Abstract
Purpose/Background:
Patellofemoral pain syndrome (PFPS) is one of the most common and clinically challenging knee pathologies. Historically, clinicians have used a myriad of interventions, many of which have benefited some but not all patients. Suboptimal outcomes may reflect the need for an evidence-based approach for the treatment of PFPS. The authors believe that integrating clinical expertise with the most current scientific data will enhance clinical practice. The purpose of this systematic review is to provide an update on the evidence for the conservative treatment of PFPS.
Methods:
The PubMed, CINAHL, and SPORTDiscus databases were searched for studies published between January 1, 2000 and December 31, 2010. Studies used were any that utilized interventions lasting a minimum of 4 weeks for subjects with PFPS. Data were examined for subject sample, intervention duration, intervention type, and pain outcomes.
Results:
General quadriceps strengthening continues to reduce pain in patients with PFPS. Data are inconclusive regarding the use of patellar taping, patellar bracing, knee bracing, and foot orthosis. Although emerging data suggest the importance of hip strengthening exercise, ongoing investigations are needed to better understand its effect on PFPS.
Conclusions:
Current evidence supports the continued use of quadriceps exercise for the conservative management of PFPS. However, inconsistent or limited data regarding the other interventions precluded the authors' ability to make conclusive recommendations about their use. Future investigations should focus on identifying cohorts of patients with PFPS who may benefit from the other treatment approaches included in this systematic review.
Keywords: foot orthosis, hip exercise, knee, patella bracing, patella taping, quadriceps exercise
INTRODUCTION
Patellofemoral pain syndrome (PFPS) is one of the most common knee problems experienced by active adults and adolescents.1 Dye2 has described PFPS as an orthopedic “enigma” since it is one of the most challenging pathologies to manage. Historically, clinicians have used a myriad of interventions, many of which have little, if any, supporting evidence.3
Recently, much attention has focused on evidence-based practice. Sackett et al4 have defined evidence-based medicine as the “conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients.” They do not imply that clinicians make clinical decisions irrespective of past clinical experiences or practices. Rather, they emphasize the “integration of individual clinical expertise with the best available external clinical evidence from systematic research.”4
Murray et al3 determined that clinicians in a sports injury clinic implemented interventions based solely on personal experience in 44% of patients treated for PFPS. Moreover, clinicians used primary research evidence in only 24% of PFPS cases. These results provided preliminary data regarding the limited use of evidence-based medicine for this patient population.
Clinicians1,5 believe that PFPS results from abnormal patella tracking that leads to excessive compressive stress to the patellar facets. Factors that may contribute to abnormal patella tracking include quadriceps weakness, quadriceps muscle imbalances, excessive knee soft tissue tightness, an increased quadriceps angle (Q-angle), hip weakness, and altered foot kinematics. Based on this clinical theory, the aim for interventions used for the treatment of PFPS is to improve patella tracking and reduce abnormal stress to patellofemoral joint structures.
Most patients with PFPS respond well to conservative interventions6 and evidence7,8 supports the use of exercise for the treatment of PFPS. Kettunen et al9 recently compared outcomes for subjects with chronic PFPS who underwent arthroscopy followed by a home exercise program to similar subjects who only participated in a home exercise program. They found that all subjects, regardless of surgical or conservative treatment, reported similar significant functional improvements.
Researchers10–13 have described many approaches for the conservative treatment of PFPS. Specific vastus medialis obliquus (VMO) and general quadriceps exercises represent the most commonly used intervention. Historically, clinicians have prescribed specific VMO exercises on the premise that a delay and/or reduction in VMO activity relative to the vastus lateralis (VL) contributes to excessive lateral patella tracking. Although evidence14 questions selective VMO activation during exercise, general quadriceps strengthening does benefit many patients with PFPS and is considered the “gold” standard treatment.7,15
Other intervention strategies have incorporated patellar taping,12,16 patellar bracing,17 and knee bracing18 to further improve patella tracking. Although most subjects reported decreased pain when using these techniques, they also performed quadriceps strengthening exercises. Moreover, findings from some studies inferred limited, if any, additional benefit with patella taping16,19 or bracing18 over quadriceps exercise alone.
Another popular belief regarding PFPS etiology is an increased Q-angle causing the quadriceps to exert a greater lateral force vector and predispose the patella to excessive lateral tracking.20 This theory is not supported by the research findings, and many works21–23 have found no relationship between an increased Q-angle and PFPS. Reasons for these findings may reflect the poor reliability and validity associated with this measure.24 Another reason may reflect the static nature of this measure. Many patients with PFPS may demonstrate a normal Q-angle when assessed in a static manner. However, many of these patients may exhibit faulty lower extremity kinematics during dynamic activities like running, jumping, or single-leg landing that can increase the Q-angle.22
To address limitations with this static measure, Powers22,25 has described use of the dynamic Q-angle since it assesses changes during dynamic, weight bearing activities. He has theorized that increased femoral adduction (relative to the pelvis) and/or femoral internal rotation (relative to the pelvis) during weight bearing activities can impart a valgus knee force and stress lateral patellofemoral joint structures. With the use of kinematic magnetic resonance imaging (MRI), preliminary evidence26,27 has shown that subjects with PFPS demonstrated increased femoral internal rotation under a relatively stable patella during a single-leg squat. These findings provided a rationale for incorporating exercises that target the hip for patients with PFPS. Faulty foot mechanics also can affect the dynamic Q-angle. Tiberio28 theorized that excessive subtalar pronation can cause increased tibial internal rotation. Excessive tibial internal rotation would then require a greater amount of relative femoral internal rotation to extend the knee (i.e., the screw-home mechanism) during weight bearing activities. Lee and colleagues29,30 reported an association between increased lateral patellofemoral joint stress and excessive femoral internal rotation. Based on these findings, researchers have examined the use of hip strengthening10,31,32 and foot orthosis use33–35 for the treatment of PFPS.
Quadriceps strengthening exercise is the most commonly prescribed intervention. Although this approach may represent the therapist perceived “gold” standard, many patients continue to experience pain and dysfunction.11,36 This cohort of patients who may report a decrease, but not total resolution of pain following quadriceps exercise, may reflect the need to identify other evidence-supported strategies. Therefore, the purpose of this literature review is to provide an update on the evidence for the conservative treatment of PFPS. It is our intent that clinicians use information gained from this review for the development and implementation of evidence-based practice for this patient population.
METHODS
Data Sources
An electronic search was performed on PubMed, CINAHL, and SPORTDiscus databases from January 1, 2000 to December 31, 2010 using the following key words (either in isolation or in combination): patellofemoral pain syndrome, anterior knee pain, quadriceps exercise, quadriceps strength, hip exercise, hip strength, tape, taping, brace, bracing, orthosis, orthotics, and orthoses. A combined total of 878 articles were identified from the above-named data bases for review (Table 1).
Table 1.
Search strategy of pub MED, CINAHL, and SPORTDiscuss from January 1, 2000 through December31, 2010 to identify potential articles eligible for inclusion in the systematic review (all terms were separately entered into each database).
| Key Words | PubMed | CINAHL | SPORTDiscus | |
|---|---|---|---|---|
| 1 | Patellofemoral pain syndrome or anterior knee pain | 1,230 | 579 | 938 |
| 2 | Quadriceps exercise or strength | 1,270 | 46 | 25,220 |
| 3 | Hip exercise or strength | 2,013 | 9 | 25,791 |
| 4 | Tape or taping | 4,220 | 1,839 | 2,014 |
| 5 | Brace or bracing | 2,341 | 876 | 1,214 |
| 6 | Orthosis or orthotics or orthoses | 3,433 | 3,046 | 2,036 |
| 7 | 1 and 2 | 46 | 11 | 170 |
| 8 | 1 and 3 | 32 | 1 | 167 |
| 9 | 1 and 4 | 41 | 79 | 49 |
| 10 | l and 5 | 55 | 16 | 57 |
| 11 | l and 6 | 57 | 60 | 37 |
| Total potential articles to be included in the systematic review | 231 | 167 | 480 |
Study Selection
The authors selected evidence consistent with current relevant practice. To do this, the original search for evidence was limited and included only peer-reviewed manuscripts published within the past 10 years that utilized interventions lasting a minimum of 4 weeks. Studies not written in English, conference abstracts, theses, and dissertations were also excluded. Each researcher initially identified potential articles based on the abstract and confirmed appropriate inclusion by reviewing each article. The researchers discussed their search findings to ensure identification of relevant articles. Based on these criteria, the authors found 22 acceptable articles.
Data Extraction
The following data were extracted from each article: subject sample, intervention duration, intervention type, and pain outcomes. The authors also identified the research design used for each study (e.g., case study, quasi-experimental, or randomized control trial).
Data Synthesis
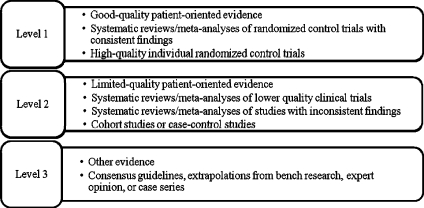
The quality of each study was evaluated using guidelines described by Ebell et al,37 who rate evidence for individual studies using a 3-level tier (Figure 1). The authors chose this taxonomy because it is patient-focused and allows the user to evaluate both a body of evidence and individual studies.
Figure 1.
Strength of Recommended Taxonomy (SORT) model37 used to evaluate the current evidence for the treatment of patients with patellofemoral pain syndrome.
According to the Philadelphia Panel Evidence-Based Clinical-Practice Guidelines,38 pain represents an important impairment associated with PFPS and was the one impairment consistently reported in all the identified studies. Therefore, changes in pain were used as the benchmark for assessing and comparing study results. Using the available data from each article, the percentage change on a visual analog scale was calculated that best represented usual pain (e.g., pain normally experienced over a week39), and the associated effect size for each intervention group was also reported (see Tables 2-6). Effect sizes were interpreted in the following manner:40 weak less than 0.40, moderate between 0.41 and 0.70, and strong greater than 0.70.
Table 2.
Summary of intervention studies aimed at hip strengthening.
| Study, Type, Level of Evidence | Intervention | % decrease in usual pain | Effect Size |
|---|---|---|---|
| Boling et al57 QE (Level 2)a | Weight bearing exercises that focused on quadriceps and hip abductor strengthening (1 group n=14) | 50 | .60 |
| Fukuda et al58 RCCT (Level 2)a | Group l(n=23): knee exercise only | 31 | .28 |
| Group 2 (n=20): knee and hip abductor and lateral rotator exercise | 42 | .54 | |
| Group 3 (n=21): control | −2† | .02 | |
| Mascal et al31 CS (Level 3)b | Recruitment and endurance training of the hip, pelvis, and trunk muscles (2 subjects) | Subject A: 100 | N/A |
| Subject B: 71 | |||
| Nakagawa et al32 RCPT (Level 2)a | Group l(n=7): non-weight bearing and weight bearing quadriceps strengthening | 15 | .13 |
| Group 2 (n=7): same as above plus transversus abdominus, hip abductor, and hip lateral rotator strengthening | 71 | .62 | |
| Tyler et al10 QE (Level 2)a | Non-weight bearing and weight bearing strengthening exercises designed to progressively strengthen the hip muscles (1 group n=35) | 45 | .96 |
CS = case study
QE = quasi-experimental
RCPT = randomized controlled pilot trial
RCCT = randomized control clinical trial
PFPS = patellofemoral pain syndrome
N/A = unable to calculate since study design did not allow for reported means or standard deviations
a = Level 2 (limited-quality patient-oriented evidence)
b = Level 3 (other evidence)
† Represents an increase in pain
Table 3.
Summary of intervention studies aimed at quadriceps strengthening.
| Study, Type, Level of Evidence | Intervention | % decrease in pain | Effect Size |
|---|---|---|---|
| Bakhtiary & Fatemi42 QE (Level 2)a | Group 1 (n=16): straight leg raise exercise | 26 | .31 |
| Group 2 (n=16): single-leg semi-squat exercise | 26 | .24 | |
| Bily et al45 RCIT (Level 2)a | Group l(n=18): combination of non-weight bearing and weight bearing hip and knee strengthening exercise82 | 75 | .50 |
| Group 2 (n=18): same exercise program as above plus 2 20-minute daily sessions of electrical stimulation | 73 | .50 | |
| Dursun et al46 RCT (Level 2)a | Group l(n=30): combination of non-weight bearing and weight bearing quadriceps exercise and stationary bike plus biofeedback | 84 | .93 |
| Group 2 (n=30): same as group 1 except no biofeedback | 90 | .93 | |
| Hazneci et al83 QE (Level 2)a | All subjects performed isokinetic knee extension exercise (1 group n=24) | 52 | .83 |
| Herrington & Al-Sherhi44 RCT (Level 2)a | Group l(n=15): non-weight bearing knee extension exercise | 44† | .56 |
| Group 2 (n=15): seated leg press exercise | 61† | .83 | |
| Group 3 (n=15): control | −20†β | .30 | |
| Loudon et al13 RCT (Level 2)a | Group 1 (n=9): combination of non-weight bearing and weight bearing exercise performed in a PT clinic | 59 | N/A |
| Group 2 (n=9): combination of non-weight bearing and weight bearing exercise performed as a home exercise program | 43 | ||
| Group 3 (n=11): control | 8 | ||
| Song et al43 RCT (Level 2)a | Group 1 (n=27): combined leg-press and hip adduction exercise | 45 | .42 |
| Group 2 (n=27): leg-press exercise | 53 | .48 | |
| Group 3 (n=25): control | 4 | .04 | |
| Syme et al41 RCT (Level 2)a | Group l(n=21): selective vastus medialis oblique exercise | 55 | .43 |
| Group 2 (n=22): general quadriceps femoris exercise | 45 | .37 | |
| Group 3 (n=20): control | 17 | .23 | |
| Witvrouw et al11 RCIT (Level 2)a | Group 1 (n=30): non-weight bearing knee extension exercise | 47 | .39 |
| Group 2 (n=30): weight bearing knee extension exercise | 54 | .43 | |
| Witvrouw et al66 PR (Level 2)a | Group 1 (n=24): non-weight bearing knee extension exercise | 71 | .59 |
| Group 2 (n=25): weight bearing knee extension exercise | 51 | .45 |
QE = quasi-experimental
RCT = randomized control trial
RCIT = randomized clinical trial
PR = prospective randomized
PFPS = patellofemoral pain syndrome
PT = physical therapy
N/A = unable to calculate since standard deviations were not reported
a = Level 2 (limited-quality patient-oriented evidence)
† Pain assessed using a 100-mm visual analog scale during a step-down test
β Represents an increase in pain
Table 4.
Summary of intervention studies incorporating patellar taping.
| Study, Type, Level of Evidence | Intervention | % decrease in pain | Effect Size |
|---|---|---|---|
| Clark et al47 RCT (Level 2)b | Group 1 (n=16): exercise, taping, and education | 53 | .54 |
| Group 2 (n=16): exercise and education | 61 | .49 | |
| Group 3 (n=18): taping and education | 31 | .32 | |
| Group 4(n=21): education | 21 | .39 | |
| Crossley et al12 RCT (Level l)a | Group 1 (n=36): exercise program and patellar taping | 77 | .81 |
| Group 2 (n=35): placebo program (sham US and taping) | 44 | .53 | |
| Whittingham et al48 RCT (Level 2)b | Group l(n=10): patella taping and exercise program | 100 | .98 |
| Group 2 (n=10): placebo taping and exercise program | 88 | .97 | |
| Group 3 (n=10): exercise program | 76 | .96 |
RCT = randomized control trial
PFPS = patellofemoral pain syndrome
PT = physical therapy
a = Level 1 (good-quality patient-oriented evidence)
b = Level 2 (limited-quality patient-oriented evidence)
Table 5.
Summary of intervention studies incorporating patellar and knee bracing
| Study, Type, Level of Evidence | Intervention | % decrease in pain | Effect Size |
|---|---|---|---|
| Lun et al77 QE (Level 2)a | Group 1 (n=34): home exercise program | 48 | .37 |
| Group 2(n=32): patellar bracing | 52 | .55 | |
| Group 3 (n=32): home exercise program with patellar bracing | 32 | .27 | |
| Group 4 (n=31): home exercise program with knee sleeve | 47 | .40 | |
| Denton et al18 RCIT (Level 2)a | Group 1 (n=17): weight bearing quadriceps exercise | 41% reported no pain during the step-up test at the end of the study 100% reported no pain during the step-up test at the end of the Study† | |
| Group 2 (n=17): weight bearing quadriceps exercise and Protonics™ brace | |||
QE = quasi-experimental
RCIT = randomized clinical trial
PFPS = patellofemoral pain syndrome
a = Level 2 (limited-quality patient-oriented evidence)
† Insufficient data reported to calculate % decrease in pain and effect size
Table 6.
Summary of intervention studies incorporating foot orthosis.
| Study, Type, Level of Evidence | Intervention | % decrease in pain | Effect Size |
|---|---|---|---|
| Collins et al33 RCT (Level l)a | Group 1 (n=39): orthoses and PT | 51 | .50 |
| Group 2(n=41): PT | 38 | .35 | |
| Group 3 (n=41): orthoses | 34 | .37 | |
| Group 4 (n=36): flat inserts | −2§ | .02 | |
| Johnston and Gross49 OBS (Level 2)b | All subjects wore a fabricated orthosis (n=16) | All subjects demonstrated significant improvements in all 3 WOMAC subscales of pain† | |
RCT = randomized control trial
OBS = observational study
PFPS = patellofemoral pain syndrome
PT = physical therapy
a = Level 1 (good-quality patient-oriented evidence)
b = Level 2 (limited-quality patient-oriented evidence)
† Insufficient data reported to calculate % decrease in pain and effect size
§ Subiects reported an increase in pain
RESULTS
Hip Strengthening Exercise
Five investigations (Table 2) specifically examined the use of hip strengthening for the treatment of subjects with PFPS. With the exception of the case study31 (Level 3 evidence), all met the criteria for a Level 2 evidence rating and provided sufficient data to calculate effect sizes for changes in usual pain. Results from all the studies showed that subjects who participated in an exercise program targeting the hip abductors and hip external rotators reported at least a moderate reduction in pain (effect sizes ranging from 0.54 to 0.62). Additionally, Tyler et al10 included hip extensor and hip flexor exercises and reported an even greater improvement in pain (effect size = 0.96).
Quadriceps Strengthening Exercise
Ten investigations (Table 3) met the inclusion criteria and all received a Level 2 evidence rating. Findings from most of the studies (8/10) suggested at least a moderate (effect size ranges ranging from 0.37 to 0.59) to strong (effect size ranges ranging from 0.83 to 0.93) improvement in pain when subjects performed either non-weight bearing or weight bearing quadriceps exercise. Although Syme et al41 found that controls who received no intervention reported 17% less pain, this difference represented a weak improvement (effect size=.23).
Conversely, Bakhtiary & Fatemi42 reported minimal changes in pain for subjects who performed either a supine straight leg raise exercise (effect size=0.31) or a single-leg squat exercise (effect size=0.24) protocol. It is noteworthy that their subjects performed a less demanding exercise program compared to others included in this review11,41,43,44 (e.g., subjects in other investigations performed a higher exercise volume).
Some investigators incorporated quadriceps electrical stimulation45 (effect size=0.50), biofeedback46 (effect size=0.93), or simultaneous hip adductor activation43 (effect size=0.42) with exercise, all of which provided no additional benefit from quadriceps exercise alone. Loudon et al13 only reported means but not standard deviations for their pain measures, which precluded our ability to calculate effect sizes. However, their subjects reported a 43% to 59% improvement in pain.
Patella Taping
Three studies (Table 4) that primarily used patella taping as an intervention met the established inclusion criteria. Crossley et al12 conducted the only study that met the Level 1 evidence criteria. This study was a randomized control trial that compared outcomes between subjects who received a true intervention (specialized exercise and corrective patella taping) and those who received a placebo intervention (sham ultrasound and loosely applied tape). Subjects in the treatment group experienced a strong reduction in pain (effect size=0.81). Although not expected to receive benefit from the placebo intervention, controls reported a moderate improvement in pain (effect size=0.53). Studies by Clark et al47 and Whittingham et al48 received a Level 2 evidence rating. They found that subjects who participated in quadriceps exercise in combination with either correctly or loosely applied tape reported a moderate-to-strong reduction in pain (effect sizes ranging from 0.54 to 0.98).
Patella Bracing and Knee Bracing
Two studies, both with Level 2 evidence ratings, met our inclusion criteria for patella bracing and knee bracing (Table 5). Lun et al17 found moderate improvements in pain with the use of either a patella brace (effect size=0.55) or a neoprene knee sleeve (effect size=0.40). In contrast to other findings11,41,43,44 regarding quadriceps exercise, they also found limited support for a home exercise program (effect size=0.37) or a home exercise program in combination with patella bracing (effect size=0.27).
Denton et al18 compared the use of the Protonics™ knee brace system to a traditional weight bearing quadriceps program. They did not assess pain in the same manner as the other studies (e.g. visual analog scale for usual pain) nor did they provide sufficient data to calculate effect sizes. However, Denton et al assessed pain during a step-down test (without bracing) and reported that subjects who performed exercise with the Protonics™ brace reported no pain during the step-down test following a 6-week intervention. Forty-one percent of the subjects who performed quadriceps exercise without the brace reported no pain during the same test.
Foot Orthosis
Collins et al33 conducted the only randomized clinical trial (Level 1 evidence) to investigate foot orthosis use (Table 6). They divided a total of 157 subjects into one of the following groups: 1) corrective orthosis use and physical therapy exercise, 2) physical therapy exercise, 3) corrective orthosis use, and 4) flat insert use. Subjects who received corrective orthosis use and physical therapy exercise reported a moderate improvement in pain (effect size=0.50). However, weak improvements in pain occurred in subjects who only received corrective orthosis use (effect size =0.37) or physical therapy exercise (effect size=0.35). Subjects who only wore a flat insole reported a 2% increase in pain (effect size=0.02).
Johnston and Gross49 examined the effect of foot orthoses on pain by issuing study participants custom-made foot orthoses. They assessed pain using the Western Ontario and McMaster Universities Arthritis Index (WOMAC) subscales of pain. All subjects reported decreased pain at the 3-month assessment period. The investigators did not provide sufficient data to calculate percentage changes in pain or effect sizes.
DISCUSSION
PFPS is one of the most common and most challenging knee pathologies to manage. Unlike anterior cruciate ligament injury, which has a specific mechanism of injury and treatment approach, patients with PFPS receive various interventions. Overall, this review of the existing evidence showed that many treatment strategies may benefit these patients. While quadriceps exercise remained an important intervention, this review also supported the addition of hip strengthening. Evidence for other popular interventions, such as patellar taping, patellar bracing, knee bracing, and foot orthosis prescription, appeared to be less efficacious than exercise alone. The following sections explain these findings and provide clinical suggestions for integrating current evidence into clinical practice.
Hip Strengthening Exercise
Computer simulation50 and cadaveric models29,30 have shown that excessive hip adduction and/or excessive hip internal rotation can stress lateral patellofemoral joint structures as these motion increase the force applied to this area. These findings have led to subsequent studies examining hip function in patients with PFPS. Souza and Powers51 recently used traditional MRI to compare femoral structure (angle of inclination and torsion), muscle performance, and kinematics during running in this patient population. Overall, subjects with PFPS exhibited a 4.4° higher femoral angle of inclination but similar femoral anteversion as controls. They also demonstrated hip weakness and greater femoral internal rotation during running, which they speculated would lead to increased lateral patellofemoral joint stress as shown in computer simulation50 and cadaveric models.29,30 Step-wise regression revealed that decreased isotonic hip extensor endurance, not femoral structure, was the only predictor of increased hip internal rotation. These findings highlighted the importance of hip muscle performance to control femoral motion and corroborated results from other investigations that have reported decreased hip strength and altered lower extremity kinematics in this patient population.52–56
The findings of the current review showed that hip strengthening exercise can benefit individuals with PFPS. Moderate evidence32,57,58 supports the use of hip abductor and external rotator strengthening, which may be further enhanced with the inclusion of exercises targeting hip flexion10 and hip extension.10 Although all works prescribed exercise for strengthening effects (i.e., 3 sets of 10 to 15 repetitions), emerging evidence51,56 has suggested the need to address muscle endurance. Therefore, clinicians should consider exercise dosage focusing on higher repetitions (i.e. 3 sets of 20 to 30 repetitions), especially in patients who participate in more demanding activities like running and jumping.
A limitation of most studies included in this review was a lack of attention toward neuromuscular factors such as activation amplitudes and timing differences between the hip and knee muscles. Preliminary evidence59,60 has inferred a potential delay in gluteus medius activation relative to the quadriceps that could affect hip function. Future investigations should examine the role of neuromuscular factors as well as changes in these factors following a hip exercise program.61
Quadriceps Strengthening
Patients with PFPS historically have exhibited quadriceps weakness thought to contribute to abnormal patella tracking and patellofemoral joint irritation.62 Another possible contributing factor may be a reduction and/or delay in VMO activity relative to the VL that can cause excessive lateral patella tracking. To date, conflicting findings have existed as some researchers57,63,64 have reported a reduction and/or delay in VMO onset whereas others59,65 have not corroborated this pattern. Even if VMO dysfunction exists, consistent data have not supported selective activation of the VMO during exercise.14
Findings agree with prior works regarding the importance of both weight bearing11,66 and non-weight bearing67–69 quadriceps strengthening for the treatment of PFPS. Consistent improvements in pain existed for subjects who performed general quadriceps strengthening exercises either in a weight bearing or non-weight bearing position. While clinicians may prefer weight bearing exercises that simulate functional activities, the use of non-weight bearing exercise may be equally beneficial, especially in patients with marked quadriceps weakness.
A key point to remember is that patients exercise in a pain-free manner.15,70 Clinicians should consider biomechanical stresses applied to the patellofemoral joint during non-weight bearing and weight bearing exercise. Patellofemoral joint stress is less from 90 to 45 degrees of knee flexion during non-weight bearing exercise and less from 45 to 0 degrees of knee flexion during weight bearing exercise.71 Finally, the additional use of neuromuscular electrical stimulation45 or biofeedback46 has no greater effect on pain than general quadriceps exercise alone.
Patella Taping
Patella taping is another intervention used to facilitate optimal patella alignment and tracking within the femoral trochlea. Often times, clinicians don tape to a patient's patella prior to exercise in hopes of decreasing pain and increasing VMO activation.
The results of this review support the use of taping in conjunction with exercise at least for the short-term treatment for PFPS. The mechanism by which patella taping may reduce symptoms remains elusive. Although initially theorized to improve patella alignment, prior works72,73 have shown taping to be ineffective for maintaining alignment during or immediately following exercise. Therefore, subjects may benefit from taping for proprioceptive input or neuromuscular control during the time of use.74
Taping also may modulate pain74 to enable a patient to perform pain-free quadriceps exercise. Using MRI to assess patella kinematics, Derasari et al75 assessed 3 displacements (medial-lateral, superior-inferior, and posterior-anterior) and 3 rotations (lateral-medial tilt, extension-flexion, and posterior-anterior) in subjects with PFPS before and after McConnell taping. They found that taping primarily resulted in an inferior shift of the patella within the femoral trochlea. Increasing patella contact within the trochlea would reduce patellofemoral stress and may partially explain the positive results with tape use.
Interestingly, results from this review indicated that the manner of tape application (i.e. either applied in a corrective manner or applied loosely) may not necessarily influence its beneficial effects.12,48 Therefore, taping may have an important effect on the neuromuscular system rather than actually altering patella movement.
The results of this review did not support the use of taping over exercise alone since exercise appeared to be an important factor.12,13,47 It is noteworthy that taping has minimal effect in treating long-term symptoms associated with PFPS.47 Therefore, clinicians may consider patella taping on a short-term basis as needed to enable patients to perform pain-free exercise.
Patellar Bracing and Knee Bracing
Similar to taping, clinicians have used both patellar and knee bracing to prevent or correct patella malalignment within the femoral trochlea. Powers et al76 examined pain and patella contact area in subjects with PFPS who donned the On-Track® (DJO, Vista, CA) and Patellar Tracking Orthosis® (BREG, Inc., Vista, CA) patella braces. They reported that all subjects reported less pain with brace use and that MRI revealed increased patella contact area with brace use. Powers et al concluded that bracing may have shifted patella contact within the femoral trochlea from areas of irritation to non-irritation. These findings may explain why Lun et al77 reported a moderate pain reduction in subjects who only wore a patellar brace.
The Protonics™ knee brace (Empi, St. Paul, MN) was the only knee brace included in this review. The brace was developed on the premise that iliopsoas and tensor fascia lata hypertonicity can lead to iliotibial band tightness and excessive lateral patella tracking.78 Based on principles of reciprocal inhibition, the brace manufacturer designed the brace to promote hamstring activation in order to normalize iliopsoas and tensor fascia lata tone.
The brace also is designed to produce a variable degree of a knee-extension moment. The manufacturer theorizes that pain occurs from increased patellofemoral joint compression from quadriceps activity. The knee-extension moment generated from brace use enables patients to perform weight bearing activities in a pain-free manner by reducing the amount of the quadriceps-produced compressive force. As patients demonstrate less patellofemoral joint irritation, the brace can be adjusted to provide a lower knee-extension moment and require a greater degree of quadriceps activity.
The current findings suggest that the Protonics™ knee brace may be an effective intervention to reduce pain. Like patellar taping, the exact mechanism for improvement remains unclear. Possible reasons for favorable outcomes may include redistributed patella stress, enhanced proprioceptive input, and improved neuromuscular control that allow subjects to perform pain-free quadriceps exercise. Additional studies are needed to conclusively determine the isolated benefits of the Protonics™ brace compared to pain-free exercise alone.18
Foot Orthosis
Although clinicians routinely prescribe foot orthoses to minimize faulty lower extremity kinematics, few researchers33,49 have examined foot orthosis use for the treatment of PFPS over the past 10 years. Moreover, the exact mechanism for pain relief remains elusive.79
No study included in this review examined kinematic changes during or following foot orthosis use, which limits the authors' ability to determine an exact mechanism of change with wear. However, Barton et al79 found very limited evidence for a foot orthosis to modify knee transverse plane kinematics for subjects with PFPS. Furthermore, prospective investigations80,81 have found inconsistent findings regarding an absolute relationship between increased foot pronation and the development of PFPS. Boling et al23 identified increased navicular drop as a significant risk factor for developing PFPS. These findings suggested that correction of excessive pronation would benefit this patient population. Conversely, Thijs and colleagues80,81 reported ambulation in a less pronated foot position as a predictor of PFPS. They concluded that the inability of the lower extremity to attenuate impact shock may contribute more to PFPS etiology. In summary, data gained from prospective studies suggest that PFPS may develop from either excessive or limited pronation.
Additional studies are needed to determine if foot orthosis use minimizes pain due to changes in kinematics (excessive pronation), kinetics (shock attenuation), or a combination of both. Moreover, evidence is needed to identify a cohort of patients likely to benefit from a foot orthosis. While isolated foot orthosis use may benefit some patients with PFPS,33,49 evidence gained from this systematic review suggests that orthosis use can augment the effects of exercise.79
Future Research
Results from this systematic review support the continued use of quadriceps exercise and the incorporation of hip strengthening exercise. However, no data exist that conclusively confirm the effectiveness of isolated hip exercise over isolated quadriceps exercise. The author's findings also showed that certain interventions may benefit some but not all patients with PFPS. Information gained from this systematic review highlights the need to determine the isolated effects of hip strengthening on PFPS as well as identify specific cohorts of patients who may benefit from a specific intervention.
CONCLUSION
The purpose of this systematic review was to provide an update on the evidence for the conservative treatment of PFPS. Quadriceps exercise continues to represent an important treatment strategy. The results of this systematic review also support the addition of hip strengthening exercise. Clinicians have used biofeedback, patella taping, and foot orthoses as interventions for this patient population, and findings from this systematic review suggest that these strategies may augment the benefits gained from quadriceps exercise. Insufficient data regarding patella bracing limits the authors's ability to make a recommendation for its use.
REFERENCES
- 1. Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30(3):447–456 [DOI] [PubMed] [Google Scholar]
- 2. Dye SF. Patellofemoral pain current concepts: An overview. Sports Med Arthrosc Rev. 2001;9:264–272 [Google Scholar]
- 3. Murray IR, Murray SA, MacKenzie K, Coleman S. How evidence based is the management of two common sports injuries in a sports injury clinic? Br J Sports Med. 2005;39:912–916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312:71–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Doucette SA, Goble EM. The effect of exercise on patellar tracking in lateral patellar compression syndrome. Am J Phys Med Rehabil. 1992;20(4):434–440 [DOI] [PubMed] [Google Scholar]
- 6. Bizzini M, Childs JD, Piva SR, Delitto A. Systematic review of the quality of randomized controlled trials for patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2003;33(1):4–20 [DOI] [PubMed] [Google Scholar]
- 7. Natri A, Kannus P, Jarvinen M. Which factors predict the long-term outcome in chronic patellofemoral pain syndrome? A 7-yr prospective follow-up study. Med Sci Sports Exerc. 1998;30:1572–1577 [DOI] [PubMed] [Google Scholar]
- 8. Barton CJ, Webster KE, Menz HB. Evaluation of the scope and quality of systematic reviews on the nonpharmacological conservative treatment of patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008;38(9):529–541 [DOI] [PubMed] [Google Scholar]
- 9. Kettunen JA, Harilainen A, Sandelin J, et al. Knee arthroscopy and exercise versus exercise only for chronic patellofemoral pain syndrome: a randomized controlled trial. BMC. 2007;5:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tyler TF, Nicholas SJ, Mullaney MJ, McHugh MP. The role of hip muscle function in the treatment of patellofemoral pain syndrome. Am J Sports Med. 2006;34(4):630–636 [DOI] [PubMed] [Google Scholar]
- 11. Witvrouw E, Lysens R, Bellemans J, Peers K, Vanderstraeten G. Open versus closed kinetic chain exercises for patellofemoral pain. Am J Sports Med. 2000;28(5):687–694 [DOI] [PubMed] [Google Scholar]
- 12. Crossley KM, Bennell KL, Green S, Cowan SM, McConnell J. Physical therapy for patellofemoral pain. A randomized, double-blinded, placebo-controlled trial. Am J Sports Med. 2002;30(6):857–865 [DOI] [PubMed] [Google Scholar]
- 13. Loudon JK, Gajewski B, Goist-Foley HL, Loudon KL. The effectiveness of exercise in treating patellofemoral-pain syndrome. J Sport Rehabil. 2004;13:323–342 [Google Scholar]
- 14. Davies GJ, Manske RC, Cooley K, Fletcher-Klos D, Johnson-Stuhr P. Selective activation of the vastus medialis oblique: What does the literature really tell us? Physiother Can. 2001;53(2):136–151 [Google Scholar]
- 15. Bolgla LA, Malone TR. Exercise prescription and patellofemoral pain: evidence for rehabilitation. J Sport Rehabil. 2005;14(1):72–88 [DOI] [PubMed] [Google Scholar]
- 16. Kowall MG, Kolk G, Nuber GW, Cassisi JE, Stern SH. Patellar taping in the treatment of patellofemoral pain. A prospective randomized study. Am J Sports Med. 1996;24(1):61–66 [DOI] [PubMed] [Google Scholar]
- 17. Lun VM, Wiley JP, Meeuwisse WH, Yanagawa TL. Effectiveness of patellar bracing for treatment of patellofemoral pain syndrome. Clin J Sport Med. 2005;15(4):235–240 [DOI] [PubMed] [Google Scholar]
- 18. Denton J, Willson JD, Ballantyne BT, Davis IS. The addition of the Protonics brace system to a rehabilitation protocol to address patellofemoral joint syndrome. J Orthop Sports Phys Ther. 2005;35(4):210–219 [DOI] [PubMed] [Google Scholar]
- 19. Harrison EI, Sheppard MS, McQuarrie AM. A randomized controlled trial of physical therapy treatment programs in patellofemoral pain syndrome. Physiother Can. 1999;51(2):93–100 [Google Scholar]
- 20. Powers CM, Chen PY, Reischl SF, Perry J. Comparison of foot rotation and lower extremity rotation in persons with and without patellofemoral pain. Foot Ankle Int. 2002;23(7):634–640 [DOI] [PubMed] [Google Scholar]
- 21. Herrington L, Nester C. Q-angle undervalued? The relationship between Q-angle and medio-lateral position of the patella. Clin Biomech. 2004;19:1070–1073 [DOI] [PubMed] [Google Scholar]
- 22. Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: A theoretical perspective. J Orthop Sports Phys Ther. 2003;33(11):639–646 [DOI] [PubMed] [Google Scholar]
- 23. Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med. 2009;37(11):2108–2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Smith TO, Hunt NJ, Donell ST. The reliability and validity of the Q-angle: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2008;16:1068–1079 [DOI] [PubMed] [Google Scholar]
- 25. Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40(2):42–51 [DOI] [PubMed] [Google Scholar]
- 26. Souza R, B., Draper CE, Fredericson M, Powers CM. Femur rotation and patellofemoral joint kinematics: a weight-bearing magnetic resonance imaging analysis. J Orthop Sports Phys Ther. 2010;40(5):277–285 [DOI] [PubMed] [Google Scholar]
- 27. Powers CM, Ward SR, Fredericson M, Guillet M, Shellock FG. Patellofemoral kinematics during weight-bearing and non-weight-bearing knee extension in persons with lateral subluxation of the patella: A preliminary study. J Orthop Sports Phys Ther. 2003;33(11):677–685 [DOI] [PubMed] [Google Scholar]
- 28. Tiberio D. The effect of excessive subtalar joint pronation on patellofemoral mechanics: A theoretical model. J Orthop Sports Phys Ther. 1987;9(4):160–165 [DOI] [PubMed] [Google Scholar]
- 29. Lee TQ, Anzel SH, Bennett KA, Pang D, Kim WC. The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clin Orthop. 1994:69–74 [PubMed] [Google Scholar]
- 30. Lee TQ, Morris G, Csintalan RP. The influence of tibial and femoral rotation on patellofemoral contact area and pressure. J Orthop Sports Phys Ther. 2003;33(11):686–693 [DOI] [PubMed] [Google Scholar]
- 31. Mascal CL, Landel R, Powers CM. Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: 2 case reports. J Orthop Sports Phys Ther. 2003;33(11):647–660 [DOI] [PubMed] [Google Scholar]
- 32. Nakagawa TH, Muniz TB, de Marche Baldon R, Marciel CD, de Menezes Reiff RB, Serrao FV. The effect of additional strengthening of hip abductor and lateral rotator muscles in patellofemoral pain syndrome: a randomized controlled pilot study. Clin Rehabil. 2008;22:1051–1060 [DOI] [PubMed] [Google Scholar]
- 33. Collins N, Crossley KM, Beller E, Darnell R, McPoil T, Vicenzino B. Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: randomised clinical trial. Br J Sports Med. 2009;43(3):169–171 [DOI] [PubMed] [Google Scholar]
- 34. Way MC. Effects of a thermoplastic foot orthosis on patellofemoral pain in a collegiate athlete: A single-subject design. J Orthop Sports Phys Ther. 1999;29(6):331–338 [DOI] [PubMed] [Google Scholar]
- 35. Sutlive TG, Mitchell SD, Maxfield SN, et al. Identification of individuals with patellofemoral pain whose symptoms improved after a combined program of foot orthosis use and modified activity: a preliminary investigation. Phys Ther. 2004;84(1):49–61 [PubMed] [Google Scholar]
- 36. Nimon G, Murray D, Sandow M, Goodfellow J. Natural history of anterior knee pain: a 14- to 20-year follow-up of nonoperative management. J Pediatr Orthop. 1998;18(1):118–122 [PubMed] [Google Scholar]
- 37. Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. Am Fam Physician. 2004;69(3):548–556 [PubMed] [Google Scholar]
- 38. Philadelphia Panel Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions for knee pain. Phys Ther. 2001;81(10):1675–1700 [PubMed] [Google Scholar]
- 39. Crossley KM, Bennell KL, Cowan SM, Green S. Analysis of outcome measures for persons with patellofemoral pain: Which are reliable and valid? Arch Phys Med Rehabil. 2004;85:815–822 [DOI] [PubMed] [Google Scholar]
- 40. Cohen J. Statistical Power Analysis for Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988 [Google Scholar]
- 41. Syme G, Rowe P, Martin D, Daly G. Disability in patients with chronic patellofemoral pain syndrome: a randomised controlled trial of VMO selective training versus general quadriceps strengthening. Manual Ther. 2009;14:252–263 [DOI] [PubMed] [Google Scholar]
- 42. Bakhtiary AH, Fatemi E. Open versus closed kinetic chain exercises for patellar chondromalacia. Br J Sports Med. 2008;42:99–102 [DOI] [PubMed] [Google Scholar]
- 43. Song C, Lin Y, Wei T, Lin D, Yen T, Jan M. Surplus value of hip adduction in leg-press exercise in patients with patellofemoral pain syndrome: a randomized controlled trial. Phys Ther. 2009;89(5):409–418 [DOI] [PubMed] [Google Scholar]
- 44. Herrington L, Al-Sherhi A. A controlled trial of weight-bearing versus non-weight-bearing exercises for patellofemoral pain. J Orthop Sports Phys Ther. 2007;37(4):155–160 [DOI] [PubMed] [Google Scholar]
- 45. Bily W, Trimmel L, Modlin M, Kaider A, Kern H. Training program and additional electric muscle stimulation for patellofemoral pain syndrome: a pilot study. Arch Phys Med Rehabil. 2008;89:1230–1236 [DOI] [PubMed] [Google Scholar]
- 46. Dursun N, Dursun E, Kilic Z. Electromyographic biofeedback- Controlled exercise versus conservative care for patellofemoral pain syndrome. Arch Phys Med Rehabil. 2001;82:1692–1695 [DOI] [PubMed] [Google Scholar]
- 47. Clark DI, Downing N, Mitchell J, Coulson L, Syzpryt EP, Doherty M. Physiotherapy for anterior knee pain: A randomised controlled trial. Ann Rheumat Dis. 2000;59:700–704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Whittingham M, Palmer S, Macmillan F. Effects of taping on pain and function in patellofemoral pain syndrome: a randomized controlled trial. J Orthop Sports Phys Ther. 2004;34(9):504–510 [DOI] [PubMed] [Google Scholar]
- 49. Johnston LB, Gross MT. Effects of foot orthoses on quality of life for individuals with patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2004;34(8):440–448 [DOI] [PubMed] [Google Scholar]
- 50. Elias JJ, Cech JA, Weinstein DM, Cosgrea AJ. Reducing the lateral force acting on the patella does not consistently decrease patellofemoral pressures. Am J Sports Med. 2004;32(5):1202–1208 [DOI] [PubMed] [Google Scholar]
- 51. Souza RB, Powers CM. Predictors of hip internal rotation during running: an evaluation of hip strength and femoral structure in women with and without patellofemoral pain. Am J Sports Med. 2009;37 579–587 [DOI] [PubMed] [Google Scholar]
- 52. Ireland ML, Willson JD, Ballantyne BT, Davis IM. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33(11):671–676 [DOI] [PubMed] [Google Scholar]
- 53. Prins MR, van der Wurff P. Females with patellofemoral pain syndrome have weak hip muscles. a systematic review. Aust J Physiother. 2009;55:9–15 [DOI] [PubMed] [Google Scholar]
- 54. Souza RB, Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39(1):12–19 [DOI] [PubMed] [Google Scholar]
- 55. Willson JD, Davis I. Lower extremity strength and mechanics during jumping in women with patellofemoral pain. J Sport Rehabil. 2009;18(1):75–89 [DOI] [PubMed] [Google Scholar]
- 56. Dierks TA, Manal KT, Hamill J, Davis IS. Proximal and distal influences on hip and knee kinematics in runners with patellofemoral pain during a prolonged run. J Orthop Sports Phys Ther. 2008;38(8):448–456 [DOI] [PubMed] [Google Scholar]
- 57. Boling MC, Bolgla LA, Mattacola CG, Uhl TL, Hosey RG. Outcomes of a weight-bearing rehabilitation program for patients diagnosed with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2006;87(11):1428–1435 [DOI] [PubMed] [Google Scholar]
- 58. Fukuda TY, Rossetto FM, Magalhães E, Bryk FF, Lucareli PR, de Almeida Aparecida Carvalho N. Short-term effects of hip abductors and lateral rotators strengthening in females with patellofemoral pain syndrome: a randomized controlled clinical trial. J Orthop Sports Phys Ther. 2010;40(11):736–742 [DOI] [PubMed] [Google Scholar]
- 59. Brindle TJ, Mattacola CG, McCrory JL. Electromyographic changes in the gluteus medius during stair ascent and descent in subjects with anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 2003;11:244–251 [DOI] [PubMed] [Google Scholar]
- 60. Cowan SM, Crossley KM, Bennell KL. Altered hip and trunk muscle function in individuals with patellofemoral pain syndrome. Br J Sports Med. 2009;43:584–588 [DOI] [PubMed] [Google Scholar]
- 61. Heiderscheit BC. Lower extremity injuries: is it just about hip strength? J Orthop Sports Phys Ther. 2010;40(2):39–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Powers CM, Perry J, Hsu A, Hislop HJ. Are patellofemoral pain and quadricpes strength associated with locomotor function? Phys Ther. 1997;77:1063–1074 [DOI] [PubMed] [Google Scholar]
- 63. Cowan SM, Bennell KL, Hodges PW, Crossley KM, McConnell J. Delayed onset of electromyographic activity of vastus medialis obliquus relative to vastus lateralis in subjects with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2001;82:183–189 [DOI] [PubMed] [Google Scholar]
- 64. Cowan SM, Bennell KL, Crossley KM, Hodges PW, McConnell J. Physical therapy alters recruitment of the vasti in patellofemoral pain syndrome. Med Sci Sports Exerc. 2002;34(12):1879–1885 [DOI] [PubMed] [Google Scholar]
- 65. Owings TM, Grabiner MD. Motor control of the vastus medialis oblique and vastus lateralis muscles is disrupted during eccentric contractions in subjects with patellofemoral pain. Am J Sports Med. 2002;30(4):483–487 [DOI] [PubMed] [Google Scholar]
- 66. Witvrouw E, Danneels L, van Tiggelen D, Willems TM, Cambier D. Open versus closed kinetic chain exercise in patellofemoral pain. A 5-year prospective randomized study. Am J Sports Med. 2004;32(5):1122–1129 [DOI] [PubMed] [Google Scholar]
- 67. McMullen W, Roncarati A, Koval P. Static and isokinetic treatments of chondromalacia patella: A comparative investigation. J Orthop Sports Phys Ther. 1990;12(6):256–266 [DOI] [PubMed] [Google Scholar]
- 68. Stiene HA, Brosky T, Reinking MF, Nyland J, Mason MB. A comparison of closed kinetic chain and isokinetic joint isolation exercise in patients with patellofemoral dysfunction. J Orthop Sports Phys Ther. 1996;24(3):136–141 [DOI] [PubMed] [Google Scholar]
- 69. Alaca R, Yilmaz B, Goktepe AS, Mohur H, Kalyon TA. Efficacy of isokinetic exercise on functional capacity and pain in patellofemoral pain syndrome. Am J Phys Med Rehabil. 2002;81(11):807–813 [DOI] [PubMed] [Google Scholar]
- 70. Dye SF. Therapeutic implications of a tissue homeostasis approach to patellofemoral pain. Sports Med Arthrosc Rev. 2001;9:306–311 [Google Scholar]
- 71. Steinkamp LA, Dillingham MF, Markel MD, Hill JA, Kaufmen KR. Biomechanical considerations in patellofemoral joint rehabilitation. Am J Sports Med. 1993;21:438–446 [DOI] [PubMed] [Google Scholar]
- 72. Gigante A, Pasquinelli FM, Paladini P, Ulisse S, Greco F. The effects of patellar taping on patellofemoral incongruence. A computed tomography study. Am J Sports Med. 2001;29(1):88–92 [DOI] [PubMed] [Google Scholar]
- 73. Pfeiffer RP, DeBeliso M, Shea KG, Kelley L, Irmischer B, Harris C. Kinematic MRI assessment of McConnell taping before and after exercise. Am J Sports Med. 2004;32(3):621–628 [DOI] [PubMed] [Google Scholar]
- 74. Aminaka N, Gribble PA. Patellar taping, patellofemoral pain syndrome, lower extremity kinematics, and dynamic postural control. J Athl Train. 2008;43(1):21–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Derasari A, Brindle TJ, Alter KE, Sheehan FT. McConnell taping shifts the patella inferiorly in patients with patellofemoral pain: a dynamic magnetic resonance imaging study. Phys Ther. 2010;90(3):411–419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Powers CM, Ward SR, Chan LD, Chen YJ, Terk MR. The effect of bracing on patella alignment and patellofemoral joint contact area. Med Sci Sports Exer. 2004;36(7):1226–1232 [DOI] [PubMed] [Google Scholar]
- 77. Lun VM, Wiley JP, Meeuwisse WH, Yanagawa TL. Effectiveness of patellar bracing for treatment of patellofemoral pain syndrome. Clin J Sports Med. 2005;15(4):235–240 [DOI] [PubMed] [Google Scholar]
- 78. Sahrmann SA. Movement impairment syndromes at the hip. Diagnosis and Treatment of Movement Impairment Syndromes. St. Louis: Mosby, Inc.; 2002:121–193 [Google Scholar]
- 79. Barton CJ, Munteanu SE, Menz HB, Crossley KM. The efficacy of foot orthoses in the treatment of individuals with patellofemoral pain syndrome: a systematic review. Sports Med. 2010;40(5):377–395 [DOI] [PubMed] [Google Scholar]
- 80. Thijs Y, Van Tiggelen D, Roosen P, De Clercq D, Witvrouw E. A prospective study on gait-related intrinsic risk factors for patellofemoral pain. Clin J Sport Med. 2007;17(6):437–445 [DOI] [PubMed] [Google Scholar]
- 81. Thijs Y, De Clercq D, Roosen P, Witvrouw E. Gait-related intrinsic risk factors for patellofemoral pain in novice recreational runners. Br J Sports Med. 2008;42(6):466–471 [DOI] [PubMed] [Google Scholar]
- 82. Thomee R. A comprehensive treatment approach for patellofemoral pain syndrome in young women. Phys Ther. 1997;77(12):1690–1703 [DOI] [PubMed] [Google Scholar]
- 83. Hazneci B, Yildiz Y, Sekir U, Atdin T, Kalyon TA. Efficacy of isokinetic exercise on joint position sense and muscle strength in patellofemoral pain syndrome. Am J Phys Med Rehabil. 2005;84(7):521–527 [DOI] [PubMed] [Google Scholar]