Abstract
Objective
To enhance students’ knowledge of and critical-thinking skills in the management of acutely ill patients using online independent learning partnered with high-fidelity patient simulation sessions.
Design
Students enrolled in the Acute Care Simulation watched 10 weekly Web-based video presentations on various critical care and advanced cardiovascular pharmacotherapy topics. After completing each online module, all students participated in groups in patient-care simulation exercises in which they prepared a pharmacotherapeutic plan for the patient, recommended this plan to the patient's physician, and completed a debriefing session with the facilitator.
Assessment
Students completed a pretest and posttest before and after each simulation exercise, as well as midterm and final evaluations and a satisfaction survey. Pharmacy students significantly improved their scores on 9 of the 10 tests (p ≤ 0.05). Students’ performance on the final evaluation improved compared with performance on the midterm evaluation. Overall, students were satisfied with the unique dual approach to learning and enjoyed the realistic patient-care environment that the simulation laboratory provided.
Conclusion
Participation in an elective course that combined self-directed Web-based learning and hands-on patient simulation exercises increased pharmacy students’ knowledge and critical-thinking skills in acute care.
Keywords: patient simulation, online learning, critical thinking, problem-solving skills, acute care, critical care, cardiovascular
INTRODUCTION
Improving student engagement and immersion in the learning environment is a focus of pharmacy education because of the demand for higher levels of learning within the pharmacy profession. Educators must incorporate active learning into the pharmacy curriculum to foster critical-thinking skills and other desirable learning outcomes in students. High-fidelity patient simulation offers a unique learning opportunity for students. The simulation of patient cases allows facilitators to control the learning environment for each student, adapting the simulation to the level of student performance, and to provide immediate debriefing and assessment. Performance-based examinations using patient simulation are a better means of evaluating students’ cognitive skills than written examinations.1 High-fidelity patient simulation is effective in the development of confidence, pharmacotherapeutic knowledge, and physical assessment skills2-4 and has a positive impact on patient care.5-11 Combining online and simulation-based learning provides an excellent way to enhance skills and knowledge as well as objectively assess knowledge and performance. With patient simulation, students can see and hear a topic, be tested and practice the skills through online assessments, and perform functions of a pharmacist in comprehensive assessments.
Students’ critical thinking and knowledge can be enhanced in an immersive learning environment with patient simulation.12 By combining Web-based technology with patient simulation, the dual immersion may better convey information and assess student knowledge, and provide immediate feedback for students and more efficient use of faculty contact time. Simulation software allows a level of formative and summative assessment of first- through third-year pharmacy students that typically is not performed until advanced pharmacy practice experiences.
The intent of integrating simulation throughout our curriculum links directly to our mission to prepare student pharmacists to be health care practitioners who optimize the health of patients and society through the effective use of medicines and other interventions. Simulation addresses our overall curricular outcomes of critical thinking, development of knowledge and skills, communication skills, patient assessment, pharmaceutical care plan development, medication therapy management, pharmacodynamic decision making, and pharmaceutical product preparation, dispensing, and administering. We describe the first immersive, dual-technology course to be offered in pharmacy education that provides a comprehensive assessment of advanced skills. By partnering online, independent learning with high-fidelity patient simulation sessions, our objective was to enhance students’ critical-thinking skills in the management of acutely ill patients in a collaborative and realistic environment.
DESIGN
This course was designed to allow students to apply clinical knowledge, skills, and attitudes gained in previous courses to the care of patients with advanced cardiovascular diseases and those who are critically ill. This approach incorporates elements from the entire spectrum of pharmacy education, from pharmacology knowledge to patient care skills and pharmacists' attitudes.
The 3-credit Acute Care Simulation elective course was first offered at the University of Pittsburgh School of Pharmacy in 2008. The course used simulation-based learning to facilitate student competency in the knowledge and use of pharmacologic agents, as well as to improve clinical pharmacotherapy decision-making. The student was expected to provide a sophisticated course of treatment, including monitoring plans, when presented with realistic patient cases. Moreover, the student was expected to demonstrate the communication skills necessary to explain to a lay person or medical colleagues the rationale for their selection of each therapeutic agent so they would be able to function effectively in an interprofessional team environment.
A major component of this course was self-study, requiring an adult-learning approach to education through online learning. Experts in cardiology and critical care delivered 45-minute presentations (viewed in 3-4 segments, each lasting 10-15 minutes) on various topics of evidence-based pharmacotherapy including prophylaxis (eg, stress ulcer and deep vein thrombosis), acid/base disorders, pharmacokinetics/pharmacodynamics, adverse drug events, sedation, cardiogenic shock, distributed shock, acute kidney injury, and advanced cardiac life support. Students watched three or four 10- to 15-minute online video modules on critical care and advanced cardiovascular pharmacotherapy topics and completed online quizzes prior to the exercise in the simulation center.” The instructor monitored students’ progress in the online learning portion of the course using the grade book capabilities of CourseWeb (Blackboard, Inc). The course instructor updated the material in the online presentations and in the simulation based on evolving evidence in the field.
Groups of 4 to 5 students participated in 3 patient-care simulation sessions each week of the semester at the Peter M. Winter Institute for Simulation Education and Research (WISER Institute). During these sessions, the students cared for simulated patients. The patient simulators had physiologic characteristics, such as heart and lung sounds, in addition to hemodynamic parameters. The patient simulations were controlled by the SimMan software (Laerdal Corporation, Stavanger, Norway), which was preprogrammed with the appropriate physiological characteristics of various diseases and a variety of medication responses. A facilitator coordinated the simulation session from a control room with one-way glass or from inside the patient room (Figure 1). Students interacted with the simulated patient and/or family member or physician to collect necessary subjective and objective data. Students prepared a pharmacotherapeutic plan that included a monitoring plan, drug administration guidance, and the rationale for each, and recommended medications at the patients' bedside to the facilitator.
Figure 1.
Pharmacy students in the Acute Care Simulation course caring for a simulated patient.
Debriefing, a key component in assessing a simulation exercise, was conducted at the conclusion of each patient case. The simulation software determined whether decisions made by the student group were appropriate based on the preprogrammed scenario and provided objective assessment for each action taken. Also, the facilitator provided verbal feedback on learner actions that occurred during the scenario and answered the students’ questions during the debriefing. The facilitator also provided the group with their grade and constructive feedback at the completion of the simulation.
EVALUATION AND ASSESSMENT
Thirteen students completed the Acute Care Simulation course in 2010. Instructors assessed 3 areas during the course: students’ (1) performance/critical-thinking skills, (2) knowledge, and (3) satisfaction with the elective course.
Weekly Pretests/Posttests
To assess their pharmacology knowledge, students completed an online multiple-choice and short-answer pretest each week for each topic in the course. Students were required to pass the pretest each week to demonstrate that they had completed the online portion of the course prior to participating in the group simulation session. After the simulation exercise, students completed a posttest to determine whether the student gained additional insight and clarity from the simulation session. There was no opportunity for students to discuss the weekly pretest with each other as the simulation occurred immediately after the pretest and the faculty members were present at all times.
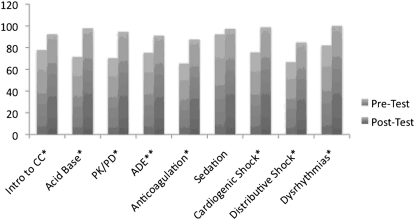
The average pretest and posttest scores for the 10 weekly lectures are presented in Figure 2. A comparison between the pretest and the posttest scores was completed using a Student t test. Scores on 9 of the 10 weekly posttests were significantly higher than scores on the pretests (p ≤ 0.05) suggesting simulation contributed to the students’ learning in addition to the online lecture.
Figure 2.
Comparison of the Average Pre-Test and Post-Test Scores (n=13 for each quiz). All of the improvements in knowledge from pretest to posttest were significant (p < 0.05) except for knowledge of sedation.
Midterm and Final Evaluations
The facilitators used a pharmacotherapy-plan rubric to comprehensively evaluate students’ clinical and critical-thinking skills using a standard method.4 The pharmacotherapy plan rubric was designed specifically for pharmacy education to measure performance and critical thinking by evaluating the steps needed to obtain and interpret clinically relevant data and to solve pharmacotherapeutic problems and develop a monitoring plan. The rubric evaluates subjective and objective data collection including medication history, allergy information, and laboratory data. After the data are collected, the student assesses the patient and makes a diagnosis. Diagnosis only accounts for 1% of the grade. If the diagnosis is incorrect, the student is given the appropriate diagnosis before developing the pharmacotherapeutic plan. The plan includes all aspects of the medication therapy (drug, dose, route, duration, administration recommendations, and monitoring plan). The course instructor distributed and described the pharmacotherapy rubric to students at the beginning of the course and the students used the rubric for group practice in the simulations and for group and individual assessment throughout the semester.
The course instructor assessed each student's performance individually in a midterm and final patient simulation evaluation. The midterm assessment involved provision of care to a patient with acute myocardial infarction and cardiogenic shock. Basic care involved assessment of patient Feeding, Analgesia, and Sedation; Thromboembolic prevention; Head of bed elevation; stress Ulcer prophylaxis, and Glucose control—a standardized approach known by the acronym FAST HUG.13 The concepts tested during the final case were acid/base disorders and septic shock. During the simulation assessments, the student verbally gathered patient data from the course instructor portraying/acting as the attending physician and from the mock patient chart and monitors at the patient's bedside. The student was expected to perform a physical assessment of the mannequin as needed. The student verbally presented the pharmacotherapeutic and monitoring plans to the course instructor acting as the attending physician, who used an electronic version of the grading rubric to assess the student's performance which is electronically programmed within the software and displayed in the patient room during the debriefing.
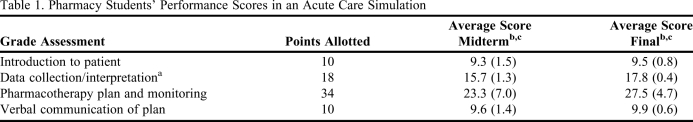
The pharmacotherapy rubric was categorized into 4 general themes for assessment including: (1) introduction to patient; (2) data collection and interpretation; (3) pharmacotherapy plan and monitoring, and (4) verbal communication of plan. The midterm and final examination scores were compared to determine how students progressed througout the course (Table 1). Students’ average scores for the pharmacotherapy plan and monitoring did improve, although not significantly. The average examination scores for data collection and interpretation did improve over time. In addition to the individual simulation evaluations, a midterm and final examination that included multiple-choice and short-answer items was administered.
Table 1.
Pharmacy Students’ Performance Scores in an Acute Care Simulation
P < 0.001
n = 13
Mean (SD)
Student Satisfaction Survey
A student satisfaction survey was administered online at the completion of the course to assess the students’ level of confidence in their abilities and their satisfaction with the learning environment. Students’ perceptions of the course were positive. In particular, students commented on the additive effect of the simulation learning above and beyond merely discussing a patient case in the classroom. Other student comments included enjoyment of the realistic setting the simulation provided, which made them feel more responsible for patient care, and the hands-on active learning.
Students’ open-ended comments also were positive as reflected by the following: “The simulations helped me to learn how to think clinically, to learn to ask the right questions, and to apply what we learned from lecture. I think this course is one of the most valuable courses I've taken in pharmacy school and I feel more prepared for rotations because of the experiences in the simulation room.”
DISCUSSION
This dual-immersive course provides an innovative, interactive educational environment that demonstrated improvement in students’ knowledge compared to online lectures alone, albeit in a small group of students. This assessment was conducted to demonstrate the potential benefit of a dual-immersive course rather than to prove that patient simulation is superior to lectures for learning. There was improvement in 9 out of 10 topic areas. There was no significant difference between scores for the pretest and posttest on sedation, but that test contained only 3 questions rather than 5 to 7 questions like the other quizzes. Improvement in critical thinking in the management of critically ill patients was demonstrated from midterm to final evaluation. The majority of students preferred this dual-immersion course, which provided a realistic hand-on learning environment, over traditional lecture-based learning. This type of learning was thoroughly enjoyed by the students potentially due to the immersion in the learning environment.
The skill set needed for contemporary pharmacy practice has expanded from simply the ability to dispense drugs to the knowledge and skills to optimize medication therapy management for patients. Pharmacists are required to solve medication-related problems using their knowledge and critical-thinking skills. This is especially important in the critical care environment where data are limited and medication therapy management can have a major impact on patient outcomes.14 The 2007 Accreditation Council for Pharmacy Education (ACPE) standards recommend that pharmacy faculty members should vary the learning methods and types of assessments used in the classroom.15 In June 2010, the ACPE Board of Directors provided the following statement on the use of simulation in pharmacy curricula: “The curriculum for a program's Introductory Pharmacy Practice Experiences (IPPE) may now include up to 60 hours (20% of the required 300 hours) of simulation. Simulation is defined as an activity or event that replicates pharmacy practice. Objective structure clinical evaluations (OSCEs), standardized patients, and high/medium fidelity manikins are all examples of approaches programs might take to simulate a patient care activity within an IPPE curriculum.”16 Simulation-based pharmacy education has continued to expand and is used in various areas of pharmacy curricula.2-5, 17-20 This technology affords a safe yet realistic environment in which the learner can observe the pharmacokinetic and pharmacodynamic properties of the medications they recommend. There are many benefits associated with incorporating patient simulation into education, and we maximized the use of this teaching method by combining it with self-study using online teaching modules.
Although the benefits of including patient simulation suggest it should be incorporated into the pharmacy curriculum whenever possible, there are barriers to implementing this technology. Because the cost of the mannequin often is a major consideration in the decision to include simulation education into a curriculum, college and schools should consider partnering with another college or department at their institution that has or wants to obtain patient simulation technology to defer some of the costs. Another consideration for courses with a large number of students is how to maximize each student's contact time with the patient simulator. One solution is dividing students into small groups for the patient simulation portion of the course. The faculty resources required to conduct multiple, simultaneous simulation sessions also may be a barrier and can be addressed by using senior students or residents to serve as facilitators.
This study had several limitations. Because this was an elective course, the students who enrolled may have been interested in patient simulation and/or self-directed learning and thus more motivated, and this may have resulted in more positive outcomes. However, we have shown similar improvements in students’ knowledge when we used patient simulation in a mandatory course within our curriculum.3,4 A final limitation to consider is that the improvement in students’ scores on the posttests compared to the pretests may have been the result of being tested on the same material a second time. Further investigation using a more rigorous study design is needed to prove definitively the benefit of simulation over other teaching methods.
SUMMARY
The implementation of dual immersive technologies of online learning and patient simulation improved learning and performance in a clinical setting and allowed for clarification, reiteration, and expansion on concepts learned by viewing online modules. By combining a self-directed Web-based technology with the immersion and realism of simulation, students’ problem-solving and critical-thinking skills improved.
ACKNOWLEDGEMENTS
This project was funded by the University of Pittsburgh Provost's Advisory Council on Instructional Excellence Innovation in Education Award for 2008-2009. The authors gratefully acknowledge the support of the Peter M. Winter Institute for Simulation, Education, and Research (WISER), and the Director, Paul Phrampus, MD. We also thank Lawrence Kobulinsky, simulation specialist for the WISER Institute, for programming the patient scenarios.
REFERENCES
- 1.Rodgers PL, Jacob H, Rashwan AS, et al. Quantifying learning in medical students during a critical care medicine elective: a comparison of three evaluation instruments. Crit Care Med. 2001;29(6):1268–1273. doi: 10.1097/00003246-200106000-00039. [DOI] [PubMed] [Google Scholar]
- 2.Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Assessment of pharmacy student response to use of patient simulation mannequins to teach performance-based pharmacotherapeutics: a novel approach. Am J Pharm Educ. 2006;70(3) doi: 10.5688/aj700348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seybert AL, Kobulinsky LR, McKaveney TM. Innovations in teaching award: simulation-based learning in pharmaceutical education. Am J Pharm Educ. 2008;72(2) doi: 10.5688/aj720237. Article 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ford DG, Seybert AL, Smithburger PL, Kobulinsky LR, Samosky JT, Kane-Gill SL. Clinical impact of simulation-based learning compared to traditional didactic lecturing on medication administration error rates in critically ill patients. Intensive Care Med. 2010;36(9):1526–1531. doi: 10.1007/s00134-010-1860-2. [DOI] [PubMed] [Google Scholar]
- 6.Weidman EK, Bell G, Walsh D, Small S, Edelson DP. Assessing the impact of immersive simulation on clinical performance during actual in-hospital cardiac arrest with CPR-sensing technology: a randomized feasibility study. Resuscitation. 2010;81(11):1556–1561. doi: 10.1016/j.resuscitation.2010.05.021. [DOI] [PubMed] [Google Scholar]
- 7.Barsuk JH, McGaghie WC, Cohen ER, et al. Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. Crit Care Med. 2009;37(10):2697–2701. [PubMed] [Google Scholar]
- 8.Barsuk JH, Cohen ER, Feinglass J, et al. Use of simulation-based education to reduce catheter-related bloodstream infections. Arch Intern Med. 2009;169(15):1420–1423. doi: 10.1001/archinternmed.2009.215. [DOI] [PubMed] [Google Scholar]
- 9.Draycott TJ, Crofts JF, Ash JP, et al. Improving neonatal outcome through practical shoulder dystocia training. Obstet Gynecol. 2008;112(1):14–20. doi: 10.1097/AOG.0b013e31817bbc61. [DOI] [PubMed] [Google Scholar]
- 10.Draycott TJ, Sibanda T, Owen L, et al. Does training in obstetric emergencies improve neonatal outcome? Br J Obstet Gynecol. 2006;113(2):177–182. doi: 10.1111/j.1471-0528.2006.00800.x. [DOI] [PubMed] [Google Scholar]
- 11.Cohen ER, Feinglass J, Barsuk JH, et al. Cost savings from reduced catheter-related bloodstream infection after simulation-based education for residents in a medical intensive care unit. Simul Healthc. 2010;5(2):98–102. doi: 10.1097/SIH.0b013e3181bc8304. [DOI] [PubMed] [Google Scholar]
- 12. Association of American Medical Colleges Institute for Improving Medical Education. Effective use of educational technology in medical education. Colloquium on Educational Technology: recommendations and guidelines for medical educators; 2007. https://services.aamc.org/Publications/showfile.cfm?file=version80.pdf&prd_id=184&prv_id=224&pdf_id=80. Accessed March 29, 2011.
- 13.Vincent JL. Give your patient a FAST HUG (at least) once a day. Crit Care Med. 2005;33(6):1225–1229. doi: 10.1097/01.ccm.0000165962.16682.46. [DOI] [PubMed] [Google Scholar]
- 14.Kane SL, Weber RJ, Dasta JF. The impact of critical care pharmacists on enhancing patient outcomes. Intensive Care Med. 2003;29(5):691–698. doi: 10.1007/s00134-003-1705-3. [DOI] [PubMed] [Google Scholar]
- 15. Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree, Standard 25.7. Chicago, Ill:2006. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf Accessed February 15, 2011. 2010.
- 16. ACPE Board Approves Changes to Professional Degree Program Policies and Procedures. ACPE Update: Assuring and Advancing Quality in Pharmacy Education. Volume 8, Issue 2; 2010. http://www.acpe-accredit.org/pdf/ACPE_Update.pdf. Accessed March 29, 2011.
- 17.Mieure KD, Vincent WR, 3rd, Cox MR, Jones MD. A high-fidelity simulation mannequin to introduce pharmacy students to advanced cardiovascular life support. Am J Pharm Educ. 2010;74(2) doi: 10.5688/aj740222. Article 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tofil NM, Benner KW, Worthington MA, et al. Use of simulation to enhance learning in a pediatric elective. Am J Pharm Educ. 2010;74(2) doi: 10.5688/aj740221. Article 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marken PA, Zimmerman C, Kennedy C, et al. Human simulators and standardized patients to teach difficult conversations to interprofessional health care teams. Am J Pharm Educ. 2010;74(7) doi: 10.5688/aj7407120. Article 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tokunage J, Takamura N, Ogata K, et al. Vital sign monitoring using human patient simulators at pharmacy schools in Japan. Am J Pharm Educ. 2010;74(7) doi: 10.5688/aj7407132. Article 132. [DOI] [PMC free article] [PubMed] [Google Scholar]