Abstract
The Messerklinger technique is an endoscopic approach to sinus surgery designed to be minimally invasive and preserve mucosa and hence physiological function. More recently there have been advocates for more radical endoscopic approaches to the frontal sinus such as the Modified Lothrop. This review discusses different approaches to frontal sinus surgery including any advantages and disadvantages to each approach. After examining the evidence from the literature, meticulously performed endoscopic frontal sinusotomy with or without computer guidance appears to be the most effective minimally invasive procedure for treating chronic frontal sinusitis secondary to outflow tract obstruction. Properly performed, it is almost always effective in dealing with even the most diseased frontal sinus. It offers clear advantages in reducing complications and recurrence rates in frontal sinus disease, even for revision cases.
Keywords: Endoscopic frontal sinusotomy, Frontal sinusitis, Recurrence, Surgical revision
Introduction
The osteoplastic flap has historically been the mainstay of surgical access to the frontal sinus [1], but with the advance of the endoscopic revolution, its stranglehold has been loosened. However, accessing the frontal sinus provides a greater surgical challenge than the other sinuses owing to the anatomical constraints present in an endoscopic approach. In this respect, navigating the frontal recess and sinus with its variable array of cells from the agger nasi to the intersinus septal and frontal cells, means that any surgeon approaching this area endoscopically must have sufficient experience as well as suitable instrumentation and training to achieve excellence in this procedure. Messerklinger developed the endoscopic technique with the aim to relieve diseased sinuses while preserving mucosa and at the same time being minimally invasive [2]. Whilst the technique has previously been championed [3], other endoscopic techniques have gained recent vogue, namely the modified Lothrop [4, 5] (frontal sinus drill out) and balloon sinuplasty [6]. Combined and open approaches to the frontal sinus are other available options, for example trephination [7, 8] and osteoplastic flaps with or without obliteration [9–11]. The key aim of operating in the frontal recess is not only to relieve obstruction of the outflow tract and thereby definitively treat the existing disease from an anatomical perspective, but also, and more importantly, prevention of recurrent disease. This is inherently easier to achieve when the primary surgical intervention is conducted with this key aim in mind. Unfortunately, iatrogenic causes have a large part to play in recurrent frontal sinusitis, with osteoneogenesis and recurrent polyposis also being significant factors.
Endoscopic Frontal Sinusotomy
The operative approach utilised at our centres for frontal sinusotomy is along the lines of the Messerklinger technique—minimally invasive and with meticulous preservation of mucosa. For this purpose the key instruments at our disposal include a 70° Karl Storz reverse-post endoscope, a variety of refined instruments including Huweiser/Kuhn frontal through-cut instruments (45 and 90° with various angled tips), frontal sinus seekers with various angles and tips (Karl Storz), frontal sinus giraffe forceps (45 and 90), as well as angled suction curettes and mushroom punches. We also double bend our suctions so that we have maximum access to the excessively angled frontal recess [12]. Alongside these the GE Instatrak 3500+ image guidance software is employed for all cases of frontal sinusotomy to ensure that any frontal recess cells such as Kuhn type 1–3 cells, supra-orbital ethmoid cells and intersinus septal cells are cleared to allow adequate drainage of the frontal sinus. Post-operative results show excellent aeration of the frontal sinus as seen in Fig. 1 in the majority of cases. Table 1 demonstrates the recurrence rates from our recent study showing a recurrence in frontal sinusitis of 19% in the group of patients who underwent their primary surgery at SPSC and 34% in those who underwent their primary surgery elsewhere [13]. However, only 8% in the primary group were symptomic enough to require a return to theatre compared to 21% in the revision group. This equates to a surgical conversion rate of 47% for primary cases. The pre-operative Lund-Mackay scores were found to have no significant correlation with the incidence of recurrent frontal sinus disease (P = 0.35). The Philadelphia group found in their series of 130 frontal sinusotomies that 10 (8%) required further intervention based on endoscopic findings and the ability to cannulate the frontal sinus [14]. Other centres have also reported excellent results using similar endoscopic techniques [3, 15] and have been able to demonstrate a significant improvement in the quality of life of the patients post-operatively [16]. Maintaining the theme of the minimally invasive approach, the frontal sinus rescue procedure is an alternative option to employ when the middle turbinate has been previously resected [17, 18]. This involves advancing a mucoperiosteal flap into the frontal sinus neo-ostium to try and restore functionality to the diseased sinus (Fig. 2).
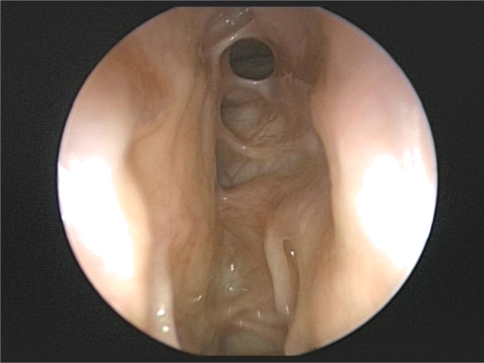
Fig. 1.
Post-operative view of frontal ostium 1 month after endoscopic frontal sinusotomy
Table 1.
Summary findings of study—primary (204 cases), revision (98 cases)
| Primary (%) | Revision (%) | |
|---|---|---|
| Recurrence rate | 18 | 34 |
| Revision rate | 8 | 21 |
| Conversion rate | 47 | 64 |
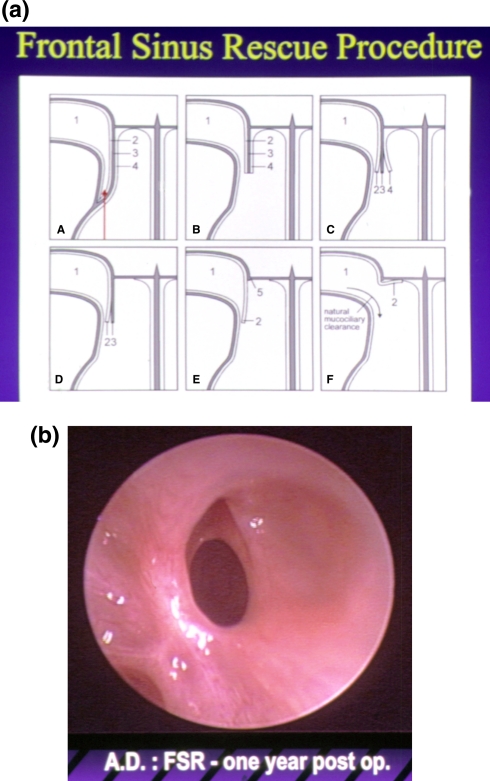
Fig. 2.
Schematic representation of the frontal sinus rescue procedure. (a) The frontal sinus (1) is completely separated from the nasal cavity by the middle turbinate stub (3) which is lateralised across the frontal sinus outflow tract. The adhesion is released by incising the area indicated by the straight arrow. (B) The thin lamella of bone, the vertical middle turbinate remnant, covered with mucous membrane on its medial (4) and lateral aspect (2) becomes apparent. (C) The mucosa on the lateral and medial (4) aspects of the bony middle turbinate stub (3) are elevated (D and E). The mucosa on the medial aspect (4) and the bony middle turbinate stub are removed to the level of the skull base. (f) The mucoperiosteal flap (2) is then draped medially. The curved arrow illustrates the natural drainage pattern for the frontal sinus. (b) Frontal sinus rescue procedure—post-operative appearance endoscopically
Balloon Sinuplasty
Balloon sinuplasty is a new technique performed endoscopically that is gaining vogue for dealing with the maxillary and frontal sinuses [19, 20]. Although the long-term results are not yet forthcoming, the immediate results show some promise with this minimally invasive technique in the properly chosen patient [21]. This technique can be undertaken as an outpatient procedure [6, 19] or as part of a formal procedure under general anaesthesia and the need for fluoroscopic guidance [22] has now been removed with the use of illuminated catheter tips.
Extended Endoscopic Approaches
The Draf III or Modified Lothrop procedure commonly known as the “frontal sinus drill out” is enjoying a period of certain vogue secondary to promotion by selected centres [5, 25]. With this technique the floors of the frontal sinuses as well as the intersinus septum and the upper septal cartilage beneath that are removed, thus creating a common median drainage pathway (Fig. 3). Cautious proponents of this technique would advocate its use in severe cases of chronic frontal sinusitis, or for specific lesions, where the only alternative is an osteoplastic flap and frontal sinus obliteration [23, 24]. However there are centres that would advocate more widespread use of the technique for routine work [5, 25]. For cases of CRS, recurrence rates for this technique generally appear to be over 20% [25–27], and although some centres have reduced the actual rate of revision surgery, the recurrence rate of chronic frontal sinusitis remains above 20% [5, 28]; in this respect the evidence for it to replace the osteoplastic flap as the gold standard is still lacking [29].
Fig. 3.
Radiographic post-operative appearance as seen on a coronal CT following a Modified Lothrop procedure
Combined and Open Approaches
With the increasing use of the endoscope as the primary tool for visualising the frontal sinus, it is not surprising that combined approaches have found their vogue in dealing with both inflammatory and neoplastic disease and even traumatic injury of the frontal sinus, although fontal sinus trephination can be dated back the early fifties [30]. There is a range of adopted techniques that rhinologic surgeons utilise here from the mini-trephine [31, 32] through to a combined osteoplastic flap and endoscopic frontal sinusotomy, although 30 years ago the endoscope was just seen as a source of illumination for the open procedure [33]. With the increasing availability of image guidance software to rhinologic surgeons, the mini-trephine is unlikely to have a credible role in the future as it is principally a means of assisting identification of the frontal sinus ostium. Frontal trephines can, however, be used as a portal for passing endoscopes or instruments from above the ostium to visualise or manipulate from the opposite direction that can be achieved endoscopically. Indications for this approach include (1) chronic frontal sinusitis and osteoneogenesis affecting the frontal recess, (2) benign neoplasia e.g., osteoma, and (3) mucocoeles [8].
A small portal externally may, however, be inadequate when the pathology involved involves the upper reaches of the frontal sinus or is more extensive and requires drilling over wider area than is permissible through a small trephine access. The next procedure up the ladder of techniques is the gull wing approach and this can be modified accordingly depending on the requirements of the individual case; in fact the gull wing approach has the advantage of being feasible both unilaterally and bilaterally to allow a local window over the site of the pathology. One requirement of the external approaches is demarcating the external margins of the sinuses which can be done in a number of ways: (1) using neuronavigation (scan set-up and headset requirements may differ) [34], (2) endoscopic illumination from below [33] and (3) X-ray template overlay [35, 36]. Beyond the gull-wing approach, the bicoronal osteoplastic flap provides unparalleled exposure of the frontal sinuses but carries with it the stigmata of being most invasive and therefore associated with greater morbidity. Table 2 shows that it is only the osteoplastic flap that has been shown to have better results than the endoscopic approaches in reducing recurrence and revision procedures and as such remains the gold-standard technique [37]. Osteoplastic flaps are often associated with frontal sinus obliteration but the surgery performed will clearly depend on the pathology and the merits or otherwise of frontal sinus obliteration are a discussion for another time [38].
Table 2.
Recurrence and revision rates for other surgical approaches to the frontal sinus
| Technique | Author/Year | Recurrence rate (%) | Revision rate (%) |
|---|---|---|---|
| Modified Lothrop | Schlosser 2002 [25] | 32+ | 32 |
| Shirazi 2007 [27] | 23+ | 23 | |
| Schulze 2002 [26] | 23 | 15 | |
| Wormald 2003 [5] | 7+ | 7 (not all CRS) | |
| Ulualp 2009 [37] | 13+ | 13 | |
| Combined endoscopic and frontal trephine | Batra 2005 [8] | 14 | Not stated (not all CRS) |
| Hahn 2009 [50] | 57+ | 57 | |
| Osteoplastic flap ± frontal obliteration | Ulualp 2009 [37] | 0 | 0 |
| Hahn 2009 [50] | 4+ | 4 |
Medical Management of Frontal Sinuses After Primary Surgery
Recurrent mucosal inflammation is frequently managed by saline irrigations containing budesonide, but not all cases of recurrent frontal sinus disease demonstrate mucopus or mucosal oedema alone; osteoneogenesis can be a potent factor in causing recurrent disease and in the worst case scenario can completely seal off the frontal sinus. This inflammatory response in the bone has a greater tendency to occur in revision cases where previous surgical intervention has left bare bone thereby promoting osteoneogenesis and synechiae in conjunction with ongoing inflammation [39].
Where revision surgery is indicated in the presence of significant osteoneogenesis, special considerations may need to be given to the use of stents [40–44] or mitomycin C [45]. The latter is only really shown to be useful in severe cases of osteoneogenesis but the use of stents can provide an effective way of preventing re-stenosis. In our centre, a modified biliary t-tube (size French 8 or 10) or silastic sheeting cut into a T-shape is a cost-effective means of stenting the frontal sinus. These stents are typically left in situ for 6 months and then either left or removed depending on patient tolerance, but there is good evidence to suggest they can be left for long periods of time without adversity [46]. Interestingly they appear not to be beneficial following the modified Lothrop procedure [47]. Their main disadvantage is the crusting and biofilm that typically forms on them [48]. More recent frontal stent developments have been seen with the advent of balloon sinuplasty, although these devices, which contain triamcinolone, are currently licenced for in situ placement of 1 month’s duration only. The only evidence for use of these devices is derived from animal experiments but do show a role for reducing the osteogenic inflammatory response in affected sinuses [49].
Conclusion
Frontal sinus disease can be managed surgically with a minimal endoscopic approach in the vast majority of cases. If recurrent disease occurs, it can be managed medically in the clinic in over 70% of cases. A similar approach can be used for recurrences to avoid more radical interventions.
Conflict of interest
There are no financial disclosures or conflicts of interest.
References
- 1.Middleton WG, Briant TD, Fenton RS. Frontal sinusitis—a 10 year experience. J Otolaryngol. 1985;14(3):197–200. [PubMed] [Google Scholar]
- 2.Stammberger H, Posawetz W. Functional endoscopic sinus surgery. Concept, indications and results of the Messerklinger technique. Eur Arch Otorhinolaryngol. 1990;247(2):63–76. doi: 10.1007/BF00183169. [DOI] [PubMed] [Google Scholar]
- 3.Hosemann W, Kuhnel T, Held P, Wagner W, Felderhoff A. Endonasal frontal sinusotomy in surgical management of chronic sinusitis: a critical evaluation. Am J Rhinol. 1997;11(1):1–9. doi: 10.2500/105065897781446793. [DOI] [PubMed] [Google Scholar]
- 4.Rajapaksa SP, Ananda A, Cain T, Oates L, Wormald PJ. The effect of the modified endoscopic Lothrop procedure on the mucociliary clearance of the frontal sinus in an animal model. Am J Rhinol. 2004;18(3):183–187. [PubMed] [Google Scholar]
- 5.Wormald PJ, Ananda A, Nair S. The modified endoscopic Lothrop procedure in the treatment of complicated chronic frontal sinusitis. Clin Otolaryngol Allied Sci. 2003;28(3):215–220. doi: 10.1046/j.1365-2273.2003.00692.x. [DOI] [PubMed] [Google Scholar]
- 6.Kim E, Cutler JL. Balloon dilatation of the paranasal sinuses: a tool in sinus surgery. Otolaryngol Clin North Am. 2009;42(5):847–856. doi: 10.1016/j.otc.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 7.Seiberling K, Jardeleza C, Wormald PJ. Minitrephination of the frontal sinus: indications and uses in today’s era of sinus surgery. Am J Rhinol Allergy. 2009;23(2):229–231. doi: 10.2500/ajra.2009.23.3298. [DOI] [PubMed] [Google Scholar]
- 8.Batra PS, Citardi MJ, Lanza DC. Combined endoscopic trephination and endoscopic frontal sinusotomy for management of complex frontal sinus pathology. Am J Rhinol. 2005;19(5):435–441. [PubMed] [Google Scholar]
- 9.Bent JP, III, Spears RA, Kuhn FA, Stewart SM. Combined endoscopic intranasal and external frontal sinusotomy. Am J Rhinol. 1997;11(5):349–354. doi: 10.2500/105065897781286098. [DOI] [PubMed] [Google Scholar]
- 10.Guggenheim P. Indications and methods for performance of osteoplastic-obliterative frontal sinusotomy with a description of a new method and some remarks upon the present state of the are of external frontal sinus surgery. Laryngoscope. 1981;91(6):927–938. doi: 10.1288/00005537-198106000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Hardy JM, Montgomery WW. Osteoplastic frontal sinusotomy: an analysis of 250 operations. Ann Otol Rhinol Laryngol. 1976;85((4 Pt 1)):523–532. doi: 10.1177/000348947608500414. [DOI] [PubMed] [Google Scholar]
- 12.Kuhn FA, Wong KK, Mechor B, Javer AR. Creating the “double curved” suctions for sinus endoscopy and surgery. Laryngoscope. 2007;117(8):1450–1451. doi: 10.1097/MLG.0b013e318063e8ba. [DOI] [PubMed] [Google Scholar]
- 13.Philpott C, Thamboo A, Lai L, Park J, Javer A. Endoscopic frontal sinusotomy—preventing recurrence or a route to revision? Laryngoscope. 2010;120(8):1682–1686. doi: 10.1002/lary.20968. [DOI] [PubMed] [Google Scholar]
- 14.Chandra RK, Palmer JN, Tangsujarittham T, Kennedy DW. Factors associated with failure of frontal sinusotomy in the early follow-up period. Otolaryngol Head Neck Surg. 2004;131(4):514–518. doi: 10.1016/j.otohns.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 15.Har-El G, Lucente FE. Endoscopic intranasal frontal sinusotomy. Laryngoscope. 1995;105((4 Pt 1)):440–443. doi: 10.1288/00005537-199504000-00020. [DOI] [PubMed] [Google Scholar]
- 16.Metson R, Gliklich RE. Clinical outcome of endoscopic surgery for frontal sinusitis. Arch Otolaryngol Head Neck Surg. 1998;124(10):1090–1096. doi: 10.1001/archotol.124.10.1090. [DOI] [PubMed] [Google Scholar]
- 17.Citardi MJ, Javer AR, Kuhn FA. Revision endoscopic frontal sinusotomy with mucoperiosteal flap advancement: the frontal sinus rescue procedure. Otolaryngol Clin North Am. 2001;34(1):123–132. doi: 10.1016/S0030-6665(05)70300-5. [DOI] [PubMed] [Google Scholar]
- 18.Kuhn FA, Javer AR, Nagpal K, Citardi MJ. The frontal sinus rescue procedure: early experience and three-year follow-up. Am J Rhinol. 2000;14(4):211–216. doi: 10.2500/105065800779954437. [DOI] [PubMed] [Google Scholar]
- 19.Luong A, Batra PS, Fakhri S, Citardi MJ. Balloon catheter dilatation for frontal sinus ostium stenosis in the office setting. Am J Rhinol. 2008;22(6):621–624. doi: 10.2500/ajr.2008.22.3240. [DOI] [PubMed] [Google Scholar]
- 20.Catalano PJ, Payne SC. Balloon dilation of the frontal recess in patients with chronic frontal sinusitis and advanced sinus disease: an initial report. Ann Otol Rhinol Laryngol. 2009;118(2):107–112. doi: 10.1177/000348940911800205. [DOI] [PubMed] [Google Scholar]
- 21.Bolger WE, Brown CL, Church CA, Goldberg AN, Karanfilov B, Kuhn FA, et al. Safety and outcomes of balloon catheter sinusotomy: a multicenter 24-week analysis in 115 patients. Otolaryngol Head Neck Surg. 2007;137(1):10–20. doi: 10.1016/j.otohns.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 22.Church CA, Kuhn FA, Mikhail J, Vaughan WC, Weiss RL. Patient and surgeon radiation exposure in balloon catheter sinus ostial dilation. Otolaryngol Head Neck Surg. 2008;138(2):187–191. doi: 10.1016/j.otohns.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 23.Khong JJ, Malhotra R, Selva D, Wormald PJ. Efficacy of endoscopic sinus surgery for paranasal sinus mucocele including modified endoscopic Lothrop procedure for frontal sinus mucocele. J Laryngol Otol. 2004;118(5):352–356. doi: 10.1258/002221504323086534. [DOI] [PubMed] [Google Scholar]
- 24.Chen C, Selva D, Wormald PJ. Endoscopic modified lothrop procedure: an alternative for frontal osteoma excision. Rhinology. 2004;42(4):239–243. [PubMed] [Google Scholar]
- 25.Schlosser RJ, Zachmann G, Harrison S, Gross CW. The endoscopic modified Lothrop: long-term follow-up on 44 patients. Am J Rhinol. 2002;16(2):103–108. [PubMed] [Google Scholar]
- 26.Schulze SL, Loehrl TA, Smith TL. Outcomes of the modified endoscopic Lothrop procedure. Am J Rhinol. 2002;16(5):269–273. [PubMed] [Google Scholar]
- 27.Shirazi MA, Silver AL, Stankiewicz JA. Surgical outcomes following the endoscopic modified Lothrop procedure. Laryngoscope. 2007;117(5):765–769. doi: 10.1097/MLG.0b013e3180337d7b. [DOI] [PubMed] [Google Scholar]
- 28.Wormald PJ. Salvage frontal sinus surgery: the endoscopic modified Lothrop procedure. Laryngoscope. 2003;113(2):276–283. doi: 10.1097/00005537-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 29.Scott NA, Wormald P, Close D, Gallagher R, Anthony A, Maddern GJ. Endoscopic modified Lothrop procedure for the treatment of chronic frontal sinusitis: a systematic review. Otolaryngol Head Neck Surg. 2003;129(4):427–438. doi: 10.1016/S0194-5998(03)01306-8. [DOI] [PubMed] [Google Scholar]
- 30.Myers D, Ersner MS. Trephine in acute frontal sinusitis. J Int Coll Surg. 1951;15(6):686–697. [PubMed] [Google Scholar]
- 31.Gallagher RM, Gross CW. The role of mini-trephination in the management of frontal sinusitis. Am J Rhinol. 1999;13(4):289–293. doi: 10.2500/105065899782102935. [DOI] [PubMed] [Google Scholar]
- 32.McIntosh DL, Mahadevan M. Frontal sinus mini-trephination for acute sinusitis complicated by intracranial infection. Int J Pediatr Otorhinolaryngol. 2007;71(10):1573–1577. doi: 10.1016/j.ijporl.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 33.Hybels RL (1981) Transillumination during osteoplastic frontal sinusotomy. Laryngoscope 91(9 Pt 1):1560 [DOI] [PubMed]
- 34.Citardi MJ, Batra PS. Intraoperative surgical navigation for endoscopic sinus surgery: rationale and indications. Curr Opin Otolaryngol Head Neck Surg. 2007;15(1):23–27. doi: 10.1097/MOO.0b013e3280123130. [DOI] [PubMed] [Google Scholar]
- 35.Fewins JL, Otto PM, Otto RA. Computed tomography-generated templates: a new approach to frontal sinus osteoplastic flap surgery. Am J Rhinol. 2004;18(5):285–289. [PubMed] [Google Scholar]
- 36.Fung MK. Template for frontal osteoplastic flap. Laryngoscope. 1986;96(5):578–579. doi: 10.1288/00005537-198605000-00020. [DOI] [PubMed] [Google Scholar]
- 37.Ulualp SO, Carlson TK, Toohill RJ. Osteoplastic flap versus modified endoscopic Lothrop procedure in patients with frontal sinus disease. Am J Rhinol. 2000;14(1):21–26. doi: 10.2500/105065800781602939. [DOI] [PubMed] [Google Scholar]
- 38.Javer AR, Sillers MJ, Kuhn FA. The frontal sinus unobliteration procedure. Otolaryngol Clin North Am. 2001;34(1):193–210. doi: 10.1016/S0030-6665(05)70306-6. [DOI] [PubMed] [Google Scholar]
- 39.Huang BY, Lloyd KM, DelGaudio JM, Jablonowski E, Hudgins PA. Failed endoscopic sinus surgery: spectrum of CT findings in the frontal recess. Radiographics. 2009;29(1):177–195. doi: 10.1148/rg.291085118. [DOI] [PubMed] [Google Scholar]
- 40.Hosemann W, Schindler E, Wiegrebe E, Gopferich A. Innovative frontal sinus stent acting as a local drug-releasing system. Eur Arch Otorhinolaryngol. 2003;260(3):131–134. doi: 10.1007/s00405-002-0534-2. [DOI] [PubMed] [Google Scholar]
- 41.Hughes JP, Rowe-Jones J. Use of a ureteric pigtail stent as a self-retaining frontal sinus stent. J Laryngol Otol. 2004;118(4):299–301. doi: 10.1258/002221504323012067. [DOI] [PubMed] [Google Scholar]
- 42.Mirza S, Johnson AP. A simple and effective frontal sinus stent. J Laryngol Otol. 2000;114(12):955–956. doi: 10.1258/0022215001904446. [DOI] [PubMed] [Google Scholar]
- 43.Freeman SB, Blom ED. Frontal sinus stents. Laryngoscope. 2000;110(7):1179–1182. doi: 10.1097/00005537-200007000-00021. [DOI] [PubMed] [Google Scholar]
- 44.Weber R, Mai R, Hosemann W, Draf W, Toffel P (2000) The success of 6-month stenting in endonasal frontal sinus surgery. Ear, Nose, and Throat J 79(12):930–2, 4, 7–8 passim [PubMed]
- 45.Chan KO, Gervais M, Tsaparas Y, Genoway KA, Manarey C, Javer AR. Effectiveness of intraoperative mitomycin C in maintaining the patency of a frontal sinusotomy: a preliminary report of a double-blind randomized placebo-controlled trial. Am J Rhinol. 2006;20(3):295–299. doi: 10.2500/ajr.2006.20.2860. [DOI] [PubMed] [Google Scholar]
- 46.Lin D, Witterick IJ. Frontal sinus stents: how long can they be kept in? J Otolaryngol Head Neck Surg. 2008;37(1):119–123. [PubMed] [Google Scholar]
- 47.Banhiran W, Sargi Z, Collins W, Kaza S, Casiano R. Long-term effect of stenting after an endoscopic modified Lothrop procedure. Am J Rhinol. 2006;20(6):595–599. doi: 10.2500/ajr.2006.20.2912. [DOI] [PubMed] [Google Scholar]
- 48.Perloff JR, Palmer JN. Evidence of bacterial biofilms on frontal recess stents in patients with chronic rhinosinusitis. Am J Rhinol. 2004;18(6):377–380. [PubMed] [Google Scholar]
- 49.Beule AG, Steinmeier E, Kaftan H, Biebler KE, Gopferich A, Wolf E, et al. Effects of a dexamethasone-releasing stent on osteoneogenesis in a rabbit model. Am J Rhinol Allergy. 2009;23(4):433–436. doi: 10.2500/ajra.2009.23.3331. [DOI] [PubMed] [Google Scholar]
- 50.Hahn S, Palmer JN, Purkey MT, Kennedy DW, Chiu AG. Indications for external frontal sinus procedures for inflammatory sinus disease. Am J Rhinol Allergy. 2009;23(3):342–347. doi: 10.2500/ajra.2009.23.3327. [DOI] [PubMed] [Google Scholar]