Abstract
Summary
Background and objectives
Although limited health literacy is estimated to affect over 90 million Americans and is recognized as an important public health concern, there have been few studies examining this issue in patients with chronic kidney disease. We sought to characterize the prevalence of and associations of demographic and clinical characteristics with limited health literacy in patients receiving maintenance hemodialysis.
Design, setting, participants, & measurements
As part of a prospective clinical trial of symptom management strategies in 288 patients treated with chronic hemodialysis, we assessed health literacy using the Rapid Estimate of Adult Literacy in Medicine (REALM). We defined limited health literacy as a REALM score ≤60 and evaluated independent associations of demographic and baseline clinical characteristics with limited health literacy using multivariable logistic regression.
Results
Of the 260 patients who completed the REALM, 41 demonstrated limited health literacy. African-American race, lower educational level, and veteran status were independently associated with limited health literacy. There was no association of limited health literacy with age, gender, serologic values, dialysis adequacy, overall symptom burden, quality of life, or depression.
Conclusions
Limited health literacy is common among patients receiving chronic hemodialysis. African-American race and socioeconomic factors are strong independent predictors of limited health literacy. These findings can help inform the design and implementation of interventions to improve health literacy in the hemodialysis population.
Introduction
Health literacy is the ability to obtain, process, and understand health information to make appropriate health decisions (1). Limited health literacy is estimated to affect over 90 million Americans and is now recognized as an important public health concern (2). Patients with limited health literacy may have difficulty understanding written medical information, communicating with healthcare providers, and navigating the increasingly complex healthcare system. Studies in various patient populations demonstrate an association of limited health literacy with poorer health-related knowledge (3,4), lower use of preventive health services (5,6), increased risk of hospitalization (7,8), decreased medication adherence (9,10), greater probability of depressive symptoms (11,12), poorer health status (13,14), higher healthcare costs (15,16), and increased mortality (17,18). In addition, there is evidence that limited health literacy contributes to racial disparities in health outcomes (19–21). Promising interventions to mitigate the effects of low health literacy include intensive disease or self-management programs, which have been shown to be effective in decreasing disease severity, improving self-management behaviors, and reducing hospitalizations (22–24).
Despite this knowledge, few studies have examined health literacy in patients with ESRD. Health literacy may be particularly germane to the care and outcome of patients with ESRD receiving hemodialysis, because this patient population must attend regular dialysis treatments to maintain electrolyte and fluid balance; follow dietary restrictions related to fluid, sodium, phosphorous, and potassium intake; and adhere to multiple medications to treat or prevent the complications of ESRD. Preliminary studies suggest that limited health literacy is prevalent in patients receiving chronic hemodialysis and may be associated with adverse outcomes including mortality (25,26). However, these studies either enrolled small numbers of patients or restricted their study populations to those suspected of having low health literacy. We sought to build upon past studies by characterizing health literacy in a broader population of patients, including those receiving care in Veterans Affairs, academic, and private practice–affiliated dialysis settings and assessing the associations of demographic and clinical characteristics, including health-related quality of life, symptom burden, and depression, with limited health literacy.
Materials and Methods
Patient Population
Subjects included in this analysis were enrolled in the SMILE study, a multicenter randomized clinical trial comparing symptom management strategies in patients treated with chronic hemodialysis (27). Study personnel recruited patients from nine outpatient dialysis units in and around Pittsburgh, Pennsylvania between January 2009 and January 2010. These dialysis units were staffed by academic and private nephrologists, nurse practitioners, and physician assistants. Eligible patients were older than 17 years of age, spoke English, and were receiving outpatient in-center hemodialysis. Patients undergoing active work-up for living donor kidney transplant and/or considering transfer to peritoneal dialysis at the time of recruitment were excluded to help ensure that the study population would remain on chronic hemodialysis for the duration of the parent trial. As part of screening, we assessed cognitive function using the mini-Cog, a three-item test of cognitive function (28). We excluded patients with scores <3, which is consistent with cognitive impairment. We enrolled all patients who met the eligibility criteria and consented to participate. The study was approved by the institutional review boards of the University of Pittsburgh, the Veterans Administration Pittsburgh Healthcare System, and the Western Institutional Review Board.
Data Collection
We assessed patient demographic characteristics including self-reported race and ethnicity, age, sex, educational level, veteran status, and annual income by conducting patient interviews. We evaluated baseline clinical characteristics including dialysis vintage, history of past renal transplant, type of vascular access, and comorbid illness burden on the basis of the Charlson Comorbidity Index by reviewing the dialysis charts. We also abstracted the most recent laboratory values (i.e. hemoglobin; serum calcium, phosphorous, albumin, and intact parathyroid hormone concentrations; and Kt/V and urea reduction ratio) at the time of the first study assessment. We assessed baseline health-related quality of life, depression, and overall symptom burden using the Short Form 12, Patient Health Questionnaire 9, and Dialysis Symptom Index, respectively (29–34).
Assessment of Health Literacy
After enrollment, research personnel assessed study participants' visual capacity by asking them to read a series of numbers typed at 14-, 20-, and 30-point-sized font. Patients unable to read all of the numbers written at 14-point font were offered reading glasses to complete the health literacy assessment. After this assessment of visual capacity, study personnel assessed patients' health literacy using the Rapid Estimate of Adult Literacy in Medicine (REALM), a 66-item word recognition tool that has been validated against general measures of literacy (35) and other health literacy tools (36,37). This instrument takes 2 to 3 minutes to administer and is designed to assess an adult patient's ability to read common medical words and lay terms for body parts and illnesses. REALM scores range from 0 to 66, with scores of 0 to 18 representing a reading level of third grade or less (“may not be able to read most low literacy materials and may need repeat oral instructions”); 19 to 44 representing a fourth to sixth grade reading level (“may need low literacy materials and may not be able to read prescription instructions”); 45 to 60 representing a seventh to eighth grade reading level (“may struggle with most currently available patient education materials”); and >60 representing a ninth grade reading level or above (“should be able to read most patient education materials”) (35). Prior studies have defined limited health literacy as REALM scores ≤60 (18,26). We used this threshold to define limited health literacy in our study participants.
Statistical Analyses
We described baseline demographic and clinical characteristics using proportions for discrete characteristics and, because of skewed distributions, medians and interquartile ranges for continuous variables. Univariate associations of demographic characteristics (e.g. age, sex, and race) and clinical variables (e.g. dialysis vintage and serologic values) with limited health literacy were assessed using Wilcoxon rank sum test for continuous variables, Fisher's exact tests for dichotomous and nominal variables, and Cochran-Mantel-Haenszel tests of trend for ordinal characteristics. Demographic and clinical factors associated with limited health literacy on the basis of two-tailed P values <0.10 in univariate analyses were included in a random effects multivariable logistic regression model to assess the independent association of these variables with limited health literacy while accounting for the nonindependence of patients treated at the same dialysis unit. We used multiple imputation to adjust for nonresponse to patient income (38). Statistical significance was denoted by a two-tailed P value of <0.05. All of the analyses were conducted using SAS 9.2 (Cary, NC) and Stata 11.0 (College Station, TX).
Results
Study Population
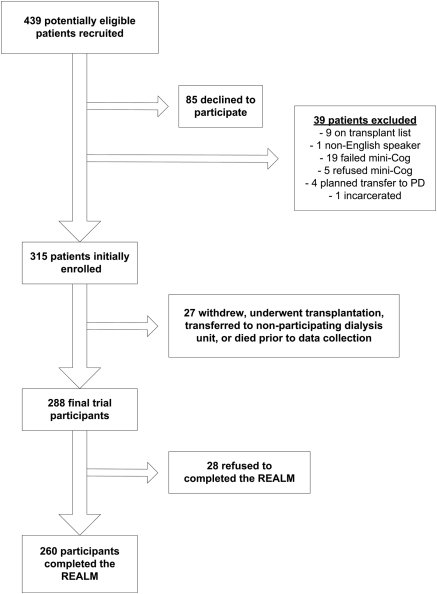
We screened 439 patients for the parent clinical trial, of whom 85 (19%) declined to participate and 39 (9%) were excluded on the basis of established criteria. Of the 315 patients who initially consented to participate, 27 (9%) withdrew, underwent renal transplantation, transferred to a nonparticipating dialysis unit, or died before data collection, resulting in a final trial population of 288 participants (Figure 1). Twenty-eight patients (10%) refused to complete the REALM, 22 (79%) of whom reported the reason for refusal to be related to problems with their vision. Two hundred sixty (90%) of the enrolled participants completed the REALM. Their median age was 64 years, 57% were male, and 40% were African American (Table 1). Compared with participants who completed the REALM, patients who refused the REALM were more likely to have a lower than high school level of education (odds ratio [OR] = 3.5; 95% confidence interval [CI], 1.3 to 8.9).
Figure 1.
Study population. PD, peritoneal dialysis.
Table 1.
Comparison of demographic and clinical characteristics by REALM score
| Variable | Overall Population (n = 288) | REALM Score ≤60 (n = 41) | REALM Score >60 (n = 219) | Pa |
|---|---|---|---|---|
| Demographic variables | ||||
| median age: years | 64.0 (56 to 73) | 61 (57 to 73) | 63 (55 to 73) | 0.76 |
| gender: male | 163 (57%) | 27 (66%) | 123 (56%) | 0.3 |
| race: African American | 114 (40%) | 24 (59%) | 79 (36%) | <0.01 |
| ethnicity: Hispanic | 8 (3%) | 1 (2%) | 6 (3%) | 1.00 |
| Education | ||||
| less than high school | 40 (14%) | 14 (34%) | 17 (8%) | <0.01 |
| high school equivalent | 92 (32%) | 17 (42%) | 64 (29%) | |
| more than high school | 154 (54%) | 10 (24%) | 136 (63%) | |
| Income | ||||
| less than $30,000/year | 144 (50%) | 22 (54%) | 105 (48%) | <0.01 |
| at least $30,000/year | 91 (32%) | 6 (15%) | 80 (37%) | |
| unknown | 52 (18%) | 13 (32%) | 33 (15%) | |
| Veteran | 86 (30%) | 18 (44%) | 60 (28%) | 0.04 |
| Married | 126 (44%) | 14 (34%) | 101 (46%) | 0.17 |
| Dialysis/clinical variables | ||||
| Dialysis vintage: years | 2.3 (1.0 to 4.4) | 2.4 (1.0 to 4.1) | 2.2 (0.8 to 4.7) | 0.82 |
| Dialysis adequacy: Kt/V | 1.5 (1.4 to 1.6) | 1.5 (1.4 to 1.7) | 1.5 (1.4 to 1.6) | 0.94 |
| Dialysis access | ||||
| Catheter | 59 (20%) | 3 (7%) | 51 (23%) | 0.02 |
| AV fistula or graft | 228 (79%) | 38 (93%) | 167 (77%) | |
| CCI score | ||||
| 1 to 2 | 64 (23%) | 6 (15%) | 57 (27%) | 0.02 |
| 3 to 4 | 109 (39%) | 13 (32%) | 83 (39%) | |
| >5 | 110 (39%) | 22 (54%) | 75 (35%) | |
| Laboratory values | ||||
| hemoglobin (g/dl) | 11.6 (10.9 to 12.2) | 11.9 (11.2 to 12.3) | 11.6 (10.9 to 12.2) | 0.18 |
| albumin (g/dl) | 3.8 (3.6 to 4.1) | 3.7 (3.5 to 4.1) | 3.8 (3.6 to 4.1) | 0.65 |
| calcium (mg/dl) | 8.9 (8.5 to 9.3) | 8.8 (8.5 to 9.1) | 8.9 (8.5 to 9.3) | 0.28 |
| phosphorous (mg/dl) | 5.0 (4.4 to 5.9) | 5.1 (4.1 to 6.9) | 5.0 (4.3 to 5.9) | 0.40 |
| iPTH (pg/ml) | 253 (175 to 397) | 266 (189 to 383) | 244 (165 to 386) | 0.55 |
| Health-related variables | ||||
| Symptom burdenb | 12.0 (7.0 to 17.0) | 12.5 (8.0 to 17.0) | 12.0 (7.0 to 17.0) | 0.86 |
| Quality of lifec | 7.0 (5.0 to 8.0) | 7.0 (5.0 to 8.5) | 7.0 (5.0 to 8.0) | 0.93 |
| mental health | 50.4 (40.2 to 58.2) | 48.0 (36.7 to 61.5) | 50.1 (41.9 to 57.5) | 0.96 |
| physical health | 35.3 (27.0 to 44.2) | 32.8 (26.9 to 38.6) | 36.6 (27.1 to 44.9) | 0.22 |
| depressiond | 72 (25%) | 14 (34%) | 50 (23%) | 0.17 |
Category percentages may not equal 100% because of rounding. REALM, Rapid Estimate of Adult Literacy in Medicine; AV, arteriovenous; CCI, Charlson Comorbidity Index; iPTH, intact parathyroid hormone.
Comparison of patients with REALM ≤60 and >60.
Number of symptoms reported on the Dialysis Symptom Index.
Scores on Short Form 12.
Proportion of patients with Patient Health Questionnaire 9 score of ≥10.
Health Literacy Scores
Overall, 41 of 260 patients (16%) who completed the REALM demonstrated scores on this instrument of ≤60, indicating the presence of limited health literacy. The prevalence of limited health literacy ranged from 7% to 37% at the nine participating dialysis units. Of the 41 patients with limited health literacy, 34 (83%) had REALM scores of 45 to 60 (i.e. seventh to eighth grade reading level), six (15%) had scores of 19 to 44 (i.e. fourth to sixth grade reading level), and one (2%) had a score <19 (i.e. less than a fourth grade reading level). Twenty-seven of the 41 (66%) patients with limited health literacy reported a high school equivalent or higher level of education. Conversely, 17 (8%) of 219 patients with adequate literacy (REALM scores >60) reported a less than high school level of education.
Factors Associated with Limited Health Literacy
In unadjusted analyses, demographic factors associated with limited health literacy included African-American race, lower educational attainment, lower income, and veteran status (Table 1). Patients with higher burdens of comorbid illness and those dialyzing with an arteriovenous fistula or graft (as compared with a catheter) were also more likely to demonstrate limited health literacy; however, additional analyses suggested that these associations were driven by educational status and study site, respectively (data not shown). There were no associations of age; gender; or markers of quality of care including hemoglobin level, serum phosphorus, and intact parathyroid hormone level or dialysis adequacy with limited health literacy. Although there was a trend for patients with limited health literacy to be more depressed than patients with adequate health literacy, these differences did not meet the level of statistical significance in unadjusted analyses (Table 1). Quality of life and overall symptom burden were similar in patients with and without limited health literacy.
In multivariable analyses, African-American race (adjusted OR = 3.01; 95% CI, 1.40 to 6.49), lower educational attainment (less than high school: OR = 12.1 and 95% CI, 4.10 to 35.7; high school equivalent: OR = 3.70 and 95% CI 1.46 to 9.36), and veteran status (adjusted OR = 3.68; 95% CI, 1.61 to 8.43) were independently associated with limited health literacy (Table 2). Veterans receiving dialysis within and outside the Veterans Affairs healthcare system were more likely to have limited health literacy than nonveterans after adjusting for potential confounders. Finally, limited health literacy was not an independent predictor of type of vascular access or Charlson Comorbidity Index score.
Table 2.
Factors independently associated with limited health literacy
| Variable | Unadjusted OR (95% CI) | Adjusted OR (95% CI)a |
|---|---|---|
| African-American race | 2.50 (1.27 to 4.94) | 3.01 (1.40 to 6.49) |
| Educationb | ||
| less than high school | 12.1 (4.43 to 32.9) | 12.1 (4.10 to 35.7) |
| high school equivalent | 3.75 (1.60 to 8.79) | 3.70 (1.46 to 9.36) |
| Incomec | ||
| less than $30,000/year | 2.56 (1.01 to 6.49) | 1.52 (0.51 to 4.57) |
| Veteran | 2.06 (1.04 to 4.09) | 3.68 (1.61 to 8.43) |
OR, odds ratio; CI, confidence interval.
Independent odds of limited health literacy.
Referent category is more than a high school level of education.
Referent category is income at least $30,000/year.
Discussion
In this cross-sectional analysis of patients receiving chronic hemodialysis, we found that limited health literacy is reasonably common and is independently associated with African-American race, lower educational level, and veteran status. However, some patients with higher educational levels also demonstrated limited health literacy. These observations build upon prior reports of health literacy in this patient population and have important clinical and research implications.
The prevalence of limited health literacy in our study is approximately 50% lower than has been reported in prior studies of patients on hemodialysis (25,26). The use of different health literacy assessment tools and criteria for enrollment as well as nonresponse bias may account for these differences. Grubbs et al. (25) administered the Short Test of Functional Health Literacy in Adults (S-TOFHLA) to 62 patients on chronic hemodialysis and reported a prevalence of limited health literacy of 32%. Unlike the REALM, which measures recognition and pronunciation of common medical words, the S-TOFHLA measures numeracy and reading comprehension. Although both instruments have been shown to be highly correlated (r = 0.80) in the general population (37), it is unclear which instrument is a more reliable and valid tool in patients on chronic hemodialysis. Cavanaugh et al. (26) used the REALM to assess health literacy in 480 incident hemodialysis patients and reported a prevalence of limited health literacy of 32%. However, this study was restricted to patients suspected, a priori, of having limited health literacy, which may have accounted for the higher prevalence than demonstrated in our study. Nonresponse bias may also account for the lower prevalence of limited health literacy in our study. Patients in our study who refused to complete the REALM were more likely to have lower educational attainment, which was independently associated with limited health literacy. Past studies have found that accounting for nonresponse bias increases the estimated prevalence of limited health literacy (39). Additional research is needed to determine the precise prevalence of limited health literacy in the overall population of patients on chronic hemodialysis.
Even if the prevalence of limited health literacy in patients on chronic hemodialysis is 16% as seen in our study, the number of patients receiving chronic hemodialysis in the United States affected by this problem would be greater than 56,000 (40). This observation is notable given the potential importance of written materials and verbal instructions to this patient population. Past research demonstrated that patients on hemodialysis take an average of 19 medications each day, and approximately 25% of patients consume more than 25 medications on a daily basis (41). Adequate health literacy may be important for patients to be able to adhere to such medication regimens as cited in a recent comprehensive review by Browne and Merighi (42). Moreover, a study by Manley et al. (43) documented that medication-related problems, including adverse drug reactions, overdosing, and underdosing, were very common in ambulatory hemodialysis patients. Whether and how limited health literacy contributes to such medication-related problems was not investigated. Many patients on chronic hemodialysis are also counseled on the importance of diet and are provided with written materials instructing them to follow diets that are low in salt, potassium, and phosphorus. Although our study did not find differences in the serum phosphorus concentration on the basis of patients' health literacy level, our assessment of this serologic parameter was cross-sectional rather than longitudinal. Nonetheless, it seems quite plausible that limited health literacy could affect patients' capacity to adhere to dietary restrictions. Efforts to understand whether and how limited health literacy impacts long-term adherence to increasingly complex medication regimens and dietary restrictions are clearly needed because dietary and treatment adherence could be directly impacted by interventions to improve health literacy.
Although we and others have demonstrated an independent association of lower educational attainment with limited health literacy, we found that a notable proportion of patients with limited health literacy reported a high school equivalent or higher level of education. This may reflect the observation that the assessment of educational level in studies such as ours is based on quantifying the years of school completed, not the reading skills obtained or their permanency. Studies in other populations have shown that the last grade completed in school is a poor indicator of reading ability (44). In light of this observation, it may not be appropriate for renal providers to guess or try to predict which patients have limited health literacy on the basis of educational attainment. Rather, as has been advocated by the Agency for Healthcare Research and Quality, the federal agency that aims to enhance the safety and effectiveness of health care, renal providers should consider adopting a “health literacy universal precautions” approach to evaluating this problem (45).
Our finding that African-American race and veteran status are each independently associated with limited health literacy is consistent with previous studies (46,47). Although we did not investigate the factors mediating these associations, this finding may reflect underlying differences in the quality of education, cultural variability in understanding health-related terminology, and/or differences in exposure to the healthcare system. Nonetheless, African-Americans with chronic kidney disease are less likely to be seen by a nephrologist, more likely to progress to ESRD, and less likely to be listed for or receive a renal transplant (48). Moreover, there is evidence from studies in patients with other chronic diseases that health literacy mediates racial disparities in health outcomes (49,50). This suggests that efforts to improve health literacy among racial minorities and sociodemographically disadvantaged patients, including veterans, with chronic renal disease and ESRD may be a means to reduce health disparities and improve outcomes. Such efforts will need to consider the cultural, racial, and sociodemographic characteristics of the patients most likely to potentially derive benefit from such interventions.
Our study has several limitations. First, although this represents one of the largest studies of health literacy in patients on chronic hemodialysis, our sample size was relatively small. Second, we excluded patients being worked up for living renal transplant or considering transfer to peritoneal dialysis. Exclusion of such subjects, who may have higher health literacy, could impact the generalizability of our prevalence estimate of limited health literacy. Furthermore, our study involved patients participating in a randomized clinical trial, so our results may not be generalizable to the overall dialysis population. Rather, our findings may be most generalizable to dialysis patients who participate in clinical trials. Third, although the REALM is a widely used measure of health literacy that assesses reading and pronunciation of medical terms, it does not capture other skills that may be important including numeracy, oral communication, and memory. Fourth, there were few Hispanics or other ethnic minorities other than African Americans in our study population, which limits the external validity of our findings to such patient groups. Fifth, our assessment of visual capacity has not been previously validated, and therefore our findings in this regard may not be accurate or generalizable. Finally, although other studies suggest that limited health literacy is associated with a lower likelihood of referral for renal transplantation and a higher likelihood of mortality (25,26), we did not assess the associations of limited health literacy with downstream, patient-centered outcomes.
In conclusion, we found that limited health literacy is quite common among hemodialysis patients and is most likely to be present in African Americans, those with lower levels of educational attainment, and veterans. Further studies are needed to assess the health implications of limited health literacy in patients on hemodialysis including whether limited health literacy is associated with patient knowledge, self-management behaviors, and access to care and how this impacts health disparities and longer-term outcomes. A broader understanding of these relationships will facilitate the development of targeted interventions to improve health literacy, quality of care, and outcomes in patients with kidney disease.
Disclosures
None.
Acknowledgments
This study was funded by a grant from the Department of Veterans Affairs Health Research and Development Service (Weisbord HSR&D IIR 07-190). These data were presented in abstract form at the 2009 annual meeting of the American Society of Nephrology. Dr. Green is supported by a grant from the American Kidney Fund Clinical Scientist in Nephrology Program. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1. Lynn Nielsen-Bohlman AMP: Health Literacy: A Prescription to End Confusion, edited by David A. Kindig, Washington DC, National Academies Press, 2004 [PubMed] [Google Scholar]
- 2. Mark Kutner EG, Ying Jin, Christine Paulsen: The Health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy. Washington DC, United States Department of Education, National Center for Education Statistics, 2006 [Google Scholar]
- 3. Williams MV, Baker DW, Parker RM, Nurss JR: Relationship of functional health literacy to patients' knowledge of their chronic disease: A study of patients with hypertension and diabetes. Arch Intern Med, 158: 166–172, 1998 [DOI] [PubMed] [Google Scholar]
- 4. Gazmararian JA, Williams MV, Peel J, Baker DW: Health literacy and knowledge of chronic disease. Patient Educ Couns 51: 267–275, 2003 [DOI] [PubMed] [Google Scholar]
- 5. White S, Chen J, Atchison R: Relationship of preventive health practices and health literacy: A national study. Am J Health Behav 32: 227–242, 2008 [DOI] [PubMed] [Google Scholar]
- 6. Scott TL, Gazmararian JA, Williams MV, Baker DW: Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care 40: 395–404, 2002 [DOI] [PubMed] [Google Scholar]
- 7. Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, Ren J, Peel J: Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health 92: 1278–1283, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baker DW, Parker RM, Williams MV, Clark WS: Health literacy and the risk of hospital admission. J Gen Intern Med 13: 791–798, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kalichman SC, Pope H, White D, Cherry C, Amaral CM, Swetzes C, Flanagan J, Kalichman MO: Association between health literacy and HIV treatment adherence: Further evidence from objectively measured medication adherence. J Int Assoc Physicians AIDS Care 7: 317–323, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kripalani S, Gatti ME, Jacobson TA: Association of age, health literacy, and medication management strategies with cardiovascular medication adherence. Patient Educ Couns 81:177–181, 2010 [DOI] [PubMed] [Google Scholar]
- 11. Lincoln A, Paasche-Orlow MK, Cheng DM, Lloyd-Travaglini C, Caruso C, Saitz R, Samet JH: Impact of health literacy on depressive symptoms and mental health-related quality of life among adults with addiction. J Gen Intern Med 21: 818–822, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bennett IM, Culhane JF, McCollum KF, Mathew L, Elo IT: Literacy and depressive symptomatology among pregnant Latinas with limited English proficiency. Am J Orthopsychiatry 77: 243–248, 2007 [DOI] [PubMed] [Google Scholar]
- 13. Wolf MS, Gazmararian JA, Baker DW: Health literacy and functional health status among older adults. Arch Intern Med 165: 1946–1952, 2005 [DOI] [PubMed] [Google Scholar]
- 14. Baker DW, Parker RM, Williams MV, Clark WS, Nurss J: The relationship of patient reading ability to self-reported health and use of health services. Am J Public Health 87: 1027–1030, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Howard DH, Gazmararian J, Parker RM: The impact of low health literacy on the medical costs of Medicare managed care enrollees. Am J Med 118: 371–377, 2005 [DOI] [PubMed] [Google Scholar]
- 16. Weiss BD, Palmer R: Relationship between health care costs and very low literacy skills in a medically needy and indigent Medicaid population. J Am Board Fam Pract 17: 44–47, 2004 [DOI] [PubMed] [Google Scholar]
- 17. Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J: Health literacy and mortality among elderly persons. Arch Intern Med 167: 1503–1509, 2007 [DOI] [PubMed] [Google Scholar]
- 18. Sudore RL, Yaffe K, Satterfield S, Harris TB, Mehta KM, Simonsick EM, Newman AB, Rosano C, Rooks R, Rubin SM, Ayonayon HN, Schillinger D: Limited literacy and mortality in the elderly: The health, aging, and body composition study. J Gen Intern Med 21: 806–812, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sentell TL, Halpin HA: Importance of adult literacy in understanding health disparities. J Gen Intern Med 21: 862–866, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Howard DH, Sentell T, Gazmararian JA: Impact of health literacy on socioeconomic and racial differences in health in an elderly population. J Gen Intern Med 21: 857–861, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bennett IM, Chen J, Soroui JS, White S: The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann Fam Med 7: 204–211, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rothman RL, DeWalt DA, Malone R, Bryant B, Shintani A, Crigler B, Weinberger M, Pignone M: Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA 292: 1711–1716, 2004 [DOI] [PubMed] [Google Scholar]
- 23. DeWalt DA, Malone RM, Bryant ME, Kosnar MC, Corr KE, Rothman RL, Sueta CA, Pignone MP: A heart failure self-management program for patients of all literacy levels: A randomized, controlled trial [ISRCTN11535170]. BMC Health Serv Res 6: 30, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Schillinger D, Handley M, Wang F, Hammer H: Effects of self-management support on structure, process, and outcomes among vulnerable patients with diabetes: A three-arm practical clinical trial. Diabetes Care 32: 559–566, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Grubbs V, Gregorich SE, Perez-Stable EJ, Hsu CY: Health literacy and access to kidney transplantation. Clin J Am Soc Nephrol 4: 195–200, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cavanaugh KL, Wingard RL, Hakim RM, Eden S, Shintani A, Wallston KA, Huizinga MM, Elasy TA, Rothman RL, Ikizler TA: Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol 21:1979–1985, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Weisbord SD, Shields AM, Mor MK, Sevick MA, Homer M, Peternel J, Porter P, Rollman BL, Palevsky PM, Arnold RM, Fine MJ: Methodology of a randomized clinical trial of symptom management strategies in patients receiving chronic hemodialysis: The SMILE study. Contemp Clin Trials, 31: 491–497, 2010 [DOI] [PubMed] [Google Scholar]
- 28. Borson S, Scanlan JM, Chen P, Ganguli M: The Mini-Cog as a screen for dementia: Validation in a population-based sample. J Am Geriatr Soc 51: 1451–1454, 2003 [DOI] [PubMed] [Google Scholar]
- 29. Ware J, Jr., Kosinski M, Keller SD: A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care 34: 220–233, 1996 [DOI] [PubMed] [Google Scholar]
- 30. Cafazzo JA, Leonard K, Easty AC, Rossos PG, Chan CT: Patient-perceived barriers to the adoption of nocturnal home hemodialysis. Clin J Am Soc Nephrol 4: 784–789, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Neri L, Rocca Rey LA, Gallieni M, Brancaccio D, Cozzolino M, Colombi A, Burroughs TE: Occupational stress is associated with impaired work ability and reduced quality of life in patients with chronic kidney failure. Int J Artif Organs 32: 291–298, 2009 [DOI] [PubMed] [Google Scholar]
- 32. Kroenke K, Spitzer RL, Williams JB: The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 16: 606–613, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Watnick S, Wang PL, Demadura T, Ganzini L: Validation of 2 depression screening tools in dialysis patients. Am J Kidney Dis 46: 919–924, 2005 [DOI] [PubMed] [Google Scholar]
- 34. Weisbord SD, Fried LF, Arnold RM, Rotondi AJ, Fine MJ, Levenson DJ, Switzer GE: Development of a symptom assessment instrument for chronic hemodialysis patients: The Dialysis Symptom Index. J Pain Symptom Manage 27: 226–240, 2004 [DOI] [PubMed] [Google Scholar]
- 35. Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, Crouch MA: Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med 25: 391–395, 1993 [PubMed] [Google Scholar]
- 36. Parker RM, Baker DW, Williams MV, Nurss JR: The test of functional health literacy in adults: A new instrument for measuring patients' literacy skills. J Gen Intern Med 10: 537–541, 1995 [DOI] [PubMed] [Google Scholar]
- 37. Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J: Development of a brief test to measure functional health literacy. Patient Educ Couns 38: 33–42, 1999 [DOI] [PubMed] [Google Scholar]
- 38. Little R, Rubin D: Statistical Analsis with Missing Data, 2nd Ed., New York, John Wiley & Sons, 2002 [Google Scholar]
- 39. Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Saha S, Snyder A, Nugent S, Baines Simon A, Gralnek I, Provenzale D, van Ryn M: Variation in estimates of limited health literacy by assessment instruments and non-response bias. J Gen Intern Med 25: 675–681, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. USRDS 2010 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, Bethesda MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2009 [Google Scholar]
- 41. Chiu YW, Teitelbaum I, Misra M, de Leon EM, Adzize T, Mehrotra R: Pill burden, adherence, hyperphosphatemia, and quality of life in maintenance dialysis patients. Clin J Am Soc Nephrol 4: 1089–1096, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Browne T, Merighi JR: Barriers to adult hemodialysis patients' self-management of oral medications. Am J Kidney Dis 56: 547–557, 2010 [DOI] [PubMed] [Google Scholar]
- 43. Manley HJ, Drayer DK, Muther RS: Medication-related problem type and appearance rate in ambulatory hemodialysis patients. BMC Nephrol 4: 10, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Davis TC, Crouch MA, Wills G, Miller S, Abdehou DM: The gap between patient reading comprehension and the readability of patient education materials. J Fam Pract 31: 533–538, 1990 [PubMed] [Google Scholar]
- 45. DeWalt D, Callahan L, Hawk V, Broucksou K, Hink A, Rudd R, Brach C: Health Literacy Universal Precautions Toolkit, AHRQ Publication No. 10-0046-EF, Rockville MD, Agency for Healthcare Research and Quality, 2010 [Google Scholar]
- 46. Dolan NC, Ferreira MR, Davis TC, Fitzgibbon ML, Rademaker A, Liu D, Schmitt BP, Gorby N, Wolf M, Bennett CL: Colorectal cancer screening knowledge, attitudes, and beliefs among veterans: Does literacy make a difference? J Clin Oncol 22: 2617–2622, 2004 [DOI] [PubMed] [Google Scholar]
- 47. Shea JA, Beers BB, McDonald VJ, Quistberg DA, Ravenell KL, Asch DA: Assessing health literacy in African American and Caucasian adults: Disparities in rapid estimate of adult literacy in medicine (REALM) scores. Fam Med 36: 575–581, 2004 [PubMed] [Google Scholar]
- 48. Powe NR: Let's get serious about racial and ethnic disparities. J Am Soc Nephrol 19: 1271–1275, 2008 [DOI] [PubMed] [Google Scholar]
- 49. Osborn CY, Cavanaugh K, Wallston KA, White RO, Rothman RL: Diabetes numeracy: An overlooked factor in understanding racial disparities in glycemic control. Diabetes Care 32: 1614–1619, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Osborn CY, Paasche-Orlow MK, Davis TC, Wolf MS: Health literacy: An overlooked factor in understanding HIV health disparities. Am J Prev Med 33: 374–378, 2007 [DOI] [PubMed] [Google Scholar]