Abstract
Background
The increasing use of complementary and alternative medicine (CAM) treatment is paralleled by a growing demand for an evidence-based approach to CAM practice. In 2007, the Helfgott Research Institute at the National College of Natural Medicine (NCNM), in partnership with Oregon Health & Science University (OHSU), both in Portland, OR, began a National Institutes of Health–funded initiative to increase the quality and quantity of evidence-based medicine (EBM) content in the curricula at NCNM.
Design
One key strategy of the Research in Complementary and Alternative Medicine Program (R-CAMP) initiative was to create a faculty development program that included four components: intensive training in EBM; professional skills enhancement; peer and mentored support; and, ultimately, utilization of these skills to incorporate EBM into the curricula. This initiative is centered on a core group of faculty at NCNM, called the Vanguard Faculty, who receives early, intensive training in EBM and works to incorporate this training into classes. Training consists of an intensive, week-long course, monthly group meetings, and periodic individualized meetings. Vanguard Faculty members also receive mentorship and access to resources to pursue individualized faculty development, research or scholarly activities.
Conclusions
Early evaluations indicate that this effort has been successful in increasing EBM content in the curricula at NCNM. This article describes the Vanguard Faculty program in an effort to share the successes and challenges of implementing a wide-ranging faculty development and curricular initiative at a complementary and alternative medicine institution.
Introduction
Approximately 38% of adults in the United States use some form of complementary and alternative medicine (CAM), and there is an increasing emphasis on the need for evidence related to efficacy and safety of CAM medical treatments.1 Evidence-based medicine (EBM) is an approach widely used in allopathic medicine as a way to systematically use current best evidence in making informed decisions about the care of individual patients.2 Education in EBM concepts has been required in allopathic medical curricula for nearly a decade,3 and CAM education accreditation bodies are beginning to address EBM in their professional competencies.4 Overall, however, the level of research and EBM skills training varies widely among CAM educational institutions,5 and, until only recently, there have not been formal research training avenues for CAM practitioners and students.6 In addition, a 2008 survey showed that CAM practitioners were less likely than conventional practitioners to feel confident interpreting research literature.7
In 1999, the National Center for Complementary and Alternative Medicine (NCCAM) at the National Institutes of Health (NIH) created a grant program to encourage the integration of CAM topics into the curriculum at allopathic health professions schools.8 A few years later, NCCAM issued research education enhancement grants targeted at CAM educational institutions.9 The Helfgott Research Institute at National College of Natural Medicine (NCNM), Portland, OR—an accredited education institution that offers a doctoral program in naturopathic medicine and two master's-level programs in classical Chinese medicine—is one of eight institutions supported by this second wave of grants. The goal of these grants is to increase the quality and quantity of research content in institutions that train CAM physicians and practitioners.5 Increasing CAM providers' knowledge of research and EBM can not only help improve CAM practice7 and facilitate better communication between allopathic and CAM health professionals,10,11 but also inspire more CAM professionals to pursue careers in research.12 In 2007, the NCNM initiated the Research in Complementary and Alternative Medicine Program, or R-CAMP, in partnership with Oregon Health & Science University (OHSU), Portland, OR. The R-CAMP program is one of a number of efforts in CAM educational institutions to include research and EBM concepts in curricula6,9,13,14 and teach EBM to CAM practitioners.15
The goals of R-CAMP are to increase EBM skills of faculty and students, strengthen the evidence-informed perspective of the curricula, and create an academic culture supportive of research at NCNM. A key element of this program is encouraging open dialogue about the benefits and limitations of EBM within CAM practice and supporting discussion about how best to incorporate and adapt these concepts to natural medicine. R-CAMP initiatives are integrated into the institutional structure at the NCNM, with deans, the provost, and other administrators planning, implementing, and participating in R-CAMP activities to ensure sustainability. R-CAMP is overseen by an executive committee and advisory board whose members include NCNM faculty, administrators and staff, OHSU collaborators, and education experts.
As medical educators, the R-CAMP leadership team members wanted to find strategies to facilitate the success of the program. A key strategy, modeled after other faculty scholar efforts,13,16,17 was to bring together a core team of faculty members who would lead, champion, and model incorporation of research literacy at NCNM. The goals of this team, called the Vanguard Faculty, are to build capacity and peer-to-peer facilitation for learning and teaching EBM concepts, create faculty ownership of the R-CAMP initiative, enhance NCNM faculty professional skills, and develop resources and support for the faculty's EBM work.
This article describes the four components of the Vanguard Faculty program, illustrates challenges and lessons learned, and discusses future directions for this initiative, in an effort to share the experience of implementing an institution-wide, EBM-focused faculty development and curricular initiative at a CAM institution.
The Vanguard Faculty Program
The Vanguard Faculty program is designed to target EBM skills training to faculty members, so they will then be equipped to restructure their curricula and pass this knowledge on to both NCNM students and other faculty members. Each year, 5–7 NCNM faculty members are identified and invited to be part of the Vanguard Faculty team. Potential Vanguard Faculty members are nominated by the Dean of Research, the Dean of the School of Naturopathic Medicine, and the Dean of the School of Classical Chinese Medicine. In addition, interested faculty members can self-select for this program. As of the third year of R-CAMP, 19 NCNM faculty members had joined the Vanguard Faculty (Table 1). The R-CAMP leadership team identifies individuals who would be early adopters and peer role models, and targets institutional and educational decision-makers, such as deans and department chairs. NCNM librarians are also included, as they are key to facilitating ongoing support for faculty regarding EBM resources and literature-searching techniques.18
Table 1.
Vanguard Faculty Demographics
| Department | ND | CCM | Both | Librarian |
|---|---|---|---|---|
| 11 | 5 | 1 | 2 | |
| Total NCNM faculty | 67 | 32 | 4 | 4 |
| Gender | Male | Female |
|---|---|---|
| 8 | 11 |
| Cohort | 2007 | 2008 | 2009 |
|---|---|---|---|
| 5 | 7 | 7 |
CCM, classical Chinese medicine; NCNM, National College of Naturopathic Medicine (Portland, OR).
An important outcome of the R-CAMP program is increased EBM in the curriculum at NCNM. The curriculum at NCNM is quite full, with many competing priorities and little room for extra classes. That being the case, a key R-CAMP strategy is to have faculty members work EBM content into existing classes, through assignments, lectures, and in-class activities. Time and resources prohibit training every faculty member at NCNM in EBM and EBM teaching methods, so R-CAMP administrators adopted a “train-the-trainers”19 approach to this initiative by developing the Vanguard Faculty team.
Components of the Vanguard Faculty Program (Structure)
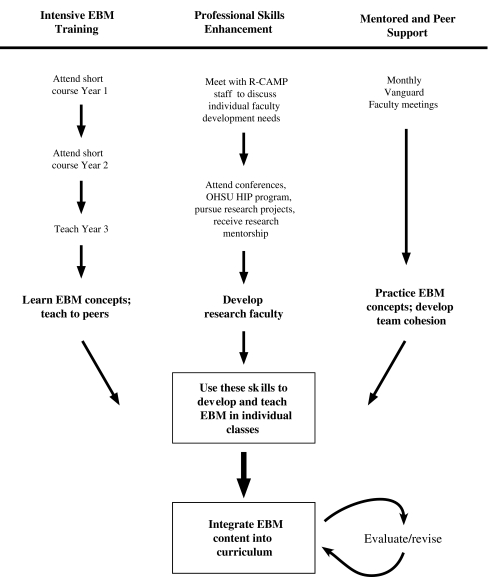
The Vanguard Faculty initiative has four components: (1) intensive training in EBM (2) professional skills enhancement: (3) peer and mentored support, and, ultimately, (4) utilization of these skills to incorporate EBM into the curriculum (Fig. 1). As the program evolves, a broader vision is to have Vanguard Faculty take leadership and development roles regarding EBM and the culture of research at NCNM, and increasingly incorporate these activities into the institutional fabric. The following is a detailed description of each of the Vanguard Faculty initiative's components.
FIG. 1.
Vanguard faculty process and goals. EBM, evidence-based medicine; R-CAMP, Research in Complementary and Alternative Medicine Program; OSHU, Oregon Health & Science University (Portland, OR); HIP, Human Investigations Program.
1. Intensive EBM training
The first activity for each new Vanguard Faculty member is to participate in Principles of Evidence-Based Medicine, R-CAMP's intensive summer short course. This 20-hour course teaches participants how to access and appraise biomedical literature, how to apply it to their work, and how to teach these concepts to their students (See Table 2 for a full list of course learning objectives). The purpose of the short course is to provide a short-term, intensive introduction to EBM concepts for NCNM faculty members, and encourage them to begin to think about how they can incorporate these concepts into their curricula.
Table 2.
Principles of EBM Learning Objectives
| General |
| • Define the role of evidence in making clinical decisions. |
| • Identify unique issues related to use of EBM in a CAM practice. |
| Framing questions |
| • Formulate clinical questions using a framework that facilitates finding answers. |
| Resources |
| • Understand how the type of clinical questions influences choice of resources. |
| • Become familiar with evidence-based resources including CAM-specific resources and understand the strengths and limitations of each. |
| • Categorize resources into four levels: studies; syntheses; synopses; and summaries. |
| • Navigate one resource from each level of evidence. |
| Validity assessment |
| • Critically appraise the validity of an article about therapy and interpret the results. |
| • Critically appraise the validity of a systematic review and interpret the results. |
| • Critically appraise the validity of a practice guideline and interpret the results. |
| Application |
| • Apply the evidence to decision making for individual patients. |
| Using and teaching EBM |
| • Identify opportunities to incorporate EBM into their own practices. |
| • Identify opportunities to role model use of EBM techniques. |
| • Identify opportunities and venues to teach EBM content. |
EBM, evidence-based medicine; CAM, complementary and alternative medicine.
A multidisciplinary team was assembled to create the course content, consisting of 2 NCNM faculty members with expertise in CAM research and clinical practice and two OHSU faculty members with expertise in EBM education and research methodology. This group also obtained guidance from the Society of General Internal Medicine (SGIM) EBM Taskforce. The short course addresses the following topics, covering how to: formulate research questions; find appropriate resources; appraise therapy and systematic reviews; and apply these concepts in the classroom and clinic. The course is team-taught, with instructors from the NCNM, OHSU, and the Portland Veterans Administration Medical Center. After practicing how to appraise articles from both CAM and non-CAM peer-reviewed journals during the course, participants form groups and lead their peers in an article appraisal exercise on the last day of the course. In addition, the library staff members at NCNM are not only course participants, but also lead course sessions in EBM resources, searching tips, and database and summary website comparisons.
The structure of this course was specifically designed to address potential challenges, such as limited faculty time and varied levels of EBM acceptance.20 The course takes place for a week in the summer, when the faculty teaching load is lessened, and is held in the mornings so that participants can still attend clinic shifts in the afternoon. Each cohort of Vanguard Faculty takes this course twice (once per summer for 2 years), which allows them to revisit the material and gain a deeper understanding of the concepts. Blending previous and new cohorts allows the more experienced cohort members to assist and mentor the newer ones. We also encourage Vanguard Faculty members who have taken the course twice to teach a section of the course the following year. As more faculty members become comfortable with instructing their peers in EBM concepts, there will be a bigger cadre of EBM-trained teachers to sustain these trainings. Finally, to engage the participants and address various philosophical perspectives about the applicability of EBM concepts to CAM,21,22 course instructors specifically choose articles that are of interest to CAM practitioners and allot time in class to discuss participants' understanding about the applications and limitations of EBM in CAM. In addition, course organizers and instructors emphasize that biomedical literature is only one form of evidence and that there are other “ways of knowing”—such as ancient texts, advice from CAM colleagues, and intuition—that can comprise the “evidence” in evidence-based medicine.13,23
Results from pre- and postcourse evaluations suggest that, overall, there were significant changes in EBM practice attitudes, self-appraised skills, and objectively assessed skills as a result of the short course.
2. Professional skills enhancement
Vanguard Faculty members are also encouraged to enhance their professional skills. Upon entering the program, each Vanguard Faculty member meets with R-CAMP staff members to set objectives for curriculum enhancements and establish personal professional goals. R-CAMP's academic leadership team helps facilitate both of these objectives. Most CAM educators were educated in a pre-EBM era and lack familiarity or expertise in research skills and EBM. The scarcity of clinical researchers at natural medicine colleges further limits exposure of teaching faculty to research and opportunities for participation. Thus, faculty development, empowerment, and support are all critical for a successful curriculum revision initiative.
Professional goals among the Vanguard Faculty vary, so this program allows for maximum flexibility according to the individual career objectives of each faculty member. Some faculty members may simply want to attend a yearly professional conference, while others would like to pursue research projects or apply for grant funding for studies. The partnership with OHSU allows R-CAMP to offer Vanguard Faculty the chance to take part in a Human Investigations Program (HIP) certificate track or obtain a Master of Clinical Research (MCR) degree.
To date, Vanguard Faculty members have attended multiple research conferences, attended lectures by external researchers, and pursued a variety of career development activities. In addition, several Vanguard Faculty members have become clinical investigators by partnering with Helfgott Research Institute staff on existing research projects.
3. Mentored and peer support
Early on, R-CAMP staff recognized the need for ongoing support in the Vanguard Faculty process. In order to provide both peer and mentored support to the Vanguard Faculty, there are evening dinner meetings held each month during the academic year. The purpose of these meetings is to reinforce what Vanguard Faculty members learned in the short course and provide a venue for them to share EBM teaching strategies and information about individual projects. In addition to building EBM skills, these meetings encourage peer interaction, build community, and help foster group cohesion. This facilitated group mentoring process has been shown to be a promising alternative to the conventional dyadic, or one-on-one, mentoring model.24
The meeting topics vary from month to month and are established by R-CAMP staff members, with Vanguard Faculty input. A few times a year, guest speakers are invited to lead a meeting, to allow Vanguard Faculty members to network and hear about current CAM-related research. Other meetings are focused on EBM teaching techniques or Vanguard Faculty members' individual research projects. During the third year of the grant, faculty will lead journal clubs during some of these meetings so the Vanguard Faculty members can practice literature appraisal skills in a group environment. Currently, these meetings are held solely for Vanguard Faculty members, but non–Vanguard Faculty members may attend if they choose.
These regular meetings have contributed successfully to Vanguard Faculty group cohesion. There are not many opportunities for faculty members at the NCNM to gather and discuss their work, and these meetings have allowed them to do so. Many Vanguard Faculty members have begun to get together outside of these meetings to help each other revise curricula, or work on joint projects. As the dinner meetings are not mandatory, R-CAMP staff periodically meets individually with Vanguard faculty members to discuss their projects, curriculum revision, and faculty development needs.
4. Incorporating EBM into the curriculum
A major goal of the R-CAMP initiative is to incorporate evidence-based medicine content into the curricula at NCNM. Curriculum revision at NCNM is an ongoing process and faculty members are continually revising and improving the courses they teach. Integration of concepts and skills throughout the medical experience is essential for students to internalize them,25,26 and Vanguard Faculty members are part of the strategy for integrating EBM skills throughout the curricula at NCNM. At the College, the faculty is in charge of both the naturopathic and Chinese medicine curricula. As the Vanguard Faculty is trained in EBM and EBM teaching techniques, Vanguard Faculty members simultaneously work to include these concepts into classes they teach as they do their routine curriculum revising. During the first 2 years of the grant, Vanguard Faculty members have used a range of different strategies to incorporate EBM in their courses. These have included assigning EBM-related homework assignments, adding citations to lectures and class handouts, including EBM concepts in lectures, and modeling literature searching during clinic shifts. The NCNM is undergoing a parallel effort to restructure the curricula at the school, working with one department at a time. To date, R-CAMP administrators have been successful in recruiting faculty from the restructuring departments to the Vanguard Faculty team, so that EBM concepts are an integral part of the curricula reworking. In addition, 2 of the 3 members of NCNM's curriculum review committee are Vanguard Faculty members, which allows them to incorporate R-CAMP goals successfully into the larger institutional structure.
Challenges
R-CAMP leadership structured this program to address proactively several key challenges and issues: the lack of faculty time; the large number of adjunct faculty members at the NCNM; and the paucity of published biomedical literature in CAM therapies.27
First, as in many medical institutions,28 faculty members have full teaching and clinic loads and are pressed for time. Two (2) potential members turned down the offer to participate because they had an already-full schedules, and many other potential members have limited time to devote to extra activities. One strategy for dealing with this challenge is to recruit faculty leaders who are eager to pursue faculty development opportunities and who see participation in the Vanguard Faculty as a chance to grow professionally. Research suggests that achievement motivation is an important indicator of leaders versus nonleaders in an academic setting.29 Another strategy has been to make the Vanguard Faculty requirements as flexible as possible. Vanguard Faculty members are free to incorporate EBM concepts into work however these members see fit and to do so to the degree that they feel comfortable. For example, some faculty members incorporated the material into one lesson or activity, while others have worked it into almost all of their courses. Finally, creating evening meeting times and providing dinner has been one successful way to work around the lack of a common meeting time during the day.
Another challenge is the high number of adjunct faculty at the NCNM. Seventy-five percent (75%) of the faculty members at the NCNM are adjunct, meaning that they are primarily clinicians who teach part-time, either in a classroom or clinic setting. Adjunct faculty members are rarely on campus, making it difficult to reach them for training sessions or foster peer-to-peer education. Previous research established that there is significantly less institutional support offered to adjunct faculty members, compared to full-time faculty members.30 In addition, any more time spent on NCNM tasks outside of their contracted teaching duties often cuts into the adjuncts' private clinic shifts and leads to lost revenue. One way to work around these issues has been to invite a few highly interested, self-motivated adjunct faculty members to become Vanguard Faculty members and pay them a stipend to take the short course. Full-time faculty members receive compensation through faculty contracts. In addition, all new adjunct faculty members will be required to view a training DVD that includes a lecture on how to practice and teach EBM.
The third challenge has been the lack of published biomedical literature on naturopathic and Chinese medicine therapies. Vanguard Faculty members have acknowledged the challenge posed by teaching EBM in a field where formally published evidence is scanty. To overcome this problem, R-CAMP administrators have adopted two strategies. First, despite the philosophical differences between allopathic and naturopathic medicine, there are many overlapping therapies and diagnostic techniques. Focusing on areas that do have ample evidence bases, such as nutrition and diagnosis, allows faculty members, and in turn, students, to practice EBM skills in areas that are clinically relevant to them. Second, R-CAMP administrators have advocated using EBM to encourage critical thinking in the classroom and clinic and have encouraged the Vanguard Faculty members to take this approach.26 Even if naturopathic and Chinese medicine therapies are not well-represented in the literature, EBM skills can help students and clinicians assess treatment options rationally and methodically, and assist these practitioners in providing the best possible care to their patients.
Future Plans
There are plans to expand the Vanguard Faculty program in the future. New Vanguard Faculty members will be added to the program until all interested full-time faculty members and 25% of adjunct faculty members are included. In addition, R-CAMP administrators are currently developing a second, more advanced short course for faculty members who are interested in pursuing clinical research. This course will also eventually be available to students. As the Vanguard Faculty program adds more people each year, there will be a greater need for more mentors to provide guidance for faculty who pursue individual faculty development projects. R-CAMP administrators are actively pursuing ways to offer more training and mentorship to Vanguard Faculty members, including a potential faculty exchange program with OHSU. Finally, it is crucial to the sustainability of the R-CAMP initiatives to offer similar training to non–Vanguard NCNM faculty members. There are efforts underway to utilize Vanguard Faculty members to teach research literacy and EBM concepts to their peers in informal lectures, periodic training sessions, and workshops at national professional conferences.
Acknowledgments
This work is supported by education grant 1R25 AT002878-01A1 from the National Institutes of Health/National Center for Complementary and Alternative Medicine (NIH/NCCAM). Many thanks to Elizabeth Allen, MD, for her work in developing and instructing the Principles of Evidence-Based Medicine course, and to Kristen Wessel, PhD, and Susan Fleishman, BA, for their invaluable expertise and input. In addition, this project would not be as successful without the dedication and hard work of the members of NCNM's Vanguard Faculty.
Disclosure Statement
No competing financial interests exist.
References
- 1.Barnes PM. Bloom B. Nahin R. Atlanta, GA: Centers for Disease Control and Prevention; 2008. Complementary and alternative medicine use among adults and children: United States, 2007. In: CDC National Health Statistics Report #12. [PubMed] [Google Scholar]
- 2.Sackett DL. Rosenberg WM. Gray JA, et al. Evidence based medicine: What it is and what it isn't. BMJ. 1996;312:71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Association of American Medical Colleges (AAMC) Washington, DC: AAMC; 2001. Report IV: Contemporary Issues in Medicine. Basic Science and Clinical Research. [Google Scholar]
- 4.Association of Accredited Naturopathic Medical Colleges (AANMC) Naturopathic Medical Colleges Professional Competency Profile. Washington, DC: AANMC; 2007. [Google Scholar]
- 5.CAM Practitioner Research Education Project Grant Partnership (PAR-04-097) NIH Guide to Grants and Contracts. http://grants.nih.gov/grants/guide/pa-files/PAR-04-097. [Oct 5;2009 ]. http://grants.nih.gov/grants/guide/pa-files/PAR-04-097
- 6.Wayne PM. Buring JE. Davis RB. Increasing research capacity at the New England School of Acupuncture through faculty and student research training initiatives. Altern Ther Health Med. 2008;14:52–58. [PubMed] [Google Scholar]
- 7.Tilburt JC. Curlin FA. Kaptchuk TJ, et al. Alternative medicine research in clinical practice: A US national survey. Arch Intern Med. 2009;169:670–677. doi: 10.1001/archinternmed.2009.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pearson NJ. Chesney MA. The CAM Education Program of the National Center for Complementary and Alternative Medicine: An overview. Acad Med. 2007;82:921–926. doi: 10.1097/ACM.0b013e31814a5014. [DOI] [PubMed] [Google Scholar]
- 9.Kreitzer MJ. Sierpina VS. NCCAM awards grants to CAM institutions to enhance research education. Explore (N Y) 2008;4:74–76. doi: 10.1016/j.explore.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 10.Gaylord SA. Mann JD. Rationales for CAM education in health professions training programs. Acad Med. 2007;82:927–933. doi: 10.1097/ACM.0b013e31814a5b43. [DOI] [PubMed] [Google Scholar]
- 11.Perlman AI. Eisenberg DM. Panush RS. Talking with patients about alternative and complementary medicine. Rheum Dis Clin North Am. 1999;25:815–822. doi: 10.1016/s0889-857x(05)70102-2. [DOI] [PubMed] [Google Scholar]
- 12.Jobst KA. Becoming and growing—what does integration mean? J Altern Complement Med. 2009;15(4):v–vi. doi: 10.1089/acm.2009.0231. [DOI] [PubMed] [Google Scholar]
- 13.Hammerschlag R. Lasater K. Salanti S. Fleishman S. Research scholars program: A faculty development initiative at the Oregon College of Oriental Medicine. J Altern Complement Med. 2008;14:437–443. doi: 10.1089/acm.2007.0813. [DOI] [PubMed] [Google Scholar]
- 14.Lasater K. Salanti S. Fleishman S, et al. Learning activities to enhance research literacy in a CAM college curriculum. Altern Ther Health Med. 2009;15:46–54. [PubMed] [Google Scholar]
- 15.Zick SM. Benn R. Bridging CAM practice and research: Teaching CAM practitioners about research methodology. Altern Ther Health Med. 2004;10:50–56. [PubMed] [Google Scholar]
- 16.Lee MY. Benn R. Wimsatt L, et al. Integrating complementary and alternative medicine instruction into health professions education: Organizational and instructional strategies. Acad Med. 2007;82:939–945. doi: 10.1097/ACM.0b013e318149ebf8. [DOI] [PubMed] [Google Scholar]
- 17.Sierpina V. Kreitzer MJ. Benn R. Warber S. Innovations in integrative healthcare education: Faculty development and the Faculty Scholars Program. Explore (N Y) 2006;2:172–174. doi: 10.1016/j.explore.2005.12.015. [DOI] [PubMed] [Google Scholar]
- 18.Isbell D. What happens to your research assignment at the library? Coll Teach. 2008;56:3–6. [Google Scholar]
- 19.Green ML. A train-the-trainer model for integrating evidence-based medicine training into podiatric medical education. J Am Podiatr Med Assoc. 2005;95:497–504. doi: 10.7547/0950497. [DOI] [PubMed] [Google Scholar]
- 20.Bradt P. Moyer V. How to teach evidence-based medicine. Clin Perinatol. 2003;30:419–433. doi: 10.1016/s0095-5108(03)00019-8. [DOI] [PubMed] [Google Scholar]
- 21.Boon H. Canadian naturopathic practitioners: Holistic and scientific world views. Soc Sci Med. 1998;46:1213–1225. doi: 10.1016/s0277-9536(97)10050-8. [DOI] [PubMed] [Google Scholar]
- 22.Mills EJ. Hollyer T. Guyatt G, et al. Evidence-Based Complementary and Alternative Medicine Working Group. Teaching evidence-based complementary and alternative medicine: 1. A learning structure for clinical decision changes. J Altern Complement Med. 2002;8:207–214. doi: 10.1089/107555302317371514. [DOI] [PubMed] [Google Scholar]
- 23.Kreitzer MJ. Sierpina V. Maiers M, et al. Ways of knowing: Integrating research into CAM education and holism into conventional health professional education. Explore (N Y) 2008;4:278–281. doi: 10.1016/j.explore.2008.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pololi L. Knight S. Mentoring faculty in academic medicine: A new paradigm? J Gen Intern Med. 2005;20:866–870. doi: 10.1111/j.1525-1497.2005.05007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mills E. Hollyer T. Saranchuk R. Wilson K. Teaching evidence-based complementary and alternative medicine (EBCAM); changing behaviours in the face of reticence: A cross-over trial. BMC Med Educ. 2002;2:2. doi: 10.1186/1472-6920-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vickers A. A proposal for teaching critical thinking to students and practitioners of complementary medicine. Altern Ther Health Med. 1997;3:57–62. [PubMed] [Google Scholar]
- 27.Marcus DM. McCullough L. An evaluation of the evidence in “evidence-based” integrative medicine programs. Acad Med. 2009;84:1229–1234. doi: 10.1097/ACM.0b013e3181b185f4. [DOI] [PubMed] [Google Scholar]
- 28.Trowbridge RAPB. A successful approach to faculty development at an independent academic medical center. Med Teach. 2008;30:e10–e14. [Google Scholar]
- 29.Rogers J. Aspiring to leadership—identifying teacher–leaders. Med Teach. 2005;27:629–633. doi: 10.1080/01421590500156228. [DOI] [PubMed] [Google Scholar]
- 30.Landrum R. Are there instructional differences between full-time and part-time faculty? Coll Teach. 2008;57:23–26. [Google Scholar]