Abstract
Interim methadone (with emergency counseling only) (IM), is an effective, but highly restricted alternative to Methadone Treatment Program (MTP) waiting lists. However, it is not known whether IM disadvantages patients as compared to standard methadone treatment (SM). In this clinical trial, conducted in two MTPs, 230 newly-admitted patients were randomly assigned to: IM, SM and “Restored” Methadone treatment (SM with a counselor with a reduced case load) (RM). Data were analyzed using generalized estimating equations and generalized linear modeling. There were no significant differences among Conditions in: days in treatment or of heroin or cocaine use and heroin or cocaine positive urine drug tests. The IM as compared to the SM group had significantly fewer self-reported days of criminal activity and lower amounts of money spent on drugs and illegal income. These findings suggest that when SM is unavailable, IM should be more widely used and less restricted. These findings suggest that when SM is unavailable IM should be more widely utilized and less restricted.
Keywords: Interim methadone, methadone treatment, waiting lists, opioid dependence, counseling
1. Introduction
From its very beginning in the United States, methadone maintenance treatment (MMT) of heroin addiction has been coupled with the provision of psychosocial services. At the time, this perspective about the necessity of psychosocial services was accepted as self-evident although it had not been subjected to a controlled clinical trial. By 1972, revised FDA regulations mandated that psychosocial services be provided as a condition of offering MMT. These regulations were modified several times over the following decades but the basic structure of the treatment system was left intact, including the requirement that approved methadone treatment programs (MTPs) provide psychosocial services in addition to methadone (Institute of Medicine, 1995). In 1989, in the context of the HIV epidemic and the recognition that patients participating in MTPs were less likely to inject, share injection equipment, and become infected with HIV, the FDA and NIDA proposed an additional option. Approved programs would be able to temporarily provide methadone without psychosocial services (interim methadone), rather than assigning patients to waiting lists when resources limited the availability of standard methadone treatment (methadone combined with psychosocial services and termed comprehensive methadone treatment in regulations). The response of treatment providers to this proposed regulatory shift was so uniformly negative that the involved Federal agencies planned to formally rescind the proposed regulatory change. One of the objections to the proposed regulatory change was based on providers’ belief that it would lead to a reduction or elimination of funding for psychosocial services. Nevertheless, subsequently an amendment to 1992 legislation reorganizing the Alcohol, Drug Abuse and Mental Health Administration gave Interim Methadone (IM) a statutory basis (Institute of Medicine, 1995).
The IM regulations that were finally approved were exceedingly restrictive: IM could be provided only by not-for-profit programs, and each program had to be specifically approved by the Centers for Substance Abuse Treatment (CSAT) and only after CSAT approved an application from the highest health official in the State affirming that the demand for standard methadone treatment (SM) exceeded the State’s capacity. Admission to IM required a complete medical exam comparable to that for SM, periodic drug testing, and emergency counseling. Once admitted to IM, patients were required to take all methadone doses under direct observation making it necessary for approved programs to remain open seven days a week including holidays. Patients could participate in IM for no more than 120 days, and thus, programs were required to discharge patients at that point or admit them to SM treatment.
Several studies are particularly relevant to an understanding of the context for these restrictive regulations. In the late 1980s, a number of multi-clinic cross-sectional studies found that MTPs that provided more psychosocial services had better retention in treatment and lower levels of illicit drug use (Ball & Ross, 1991; Hubbard et al., 1984). Working under an Investigational New Drug (IND), Yancovitz and colleagues compared patients provided with methadone alone (naming it Interim Methadone) for 30 days to treatment applicants who were randomly assigned to a waiting list (Yancovitz et al., 1991). They reported that at the end of the 30 day follow-up, those provided with only methadone substantially reduced their heroin use compared to the waiting list controls, and were more likely to be enrolled in SM at 16 month follow-up. However, McLellan et al. (1993) randomly assigned 102 male veterans to three groups: “minimal services” methadone treatment (the lowest level of supervised care possible under the FDA regulations then in force), SM, and MMT with enhanced services (including on-site psychiatric care, family therapy, and employment services) over 24 weeks. They concluded that methadone and minimal services may be effective only for a minority of patients and that higher levels of psychosocial services resulted in significantly greater reductions in illicit drug use.
In its review of Federal regulations of MMT in the early 1990s, the Institute of Medicine (IOM) concluded that “the full potential of methadone maintenance as a significant public health service to society will be realized only if it is financially and professionally supported to the point at which it can offer necessary habilitative and rehabilitative services (Institute of Medicine, 1995).” It also recognized standard methadone programs offering drug counseling alone with caseloads of 50 patients did not meet that standard, and that many programs could provide only minimal counseling with these caseloads.
Fifteen years after that IOM report was published, only minimal counseling is provided in many MTPs. “Comprehensive” programs, as SM is called in the federal regulations, are rarely comprehensive, yet they do provide some benefit in reducing opioid use and criminal behavior (Ball & Ross, 1991). However, access to even SM is not always readily available or is beyond the economic means of many patients seeking treatment. The question remains: Should these patients be denied whatever benefit they might derive from methadone plus emergency counseling (IM) even if it cannot be accompanied by the minimal levels of scheduled counseling that most MTPs now offer? Providing IM would not be inconsistent with the position that counseling and other psychosocial services are valuable.
Baltimore City had experienced a persistent shortage of SM capacity over many years. In 2001, Schwartz and colleagues undertook a trial of IM, the first to be reported under the conditions dictated by the final 1993 federal regulations (Schwartz et al., 2006, 2008, 2009), and one that of longer duration than that of Yancovitz and colleagues (Yancovitz et al., 1991). In the Schwartz study, at a single MTP, 320 opioid-dependent adults were randomly assigned to IM or to remain on a waiting list. At 4-month follow-up, participants assigned to IM reported sharply reducing their use of illicit opiates in the past 30 days (29.5 days at baseline to 4.2 days at 4 months), obtaining significantly less money from illicit activity ($459 at baseline to $36 at 4 months), and had significantly reduced positive urine tests for opiates (99% to 56%). Patients randomly assigned to IM had a high likelihood of entering regular treatment (75.9% v. 20.8% for waiting list). These authors found similar reductions in heroin use as measured by urine tests at baseline and the time of transfer to standard MTP (from 89.6% to 38.4%) when IM was introduced in 6 not-for-profit MTPs in Baltimore and provided treatment to more than 1,000 patients (Schwartz et al., 2009). These studies demonstrated the benefits of IM compared to no treatment but did not examine the extent to which the absence of regularly scheduled counseling for the 4-month period disadvantaged these patients.
The present study was aimed at clarifying this question and was designed as an extension of our prior studies of IM. In the present study, new admissions to two MTPs in Baltimore were randomly assigned to IM, standard methadone with regular scheduled counseling (SM), or ‘restored’ methadone treatment (RM) in which participants met with a counselor who had a limited case load (at one of the sites only). We hypothesized that the SM and RM conditions would have greater treatment retention, lower self-reported heroin and cocaine use rates, less self-reported criminal behavior, and fewer opiate and cocaine positive drug tests than would the IM condition.
2. Methods
2.1 Participants
Participants were recruited from among heroin-dependent adults who were deemed suitable for admission to one of two MTPs in Baltimore, Maryland. Because no openings for SM were available, these individuals would have been placed on a waiting list for at least two weeks. Study inclusion criteria required that participants: (1) be at least 18 years old; (2) be willing to provide informed consent for study participation; and (3) meet criteria for admission to an MTP (at least one year of meeting DSM-IV criteria for opioid dependence). Study applicants were excluded if they were pregnant or had an acute medical or psychiatric illness that required immediate treatment.
2.2 Sites
The two MTPs were located at a community hospital and at a University Hospital. The study was approved by the IRBs of Friends Research Institute and the participating hospitals/institutions and all participants provided informed consent.
2.3 Measures
Assessments were conducted by one of two trained and unblinded research assistants at study entry and at 2- and 4- months post-study entry and included: (1) Treatment Enrollment Status, and (2) the Addiction Severity Index (ASI). Treatment enrollment status was obtained at follow-up interview through participant self-report and confirmed with the MTP. The ASI is an instrument that has been used extensively in drug-abuse research (McLellan et al., 1992). It measures problem severity in seven domains including alcohol use, drug use, medical, psychological, legal, family and social relationships, and employment status. In each area, specific items can be combined into a composite score, ranging from 0 (no problem) to 1.0 (extreme problem). For the purposes of the present study, items indicating the number of days in the 30 days prior to the interview of heroin and cocaine use and illegal activity, the amount of money spent on drugs and the amount of money obtained from illegal activity were analyzed in addition to the composite scores for all seven domains. Other measures were collected during assessments that are not germane to the present study and hence are not reported here.
The number of counseling sessions received by the participants was measured by counting counselor reports during the course of treatment. The methadone dose during treatment was obtained from the MTPs’ computerized dosing records, and urine samples were obtained at baseline and 1, 2, and 4 months post-baseline and analyzed by a certified laboratory using enzyme multiplied immunoassay testing (EMIT). Urine specimen collection at the clinics for participants who were still enrolled in treatment was observed by clinic staff as per usual procedures while specimens collected by research staff for out-of-treatment participants were not observed. However, because the out-of-treatment urine tests results were for research purposes only and had no consequences, we believe participants had no incentive to falsify specimens. Participants were paid $15 for the baseline and $25 for each of the two follow-up interviews.
2.4 Randomization
The study was a randomized clinical trial conducted utilizing an incomplete factorial design. Participants were block randomized to study condition. Following completion of the informed consent process, baseline assessment procedures, and the physical performed at the program, the research assistant opened a sealed, numbered, and opaque envelope provided by the study’s project director to assign the participants’ study condition. Participants at the first site were randomly assigned to IM or SM. Participants at the second site were randomly assigned to IM, SM, or a third Condition called “Restored” Methadone (RM) in which participants were assigned to an experienced counselor with a lower case load, in an attempt to restore the case loads more typically available at the advent of MTPs in the US. The RM Condition was offered only at one site because of resource limitations.
2.5 Conditions
Participants were admitted to their assigned condition usually within 72 hours following study intake and the usual medical and psychosocial intake procedures of the MTP. IM treatment was provided following federal regulations (42 CFR 8.12), which require: 1) daily methadone administration (i.e., no take-home doses); 2) that IM can not exceed 120 days; and, 3) a minimum of three drug tests. Although no regularly scheduled counseling is available in IM, there was a counselor available to deal with participant crises.
SM treatment was provided in keeping with federal and state regulations, current accrediting standards, and the MTPs usual practices, which permitted take-home doses contingent upon tenure and progress in treatment (e.g., negative drug tests), required regularly scheduled counseling, treatment planning, other psychosocial treatment as needed, and more frequent drug testing than in IM. In keeping with the usual practice of the participating MTPs, participants assigned to SM were expected to attend weekly group and/or individual counseling sessions, although the frequency of counseling could vary with the needs of the participant. Payment for both treatments was based on Maryland’s sliding fee scale. Indigent participants at one site had their fee waived and at the second site were asked to pay $2.00 per week.
RM provided participants with all the services offered in SM. For this Condition, the second site was given additional financial support and the clinic director agreed to provide one of that MTP’s best counselors to provide counseling. That counselor carried a reduced case load not to exceed 25 patients. Such a caseload represented half of the maximum caseload permitted by the Maryland Opioid Treatment Program regulations (Code of Maryland Regulations: 10.47.02.11). Other than the lower case load, the counselor was instructed to see the participants as frequently as the participants wanted and the counselor deemed appropriate. Methadone dosing in all Conditions was provided in a similar manner, usually beginning at around 20 mg daily with gradual daily or every other day increases to an initial target of between 60 and 80 mg.
2.5.1 Statistical analysis
Because of prolonged clinic closures due to counselor shortages at the second site, the sample size for that site did not reach its target of 150 participants. As a result, when intake was stopped only 80 participants had been admitted at this site, including 27 to the Restored Condition, rather than the planned 50 participants for that Condition. Therefore, we present the data two ways. First as three treatment conditions: IM v. SM v. RM and secondly as IM v. both counseling conditions (SM and RM) combined.
Initial analyses involved simple comparisons of the three conditions on various demographic and background drug and criminal history variables using oneway analysis of variance for continuous variables and χ2 goodness-of-fit tests for categorical variables. Analysis comparing the number of days on IM by treatment program site was conducted using oneway analysis of variance. Tests of differences in retention and the number of counseling sessions among the three conditions were conducted using χ2 goodness-of-fit methods.
Regarding drug use and criminal activity outcome variables, separate generalized linear model Poisson regression analyses were conducted for each of the continuous. For the binary outcome variables a generalized estimating equations (GEE) approach was used. Finally, a linear model approach was utilized to assess differences among groups on the seven ASI Composite scores.
3. Results
3.1 Sample Description
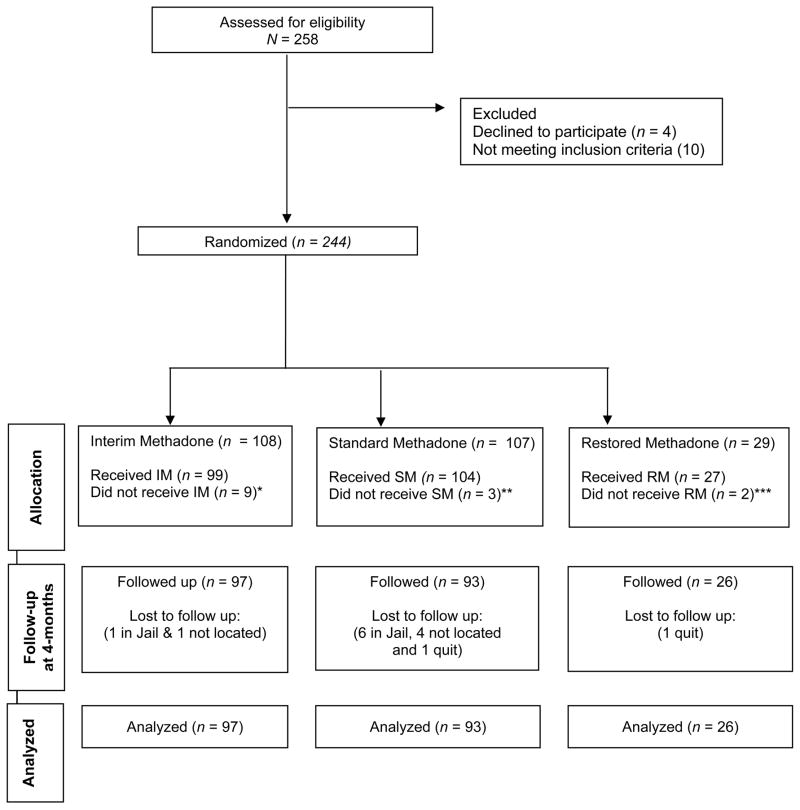
As shown in Table 1, the three conditions were well matched at baseline in terms of their age, gender, race, heroin and cocaine use, positive drug test results, and criminal behavior. As seen in Figure 1 (Consort Diagram), we were able to locate 98.9%, 96.2% and 100% of analyzable participants and successfully interviewed at 4-month follow-up 97.9%, 89.4% and 96.3% of participants in the IM, SM and RM Conditions, respectively.
Table 1.
Participant Characteristics at Baseline
| Variable* | Total (N = 230) | Interim (n = 99) | Standard (n = 104) | Restored (n = 27) |
|---|---|---|---|---|
| Age, Mean (SD) | 43.2 (8.0) | 43.6 (8.2) | 43.5 (7.7) | 40.7 (7.8) |
| Male, Number (%) | 161 (70.0) | 69 (69.7) | 74 (71.2) | 18 (66.7) |
| Race, Number (%) | ||||
| Black | 178 (77.4%) | 78 (78.8) | 79 (76.0) | 21 (77.8) |
| White | 49 (21.3%) | 19 (19.2) | 24 (23.1) | 6 (22.2) |
| Native-American | 2 (0.9%) | 1 (1.0) | 1 (1.0) | 0 |
| Asian | 1 (0.4%) | 1 (1.0) | 0 | 0 |
| Married, Number (%) | 31 (13.5%) | 12 (12.1) | 16 (15.4) | 3 (11.1) |
| Employed in last 30 days, Number (%) | 75 (32.6%) | 27 (27.3) | 42 (40.4) | 6 (22.2) |
| Years of education, Mean (SD) | 11.3 (1.9) | 11.3 (1.6) | 11.3 (1.9) | 11.1 (2.6) |
| Age of onset heroin use, Mean (SD) | 21.5 (7.0) | 20.4 (6.4) | 22.5 (7.5) | 22.0 (7.0) |
| Days of heroin use/last 30 days, Mean (SD) | 29.1 (3.4) | 29.2 (3.0) | 29.1 (3.8) | 29.1 (2.7) |
| Age of onset of cocaine use 1, Mean (SD) | 23.2 (6.8) | 23.0 (6.4) | 23.8 (7.4) | 21.2 (5.1) |
| Days of cocaine use/last 30 days, Mean (SD) | 5.8 (9.1) | 5.4 (8.3) | 6.2 (9.9) | 6.0 (9.3) |
| Age at first crime 2, Mean (SD) | 19.8 (7.8) | 20.5 (8.5) | 19.3 (7.2) | 19.8 (7.3) |
| Money spent on drugs/last 30 days, Mean (SD) | 981 (858) | 962 (1,003) | 927 (737) | 1,256 (670) |
| Illegal income/last 30 days, Mean (SD) | 549 (1,141) | 657 (1,275) | 475 (1,083) | 443 (785) |
| Lifetime months of incarceration, Mean (SD) | 50.6 (67.3) | 51.8 (71.2) | 49.5 (65.6) | 50.2 (61.1) |
| Lifetime number of arrests, Mean (SD) | 10.8 (10.7) | 11.6 (12.4) | 10.5 (9.1) | 8.9 (9.7) |
| Prior MTP episode, (yes) | 107 (46.5) | 53 (53.5) | 39 (37.5) | 15 (55.6) |
Values are mean (SD), except for gender, race, marital and employment status, heroin and cocaine drug test results and prior MTP episode, which are expressed as number of participants (%).
7 participants in the Interim Group, 6 participants in the Standard Group, and 5 participants in the Restored Group never used cocaine, n = 212.
13 participants in the Interim Group, 15 participants in the Standard Group, and 4 participants in the Restored Group denied ever committing a crime, n = 198.
Note: There were no statistically significant differences between groups on any of the variables reported in this table (all ps > .05), except for prior MTP episodes (p = .044).
Figure 1. Consort Diagram.
*Excluded: unstable psychiatric illness (4), not being admitted by MTP (4) and not being heroin-addicted (1)
**Excluded: not admitted by MTP (n = 3)
*** Excluded: sister enrolled in same Condition, excluded by treatment program from Condition, 1 previously enrolled in study at other site
3.2 Treatment
The mean and standard deviation for methadone doses in milligrams for the IM, SM, and RM groups were as follows: at 1 month: 69.9 (10.3); 65.7 (10.9); and 65.6 (8.5); at 2 months: 75.3 (14.6); 71.4 (12.6); and, 66.9 (10.8); and at 4 months: 79.4 (18.5); 76.3 (15.4); and 68.1 (12.6). The differences among the groups at each time period were significant with ps = .014, .01, and .014.
There were significant differences in the number of individual, group, and total number of counseling sessions received by each study condition during the 4-month (17 week) follow-up period (all ps < .001), with the exception of the contrast between the number of group counseling sessions between SM and RM (p=.81). The IM Condition received virtually no counseling, a mean (SD) of 0.7 (1.7) sessions over the 4-month study period. The SM Condition received a mean (SD) of 8.3 (4.8) sessions, including 5.4 individual and 2.9 group sessions, which is approximately one session every other week. In contrast, the RM Condition received the most sessions, a mean (SD) of 17.7 (5.5) sessions, including 14.9 individual and 2.8 group, averaging approximately one session per week.
The mean (SD) number of days in IM prior to transfer to standard treatment at the two sites were 114.2 (20.6) and 112.0 (22.8) days, p > .67. As shown in Table 2, there were no significant differences among groups in terms of retention in treatment at 2 and 4 months (all ps > .05). At 2 months, retention rates were 96%, 89.4% and 96.3%, respectively for IM, SM and RM, and at 4 months, the rates were 91.9%, 80.8%, and 88.9%, respectively.
Table 2.
Outcomes at Baseline, 2- and 4-Month Follow-up
| Variable | Interim (n = 99) | Standard (n = 104) | Restored (n = 27) | Group X Time Interaction Test Statistic | p |
|---|---|---|---|---|---|
|
Drug and criminal activity
| |||||
| Days of heroin use/last 30 days, Mean (SE) | χ2(4) = 5.88 | .21 | |||
| Baseline | 29.2 (0.3) | 29.1 (0.4) | 29.1 (0.5) | ||
| 2-month | 3.3 (0.6) | 5.5 (0.9) | 3.0 (1.1) | ||
| 4-Month | 2.6 (0.5) | 3.6 (0.8) | 2.8 (1.0) | ||
| Days of cocaine use/last 30 days, Mean (SE) | χ2(4) = 8.28 | .082 | |||
| Baseline | 5.4 (0.8) | 6.2 (1.0) | 6.0 (1.7) | ||
| 2-month | 2.1 (0.5) | 3.7 (7.7) | 1.6 (0.5) | ||
| 4-Month | 1.6 (3.8) | 3.0 (7.3) | 1.4 (0.8) | ||
| Days of illegal activity/last 30 days, Mean (SE) | χ2(4) = 15.81 | .003 | |||
| Baseline | 10.44 | 9.40 (1.24) | 10.22 (2.43) | ||
| 2-month | .41 (.32) | 1.78 (.57) | .52 (.51) | ||
| 4-Month | .48 (.29) | 1.11 (.47) | 1.13 (1.13) | ||
| Money spent on drugs/last 30 days, Mean (SE) | χ2(4) = 10.30 | .036 | |||
| Baseline | 962 (100) | 927 (72) | 1256 (127) | ||
| 2-month | 54 (9) | 98 (18) | 59 (11) | ||
| 4-Month | 58 (10) | 80 (21) | 55 (16) | ||
| Illegal income/last 30 days, Mean (SE) | χ2(4) = 68.97 | < .001 | |||
| Baseline | 657 (1275) | 475 (106) | 443 (148) | ||
| 2-month | 9 (7) | 116 (45) | 37 (36) | ||
| 4-Month | 8 (3) | 336 (287) | 113 (113) | ||
| Opiate positive test, n (%) | χ2(4) = .43 | .98 | |||
| Baseline | 95 (97%) | 101 (98%) | 26 (96%) | ||
| 2-month | 50 (54%) | 54 (58%) | 15 (56%) | ||
| 4-month | 44 (46%) | 47 (51%) | 10 (40%) | ||
| Cocaine positive test, n (%) | χ2(4) = 1.90 | .75 | |||
| Baseline | 48 (49%) | 56 (54%) | 10 (37%) | ||
| 2-month | 36 (39%) | 43 (46%) | 10 (37%) | ||
| 4-month | 32 (33%) | 41 (45%) | 6 (24%) | ||
|
| |||||
|
ASI Composite
| |||||
| Medical | F(4, 408) = .55 | .70 | |||
| Baseline | .09 (.02) | .08 (.02) | .08 (.05) | ||
| 2-month | .10 (.03) | .11 (.03) | .07 (.05) | ||
| 4-month | .13 (.03) | .10 (.03) | .19 (.06) | ||
| Employment | F(4, 429) = .87 | .48 | |||
| Baseline | .84 (.03) | .74 (.02) | .66 (.05) | ||
| 2-month | .85 (.03) | .77 (.03) | .58 (.06) | ||
| 4-month | .86 (.03) | .79 (.03) | .57 (.05) | ||
| Alcohol | F(4, 420) = .22 | .93 | |||
| Baseline | .06 (.01) | .06 (.01) | .04 (.02) | ||
| 2-month | .05 (.01) | .04 (.01) | .01 (.02) | ||
| 4-month | .05 (.01) | .04 (.01) | .01 (.02) | ||
| Drug | F(4, 432) = 1.70 | .15 | |||
| Baseline | .35 (.01) | .35 (.01) | .34 (.01) | ||
| 2-month | .08 (.01) | .12 (.01) | .14 (.02) | ||
| 4-month | .08 (.01) | .10 (.01) | .11 (.02) | ||
| Legal | F(4, 423) = .19 | .94 | |||
| Baseline | .24 (.03) | .25 (.03) | .20 (.05) | ||
| 2-month | .05 (.02) | .09 (.02) | .04 (.03) | ||
| 4-month | .03 (.01) | .06 (.01) | .01 (.02) | ||
| Family/Social | F(4, 485) = .39 | .81 | |||
| Baseline | .04 (.01) | .04 (.01) | .06 (.02) | ||
| 2-month | .04 (.01) | .02 (.01) | .04 (.02) | ||
| 4-month | .02 (.01) | .02 (.01) | .02 (.02) | ||
| Psychiatric | F(4, 423) = .48 | .75 | |||
| Baseline | .04 (.01) | .03 (.01) | .01 (.02) | ||
| 2-month | .04 (.01) | .02 (.01) | .02 (.02) | ||
| 4-month | .05 (.01) | .02 (.01) | .01 (.02) | ||
|
| |||||
| Retention in Treatment | χ2(2) | p | |||
|
| |||||
| 2-month | 96.0% | 89.4% | 96.3% | 3.88 | .14 |
| 4-month | 91.9% | 80.8% | 88.9% | 5.62 | .06 |
Note: Due to missing urine samples, the ns for opioid and cocaine urine tests for IM, SM and RM groups are as follows; At Baseline: 98, 103 and 27; At 2 -Month Follow-up: 93, 93 and 27; and 4 -Month Follow-up: 96, 92 and 25).
3.3 Significant Events during the Study
There were 18 serious adverse events during the study, all of which were determined by the FRI IRB to be not study related. Nine participants in IM were hospitalized for medical treatment (two of these individuals had two hospitalizations for the same disorder). Six participants in SM and 1 participant in RM were hospitalized. No study participants were withdrawn from participation as a result of these events. Also, there were seven incarcerations at the 4-month follow-up (1 in IM and 6 in SM) and 38 total incarcerations during the 4 month follow-up period (17 in IM, 18 in SM and 3 in RM).
3.4 Treatment Outcomes
ASI Composite Scores
There were no significant Group X Time interactions on the Alcohol (p=.93), Drug (p=.15), Employment (p=.48), Family (p=.81), Legal ( =.94), Medical (p =.70) or Psychiatric (p=.75) Composite Scores. The main effect for Time was significant only for the Drug Use (p<.001), Legal (p<.001) and Family (p=.044) Composite Scores, all of which declined over Time.
3.5 Drug Use Outcomes
Heroin
There was a significant reduction in self-reported heroin use [χ2(2)=256.04; p<.001] and opioid-positive drug tests [χ2(2)=62.76; p<.001] over Time. As shown in Table 2, all three groups showed a marked decrease in heroin use from baseline (approximately 29 of the last 30 days) to 2 month follow-up period (3.3, 5.5, and 3.0 days for IM, SM and RM, respectively) that was sustained at the 4-month follow-up (2.6, 3.6, and 2.8 days for IM, SM and RM, respectively). However, there was no significant Group x Time interaction effect (p=.21). Similarly, all three groups showed a marked decrease in opioid-positive drug tests from baseline (approximately 97%) to 2-month follow-up (54%, 58%, and 56% for IM, SM and RM, respectively) that was sustained at 4 months post-baseline (46%, 51%, 41% for IM, SM and RM groups, respectively). However, the Group X Time interaction was not significant (p=.98).
Cocaine
There was a significant reduction in self-reported cocaine use [χ2(2)=74.74; p<.001] and cocaine positive drug tests [χ2(2)=6.57; p=.038] over Time. Participants showed a much more modest decrease in self-reported days of cocaine use from baseline to follow-up compared to the decrease shown in heroin use (see Table 2). The Group X Time interaction effect for self-reported cocaine use was not significant (p=.82). In terms of cocaine-positive urine tests, a decrease was seen from baseline to follow-up but the Group X Time interaction was not significant (p=.75).
Crime Outcomes
There was a significant decrease over Time for past 30-day self-reported days of criminal activity, money spent on drugs, and illegal income (all ps<.001). The Group X Time interaction effects for these variables were significant (p =.003, .036, and p < .001, respectively). In all cases, the IM and RM showed greater decreases than the SM group (see Table 2), although only the comparisons between the IM and SM groups in terms of the number of days of illegal activities, money spent on drugs and illegal income at 2 months were significant (all ps<.05).
3.6 Analysis of Interim Methadone vs. Combined Counseling Groups
In order to compare the impact of methadone plus scheduled counseling (combining the SM and RM groups) as compared to IM, we conducted the same analyses as reported above with only two groups. The findings were quite similar. As in the analysis reported above for three groups, χ2 goodness-of-fit tests of 2-month retention showed no significant difference between the two groups (96% retained for the IM group v. 91% for the combined SM and RM group; p = .12). In addition, there were no significant Group X Time interactions for the ASI Composite Scores, the number of days of heroin (p=.23) or cocaine (p=.43) use, or the percentage of opioid (p=.98) or cocaine (p=.79) positive tests. This analysis was also concordant with the three-group analysis in terms of a significant difference in self-reported illegal income (p<.001) favoring the IM group. In contrast to the three-group analysis, there was not a significant difference between the groups in terms of days of criminal activity (p=.12) or the money the participants reported spending on drugs (p=.21), and there was a significant difference between the two groups on 4-month retention with more participants in the IM compared to Combined Counseling group retained (92% v. 82%; p=.03).
4. Discussion
Our hypothesis that the participants receiving scheduled counseling as compared to IM would show greater treatment retention, and greater reductions in illicit drug and self-reported illegal activities was not supported. All groups showed improvement over time, but we found no significant differences favoring the counseling conditions with regard to any of these outcome measures. No significant differences in these measures emerged favoring the counseling conditions when the data were re-analyzed using two conditions by combining SM and RM, except for 4-month retention rate which favored IM.
We found no evidence in our measures that would indicate that the IM participants were substantially disadvantaged by the 4-month period during which only emergency counseling was available. Some medical hospitalizations occurred among these patients, but none were judged to be study-related, nor were they likely to have been prevented by more counseling, although some might have been averted by greater availability of medical services.
There are a number of limitations of the present report that suggest caution in generalizing these findings. First, we note that the amount of counseling patients received even in SM treatment was minimal, averaging only 1 session every other week over the entire 4-month period. Even in the RM group, participants received on average only one session every week over the 4-month period. It is possible that in other programs in other parts of the country where more psychosocial support may be provided, substantial differences between IM and standard MTP would have been seen.
Second, since under current regulations all patients in IM had to be admitted to SM after 120 days, we cannot know whether the patients receiving IM would have remained in treatment and continued to show decreased drug use and self reported illegal activity over a longer period had they not been admitted to SM. More research on this question is needed. In addition, research is needed to better match what is offered to what patients consider helpful and to do so without regulatory constraints. Finally, in the present study, participants were assessed 4 months after starting treatment. There could be a delayed impact of counseling that is not apparent at 4 months but will emerge at a later point (Carroll et al., 1994).
These results appear to be inconsistent with the study of McLellan et al. (1993), but that study of minimal services is probably not entirely comparable to studies of IM in community-based programs because it was conducted with all male veterans at a richly staffed, stable, university-affiliated treatment program. Furthermore, the research design of the McLellan et al. study required that participants receiving minimal services had to be transferred to SM if they tested positive for either heroin or cocaine for eight consecutive weeks or experienced three emergency situations requiring health care. Because of this aspect of the design, 22 (69%) of the 32 patients assigned to the minimal care group were transferred to SM by the 12th week. However, the 10 remaining patients (31%) showed substantial decreases in opiate use, achieving 8 consecutive weeks of opiate-free urine tests.
Our results are largely consistent with studies in community-based programs. In a community-based program with a staffing pattern similar to that in Baltimore clinics, Calsyn and coworkers (Calsyn et al., 1994) in a random assignment study with 360 new MTP admissions found that there was no effect for level of counseling (standard vs. minimal) on the number of positive cocaine drug tests and that the number of positive heroin drug tests was not significantly different based on level of counseling within two groups where positive urine tests jeopardized remaining in treatment; however participants in a “medication only” condition had more positive urine tests when there were no adverse consequences for testing positive. In a randomized trial of levels of counseling for methadone patients receiving isoniazid, increased counseling did not appear to result in further reductions in heroin use (Gruber et al., 2008).
Although not statistically significant, the IM and RM groups had lower reported mean number of days of heroin and cocaine use and mean amounts of illegal income. In this intent-to-treat analysis, these findings could be related to the non-significant differences in 4 month retention in treatment for these groups, since the data were based on all randomly assigned participants regardless of whether they were in or out of treatment.
The findings from our study do not show and should not be interpreted as showing that counseling or other psychosocial services are without value. There are ample studies in the literature, including random assignment designs that demonstrate the importance of the therapeutic alliance and of the efficacy of specific psychosocial treatments in modifying drug using behaviors among methadone patients (Simpson et al., 1997) and non-methadone patients (Carroll et al., 1994). Yet, despite the limitations noted above, the findings of this study support the proposition that providing patients with IM for 4 months results in a sharp reduction in illicit opiate use and illegal activities and appears to do so without causing significant adverse effects when compared with providing patients with methadone along with the regularly scheduled counseling that is typically delivered by many current existing programs.
The finding that some heroin-dependent individuals admitted to IM reduce their drug use and remain in community-based treatment at rates comparable to patients receiving methadone plus scheduled drug counseling has now been replicated in random assignment studies by four different research groups including the present study over a span of almost four decades (Calsyn et al., 1994; Gruber et al., 2008; Senay et al., 1973). It is worthy of note here that in the UK and Australia counseling for methadone treatment is not mandatory, yet evaluations in those countries of methadone treatment consistently find significant improvement in drug use, criminality, and morbidity (Burns et al., 2009; Gossop et al., 2003; Teesson et al., 2008). Nevertheless, methadone regulatory structures at both federal and state levels maintain high barriers to providing IM even on a temporary basis, and impose far more restrictive rules on how such patients are treated after entry. These barriers have the net effect of keeping many treatment-seeking heroin-addicted individuals on the streets engaging in their typical drug-using behavior. Some are relegated to waiting for admission to a subsidized program; while others, where such subsidies are uncommon, are denied methadone because they cannot pay for the required psychosocial services that are by regulation coupled with it. In either case, remaining out-of-treatment for this population has an increased risk of arrest, morbidity, mortality (Clausen et al., 2009; Schwartz et al., 2009).
In the present study, both of the participating clinics had more than one period when intake was curtailed because of a shortage of counselors. Addicted individuals seeking treatment were put on a waiting list. Even if our original hypothesis that SM treatment would be superior to methadone alone had been supported, it would still seem to be a curious policy to prohibit out-of-treatment heroin-addicted individuals from receiving some benefit from methadone alone unless it can be shown that this is in someway harmful to the patients.
Our results strongly suggest that the regulatory structure not just for IM but for opioid agonist treatment of opioid dependencies in general must continue to evolve. One way would be to allow for provision of additional services where these services are both helpful to patients and wanted by them, as suggested by Vincent Dole in 1971 and again in 1991, rather than making such services obligatory. The issue is not just a matter of the economics of paying for services that may or may not be needed, but of a system that for many heroin-addicted individuals has the unintended consequence of denying access to treatment that is demonstrably valuable to the patients and to the society in which they live.
Acknowledgments
We thank Dr. John Urbaitis and Suzanne Harrison at the Sinai Hospital Addiction Recovery Program and Dr. Eric Weintraub, Jewell Benford and Wayne Clemons at the University of Maryland Drug Treatment Center. This research was supported by the National Institutes on Drug Abuse (NIDA) grant 2R01 DA 13636 entitled “Entry into Comprehensive Methadone Treatment via Interim Opioid Maintenance” and by the Abell Foundation which supported the counselor in the Restored Condition. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIDA or the Abell Foundation.
References
- Ball JC, Ross A. The effectiveness of methadone maintenance treatment: Patients, programs, services, and outcomes. New York: Springer-Verlag; 1991. [Google Scholar]
- Burns L, Randall D, Hall WD, Law M, Butler T, Bell J, Degenhardt L. Opioid agonist pharmacotherapy in New South Wales from 1985 to 2006: Patient characteristics and patterns and predictors of treatment retention. Addiction. 2009;104:1363–1372. doi: 10.1111/j.1360-0443.2009.02633.x. [DOI] [PubMed] [Google Scholar]
- Calsyn DA, Wells EA, Saxon AJ, Jackson TR, Wrede AF, Stanton V, Fleming C. Contingency management of urinalysis results and intensity of counseling services have an interactive impact on methadone maintenance treatment outcome. Journal of Addictive Diseases. 1994;13:47–63. doi: 10.1300/j069v13n03_05. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ, Nich C, Gordon LT, Wirtz PW, Gawin F. One-year follow-up of psychotherapy and pharmacotherapy for cocaine dependence. Delayed emergence of psychotherapy effects. Archives of General Psychiatry. 1994;51:989–997. doi: 10.1001/archpsyc.1994.03950120061010. [DOI] [PubMed] [Google Scholar]
- Clausen T, Waal H, Thoresen M, Gossop M. Mortality among opiate users: Opioid maintenance therapy, age and causes of death. Addiction. 2009;104:1356–1362. doi: 10.1111/j.1360-0443.2009.02570.x. [DOI] [PubMed] [Google Scholar]
- Code of Maryland Regulations. Opioid Maintenance Therapy (10.47.02.11) Department of Health and Mental Hygiene. Alcohol and Drug Abuse Administration; Retrieved February 4, 2001 at: http://www.dsd.state.md.us/comar/comarhtml/10/10.47.02.11.htm. [Google Scholar]
- Gossop M, Stewart D, Browne N, Marsden J. Methadone treatment for opiate dependent patients in general practice and specialist clinic settings: Outcomes at 2-year follow-up. Journal of Substance Abuse Treatment. 2003;24:313–321. doi: 10.1016/s0740-5472(03)00040-0. [DOI] [PubMed] [Google Scholar]
- Gruber VA, Delucchi KL, Kielstein A, Batki SL. A randomized trial of 6-month methadone maintenance with standard or minimal counseling versus 21-day methadone detoxification. Drug and Alcohol Dependence. 2008;94:199–206. doi: 10.1016/j.drugalcdep.2007.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbard RL, Rachal JV, Craddock SG, Cavanaugh ER. Treatment outcome prospective study tops: Client characteristics and behaviors before, during, and after treatment. In: Tims FM, Ludford JP, editors. Drug abuse treatment evaluation. Rockville, MD: National Institute on Drug Abuse; 1984. pp. 42–68. [NIDA Research Monograph No. 51] [PubMed] [Google Scholar]
- Retting RA, Yarmolinsky A, editors. Institute of Medicine (IOM) Federal regulation of methadone treatment. Washington, DC: National Academy Press; 1995. [PubMed] [Google Scholar]
- McLellan AT, Arndt IO, Metzger DS, Woody GE, O’Brien CP. The effects of psychosocial services in substance abuse treatment. Journal of the American Medical Association. 1993;269:1953–1959. [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Schwartz RP, Highfield DA, Jaffe JH, Brady JV, Butler CB, Rouse CO, Callaman JM, O’Grady KE, Battjes RJ. A randomized controlled trial of interim methadone maintenance. Archives of General Psychiatry. 2006;63:102–109. doi: 10.1001/archpsyc.63.1.102. [DOI] [PubMed] [Google Scholar]
- Schwartz RP, Jaffe JH, O’Grady KE, Das B, Highfield DA, Wilson ME. Scaling-up interim methadone maintenance: Treatment for 1,000 heroin-addicted individuals. Journal of Substance Abuse Treatment. 2009;37:362–367. doi: 10.1016/j.jsat.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz RP, Jaffe JH, O’Grady KE, Kinlock TW, Gordon MS, Kelly SM, et al. Interim methadone treatment: Impact on arrests. Drug and Alcohol Dependence. 2009;103:148–154. doi: 10.1016/j.drugalcdep.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz RP, Kelly SM, O’Grady KE, Peterson JA, Reisinger HS, Mitchell SG, Wilson ME, Agar MH, Brown BS. In-treatment vs. Out-of-treatment opioid dependent adults: Drug use and criminal history. American Journal of Drug and Alcohol Abuse. 2008;34:17–28. doi: 10.1080/00952990701653826. [DOI] [PubMed] [Google Scholar]
- Senay EC, Jaffe JH, diMenza S, Renault PF. A 48-week study of methadone, methadyl acetate and minimal services. In: Fisher S, Freeman A, editors. Opiate dependence: Origins and treatment. New York, NY: Halstead Press; 1973. pp. 185–201. [Google Scholar]
- Simpson DD, Joe GW, Rowan-Szal GA, Greener JM. Drug abuse treatment process components that improve retention. Journal of Substance Abuse Treatment. 1997;14:565–572. doi: 10.1016/s0740-5472(97)00181-5. [DOI] [PubMed] [Google Scholar]
- Teesson M, Mills K, Ross J, Darke S, Williamson A, Havard A. The impact of treatment on 3 years’ outcome for heroin dependence: Findings from the Australian Treatment Outcome Study (ATOS) Addiction. 2008;103:80–88. doi: 10.1111/j.1360-0443.2007.02029.x. [DOI] [PubMed] [Google Scholar]
- Yancovitz SR, Des Jarlais DC, Peyser NP, Drew E, Friedmann P, Trigg HL, Robinson JW. A randomized trial of an interim methadone maintenance clinic. American Journal of Public Health. 1991;81:1185–1191. doi: 10.2105/ajph.81.9.1185. [DOI] [PMC free article] [PubMed] [Google Scholar]