Abstract
Purpose
To investigate the activities, motivations, and attitudes of radiologists regarding specific computed tomographic (CT) screening examinations by using a survey.
Materials and Methods
All study activities were approved by the institutional review board. A self-administered, mailed survey was used to collect data on the practices and attitudes of U.S. radiologists regarding three CT screening tests—coronary artery calcium scoring (CACS), lung cancer screening CT, and whole-body screening CT. The survey was sent to 1000 diagnostic radiologists who were randomly sampled from the American Medical Association Physician Master-file.
Results
A total of 398 (41.4%) of 961 eligible radiologists completed the survey. Among respondents, 33.6% reported reading CT screening studies, the most common being CACS (26.7%), followed by lung screening (19.2%) and whole-body screening (9.5%). Among respondents, 34.1% supported CACS and 29.9% supported lung CT screening for particular patients, while 1.9% supported whole-body CT screening. The most common reasons reported for reading CT screening studies were responses to requests from physicians (83.3%) or patients (75.0%), while fewer (40.8%) cited patient benefit from screening as a reason.
Conclusion
A substantial proportion of a nationally representative sample of radiologists in the United States reads CT screening studies of the heart, lungs, and whole body and holds favorable attitudes toward CACS and lung CT screening. These attitudes may allow for the premature diffusion of new screening tests into practice before higher-level evidence demonstrates their benefits for population mortality.
The primary goal of population-based screening is to decrease disease-specific morbidity and mortality at a reasonable cost (1–3). Screening examinations performed by using computed tomography (CT)—including CT screening for lung cancer and coronary artery disease and whole-body screening—in asymptomatic patients appeared in clinical practice in the early 1990s, prior to conclusive evidence and professional agreement about their efficacy and cost-effectiveness (4–9). While most population-based CT screening examinations have not been recommended by professional societies, individual physicians and physician groups offer a variety of radiologic screening tests, at times marketing these services directly to consumers (10).
In an era of evidence-based medicine and concern for cost-effectiveness, the marketing and diffusion of CT screening examinations into practice before thorough empirical evaluation raises concern. Screening exposes patients to radiation risks, and there are high false-positive rates. Furthermore, it may provoke patient anxiety, invasive follow-up procedures, and overdiagnosis of disease, leading some to believe that the risks and costs currently outweigh the benefits (6,11–15). Supporters of screening, however, have argued that the benefits of early detection outweigh the risks, and patients should not need to wait for the results of randomized controlled trials to access screening (16–18).
Prior studies by Illes et al (4) and Kalish et al (5) revealed the prevalence of self-referred screening centers through a systematic search of centers advertised on the Internet. In 2001, Illes et al (4) identified 88 centers in the United States, most offering a variety of screening examinations, including coronary artery calcium scoring (CACS), lung CT, whole-body CT, CT colonography, and head CT. In a 2003 follow-up study, Kalish et al (5) found the number of self-referred screening CT centers had increased. They identified 166 self-referred body imaging centers providing a mix of CACS, whole-body CT, lung CT, and CT colonography. While these two studies indicate a rise in the number of self-referral body centers from 2001 to 2003, several large screening franchises have gone out of business since that time, leaving uncertainty about whether CT screening has gone out of fashion or rather taken on a different model in terms of the setting in which screening occurs and the nature of patient referral (19).
The extent to which CT screening—either self-referred or physician referred—has diffused into practice is unknown. In this study, we aimed to estimate the percentage of U.S. radiologists who currently read CACS screening, lung cancer screening CT, and whole-body screening CT studies. We also aimed to assess the demographic differences between radiologists who read CT screening studies and those who do not and describe the motivations of radiologists for reading or not reading CT screening studies. Finally, we aimed to describe radiologists’ personal beliefs about recommending CT screening for specific types of patients and to assess whether these beliefs vary by whether radiologists do or do not read CT screening studies.
Advances in Knowledge.
-
■
One-third of a random sample of U.S. radiologists who read diagnostic CT images of the chest, abdomen, or pelvis also read CT screening studies of the heart, lungs, or whole body.
-
■
Among the items surveyed, radiologists reported responding to physician and patient requests as more important motivations for reading CT screening studies than the belief that patients benefit from screening.
-
■
Most radiologists surveyed are in favor of coronary artery calcium scoring screening and lung cancer CT screening, while few support whole-body CT screening.
-
■
Radiologists are significantly more likely to believe CT screening studies are appropriate if they read them than if they do not.
-
■
Radiologists who read CT screening studies are significantly less likely to believe that professional society endorsement is necessary before offering screening to patients than radiologists not reading CT screening studies.
Implications for Patient Care.
-
■
As experts in imaging, radiologists can play a key role in whether and how CT screening examinations enter practice.
-
■
There should be more professional reflection and discussion about when and under what circumstances providing new image-based screening tests to patients can be beneficial and appropriate.
-
■
CT screening has diffused into practice ahead of strong empirical evidence demonstrating its benefit: Where possible, radiologists should educate themselves and their fellow clinicians and patients about the risks, benefits, and empirical evidence behind CT screening.
Materials and Methods
Study Population
One thousand diagnostic radiologists were randomly sampled from the American Medical Association (AMA) Physician Masterfile database in September 2005. The AMA database contains updated contact information for all practicing physicians in the United States, not only members of the AMA. Interventional radiologists, retired radiologists, and residents were excluded from the sample. All study activities were approved by the institutional review board at the Johns Hopkins Bloomberg School of Public Health.
Questionnaire Development
The survey was designed to collect radiologists’ demographic information, CT screening activities, and attitudes about the risks, benefits, and provision of CT screening tests. Survey questions were developed from the literature and from 12 formative interviews with radiologists, primary care physicians, health services researchers, and those involved in health policy and technology assessment. All interviewees had some expertise in screening, and most were not affiliated with our institution.
Within the survey, we defined CT screening as “an imaging study using Computed Tomography (spiral, electron beam CT, multidetector CT, etc) in asymptomatic patients who may or may not have risk factors for disease.” Specific questions targeted CT screening for lung cancer, CACS, and whole-body CT because these tests were the most commonly marketed to patients at that time (4,5). We designed patient scenarios pertaining to lung screening to reflect the current scientific uncertainty about the benefit of lung screening in smokers: “Should a 55-year-old asymptomatic patient with a 20 pack-year smoking history get lung screening CT?” Similarly, we designed questions about CACS and whole-body CT to reflect the current scientific questions about the appropriateness of these examinations for particular patients. We also included questions about radiologists’ motivations for reading or not reading CT screening studies. Finally, we asked a range of attitudinal questions about evidence requirements, costs, physicians’ roles, direct-to-consumer marketing, and patient self-referral for CT screening examinations.
To achieve face and content validity, the questionnaire was pilot tested and revised at three separate stages with a total of 18 radiologists, six of whom had experience reading CT screening studies and 12 of whom had none. The final 47-question survey took 15–18 minutes to complete. The nature of the study was described in a cover letter, and potential responders were made aware that consent was assumed if they completed the survey. A copy of the survey is available upon request.
Results related to radiologists’ screening practices, motivations for screening, and beliefs about the appropriateness of screening in particular patients, evidence requirements, costs, and provision of screening are presented here.
Data Collection
Each radiologist in the sample received a self-administered, mailed questionnaire. Surveys were mailed in October 2005, and data collection continued through February 2006. Surveys were re-sent to all nonresponders at 1 month and 2 months after initial distribution; there were three total attempts to collect responses. After survey data were entered, links to names and addresses were destroyed before analysis was begun.
Statistical Analysis
Descriptive statistics were used to assess the prevalence of screening activities, attitudes, and beliefs for the total sample. The χ2 tests and Mann-Whitney U tests were used to compare the attitudes and beliefs of those who do and those who do not read CT screening studies. A two-sided P value of less than .05 was considered to indicate a statistically significant difference. All analyses were performed by using a software package (Stata, version 9; StataCorp, College Station, Tex).
Results
Response Rate
A total of 398 (41.4%) of 961 eligible radiologists completed the survey. Of the initial 1000 radiologists sampled, 22 surveys were returned to sender because of a wrong address, 15 radiologists reported they were retired, and two were deceased, leaving 961 eligible for participation. In addition, 25 declined to participate by returning blank surveys, and 538 did not respond to any of the three mailings. There were no significant differences in age, sex, number of years since medical school graduation, or geographic region between responders and nonresponders.
Radiologists who indicated that they never read diagnostic CT studies of the chest, abdomen, or pelvis (n = 30) were excluded from the analysis. We also excluded eight radiologists who indicated that they read virtual colonoscopic CT screening studies, but did not read CACS screening, lung cancer screening, or whole-body CT screening studies. Thus, 360 respondents were included in the analysis. Among these, 348 (96.7%) answered all 47 questions of the survey. The number of respondents who answered each individual question is indicated in the data tables.
Radiologist Demographics and Screening Activities
The demographic and practice characteristics of respondents are shown in Table 1. Among the total sample (n = 360), the mean age was 51.5 years, and the majority were male (78.0% [281 of 360]), in private practice (77.0% [274 of 356]), had practiced radiology for more than 15 years (62.1% [223 of 359]), and were fellowship trained (51.6% [182 of 353]). Most radiologists (84.4% [304 of 360]) spent between 1% and 50% of their professional time reading diagnostic CT studies of the chest, abdomen, and pelvis, while 15.6% (56 of 360) spent more than 50% of their time in this activity. Comparison of the mean age, sex, and regional distribution of radiologists in the entire AMA Physician Masterfile database to those of the 360 radiologists in our sample demonstrates that our sample is nationally representative of radiologists in terms of these demographics: mean age in AMA database (51.8 years) versus that of our respondents (51.5 years), percentage of male radiologists in the AMA database (80.5% [18 889 of 23 451]) versus that of our respondents (78.0% [281 of 360]), and regional distribution in the AMA database versus that of our respondents as follows: Northeast, 25.6% (6012 of 23 451) versus 22.9% (82 of 358); South, 24.1% (5636 of 23 451) versus 26.8% (96 of 358); Midwest, 22.9% (5365 of 23 451) versus 26.0% (93 of 358); Southwest, 11.6% (2725 of 23 451) versus 10.6% (38 of 358); and Pacific, 15.8% (3713 of 23 451) versus 13.7% (49 of 358).
Table 1.
Demographic Characteristics of 360 Radiologists Responding to a National Random Sample Survey
| Parameter | Total (n = 360) | Does Not Read CT Screening Studies (n = 239) |
Reads CT Screening Studies (n = 121) |
P Value* |
|---|---|---|---|---|
| Age (y)† | 51.5 ± .51 | 53.0 ± .63 | 48.5 ± .80 | <.001 |
| Years of practice | .001 | |||
| <5 | 5.9 (21/359) | 4.6 (11/238) | 8.3 (10/121) | |
| 5–15 | 32.0 (115/359) | 28.2 (67/238) | 39.7 (48/121) | |
| 15–30 | 45.1 (162/359) | 46.2 (110/238) | 43.0 (52/121) | |
| >30 | 17.0 (61/359) | 21.0 (50/238) | 9.1 (11/121) | |
| Male | 78.0 (281/360) | 78.6 (187/238) | 76.9 (93/121) | .711 |
| Geographic region | .951 | |||
| Northeast | 22.9 (82/358) | 23.2 (55/237) | 22.3 (27/121) | |
| South | 26.8 (96/358) | 27.4 (65/237) | 25.6 (31/121) | |
| Midwest | 26.0 (93/358) | 26.2 (62/237) | 25.6 (31/121) | |
| Southwest | 10.6 (38/358) | 9.7 (23/237) | 12.4 (15/121) | |
| Pacific | 13.7 (49/358) | 13.5 (32/237) | 14.1 (17/121) | |
| Training other than residency | .539 | |||
| None | 37.1 (131/353) | 37.8 (89/235) | 35.6 (42/118) | |
| Fellowship | 51.6 (182/353) | 51.5 (121/235) | 51.7 (61/118) | |
| PhD | 1.7 (6/353) | .85 (2/235) | 3.4 (4/118) | |
| Master’s | 7.1 (25/353) | 7.2 (17/235) | 6.8 (8/118) | |
| Other | 2.5 (9/353) | 2.5 (6/235) | 2.5 (3/118) | |
| Practice setting | .001 | |||
| Academic | 16.3 (58/356) | 19.1 (45/235) | 10.7 (13/121) | |
| Private | 77.0 (274/356) | 71.5 (168/235) | 87.6 (106/121) | |
| Other | 6.7 (24/356) | 9.4 (22/235) | 1.7 (2/121) | |
| Work time spent reading diagnostic CT studies of chest, abdomen, or pelvis | .001 | |||
| 0%–25% | 47.5 (171/360) | 53.6 (128/239) | 35.5 (43/121) | |
| 25%–50% | 36.9 (133/360) | 33.5 (80/239) | 43.8 (53/121) | |
| 50%–75% | 13.1 (47/360) | 10.9 (26/239) | 17.4 (21/121) | |
| >75% | 2.5 (9/360) | 2.1 (5/239) | 3.3 (4/121) | |
| Compensation method | .201 | |||
| Annual set salary | 27.1 (97/358) | 27.0 (64/237) | 27.3 (33/121) | |
| Partnership profits | 42.5 (152/358) | 39.6 (94/237) | 47.9 (58/121) | |
| Per study read | 5.3 (19/358) | 6.7 (16/237) | 2.5 (3/121) | |
| Some combination | 25.1 (90/358) | 26.6 (63/237) | 22.3 (27/121) | |
| Involved with industry to develop imaging technology | 4.2 (15/359) | 3.4 (8/238) | 5.8 (7/121) | .280 |
Note.—Unless otherwise indicated, data are percentages, with numbers of radiologists in parentheses.
P values were calculated by using the t test for continuous variables, χ2 tests for nominal variables, and the Mann-Whitney U test for ordinal variables.
Data are means ± standard errors of the mean.
One-third of the overall sample (121 of 360 [33.6%]) reported that they read at least one of the three specific CT screening studies for asymptomatic patients. We refer to this group of 121 radiologists as the “screener” group. More specifically, 96 (26.7%) of 360 read CACS screening, 69 (19.2%) of 360 read lung cancer screening, and 34 (9.4%) of 360 read whole-body screening studies. When divided into mutually exclusive screening practice groups, 6.9% (25 of 360) of the overall sample read CACS, lung, and whole-body screening studies, 7.2% (26 of 360) read CACS and lung screening studies, 1.1% (four of 360) read lung and whole-body screening studies, 1.1% (four of 360) read CACS and whole-body screening studies, 11.9% (43 of 360) read only CACS screening studies, 4.4% (16 of 360) read only lung screening studies, and 0.83% (three of 360) of the overall sample read only whole-body screening studies. In addition, 4.2% (15 of 360) of the overall sample reported reading virtual colonographic studies and 1.1% (four of 360) reported reading coronary CT angiographic studies, but these radiologists were included in the sample only if they also read CACS, lung, or whole-body screening CT studies.
Those who read any screening studies were significantly younger (48.5 vs 53.0 years, P < .001), were more likely to work in private practice (87.6% [106 of 121] vs 71.5% [168 of 235], P = .001) than academic or government practice, and spend more time at work reading diagnostic CT studies of the chest, abdomen, or pelvis than those who do not read screening studies (P = .001). Approximately one-third of those who read screening studies (34.5% [41 of 119]) said those examinations were marketed directly to consumers.
Radiologists’ Motivations
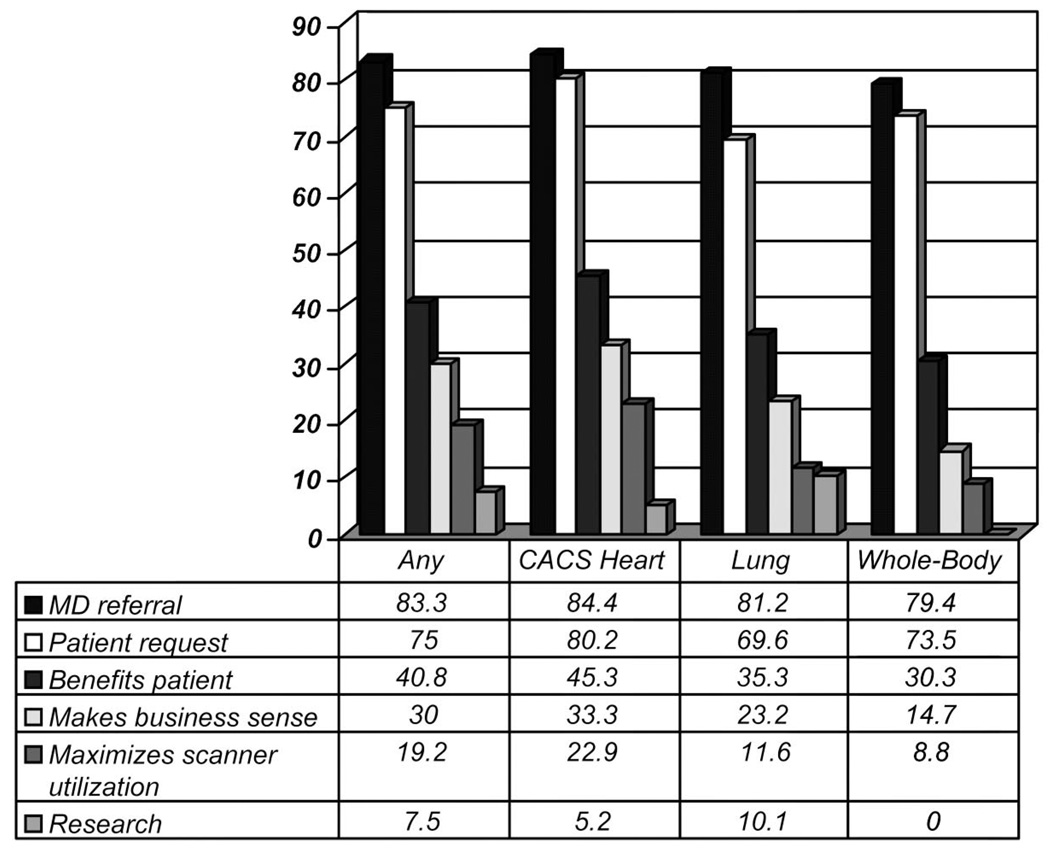
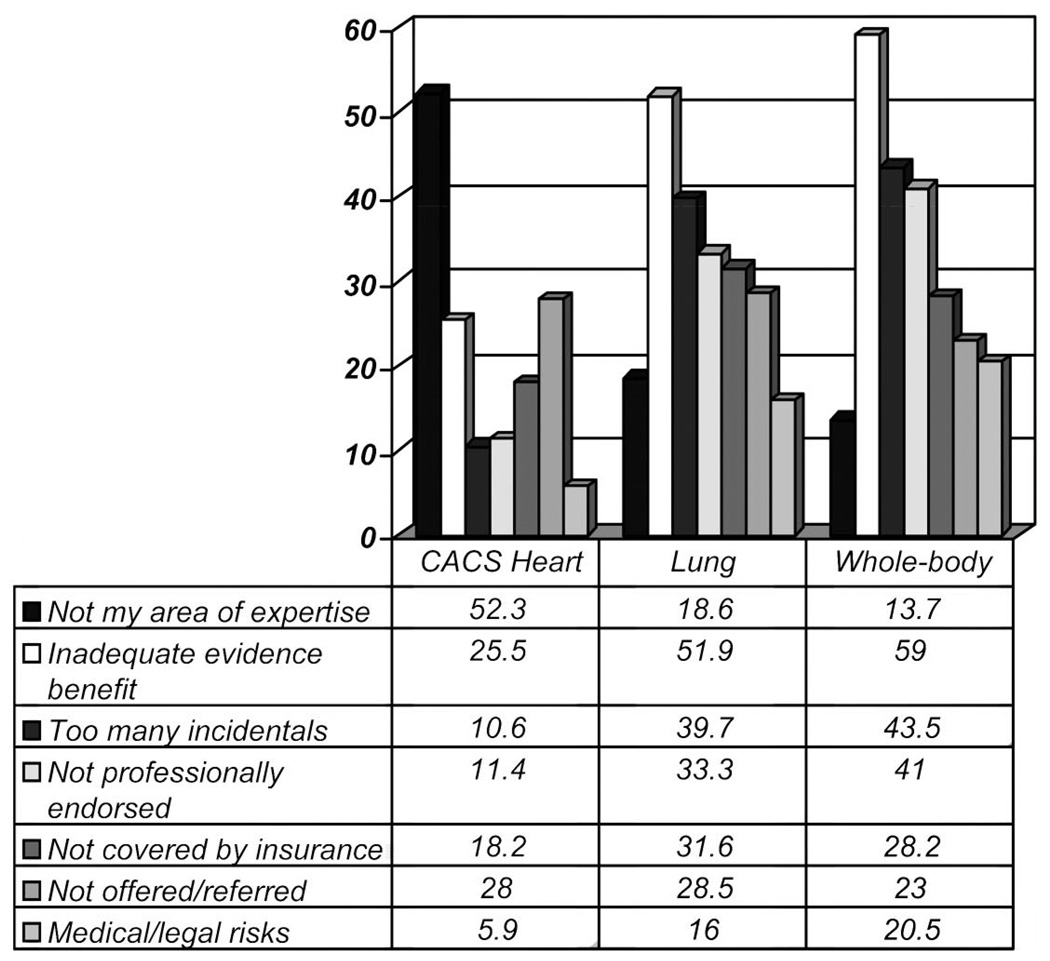
Radiologists who read any CT screening studies (n = 121) were asked to “circle all that apply” from a list of potential reasons why they read CT screening studies (Fig 1). Radiologists who read neither CACS, lung, nor body screening studies (n = 239) similarly were asked to “circle all that apply” of potential reasons for not reading CT screening studies (Fig 2).
Figure 1.
Graph of radiologists’ motivations for reading CT screening studies, among the total sample of radiologists who read them (n=120) and among those who specifically read CACS screening (n=96), lung cancer CT screening (n=69), and whole-body CT screening (n=34) studies. Data in table and bars represent percentage in each group that selected that motivation.
Figure 2.
Graph of radiologists’ motivations for not reading CT screening studies, among those who read neither CACS screening, lung screening, nor whole-body screening studies (n=239). Data in table and bars represent percentage in each group that selected that motivation.
Screeners
Among the radiologists reading any CT screening studies, the two most common reasons for reading screening studies were “referring physicians request it” (83.3% [100 of 120]) and “patients request it” (75.0% [90 of 120]). By contrast, 40.8% (49 of 120) of the total group responded that they read screening CT studies because “it benefits patients.” Thirty percent (36 of 120) of the total group read screening because “it makes good business sense,” and 19.2% (23 or 120) because “it maximizes the utilization of our scanners.”
Nonscreeners
The most popular reason given for not reading CACS studies was “not my area of expertise” (52.3% [125 of 239]), followed by “inadequate evidence that it benefits patients” (25.5% [61 of 239]). The most common reasons given for not reading lung and body screening studies were inadequate evidence of benefit (51.9% [124 of 239] and 59.0% [141 of 239], respectively), followed by “too many incidental findings” (39.7% [95 of 239] and 43.5% [104 of 239], respectively). One hundred twelve radiologists wrote in that one reason they did not read these three studies was because they were not offered by their practice or because they were not requested by referring physicians.
Because factors underlying the decision not to read screening studies might be different for these respondents, a separate analysis of the data for all demographic and attitudinal variables was performed after excluding these 112 individuals; no significant differences in associations were detected.
Radiologists’ Beliefs about the Appropriateness of CT Screening
All radiologists in the sample were asked to respond to three patient scenarios, one each concerning lung, CACS, and body screening (Table 2). The first scenario described a 55-yearold asymptomatic patient with a 20 pack-year smoking history. We found that 29.9% (106 of 354) of radiologists believed that “all such patients should be screened with chest CT for lung cancer,” while 42.4% (150 of 354) believed patients like this should be screened if it is very important to them and 27.7% (98 of 354) believed such patients should not be screened for lung cancer with CT at this time. The second scenario described a 55-year-old asymptomatic patient with hyperlipidemia and family history of heart attack. We found that 34.1% (120 of 352) of radiologists believed that all such patients should be screened for coronary artery disease with CACS, while 46.6% (164 of 352) believed such patients should be screened if it is very important to them and 19.3% (68 of 352) believed such patients should not be screened for coronary artery disease with CACS at this time. Finally, the third scenario described a 55-year-old asymptomatic patient with a family history of either heart attack or cancer. Only 1.9% (seven of 356) of radiologists believed all such patients should undergo whole-body screening CT, while 28.9% (103 of 356) believed such patients should be screened if it is very important to them and 69.1% (246 of 356) believed such patients should not undergo whole-body screening CT at this time. For each of the three screening scenarios, respondents who read a specific CT screening study were significantly more likely to recommend that screening study (CACS, P = .038; lung screening, P = .001; whole-body screening, P = .001).
Table 2.
Radiologists’ Beliefs about the Appropriateness of Lung, Heart, and Whole-Body Screening for Particular Patients
| Parameter | Total Sample | Nonscreeners | Screeners | P Value* |
|---|---|---|---|---|
| Should a 55-year-old with a 20 pack-year smoking history be screened with chest CT for lung cancer? | .001 | |||
| Yes, all such patients | 29.9 (106/354) | 25.5 (73/286) | 48.5 (33/68) | |
| Only if very important to the patient | 42.4 (150/354) | 43.0 (123/286) | 39.7 (27/68) | |
| No, not at this time | 27.7 (98/354) | 31.5 (90/286) | 11.8 (8/68) | |
| Should a 55-year-old with hyperlipidemia and family history of heart attack be screened with CACS? | .038 | |||
| Yes, all such patients | 34.1 (120/352) | 32.3 (83/257) | 38.9 (37/95) | |
| Only if very important to the patient | 46.6 (164/352) | 45.2 (116/257) | 50.5 (48/95) | |
| No, not at this time | 19.3 (68/352) | 22.6 (58/257) | 10.5 (10/95) | |
| Should a 55-year-old with family history of heart attack or cancer undergo a whole-body screening CT? | .001 | |||
| Yes, all such patients | 1.9 (7/356) | 2.2 (7/322) | 0.0 (0/34) | |
| Only if very important to the patient | 28.9 (103/356) | 24.2 (78/322) | 73.5 (25/34) | |
| No, not at this time | 69.1 (246/356) | 73.6 (237/322) | 26.5 (9/34) |
Note.—Data are percentages, with numbers of radiologists in parentheses.
P values are from χ2 comparisons of the distribution of specific screener versus nonscreener responses.
Radiologists’ Attitudes about Evidence Requirements for CT Screening
Respondents were asked four separate questions concerning how important different types of evidence are before recommending screening to individual patients. A majority of radiologists believed that expert opinion, professional endorsement, observational studies, and randomized controlled trials were either preferable or necessary before a CT screening test should be offered to a patient (Table 3). Expert opinion was most likely to be considered necessary (54.3% [195 of 359]), while professional society endorsement was believed to be the least necessary (23.4% [84 of 359]). Compared with non-screeners, screeners were significantly less likely (P = .001) to believe that professional society endorsement was necessary before offering screening examinations to patients.
Table 3.
Radiologists’ Attitudes about Evidence Requirements before Offering CT Screening
| Parameter | Total Sample (n = 359) | Nonscreeners (n = 238) | Screeners (n = 121) | P Value* |
|---|---|---|---|---|
| Experts in the field endorse the screening test | .123 | |||
| Necessary | 54.3 (195/359) | 57.1 (136/238) | 48.8 (59/121) | |
| Preferable | 43.2 (155/359) | 40.8 (97/238) | 47.9 (58/121) | |
| Probably unnecessary | 1.1 (4/359) | 0.42 (1/238) | 2.5 (3/121) | |
| Unnecessary | 1.4 (5/359) | 1.7 (4/238) | 0.83 (1/121) | |
| Professional societies endorse the screening test | .001 | |||
| Necessary | 23.4 (84/359) | 27.3 (65/238) | 15.7 (19/121) | |
| Preferable | 65.5 (235/359) | 64.7 (154/238) | 66.9 (81/121) | |
| Probably unnecessary | 7.5 (27/359) | 5.5 (13/238) | 11.6 (14/121) | |
| Unnecessary | 3.6 (13/359) | 2.5 (6/238) | 5.8 (7/121) | |
| Results of observational studies support the benefit of the screening test | .404 | |||
| Necessary | 46.2 (166/358) | 48.3 (115/238) | 42.2 (51/121) | |
| Preferable | 49.9 (179/358) | 47.1 (112/238) | 55.4 (67/121) | |
| Probably unnecessary | 1.7 (6/359) | 1.7 (4/238) | 1.6 (2/121) | |
| Unnecessary | 2.2 (8/359) | 2.9 (7/238) | 0.83 (1/121) | |
| Results of randomized clinical trials support the benefit of the screening test | .057 | |||
| Necessary | 45.1 (162/359) | 48.7 (116/238) | 38.0 (46/121) | |
| Preferable | 52.6 (189/359) | 49.2 (117/238) | 59.5 (72/121) | |
| Probably unnecessary | 0.28 (1/359) | 0.42 (1/238) | 0.0 (0/121) | |
| Unnecessary | 2.0 (7/359) | 1.7 (4/238) | 2.5 (3/121) |
Note.—Data are responses to the question: “In order to offer a new CT screening test to a patient, how necessary or unnecessary are the following types of evidence?” Data are percentages, with numbers of radiologists in parentheses.
P values are from Mann-Whitney U test comparisons of the distribution of screener versus nonscreener responses.
Discussion
To our knowledge, this is the first study to describe the prevalence of radiologists reading CT screening studies in the United States from a nationally representative rather than targeted sample. This study revealed that one-third of a nationally representative sample of radiologists who read diagnostic CT studies of the chest, abdomen, and pelvis also read CT screening studies of the coronary arteries, lungs, and/or whole body. We found that the most commonly read study was CACS screening (26.7%), followed by lung cancer CT screening (19.2%) and whole-body CT screening (9.4%). These results are similar to unpublished data gathered by using the American College of Radiology’s 2003 Survey of Radiologists (20, 21), a stratified random sample survey of U.S. radiologists that revealed that 24% of diagnostic radiologists personally read lung screening CT studies and 13% read whole-body screening CT studies. Furthermore, while our data reflect the same relative prevalence of the different tests among screening centers that advertise on the Internet as reported by Illes et al (4) and Kalish et al (5), our study results suggest that CT screening is more prevalent than their estimates, probably because they identified only screening that was advertised on the Internet (4,5).
The three CT screening examinations explored in this study—lung cancer screening CT, CACS screening, and whole-body CT screening—are at different stages of evidence and have different professional society recommendations. For example, CACS screening has the most conclusive research evidence of benefit (22,23), and the American College of Cardiology has recently recommended CACS screening for patients with intermediate Framingham risk scores (24). Evidence demonstrating a decreased disease-specific mortality from lung screening in smokers is still emerging and is intensely debated (18,25–27). Results from the Early Lung Cancer Action Program study (18) found that lung screening detects cancers at an earlier stage, while results from the National Lung Screening Trial (28), which uses a randomized controlled design, are anticipated to provide stronger evidence about the impact of screening on population mortality. Professional societies do not advocate lung screening, but some have suggested it may be appropriate for individuals after a careful discussion with their physician regarding the risks, benefits, and uncertainties (29,30).
Few data exist for the impact of whole-body screening. Results of one large case series (31) showed that 32% of patients undergoing whole-body screening required follow-up of important findings, and results of one cost-effectiveness analysis (32) suggest that it has minimal impact on population-based mortality at high cost. Professional societies uniformly discourage whole-body CT screening (8,9,33,34), while several individuals have advocated the development of guidelines in response to the high rate of findings requiring follow-up (31,35). For any emerging screening test, targeting screening at a population with high prevalence of the disease is necessary to avoid excessive false-positive rates. Emerging professional guidelines aim to guide individual risk assessment and define which patients should be included in high disease-prevalence groups.
Given the different stages of evidence and recommendations for these three screening examinations, we were not surprised to find radiologists more likely to believe CACS and lung CT screening appropriate as opposed to whole-body screening. Furthermore, screeners were significantly more likely than nonscreeners to favor screening in all scenarios. The favorable attitudes regarding heart and lung screening reported by most radiologists in this study may contribute to an environment that allows for the diffusion of CT screening into practice before conclusive empirical evidence and professional society endorsement. Furthermore, we were intrigued to find that whereas 70%– 80% cited physician or patient request of the examination as a reason for reading CT screening studies, only 40% cited patient benefit from the examination as a reason. It is also noteworthy that 30% reported “good business sense” and 19.2% reported “maximizing the use of our scanners” as reasons for screening.
As consultants who do not primarily manage patients’ care, the degree to which a radiologist’s screening practices are influenced by hospital or practice policy or by personal estimation of risk and benefit of the examination will vary. Nonetheless, radiologists are in a unique position regarding the diffusion of image-based screening tools. These findings raise questions about the extent of radiologists’ professional duties to educate and discuss the appropriateness of screening CT examinations with referring physicians and patients.
Most radiologists in this study believed that there should be endorsement from experts and professional societies, as well as evidence from observational studies and randomized controlled trials, before screening tests are offered to patients. Notably, we found no significant difference between screeners and nonscreeners in their demand for evidence. This may suggest differences among radiologists in the interpretation of existing evidence for screening or the degree to which evidence is the sole influence on their practice decisions. For example, the literature reveals sharp disagreement regarding whether current data are sufficient to support lung CT screening for smokers. It is possible that those who do and those who do not read lung CT screening studies in our study agree that there should be evidence from clinical trials, but disagree in their view of what counts as convincing evidence. It is also possible that all agree that trials are important, but disagree about whether trials are necessary before they will personally be willing to read studies.
Surveying a national, random sample of all practicing diagnostic radiologists allows for some generalizations about the differences in attitudes between those who do and those who do not read CT screening studies. The response rate of 41% limits generalizability; it remains unknown whether nonresponders were more or less likely to read CT screening studies or have different views about these examinations. While no response bias was found for characteristics we could test, it may exist for other factors. Furthermore, our study could not assess the rate of diffusion of CT screening, given its cross-sectional design. Since these data were collected in 2005, evidence, practices, and attitudes have evolved. Nevertheless, our data provide a baseline against which trends can be measured in the future. To obtain a reasonable response rate, it was necessary to limit the length of the survey questionnaire. Therefore, the depth in which individual issues were covered by our study was limited. For the same reason, we did not explore in detail screening examinations such as CT colonography and coronary CT angiography, which were not among the three most common examinations advertised at the time of our study. A further limitation involved social desirability bias; given the somewhat controversial nature of CT screening, respondents may have been hesitant to give their true opinions. We attempted to minimize this by emphasizing the confidential nature of this study. Because our questionnaire is new, its validity is limited, though we attempted to mitigate this with rigorous pilot testing. Finally, this study was focused on radiologists’ attitudes, but clearly an understanding of referring physicians’ practices and attitudes and patient experiences also are important (36); the results of our study can contribute to future work that explores these perspectives.
As experts in imaging, radiologists should play a key role in whether and how CT screening examinations enter practice. Much of the confusion and controversy surrounding the provision of the three examinations studied will resolve as research continues to better quantify their utility. In light of the current uncertainty, however, we hope that the results from this study stimulate more discussion about when and under what circumstances providing new image-based screening tests to patients can be appropriate. Thinking through these issues now will aid our approach to new image-based screening tests that emerge in the future.
Acknowledgment
We thank Elizabeth Ann Skinner, MSW, for assistance in design of the questionnaire used in this study.
I.M.B. supported by a National Research Service Award from the Agency for Healthcare Research and Quality.
Abbreviations
- AMA
American Medical Association
- CACS
coronary artery calcium scoring
Footnotes
From the 2006 RSNA Annual Meeting.
Author contributions:
Guarantors of integrity of entire study, I.M.B., N.E.K.; study concepts/study design or data acquisition or data analysis/interpretation, all authors; manuscript drafting or manuscript revision for important intellectual content, all authors; manuscript final version approval, all authors; literature research, I.M.B.; statistical analysis, I.M.B.; and manuscript editing, all authors
Authors stated no financial relationship to disclose.
References
- 1.Morrison A. Screening in chronic disease. New York, NY: Oxford University Press; 1992. [Google Scholar]
- 2.Black WC, Welch HG. Screening for disease. AJR Am J Roentgenol. 1997;168:3–11. doi: 10.2214/ajr.168.1.8976910. [DOI] [PubMed] [Google Scholar]
- 3.Kopans DB, Monsees B, Feig SA. Screening for cancer: when is it valid?— lessons from the mammography experience. Radiology. 2003;229:319–327. doi: 10.1148/radiol.2292021272. [DOI] [PubMed] [Google Scholar]
- 4.Illes J, Fan E, Koenig BA, Raffin TA, Kann D, Atlas SW. Self-referred whole-body CT imaging: current implications for health care consumers. Radiology. 2003;228:346–351. doi: 10.1148/radiol.2282021083. [DOI] [PubMed] [Google Scholar]
- 5.Kalish GM, Bhargavan M, Sunshine JH, Forman HP. Self-referred whole-body imaging: where are we now? Radiology. 2004;233:353–358. doi: 10.1148/radiol.2332031964. [DOI] [PubMed] [Google Scholar]
- 6.Lee TH, Brennan TA. Direct-to-consumer marketing of high-technology screening tests. N Engl J Med. 2002;346:529–531. doi: 10.1056/NEJM200202143460715. [DOI] [PubMed] [Google Scholar]
- 7.Hillman BJ. CT screening: who benefits and who pays. Radiology. 2003;228:26–28. doi: 10.1148/radiol.2281021733. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Preventive Services Task Force. Cancer screening recommendations. [Accessed November 2004]; http://www.ahrq.gov/clinic/uspstfix.htm.
- 9.American College of Radiology. Position statement on full-body CT screening. [Accessed December 2004]; http://www.acr.org.
- 10.Illes J, Kann D, Karetsky K, et al. Advertising, patient decision making, and self-referral for computed tomographic and magnetic resonance imaging. Arch Intern Med. 2004;164:2415–2419. doi: 10.1001/archinte.164.22.2415. [DOI] [PubMed] [Google Scholar]
- 11.Brenner DJ, Elliston CD. Estimated radiation risks potentially associated with full-body CT screening. Radiology. 2004;232:735–738. doi: 10.1148/radiol.2323031095. [DOI] [PubMed] [Google Scholar]
- 12.Stanley RJ. Inherent dangers in radiologic screening. AJR Am J Roentgenol. 2001;177:989–992. doi: 10.2214/ajr.177.5.1770989. [DOI] [PubMed] [Google Scholar]
- 13.Hunink MG, Gazelle GS. CT screening: a trade-off of risks, benefits, and costs. J Clin Invest. 2003;111:1612–1619. doi: 10.1172/JCI18842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fenton JJ, Deyo RA. Patient self-referral for radiologic screening tests: clinical and ethical concerns. J Am Board Fam Pract. 2003;16:494–501. doi: 10.3122/jabfm.16.6.494. [DOI] [PubMed] [Google Scholar]
- 15.Welch HG. Berkeley, Calif: University of California Press; 2004. Should I be tested for cancer? maybe not and here’ s why. [Google Scholar]
- 16.Brant-Zawadzki M. CT screening: why I do it. AJR Am J Roentgenol. 2002;179:319–326. doi: 10.2214/ajr.179.2.1790319. [DOI] [PubMed] [Google Scholar]
- 17.Brant-Zawadzki MN. Screening on demand: potent of a revolution in medicine. Diagn Imaging (San Franc) 2000;22:25–27. [PubMed] [Google Scholar]
- 18.Henschke CI, Yankelevitz DF, Libby DM, Pasmantier MW, Smith JP, Miettinen OS. Survival of patients with stage I lung cancer detected on CT screening. N Engl J Med. 2006;355:1763–1771. doi: 10.1056/NEJMoa060476. [DOI] [PubMed] [Google Scholar]
- 19.Kolata G. New York Times: 2005. Jan 23, Rapid rise and fall for body-scanning clinics. [Google Scholar]
- 20.Sunshine JH, Lewis RS, Bhargavan M. A portrait of interventional radiologists in the United States. AJR Am J Roentgenol. 2005;185:1103–1112. doi: 10.2214/AJR.05.0237. [DOI] [PubMed] [Google Scholar]
- 21.Bhargavan M, Sunshine JH. Workload of radiologists in the United States in 2002–2003 and trends since 1991–1992. Radiology. 2005;236:920–931. doi: 10.1148/radiol.2363041316. [DOI] [PubMed] [Google Scholar]
- 22.O’ Rourke RA, Brundage BH, Froelicher VF, et al. American College of Cardiology/American Heart Association Expert Consensus document on electron-beam computed tomography for the diagnosis and prognosis of coronary artery disease. Circulation. 2000;102:126–140. doi: 10.1161/01.cir.102.1.126. [DOI] [PubMed] [Google Scholar]
- 23.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291:210–215. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- 24.Greenland P, Bonow RO, Brundage BH, et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force. J Am Coll Cardiol. 2007;49:378–402. doi: 10.1016/j.jacc.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 25.Hartman TE, Swensen SJ. CT screening for lung cancer. Semin Roentgenol. 2005;40:193–196. doi: 10.1053/j.ro.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 26.Swensen SJ, Jett JR, Hartman TE, et al. CT screening for lung cancer: 5-year prospective experience. Radiology. 2005;235:259–265. doi: 10.1148/radiol.2351041662. [DOI] [PubMed] [Google Scholar]
- 27.Black C, Bagust A, Boland A, et al. The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews. Health Technol Assess. 2006;10(iii–iv, ix–x,):1–90. doi: 10.3310/hta10030. [DOI] [PubMed] [Google Scholar]
- 28.National Cancer Institute National Lung Screening Trial. [Accessed November 2007]; http://www.cancer.gov/nlst.
- 29.Ganti AK, Mulshine JL. Lung cancer screening. Oncologist. 2006;11:481–487. doi: 10.1634/theoncologist.11-5-481. [DOI] [PubMed] [Google Scholar]
- 30.Strauss GM, Dominioni L, Jett JR, Freedman M, Grannis FW., Jr Como international conference position statement: lung cancer screening for early diagnosis 5 years after the 1998 Varese conference. Chest. 2005;127:1146–1151. doi: 10.1378/chest.127.4.1146. [DOI] [PubMed] [Google Scholar]
- 31.Furtado CD, Aguirre DA, Sirlin CB, et al. Whole-body CT screening: spectrum of findings and recommendations in 1192 patients. Radiology. 2005;237:385–394. doi: 10.1148/radiol.2372041741. [DOI] [PubMed] [Google Scholar]
- 32.Beinfeld MT, Wittenberg E, Gazelle GS. Cost-effectiveness of whole-body CT screening. Radiology. 2005;234:415–422. doi: 10.1148/radiol.2342032061. [DOI] [PubMed] [Google Scholar]
- 33.U.S. Food and Drug Administration. Whole body scanning using computed tomography. [Accessed August 2002]; http://www.fda.gov/cdrh/ct/
- 34.Council on Scientific Affairs, American Medical Association. Featured report: commercialized medical screening (A-03) [Accessed July 2003]; http://www.ama-assn.org/ama/pub/category/13628.html.
- 35.Hall FM, Casola G, Sirlin CB, Furtado CD, Aguirre DA, Brown MA. Callback and follow-up guidelines for whole-body CT screening. Radiology. 2006;241:627–629. doi: 10.1148/radiol.2412051871. [DOI] [PubMed] [Google Scholar]
- 36.Iglehart JK. The new era of medical imaging: progress and pitfalls. N Engl J Med. 2006;354:2822–2828. doi: 10.1056/NEJMhpr061219. [DOI] [PubMed] [Google Scholar]