Abstract
Objectives
The purpose of this analysis was to compare health care expenditures between insured patients with back pain, fibromyalgia syndrome, or menopause symptoms who used complementary and alternative medical (CAM) providers for some of their care to a matched group of patients who did not use any CAM care. Insurance coverage was equivalent for both conventional and CAM providers.
Design
Insurance claims data for 2000–2003 from Washington State, which mandates coverage of CAM providers, were analyzed. CAM-using patients were matched to CAM-nonusing patients based on age group, gender, index medical condition, overall disease burden, and prior-year expenditures.
Results
Both unadjusted tests and linear regression models indicated that CAM users had lower average expenditures than nonusers. (Unadjusted: $3,797 versus $4,153, p = 0.0001; β from linear regression -$367 for CAM users.) CAM users had higher outpatient expenditures that which were offset by lower inpatient and imaging expenditures. The largest difference was seen in the patients with the heaviest disease burdens among whom CAM users averaged $1,420 less than nonusers, p < 0.0001, which more than offset slightly higher average expenditures of $158 among CAM users with lower disease burdens.
Conclusions
This analysis indicates that among insured patients with back pain, fibromyalgia, and menopause symptoms, after minimizing selection bias by matching patients who use CAM providers to those who do not, those who use CAM will have lower insurance expenditures than those who do not use CAM.
Introduction
The use of complementary and alternative medicine (CAM) has grown in recent decades,1,2 and as a result insurance coverage for various types of CAM providers has become more prevalent.1,3–5 But due to concern over ever-increasing health care costs, increasing emphasis is being given to cost-effectiveness of care. Patients desire choices in sources of health care, but if CAM providers are to be added to insurance coverage, their care must be cost effective.
One researcher noted that CAM therapies may be good candidates not only for cost-effective care but even cost savings, because “they avoid high technology, offer inexpensive remedies, and harness the power of vis medicatrix naturae (the body's natural ability to heal itself )”6. However, several difficulties have hindered the assessment of CAM's cost effectiveness. One of the biggest challenges in evaluating the effect of CAM use on health care costs is the selection bias inherent in patients' self-selection into CAM using and non-CAM using groups.7 Researchers have consistently reported that CAM users have poorer health status, more visits to conventional providers, and/or higher rates of hospitalization than nonusers.8–14 Thus, it has been difficult to find or create comparable groups of CAM users and nonusers for which costs can be compared.
In the early 1990s, a Swiss group conducted a randomized clinical trial offering free insurance coverage of CAM providers to half of a group of insured individuals. They reported that covering CAM care did not lead to an increase in costs for the insurance company because CAM utilization comprised only a tiny percentage of overall expenditures.15 Given the increase in CAM use since the early 1990s in the United States,12 the cost of CAM coverage today might be larger than that found in the Swiss study. However, data from Washington State, which mandates private insurance coverage of all licensed CAM providers,16 found a similar tiny percentage of expenditures devoted to CAM care based on data from 2002.17 The Washington State data reflect self-selection of patients into CAM-using and nonusing groups and thus may reflect a more “real-world” experience for insurance companies than the Swiss randomized study.
Another difficulty in performing economic analyses of CAM use occurs because many CAM providers are not covered by insurance, and patients pay for their services out of pocket. As a result, data on CAM utilization and expenditures are not available in administrative databases and must be collected through primary data collection,6 which may be subject to recall bias and response bias. Washington State provides a unique environment in which to perform an economic analysis of CAM use because of the state-mandated insurance coverage referenced above. As a result, administrative claims data from Washington State include data on CAM utilization and expenditure that are consistent with data for conventional care.
A final difficulty in performing a cost–benefit evaluation of CAM involves measuring outcomes of care. Data on outcomes of care are not available in the administrative claims databases often used to provide data on expenditures. With CAM care, a further difficulty lies in how to quantify what Hollinghurst refers to as “the wider benefits of CAM,” some of which may appear over long periods of time or be based more on a patient's sense of well-being than a measurable clinical outcome.7,18 To avoid these problems in measuring outcomes, this analysis takes a cost-minimization approach,6 analyzing which of two approaches to care is associated with lower overall expenditures, assuming comparable health outcomes between the two approaches.
The purpose of this article is to compare insurance expenditures for matched groups of CAM users and nonusers with selected health conditions, to evaluate whether use of CAM for some care is associated with higher or lower overall health care expenditures.
Materials and Methods
Population
This research was approved by the institutional review boards of the University of Washington and Boise State University. The study sample was constructed using 2000–2003 enrollment and claims data from two large insurance companies in Washington State that offer a variety of product types. The analysis was restricted to insured individuals covered by the law requiring coverage of CAM providers, which excluded enrollees funded through Medicare, Medicaid, or other state or federal programs. The data acquisition process, data cleaning, and the creation of analytic variables have been previously described.19 The analyses presented here were limited to adults aged 18–64 who had at least 2 continuous years of coverage and at least one visit that contained a diagnosis for one of the index conditions defined below.
Index conditions
Three health conditions were chosen for study: back pain, fibromyalgia syndrome (FMS), and menopause symptoms. These index conditions were selected because a substantial proportion of associated patients use CAM for at least part of their care.17,20,21 FMS was defined as at least one visit containing ICD-9 code 729.1. Low back pain and menopause symptoms were defined using the Johns Hopkins Adjusted Clinical Group (ACG) software, Version 8,22 which groups ICD-9 codes per visit into expanded diagnosis clusters (EDC). Low back pain was defined as EDC MUS14 (Low Back Pain) and menopause symptoms was defined as EDC FRE11 (Menopausal Symptoms).
Time frame
Two (2) time periods of interest were created. The “study year” for each patient started on the day of the first visit for an index condition and continued for 365 days; and the “prior year” for each patient was defined as the 365 days preceding the first visit for the index condition. All data were derived from calendar years 2000–2003.
Patients included in the analysis had at least one provider visit containing an ICD-9 code/EDC for an index condition during the study year and no visits containing an ICD-9 code/EDC for the index condition during the prior year.
Provider types
CAM providers were defined as chiropractors, licensed massage therapists, acupuncturists, and naturopathic physicians. Conventional providers were defined as physicians (including osteopaths and specialists), advanced registered nurse practitioners, and physician assistants.
Dependent variables
Dependent variables were total allowed expenditures in the study year, outpatient expenditures, expenditures related to the index condition, and expenditures related to imaging procedures (back pain patients only). Data for each visit included the dollar amount the insurance company allowed for that visit. These amounts were totaled over the study year to create total allowed expenditures. For some analyses, these totals are broken out into allowed expenditures for CAM visits versus allowed expenditures for conventional visits. Imaging expenditures were divided into expenditures for plain radiographs and expenditures for all other types of imaging (e.g., magnetic resonance imaging [MRI], computed tomography). Imaging expenditures were further divided into those that occurred within 28 days of the initial diagnosis (called “early” imaging) and those that occurred more than 28 days after initial diagnosis. This division was based on the Healthcare Effectiveness Data and Information Set recommendation that no imaging should be performed within the first 28 days after an initial diagnosis of back pain.23
Independent variables
Age, gender, and zip code were included in the claims information along with ICD-9 diagnosis codes, dates and types of visits, and providers seen. County population was calculated based on 2000 census data and then categorized as <100,000; 100,000–400,000; and >400,000.
CAM users were defined as patients with at least one visit to a CAM provider for the index condition during the study year. Most also had at least one visit to a conventional provider for the index condition. CAM nonusers were those with no visits to a CAM provider for any reason during the study year and at least one visit to a conventional provider for the index condition during the study year.
Overall disease burden for each patient was constructed using the Resource Utilization Band (RUB) index created by the Johns Hopkins ACG software described above. RUBs estimate the overall disease burden and expected resource use for each individual, and are created by grouping individuals with similar levels of expected resource use based on the ACG index. Lower RUBs included individuals with less expected resource use and higher RUBs included those with greater expected resource use. Throughout the Results and Tables, the term “Low disease burden” refers to patients in RUBs 1 and 2; “Moderate disease burden” refers to patients in RUB 3; and “High disease burden” refers to patients in RUBs 4 and 5. For the regression analysis, disease burden was dichotomized into high versus moderate or low.
Matching
Because patients were not randomly assigned to use CAM but rather self-selected into CAM users and nonusers, we used a matching process to create groups that were as comparable as possible, using a frequency matching process. That is, each CAM user was placed into a stratum based on index condition, gender, 10-year age group, total allowed expenditures during the prior year (matched within $1,000 up to $9,999; all expenditures $10,000 or above were grouped), and disease burden categorized as high, medium, or low during the study year. The number of CAM users in each stratum was determined and half that number of CAM nonusers in each stratum was randomly identified, resulting in a 2:1 match. The 2:1 matching process was necessary because there were too few CAM nonusers in many strata to create a 1:1 match. There were 1330 potential strata, of which 770 contained at least one CAM user. In 256 strata there were an odd number of CAM users, creating the need for a de facto 3:1 match for these individuals. In addition, there were 125 CAM users who could not be matched due to too few controls in the stratum. All CAM users were included in the analysis, including the total of 381 (1.4%) described above who could not be placed in a 2:1 match. Characteristics of unmatched CAM users are described in the Results section.
Statistical analysis
Independent samples t tests were used for unadjusted comparisons of expenditures (total, outpatient, and expenditures related to index condition) between CAM users and nonusers, also to compare mean age. Chi-square tests were used to compare distributions of gender, disease burden, county population, and insurance companies between CAM users and nonusers.
Linear regression analysis was used to perform adjusted comparisons of total expenditures between CAM users and nonusers after adjustment for age, gender, disease burden, county population, and insurance company. Disease burden was dichotomized as high disease burden versus low or moderate disease burden, and an interaction term between CAM use status and disease burden was included in the model. Beta estimates for the interaction terms were calculated using the lincom function in Stata (Stata Corp., College Station, TX).24 Models were constructed for all patients combined and then separately for those with each index condition.
Although expenditure data are highly skewed, leading to a violation of the requirement for constant variance and for normally distributed residuals from the model, the large sample size available here ensures that estimates will be accurate, based on the Central Limit Theorem (CLT).25 However, it was not apparent whether the groups with FMS (n = 5508) or menopause (n = 6566) were large enough for the CLT to apply for the two models created from these smaller samples. Two (2) simulation analyses were performed to determine this, one analysis for the FMS group and the other for the menopause group. In each case, 1000 bootstrap samples were created from the original sample and regression analyses were performed. If the CLT is applicable, 95% of the β estimates from these 1000 models should fall in the 95% confidence interval based on the entire group. Results of the analysis showed that for the FMS group, 97.2% of the β estimates fell into the 95% confidence interval, and for the menopause group, 96.8% of the β estimates fell into the 95% confidence interval. Based on these results, we were confident that the linear regression models would give us accurate estimates in spite of the skewed nature of the dependent variable. To ensure accurate inference, “robust” standard errors were used.26 Stata version 10 was used for all analyses.27
Results
A total of 26,466 CAM users were identified for this analysis: 18,343 with back pain, 3722 with FMS, and 4401 with menopause. These were matched to 13,025 CAM nonusers on a 2:1 basis. There were 381 (1.4%) CAM users who were not matched in this process; 125 due to having no matching controls available and the remaining 256 due to having an odd number of CAM users in some strata. All CAM users were included in the analysis. Those who were unmatched were younger (mean 42.4 versus 45.2 years, p < 0.0001); had higher average total expenditures in the study year ($5,902 versus $3,766, p < 0.0001), and had heavier disease burdens in the study year (46% in highest category versus 33% among matched CAM users, p < 0.0001). To the extent the inclusion of these unmatched CAM users may lead to bias, it will make CAM users look more expensive than the matched controls. However, because the unmatched CAM users are only 1.4% of all CAM users, any bias will be small. For example, as stated above, the mean total expenditure was $3766 for matched CAM users. When the 381 unmatched CAM users were included, mean expenditure for all CAM users was $3,797.
Table 1 displays the comparison of the CAM users and nonusers. The groups did not differ on average age, average allowed expenditures in the prior year, percent female, or disease burden in the study year; that is, as expected, users and nonusers did not differ on any of the matching criteria. CAM users and nonusers were not matched on county population or insurance company, and CAM users were less likely to live in urban counties than nonusers, also more likely to be from insurance company B.
Table 1.
Comparison of Complementary and Alternative Medicine (CAM) Users and Nonusersa Matched on Age Group, Gender, Allowed Expenditures in Prior Year, and Disease Burden in Study Year
| CAM users (n = 26,466) | CAM nonusers (n = 13,025) | p-value | |
|---|---|---|---|
| Average age (SD) | 45.2 (10.5) | 45.4 (10.6) | 0.14 |
| Average allowed expenditures in prior year (SD) | $2,494 (6351) | $2,454 (6114) | 0.55 |
| Percent female | 66.6% | 66.7% | 0.80 |
| Disease burden in study year | |||
| Low | 8.3% | 8.1% | 0.72 |
| Moderate | 58.3 | 58.7 | |
| High | 33.4 | 33.2 | |
| County population | |||
| <100,000 | 11.9 | 8.4 | <0.001 |
| 100,000–400,000 | 15.2 | 11.0 | |
| >400,000 | 72.9 | 80.6 | |
| Insurance company | |||
| A | 90.8 | 92.6 | <0.001 |
| B | 9.2 | 7.4 | |
CAM users, those with at least one visit to a CAM provider related to index condition during study year; nonusers, no visit to a CAM provider for any reason during study year.
SD, standard deviation.
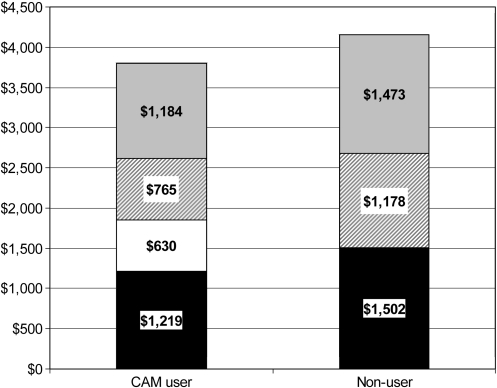
Table 2 displays the results of unadjusted t-tests which showed that CAM users had lower overall average expenditures than nonusers in the study year ($3,797 versus $4,153, p = 0.0001). The distribution of expenditures for outpatient, inpatient, and other expenditures differed between the two groups; CAM users had higher average outpatient expenditures ($1,848 versus $1,502, p < 0.0001) but lower inpatient expenses and lower expenses for other types of claims not linked to a specific provider visit such as imaging and lab claims (Fig. 1). Among CAM users, expenditures for conventional outpatient care were lower than among CAM nonusers ($1,219 versus $1,502, p < 0.0001), but this was offset by CAM expenditures, which averaged $630 per user.
Table 2.
Comparison of Expenditures Between Complementary and Alternative Medicine (CAM) Users and Nonusers in Study Year
| CAM users (n = 26,466) | CAM nonusers (n = 13,025) | p value | |
|---|---|---|---|
| Average allowed expenditures in study year: | Mean (SD) | Mean (SD) | |
| Total | $3,797 (7623) | $4,153 (9505) | 0.0001 |
| Outpatient: Total | $1,848 (2370) | $1,502 (3027) | <0.0001 |
| Conventional | $1,219 (2214) | $1,502 (3027) | <0.0001 |
| CAM | $630 (746) | 0 | |
| Total related to index condition | $588 (1280) | $554 (1947) | 0.04 |
| Outpatient related to index condition | 445 (594) | 231 (438) | <0.0001 |
SD, standard deviation.
FIG. 1.
Average annual allowed expenditures by complementary and alternative medicine (CAM) use status. Solid black, outpatient expenditures from conventional providers; solid white, outpatient expenditures from CAM providers; gray stripe, inpatient expenditures; solid gray, other expenditures not related to a provider visit, such as imaging and lab work.
When analyses were restricted to visits related to the index condition, total average expenditures were slightly higher among CAM users ($588 versus $554, p = 0.04), while average outpatient expenditures related to the index condition were much higher among CAM users ($445 versus $231, p < 0.0001) (Table 2). The expenditure patterns were similar within each condition (Table 3).
Table 3.
Expenditures by Disease Condition and CAM Use Status
| |
Back pain |
FMS |
Menopause |
|||
|---|---|---|---|---|---|---|
| User | Nonuser | User | Nonuser | User | Nonuser | |
| N | 18,343 | 9074 | 3722 | 1786 | 4401 | 2165 |
| Mean allowed expenditures in study year | ||||||
| Total | $3,410*** | $3,739 | $4,830* | $5,449 | $4,535 | $4,818 |
| Outpatient | $1,637*** | $1,312 | $2,374*** | $1,840 | $2,285** | $2,019 |
| Total related to index condition | $677 | $660 | $554*** | $412 | $249** | $223 |
| Outpatient related to index condition | $511*** | $259 | $407*** | $170 | $207** | $166 |
p < 0.05; **p < 0.01; ***p < 0.001.
FMS, fibromyalgia syndrome.
The linear regression analysis revealed a significant interaction between CAM use and disease burden. Among those in the low or moderate disease burden category, CAM users were predicted to have mean total expenditures $160 higher than nonusers. However, among those with high disease burden, predicted mean expenditures for CAM users were $1,421 lower than for nonusers (β: $6,726 for nonusers compared to $5,305 for CAM users, p < 0.001) (Table 4). When a model was fit excluding the interaction term, the β coefficient for CAM use was -$367 (standard error = $90, p < 0.001), confirming that overall, after adjustment, CAM users as a group have lower average total expenditures than nonusers. Similar results were seen in regression models restricted to each index condition.
Table 4.
Results of Linear Regression Modela
| |
All conditions (n = 39,491) |
Back pain (n = 27,417) |
FMS (n = 5508) |
Menopause (n = 6566) |
||||
|---|---|---|---|---|---|---|---|---|
| β | SE | β | SE | β | SE | β | SE | |
| Interaction of CAM use and disease burden: | ||||||||
| Low disease burden, CAM nonuser | Reference category | |||||||
| Low disease burden, CAM user | $160*** | $37 | $93* | $41 | $392*** | $114 | $322** | $108 |
| High disease burden, CAM nonuser | $6,726*** | $230 | $6526*** | $267 | $7,973*** | $747 | $6468*** | $476 |
| High disease burden, CAM user | $5305*** | $129 | $5,196*** | $164 | $5,849*** | $302 | $5,335*** | $287 |
| Other covariates in the model: | ||||||||
| Age | $28*** | $4 | $31*** | $4 | $11 | $17 | $22 | $19 |
| Sex | $478*** | $88 | $452*** | $87 | $615 | $333 | – | – |
| County pop 100k–400kb | $166 | $150 | $267 | $168 | $-98 | $469 | $-45 | $408 |
| County pop >400kb | $239* | $121 | $294* | $127 | $96 | $418 | $127 | $349 |
| Insurance co. | $716*** | $167 | $771*** | $204 | $1,068* | $530 | $416 | $337 |
| Constant | $-1,223 | $280 | $-1,362 | $312 | $-651 | $1,001 | $433 | $952 |
Outcome = total allowed expenditures in study year.
Compared to counties with population <100k.
p < 0.05; **p < 0.01; ***p < 0.001.
CAM, complementary and alternative medicine; FMS, fibromyalgia syndrome; SE, standard error.
The next set of analysis was aimed at identifying where the differences in expenditures between CAM users and nonusers occurred. Expenditures were analyzed by gender, and results showed that among males, CAM users had significantly lower expenditures than nonusers ($2,863 versus $3,634, p < 0.0001), while among females average expenditures did not differ significantly between CAM users and nonusers ($4,266 versus $4,412, p = 0.19). CAM users were less likely to be hospitalized (5.2% versus 7.5%, p < 0.001), and among those with menopause symptoms, CAM users were less likely to get a hysterectomy within 1 year of diagnosis (1.3% versus 2.9%, p < 0.001). Next we looked at the contribution of imaging to expenditures among back pain patients. CAM users were more likely than nonusers to have some type of imaging done (42.6% versus 38.3%, p < 0.001) and were also more likely to have imaging done “early” (within 28 days of diagnosis): 12.5% versus 9.8%, p < 0.001. However, overall expenditures related to imaging were higher among nonusers, averaging (standard deviation) $197 ($485) compared to $140 ($388) among CAM users (p < 0.0001). This apparently contradictory finding is explained in that CAM users are more likely than nonusers to have plain radiographs (39% versus 28%, p < 0.001), and CAM users are less likely to have the other, more expensive types of imaging such as MRIs (11.4% versus 19.4%, p < 0.001).
Because CAM users were more likely to be covered by Company B and less likely to live in urban counties than nonusers, analyses were then performed to ensure that the differences in imaging were not due to differences in coverage between companies or differences in access to imaging between rural and urban residents. There was no significant difference in the percentage of back pain patients from Company A versus Company B who had MRI or other “high tech” imaging (all imaging other than plain x-ray). Rates were 14.0% for Company A and 14.7% for Company B (p = 0.35). Looking at the issue of access to high-tech imaging in rural areas, Table 5 shows that use of high-tech imaging was substantially lower for CAM users than nonusers for all three categories of county size. Furthermore, for nonusers, rates of high-tech imaging were very similar in the smallest counties (18%) and most urban counties (19%), indicating that lack of access in more rural areas does not explain the difference between CAM users and nonusers.
Table 5.
Percent of Back Pain Patients Receiving Magnetic Resonance Imaging or Other “High-Tech” Imaging by County Population Among Complementary and Alternative Medicine (CAM) Users and Nonusers
| County population | CAM nonusers | CAM users | Total |
|---|---|---|---|
| <100k | 18% | 9% | 11% |
| 100–400k | 21 | 10 | 13 |
| >400k | 19 | 12 | 15 |
| Total | 19 | 11 | 14 |
Discussion
The results of this analysis indicated that among patients with back pain, FMS, or menopause symptoms, those who used CAM providers for at least part of their care had slightly lower overall average expenditures than matched patients who saw conventional providers exclusively. The largest difference was seen among the patients with the heaviest disease burden, who tend to be the most expensive patients. Among patients with the lightest disease burden, CAM users tended to be slightly more expensive than nonusers. The majority of patients fall into the low and moderate disease categories, so this is not an inconsequential finding. However, the size of the cost saving among those with heavy disease burdens more than compensated for this; both the unadjusted results and the regression model omitting the interaction term showed that overall, CAM users had lower mean expenditures than nonusers. In fact, given the expected $356 lower expenditure for each CAM user, we would expect an overall $9.4 million lower expenditure in a group of 26,466 CAM patients with these medical conditions compared to a similar group of CAM nonusers of equal size. CAM users actually had higher outpatient expenditures and more outpatient visits than nonusers, but this was offset by lower inpatient and other expenditures (such as high-tech imaging) among CAM users.
Both Nelson et al.28 and Legorreta29 et al. compared insured back pain patients with chiropractic insurance coverage to those without chiropractic insurance coverage and found that those with chiropractic coverage had lower average back pain episode-related costs as well as lower rates of both MR and radiographic imaging. Our findings extend these analyses in finding that among those with chiropractic insurance coverage, those who actually use this benefit have lower costs than those who do not. Our findings also confirm the findings of Sarnat30 that use of CAM-oriented primary care providers was associated with lower costs than conventional primary care providers.
This analysis has several limitations. First, although CAM users and nonusers were matched as closely as possible, the results may reflect differences between the groups that were unaccounted for in the matching process. Demographic information available in claims data is quite limited and does not include potentially important factors such as income, education, or race. Earlier regression analyses with these data used zip code–level income, education, and race to attempt to adjust for these factors, but none were significant. This likely indicates that the zip code–level aggregation was not sensitive enough to model the effects of these variables in this instance (unpublished data). Due to the correlation between health status and income, matching by disease burden provided limited matching on income.
A second limitation is that claims data are collected primarily for billing reasons and as such may not reflect all diagnosis codes with ideal accuracy. Third, cost minimization assumes that health outcomes are equivalent between groups. We did not have appropriate data available to test this assumption. Finally, we do not know how CAM-using patients would have behaved if insurance coverage was not available for these visits; if they had substituted conventional care in place of CAM care, costs to the insurance company would likely have been higher, while if they had paid out-of-pocket for CAM care, costs to the insurance company would have been lower.
Conclusions
The conclusion of this analysis is that in a large group of insured individuals, patients who use CAM providers for some of their care have lower expenditures as a group than a matched group of patients who do not use CAM, and the difference in expenditures is related in large part to less inpatient care and less use of high-tech imaging.
Acknowledgments
This work was supported by supported by R01–AT 00891 from the National Institutes of Health. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the funding agencies.
Disclosure Statement
No competing financial interests exist.
References
- 1.Eisenberg DM. Davis RB. Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: Results of a follow-up national survey. JAMA. 1998;280:1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC. Davis RB. Foster DF, et al. Long-term trends in the use of complementary and alternative medical therapies in the United States. Ann Intern Med. 2001;135:262–268. doi: 10.7326/0003-4819-135-4-200108210-00011. [DOI] [PubMed] [Google Scholar]
- 3.Pelletier KR. Astin JA. Integration and reimbursement of complementary and alternative medicine by managed care and insurance providers: 2000 update and cohort analysis. Altern Ther Health Med. 2002;8:38–39. 42, 44 passim. [PubMed] [Google Scholar]
- 4.Final Report of the White House Commission on Complementary and Alternative Medicine. 2002.
- 5.Landmark Healthcare Inc. The Landmark Report II on HMOs and Alternative Care. Sacramento, CA: Landmark Healthcare Inc.; 1999. [Google Scholar]
- 6.Herman PM CB. Caspi O. Is complementary and alternative medicine (CAM) cost-effective? A systematic review. BMC Comp Alt Med. 2005;5:11. doi: 10.1186/1472-6882-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hulme CLA. Square pegs and round holes? A review of economic evaluation in complementary and alternative medicine. J Alt Comp Med. 2005;11:179–188. doi: 10.1089/acm.2005.11.179. [DOI] [PubMed] [Google Scholar]
- 8.Astin JA. Why patients use alternative medicine: Results of a national study. JAMA. 1998;279:1548–1553. doi: 10.1001/jama.279.19.1548. [DOI] [PubMed] [Google Scholar]
- 9.Barnes PM. Powell-Griner E. McFann K. Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004;343:1–19. [PubMed] [Google Scholar]
- 10.Lind BK. Abrams C. Lafferty WE, et al. The effect of complementary and alternative medicine claims on risk adjustment. Med Care. 2006;44:1078–1084. doi: 10.1097/01.mlr.0000233695.65616.ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bausell RB. Lee WL. Berman BM. Demographic and health-related correlates to visits to complementary and alternative medical providers. Med Care. 2001;39:190–196. doi: 10.1097/00005650-200102000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Eisenberg DM. Kessler RC. Foster C, et al. Unconventional medicine in the United States: Prevalence, costs, and patterns of use. NEJM. 1993;328:246–252. doi: 10.1056/NEJM199301283280406. [DOI] [PubMed] [Google Scholar]
- 13.Ni H. Simile C. Hardy AM. Utilization of complementary and alternative medicine by United States adults: Results from the 1999 national health interview survey. Med Care. 2002;40:353–358. doi: 10.1097/00005650-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Paramore LC. Use of alternative therapies: Estimates from the 1994 Robert Wood Johnson Foundation National Access to Care Survey. J Pain Symptom Manage. 1997;13:83–89. doi: 10.1016/s0885-3924(96)00299-0. [DOI] [PubMed] [Google Scholar]
- 15.Sommer JHBM. Theiss R. A randomized experiment of the effects of including alternative medicine in the mandatory benefit package of health insurance funds in Switzerland. Comp Ther Med. 1999;7:54–61. doi: 10.1016/s0965-2299(99)80083-1. [DOI] [PubMed] [Google Scholar]
- 16.Revised Code of Washington. Olympia, WA: Washington State Law Committee; 1995. § 48.43.045. [Google Scholar]
- 17.Lafferty WE. Tyree PT. Bellas AS, et al. Insurance coverage and subsequent utilization of complementary and alternative medicine providers. Am J Manag Care. 2006;12:397–404. [PMC free article] [PubMed] [Google Scholar]
- 18.Hollinghurst SSA. Thompson EA. Capturing the value of complementary and alternative medicine: Including patient preferences in economic evaluation. Comp Ther Med. 2008;16:47–51. doi: 10.1016/j.ctim.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Tyree PT. Lind BK. Lafferty WE. Challenges of using medical insurance claims data for utilization analysis. Am J Med Qual. 2006;21:269–275. doi: 10.1177/1062860606288774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lind BK. Lafferty WE. Tyree PT, et al. The role of alternative medical providers for the outpatient treatment of insured patients with back pain. Spine. 2005;30:1454–1459. doi: 10.1097/01.brs.0000166527.18442.10. [DOI] [PubMed] [Google Scholar]
- 21.Lind BK. Lafferty WE. Tyree PT, et al. Is use of complementary and alternative medicine providers associated with lower health care costs in fibromyalgia patients? Arthritis Care Res. 2007;57:71–76. doi: 10.1002/art.22471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weiner JP. The Johns Hopkins ACG Case-Mix System. Baltimore, MD: The Johns Hopkins University Press; 2001. [Google Scholar]
- 23.National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS), vol 2: Technical Specifications. Washington, DC: NCQA; 2007. [Google Scholar]
- 24.Stata Base Reference Volume 2. College Station, TX: Stata Corp.; 2007. p. 123. [Google Scholar]
- 25.Lumley T. Diehr P. Emerson S. Chen L. The importance of the normality assumption in large public health data sets. Annu Rev Public Health. 2002;23:151–169. doi: 10.1146/annurev.publhealth.23.100901.140546. [DOI] [PubMed] [Google Scholar]
- 26.Stata User's Guide Release 10. College Station, TX: Stata Corp.; 2007. p. 268. [Google Scholar]
- 27.StataCorp 2007. Stata Statistical Software: Release 10. College Station, TX: StataCorp LP; [Google Scholar]
- 28.Nelson CF. Metz RD. LaBrot TM. Pelletier KR. The selection effects of the inclusion of a chiropractic benefit on the patient population of a managed health care organization. J Manipulative Physiol Ther. 2005;28:164–169. doi: 10.1016/j.jmpt.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 29.Legorreta AP. Metz RD. Nelson CF, et al. Comparative analysis of individuals with and without chiropractic coverage: Patient characteristics, utilization, and costs. Arch Intern Med. 2004;164:1985–1992. doi: 10.1001/archinte.164.18.1985. [DOI] [PubMed] [Google Scholar]
- 30.Sarnat RL. Winterstein J. Cambron JA. Clinical utilization and cost outcomes from an integrative medicine independent physician association: An additional 3-year update. J Manipulative Physiol Ther. 2007;30:263–269. doi: 10.1016/j.jmpt.2007.03.004. [DOI] [PubMed] [Google Scholar]