Abstract
Objective
Skin cancer is a major public health concern in the United States. Chiropractic physicians and interns need to recognize and refer patients with atypical moles and skin cancer. The purpose of this study was to test chiropractic interns about their current knowledge, practices, and perceptions of atypical moles and skin cancer.
Methods
This study was a cross-sectional study using chiropractic interns at 2 chiropractic colleges who received a 26-item survey that used a 5-point Likert scale involving close-ended questions regarding demographics, importance, knowledge, and clinical images regarding atypical moles and skin cancer. Frequencies and odds ratios (ORs) were generated using multiple regression models.
Results
A total of 217 surveys were collected in the study. The importance of skin cancer recognition as a predictor of practice patterns was examined. Interns who stated it was “important/very important” to recognize skin cancer were slightly more likely to state they “frequently/always” scanned patient's skin on the initial visit, were more likely to state they “frequently/always” scanned on a treatment visit (OR = 3.30; 95% confidence interval [CI], 1.6-6.9), and stated they had noticed a mole that needed follow-up (OR = 3.04; 95% CI, 1.52-6.10). However, interns were no more likely to state they documented moles in the soap notes (OR = 1.38; 95% CI, 0.77-2.47) or to know the warning signs of melanoma (OR = 0.76; 95% CI, 0.40-1.46).
Conclusion
As skin cancer continues to increase in prevalence, chiropractic interns can serve in the primary screening process of patients with atypical moles; and chiropractic education should emphasize the opportunity to detect and assess atypical moles as a routine part of primary prevention in clinical education.
Key indexing terms: Chiropractic, Skin cancer, Atypical moles, Early detection, Prevention, Screening practices, Public health
Introduction
Public health concerns of skin cancer
Although most incidence rates of cancers have stabilized or decreased in the United States, rates of skin cancers including melanomas have increased in the last few decades. More than a million people are diagnosed annually with the 2 most frequent forms of skin cancer, which are basal cell and squamous cell carcinoma. Skin cancer is the most common form of all cancers, which makes skin cancer a major public health concern.1 In addition, an estimated 5% to 10% of the population has atypical moles (AMs), with a higher incidence in immune-suppressed adults.2 Because AMs are markers for melanoma and are possible precursor lesions, careful clinical attention is warranted for all health care clinicians who have the opportunity to evaluate a patient's skin. Melanoma is the deadliest form of skin cancer. The early detection of AMs can offer the patient an opportunity to have them removed and therefore potentially reduce skin cancer risks.3
Basal cell carcinoma is the most common form of skin cancer, and about 1 million of the cases diagnosed annually are basal cell carcinoma.4 Basal cell carcinomas are rarely fatal, but can be highly disfiguring. Squamous cell carcinoma is the second most common form of skin cancer in individuals 15 to 29 years of age. More than 250 000 cases are diagnosed each year, resulting in approximately 2500 deaths.5,6 In the United States, melanoma of the skin is the sixth most common type of cancer in white men and women.7 The incidence of both melanoma and nonmelanoma skin cancer has been increasing over the past 3 decades.8,9 Melanoma is the only detectable cancer for which death rates are not decreasing, yet health care provider screening rates have remained the same.10
Screening for prevention and early detection
Screening for pathological skin lesions and AMs has been evaluated from a public health screening and individual level as well.11 Current literature has indicated that random screening of the population has not proven to be an effective means for reducing the risk or incidence of skin cancers.12,13 However, increasing the clinical skills of primary care providers in the identification of AMs or populations at greater risks of AMs may theoretically result in reducing the incidence of potential pathological lesions.14,15 With the typical American only seeing a primary care physician about twice a year,16 the potential for a doctor of chiropractic (DC) to screen and detect AMs could be substantial. An average chiropractic patient will be seen multiple times per year, and some patients even use DCs on a regular basis as a part of their routine health and wellness plan.17
Education is the key element to awareness and prevention when it comes to skin cancer. With this in mind, the purpose of this study was to test interns at 2 colleges as to their perceptions regarding the importance of DCs identifying possible skin cancer or AMs and to investigate their current knowledge regarding detection of an AM. An additional aim was to determine how frequently they assessed for, identified, and referred patients with AMs.
Methods
Study design, material, and subjects
The study was a cross-sectional epidemiological study using a survey design. The survey instrument was a self-reporting, anonymous questionnaire that was designed to capture information on the perceptions, current practices, and knowledge of chiropractic interns regarding the detection of AMs The 2-page document was divided into 3 sections: a section that queried the perceptions regarding the importance of DCs identifying possible skin cancer or AMs and their current practices (how frequently they assessed for, identified, and referred out patients with AMs) and a section that included 4 clinical images representing normal typical vs AMs and asked questions to assess the knowledge of the interns relating to skin cancer awareness. A final section that gathered demographic information was included in the survey. Most of the survey questions were close-ended using a 5-point Likert scale. Questions were generated by the study investigators and were critiqued by research colleagues. A draft version was pretested on a pilot group of students, and the feedback was used in augmentation of the survey. The final version of the survey (Fig 1) was tested for face validity by both research and clinical faculty before administering.
Fig 1.
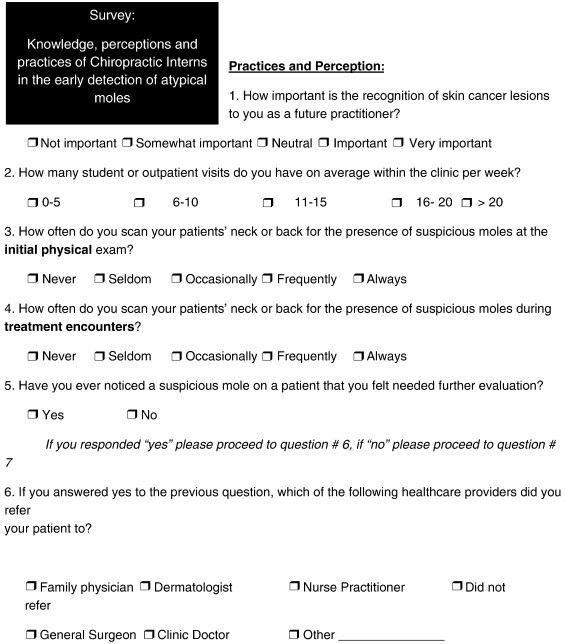
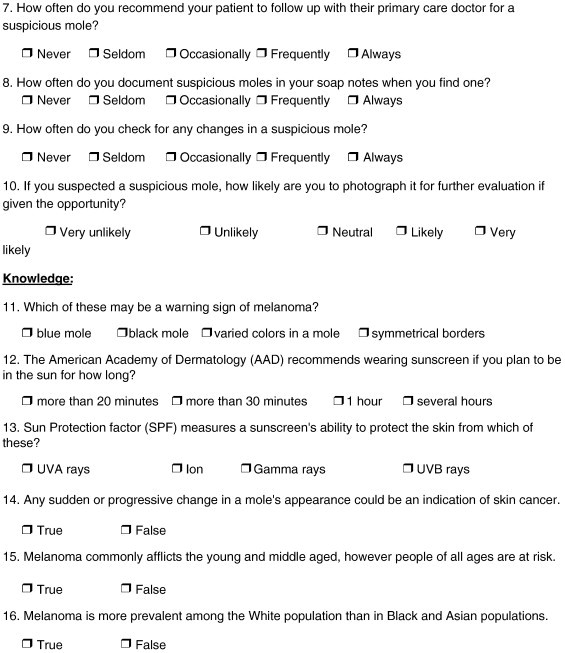
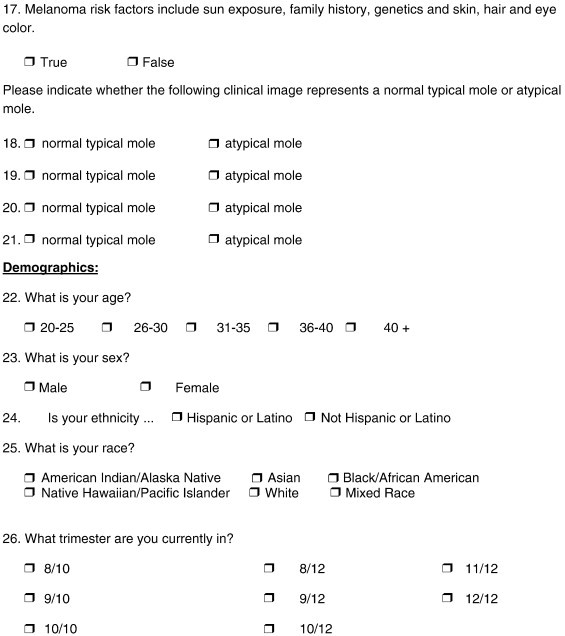
Atypical mole survey.
The actual survey was administered to a convenience sample of chiropractic interns at 2 different chiropractic institutions in the United States. Before administering the survey, interns were advised that their participation in this study was voluntary and that participation or nonparticipation would not affect their relationships with their professors, clinic, or the college in any way. The colleges that participated in this study were located in different regions of the United States, with campus 1 in the Midwest and campus 2 in the Southwest. This study was approved by both the research committees and the institutional review boards of the participating institutions.
Statistical methods and analysis
All surveys were collected and sent to the primary research site for the project and entered into an SPSS for Windows version 16.0 (SPSS Inc, Chicago, IL) database. Before statistical analysis, the data set was reviewed and cleaned by the project biostatistician. Surveys with largely incomplete responses were eliminated from the final analysis. Frequencies and distributions across demographics were generated for each question. Responses related to the major outcomes (perceptions of importance and current knowledge regarding detection of AM, and current practices regarding scanning patients for AM and referring patients with AM) were dichotomized. Odds ratios (ORs) and 95% confidence intervals (CIs) were generated from multiple logistic regression models that controlled for possible confounding demographic variables. All inferences were made based on the α = .05 level of significance.
Results
Study participant demographics
A total of 217 surveys were collected in the study, with campus 1 making up 37% of the sample (n = 81) and campus 2, with a larger enrollment, making up 63% (n = 136). The study population consisted of 57% male, 81% white, and 6% black; and other races made up the rest of the sample. Approximately 79% of the chiropractic interns were between the ages of 20 and 30 years.
Importance of recognizing skin cancer
In the perception of interns related to the importance of their recognizing skin cancer signs among their patients, 85.7% said it was either “important or very important.” Only 14.3% gave a neutral to “not important” response.
Scanning practices with patients
When asked how often they scan the neck or back of a patient for skin lesions on an initial examination, 66.2% said they “frequently or always” did this. Whereas 33.8% said they did this “often to never,” only 5.7% of the participants said they “never” scanned a patient's skin during an initial examination. As to scanning the skin during a routine visit, 22.6% said they did this “frequently to always.” And although a majority fell into the “often to never” categories, 18.4% said they “never” did this on a routine visit and 29% said they “sometimes” did.
Detection of moles needing further evaluation and referral patterns
When the interns we asked about further evaluation of AMs and referral patterns, 24.9% (n = 54) said they had seen a mole they felt was suspicious and needing further evaluation. They stated either a dermatologist (22.6%) or general surgeon (21.3%) was where they referred the patient. Only 14.8% of the interns referred a patient to the family doctor, and 16.4% said their supervising clinic doctor. The remainder did not answer the question as to referral patterns. As to whether they recommended the patient follow up with their primary care doctor, only 26.4% said they “always” recommended this. Another 12% said they “frequently” recommended this, and 18.1% said they “often” did. However, 43.5% said they “seldom or never” recommended this level of follow-up.
Documentation of an AM in patient chart and tracking of changes
Regarding how often interns documented a mole that looked abnormal or atypical in the patient's chart, 32.6% said they “always” did this, 34.4% said they “never” did, and the rest stated they “frequently to seldom” did. As to checking the patient for changes in an AM they had discovered, only 27.2% said they “frequently to always” did this, whereas 26.8% stated they “never” did. As to documenting the mole with a photograph if this were an option, 60.2% said they would “likely to very likely” do this; and 38.6% said they would “unlikely to very unlikely” perform this level of surveillance.
Knowledge regarding signs of melanoma and prevention of skin cancer
When asked to identify the color that is a warning of a potential melanoma, 76.8% accurately chose “variation in color” of a mole as the correct response; and 72.4% accurately selected the correct response for using sunscreen if in the sun for longer than 20 minutes. However, only 28.8% could accurately state what type of UV light sun protection factor in a sunscreen typically blocks. When asked about sudden progression or change in a mole being indicative of skin cancer, 97.7% accurately stated this was true; and 80.5% knew melanoma could be a risk for most ages. Furthermore, 88.9% accurately stated that melanoma was more prevalent in whites and that risk increased with age (97.7% stated this was a true statement).
Identification of an AM in a color photograph
When provided with 4 slides showing various moles in color photographs, the most obvious pathological melanoma or AM was accurately identified by 95.9% of the participants. However, when slight variations of an atypical, yet nonmalignant mole was observed, fewer interns were able to accurately identify the AMs. When asked to accurately identify a typical nonpathological nevus, 93.5% were able to do so. A table with complete results is labeled Table 1.
Table 1.
Demographics, perceptions on importance, knowledge, and current practices of interns regarding identification of AMs
| Demographics | ||||||
| Age range (y) (n = 216) | N | (%) | ||||
| 20-25 | 64 | (29.6) | ||||
| 26-30 | 107 | (49.5) | ||||
| >30 | 45 | (20.9) | ||||
| Sex (n = 216) | ||||||
| Male | 124 | (57.4) | ||||
| Female | 92 | (42.6) | ||||
| Race (n = 125) | ||||||
| White | 173 | (80.5) | ||||
| Black | 13 | (6) | ||||
| Other | 29 | (13.5) | ||||
| Importance of recognizing skin cancer (n = 217) | ||||||
| Very important | 124 | (57.1) | ||||
| Important | 62 | (28.6) | ||||
| Neutral | 16 | (7.4) | ||||
| Somewhat | 12 | (5.5) | ||||
| Not important | 3 | (1.4) | ||||
| Knowledge/awareness | Total responding | Yes n (%) | No n (%) | |||
| Warning signs of melanoma | 216 | 166 (76.9) | 50 (23.1) | |||
| Sudden change in mole is indication of possible cancer | 216 | 211 (97.7) | 5 (2.3) | |||
| Aware all ages are at risk | 215 | 173 (80.5) | 42 (19.5) | |||
| >Prevalence in whites | 217 | 193 (88.9) | 24 (11.1) | |||
| Risk increases with age | 215 | 210 (97.7) | 5 (2.3) | |||
| Greatest risk for male is on backa | 134 | 62 (46.3) | 72 (53.3) | |||
| Greatest risk for female is on back of legsa | 134 | 21 (15.7) | 113 (84.3) | |||
| Correctly ID probable melanoma in photo | 217 | 208 (95.9) | 9 (4.1) | |||
| Correctly ID AM in photo | 217 | 67 (30.9) | 150 (69.1) | |||
| Correctly ID normal nevus in photo | 217 | 202 (93.5) | 14 (6.5) | |||
| Correctly ID AM #2 in photo | 217 | 190 (87.6) | 27 (12.4) | |||
| Scanning practices | Initial visit (n = 215) | Treatment visit (n = 217) | ||||
| Scanned frequently/always | 143 (66.2) | 49 (22.6) | ||||
| Did not | 72 (33.8) | 168 (77.4) | ||||
| Noticed suspicious mole needing evaluation (n = 217) | ||||||
| Yes | 57 | (24.9) | ||||
| No | 163 | (75.1) | ||||
| If seen suspicious mole, made referral (n = 51/94%) | ||||||
| Family medical doctor | 8 | (15.7) | ||||
| General surgeon | 9 | (17.7) | ||||
| Dermatologist | 25 | (49) | ||||
| Clinic supervisor | 9 | (17.6) | ||||
| Did not refer | 3 | (5.6) | ||||
| Practices regarding documenting and follow-up on AMs | ||||||
| Activity/practice | Total n | Always | Frequently | Often | Seldom | Never |
| Documents AM in patient chart | 215 | 70 (32.6) | 23 (10.7) | 18 (8.4) | 30 (14.0) | 74 (34.4) |
| Checks for changes in AM | 213 | 28 (13.1) | 30 (14.1) | 51 (23.9) | 47 (22.1) | 57 (26.8) |
Included only at campus 2.
At campus 2, two additional questions were asked about the most common sites for melanomas in men and women; and of 134 answering this question, 43.3% accurately identified the back as the most common site for melanoma in men, and only 15.7% identified the lower limb as the most common site for melanoma in women.
Importance of skin cancer recognition as a predictor of practice patterns
Those who stated it was “important/very important” to recognize skin cancer in question 1 were more likely to state they “frequently/always” scanned patient's skin on the initial visit (OR = 1.64; 95% CI, 0.9-2.9), those who were more likely to state they “frequently/always” scanned on a treatment visit (OR = 3.30; 95% CI, 1.6-6.9), and those who stated they had noticed a mole that needed further follow-up to a practitioner (OR = 3.04; 95% CI 1.52-6.10). However, they were no more likely to state they documented moles in the notes (OR = 1.38 95%; CI, 0.77-2.47) or to know the warning signs of melanoma (OR = 0.76; 95% CI, 0.40-1.46). In addition, this importance level only predicted who could accurately identify the most obvious AM that was pathognomonic of melanoma (OR = 4.97; 95% CI, 1.01-24.48). Whereas age and sex did not affect the rate at which participants stated identification was important, race did. Whites were less likely to state it was important to identify these lesions when compared with all other racial groups (OR = 0.47; 95% CI, 0.22-0.97). A table with complete OR results is labeled Table 2.
Table 2.
Cross-tabulation of importance of recognition of skin cancer in question 1 with practice behaviors and correct identification of photographs and most common location based on sex
| Activity or practice behavior | OR 95% (CI) | P Value |
|---|---|---|
| Likely to scan patient on first visit | 1.64 (0.9-2.9) | .09 |
| Likely to scan patient on treat visit | 3.30 (1.60-6.9) | .002a |
| Notices mole needing follow-up | 3.04 (1.52-6.10) | .002a |
| Documents AM in notes | 1.38 (0.77-2.47) | .29 |
| Knows warnings of melanoma | 0.76 (0.77-1.46) | .41 |
| ID image of probable melanoma in photo | 4.97 (1.01-24.48) | .049a |
| ID image of AM in photo | 0.98 (0.55-1.74) | .30 |
| ID image of normal nevus in photo | 1.35 (0.46-3.99) | .59 |
| ID image of AM #2 in photo | 1.28 (0.57-2.86) | .55 |
| Greatest risk for male is back | 1.14 (0.58-2.25) | .71 |
| Greatest risk for female is legs | 2.11 (0.79-5.62) | .14 |
Statistically significant α = .05.
Discussion
The World Health Organization estimates that as many as 65 000 people per year worldwide die mostly from malignant skin cancer.18 People with more than 50 AMs or a family history of melanoma are at an increased risk of developing melanoma, and the American Cancer Society recommends a skin cancer–related checkup and counseling about sun exposure as part of any periodic health examination for men and women beginning at age 20 years.1 Chiropractic physicians and interns may be in an optimal position to provide early detection, screening, and risk education for AMs with frequent patient encounters due to the nature and their scope of practice. These practitioners routinely interact with patients with musculoskeletal maladies involving the posterior aspect of the head, neck, and back and therefore have an increased opportunity for frequent surveillance of AMs where they may often go unnoticed by the patient. This is especially so when the patient is gowned or, in the case of a male patient, has his shirt removed for physical treatments.
In theory, education and early detection of melanoma and identification of potential markers or precursor lesions could substantially reduce morbidity and mortality associated with melanoma, although a lack of randomized trials on the topic is noted. This preliminary assessment at 2 campuses indicates that, in the most obvious of cases, interns can identify a clearly pathological mole when they see one. Although screening on an initial examination seems common, some may not routinely scan patient for AMs This is unfortunate because they may see the patient with more frequency than the primary care doctor in a given year, and studies have demonstrated that increasing the primary care doctors' ability to screen can potentially detect pathologies and/or provide those at high risk an opportunity for education and advise on risk prevention.19 Training chiropractors to detect these AMs on routine visits and educate patients as to risks as well as self-examination could theoretically reduce morbidity and early mortality from skin cancer if this is emphasized as part of routine primary prevention.
This study, though preliminary, also indicates some gaps that need to be filled in training at these institutions. Only 26% stated they suggested the patient follow up with their primary care physician. Clearly, the primary care physician needs to know about any pathological change in the patient, and this causes concern. In addition, the level of self-reported documentation in the patient file was low (32.6%). This is indicative of poor charting practices; and if it is not recorded, it is hard to see how the patient could adequately be followed for changes in an AM. Only 27.2% said they “frequently/always” checked for changes in an AM with patients. Once again, this is concerning. And although most knew variation in color and sudden progression or change in a mole were signs of melanoma in photographs, only the most obvious could be accurately detected. Atypical moles that were not melanoma were not as easily detected and, in fact, at times were detected by the minority of interns in the sample. However, the same has been said about primary care doctors when it comes to the ability to adequately detect AMs needing further evaluation.19 Clinically, DCs will see patients with more frequency than their primary care physician; therefore, more opportunity exists to regularly evaluate their back and legs, which are the 2 most frequent sites for AMs to occur.
Limitations of the study
This study took place at 2 campuses with a convenience sample of interns and may not be representative of all chiropractic interns or practicing doctors of chiropractic. Although the photographs were good examples of the typical lesions seen in practice in the opinion of the investigators, a broader selection of photographs might enhance the ability of the participants to accurately detect AMs when compared with others because only 3 AMs were used. On the other hand, some responses were likely guesses; and there is no way to know from a preliminary study such as this how many were guesses and how many were accurate detections of the correct response.
Another limitation is the scant evidence of early detection as a means of reducing morbidity and early mortality. It stands to reason that earlier detection of a pathological mole could result in earlier diagnosis of cancer, but lack of randomized trials on the subject creates this limitation.
Conclusion
Skin cancer continues to increase in prevalence. Surveillance should be performed by all health care providers, and the unique role of chiropractors should not be overlooked. They are trained in diagnostic sciences and dermatology, and typically see patients with more frequency in a year than their primary care counterpart. Typically, they see patients with a gown on or, in case of the male patients, often with the shirt removed. There is an excellent opportunity to evaluate the back and legs of patients on a routine basis so that those with AMs can be followed. Education about risk behaviors, teaching self-examination skills, and partnering with the patient's primary care doctor on general surveillance seem like a sensible approach for the profession to consider. Adequate charting and tracking of pathological moles could result in early detection and referral that may reduce morbidity and mortality from skin cancer if a systematic process can be developed.
Further research should test the ability of DCs to identify pathological moles on a broader, evaluative basis. Chiropractic education should emphasize the opportunity to detect and assess AMs as a routine part of primary prevention and should correct deficiencies in the training of chiropractic interns where this is needed. To determine the effectiveness of AM education of interns, it would be interesting to survey the same group of interns who were tested at each institution at least 1 year into clinical practice to determine their practice behaviors relating to AM detection.
Chiropractic inspection of AMs and other lesions on the skin could save lives and have an impact on public health, and this topic deserves further investigation from a research and academic training perspective. Future focus should determine effectiveness of education campaigns to persuade DCs and interns to engage the patient in reducing risk factors associated with skin cancer. Further research is needed in examining the effectiveness of screening AMs in primary care as well as other specialty care or complementary health care providers.
Funding sources and potential conflicts of interest
Each campus internally funded this project. The authors declare no conflicts of interest.
Acknowledgment
The authors thank the research and education faculty at each institution who gave us access to students as well as Maria Dominguez at the Parker Research Institute for her assistance.
References
- 1.American Cancer Society . American Cancer Society skin cancer facts sheet. 2009. http://www.cancer.org/docroot/PED/content/ped_7_1_What_You_Need_To_Know_About_Skin_Cancer.asp Available from. Accessed May 6, 2010. [Google Scholar]
- 2.Young S.E., Giulano A.E., Morton D.L. Three decades of evolving treatment for melanoma: no improvement in survival? J Clin Oncol. 2005;23:7511. [Google Scholar]
- 3.Beddingfield F.C. The melanoma epidemic: res ipsa loquitur. Oncologist. 2003;8:459–465. doi: 10.1634/theoncologist.8-5-459. [DOI] [PubMed] [Google Scholar]
- 4.Jemal A., Clegg L.X., Ward E., Ries L.A., Wu X., Jamison P.M. Annual report to the nation on the status of cancer, 1975-2001, with a special feature regarding survival. Cancer. 2004;101:3–27. doi: 10.1002/cncr.20288. [DOI] [PubMed] [Google Scholar]
- 5.MayoClinic.com Squamous cell carcinoma. www.mayoclinic.com/health/Squamous-cell-carcinoma/DS0094 Available from. Accessed April 5, 2008.
- 6.American Academy of Dermatology Squamous cell carcinoma. www.add.org/public/publications/pamphlets/sun_squamous.html Available from. Accessed April 15, 2008.
- 7.Diepgen T.L., Mahler V. The epidemiology of skin cancer. Br J Dermatol. 2002;146(Suppl 61):1–6. doi: 10.1046/j.1365-2133.146.s61.2.x. [DOI] [PubMed] [Google Scholar]
- 8.Goldsmith L.A., Koh H.K., Bewerse B.A. Full proceedings from the National Conference to Develop a National Skin Cancer Agenda, American Academy of Dermatology and Centers for Disease Control and Prevention, Washington, D.C., April 8-10, 1995. J Am Acad Dermatol. 1996;35(5, pt 1):748–756. doi: 10.1016/s0190-9622(96)90731-8. [DOI] [PubMed] [Google Scholar]
- 9.Geller A.C., Swetter S.M., Brooks K.R., Demierre M.F., Yaroch A. Screening, early detection, and trends for melanoma: current status (2000-2006) and future directions. J Am Acad Dermatol. 2007;57(4):555–576. doi: 10.1016/j.jaad.2007.06.032. [DOI] [PubMed] [Google Scholar]
- 10.American Cancer Society ACS cancer facts and figures. 2008. http://www.cancer.org/Research/CancerFactsFigures/cancer-facts-figures-2008 Available from. Accessed September 10, 2009.
- 11.Manson J.E., Rexrode K.M., Garland F.C., Garland C.F., Weinstock M.A. The case for a comprehensive national campaign to prevent melanoma and associated mortality. Epidemiol. 2000;11(6):728–734. doi: 10.1097/00001648-200011000-00021. [DOI] [PubMed] [Google Scholar]
- 12.Wolfe J.T. The role of screening in the management of skin cancer. Curr Opin Oncol. 1999;11:123–128. doi: 10.1097/00001622-199903000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Losina E., Walensky R.P., Geller A. Visual screening for malignant melanoma: a cost-effective analysis. Arch Dermatol. 2007;143(1):21–28. doi: 10.1001/archderm.143.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glanz K., Schoenfeld E., Weinstock M.A., Layi G., Kidd J., Shigaki D.M. Development and reliability of a brief skin cancer risk assessment tool. Cancer Detect Prev. 2003;27:311–315. doi: 10.1016/s0361-090x(03)00094-1. [DOI] [PubMed] [Google Scholar]
- 15.Epstein D.S., Lange J.R., Gruber S.B. Is physician detection associated with thinner melanomas? JAMA. 1999;281:640–643. doi: 10.1001/jama.281.7.640. [DOI] [PubMed] [Google Scholar]
- 16.Wolf S.H., Jonas S., Kaplan-Liss E. Health promotion and disease prevention in clinical practice. 2nd ed. Wolters Kluwer/Lippincott, Williams & Wilkins; Philadelphia, PA: 2008. [Google Scholar]
- 17.Christensen M.G., Kollasch M.W. Job analysis of chiropractic: a project report, survey analysis and summary of the practice of chiropractic within the United States—2005. National Board of Chiropractic Examiners; Greeley: 2005. [Google Scholar]
- 18.World Health Organization. Solar ultraviolet radiation: global burden of disease from solar ultraviolet radiation. Environmental burden of disease series, N.13. 2006.
- 19.Saraiya M., Glanz K., Briss P.A. Interventions to prevent skin cancer by reducing exposure to ultraviolet radiation: a systematic review. Am J Prev Med. 2004;27(5):422–466. doi: 10.1016/j.amepre.2004.08.009. [DOI] [PubMed] [Google Scholar]


