Abstract
Objective
To compare the clinical consultations provided by American and Kenyan pharmacy students in an acute care setting in a developing country.
Methods
The documented pharmacy consultation recommendations made by American and Kenyan pharmacy students during patient care rounds on an advanced pharmacy practice experience at a referral hospital in Kenya were reviewed and classified according to type of intervention and therapeutic area.
Results
The Kenyan students documented more interventions than American students (16.7 vs. 12.0 interventions/day) and provided significantly more consultations regarding human immunodeficiency virus (HIV) and antibiotics. The top area of consultations provided by American students was cardiovascular diseases.
Conclusions
American and Kenyan pharmacy students successfully providing clinical pharmacy consultations in a resource-constrained, acute-care practice setting suggests an important role for pharmacy students in the reconciliation of prescriber orders with medication administration records and in providing drug information.
Keywords: clinical interventions, advanced pharmacy practice experience (APPE), international pharmacy, Kenya
INTRODUCTION
Despite advancements in clinical pharmacy services in the United States and other developed nations,1 profound disparities exist in developing nations in both the supply of pharmacists and the implementation of clinical pharmacy services.2-5 Because of limited resources, colleges and schools of pharmacy in developing nations may face even greater challenges to meet basic workforce demands. The current shortage of pharmacists may detract from training pharmacists in clinical pharmacy provided by academic institutions.6 As a result, by comparison to pharmacy education in developed nations, there may be relatively fewer learning opportunities in clinical pharmacy in developing nations and the relative need is greater.
In addition to gaining exposure to clinical pharmacy, pharmacy students participating in advanced pharmacy practice experiences (APPEs) may contribute positively to direct patient care. Students may reduce medication costs by assisting with the conversion of medications from an intravenous to oral route of administration, provision of pharmacotherapy and drug information consultations during patient care rounds, provision of medication education and adherence counseling, and prevention of adverse drug events.7-10 Although the role of students assisting in the provision of clinical pharmacy services has been explored in the United States and other developed nations, little is known about the potential role of pharmacy students in resource-constrained patient care settings.
Since 2004, Purdue University College of Pharmacy (PUCOP) has offered the Purdue Pharmacy Kenya program in conjunction with the Academic Model Providing Access to Healthcare.11 The Purdue Pharmacy Kenya program includes 2 credit hours of didactic coursework to prepare students for an 8-week advanced international medicine APPE in Eldoret, Kenya, during the fourth year of the doctor of pharmacy (PharmD) program.12 The required international elective addresses cultural and travel preparation and management of tropical diseases through didactic lectures and small-group discussions. The experiential learning site is in western Kenya at Moi Teaching and Referral Hospital (MTRH).
At MTRH, American pharmacy students are paired with pharmacy students from the University of Nairobi School of Pharmacy (UNSOP) to create a bilateral exchange where students partner to deliver patient care. Students from the UNSOP enrolled in the bachelor of pharmacy curriculum participate in 12 months of clerkships after completing 4 years of didactic education. Didactic coursework at UNSOP includes a similar emphasis on pharmacology, pharmaceutics, anatomy, and physiology to the PharmD curricula offered by Accreditation Council for Pharmacy Education (ACPE)-accredited institutions, but lacks coursework in pharmacotherapeutics.13 Clerkships at UNSOP are typically 8 weeks in duration and UNSOP students may be placed at MTRH for multiple practice experiences.
MRTH is the second-largest public referral center in Kenya with over 600 inpatient beds. Each of the 4 public adult medicine wards may have 30 to 50 patients, with 2 or more patients occupying each bed. The limitations in healthcare worker resources in this setting are consistent with the staff-to-patient ratios seen in public sub-Saharan African health care institutions.14 Within the medicine wards, tropical diseases, human immunodeficiency virus (HIV), and tuberculosis are commonly encountered alongside many of the diseases seen in resource-rich settings such as hyperglycemic crisis, hypertensive emergency, and psychiatric illness.15 The MTRH Department of Pharmacy typically hosts 25-40 American students and 8-10 Kenyan students throughout the year. American and Kenyan pharmacy students attend daily interdisciplinary patient care rounds in the adult internal medicine hospital. The 4 patient care teams each include 1 Kenyan and 1 American student supervised during patient care rounds by 2 full-time clinical pharmacists from MTRH.
Colleges and schools of pharmacy are increasing international clerkships opportunities for their students.16,17 Most reports have focused on how students and faculty members perceive these learning experiences and have not described the impact of the pharmacy services provided. The Purdue Pharmacy Kenya model may enable American pharmacy students to overcome language and cultural barriers that exist in an international learning experience. On the other hand, local pharmacy students training in developing nations that do not have these barriers may have less exposure to clinical pharmacy. This study was conducted to characterize and compare clinical pharmacy consultations provided by American and Kenyan pharmacy students during an acute care pharmacy practice experience in a resource-constrained setting.
METHODS
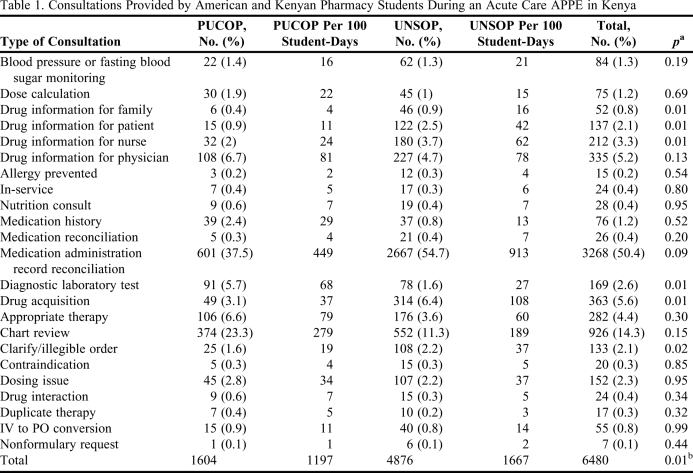
Purdue pharmacy students on this APPE were required to document consultations provided using Clini-Doc (Gold Standard; Tampa, FL), an Internet-based clinical documentation system that institutions use to quantify cost savings associated with specific types of interventions. A similar requirement was not made of Kenyan pharmacy students. Beginning in August 2008, for quality assurance and improvement purposes, MTRH preceptors required all students to document accepted consultations using a tool modeled after Clini-Doc. Documented information included the provision of medical information, drug therapy review, and proper dosing and administration (Tables 1 and 2). All documentation was completed on the same day as the consult. Students also noted specific drug classes included in consultations and the estimated amount of time spent on consultations. MTRH and American clinical pharmacists supervised students on rounds and reviewed the students' documented consultations with them.
Table 1.
Consultations Provided by American and Kenyan Pharmacy Students During an Acute Care APPE in Kenya
Abbreviations: APPE = advanced pharmacy practice experience, PUCOP = Purdue University College of Pharmacy, UNSOP = University of Nairobi School of Pharmacy, IV = intravenous, PO = per oral.
Wilcoxon rank-sum test performed to compare interventions adjusted by the number of days
A t test was performed to compare total interventions adjusted by the number of days
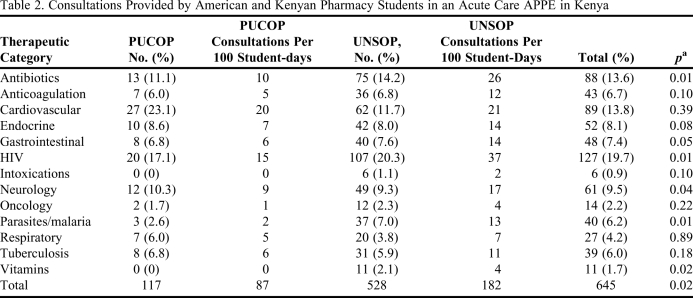
Table 2.
Consultations Provided by American and Kenyan Pharmacy Students in an Acute Care APPE in Kenya
Abbreviations: advanced pharmacy practice experience (APPE), Purdue University College of Pharmacy (PUCOP), University of Nairobi School of Pharmacy (UNSOP), Intravenous (IV), Per oral (PO)
Wilcoxon rank-sum test performed to compare interventions adjusted by the number of days
This study was a retrospective, pilot study of documented consultations provided by all pharmacy students at MTRH from August 2008 to October 2008, which included two 8-week APPEs. The primary objective was to describe and compare consultations provided by both American and Kenyan pharmacy students to identify differences between American and Kenyan student activities and further advocate for expansion of clinical pharmacy services. No patient identifiers were collected on documentation forms. The Institutional Review and Ethics Committee at MTRH and the Indiana University Purdue University Indianapolis Institutional Review Board approved this study.
Descriptive statistics were used to evaluate commonly accepted consultations for type of consultation and pharmacotherapy area of consultation. Additionally, mean and median values were used to describe consultations provided by each student. The number, type, and pharmacotherapy area of commonly provided consultations were measured for Kenyan and American students. The intervention data were adjusted to 100 days of participation in patient care rounds. Parametric data were compared using the t test and nonparametric data were compared using the Wilcoxon rank-sum test.
RESULTS
During the study period, 6 American students each completed one 8-week practice experience and 4 Kenyan students each completed two 8-week practice experiences. American students documented 1,604 consultations over an average of 23 days of patient care and Kenyan students documented 4,876 consultations over an average of 73 days of patient care. When calculated as number of interventions per 100 student-days based on 134 student-days for American students and 292 student-days for Kenyan students, American students documented 1197 consultations compared with 1671 consultations provided by Kenyan students. On average, students provided 15.2 consultations per day. American students documented 12 consultations per day compared with 16.7 consultations per day documented by Kenyan students (p < 0.001). The most common areas of consultation were medication reconciliation, chart review, medication acquisition, and drug information for physicians (Table 1). Kenyan students provided more consultations in the areas of drug information for families, patients, and nurses, medication acquisition from the pharmacy, and in clarification of medication orders (p < 0.05). American students provided more consultations in the area of diagnostic laboratory tests (p < 0.001).
Among all consultations provided, students documented the therapeutic category for 645 (10.0%) consultations. The top 3 areas for consultations were HIV, cardiovascular symptoms/disease, and antibiotics, which combined to account for nearly half of all the consultations documented (Table 2). Kenyan students documented greater proportions of the consultations conducted on antibiotics, HIV, parasites/malaria, neurology, and vitamins (p < 0.05).
Each student documented an average of 32.7 minutes/day of consultations, and the average for American students was less than that for Kenyan students (26.3 minutes vs. 35.6 minutes, respectively; p = 0.022). However, the amount of time students spent providing each consultation was similar: 2.2 minutes per consultation for American students vs. 2.1 minutes per consultation for Kenyan students (p = 0.084).
DISCUSSION
Reports describing pharmacy practice models and demonstrating the value of clinical pharmacy services in developing nations are scarce.2,3 Under the supervision of onsite clinical pharmacists, an international group of pharmacy students successfully collaborated to provide approximately 15 consultations per day for about 30 minutes per day. Nearly half of consultations provided were in the area of medical administration record reconciliation and consultations were most commonly in the areas of HIV, cardiovascular diseases, and antibiotics. The value to developed nations of clinical pharmacy services in these therapeutic areas has been well documented.18-20
The value of clinical pharmacists in the care of hospitalized patients with HIV reduces medication errors and medication costs.21-23 In Kenya, nearly 7% of adults are infected with HIV and it continues to be one of the main causes for hospitalization in this setting.15 Although data regarding the impact of clinical pharmacy services provided was not collected, a previous study in a different practice setting reported that students may reduce adverse drug events and medication costs.24 Pharmacy students at MTRH provided medication administration record (MAR) reconciliation routinely during patient care rounds to assist physicians and nurses in maintaining accurate medication lists for patients in a system that used paper-based medical records and prescriber orders. Additionally, students often clarified medication orders, facilitated drug distribution, and assisted with drug dosing. Where disparities in the supply of health care professionals exist, pharmacy students and pharmacists may have an even greater role in ensuring medication safety.
The collaborative model between American and Kenyan pharmacy students is unique and the comparison of consultations provided by each group is novel. Kenyan students generally documented more consultations and also seemed to be less limited by cultural and language barriers than did their American counterparts. The finding of more consultations provided by Kenyan students may have been due to Kenyan students' confidence and familiarity with the patient care teams because they each had completed 2 consecutive 8-week practice experiences at MTRH compared to the 1 practice experience completed by American students. Kenyan students provided more drug information consultations to Kenyan patients, family members, and nurses than did American students, in part because these individuals were less likely to speak English. Most of the medical residents and students spoke English and no difference was found between the amount of drug information provided to physicians by American and Kenyan pharmacy students. American students receive instruction in Kiswahili during the required elective course and attend Kiswahili classes while in Kenya but do not typically achieve conversational skills that would allow them to communicate easily with native speakers. This is an inherent limitation in any international learning experience where the languages spoken differ between the host and visiting students. Additionally, American students commonly cite difficulty hearing discussions on rounds due to the barely audible voice levels used by Kenyan health care workers, and this barrier may have hindered the involvement of American students with the team.
Limited resources at MTRH and in Kenya and overuse of available resources in US institutions may have contributed to the difference between American and Kenyan pharmacy students regarding laboratory monitoring.25 Patient monitoring may be more heavily emphasized in the PharmD curriculum in the United States, which emphasizes pharmacotherapeutics more than the BPharm program in Kenya, where laboratory testing resources may be limited. Educational and socioeconomic differences also may have contributed to differences in therapeutic areas of consultations. Cardiovascular diseases are more prevalent in developed nations and American students provided more consultations in this area compared with HIV and antibiotic consultations, which are more common in developing nations. American students participate in small-group learning activities and direct instruction about the pharmacotherapy of tropical diseases, both in the required elective course and in the international APPE in Kenya. By comparison, the UNSOP bachelor of pharmacy curriculum may focus more on the management of tropical diseases on a local level. In this setting, given the differences noted, partnered multinational pharmacy students may complement each other to provide improved clinical pharmacy services. Further investigation is necessary to better understand the qualitative and quantitative differences described in this investigation.
This study was limited by the small sample size and short timeframe of student enrollment. Although students received education about intervention documentation and classification, there was no assessment of baseline understanding of different intervention types, therapeutic areas, or time spent providing consultations to ensure consistency before conducting this study. Adherence to the documentation tool could have been variable and differences in practice experience length among the Kenyan and American students may have contributed to differences between the student groups. Additionally, there was no assessment of recommendations that were not accepted. Despite noted limitations, the differences found between consultations provided by American and Kenyan students are interesting and may reflect curricular differences that should be further explored. Although this study did not directly measure student learning, students who have participated in this international clerkship provided generally positive qualitative assessments of their learning experiences.26
CONCLUSIONS
A retrospective pilot study of clinical pharmacy consultations provided by a small sample of American and Kenyan pharmacy students in a resource-constrained, acute-care practice setting suggests an important role for pharmacy students in the reconciliation of prescriber orders with medication administration records and in providing drug information. Differences between Kenyan and American students' provision of drug information to nurses, patients, and patient's families, and in laboratory test monitoring were identified. Kenyan students documented more interventions for patients with HIV and infectious diseases and American students documented more interventions for patients with cardiovascular diseases.
REFERENCES
- 1.Bond CA, Raehl CL. 2006 National clinical pharmacy services survey: clinical pharmacy services, collaborative drug management, medication errors, and pharmacy technology. Pharmacotherapy. 2008;28(1):1–13. doi: 10.1592/phco.28.1.1. [DOI] [PubMed] [Google Scholar]
- 2.LeBlanc JM, Seoane-Vazquez E, Dasta JF. Survey of hospital pharmacist activities outside of the United States. Am J Health-Syst Pharm. 2007;64(16):1748–1755. doi: 10.2146/ajhp060540. [DOI] [PubMed] [Google Scholar]
- 3.Doloresco F, Vermeulen LC. Global survey of hospital pharmacy practice. Am J Health-Syst Pharm. 2009;66(5 Suppl 3):S13–S9. doi: 10.2146/ajhp080674. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization and International Pharmaceutical Federation. Developing pharmacy practice: a focus on patient care. www.who.int/entity/medicines/publications/WHO_PSM_PAR_2006.5.pdf. Accessed February 15, 2011.
- 5.Mullan F, Panosian C, Cuff P, editors. Healers Abroad: Americans Responding to the Human ResourceCcrisis in HIV/AIDS. Washington, DC: National Academies Press; 2005. [Google Scholar]
- 6.Anderson C, Bates I, Beck D, et al. The WHO UNESCO FIP Pharmacy Education Taskforce: enabling concerted and collective global action. Am J Pharm Educ. 2008;72(6) doi: 10.5688/aj7206127. Article 127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCollum M, Nuffer W, Ellis SL, Turner CJ. Physician acceptance of pharmacotherapy recommendations made by pharmacy students in a rural pharmacy-based diabetes care and education clinic. Am J Pharm Educ. 2009;73(2) doi: 10.5688/aj730224. Article 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sweeney MA, Marazon DJ, Burke WJ, Fuci DR, Huffman SG. Effects of pharmacy student interventions on a family medicine residency program. J Am Pharm Assoc. 2000;40(1):92–94. doi: 10.1016/s1086-5802(16)31042-7. [DOI] [PubMed] [Google Scholar]
- 9.Bock LM, Duong MT, Williams JS. Enhancing clinical services by using pharmacy students during advanced experiential rotations. Am J Health-Syst Pharm. 2008;65(6):566–569. doi: 10.2146/ajhp070336. [DOI] [PubMed] [Google Scholar]
- 10.Gerdemann A, Griese N, Schulz M. Pharmacy interns on the ward – a pilot study. Pharm World Sci. 2007;29(1):34–38. doi: 10.1007/s11096-005-5044-z. [DOI] [PubMed] [Google Scholar]
- 11.Einterz RM, Kimaiyo S, Mengech HN, et al. Responding to the HIV pandemic: the power of an academic medical partnership. Acad Med. 2007;82(8):812–818. doi: 10.1097/ACM.0b013e3180cc29f1. [DOI] [PubMed] [Google Scholar]
- 12.Pastakia SD, Schellhase EM, Jakait B. Collaborative partnership for clinical pharmacy services in Kenya. Am J Health-Syst Pharm. 2009;66(15):1386–1390. doi: 10.2146/ajhp080483. [DOI] [PubMed] [Google Scholar]
- 13. Bachelor of Pharmacy Degree Program, University of Nairobi School of Pharmacy. http://www.uonbi.ac.ke/faculties/?fac_code=62. Accessed February 15, 2011.
- 14.Anyangwe SC, Mtonga C. Inequities in the global health workforce: the greatest impediment to health in sub-Saharan Africa. Int J Environ Res Public Health. 2007;4(2):93–100. doi: 10.3390/ijerph2007040002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tornheim JA, Manya AS, Oyando N, et al. The epidemiology of hospitalization with diarrhea in rural Kenya: the utility of existing health facility data in developing countries. Int J Infect Dis. 2010;14(6):e499–505. doi: 10.1016/j.ijid.2009.07.021. [DOI] [PubMed] [Google Scholar]
- 16.Mashburn JH, Brown CM. Pharmacy students' awareness of and interest in pharmacy-related international education/study abroad programs. Am J Pharm Educ. 2000;64(1):62–67. [Google Scholar]
- 17.Ward CT, Nemire RE, Daniel KP. The development and assessment of a medical mission elective course. Am J Pharm Educ. 2005;69(3) Article 50. [Google Scholar]
- 18.Dellit TH, Owens RC, McGowan JE, Jr, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44(2):159–177. doi: 10.1086/510393. [DOI] [PubMed] [Google Scholar]
- 19.Carter BL, Ardery G, Dawson JD, et al. Physician and pharmacist collaboration to improve blood pressure control. Arch Intern Med. 2009;169(21):1996–2002. doi: 10.1001/archinternmed.2009.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.ASHP statement on the pharmacist's role in the care of patients with HIV infection. Am J Health-Syst Pharm. 2003;60(19):1998–2003. doi: 10.1093/ajhp/60.19.1998. [DOI] [PubMed] [Google Scholar]
- 21.Bozek PS, Perdue BE, Bar-Din M, Weidle PJ. Effect of pharmacist interventions on medication use and cost in hospitalized patients with or without HIV infection. Am J Health-Syst Pharm. 1998;55(11):1151–1155. doi: 10.1093/ajhp/55.11.1151. [DOI] [PubMed] [Google Scholar]
- 22.Pastakia SD, Corbett AH, Raasch RH, Napravnik S, Correll TA. Frequency of HIV-related medication errors and associated risk factors in hospitalized patients. Ann Pharmacother. 2008;42(4):491–497. doi: 10.1345/aph.1K547. [DOI] [PubMed] [Google Scholar]
- 23.Heelon M, Skiest D, Tereso G, et al. Effect of a clinical pharmacist's interventions on duration of antiretroviral-related errors in hospitalized patients. Am J Health-Syst Pharm. 2007;64(19):2064–2068. doi: 10.2146/ajhp070072. [DOI] [PubMed] [Google Scholar]
- 24.Mackinnon GE. Analysis of pharmacy student interventions collected via an internet based system. Am J Pharm Educ. 2003;67(3) Article 90. [Google Scholar]
- 25.van Walraven C, Naylor CD. Do we know what inappropriate laboratory utilization is? A systematic review of laboratory clinical audits. JAMA. 1998;280(6):550–558. doi: 10.1001/jama.280.6.550. [DOI] [PubMed] [Google Scholar]
- 26.Pastakia SD, Schellhase EM. AMPATH and Purdue - Collaboration for Access. http://www.ampathpurdue.blogspot.com/. Accessed February 15, 2011.