Abstract
Objective
To implement and assess a medication therapy management (MTM) training program for pharmacy students using the MirixaPro (Mirixa Corporation, Reston, VA) platform and case studies.
Design
Students received lectures introducing MTM and were given a demonstration of the MirixaPro platform. They were divided into teams and assigned cases and times to interview patients portrayed by faculty members. Using the MirixaPro system, students performed 2 comprehensive medication reviews during the semester, recording the patient's current medications, indications, side effects, allergies, health conditions, and laboratory test recommendations and developed a personal medication record and medication action plan.
Assessment
Based on a rubric with a rating scale of 0-10, campus and distance pathway students received mean scores ranging from 6.3-7.4 for their performance on the second MTM exercise, an increase of 47%-54% over the first MTM exercise. In qualitative assessments, the majority of students believed that their confidence in providing MTM was enhanced by the activity, while faculty members recognized the advantage of using MirixaPro, which allowed students to experience what is required in processing a pharmacist led, billable MTM encounter.
Conclusions
Use of the MirixaPro system and patient cases provides students with a “hands-on” experience that may encourage them to promote MTM during their APPEs and provide MTM services as practicing pharmacists.
Keywords: medication therapy management (MTM), Web-based technology, active learning, patient simulation, case-based learning
INTRODUCTION
Medication therapy management services evolved as part of the Medicare Part D prescription drug plans under the Medicare Prescription Drug Improvement and Modernization Act of 2003.1 The act requires that MTM programs “optimize therapeutic outcomes through improved medication use and reduce the risk of adverse events, including adverse drug reactions, in certain high risk patients.” The Joint Commission of Pharmacy Practitioners (JCPP) envisions that pharmacy education will prepare pharmacists to provide patient-centered care that optimizes medication therapy, and that pharmacists will be accountable for patients’ therapeutic outcomes.2 By doing so, pharmacists will be recognized by the public as those who improve medication use by empowering patients and by ensuring that MTM is readily accessible to all.
As of July 1, 2007, the accreditation standards of the Accreditation Council for Pharmacy Education (ACPE) require colleges and schools of pharmacy to provide graduates with basic MTM training.3
The National Association of Boards of Pharmacy (NABP), in their NAPLEX Blueprint, designates that student pharmacists should have knowledge, judgment, and skills demonstrated in the management of drug regimens by monitoring and assessing the patient and patient information, collaborating with other health care professionals, and providing patient education. The Blueprint is explicit in its management section 1.3 that student pharmacists actively manage their patient's drug therapy by identifying, preventing, and resolving medication-related problems and enhancing therapeutic outcomes.4
In Quality and Safety Pharmacy Principles for Health Care Reform of 2008, a broad range of stakeholders that included professional organizations and national retailers stated that pharmacists help achieve the best possible medical outcomes through various types of medication-related services. Principle I (A) of that document notes that reform must “incorporate coverage for pharmacist-provided patient care services into … healthcare programs … (that) include medication therapy reviews … (and) medication therapy management…”5 This document shows a united effort by the profession regarding the role of pharmacists in a reformed health care system. Educators must ensure their graduate pharmacists are trained and they are proficient and confident in providing MTM services.
The core elements of MTM (medication therapy review, personal medication record, medication-related action plan, intervention and/or referral, and documentation and follow-up)6 are part of the specific professional requirements of patient assessment, pharmaceutical care plan development, and drug therapy evaluations of the ability-based outcomes for Creighton University's doctor of pharmacy (PharmD) curriculum.7 Our newly revised educational outcomes for pharmacy graduates mirror the NAPLEX Blueprint in regard to MTM. This report describes the development, implementation, and assessment of the use of the MirixaPro platform in the Dispensing and Pharmaceutical Care laboratory course in order to enhance student skills in the provision of MTM.
The purpose of the exercise in the Dispensing and Pharmaceutical Care course was to provide the students an opportunity to have a practical MTM experience using the MirixaPro platform. The MirixaPro platform provides an electronic guide that indicates information that must be obtained to successfully complete a pharmacist-led billable MTM case. The learning outcomes objective was improvement in students’ performance of MTM including making appropriate recommendations for changes in a patient's medication therapy, lifestyle, and disease-state monitoring, as documented by faculty assessment using a rubric and by review of Mirixa MTM case records.
DESIGN
Mirixa Corporation, sponsored by the National Community Pharmacists Association (NCPA), offers targeted patient care services delivered via one of the nation's largest pharmacy-based patient care networks. Mirixa contracts with community pharmacists to provide diverse patient care services, such as MTM, to improve the quality and accessibility of healthcare for patients through community pharmacy. Mirixa began contracting with colleges and schools of pharmacy in 2007 to use the MirixaPro Web-based platform in the classroom. This allows student pharmacists to become familiar with the system and, in turn, assist in the provision of patient care services while completing introductory pharmacy practice experiences (IPPE) and advanced pharmacy practice experiences (APPE).
Realizing the need for more training opportunities for MTM in the curriculum, an MTM component was added to the spring semester of the Dispensing and Pharmaceutical Care laboratory in 2008 and 2009. These students were in the final semester of their third year in the pharmacy program, had completed pharmacology, and were enrolled in their last semester of therapeutics. The MTM portion of the course involved one 50-minute lecture, a 30-minute demonstration of the MirixaPro system, and two 1-hour laboratory sessions in which the students conducted patient interviews. The introductory lecture presented the 5 key components of MTM. A demonstration of the MirixaPro system entailed navigation of the Internet-based platform and basic information about system entry. The initial laboratory session introduced students to the process and the platform. In both the first and second sessions, students completed their case assignments and were assessed on their ability to provide MTM. Creighton University School of Pharmacy and Health Professions is unique in that it has both a campus and a distance-learning pathway, so parity in the programs must be demonstrated. The time between the baseline MTM session and the follow-up session was 7 weeks for the 2008 campus group, 6 weeks for the 2009 campus group, and 5 days for the distance group because of summer laboratory time constraints.
One of the co-instructors of the Dispensing and Pharmaceutical Care course developed 24 cases for student use in patient interviews. All cases were standardized to contain the same types of information: number of patient medications, patient allergies, drug-disease interactions, drug-drug interactions, therapeutic duplications, follow-up laboratory test recommendations, inappropriate dosing or dosing regimens, adherence to therapy issues, and medication cost considerations.
Mirixa assigned students their own virtual pharmacy under the Creighton University account and gave each student a username and password. The co-instructor loaded patient cases into each student's pharmacy. When the students logged on to the MirixaPro platform, they were only able to access their own pharmacy and patient cases.
Scenarios for each patient case were given to the course instructors and 6 other pharmacy practice faculty members from the school who agreed to play the role of patients. To accommodate the class size, groups of 8 to 10 students interviewed 1 of the 8 faculty members playing the role of the patient. Each group of students was matched to the faculty member who had their case. Each patient case contained specific embedded information that only would be revealed if the student asked appropriate questions. Examples of embedded information included: the patient's list of medications was not current; the patient had been given samples of medication from his physician that did not appear in the patient profile in the MirixaPro system; the patient's physician had made dosing changes that were not reflected on the patient's prescription medication labels; the patient had experienced side effects that mandated laboratory monitoring or possible drug discontinuation; the patient had been noncompliant with taking his medication due to medication cost (ie, the cost of the patient's brand name medication included a $50 co-pay so he decided not to get it refilled); and the patient was not taking her medication as directed (ie, instead of 1 tablet 3 times daily, the patient was taking all 3 tablets at bedtime). The students were allotted 1 hour during the Dispensing and Pharmaceutical Care laboratory to conduct their patient interview.
Students were required to complete 2 MTM patient cases during the semester. The students received their case 1 week prior to their assigned interview time to allow for research and preparation. The students logged into their pharmacy and viewed their patient demographics, medications, and computer-generated alerts. To facilitate their understanding of MTM, they were instructed that they would be recording their recommendations into the Mirixa pharmacy program immediately after completing the patient interview to simulate a real life, “hands-on” experience. Prior to the laboratory session, they were to study the case for potential medication problems and make a list of questions they had for the patient.
The 159 third-year students interviewed the simulated patient with regard to their medication use and lifestyle. Each student in the group was required to ask a minimum of 3 questions. Those questions included information on their patient's medication history, medication-taking behavior, and lifestyle and social history. Students took turns asking questions. After the student group conducted their interviews, each student completed their comprehensive medication review by recording information into the MirixaPro platform. Although students were allowed to work in groups for the patient interview, all student recommendations were completed individually. Their entry required inclusion of current medications (prescription and nonprescription), strength and dose, dosing interval, medication indications, patient allergies and health conditions, side effects, SOAP (subjective, objective, assessment, and plan) notes, and laboratory test recommendations. Students were required to explain how they resolved therapeutic duplications, significant drug-drug interactions, inappropriate dosing, therapeutic substitution issues, and any circumstance flagged by the program. Additionally, each student developed a personal medication record and medication action plan for the patient.
EVALUATION AND ASSESSMENT
Over a 2-year period, 318 third-year student pharmacists from campus and distance pathways participated in MTM training. One hundred percent of the students completed the 2 MTM cases. All students successfully resolved medication therapy difficulties and closed their cases in the MirixaPro platform.
After reviewing each case, course instructors and faculty members who portrayed the patients graded the students’ MTM recommendations and plans using a case-specific rubric to evaluate the thoroughness of their work. Both faculty members and students provided written reflections on the use of the platform as a training tool.
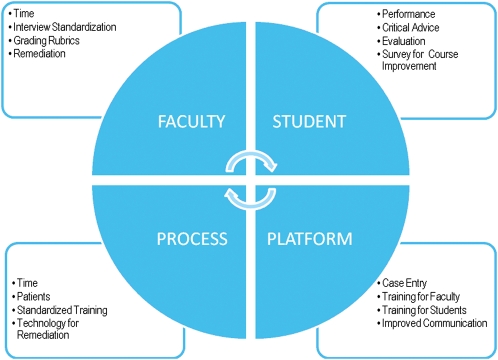
Faculty members participated in a discussion session to review student survey data results and assess the strengths and weaknesses of the MirixaPro program and this laboratory sequence. The approach used a quadrant perspective (students, platform, process, and faculty) that analyzed students’ opinions, performance, and acceptance of the activity; various aspects of the use of the MirixaPro platform; the entire process sequence in regard to time, training, patient interviews, and potential for remediation; and, faculty members’ opinions with regard to time spent on the entire sequence, interview standardization, use of grading rubrics, and potential remediation activities (Figure 1).
Figure 1.
Analysis of the medication therapy management training experience.
Faculty members submitted the case-specific rubrics with scores to the course instructors. A point was earned in the rubric for each problem item identified by the student. The course instructors set a minimum number of points as a passing score. Additional points were awarded if the students made other health maintenance recommendations that enhanced patient outcomes. Due to the introductory nature of the MTM process, the number of points required to pass the initial experience was minimal. Sixty-nine students’ scores were not included because of incomplete rubric scores or grader inconsistencies in earning points. Scores from the other 249 students were analyzed according to year and pathway.
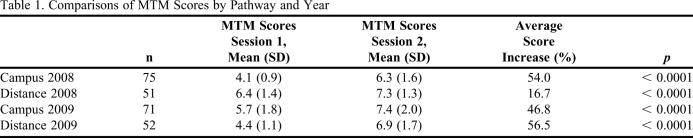
Individual scores were assessed for improvement in performance of MTM by comparing points earned in the first session with those earned in the second session using the paired t test. Average score increases/decreases for each cohort were arrived at by first calculating the percentage change in each student's rubric scores (eg, an initial score of 3 and a subsequent score of 6 would be calculated as a change of +100%, and an initial score of 4 with a subsequent score of 3 would be calculated as -25%). Those results were then averaged. The first cohort of campus-pathway students had an average rubric score of 4.1 (with a range of 3 to 6) out of 10 on their initial performance of the MTM case. Rubric scores improved to an average of 6.3 (with a range of 3 to 9) out of 10. The average increase in those scores was 54%. The first cohort of distance-pathway students had an average rubric score of 6.4 (with a range of 4 to 8). Rubric scores improved to an average of 7.3 (with a range of 5 to 10). The average increase in those scores was 17% (Table 1).
Table 1.
Comparisons of MTM Scores by Pathway and Year
The second cohort of campus-pathway students had an average rubric score of 5.6 (with a range of 2 to 9) out of 10 on their initial performance of the MTM case. Rubric scores improved to an average of 7.4 (with a range of 3 to 10) out of 10. The average of the increase in those scores was 46.8%. The second cohort of distance-pathway students had an average rubric score of 4.4 (with a range of 3 to 7). Rubric scores improved to an average of 6.9 (with a range of 3 to 10). The average increase in those scores was 56.5%. The paired t test results (p < 0.0001 in all cohort comparisons) indicated improvement in MTM skills from the initial to the second session. The data support the learning outcome objective of this approach. The cohort comparisons are summarized in Table 1.
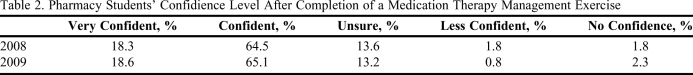
A questionnaire assessing student opinions about the MTM laboratory assignments was completed by 235 (88%) students. The first group of 51 distance-pathway students was not surveyed due to time constraints. Thirty-two students did not respond. Responses from students regarding their confidence level based on a 5-point Likert scale are shown in Table 2. In both offerings, the majority of students believed that their confidence in providing MTM was enhanced by this activity.
Table 2.
Pharmacy Students’ Confidience Level After Completion of a Medication Therapy Management Exercise
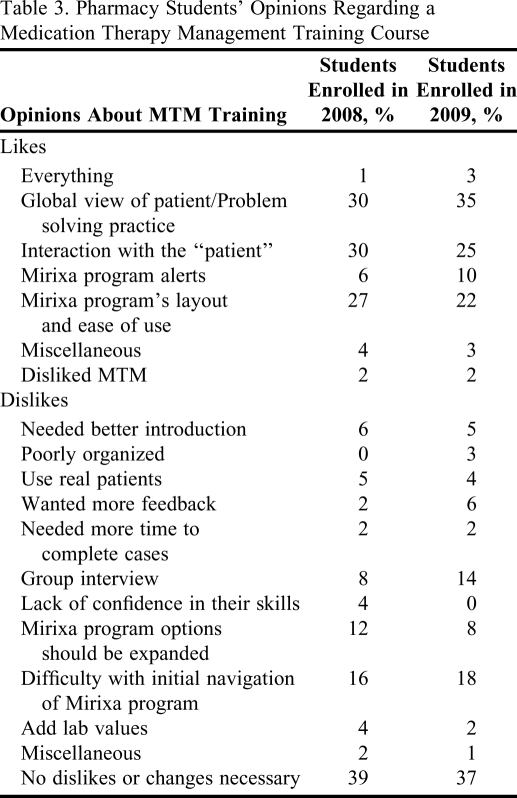
Open-ended questions regarding the most and least valuable aspects of the projects, what could be changed in the future, and any additional comments providing descriptive feedback also were given to the students. Student “likes” and “dislikes” of the MirixaPro program and training process are shown in Table 3.
Table 3.
Pharmacy Students’ Opinions Regarding a Medication Therapy Management Training Course
Students Theme Analysis of Reflective Responses
At the completion of the laboratories, students provided written reflections of their training. Qualitative data collected from student reflections and a theme analysis was conducted by a group of pharmacy faculty members with experience in MTM. Four hundred seventy open-ended comments from 235 students were included. The majority of students (88) communicated that they saw the benefit, functionality, and practicality of using the MirixaPro platform.
The most prominent theme (comments expressed by 71 students) was one of increased appreciation for MTM and the importance of that service. Pharmacy students reported value in their interactions with the patient and how it gave a more realistic approach to their problem-solving activities. Students also perceived an increase in their confidence in the use of the MirixaPro platform as they conducted the MTM exercises. They reflected on how they developed a better perspective on applying their MTM skills by having to use all of their therapeutic knowledge. Some students expressed that the experience increased their self-confidence by having to think with a global perspective.
Sixty-six pharmacy students articulated that the interview process was the most positive aspect of the experience. They focused more on the patient interaction than their perspective on MTM and the use of an online platform. One student commented, “I loved finding out how the patient is actually taking their medications, how they are working, and what problems they are having. After interviewing patients, you get to know them and can relate to them better, and you see that you aren't just dealing with a case on a piece of paper.” This thought was frequently expressed as students spoke with their patients and realized all of the intricacies that come into play and may hinder patient compliance. A limitation expressed by 35 students was that they would have preferred an individual interview versus a group interview with the patient.
There also was an underlying sense of fulfillment as students realized that their contribution through MTM would impact patient outcomes (52). There was a recurring theme of the pharmacist's positive effect on the management of a patient's therapy and ultimately the application of MTM principles in their future practices. One student wrote, “As a pharmacist, I am one of the major players. We have to ensure that the patients are being compliant and identify any problems that other health care professionals have missed. Patients may have various physicians who do not know that they have other drug therapies. We are the ones who put it all together and can impact patient lives. MTM is a wonderful opportunity and pharmacists need to take advantage of it before it is gone.”
Another common theme shared by 21 students was their sense of understanding and accomplishment in providing patient-focused services, even though it all occurred in a laboratory setting. They expressed being able to “think like a pharmacist” and felt benefit from the whole project—from the initial interview to the completion of the case with the Mirixa pharmacy system. They felt the process simulated a real-life experience and believed that they could successfully conduct MTM in their fourth year and beyond.
Faculty Theme Analysis of Reflective Responses
The general themes with regard to the MirixaPro program were that more time was needed for students to navigate through the system, more time was needed to train faculty members who assisted with the interviews and grading, and improved communication was needed between faculty members and students with regard to accessing/using the Mirixa program.
When reviewing the second MTM case, all faculty members noted that students felt more comfortable with the use of the platform. Faculty members also recognized the advantage of using MirixaPro as a training tool, allowing students to experience what is required in processing a pharmacist led, billable MTM encounter. Faculty members agree that MTM should continue to be a required component of pharmacy education.
DISCUSSION
As the number of prescription and nonprescription medications used by patients increases,8 pharmacy educators have the responsibility to teach students the importance of MTM. The simulated use of technology in training student pharmacists is necessary. The fact that the MirixaPro platform was available as a resource at no charge to universities and provides a real-life training resource is invaluable. Even with the use of faculty-simulated patients, students appreciated the value of being able to interview a patient when providing MTM. Students acknowledged that much information can be gleaned during an interview that cannot be communicated when completing MTM for a patient described in a paper case or a medical record.
In our school's experience, students’ exposure to MTM in internship activities is limited. Students have reported that MTM is not being routinely modeled in community pharmacy practice experiences. By providing this experience in the classroom curriculum, the knowledge and skills necessary for students’ confidence to provide MTM are reinforced prior to their clinical experiences.
Faculty members discussed the Mirixa flags. The program alerted students to many therapeutic duplications, drug-disease interactions, drug-drug interactions, and inappropriate dosing regimens. The specially designed cases added more complexities to the patient profile that the program did not display, so the students still were required to resolve therapeutic issues. Faculty members questioned whether the program's identification of therapeutic problems through its flagging alert system altered the students’ scope of recommendations. For the practicing pharmacist, the flags assist in swift identification and resolution of interactions and duplications, but as a training tool, they may have detracted from the students’ critical thinking and problem-solving abilities.
The extensive time required for faculty members to be present for laboratory activities and provide timely feedback to the students also was a challenge. Each faculty member had to review over 20 MirixaPro cases per semester and provide timely feedback to the students. The course instructors identified gaps in interrelator reliability and realize that faculty members need improved training to ensure uniform use of the rubric and evaluation of the students, and that the scenarios need to be standardized to ensure that each student is given the same patient history and information. The grading among faculty members was not consistent because some gave additional points for health maintenance recommendations, while others focused only on specific criteria. Scenarios were not explicitly “standardized” because from one laboratory to the next, the questions the students posed could change the outcomes of the patient therapy. One way to correct this would be to expand the standard patient information to include health maintenance history and psychosocial components of the patients in the scenarios.
Course instructors also faced the problem of how remediation should be accomplished for those students who did not meet the minimum score requirement for the MTM exercise. One approach the instructors will take for future sessions is to have faculty MTM experts record their main comments about the case and allow students who need remediation to view the video-taped session on the course Web site. These students then would be offered a third case to determine whether their MTM skills had improved sufficiently.
CONCLUSION
Student pharmacists have a desire to provide direct patient care and to improve patient outcomes through optimizing patient medication therapy and reducing adverse events. Use of the patient interview and the MirixaPro platform provided third-year students with MTM experience prior to starting their clinical pharmacy practice experiences. The MirixaPro platform provided a technological tool for the training process that was accepted by students and faculty members as a method to record and document MTM activities. The repeated use of the MirixaPro program improved students’ MTM performance in general and enhanced their comfort level with regard to patient interviews, MTM format, and recommending changes to optimize medication therapy. Most students believed the activity was helpful in developing their practical knowledge of MTM. Experiences like this serve to empower students to promote MTM during their APPEs and to provide MTM services as practicing pharmacists.
ACKNOWLEDGEMENTS
We acknowledge Mirixa Corporation, the National Community Pharmacists Association (NCPA), and Rebekah Jackowski, PharmD, who was with the Mirixa Corporation when this training experience was developed.
REFERENCES
- 1. Public Law 108-13. The Medicare Prescription Drug, Improvement, and Modernization Act of 2003. HR 1. December 8, 2003. http://www.cms.hhs.gov/MMAUpdate/downloads/PL108-173summary.pdf. Accessed March 25, 2011.
- 2. Joint Commission of Pharmacy Practitioners. An Action Plan for Implementation of the JCPP Future Vision of Pharmacy Practice, January 31, 2008. www.papharmacists.com/JCPPVisionPharmacyPractice_ExecutiveSummaryrevised.doc. Accessed March 25, 2011.
- 3. Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed March 25, 2011.
- 4. National Association of Boards of Pharmacy NAPLEX Blueprint. http://www.nabp.net/programs/examination/naplex/naplex-blueprint/. Accessed March 19, 2011.
- 5. Pharmacy Principles for Health Care Reform. December 2008. http://www.ashp.org/DocLibrary/News/PharmacyHealthCareReformPrinciples.pdf. Accessed March 25, 2011.
- 6.American Pharmacists Association and National Association of Chain Drug Stores Foundation. Medication therapy management in community pharmacy practice: core elements of an MTM service (version 2.0) J Am Pharm Assoc. 2008;48(3):341–353. doi: 10.1331/JAPhA.2008.08514. [DOI] [PubMed] [Google Scholar]
- 7. Creighton University School of Pharmacy and Health Professions Bulletin Varsity Press, Omaha, Nebraska, 2009-2011;94(3):1-82.
- 8. Prescription Drug Use Continues to Increase: U.S. Prescription Drug Data for 2007–2008. http://www.cdc.gov/nchs/data/databriefs/db42.pdf. Accessed March 19, 2011.