
▶
Ratio of IGF-2/IGF-1 – 17.4 (normal <10).
These results demonstrate that insulin and C-peptide levels were appropriately suppressed. However, there is a high IGF-2/IGF-1 ratio, which is in keeping with excess IGF-2 secretion from the tumour.
CT abdomen confirmed a 15 × 18 × 22 cm pelvic mass with bilateral hydronephrosis worse on the right (figures 1 and 2). Ultrasound of his swollen leg revealed a large thrombus in the external iliac and common femoral veins. A filter was inserted into the inferior vena cava.
Figure 1.

CT scan of pelvis demonstrated a large pelvic tumour 18 × 22 cm with necrotic sections following embolisation.
Figure 2.
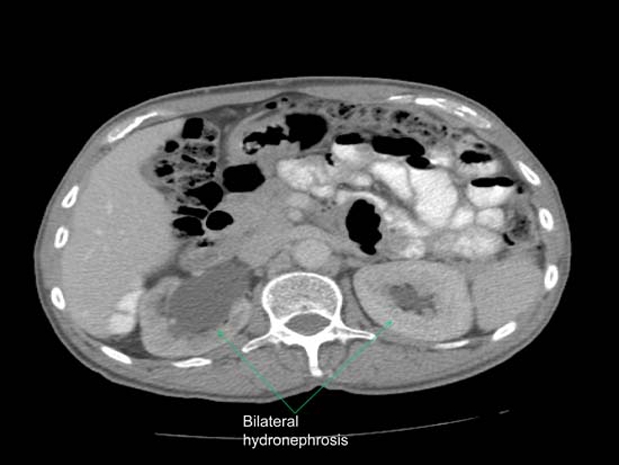
CT scan of abdomen showing bilateral hydronephrosis worse on the right side.
Differential diagnosis
Once hypoglycaemia was diagnosed to be the cause of the symptoms, the differential diagnosis was between:
-
▶
Insulinoma – but a high or non-suppressed insulin level would be expected in the face of low blood glucose levels
-
▶
Tumour infiltration from hepatic or adrenal metastases – if there was malignant conversion of the benign tumour
-
▶
Cortisol insufficiency
-
▶
Inappropriate use of insulin and of drugs releasing insulin and
-
▶
IGF-2 secreting non-islet cell tumour – which was finally confirmed with a high IGF-2/IGF-1 ratio.
Treatment
To avoid hypoglycaemia, the patient required a diet containing high glycaemic index nutrients and a continuous 10% glucose intravenous infusion (15 g/h).
Diazoxide was started but found to cause no increase in blood glucose levels and no protection from hypoglycaemia.
Prednisolone 20 mg twice daily was very successful in raising blood glucose levels, enabling the intravenous glucose infusion to be stopped and the patient discharged home.
Surgical review in the tertiary centre considered that the tumour was too large and vascular for surgery. Therefore, further tumour embolisation and radiotherapy were arranged.
Outcome and follow-up
Currently the patient still requires 40 mg prednisolone daily to avoid hypoglycaemia. No clinical benefit was observed from second episode of tumour embolisation (December 2010) and radiotherapy was commenced (February 2011).
Discussion
We present a case of a 67-year-old man who presented with a 6-week history of confusion and collapses, who was known to have a solitary fibrous tumour. Investigations confirmed that several weeks after tumour embolisation the tumour had started to secrete excessive quantities of IGF-2, resulting in severe recurrent hypoglycaemia.
Non-islet cell tumour hypoglycaemia is a rare paraneoplastic phenomenon seen classically with large mesenchymal tumours, such as fibrosarcomas, mesotheliomas, leiomyosarcomas, gastrointestinal stromal tumours and haemangiopericytomas.1 2 4 However, it can also be seen in epithelial tumours particularly hepatocellular carcinoma.
The first reported cases were in 1930 when Doege and Potter reported the occurrence of hypoglycaemia in a patient with an intrathoracic tumour. Since then hypoglycaemia caused by a non-pancreatic tumour has occasionally been referred to as ‘Doege-Potter syndrome’.
Tumours causing hypoglycaemia are most commonly pancreatic insulinomas or ectopic islet cell tumours producing insulin. Rarely in Hodgkin’s disease and other haematological malignancies, hypoglycaemia is produced by secretion of substances interfering with glucose metabolism, such as insulin receptor antibodies.1 In NICTH tumours have been shown to secrete excess IGF-2, as in the presented case, as well as binding to IGF receptors. IGF-2 has high affinity for the insulin receptor, which produces the ensuing hypoglycaemia. However, normally IGF-2 is tightly bound to IGF binding proteins preventing receptor activation. IGF-2 circulates in ternary complexes composed of IGF-2, insulin-like growth factor binding protein-3 (IGFBP-3) and acid-labile α subunit. In NICTH high molecular weight IGF-2 (‘big’ IGF-2) is secreted which binds to IGFBP but the resulting complex binds less well to the α subunit. The smaller complexes can travel across capillary membranes and reach target tissues more easily leading to receptor activation.5–7
Diagnosis can be made if blood results show a raised level of IGF-2 in the presence of suppressed insulin and C-peptide levels during spontaneous hypoglycaemia.
Treatment of hypoglycaemia in NICTH is curative if resection of the tumour is possible. If the tumour is too advanced for surgical cure, then medical treatment is the next step. There are reported cases where glycogen,8 diazoxide,1 have been used with effect. Growth hormone9 and glucocorticoids1 have been helpful individually at high doses or in combination at smaller doses.10 The mechanism of action is by stimulation of gluconeogenesis and suppression of ‘big’-IGF-2. Moderate to high doses of glucocorticoids may also cause shrinkage of the tumour. Tumour targeted chemotherapy and radiotherapy have also given good results.11 12
Our patient has had a good biochemical response to treatment with glucocorticoids and we are waiting to see if there is any further benefit from tumour embolisation and radiotherapy.
Learning points.
-
▶
Episodes of sudden confusion and disorientation should always trigger a check for hypoglycaemia.
-
▶
Tumours can cause hypoglycaemia through secretion of IGF-2.
-
▶
Approximately one-half of solitary fibrous tumours may present with hypoglycaemia as the initial symptom; therefore awareness of this metabolic complication is essential for tumour diagnosis.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Marks V, Teale JD. Tumours producing hypoglycaemia. EndocrRelat Cancer 1998;5:111–29 [Google Scholar]
- 2.Fukuda I, Hizuka N, Ishikawa Y, et al. Clinical features of insulin-like growth factor-II producing non-islet-cell tumor hypoglycemia. Growth Horm IGF Res 2006;16:211–16 [DOI] [PubMed] [Google Scholar]
- 3.de Groot JW, Rikhof B, van Doorn J, et al. Non-islet cell tumour-induced hypoglycaemia: a review of the literature including two new cases. EndocrRelat Cancer 2007;14:979–93 [DOI] [PubMed] [Google Scholar]
- 4.Anderson N, Lokich JJ. Mesenchymal tumors associated with hypoglycemia: case report and review of the literature. Cancer 1979;44:785–90 [DOI] [PubMed] [Google Scholar]
- 5.LeRoith D. Insulin-like growth factors. N Engl J Med 1997;336:633–40 [DOI] [PubMed] [Google Scholar]
- 6.Twigg SM, Kiefer MC, Zapf J, et al. Insulin-like growth factor-binding protein 5 complexes with the acid-labile subunit. Role of the carboxyl-terminal domain. J Biol Chem 1998;273:28791–8 [DOI] [PubMed] [Google Scholar]
- 7.Baxter RC, Daughaday WH. Impaired formation of the ternary insulin-like growth factor-binding protein complex in patients with hypoglycemia due to nonislet cell tumors. J Clin Endocrinol Metab 1991;73:696–702 [DOI] [PubMed] [Google Scholar]
- 8.Hoff AO, Vassilopoulou-Sellin R. The role of glucagon administration in the diagnosis and treatment of patients with tumor hypoglycemia. Cancer 1998;82:1585–92 [PubMed] [Google Scholar]
- 9.Drake WM, Miraki F, Siddiqi A, et al. Dose-related effects of growth hormone on IGF-I and IGF-binding protein-3 levels in non-islet cell tumour hypoglycaemia. Eur J Endocrinol 1998;139:532–6 [DOI] [PubMed] [Google Scholar]
- 10.Bourcigaux N, Arnault-Ouary G, Christol R, et al. Treatment of hypoglycemia using combined glucocorticoid and recombinant human growth hormone in a patient with a metastatic non-islet cell tumor hypoglycemia. Clin Ther 2005;27:246–51 [DOI] [PubMed] [Google Scholar]
- 11.de Boer J, Jager PL, Wiggers T, et al. The therapeutic challenge of a nonresectable solitary fibrous tumor in a hypoglycemic patient. Int J Clin Oncol 2005;11:478–81 [DOI] [PubMed] [Google Scholar]
- 12.Kampitak T. Successful treatment of non-islet cell tumor hypoglycemia in hepatocellular carcinoma with doxorubicin. Cancer Chemother Pharmacol 2008;62:929–30 [DOI] [PubMed] [Google Scholar]


