Abstract
Objectives. We investigated tuberculosis (TB) incidence rates and characteristics of patients with TB in large US cities.
Methods. Using the Centers for Disease Control and Prevention's National Tuberculosis Surveillance System data, we categorized 48 cities annually from 2000 to 2007 as reporting decreasing or nondecreasing rates with Joinpoint analysis. We compared demographic, clinical, and treatment characteristics of patients with TB using bivariate and multivariate analyses.
Results. We found that 42 448 patients with TB in 48 cities accounted for 36% of all US patients with TB; these cities comprised 15% of the US population. The average TB incidence rate in the 48 cities (12.1 per 100 000) was higher than that in the US excluding the cities (3.8 per 100 000) but decreased at a faster rate. Nineteen cities had decreasing rates; 29 cities had nondecreasing rates. Patient characteristics did not conclusively distinguish decreasing and nondecreasing rate cities.
Conclusions. A significant TB burden occurs in large US cities. More than half (60%) of the selected cities did not show decreasing TB incidence rates. Studies of city-level variations in migration, socioeconomic status, and resources are needed to improve urban TB control.
In the next 30 years, nearly two thirds of the world's population is expected to live in urban areas.1 Recent publications have emphasized important issues related to urban health, such as population composition, physical and social environment, and availability and access to health services.2–5 In terms of health outcomes, the most urban and rural areas are often considerably disadvantaged compared with suburban areas.6
Tuberculosis (TB) has been called a social disease.7 Social conditions affecting urban areas such as homelessness or those that create other marginalized populations—such as the HIV epidemic, high population density, suboptimal access to health care, and declining public health infrastructures—have been closely associated with TB.8–13 In addition, the migration of people from highly endemic countries from rural areas to cities and urban areas in low-incidence countries has increasingly affected urban TB incidence rates.14–16 In a study of European cities surveyed from 1999 to 2000, 27 of 29 cities reported TB incidence rates higher than their respective national averages.17 A study in Denmark found that TB incidence rates in urban areas were twice as high as were incidence rates in rural areas.18 During and after the 1990s TB resurgence in the United States, TB incidence rates in New York City were 4 times the US national average, with central Harlem experiencing rates 20 times the national average.19
Although TB incidence rates have declined overall in the United States since the mid-1990s, urban areas remain a focus for TB control.13 We examined TB epidemiology in large cities in the United States, using national data from 2000 to 2007 to document patient characteristics associated with urban TB. Furthermore, we evaluated trends in TB incidence case counts and incidence rates and determined characteristics of patients with TB in cities with decreasing versus nondecreasing TB incidence rates from 2000 to 2007.
METHODS
The study population included all verified incident cases of TB reported to the Centers for Disease Control and Prevention's National Tuberculosis Surveillance System (NTSS) for persons residing in selected US cities from 2000 through 2007. Year 2000 was chosen as a baseline because of census data availability as well as recent findings documenting slower average annual decline in nationwide TB rates from 2000 compared with those from 1993 to 2000.20 Case reports that local and state health departments submitted to the NTSS included the demographic, clinical, and treatment information of patients with TB. Foreign-born patients with TB were defined as persons who were born outside the United States to non-US citizen parents and who were diagnosed with TB while resident in the United States.21
Cases of TB were considered to occur in a selected city if the residence address for case counting included the city name and the health department reported it as within city limits. More than 99.0% (99.7%) of the patients with TB met this criteria, and 0.3% had a residence address that included the city name but did not specify whether it was within city limits. The 100 most populated US cities in the 2000 census were initially considered for analysis.22 Of the 100 most populated US cities, we selected only the 48 cities that reported at least 20 cases of TB each year between 2000 and 2007 for this study to be consistent with confidentiality and statistical quality guidelines.23
We tabulated annual TB case counts and incidence rates for all 48 cities for each year and compared relative changes in case counts and rates over the study period with these estimates in the rest of the United States minus these cities. We obtained annual population denominators for 2000 through 2007 for each city and for the remainder of the United States, excluding these cities from the US Census Bureau, Population Estimates Program.24 We calculated changes in incidence rates and case counts from 2000 through 2007 for the 48 cities and for the remainder of the United States using linear regression in Microsoft Excel (Microsoft, Redmond, WA). The average annual percentage change (AAPC) in rates was calculated for each city by using Joinpoint regression software version 3.0 (Statistical Research and Applications Branch, National Cancer Institute, Bethesda, MD) to examine TB rate trends. We considered cities to have experienced a significant decrease in incidence rate from 2000 to 2007 if the estimated AAPC was negative and the 95% confidence interval (CI) around the AAPC excluded zero. We measured the correlation between the population size of the cities and incidence rates of TB throughout this period using the Pearson correlation coefficient.
We performed univariate analysis to describe the patient population diagnosed with TB in the 48 cities over the study period. We performed bivariate analyses to explore differences in characteristics of patients with TB residing in cities experiencing significantly decreasing TB case rates compared with those residing in cities experiencing no significant change in rates from 2000 to 2007. We compared categorical variables using the χ2 test of association, with a P value of less than .05 considered statistically significant. We assessed clinical characteristics for all patients, regardless of disease site or vital status at diagnosis, unless otherwise indicated.
We used multivariate logistic regression to estimate associations between characteristics of patients with TB and the outcome of being diagnosed in a city with a decreasing rate of TB. Odds ratios are defined as the odds of a patient diagnosed with TB in a decreasing rate city having the characteristic of interest compared with a patient diagnosed with TB in a nondecreasing rate city, adjusted for all other factors in the model. The independent variables were age, race/ethnicity, foreign-born origin, HIV status, whether the patient was diagnosed with TB while in a correctional facility, injection drug use, noninjection drug use, and excess alcohol use during the past year. Excess alcohol use was defined using standard Centers for Disease Control and Prevention surveillance criteria, and patients may have participated in alcohol treatment programs or been assessed using screening instruments. We excluded observations from bivariate analyses if variable status was unknown or missing and from univariate and multivariate analyses if variable status was unknown or missing when the percentage missing was less than 2%; otherwise, we analyzed missing values as a separate level of data using indicator coding.
RESULTS
From 2000 through 2007, 42 448 individuals with TB were reported to the NTSS as residing in 1 of the 48 selected cities in the analysis. The population of the cities ranged from 207 000 to 8 156 000 (per year 2000 census data). The sum of TB case counts in the 48 US cities accounted for 36% of the US tuberculosis case burden, yet the sum of these cities’ populations consisted of 15% of the US population. The average number of incident cases of TB for these 48 cities was 111, with a median of 66 (range 26–1075). Change in TB case count reported during the study period ranged from a decrease of 76% to an increase of 56%, with 38 (79%) cities reporting a decrease and 9 (19%) cities reporting an increase in the absolute number of cases of TB in 2007 compared with 2000.
The average annual TB incidence rate of the 48 cities during the study period was 12.1 patients with TB per 100 000 population (median 11.5 per 100 000; range 4.5–32.1 per 100 000). By contrast, the average incidence rate in the United States excluding the 48 cities was 3.8 patients with TB per 100 000 over the same period. There was no correlation between the population size of the cities and incidence rates of TB throughout this period (r = −0.1).
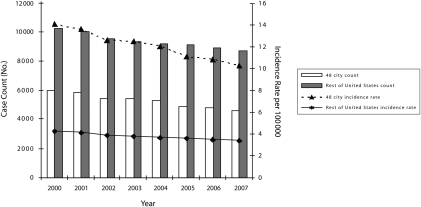
When compared with the rest of the United States (Figure 1), TB incidence rates in the 48 large cities decreased at 4 times the rate from 2000 to 2007 (slope = −0.54 per 100 000/y compared with −0.13 per 100 000/y). However, the rate of the decline in TB case counts in the 48 cities was similar to that of the rest of the United States over the same period (slope = −206 per 100 000/y compared with −215 per 100 000/y).
FIGURE 1.
Tuberculosis case counts and incidence rates comparing 48 large US cities with the rest of the United States: 2000–2007.
Demographic and Clinical Characteristics
From 2000 through 2007, patients with TB in the 48 cities were predominantly aged 25 to 64 years (median = 43 years) and male (63%; Table 1). Thirty-six percent of patients were Black, 28% were Hispanic, and 24% were Asian. Fifty-six percent of patients were born outside the United States, with 42% of foreign-born patients diagnosed within 5 years of arrival in the United States. Twelve percent of patients with TB reported a positive HIV test result, and 7% refused testing. However, 11% of patients were reportedly not offered an HIV test at the time of TB diagnosis, and HIV status was unknown or missing for an additional 27% of patients. Nine percent of patients were homeless the year preceding TB diagnosis, and 3% were diagnosed while resident in correctional facilities. Three percent of patients were injecting drug users, 9% were noninjecting drug users, and 16% reported excessive alcohol use. One percent of patients exhibited multidrug resistance. The proportion of patients completing therapy was 85%, with 7% reported to have died during therapy (all-cause mortality).
TABLE 1.
Characteristics of Patients Diagnosed With Tuberculosis (TB) Residing in 48 Cities With More Than 20 TB Patients Per Year: United States, 2000–2007
| Characteristics | No. (%)a |
| Total | 42 448 (100.00) |
| Age at diagnosis, y | |
| 0–4 | 1451 (3.40) |
| 5–14 | 1160 (2.70) |
| 15–24 | 4535 (10.70) |
| 25–44 | 15 501 (36.50) |
| 45–64 | 12 823 (30.20) |
| ≥ 65 | 6976 (16.40) |
| Gender | |
| Men | 26 685 (62.90) |
| Women | 15 763 (37.10) |
| Race/ethnicity | |
| Hispanicb | 12 059 (28.40) |
| American Indian, non-Hispanic | 221 (0.50) |
| Asian, non-Hispanic | 10 241 (24.10) |
| Black, non-Hispanic | 15 122 (35.60) |
| Native Hawaiian, non-Hispanic | 142 (0.30) |
| White, non-Hispanic | 4476 (10.50) |
| Country of originc | |
| US born | 18 729 (44.10) |
| Foreign born | 23 555 (55.50) |
| Time from US arrival to diagnosis, yd | |
| 0–4 | 9920 (42.10) |
| 5–9 | 3706 (15.70) |
| 10–19 | 4617 (19.60) |
| ≥ 20 | 4302 (18.30) |
| Missing | 1010 (4.30) |
| Sputum smear result | |
| Positive | 15 766 (37.10) |
| Negative | 18 609 (43.80) |
| Not done | 7958 (18.80) |
| Sputum culture result | |
| Positive | 24 703 (58.20) |
| Negative | 9279 (21.90) |
| Not done | 8074 (19.00) |
| Chest radiographic result | |
| Normal | 5222 (12.30) |
| Abnormal | 36 088 (85.00) |
| Not done | 818 (1.90) |
| Chest radiographic abnormalitye | |
| Cavitary | 9025 (25.10) |
| Noncavitary, consistent | 24 665 (68.40) |
| Noncavitary, not consistent | 1517 (4.20) |
| Unknown | 811 (2.30) |
| Site of disease | |
| Pulmonary | 30 143 (71.00) |
| Extrapulmonary | 8392 (19.80) |
| Both | 3904 (9.20) |
| HIV statusf | |
| Negative | 18 681 (44.00) |
| Positive | 4978 (11.70) |
| Indeterminate | 9 (0.02) |
| Refused | 2888 (6.80) |
| Not offered | 4438 (10.50) |
| Test done, results unknown | 585 (1.40) |
| Unknown | 1653 (3.90) |
| Missing | 9216 (21.70) |
| Homeless in past y | |
| No | 37 585 (88.50) |
| Yes | 3760 (8.90) |
| Unknown | 1080 (2.50) |
| Correctional facility residence at time of diagnosis | |
| No | 40 997 (96.60) |
| Yes | 1393 (3.30) |
| Long-term facility residence at time of diagnosis | |
| No | 41 510 (97.80) |
| Yes | 873 (2.10) |
| Injecting drug use in past y | |
| No | 39 753 (93.40) |
| Yes | 1258 (3.00) |
| Unknown | 1422 (3.40) |
| Noninjecting drug use in past y | |
| No | 36 989 (87.10) |
| Yes | 3952 (9.30) |
| Unknown | 1468 (3.50) |
| Excess alcohol use in past yg | |
| No | 34 292 (80.80) |
| Yes | 6771 (16.00) |
| Unknown | 1364 (3.20) |
| Multidrug resistance | |
| Yes | 419 (1.30) |
| No | 31 505 (98.70) |
| Mode of treatmenth | |
| Any directly observed therapy | 25 618 (81.40) |
| All self-administered therapy | 5840 (18.60) |
| Reason therapy stoppedh | |
| Completed | 27 120 (84.80) |
| Moved | 728 (2.30) |
| Lost | 946 (3.00) |
| Refused | 207 (0.70) |
| Died | 2359 (7.40) |
Because of rounding, percentages may not total 100. Missing or unknown data are excluded if they are < 2% of total.
Persons of Hispanic ethnicity may be of any race or multiple races.
Foreign born includes persons born outside the United States, American Samoa, the Federated States of Micronesia, Guam, the Republic of the Marshall Islands, Midway Island, the Commonwealth of the Northern Mariana Islands, Puerto Rico, the Republic of Palau, the US Virgin Islands, and US minor and outlying Pacific islands.
Among foreign-born patients.
Among patients with an abnormal chest x-ray.
HIV status reported for all jurisdictions 2000–2007, except California, which reported patients with TB matched to the California AIDS registry through 2004; all other California data were missing.
Excess alcohol use was defined using standard Centers for Disease Control and Prevention surveillance criteria, and patients may have participated in alcohol treatment programs or been assessed using screening instruments.
Restricted to patients alive at diagnosis who were diagnosed before 2006 and started on at least 1 drug.
Comparison of Decreasing Rate Cities to Nondecreasing Rate Cities
Of the 48 cities, 19 (40%) demonstrated a significantly decreasing rate from 2000 through 2007 (decreasing rate cities AAPC range, –21% [95% CI = −28, −13] to –4% [95% CI = −7, −1]; Technical Appendix Table 1 available as a supplement to the online version of this article at http://www.ajph.org). No cities demonstrated a significantly increasing incidence rate. Twenty-nine cities demonstrated neither a significantly decreasing nor a significantly increasing incidence rate (nondecreasing rate cities AAPC range of −7% [95% CI = −14, 1] to 3% [95% CI = −3, 10]). Decreasing rate cities had a greater percentage of non-Hispanic Black (37% vs 35%) and foreign-born (57% vs 54%) patients than did cities with nondecreasing TB rates (P < .001; Table 2). Patients in decreasing rate cities were less likely to be non-Hispanic White (10% vs 12%). Among patients with HIV status reported to the NTSS, TB and HIV coinfection was higher in the decreasing rate cities (23% vs 19%). The prevalence of reported history of injecting and noninjecting drug use was higher among decreasing rate cities. Decreasing rate cities had a significantly lower percentage of patients with histories of homelessness, diagnosis of TB in a correctional facility, or excess alcohol use in the year before TB diagnosis than did nondecreasing rate cities (Table 2).
TABLE 2.
Characteristics of Patients Diagnosed With Tuberculosis (TB) in Decreasing and Nondecreasing TB Rate Cities: United States, 2000–2007
| Characteristics | Decreasing Rate, No. (%)a (n = 22 172) | Nondecreasing Rate, No. (%)a (n = 20 276) | P |
| Age at diagnosis, y | < .001 | ||
| 0–4 | 700 (3.2) | 751 (3.7) | |
| 5–14 | 557 (2.5) | 603 (3.0) | |
| 15–24 | 2235 (10.1) | 2300 (11.3) | |
| 25–44 | 8205 (37.0) | 7296 (36.0) | |
| 45–64 | 6657 (30.0) | 6166 (30.4) | |
| ≥ 65 | 3818 (17.2) | 3158 (15.6) | |
| Men | 13 872 (62.6) | 12 813 (63.2) | .181 |
| Race/ethnicity | < .001 | ||
| Hispanic | 6165 (28.0) | 5894 (29.2) | |
| American Indian, non-Hispanic | 87 (0.4) | 134 (0.7) | |
| Asian, non-Hispanic | 5571 (25.3) | 4670 (23.1) | |
| Black, non-Hispanic | 8108 (36.8) | 7014 (34.7) | |
| Native Hawaiian, non-Hispanic | 31 (0.1) | 111 (0.6) | |
| White, non-Hispanic | 2093 (9.5) | 2383 (11.8) | |
| Foreign born | 12 625 (57.2) | 10 930 (54.1) | < .001 |
| Time from US arrival to diagnosis, y | < .001 | ||
| 0–4 | 5136 (43.0) | 4784 (45.1) | |
| 5–9 | 1962 (16.4) | 1744 (16.5) | |
| 10–19 | 2574 (21.6) | 2043 (19.3) | |
| ≥ 20 | 2271 (19.0) | 2031 (19.2) | |
| Sputum smear result | .991 | ||
| Positive | 8445 (45.9) | 7321 (45.9) | |
| Negative | 9969 (54.1) | 8640 (54.1) | |
| Sputum culture result | < .001 | ||
| Positive | 12 929 (71.0) | 11 774 (74.6) | |
| Negative | 5271 (29.0) | 4008 (25.4) | |
| Chest radiographic abnormality | < .001 | ||
| Cavitary | 4322 (23.0) | 4703 (28.6) | |
| Noncavitary, consistent | 13 656 (72.7) | 11 009 (67.0) | |
| Noncavitary, not consistent | 801 (4.3) | 716 (4.4) | |
| Site of disease | .982 | ||
| Pulmonary | 15 739 (71.0) | 14 404 (71.1) | |
| Extrapulmonary | 4388 (19.8) | 4004 (19.8) | |
| Both | 2044 (9.2) | 1860 (4.3) | |
| HIV statusb | < .001 | ||
| Positive | 2660 (22.8) | 2318 (19.4) | |
| Negative | 9027 (77.2) | 9654 (80.6) | |
| Homeless in past y | .002 | ||
| Yes | 1835 (8.7) | 1925 (9.6) | |
| No | 19 356 (91.3) | 18 229 (90.5) | |
| Correctional facility residence at diagnosis | < .001 | ||
| Yes | 508 (2.3) | 885 (4.4) | |
| No | 21 637 (97.7) | 19 360 (95.6) | |
| Long-term facility residence at diagnosis | .676 | ||
| Yes | 450 (2.0) | 423 (2.1) | |
| No | 21 693 (98.0) | 19 817 (97.9) | |
| Injecting drug use in past y | .027 | ||
| Yes | 692 (3.3) | 566 (2.9) | |
| No | 20 610 (96.8) | 19 143 (97.1) | |
| Noninjecting drug use in past y | .008 | ||
| Yes | 2131 (10.0) | 1821 (9.3) | |
| No | 19 127 (90.0) | 17 862 (90.8) | |
| Excess alcohol use in past y | < .001 | ||
| Yes | 3355 (15.8) | 3416 (17.3) | |
| No | 17 947 (84.3) | 16 345 (82.7) | |
| Multidrug resistancec | < .001 | ||
| Yes | 270 (1.6) | 149 (1.0) | |
| No | 16 266 (98.4) | 14 865 (99.0) | |
| Directly observed therapyd | < .001 | ||
| Yes | 12 324 (72.4) | 13 294 (92.1) | |
| No | 4695 (27.6) | 1145 (7.9) | |
| Completed treatmentd | .02 | ||
| Yes | 14 560 (85.8) | 12 560 (86.7) | |
| 2406 (14.2) | 1922 (13.3) |
Because of rounding, percentages may not total 100. Missing or unknown data were excluded.
HIV status reported for all jurisdictions 2000–2007, except California, which reported patients with TB matched to the California AIDS registry through 2004; all other California data were missing.
Among those with known results for both isoniazid and rifampin and restricted to patients alive at diagnosis with positive culture and testing results available for isoniazid and rifampin.
Among those with known responses and restricted to patients alive at diagnosis who were diagnosed before 2006 and started on at least 1 drug. Reasons for not completing treatment included moved, lost, refused, died, and other.
Among patients with known sputum culture results, those with TB in the decreasing rate cities were less likely to have positive sputum cultures. Cavitary radiographic abnormality was also lower among these patients (23% vs 29%). Decreasing rate city patients were more likely to be infected with a multidrug-resistant (resistant to at least isoniazid and rifampin) strain of TB than were patients in nondecreasing rate cities. However, pulmonary versus extrapulmonary disease distribution was similar between patients in decreasing and nondecreasing rate cities.
Approximately equal proportions of patients with TB with known outcomes completed treatment in both decreasing (86%) and nondecreasing (87%) rate cities, although the difference was statistically significant (P = .02). However, among decreasing rate cities patients with TB were almost 20% less likely to be reported as having received directly observed therapy (DOT) as compared with TB patients in nondecreasing rate cities (Table 2).
Patients with TB with the following demographics and risk factors had significantly higher odds of living in a decreasing rate city, when compared with referent groups in multivariate adjusted analyses: aged 25 years or older, non-Hispanic Black race, foreign-born, HIV-positive, and history of noninjecting drug use. Patients with TB with the following characteristics had significantly lower odds of living in decreasing rate cities: non-Hispanic American Indian, non-Hispanic White, TB diagnosed in a correctional facility, and excess alcohol use (Table 3).
TABLE 3.
Multivariate Logistic Regression Model of the Association Between Characteristics of Patients and Tuberculosis (TB) Diagnosis in Decreasing and Nondecreasing TB Rate Cities: United States, 2000–2007
| Characteristic (n = 40 996) | AOR (95% CI) |
| Age at diagnosis, y | |
| 0–4 (Ref) | 1.00 |
| 5–14 | 0.95 (0.81, 1.11) |
| 15–24 | 1.08 (0.95, 1.23) |
| 25–44 | 1.25 (1.11, 1.40) |
| 45–64 | 1.20 (1.07, 1.35) |
| ≥65 | 1.25 (1.11, 1.41) |
| Gender | |
| Men (Ref) | 1.00 |
| Women | 0.99 (0.95, 1.04) |
| Race/ethnicity | |
| Hispanic (Ref) | 1.00 |
| American Indian, non-Hispanic | 0.75 (0.56, 0.99) |
| Asian or Native Hawaiian, non-Hispanic | 1.00 (0.95, 1.06) |
| Black, non-Hispanic | 1.23 (1.16, 1.30) |
| White, non-Hispanic | 0.88 (0.81, 0.95) |
| Country of origin | |
| US born (Ref) | 1.00 |
| Foreign born | 1.13 (1.07, 1.19) |
| HIV status | |
| Negative (Ref) | 1.00 |
| Positive | 1.12 (1.04, 1.20) |
| Missinga | 1.39 (1.33, 1.45) |
| Homeless in past y | |
| No (Ref) | 1.00 |
| Yes | 0.94 (0.87, 1.02) |
| Unknown | 10.48 (8.22, 13.37) |
| Correctional facility residence at time of diagnosis | |
| No (Ref) | 1.00 |
| Yes | 0.48 (0.43, 0.54) |
| Injecting drug use in past y | |
| No (Ref) | 1.00 |
| Yes | 1.13 (0.99, 1.28) |
| Unknown | 0.68 (0.50, 0.93) |
| Noninjecting drug use in past y | |
| No (Ref) | 1.00 |
| Yes | 1.26 (1.17, 1.37) |
| Unknown | 1.20 (0.88, 1.63) |
| Excess alcohol use in past yb | |
| No (Ref) | 1.00 |
| Yes | 0.91 (0.86, 0.97) |
| Unknown | 1.34 (1.05, 1.71) |
Note. AOR = adjusted odds ratio; CI = confidence interval. All confirmed cases of TB in 48 included cities, 2000–2007, were adjusted for age, race, foreign born, time since arrival, HIV status, correctional facility residence at the time of diagnosis, injecting drug use, noninjecting drug use, and excess alcohol use.
Missing includes indeterminate results, refusals, test not offered, test done but results unknown, missing results, and unknown whether test done. California reported cases of patients with TB matched to the California AIDS registry through 2004 as HIV positive; all other California HIV data were missing.
Excess alcohol use was defined using standard Centers for Disease Control and Prevention surveillance criteria, and patients may have participated in alcohol treatment programs or assessment using screening instruments.
Significant differences were observed between decreasing and nondecreasing rate cities when select city-level variables were compared on the basis of the 2000 census, including race, foreign birth, and socioeconomic factors (Technical Appendix Table 2 available as a supplement to the online version of this article at http://www.ajph.org).
DISCUSSION
We used national TB surveillance data to describe characteristics and trends of cases of patients with TB in large cities in the United States. We believe there are 2 important findings. First, the 48 cities we selected accounted for 36% of the US tuberculosis case burden, although only 15% of the US population lived in these cities. Second, 29 of the 48 cities showed no significant change in TB incidence rates over the course of the study, which raises concerns for the elimination of TB.
The 48 selected cities had a rate of decline in TB incidence rate that was 4 times as fast as that of the rest of the United States, but the incidence rates of the large cities remained more than twice as high as reported in the rest of the United States. The decline in TB incidence rates may reflect successful TB control interventions. However, persistently high urban incidence rates may be related to high proportions of individuals with risk factors for progression to TB and with latent TB infection, including minority groups who are foreign born and of lower socioeconomic status.
TB case counts in urban centers remain disproportionately higher than does the percentage of the US population residing in those cities. The 48 large cities selected for this study showed wide variability in their change in TB case count over the study period, with 9 of 48 cities (19%) having an increase in case counts when comparing 2007 and 2000. Although change in the incidence rate may reflect the relative success of TB control, a larger case count affects the work burden for local TB control programs.
The TB epidemiology of the selected 48 cities mirrors overall US tuberculosis epidemiology, with higher TB rates among minorities and among the foreign born in 2007.21 For selected risk factors, 6% of patients with TB in the United States were homeless, 4% were diagnosed with TB in correctional facilities, and 13% had a history of excess alcohol use.20 Substance abuse has been associated with both TB transmission and generation of secondary cases of patients with TB.25,26 Increased risk for TB transmission has also been well documented in both jails21,27 and homeless shelters.28 Untreated HIV infection remains an important risk factor for progression to TB disease among individuals with latent TB infection.29 We examined sputum smear and chest radiographs because higher bacillary load and abnormal radiographs may indicate an increased period of infectivity in the community, a delay in treatment, and a more severe form of the disease.30
More than half of the patients with TB in this study were born outside the United States. TB case rates for foreign-born persons from selected countries and world regions remain elevated because of a higher prevalence of latent TB infection in the country of origin.31 Because foreign-born persons are more likely to have been infected in the past, they are also more likely to have reactivated TB. Population-based studies have provided both epidemiological and molecular evidence of the lack of recent transmission among foreign-born patients with TB,32,33 and recent findings highlight increased TB incidence with greater time since US entry among some age groups.34
Use of DOT in the 48 cities was 81%, which is comparable with US data from 2000 to 2005.21 Interestingly, DOT was used less often in the decreasing rate cities. DOT reduces the frequency of primary and acquired drug resistance and relapse and potentially reduces the transmission of TB in a community.20,35 DOT is an important component of TB control, yet we did not examine the effect of DOT on individual patient outcomes. There may be substantial misclassification of DOT status; a recent study from California found concordance for recording DOT between medical records and TB case reports was only 48%.36 Moreover, declines in TB incidence may result primarily from improvements in city health systems and economic growth, rather than from DOT.37–39 Declines in decreasing rate cities may be the result of migration to more affluent cities or less urban areas, which we were not able to measure. Furthermore, cities using DOT more judiciously may spend their resources on other activities, such as increased community engagement for TB control.
Although statistically significant, differences in patient characteristics were small when comparing the 2 groups of cities. With our ecological study design, we could not conclusively determine which patient factors were associated with decreasing incidence rates. The extent to which characteristics of urban areas are generalizable across cities has not been adequately assessed and serves as a limitation to the scope of our study, given the inclusion of only 48 cities because of the unstable number of cases of patients with TB (< 20 patients with TB per year) in other cities. Within-city disparities also occurred and were not captured in this analysis.
Another limitation of our study is that NTSS data were self-reported by public health jurisdictions, and some variables were reported with high rates of missing or unknown values, which were noninformative for our analyses. Because we had significant results for unknown values of categorical variables, we may not be able to rely on the interpretation of the multivariate model results.
Decreases in incidence rates among cities may be influenced by factors that are unavailable for this study, such as TB control program funding levels, public health staffing, type and pattern of immigration and migration rates, and extent of community engagement for TB prevention and control activities. Additionally, socioeconomic context (both individually and on a citywide basis), such as education, income, and poverty status, may contribute to TB rates independently of effects we measured.40–42 An alternative explanation is that areas with patients with more TB risk factors attract more funding, including federal, state, and local sources, to control TB. Such a hypothesis would need to be followed up with a more comprehensive study analyzing the association of TB with funding and resource data.
Our study illustrates the need to address the continuing challenges of urban TB control and highlights some of the factors contributing to variability of TB trends among cities. It is important to detail how specific characteristics of the urban environment shape health and how observations may extend to different urban contexts.43 Future studies could thus examine different groupings of cities, potentially chosen to reflect the demographic diversity of US cities. Our results can serve as a starting point to identify new focus areas for program intervention or needed enhancement of current TB control infrastructure in urban settings.
Acknowledgments
The National Association of County and City Health Officials provided general support for this work.
We would also like to thank the Centers for Disease Control and Prevention, Division of Tuberculosis Elimination for providing access to the NTSS data. We would like to thank Thomas Navin at the Centers for Disease Control and Prevention, David Fleming and David Bibus at Public Health—Seattle and King County, and Masae Kawamura at the San Francisco Department of Health for their helpful comments and suggestions. We also thank the health departments who reported data for these analyses.
Human Participant Protection
No institutional review board approval was necessary because data were obtained from secondary sources.
References
- 1.Brockerhoff M. The urban demographic revolution. Popul Today. 2000;28(6):1–2 [PubMed] [Google Scholar]
- 2.Freudenberg N. Urban Health: Cities and the Health of the Public. Nashville, TN: Vanderbilt University Press; 2005 [Google Scholar]
- 3.Vlahov D, Freudenberg N, Proietti F, et al. Urban as a determinant of health. J Urban Health. 2007;84(suppl 3):i16–i26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galea S, Freudenberg N, Vlahov D. Cities and population health. Soc Sci Med. 2005;60(5):1017–1033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baker J, Schuler N. Analyzing Urban Poverty: A Summary of Methods and Approaches. World Bank Policy Research Working Paper no 3399; Washington, DC: World Bank; 2004 [Google Scholar]
- 6.Eberhardt MS, Pamuk ER. The importance of place of residence: examining health in rural and nonrural areas. Am J Public Health. 2004;94(10):1682–1686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dubos J, Rosenkrantz B. The White Plague: Tuberculosis, Man, and Society. Newark, NJ: Rutgers University Press; 1987 [Google Scholar]
- 8.Cantwell MF, Snider DE, Jr., Cauthen GM, Onorato IM. Epidemiology of tuberculosis in the United States, 1985 through 1992. JAMA. 1994;272(7):535–539 [PubMed] [Google Scholar]
- 9.Chaulk CP, Moore-Rice K, Rizzo R, Chaisson RE. Eleven years of community-based directly observed therapy for tuberculosis. JAMA. 1995;274(12):945–951 [PubMed] [Google Scholar]
- 10.Small PM, Hopewell PC, Singh SP, et al. The epidemiology of tuberculosis in San Francisco. A population-based study using conventional and molecular methods. N Engl J Med. 1994;330(24):1703–1709 [DOI] [PubMed] [Google Scholar]
- 11.Brudney K, Dobkin J. Resurgent tuberculosis in New York City. Human immunodeficiency virus, homelessness, and the decline of tuberculosis control programs. Am Rev Respir Dis. 1991;144(4):745–749 [DOI] [PubMed] [Google Scholar]
- 12.Barnes PF. Tuberculosis among the inner city poor. Int J Tuberc Lung Dis. 1998;2(9 suppl. 1):S41–S45 [PubMed] [Google Scholar]
- 13.Institute of Medicine Ending Neglect: The Elimination of Tuberculosis in the United States. Washington, DC: National Academic Press; 2000 [Google Scholar]
- 14.Rose RC, III, McGowan JE., Jr. Urban tuberculosis: some modern problems. Am J Med Sci. 1984;287(1):24–26 [DOI] [PubMed] [Google Scholar]
- 15.Fujiwara PI, Frieden TR. Tuberculosis epidemiology and control in the inner city. : Rom WM, Garay S, Tuberculosis. New York: Little Brown; 1996: 99–112 [Google Scholar]
- 16.McGowan JE, Jr, Blumberg HM. Inner-city tuberculosis in the USA. J Hosp Infect. 1995;30(suppl):282–295 [DOI] [PubMed] [Google Scholar]
- 17.Hayward AC, Darton T, Van-Tam J, Watson JM, Coker R, Schwoebel V. Epidemiology and control of tuberculosis in Western European cities. Int J Tuberc Lung Dis. 2003;7(8):751–757 [PubMed] [Google Scholar]
- 18.Horwitz O, Knudsen J. A follow-up study of tuberculosis incidence and general mortality in various occupational-social groups of the Danish population. Bull World Health Organ. 1961;24:793–805 [PMC free article] [PubMed] [Google Scholar]
- 19.Frieden T, Fujiwara P, Washko R, Hamburg M. Tuberculosis in New York City—turning the tide. N Engl J Med. 1995;333(4):229–233 [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention Decrease in reported tuberculosis cases—United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(10):289–294 [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention Reported Tuberculosis in the United States, 2007. Atlanta, GA: US Department of Health and Human Services; 2008 [Google Scholar]
- 22.US Census Bureau Annual Estimates of the Population for Incorporated Places Over 100,000, Ranked by July 1, 2007 Population: April 1, 2000 to July 1, 2007. Available at: http://www.census.gov/popest/cities/SUB-EST2007.html. Accessed August 16, 2010
- 23.National Center for Health Statistics NCHS Staff Manual on Confidentiality. Available at: http://www.cdc.gov/nchs/data/misc/staffmanual2004.pdf. Accessed June 7, 2010
- 24.US Census Bureau Population Estimates Program. Available at: http://www.census.gov/popest/estimates.html. Accessed August 16, 2010
- 25.Rodrigo T, Caylà J, García de Olalla P, et al. Characteristics of tuberculosis patients who generate secondary cases. Int J Tuberc Lung Dis. 1997;1(4):352–357 [PubMed] [Google Scholar]
- 26.Oeltmann JE, Oren E, Haddad MB, et al. Tuberculosis outbreak in marijuana users, Seattle, Washington, 2004. Emerg Infect Dis. 2006;12(7):1156–1159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roberts CA, Lobato MN, Bazerman LB, Kling R, Reichard AA, Hammett TM. Tuberculosis prevention and control in large jails: a challenge to tuberculosis elimination. Am J Prev Med. 2006;30(2):125–130 [DOI] [PubMed] [Google Scholar]
- 28.Curtis AB, Ridzon R, Novick LF, et al. Analysis of mycobacterium tuberculosis transmission patterns in a homeless shelter outbreak. Int J Tuberc Lung Dis. 2000;4(4):308–313 [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention Targeted tuberculin testing and treatment of latent tuberculosis infection. MMWR Recomm Rep. 2000;49(RR-6):1–51 [PubMed] [Google Scholar]
- 30.Taylor Z, Nolan CM, Blumberg HM, et al. ; American Thoracic Society. Controlling tuberculosis in the United States: recommendations from the American Thoracic Society, CDC, and the Infectious Diseases Society of America. MMWR Recomm Rep. 2005;54(RR-12):1–81 [PubMed] [Google Scholar]
- 31.Cain KP, Haley CA, Armstrong LR, et al. Tuberculosis among foreign-born persons in the United States: achieving tuberculosis elimination. Am J Respir Crit Care Med. 2007;175(1):75–79 [DOI] [PubMed] [Google Scholar]
- 32.Ellis BA, Crawford JT, Braden CR, et al. ; National Tuberculosis Genotyping and Surveillance Network Work Group. Molecular epidemiology of tuberculosis in a sentinel surveillance population. Emerg Infect Dis. 2002;8(11):1197–1209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borgdorff MW, Behr MA, Nagelkerke NJ, Hopewell PC, Small PM. Transmission of tuberculosis in San Francisco and its association with immigration and ethnicity. Int J Tuberc Lung Dis. 2000;4(4):287–294 [PubMed] [Google Scholar]
- 34.Cain KP, Benoit MD, Winston CA, MacKenzie WR. Tuberculosis among foreign-born persons in the United States. JAMA. 2008;300(4):405–412 [DOI] [PubMed] [Google Scholar]
- 35.Weis SE, Slocum PC, Blais FX, et al. The effect of directly observed therapy on the rates of drug resistance and relapse in tuberculosis. N Engl J Med. 1994;330(17):1179–1184 [DOI] [PubMed] [Google Scholar]
- 36.Sprinson JE, Lawton ES, Porco TC, Flood JM, Westenhouse JL. Assessing the validity of tuberculosis surveillance data in California. BMC Public Health. 2006;6:217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dye C, Lonnroth K, Jaramillo E, Williams BG, Raviglione M. Trends in tuberculosis incidence and their determinants in 134 countries. Bull World Health Organ. 2009;87(9):683–691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Oxlade O, Schwartzman K, Behr MA, et al. Global tuberculosis trends: a reflection of changes in tuberculosis control or in population health? Int J Tuberc Lung Dis. 2009;13(10):1238–1246 [PubMed] [Google Scholar]
- 39.Volmink J, Garner P. Directly observed therapy for treating tuberculosis. Cochrane Database of Syst Rev. 2007;4:CD003343 [DOI] [PubMed] [Google Scholar]
- 40.Davidow AL, Mangura BT, Napolitano EC, Reichman LB. Rethinking the socioeconomics and geography of tuberculosis among foreign-born residents of New Jersey, 1994–1999. Am J Public Health. 2003;93(6):1007–1012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cantwell MF, McKenna MT, McCray E, Onorato IM. Tuberculosis and race/ethnicity in the United States: impact of socioeconomic status. Am J Respir Crit Care Med. 1998;157(4 pt 1):1016–1020 [DOI] [PubMed] [Google Scholar]
- 42.Acevedo-Garcia D. Zip code-level risk factors for tuberculosis: neighborhood environment and residential segregation in New Jersey, 1985–1992. Am J Public Health. 2001;91(5):734–741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vlahov D, Gibble E, Freudenberg N, Galea S. Cities and health: history, approaches, and key questions. Acad Med. 2004;79(12):1133–1138 [DOI] [PubMed] [Google Scholar]