Abstract
Background:
Injury to the ipsilateral graft used for reconstruction of the anterior cruciate ligament (ACL) or a new injury to the contralateral ACL is a devastating outcome following successful ACL reconstruction, rehabilitation, and return to sport. Little evidence exists regarding the intermediate to long-term risk of these events.
Methods:
The present study is a systematic review of Level-I and II prospective studies that evaluated the rate of rupture of the ACL graft and the ACL in the contralateral knee following a primary ACL reconstruction with use of a mini-open or arthroscopic bone-tendon-bone or hamstring autograft after a minimum duration of follow-up of five years.
Results:
Six studies met the inclusion and exclusion criteria. The ipsilateral ACL graft rupture rate ranged from 1.8% to 10.4%, with a pooled percentage of 5.8%. The contralateral injury rate ranged from 8.2% to 16.0%, with a pooled percentage of 11.8%.
Conclusions:
This systematic review demonstrates that the risk of ACL tear in the contralateral knee (11.8%) is double the risk of ACL graft rupture in the ipsilateral knee (5.8%). Additional studies must be performed to determine predictors for these injuries and to improve our ability to avoid this devastating outcome.
Level of Evidence:
Prognostic Level II. See Instructions to Authors for a complete description of levels of evidence.
Patients undergoing anterior cruciate ligament (ACL) reconstruction typically have good short-term results. Following postoperative rehabilitation and return to activity, one of the most devastating outcomes for the patient who has had an ACL reconstruction is a tear of the ACL graft in the ipsilateral knee or a tear of the ACL in the contralateral knee. This issue has been most extensively studied in terms of the graft in the ipsilateral knee. Multiple studies have demonstrated a rate of graft rerupture in the range of 2% to 6% after less than five years of follow-up1,2. The rate of ipsilateral ACL rerupture and contralateral ACL rupture is similar after short-term follow-up, with a risk of approximately 3%3,4.
Increased knowledge regarding the risk of additional ACL injuries after longer-term follow-up would assist in counseling patients with regard to the expected outcome of ACL reconstruction. This patient group is typically young, with expectations of resuming and maintaining their activities. While two-year results are important, patients really want to know how long the knee can maintain the activity level that they desire. Thus, results after five years or more are pertinent. The primary aim of the present systematic review was to compare the overall ipsilateral ACL rerupture rate with the contralateral ACL rupture rate on the basis of published prospective studies with a minimum duration of follow-up of five years. Our hypotheses are that the contralateral knee remains at equal or higher risk with longer-term follow-up and that both knees have increased failure rates in longer-term as compared with shorter-term studies.
Materials and Methods
Literature Review
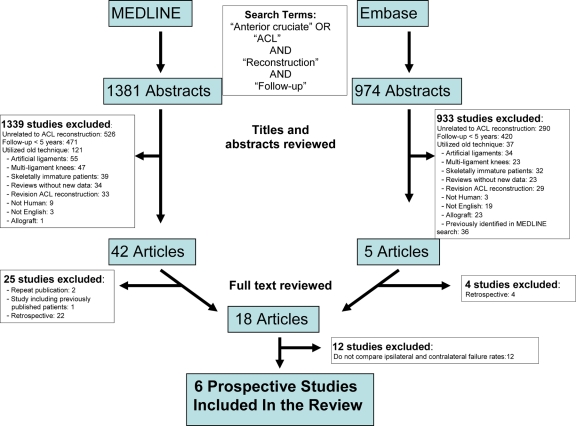
A MEDLINE literature search was performed to identify all studies published from January 1, 1966, through May 1, 2009, in which the long-term outcomes of ACL reconstruction were evaluated. A search for articles containing the terms “reconstruction,” “follow-up,” and either “anterior cruciate” or “ACL” yielded 1381 results. The title, abstract, and full text were reviewed when the title or abstract suggested appropriateness of these publications. Studies that failed to meet the inclusion and exclusion criteria (see Appendix) were excluded. Both retrospective and prospective series were initially reviewed. The full-text versions of the resulting forty-two articles were obtained. Subsequent review led to the exclusion of twenty-two studies that were retrospective in nature, two that were repeat publications, and one that included patients who were represented at longer follow-up in another included study. The literature search is summarized in Figure 1.
Fig. 1.
Flow diagram depicting the literature search.
A search of the Embase database was then performed with use of the same search strategy. The title and abstracts of the resulting 974 studies were reviewed, and 933 papers were excluded in the same manner as in the MEDLINE search. Thirty-six of the remaining forty-one articles had previously been identified in the MEDLINE search. The full text of the remaining five articles was obtained, and four of those studies were excluded because they were retrospective. A Cochrane search did not demonstrate previous reviews of this topic.
The bibliographies of the remaining eighteen studies5-22 were reviewed, and no additional manuscripts meeting the criteria were identified. Twelve papers were excluded as they did not mention ipsilateral and contralateral failure rates. The remaining six papers constituted the data used in the following analysis5,6,10,16,18,19. All papers included prospective (Level-I or II) data and had a minimum duration of follow-up of five years. The study by Drogset and Grøntvedt6 included two groups: one with and one without a ligament-augmentation device. For the purpose of the present study, both groups were used to determine the contralateral rupture rate. Only the group without a ligament-augmentation device was utilized to determine the ipsilateral rerupture rate.
Data Extraction
A templated evidence-based medicine literature-review form was utilized to assist in data collection. Extracted data included demographic characteristics (age, sex, and body-mass index), graft choice, surgical technique, rehabilitation details, duration of follow-up, and ACL graft and contralateral ACL failure rates. Data were extracted by two authors (R.A.M., W.R.D.) independently, and discrepancies were resolved by consensus23,24.
Statistics
Heterogeneity was assessed qualitatively by comparing the populations and designs of individual studies as well as quantitatively with use of a chi-square test. In order to account for between-study variation (heterogeneity), a random-effects model was developed in Review Manager version 5 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark), which uses the method of DerSimonian and Laird to calculate an overall pooled estimate of effect. This method uses an inverse-variance approach to adjust the study weights according to the extent of heterogeneity present among the varying effects reported in the individual studies25.
Source of Funding
One or more authors received salary support from the following sources: the Kenneth D. Schermerhorn Endowment, the Vanderbilt Sports Medicine Research Fund, an NIH grant (#5 K23 AR052392-04), and an AOSSM-MTF Career Development Award Supplement.
Results
The six studies that were identified during the literature review included one randomized controlled trial18 and two prospective cohort studies10,16 comparing the outcomes of ACL reconstruction with bone-patellar tendon-bone autografts with those of reconstruction with hamstring tendon autografts, one randomized controlled trial comparing the outcomes of ACL reconstruction with and without the use of a ligament-augmentation device6, and two prospective reports describing the outcomes of ACL reconstruction at a minimum of five years postoperatively5,19. The study involving the augmentation device only included the group without the device for determination of the ipsilateral failure rates.
Demographic Characteristics
The mean age at the time of reconstruction for the 2026 included patients was 23.4 years, with the mean age in the six studies ranging from twenty-three to twenty-seven years. Overall, 67% of the patients were male, with the percentage in the six studies ranging from 45% to 72%. The time from injury to ACL reconstruction varied considerably between the studies. In all studies, ACL reconstruction was performed with use of autograft and all-arthroscopic, arthroscopic-assisted, or two-incision mini-arthrotomy techniques. The exclusion criteria varied among the studies, but all studies excluded knees with multiple ligamentous injuries other than low-grade medial collateral ligament injuries. Demographic information is detailed in Table I.
TABLE I.
Data on the Studies
| Author | Journal* | Year | Initial Cohort (no. of patients) | Age†(yr) | Percentage Male | Chronicity | Method of Reconstruction‡ | Graft‡ | Other Exclusion Criteria |
| Deehan et al.5 | JBJS-Br | 2000 | 90 | 25 (13 to 42) | 53% | 74% reconstructed within 3 months after injury | All-arthroscopic, femoral tunnel drilled through medial portal | BTB autograft | Multiligamentous injuries, chondral or meniscal pathology, Workers’ Compensation, abnormal radiographs at reconstruction |
| Drogset and Grøntvedt6 | AJSM | 2002 | 100 | 26 (16 to 48) | 45% | Mean time from injury to reconstruction, 3.5 yrs | Arthroscopic-assisted, 2-incision | BTB autograft | Multiligamentous injuries |
| Keays et al.10 | AJSM | 2007 | 62 | 27 (18 to 38) | 71% | Mean time from injury to reconstruction, 3 yrs | All-arthroscopic for hamstring, mini-arthrotomy for BTB. Femoral tunnel drilled through tibia | BTB or hamstring autograft | Multiligamentous injuries, age >40 yrs, acute injuries, evidence of osteoarthritis at reconstruction |
| Roe et al.16 | AJSM | 2005 | 180 | 24 (13 to 52) | 53% | 62% reconstructed within 12 weeks after injury | All-arthroscopic with femoral tunnel drilled through anteromedial portal | BTB or hamstring autograft | Multiligamentous injuries, chondral injuries, meniscal pathology involving >2/3 of meniscus, contralateral knee injury, abnormal radiographs |
| Sajovic et al.18 | AJSM | 2006 | 64 | 25 (14 to 46) | 50% | Mean time from injury to reconstruction, 2.0 yrs | All-arthroscopic | BTB or hamstring autograft | Multiligamentous injuries, abnormal radiographs, previous meniscal surgery, subsequent contralateral rupture |
| Shelbourne and Gray19 | AJSM | 2009 | 1545 | 23 (11 to 53) | 72% | Mean time from injury to reconstruction, 1.5 yrs | 2-incision mini-arthrotomy | BTB autograft | Bilateral injuries, subsequent contralateral ruptures, revision procedures |
JBJS-Br = The Journal of Bone and Joint Surgery (British Volume), and AJSM = The American Journal of Sports Medicine.
The values are given as the mean, with the range in parentheses.
BTB = bone-tendon-bone.
Rehabilitation
All reports included details on the rehabilitation protocol. Immediate full weight-bearing was allowed in all studies. Postoperative extension bracing was utilized in two studies for time periods ranging from one to three weeks. A table in the Appendix details the protocols for each study.
Follow-up
All studies had a minimum of five years of follow-up after ACL reconstruction. The mean duration of follow-up ranged from five to fourteen years.
Ipsilateral Rerupture Versus Contralateral Rupture
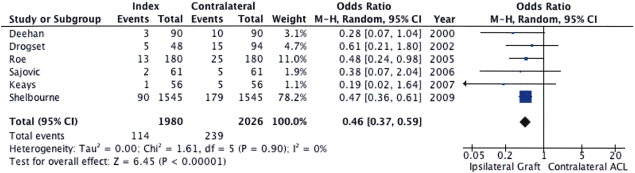
The ipsilateral ACL graft rupture rate ranged from 1.8% to 10.4%, with a pooled percentage of 5.8%. The contralateral ACL injury rate ranged from 8.2% to 16.0%, with a pooled percentage of 11.8%. An annualized rate of injury was 0.73 for ipsilateral tears and 1.69 for contralateral tears (Table II). A sensitivity analysis was performed to determine if the large sample size of the study by Shelbourne and Gray19 was overly influential, and the pooled estimates were similar with and without this study included in the model. The results of the individual studies are listed in Figure 2, along with a forest plot that graphically displays the point estimates on a common scale surrounded by the 95% confidence interval.
TABLE II.
Ipsilateral Graft Versus Contralateral ACL Tears
| Author | Year | Initial Cohort (no. of patients) | No. of Patients Included in Follow-up | Duration of Clinical Follow-up*(yr) | No. of Ipsilateral Ruptures | Ipsilateral Annualized Rate | No. of Contralateral Ruptures | Contralateral Annualized Rate |
| Deehan et al.5 | 2000 | 90 | 90 (100%) | 5 | 3/90 (3.3%) | 0.66 | 10/90 (11.1%) | 2.22 |
| Drogset and Grøntvedt6† | 2002 | 100 | 94 (94%) | 8 | 5/48 (10.4%) | 1.3 | 15/94 (16.0%) | 2 |
| Keays et al.10 | 2007 | 62 | 56 (90%) | 6 | 1/56 (1.8%) | 0.3 | 5/56 (8.9%) | 1.48 |
| Roe et al.16 | 2005 | 180 | 180 (100%) | 7 | 13/180 (7.2%) | 1.03 | 25/180 (13.9%) | 1.97 |
| Sajovic et al.18 | 2006 | 64 | 61 (95%) | 5 | 2/61 (3.3%) | 0.66 | 5/61 (8.2%) | 1.64 |
| Shelbourne and Gray19 | 2009 | 1545 | 1545 (100%) | 14 (10 to 24) | 90/1545 (5.8%) | 0.41 | 179/1545 (11.6%) | 0.83 |
| All | 2041 | 2026 (99%) | 114/1980 (5.8%) | 0.73 | 239/2026 (11.8%) | 1.69 |
The values are given as the mean, with or without the range in parentheses.
Study included patients with and without a ligament-augmentation device. All ninety-four patients were considered when determining contralateral rupture rate. Only the forty-eight patients without a ligament-augmentation device were considered when calculating the ipsilateral rerupture rate.
Fig. 2.
Results of individual studies along with a Forest plot that graphically displays the point estimates on a common scale surrounded by the 95% confidence interval (indicated by the horizontal lines). M-H = Mantel-Haenszel, CI = confidence interval, df = degrees of freedom.
Discussion
An ACL graft rupture or a new ACL rupture on the contralateral side remain among the most devastating complications following primary ACL reconstruction. Patients are greatly dismayed to face repeat surgery and the long process of rehabilitation after having previously successfully completed this process. Educating patients with regard to the risk of these complications is important following the treatment of an ACL injury.
We hypothesized that the rate of ACL graft rupture is greater than historical rates that have been reported after shorter follow-up and that the contralateral ACL is also at equal or greater risk after a minimum of five years of follow-up. Our hypothesis was supported by this systematic review of Level-I and II studies with a minimum duration of follow-up of five years. In our review of the literature, we identified only six Level-I and II studies that evaluated ipsilateral and contralateral injury rates after a minimum of five years of follow-up, but the findings of the six studies were consistent. The contralateral knee is at greater risk than the ipsilateral knee is with continued follow-up. Our findings demonstrated that, after a minimum of five years of follow-up, the risk of an ACL tear in the contralateral knee (11.8%) is approximately twice as high as the risk of an ACL graft rupture in the ipsilateral knee (5.8%).
A study of this type has a variety of strengths and limitations. One limitation was the difficulty of ensuring that all ipsilateral and contralateral injuries were identified. If some injuries were missed, this would only increase the already worrisome rates of injury for these knees at a minimum of five years postoperatively. Another limitation exists because of the lack of data regarding age, sex, and activity level at the time of reinjury. Future studies involving a validated activity level (i.e., the Marx activity score26) will be able to provide this information to advise patients and clinicians. The strengths of the present study include the high level of evidence and the novelty of the data collected. This information will make counseling patients on the true long-term risk of reinjury more appropriate.
Previous studies have identified a risk for ACL graft rupture in the 2% to 5% range at two years of follow-up1-4,27. The contralateral ACL tear rate has rarely been described, but, at shorter (two-year) follow-up, it has been identified as remaining closer to the ipsilateral ACL graft rupture rate3. Pinczewski et al. described a contralateral ACL tear rate of 12% (similar to the rate in our study) at five years of follow-up28 in a group of patients whom he had initially followed for two years after primary ACL reconstruction4.
The etiology of the increased risk for the contralateral knee as compared with the initially-injured knee following primary ACL reconstruction is unknown. Risk factors for bilateral ACL tear have been hypothesized to include notch width, sex, knee alignment, and/or genetic predisposition29-31. None of these factors explain the increased risk for the contralateral knee. Clinicians hypothesize, without evidence, that the contralateral knee may represent some form of protection for the ipsilateral reconstructed knee. While this may be true, it does not explain why the ipsilateral knee and the contralateral knee have equal injury rates at the time of the two-year follow-up whereas the contralateral knee has double the risk at more than five years of follow-up. This increased risk for the contralateral knee could result from a lack of rehabilitation of the contralateral knee that was deconditioned during the recovery from the ipsilateral knee surgery. The increased contralateral risk may be multifactorial, and it is difficult to determine predictors that could be modified to prevent these injuries. Long-term prospective longitudinal studies will need to be performed to identify predictors for these contralateral injuries. An analysis of this type is not possible in a systematic review such as ours. The overarching goal is to be able to identify strategies that will decrease the risk of injury in both knees. This may include activity modification, rehabilitation protocol modification, return to sports training modification that emphasizes training the contralateral knee, or other yet unidentified approaches.
This systematic review of Level-I and II studies with a minimum of five years of follow-up that identify ipsilateral and contralateral injury rates after primary ipsilateral ACL reconstruction demonstrates a contralateral ACL tear rate that is double (11.8%) that of the risk of ACL graft rupture in the ipsilateral knee (5.8%). This risk increases with time compared with two-year follow-up studies. Additional studies with a high level of evidence must be performed to determine predictors (age, sex, activity level, type of sport) for these injuries and improve our ability to avoid this devastating outcome.
Appendix
Supporting Data
Footnotes
Disclosure: In support of their research for or preparation of this work, one or more of the authors received, in any one year, outside funding or grants in excess of $10,000 from the Kenneth D. Schermerhorn Endowment, the Vanderbilt Sports Medicine Research Fund, an NIH grant (#5 K23 AR052392-04), and an AOSSM-MTF Career Development Award Supplement. Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity.
References
- 1.Freedman KB, D'Amato MJ, Nedeff DD, Kaz A, Bach BR., Jr Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31:2-11 [DOI] [PubMed] [Google Scholar]
- 2.Yunes M, Richmond JC, Engels EA, Pinczewski LA. Patellar versus hamstring tendons in anterior cruciate ligament reconstruction: A meta-analysis. Arthroscopy. 2001;17:248-57 [DOI] [PubMed] [Google Scholar]
- 3.Wright RW, Dunn WR, Amendola A, Andrish JT, Bergfeld J, Kaeding CC, Marx RG, McCarty EC, Parker RD, Wolcott M, Wolf BR, Spindler KP. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35:1131-4 [DOI] [PubMed] [Google Scholar]
- 4.Corry IS, Webb JM, Clingeleffer AJ, Pinczewski LA. Arthroscopic reconstruction of the anterior cruciate ligament. A comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med. 1999;27:444-54 [DOI] [PubMed] [Google Scholar]
- 5.Deehan DJ, Salmon LJ, Webb VJ, Davies A, Pinczewski LA. Endoscopic reconstruction of the anterior cruciate ligament with an ipsilateral patellar tendon autograft. A prospective longitudinal five-year study. J Bone Joint Surg Br. 2000;82:984-91 [DOI] [PubMed] [Google Scholar]
- 6.Drogset JO, Grøntvedt T. Anterior cruciate ligament reconstruction with and without a ligament augmentation device: results at 8-Year follow-up. Am J Sports Med. 2002;30:851-6 [DOI] [PubMed] [Google Scholar]
- 7.Hanypsiak BT, Spindler KP, Rothrock CR, Calabrese GJ, Richmond B, Herrenbruck TM, Parker RD. Twelve-year follow-up on anterior cruciate ligament reconstruction: long-term outcomes of prospectively studied osseous and articular injuries. Am J Sports Med. 2008;36:671-7 [DOI] [PubMed] [Google Scholar]
- 8.Hart AJ, Buscombe J, Malone A, Dowd GS. Assessment of osteoarthritis after reconstruction of the anterior cruciate ligament: a study using single-photon emission computed tomography at ten years. J Bone Joint Surg Br. 2005;87:1483-7 [DOI] [PubMed] [Google Scholar]
- 9.Ibrahim SA, Al-Kussary IM, Al-Misfer AR, Al-Mutairi HQ, Ghafar SA, El Noor TA. Clinical evaluation of arthroscopically assisted anterior cruciate ligament reconstruction: patellar tendon versus gracilis and semitendinosus autograft. Arthroscopy. 2005;21:412-7 [DOI] [PubMed] [Google Scholar]
- 10.Keays SL, Bullock-Saxton JE, Keays AC, Newcombe PA, Bullock MI. A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and Gracilis tendon graft. Am J Sports Med. 2007;35:729-39 [DOI] [PubMed] [Google Scholar]
- 11.Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C. Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med. 2008;36:1275-82 [DOI] [PubMed] [Google Scholar]
- 12.Lidén M, Ejerhed L, Sernert N, Laxdal G, Kartus J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-Year follow-up. Am J Sports Med. 2007;35:740-8 [DOI] [PubMed] [Google Scholar]
- 13.Matsumoto A, Yoshiya S, Muratsu H, Yagi M, Iwasaki Y, Kurosaka M, Kuroda R. A comparison of bone-patellar tendon-bone and bone-hamstring tendon-bone autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34:213-9 [DOI] [PubMed] [Google Scholar]
- 14.O'Neill DB. Arthroscopically assisted reconstruction of the anterior cruciate ligament. A follow-up report. J Bone Joint Surg Am. 2001;83:1329-32 [DOI] [PubMed] [Google Scholar]
- 15.Panni AS, Milano G, Tartarone M, Demontis A, Fabbriciani C. Clinical and radiographic results of ACL reconstruction: a 5- to 7-year follow-up study of outside-in versus inside-out reconstruction techniques. Knee Surg Sports Traumatol Arthrosc. 2001;9:77-85 [DOI] [PubMed] [Google Scholar]
- 16.Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M. A. 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med. 2005;33:1337-45 [DOI] [PubMed] [Google Scholar]
- 17.Ruiz AL, Kelly M, Nutton RW. Arthroscopic ACL reconstruction: a 5-9 year follow-up. Knee. 2002;9:197-200 [DOI] [PubMed] [Google Scholar]
- 18.Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K. A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med. 2006;34:1933-40 [DOI] [PubMed] [Google Scholar]
- 19.Shelbourne KD, Gray T. Minimum 10-year results after anterior cruciate ligament reconstruction: how the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am J Sports Med. 2009;37:471-80 [DOI] [PubMed] [Google Scholar]
- 20.Spindler KP, Warren TA, Callison JC, Jr., Secic M, Fleisch SB, Wright RW. Clinical outcome at a minimum of five years after reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 2005;87:1673-9 [DOI] [PubMed] [Google Scholar]
- 21.Wu WH, Hackett T, Richmond JC. Effects of meniscal and articular surface status on knee stability, function, and symptoms after anterior cruciate ligament reconstruction: a long-term prospective study. Am J Sports Med. 2002;30:845-50 [DOI] [PubMed] [Google Scholar]
- 22.Zaffagnini S, Marcacci M, Lo Presti M, Giordano G, Iacono F, Neri MP. Prospective and randomized evaluation of ACL reconstruction with three techniques: a clinical and radiographic evaluation at 5 years follow-up. Knee Surg Sports Traumatol Arthrosc. 2006;14:1060-9 [DOI] [PubMed] [Google Scholar]
- 23.Greenhalgh T. How to read a paper: The basics of evidence based medicine. 2nd ed. London: BMJ Publishing Group; 2001 [Google Scholar]
- 24.Spindler KP, Kuhn JE, Dunn W, Matthews CE, Harrell FE, Dittus RS. Reading and reviewing the orthopaedic literature: a systematic, evidence-based medicine approach. J Am Acad Orthop Surg. 2005;13:220-9 [DOI] [PubMed] [Google Scholar]
- 25.Higgins JPT, Green S, Cochrane handbook for systematic reviews of interventions. West Sussex: John Wiley & Sons Ltd.; 2008 [Google Scholar]
- 26.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29:213-8 [DOI] [PubMed] [Google Scholar]
- 27.Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE., Jr Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32:1986-95 [DOI] [PubMed] [Google Scholar]
- 28.Pinczewski LA, Deehan DJ, Salmon LJ, Russell VJ, Clingeleffer A. A five-year comparison of patellar tendon versus four-strand hamstring tendon autograft for arthroscopic reconstruction of the anterior cruciate ligament. Am J Sports Med. 2002;30:523-36 [DOI] [PubMed] [Google Scholar]
- 29.Harner CD, Paulos LE, Greenwald AE, Rosenberg TD, Cooley VC. Detailed analysis of patients with bilateral anterior cruciate ligament injuries. Am J Sports Med. 1994;22:37-43 [DOI] [PubMed] [Google Scholar]
- 30.Motohashi M. Profile of bilateral anterior cruciate ligament injuries: a retrospective follow-up study. J Orthop Surg (Hong Kong). 2004;12:210-5 [DOI] [PubMed] [Google Scholar]
- 31.Souryal TO, Moore HA, Evans JP. Bilaterality in anterior cruciate ligament injuries: associated intercondylar notch stenosis. Am J Sports Med. 1988;16:449-54 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.