Abstract
Objective
The purpose of this case report is to describe and discuss the clinical presentation, diagnosis, and management of 3 female long distance runners with high hamstring tendinopathy.
Clinical Features
Three female runners presented to a chiropractic office with proximal hamstring pain that was aggravated by running. Increasing mileage, hills, and/or interval training preceded the onset of symptoms in each case. The subjects all displayed weakness of the hip abductors, pelvic joint dysfunction, hamstring tightness, and ischial tuberosity tenderness. Other clinical findings included overpronation, proprioceptive weakness, and lumbar dysfunction.
Intervention and Outcome
All 3 patients were treated with Graston Instrument Assisted Soft Tissue Mobilization, lumbopelvic manipulation, and electrical muscle stimulation with ultrasound. Active exercise focused on hamstring stretching and strengthening, gluteal strengthening, and proprioceptive training. The 3 runners seen in this clinic had resolution of hamstring pain in an average of 13 treatments and were able to continue competing without restriction.
Conclusion
Runners with high hamstring tendinopathy may respond favorably to conservative chiropractic treatment and active rehabilitation with minimal time off of training.
Key indexing terms: Tenosynovitis, Lower extremity, Thigh, Athletic injuries, Sports medicine, Soft tissue injuries
Introduction
High hamstring tendinopathy is a relatively uncommon injury that is often overlooked as a cause of chronic gluteal pain. This injury is common in long distance runners and presents as persistent deep gluteal pain that is aggravated by running and acceleration.1 In more severe cases, patients may also complain of pain when sitting on hard surfaces.1
The common hamstring tendon originates on the posterior aspect of the ischial tuberosity and is composed of the semimembranosus, semitendonosus, and the long head of the biceps femoris.2 These 3 muscles are innervated by the tibial branch of the sciatic nerve and perform the action of extending the hip and flexing the knee.
Maximum tension is placed on the tendons of the hamstring during the eccentric phase of contraction when the hip is flexed and knee is extended.3,4 Running predisposes to hamstring tendon injury because it allows for long periods of time in eccentric contraction. The hamstrings are most susceptible to injury as they are working to decelerate knee extension during activities such as sprinting and hill training.5
Predisposing factors to general hamstring injury include low hamstring to quad ratio, hamstring inflexibility, inadequate warm-up, and history of previous injury.1,6,7 There is little literature available on the etiology of hamstring tendinopathy, but core weakness and pelvic dysfunction appear to be closely linked.1 The purpose of this case report is to describe and discuss the clinical presentation, diagnosis, and management of 3 female long distance runners with high hamstring tendinopathy. Consent was provided by each patient to publish their health information in this report.
Case report
Case 1
A 36-year-old white competitive female distance runner presented to the chiropractic clinic with complaints of left hip and posterior thigh pain. The patient had been training for a half marathon and experienced increasing gluteal pain over a 3-week period. She described her pain as a localized, sharp pull at the origin of the hamstring that was worse during acceleration and prevented her from taking a full stride. She also described weakness or “giving way” of her left hip. The pain did not prevent running, but she could not run at her desired pace.
A lower extremity and lumbar evaluation was performed. The patient had dropped arches bilaterally and moderate pronation, which was worse on the right. A Trendelenburg sign was positive on the left with weakness +4/5 of the left gluteus medius and gluteus maximus. A straight leg raise test was positive at 80° for localized pain at the origin of the hamstring. Results of Slump, Braggard, and Sicard tests were negative for radicular pain. Active hip flexion was limited because of hamstring tension. Trigger points were found in the gluteus medius and gluteus minimus on the left. Restricted motion of the sacroiliac joint was found and there was palpable tension of the proximal hamstring tendon with reproduction of pain over the ischial tuberosity.
The working diagnosis was high hamstring tendinopathy. The patient was treated with Thompson prone sacroiliac manipulation to correct pelvic and sacral dysfunction. Trigger point compression and cross friction massage were applied to the affected gluteus medius, gluteus minimus, and piriformis. Electrical muscle stimulation at 80 to 120 Hz combined with ultrasound (US) at 1 W/cm2 1.2 MHz was applied for 8 minutes over the ischial tuberosity. Treatments were given 5 times during a 2-week period. The patient applied ice massage for 5 minutes 2 times per day and performed hamstring stretching. The ischial pain was resolved after 5 treatments.
While running a half marathon she developed illiotibial band (ITB) syndrome that may have resulted from unresolved abductor weakness. She was subsequently treated with manipulation, trigger point therapy, electrical muscle stimulation/US, and Graston Instrument Assisted Soft Tissue Mobilization to the hamstring and ITB. Clam exercises, hip extensions, one-leg stance, and ball squats were given as at-home active care along with continued ice massage. The patient was treated twice per week for 3 weeks, then once per week for 3 weeks. She continued to run during the course of treatment and was symptom-free 2 months after initial presentation. The patient began wearing custom orthotics at this time. The patient continues to train for marathons with no recurrence of hamstring or ITB symptoms.
The patient received a total of 14 treatments over a period of 8 weeks. At the end of the treatment period, there was improved strength of hip abduction and hip extension +5/5. At reexamination, no Trendelenburg sign was noted. Straight leg raise was unrestricted and nonpainful. The patient was also able to perform one-leg stance on an unstable surface with the eyes closed.
Case 2
A 40-year-old female triathlete presented to the chiropractic office with complaints of left gluteal pain of 2 weeks' duration. She began running trails during her offseason and stated that pain was aggravated by ascending hills. Pain mostly occurred with running, but she had begun experiencing pain at the ischium when sitting on hard surfaces. Active care included ice and stretching, which would give temporary relief. Pain would resume with activity and would worsen with sitting. The patient had a history of recurrent running injuries including ITB syndrome, plantar fasciitis, and chronic adductor strain. Her injuries were often the result of overtraining. She wore custom orthotics when running.
Result of a straight leg raise test was negative. Braggard and Sicard tests elicited pain at the hamstring insertion. There was no major limitation in hamstring flexibility. A Trendelenburg sign was positive on the right. During one-leg stance, the patient had significant body lean to the right, nondependent of the stationary leg. Proprioceptive testing revealed inability to perform one-leg stance with eyes closed; the right side had significantly less proprioceptive control. The patient had bilateral pronation and dropped arches. Deep gluteal trigger points were found on the left. Joint dysfunctions included a right posterior-inferior ilium and anterior-superior sacrum. Tenderness was present over the hamstring with adhesions in the semimembranosus. A quadratus lumborum trigger point was found on the left along with nonpainful restriction during passive lumbar flexion. Pinpoint tenderness was present over the hamstring insertion with palpable hypertonicity of the proximal hamstring.
The patient was diagnosed with high hamstring tendinopathy and chronic pelvic dysfunction. Chiropractic treatment consisted of prone sacroiliac manipulation and lumbar flexion distraction to restricted segments. Graston Instrument Assisted Soft Tissue Mobilization was used over the distal hamstring. Electrical muscle stimulation (80-120 Hz) with US (100%, 1 MHz, 1.2 W/cm2) for 8 minutes was applied to the proximal hamstring tendon. The patient was treated in the office 2 to 3 times per week for 4 weeks, then once per week 4 weeks. Afterward, the patient was seen every 2 weeks for 1 month. During this time, active care included ice massage and hamstring stretching. Ball squats, one-leg stance, gluteal bridge, forward lunges, and resisted hamstring curls were given for hamstring and gluteal strengthening. Proprioceptive exercise included one-leg stance with eyes open/closed and with contralateral hip extension.
The patient continued to run, swim, and ride a stationary bike, but was strongly advised to discontinue trail running. Her continued running prolonged treatment; but within 11 weeks, she was symptom-free and competed in a half marathon. The patient subsequently developed ITB syndrome that was treated with continued gluteal strengthening and ITB stretching. The patient received a total of 16 treatments over a period of 11 weeks for pain associated with hamstring tendinopathy. Hip extension was improved at the end of treatment, but abductor weakness persisted. She continued to have significant loss of proprioceptive control, but right one-leg stance had improved.
Currently, the patient competes in triathlon and has run several marathons since the initial onset of hamstring tendinopathy. This patient continues to have episodic high hamstring tendinopathy with symptoms of ischial bursitis. Her episodes are almost always associated with interval and hill training. Treatment of subsequent episodes has included the same modalities as mentioned above, and the patient has responded favorably without requiring time off from training.
Case 3
A 37-year-old female competitive marathoner and track coach presented to the office for the treatment of hamstring pain of 5 days duration. She stated that pain began during an 18-mile run. During subsequent runs, she noticed a significant shortening in her side. She had a lot of pain when sitting on a chair and reported feeling as though there was a “bruise on her bottom.” She rated pain as 7/10 to 8/10 at the time of presentation. The patient also complained of posterior left hip pain that began about 9 months prior. She had begun running shortly after the birth of her third child, and hip pain began shortly thereafter. It had not prevented running but caused discomfort, especially during stretching and when doing core exercises. The patient had a history of acute lower hamstring strain 2 years prior that had fully resolved.
Hip extension and abduction were decreased, +4/5 weakness, and elicited pain in the left high hamstring. Hip flexor tension was noted on the left with a positive Thomas test result. Gluteus medius and gluteus minimus trigger points were present on the left with reproduction of posterior hip pain. There was a slight drop in the right hip with one-leg stance on the left. No proprioceptive deficit was identified. Adhesion was found in the distal two thirds of the left biceps femoris. Tenderness over the left proximal hamstring with some mild swelling was noted upon palpation. A posterior-inferior ilium and anterior superior sacrum was found on the right. There was a paraspinal trigger point lateral to L3 on the left. L2-5 segmental flexion and lateral flexion restrictions were noted.
The patient was treated with Graston Instrument Assisted Soft Tissue Mobilization, myofascial release, and trigger point therapy to hamstring and gluteals. Prone sacroiliac and lumbar flexion distraction manipulations were performed. Electrical muscle stimulation with US was administered over the proximal hamstring tendon. The initial phase of active care included hamstring stretching and unresisted hamstring strengthening. Gluteal strengthening including lunges, clam exercise, and wall squats were incorporated after 2 weeks. The patient was treated at a frequency of 2 times per week. The patient's condition initially deteriorated 1 week into treatment after she ran a 10-km race, against advice to decrease running intensity. She was subsequently taken off of running and advised to cross train only for 2 weeks. Within 5 weeks, she had resumed normal training with normal mechanics and was pain-free. The patient received a total of 10 treatments over a period of 5 weeks. At the end of treatment, hip flexion was full and nonpainful. Upon reevaluation, contracture of the psoas had resolved, hip extension and abduction were +5/5, and no hip drop was visualized.
Discussion
High hamstring tendinopathy, although uncommon in the general population, should be considered a possible cause of chronic gluteal pain in middle and long distance runners. Because forceful eccentric contraction is the prime mechanism of injury, careful consideration of the history should be made; and patient should be asked about recent interval workouts and/or hill training.7-9 Pain is often localized to the ischium; but because of its location close to the sciatic nerve, patients may also present with radicular pain.10,11 Clinical diagnosis may be difficult if the patient is complaining of gluteal and posterior thigh pain; therefore, lumbar pathology and piriformis syndrome should be considered and ruled out in the chiropractic examination.11,12 If hamstring tendinopathy is suspected, a focused lower extremity examination may include gait analysis, proprioceptive testing, and evaluation of hamstring flexibility and eccentric strength.8,13 Performing a Trendelenburg test may also be beneficial as weak hip abductors may lead to subsequent lower extremity injuries (Fig 1).3
Fig 1.
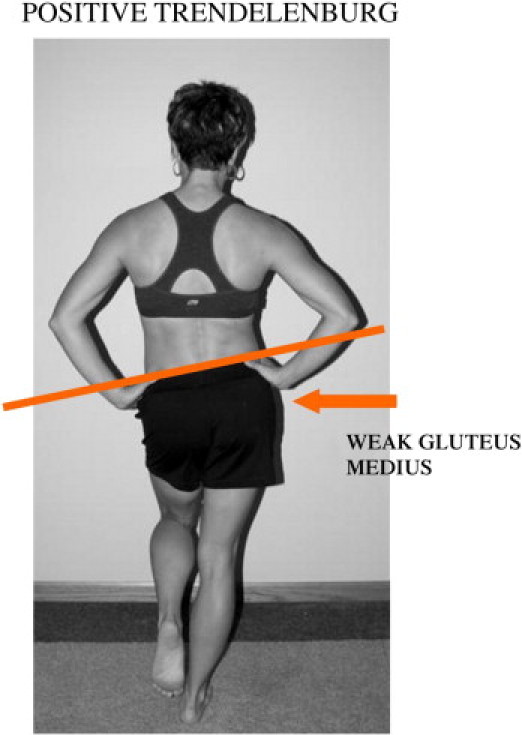
Positive Trendelenburg demonstrating weak gluteus medius on the right.
The diagnosis of hamstring tendinopathy can be confirmed with magnetic resonance imaging, which also allows for visualization of the surrounding structures. On magnetic resonance imaging, the hamstring tendon will appear thickened and there will be signal variation within the tendon.10-12 Fluid accumulation in the tendon will appear as a high-intensity signal on T2-weighted images (Fig 2). Advanced imaging can also help to identify compression of the sciatic nerve or inflammation of the ischial bursa that may also present with pain when sitting on hard surfaces.10,11
Fig 2.
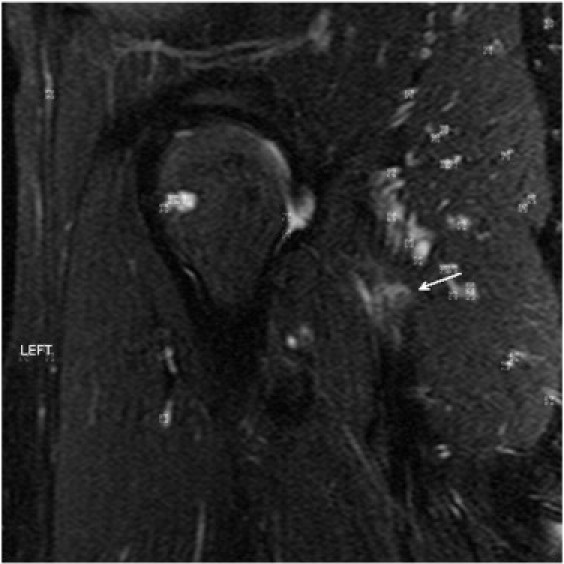
Fat-suppressed T2 image showing fluid within the hamstring tendon.
Because of poor vascularity to the tendon, overload due to prolonged or abnormal stress often results in the lack of inflammatory response. The lack of inflammatory mediators results in disorganization and weakening of the soft tissue matrix.1,11,14 Graston Instrument Assisted Soft Tissue Mobilization (GRASTON) is thought to create a local inflammatory response, augmenting the production of fibroblasts and therefore promoting healing of the injured tissue.15,16 Once an inflammatory response has been initiated, controlled load to the musculotendinous structure, in the form of exercise, can help restore tensile strength.14 Trigger point therapy may also be effective for treating active trigger points distal from the site of tendinopathy.
Hamstring injuries are extremely like to recur without proper rehabilitation; therefore, exercise-based therapy should be considered.1,2,5,7,10,17 The subjects were given exercise instruction in the office but were put on a home exercise program that proved to be beneficial. However, it should be noted that the efficacy of home-based exercise programs is dependent on the motivation of the patient.18-20 Eccentric exercise programs were implemented and have been extremely successful in treating tendinopathy by improving flexibility and strengthening the musculotendinous junction.5-7,9,14,17,21,22 Proprioceptive training was also used to improve neuromuscular control and prevent future injury.1,7,13,14,23,24 Correcting proprioceptive weakness of the lower extremity was accomplished with one-leg stance variations: eyes open/closed progressing to airplane stance (Fig 3), with further progressions to performing lunges and squats on an unstable surface or stability platform.
Fig 3.
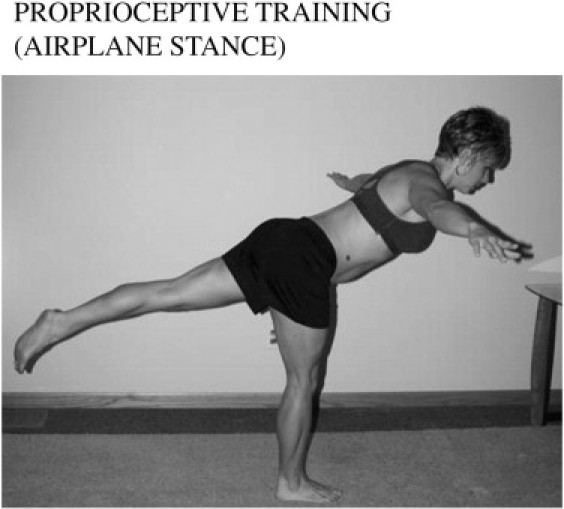
One leg stance with hip extension.
Gluteus medius strengthening exercises were incorporated into the home exercise program and included side-lying hip abductions (clam exercises) (Fig 4), step-ups, and one-leg stance. The gluteus medius acts a dynamic stabilizer of the pelvis, and impairment can lead to kinetic chain dysfunction and injuries of the lower extremity.3,25-28 Two of the athletes developed ITB syndrome subsequent to resolution of hamstring tendon pain that may have been attributed to persistent abductor weakness.
Fig 4.
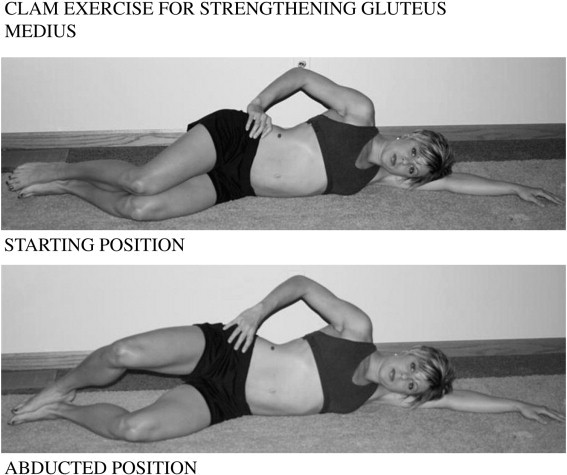
Gluteus medius strengthening exercise.
Combination interferential and US therapy was effective in providing pain relief and assisted in improving hamstring mobility for patients in this clinic. Although there is no research showing that combination therapy is superior to interferential or US therapies alone, it is often used by practitioners when there are indications for both modalities.
It should be advised that patients refrain from running from anywhere between 2 weeks and 3 months.1,5,29 Cardiovascular fitness can be maintained with low-impact activity such as swimming or deep water running.
Limitations
Case studies, in general, are subject to potential for bias of both the clinician and the subjects. In this series, there was only one clinician who was familiar with the educational, socioeconomic, and emotional background of the patients and had treated the athletes for previous injuries. The clinician also used multiple therapeutic modalities, and it is difficult to distinguish which therapies were of the most value.
Magnetic resonance imaging evaluation of the high hamstring tendon would allow visualization of the degree of tendon inflammation and would give image of the ischial bursa that can also produce similar symptoms. It is also noted that high hamstring tendinopathy and ischial bursitis may coexist; but because no advanced imagining was performed, this cannot be confirmed by this study.
The 3 women in this series were all competitive runners and were training at higher volumes than the average population. In all 3 cases, the patients continued to train and compete at levels that could have influenced the rate of improvement. Avoidance of running during the treatment period may have decreased the amount of treatment required to reach maximal therapeutic benefit.
Conclusion
Chiropractic sports management may be an appropriate treatment for athletes with hamstring tendinopathy. Trained chiropractic physicians may be able to identify potential weak links in the lower trunk and prevent future running injuries by evaluating kinetic chain disturbances. Research suggests that conservative management of hamstring tendinopathy is favorable and chiropractic clinicians may provide an effective solution.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study.
References
- 1.Frederickson M., Morre W., Guillet M., Beaulieu C. High hamstring tendinopathy in runners. Physi Sportsmed. 2005;33:32–43. doi: 10.3810/psm.2005.05.89. [DOI] [PubMed] [Google Scholar]
- 2.Kendall F.P., McCreary E.K., Provance P.G. Lower extremity. In: Lappies P., Seitz A., editors. ed. 5. Lippincott Williams & Wilkins; Baltimore: 2005. (Muscles: testing and function in posture and pain). [Google Scholar]
- 3.Fredericson M., Cookingham C.L., Chaudhari A.M., Dowdell B.C., Oestreicher N., Sahrmann S.A. Hip abductor weakness in distance runners with illiotibial band syndrome. Clin J sport Med. 2000;10(3):169–175. doi: 10.1097/00042752-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Croisier J.L., Forthomme B., Namurois M.H. Hamstring muscle strain disorders and strength performance disorders. Am J Sports Med. 2002;30:199–203. doi: 10.1177/03635465020300020901. [DOI] [PubMed] [Google Scholar]
- 5.Petersen J., Holmich P. Evidence based prevention of hamstring injuries in sport. Br J Sports Med. 2005;39:319–323. doi: 10.1136/bjsm.2005.018549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hartig D. Increasing hamstring flexibility decreases lower extremity overuse injuries in military basic trainees. Am J Sports Med. 1999;27(2):173–176. doi: 10.1177/03635465990270021001. [DOI] [PubMed] [Google Scholar]
- 7.Clark R.A. Hamstring injuries: risk assessment and injury prevention. Ann Acad Med Singapore. 2008;37(4):341–346. [PubMed] [Google Scholar]
- 8.Rees J., Maffulli N., Cook J. Management of tendinopathy. Am J Sports Med. 2009;37:1855–1863. doi: 10.1177/0363546508324283. [DOI] [PubMed] [Google Scholar]
- 9.Mjølsnes R., Amason A., Osthagen T., Raastad T., Bahr R.A. 10 week randomized trial comparing eccentric versus concentric hamstring training in well trained soccer players. Scand J Med Sci Sports. 2004;14:311–317. doi: 10.1046/j.1600-0838.2003.367.x. [DOI] [PubMed] [Google Scholar]
- 10.Cacchio A., Rompe J., Furia J., Susi P., Santilli V., Paultis F. Shockwave therapy for the treatment of chronic proximal hamstring tendinopathy in professional athletes. Am J Sports Med. 2010;38:1–8. doi: 10.1177/0363546510379324. [DOI] [PubMed] [Google Scholar]
- 11.Lempaninen L., Sarimo J., Mattila J., Vaittinen S., Orava S. Proximal hamstring tendinopathy: results of surgical management and histopathologic findings. Am J Sports Med. 2009;37:727–734. doi: 10.1177/0363546508330129. [DOI] [PubMed] [Google Scholar]
- 12.Brandser E., El-Khoury G., Kathol M., Callaghan J., Tearse D. Hamstring injuries: radiographic, conventional tomographic, CT, and MR imaging characteristics. Semin Musculoskel Radiol. 1995;197:257–262. doi: 10.1148/radiology.197.1.7568833. [DOI] [PubMed] [Google Scholar]
- 13.Willardson J.M. The effectiveness of resistance exercises performed on unstable equipment. Strength Cond J. 2004;26:70–74. [Google Scholar]
- 14.Emery C.A., Cassidy J.D., Klassen T.P., Rosychuck R.J., Rowe B.H. Effectiveness of a home-based training program in reduce sports-related adolescents: a cluster randomized controlled trail. Can Med Assoc J. 2005;172:749–754. doi: 10.1503/cmaj.1040805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoskins W., Polland H. A descriptive study of manual therapy intervention within a randomized controlled trial for hamstring and lower limb prevention. Chiropr Osteopath. 2010;18:23. doi: 10.1186/1746-1340-18-23. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 16.Hammer W.I. The effect of mechanical load on degenerated soft tissue. Bodyw Mov Ther. 2008;3:246–256. doi: 10.1016/j.jbmt.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 17.Jonhagen S., Nemeth E., Eriksson E. Hamstring injuries in sprinters. The role of concentric and eccentric hamstring muscle strength and flexibility. Am J Sports Med. 1994;22:262–266. doi: 10.1177/036354659402200218. [DOI] [PubMed] [Google Scholar]
- 18.Grant J., Mohatidi N., Maitland M., Zernicke R. Comparison of home versus physical therapy-supervised rehabilitation programs after anterior cruciate ligament reconstruction: a randomized clinical trial. Am J Sports Med. 2005;33:1287. doi: 10.1177/0363546504273051. [DOI] [PubMed] [Google Scholar]
- 19.Duda J., Smart A., Tappe M. Predictors of adherence in the rehabilitation of athletic injuries: an application of personal investment theory. J Sport Exerc Psychol. 1989;11:367–381. [Google Scholar]
- 20.Taylor A., May S. Threat and coping appraisal as determinants of compliance with sports injury rehabilitation: an application of protection motivation theory. J Sports Sci. 1996;14:471–482. doi: 10.1080/02640419608727734. [DOI] [PubMed] [Google Scholar]
- 21.Kujala U.M., Orava S., Jarvinsen M. Hamstring injuries—current trends in treatment and prevention. Sports Med. 1997;23:397–404. doi: 10.2165/00007256-199723060-00005. [DOI] [PubMed] [Google Scholar]
- 22.Malliaropoulos N., Papacostas E., Kiritsi O. Posterior thigh muscle injuries in elite track and field athletes. Am J Sports Med. 2010;38:1813–1820. doi: 10.1177/0363546510366423. [DOI] [PubMed] [Google Scholar]
- 23.Biewener A., Daley M. Unsteady locomotion: integrating muscle function with whole body dynamics and neuromuscular control. J Exp Biol. 2007;210:2949–2960. doi: 10.1242/jeb.005801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Riskowski J., Mikesky R., Bahamonde R., Alvey T., Burr D. Proprioception, gait kinematics, and rate of loading during walking: are they related? J Musculoskelet Neuronal Interact. 2005;5:379–387. [PubMed] [Google Scholar]
- 25.Dwyer M., Boudreau S., Mattacola C., Uhl T., Lattermann C. Comparison of lower extremity kinematics and hip muscle activation during rehabilitation tasks between sexes. J Athl Train. 2010;45:181–190. doi: 10.4085/1062-6050-45.2.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zeller B., McCory J., Kibler W., Uhl T. Differences in kinematics and electromyographic activity between men and women during the single-legged squat. Am J Sports Med. 2003;31:449–456. doi: 10.1177/03635465030310032101. [DOI] [PubMed] [Google Scholar]
- 27.Ireland M., Willson J., Ballantyne B., Davis M. Hip strength in females with and without patellofemoral pain. J Orthop sports Phys Ther. 2003;33:671–676. doi: 10.2519/jospt.2003.33.11.671. [DOI] [PubMed] [Google Scholar]
- 28.Earl J. Gluteus medius activity during 3 variation of isometric single leg stance. J sport Rehabil. 2002;11:179–188. [Google Scholar]
- 29.Browning M.D., Kara H. Hip and pelvis injuries in runners. Phys Sportsmed. 2001;29:23–34. doi: 10.3810/psm.2001.01.303. [DOI] [PubMed] [Google Scholar]


