Abstract
Background
Traditional Chinese Medicine (TCM) is popular for treatment of fibromyalgia (FM) although there is a lack of comprehensive evaluation of current clinical evidence for TCM's therapeutic effect and safety.
Objective
To review systematically the beneficial and harmful effects of TCM therapies for FM.
Methods
We searched six English and Chinese electronic databases for randomized clinical trials (RCTs) on TCM for treatment of FM. Two authors extracted data and assessed the trial quality independently. RevMan 5 software was used for data analyses with an effect estimate presented as mean difference (MD) with a 95% confidence interval (CI).
Results
Twenty-five RCTs were identified with 1516 participants for this review. Seven trials (28%) were evaluated as having a low risk of bias and the remaining trials were identified as being as unclear or having a high risk of bias. Overall, ten trials were eligible for the meta-analysis, and data from remaining 15 trials were synthesized qualitatively. Acupuncture reduced the number of tender points (MD, –3.21; 95% CI –4.23 to –2.11; p < 0.00001, I2 = 0%), and pain scores compared with conventional medications (MD, –1.78; 95% CI, –2.24 to –1.32; p < 0.00001; I2 = 0%). Acupuncture showed no significant effect, with a random-effect model, compared with sham acupuncture (MD, –0.55; 95% CI, –1.35–0.24; p = 0.17; I2 = 69%), on pain reduction. A combination of acupuncture and cupping therapy was better than conventional medications for reducing pain (MD, –1.66; 95% CI, –2.14 to –1.19; p < 0.00001; I2 = 0%), and for improving depression scores with related to FM (MD, –4.92; 95% CI, –6.49 to –3.34; p < 0.00001; I2 = 32%). Other individual trials demonstrated positive effects of Chinese herbal medicine on pain reduction compared with conventional medications. There were no serious adverse effects reported that were related to TCM therapies in these trials.
Conclusions
TCM therapies appear to be effective for treating FM. However, further large, rigorously designed trials are warranted because of insufficient methodological rigor in the included trials.
Introduction
Fibromyalgia (FM) is nonspecific rheumatism in which typical symptoms are chronic widespread musculoskeletal pain and stiffness with accompanying fatigue, anxiety, sleep disorder; and/or irritable bowel syndrome.1 Experts in the United States and Canada have developed diagnostic criteria for identifying this disease for the American College of Rheumatology (ACR),2 which are also commonly used in China. This disease appears to affect increasing numbers of people, with a disabling outcome on their quality of life (QoL).3
As the cause of FM is unknown, it is characterized and diagnosed by its symptoms of chronic widespread pain and multiple tender points associated to some degree of facilitation by the central nervous system.4 There are two important goals for treating these symptoms.4 The first goal is reduction of pain, and the second goal is restoring functionality. Many peer-reviewed articles about the treatment of FM have been published involving different pharmacologic agents including nonsteroidal anti-inflammatory drugs (NSAIDs), opioid and nonopioid analgesics, anticonvulsants, antidepressants, α-adrenergic agonists, muscle relaxants, topical agents, local anesthetics, N-methyl-d-aspartate (NMDA) receptor antagonists, and botulinum toxin. None of these medications have proven to be effective for the entire scope of symptoms and disabilities associated with FM.4 One recent systematic review5 concluded that antidepressants are associated with improvements in pain, depression, fatigue, sleep disturbances, and health-related QoL in people with FM, with large effect sizes for tricyclic and tetracyclic antidepressants (TCAs; standard mean difference [SMD] = –1.64; 95% confidence interval [CI], –2.57 to –0.71). Uceyler et al.6 came to similar conclusions about amitriptyline. Tofferi et al.7 suggested that cyclobenzaprine offered some benefit to patients with FM, with 1 of 5 patients experiencing improvements, while Moore et al.8 showed that pregabalin had proven efficacy for relieving neuropathic pain and FM, although many patients experienced trivial benefit or discontinued treatment because of adverse effects.
Antidepressants have been shown to have some effect, whereas NSAIDs, steroids, and calcitonin have not. Cyclobenzaprine, alprazolam, tramadol, and SAM-e have shown some benefit to patients in small studies.7 Many medications produce significant sedation and physical dependence as well as causing psychologic dependence.4
A systematic review9 of randomized clinical trials (RCTs) of nonpharmacologic interventions concluded that, although significant differences between groups occurred, the varying combinations of intervention in the studies studies and the wide range of outcome measures used made it hard to form clear conclusions across studies. The interventions included education, relaxation therapy, cognitive–behavioral therapy, acupuncture, and hydrotherapy, and there was some preliminary support for aerobic exercise.
In Traditional Chinese Medicine (TCM) theory, FM is mainly caused by emotional upsets, which affect the Liver. Stagnation of qi activity leads to the stasis of Blood, which causes pain. The principle of treatment is regulating the qi and Blood, combined with dispelling Cold and removing Damp.10 TCM is a whole system that uses a range of therapies to treat FM; these include acupuncture, moxibustion, herbal medicine, and massage. Two systematic reviews have suggested that acupuncture alone is effective for treating FM; one analysis involved three RCTs and four cohort studies and the other analysis included three positive RCTs and two negative RCTs.11,12 No systematic review reported the effect of herbal medicine or other TCM therapies for FM, but a review published in 200513 suggested that “many of the herbs and other dietary supplements used by our patients are known to have potential adverse effects and may pose a risk to the patient.” This current systematic review aims to update the evidence from RCTs to evaluate the therapeutic effect and safety of TCM, including Chinese herbal medicine for FM.
Methods
Inclusion Criteria
We included parallel-group RCTs of any kind of TCM treatment, including acupuncture, herbal medicine, massage, and/or cupping compared with no treatment, placebo, and/or conventional medication in patients with FM. We also included combined therapy with TCM and other interventions compared with other interventions in RCTs, or combined therapy of two kinds of TCM compared with medication or other interventions. FM was diagnosed according to recognized criteria. Outcome measures included reduction in severity of pain or depression, improvement of QoL, and reduction of relapse rate. When multiple publications reported the same groups of participants, we only included the primary publication and excluded the duplicated publications. There was no limitation on language and publication type.
Identification and selection of studies
We searched the China Network Knowledge Infrastructure (CNKI; 1979–2009), Chinese Scientific Journal Database VIP (1989–2009), Wan Fang Database (1985–2009), Chinese Biomedicine (CBM) database (1978–2009), PubMed (1966–2009) and Cochrane Library (Issue 3, 2009). All searches ended at August 2009. The search terms included fibromyalgia, fibrosis, fibrositis, myofascitis, ormyofibrositis, combined with traditional Chinese medicine, TCM, herbal, acupuncture, massage, cupping, or Tui Na. Two authors (Cao H and Liu JP) selected studies for eligibility and checked against the inclusion criteria independently.
Data extraction and quality assessment
Two authors (Cao H and Liu JP) extracted the data from the included trials independently. The methodological quality for RCTs was assessed, using criteria from the Cochrane Handbook for Systematic Reviews of Interventions, Version 5.0.1.14 The quality of trials was categorized into low risk of bias, unclear risk of bias, or high risk of bias according to the risk for each important outcome within included trials, including adequacy of generation of the allocation sequence, allocation concealment, blinding, whether there were incomplete outcome data (“Describe the completeness of outcome data for each main outcome, including attrition and exclusions from the analysis. State whether attrition and exclusions were reported, the numbers in each intervention group [compared with total randomized participants], reasons for attrition/exclusions where reported, and any reinclusions in analyses performed by the review authors”),14 or selective outcome, or other sources of bias.
Data analysis
Data were summarized using risk ratio (RR) with 95% CIs for binary outcomes or mean difference (MD) with a 95% CI for continuous outcomes. We used Revman 5.0.2 software from the Cochrane Collaboration for data analyses. Meta-analysis was used if the trials had acceptable homogeneity of study design, participants, interventions, controls, and outcome measures. Statistical heterogeneity was tested by examining I2square15 or p-value; an I2 > 50% or a p-value < 0.1 indicates the possibility of statistical heterogeneity. Both a fixed-effect model and a random-effects model were used if there was a possibility of statistical heterogeneity among the trials. If the I2 was <50%, or the p-value was >0.1, only a fixed-effect model was used for meta-analysis. Publication bias was explored via a funnel-plot analysis.
Results
Description of studies
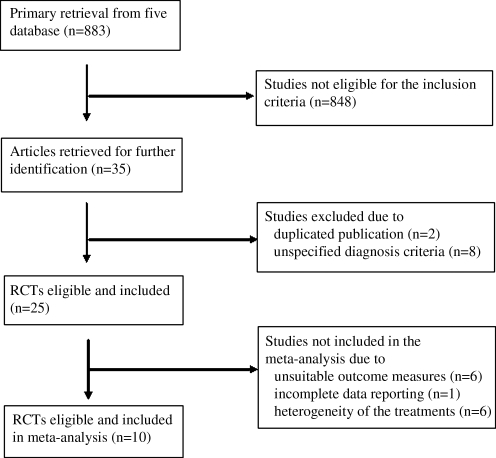
After primary searches in six databases, 883 citations were identified. The majority was excluded because of obvious ineligibility, and full-text papers of 35 studies were retrieved. Finally, 2516–38 randomized trials were included in this review, two trials39,40 were excluded as duplicated publications, and eight trials41–48 were excluded because the diagnosis criteria were not specified (Fig. 1). The characteristics of included trials are listed in Table 1. Of the included trials, two were unpublished postgraduate student dissertations.*,†
FIG. 1.
Study enrollment process. RCTs, randomized controlled trials.
Table 1.
Characteristics of Included Studies
| Lead author, year, & Ref. # | Diagnostic criteria | Sample Size (Rx/C) | Age (yr, Rx/C) | Duration of disease (m, Rx/C) | Experimental intervention | Control intervention | Duration of treatments | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Assefi NP 200516 | ACR 1990 | 25/24 | 46 ± 11/49 ± 14 | 72/84 | Acupuncture, 2X/week | Sham acupuncture (false acupoints) 2X/week | 12 weeks | VAS, SF-36 |
| 25/23 | 46 ± 11/48 ± 10 | 72/84 | Sham acupuncture (not insertion) 2X week | |||||
| Brattberg G 199917 | ACR 1990 | 11/12 | 48 ± 12.4 | Unclear | Connective tissue massage 15X during 10 weeks | No treatment | 10 weeks | VAS, DRI, HAD, FIQ, QoLS, mean value for 10 questions about sleep |
| 16/13 | Connective tissue massage 15X during 10 weeks | Discussion 1X/week | ||||||
| Cao JY 200318 | ACR 1990 | 28/28 | 42.1 ± 14.5 | 19.3 ± 15.1 | Acupuncture + cupping therapy 3X/day, seroxat, 20 mg/day | Seroxat, 20 mg/day | 4 weeks | HAMD, VAS, number of tender points |
| Deluze C 199219 | ACR 1990 | 36/34 | 46.8 ± 2.3/49 ± 2 | 172.8 ± 40.8/82.8 ± 15.6 | Electroacupuncture 1X/day for 6 sessions | Sham electroacupuncture (false acupoints) 1X/day for 6 sessions | 3 weeks | VAS, Sleep Quality |
| Fu HW 200620 | ACR 1990 | 21/21 | 36.2 ± 7.82/35.92 ± 10.28 | 7–36 | Herbal medicine, (decoction) 200 mL 2X/day | Amitriptyline hydrochloride, 25–50 mg/night | 12 weeks | HAMA, HAMD, scores for reduction of symptoms |
| Fu XY 2004a | ACR 1990 | 33/33 | 39.16/39.1 | Unclear | Acupuncture 30 min, 1X/daiy + cupping therapy 5 min, 1X every 2 days | Amitriptyline, 25mg 2X/day | 2 weeks | MPQ, PPI, HAMD |
| Gao GM 200721 | ACR 1990 | 30/28 | 32 ± 13/31 ± 12 | 2.5 ± 1.9/2.3 ± 1.8 | Flavone of Rhizoma Drynariae, 0.25 g 3X/day | Meloxicam, 7.5mg 1X/day | 12 weeks | FIQ, Zung Self-rating Depression Scale, Scores of Index of Pain |
| 30/29 | 32 ± 13/ 33 ± 14 | 2.5 ± 1.9/2.4 ± 1.6 | Flavone of Rhizoma Drynariae, 0.25g 3 X/day | Meloxicam, 7.5 mg + amitriptyline 12.5–50mg 1X/day | ||||
| 28/29 | 30 ± 11/33 ± 14 | 2.3 ± 2.1/2.4 ± 1.6 | Flavone of Rhizoma Drynariae, 0.25 g 3X/day + amitriptyline, 12.5—50 mg 1X/day | Meloxicam, 7.5 mg + amitriptyline, 12.5–50 mg 1X/day | ||||
| 27/29 | 32 ± 10/33 ± 14 | 2.4 ± 1.9/2.4 ± 1.6 | Flavone of Rhizoma Drynariae, 0.25g 3X/day, meloxicam, 7.5 mg + amitriptyline, 12.5–50 mg 1 X/day | Meloxicam, 7.5mg + amitriptyline 12.5–50 mg 1X/day | ||||
| Guo XJ 200322 | ACR 1990 | 22/22 | 50 ± 3.1/51 ± 1.9 | 10 ± 3.6/ 11 ± 1.9 | TENSc 30 min 1X/day | Oryzanol, 30 mg, vitamin B1, 30 mg 3X/day + amitriptyline, 10–30 mg/night | 45 days | Reduction of symptoms, effectiveness rate |
| 22/22 | 49 ± 6.7/51 ± 1.9 | 11 ± 2.4/ 11 ± 1.9 | Electroacupuncture,c 30 min 1 X/day | Oryzanol, 30 mg, vitamin B1, 30 mg 3 X/day + amitriptyline, 10–30 mg/night | ||||
| Guo Y 200523 | ACR 1990 | 19/19 | 50 ± 2.9/ 49 ± 3.4 | 11 ± 2.3/10 ± 3.6 | Acupuncture 30 min 1X/day | Amitriptyline 10–30 mg 2X/day | 30 days | VAS, number of tender points |
| Guo Y 2005b | ACR 1990 | 20/20 | 50 ± 7.1/ 49 ± 7.3 | 11 ± 2.5/10 ± 2.1 | Acupuncture 30 min 1X/day | Amitriptyline, 10-30mg twice daily | 30 days | VAS, number of tender points |
| Harris RE 200524 | ACR 1990 | 29/28 | 46 ± 10.1/51.3 ± 10.0 | 66 ± 44.52/62.04 ± 50.88 | Acupuncture on traditional site with stimulation 20 min 1–3X/week | Acupuncture on nontraditional site with stimulation, 20 min 1–3X/week | 9 weeks | Numeric Rating Scale NRS, Multi-Dimensional Fatigue Inventory questionnaire, RC, SF-36 |
| 30/27 | 44.5 ± 10.9/48.1 ± 10.9 | 63.12 ± 57.96/69.24 ± 49.2 | Acupuncture on traditional site without stimulation, 20 min 1–3X/week | Acupuncture on nontraditional site without stimulation, 20 min 1–3X /week | ||||
| Jiang F 200425 | ACR 1990 | 10/10 | 38 ± 11/35 ± 11 | 48 ± 36/48 ± 48 | Baishao Zongdai capsule, 0.6 g 3X/day, amitriptyline hydrochloride 25–50 mg/night + usual care | Amitriptyline hydrochloride 25–50 mg/night + usual care | 12 weeks | VAS, HAMA, HAMD, SCL-90 |
| 10/10 | 40 ± 9/37 ± 10 | 60 ± 60/60 ± 48 | Baishao Zongdai capsule, 0.6 g 3X/day, mirtazapine 7.5–15mg, amitriptyline hydrochloride, 25–50 mg/night + usual care | Mirtazapine, 7.5–15 mg, amitriptyline hydrochloride, 25–50 mg/night + usual care | ||||
| Lautenschlager J 198926 | Clinical symptoms | 25/25 | Unclear | Unclear | Electroacupuncture | Sham acupuncture with disconnected laser equipment | Unclear | VAS |
| Li AL 200427 | ACR 1990 | 28/30 | 46.8 | 27.6 | Herbal decoction 150 mL 2X/day plus acupuncture 20 min 1X/day | Amitriptyline 50 mg, 2X/day | 15 days | Self-rating scores of pain, sleep disorder, fatigue, etc., scores of product of number of tender points and pain intensity |
| Li CD 200628 | ACR 1990 | 33/33 | 38.26/39.10 | Unclear | Acupuncture 30 min + cupping therapy 5 min 1X/day, amitriptyline 25mg twice daily | Amitriptyline, 25 mg 2X/day | 12 days | MPQ, HAMD |
| Li J 200529 | ACR 1990 | 23/23 | 40 ± 2/40 ± 1.8 | 36 ± 6/36 ± 5.4 | Acupuncturec 30 min + computerized intermediate frequency (electromagnetic wave) treatment 20 min 1X/day | Amitriptyline, 25 mg/night | 30 days | Effective rate calculated according to VAS and reduction of symptoms |
| Liu JZ 200230 | ACR 1990 | 34/30 | 31 ± 4.3/30 ± 4.5 | 24 ± 6/24 ± 9.6 | Zheng Qing Feng Tong Ning Tablet 40–60 mg 3 X/day + usual care | Doxepin 25 mg/ night + usual care | 8 weeks | Effective rate calculated according to product of number of tender points and pain intensity andreduction of symptoms |
| Liu Q 200231 | IASR | 30/30 | 29–68/31–69 | 45.6 ± 16.8/46.8 ± 14.4 | Acupuncture with heavy manual stimulation 6 min 1X/day | Ibuprofen, 0.3 g 3X/day | 2 weeks | VAS, number of tender points |
| Martin DP 200632 | ACR 1990 | 25/25 | 51.7 ± 14.1/47.9 ± 11.2 | Unclear | Electroacupuncture, 20 min 1X every 2–4 days | Sham electroacupuncture (not insertion) 20 min 1X every 2 –4 days | 2–3 weeks | FIQ, MPI |
| Sprott H 199833 | ACR 1990 | 10/10 | 55 | Unclear | Electroacupuncture on points according to TCM 2X/week + basic therapy | Sham acupuncture disconnected laser equipment plus basic therapy | 3 weeks | Number of tender points, VAS |
| 10/10 | Basic therapy with no puncture treatment | |||||||
| Targino RA 200834 | ACR 1990 | 34/24 | 52.09 ± 10.97/51.17 ± 11.20 | 118.8 ± 117.3/93 ± 75.25 | Acupuncture 20 min 2X/week + tricyclic antidepressants 12.5–75 mg 1X/day, exercise 2X/week | Tricyclic antidepressants, 12.5–75 mg 1X/day + exercise 2X/week | 10 weeks | VAS, number of tender points below 4 kg/cm2, mean PPT, SF-36 |
| Wang CM 200835 | ACR 1990 | 28/28 | 44.3 | Unclear | Acupuncture 20 min + laser radiation on tender points 3 min 1X/day | Amitriptyline, 10 mg 2X/day | 20 days | VAS |
| Yang HB 200836 | ACR 1990 | 38/38 | 46.8 | 27.6 | Herbal decoction, 20 mL 2X/daydaily + psychologic treatment | Indometacin, 75 mg 1X/day + carbamazepine, 0.2 mg 3X/day | 8 weeks | Effective rate calculated according to reduction of symptoms |
| Yang TG 200737 | ACR 1990 | 33/17 | 38.2 ± 8.29/36.7 ± 10.13 | 39.36 ± 16.32/47.64 ± 17.76 | Herbal decoction (Jiawei Xiaoyao powder), 100 mL 2X/day | Amitriptyline, 25 mg, and ibuprofen sustained release capsules, 1 grain 2X/day | 4 weeks | VAS, effective rate calculated according to reduction of symptoms |
| Zhang YG 200138 | ACR 1990 | 34/30 | 36 | 30 | Acupuncture 30 min 1X/day | Amitriptyline, 25 mg/night | 30 days | Effective rate calculated according to reduction of symptoms |
Fu XY, Li CD. Clinical randomized controlled trial on combination of acupuncture, cupping and medicine for treatment of fibromyalgia syndrome [dissertation for Master's degree from Chengdu University of Traditional Chinese Medicine, Chengdu, China]. 2004.
Guo Y, Sun YZ. Clinical observation of therapeutic effect of penetration needling at the back in treating with fibromyalgia syndrome [dissertation for Master's degree from Heilongjiang University of Traditional Chinese Medicine, Heilongjiang, China]. 2005.
Selection of the acupoints according to Syndrome Differentiation.
±represents plus/minus standard deviation (for age and duration of disease).
m/f, male /female; Rx/C, experimental group/control group; m, months; ACR 1990, American College of Rheumatology 1990 criteria for classifying fibromyalgia; VAS, visual analogue scale; SF-36, Short Form–36; DRI, Disability Rating Index; HAD, Hospital Anxiety and Depression Scale; FIQ, Fibromyalgia Impact Questionnaire; QoLS, Quality of Life Scale; HAMD, Hamilton Depression Scale; HAMA, Hamilton Anxiety Scale; MPQ, McGill PainQuestionnaire; PPI, present pain intensity; TENS, transcutaneous electrical nerve stimulation; NRS, Numeric Rating Scale; SCL-90,RC, reliability of change; IASR, International Academy of Soreness Research; SCL-90, symptom checklist 90; TCM, Traditional Chinese Medicine; MPI, Multidimensional Pain Inventory; PPT, pain pressure threshold.
The twenty-five RCTs involved a total of 1516 patients with FM. The participants were ages 17–77, and the disease duration was from 3 months to 20 years. Twenty-three trials used ACR 1990 as the diagnostic criteria, one trial31 used the International Academy of Soreness Research (IASR)53 for diagnosing FM, and one trial26 made diagnoses according to the subjects' symptoms. The interventions included acupuncture (electroacupuncture, auricular acupuncture), cupping, herbal medicine (decoctions, capsules, and external preparations), massage, moxibustion, and combinations of acupuncture and cupping, or acupuncture and herbal medicine. The controls included no treatment, sham acupuncture, or conventional medications. The treatment duration ranged from 12 days to 12 weeks. Changes in visual analogue scale (VAS) scores as the major outcome measurement were reported in 15 trials. Seven trials18,23,27,31,33,34,† calculated the change of number of tender points, and used the McGill Pain Questionnaire (MPQ), Present Pain Intensity (PPI), or Fibromyalgia Impact Questionnaire (FIQ) for assessing intensity of pain. Four trials20,25,28,* used the Hamilton Depression Scale (HAMD) or Hamilton Anxiety Scale (HAMA) to assess depression or anxiety. Three trials16,24,34 used the Short-Form–36 (SF-36) and QoL scale (QoLS) for measuring QoL. Six trials used four categories to evaluate treatment effects including cure (symptoms disappeared and no tender points existed), markedly effective (symptoms reduced more than >50%), effective/reduced (symptoms reduced between 25% and 50%), and ineffective (symptoms reduced <25%). The combined rates of the markedly effective and effective treatments were used to calculate a total effective rate, which was the main outcome measure in some trials.
Methodological quality
According to our predefined quality assessment criteria, seven 16,19,24,28,32,34,† of the 25 trials (28%) were evaluated as having a low risk of bias, and another 18 included trials were evaluated as having an unclear risk of bias (Table 2). The sample size varied from 10 to 38 participants, with an average of 25 patients per group. None of the trials reported prior sample-size calculation, 11 trials16,19,21,24,25,28,32,34,35,37 described randomization procedures (using a random number table, computer generation of random numbers, or a drawing), but only two trials19,24 reported adequate allocation concealment. Four trials19,24,32,34 blinded both patients and outcome assessors, one trial16 only blinded patients, and three trials28,33,* blinded the outcome assessors. Nine trials16,17,19,21,24,28,32,34,* reported the number of dropouts, and three trials16,32,34 used intention-to-treat analysis.
Table 2.
Assessing Risk of Bias of Included Trials
| Lead author, year & ref. # | Sequence generation | Allocation concealment | Blinding of participants, personnel, and outcome assessors | Incomplete outcome data | Selective outcome reporting | Other sources of bias | Risk of bias |
|---|---|---|---|---|---|---|---|
| Assefi NP 200516 | Computer-generated, blocked random-allocation sequence with a block size of 4 | Unclear | Blinded to patients | No | No | No | Low risk of bias |
| Brattberg G 199917 | Unclear | Unclear | Not mentioned | No | No | No | Unclear risk of bias |
| Cao JY 200318] | Unclear | Unclear | Unclear | No | No | No | Unclear risk of bias |
| Deluze C 199219 | Electronic numbers generator | Closed envelopes | Blinded to patients and outcome assessors | No | No | No | Low risk of bias |
| Fu HW 200620 | Unclear | Unclear | Unclear | No | No | No | Unclear risk of bias |
| Fu XY 2004a | Table of random numbers | Unclear | Blinded to outcome assessors | No | No | No | Low risk of bias |
| Gao GM 200721 | Table of random numbers | Unclear | Unclear | No | No | No | Unclear risk of bias |
| Guo XJ 200322 | Unclear | Unclear | Unclear | No | No | No | Unclear risk of bias |
| Guo Y 200523 | Unclear | Unclear | Unclear | No | No | No | Unclear risk of bias |
| Guo Y 2005b | Unclear | Unclear | Unclear | No | No | No | Unclear risk of bias |
| Harris RE 200524 | Computer-generated random numbers in a four-block design | Closed envelope | Blinded to patients and outcome assessors | No | No | No | Low risk of bias |
| Jiang F 200425 | Draw cast | Unclear | unclear | Yes (SDfinal) | No | No | Unclear risk of bias |
| Lautenschlage 198926 | Unclear | Unclear | Blinded to patients | Yes (SD) | No | No | Unclear risk of bias |
| Li AL 200427 | Unclear | Unclear | Unclear | No | No | No | Unclear risk of bias |
| Li CD 200628 | Table of random number | Unclear | Blinded to outcome assessors | No | No | No | Low risk of bias |
| Li J 200529 | Unclear | Unclear | Unclear | Yes (VAS scores) | No | No | Unclear risk of bias |
| Liu JZ 200230 | Unclear | Unclear | Unclear | Yes (continuous data) | No | No | Unclear risk of bias |
| Liu Q 200231 | Unclear | Unclear | Unclear | No | No | No | Unclear risk of bias |
| Martin DP 200632 | In blocks of 4 | Unclear | Blinded to patients and outcome assessors | No | No | No | Low risk of bias |
| Sprott H 199833 | Unclear | Unclear | Blinded to outcome assessors | Yes (SD of number of tender points) | No | No | Unclear risk of bias |
| Targino RA 200834 | Computer-generated | Unclear | Blinded to patients and outcome assessors | No | No | No | Low risk of bias |
| Wang CM 200835 | Draw cast | Unclear | Unclear | No | No | No | Unclear risk of bias |
| Yang HB 200836 | Unclear | unclear | Unclear | No | No | No | Unclear risk of bias |
| Yang TG 200737 | Table of random number | unclear | Unclear | No | No | No | Unclear risk of bias |
| Zhang YG 200138 | Unclear | Unclear | Unclear | No | No | No | Unclear risk of bias |
Fu XY, Li CD. Clinical randomized controlled trial on combination of acupuncture, cupping and medicine for treatment of fibromyalgia syndrome [dissertation for Master's degree from Chengdu University of Traditional Chinese Medicine, Chengdu, China]. 2004.
Guo Y, Sun YZ. Clinical observation of therapeutic effect of penetration needling at the back in treating with fibromyalgia syndrome [dissertation for Master's degree from Heilongjiang University of Traditional Chinese Medicine, Heilongjiang, China]. 2005.
SDfinal, standard deviation at the end of the treatment SD, standard deviation; VAS, visual analogue score SD, standard deviation.
Effect estimates (Table 3)
Table 3.
Estimated Effect of Included Trials in Meta-Analyses
| Lead author, year and ref. # | Interventions | Estimate effects | Weight | p-value |
|---|---|---|---|---|
| 1. VAS scores after treatment | ||||
| 1.1 Therapeutic effect of acupuncture | ||||
| 1.1.1 Acupuncture versus sham acupuncture | ||||
| Assefi NP 200516 | Acupuncture versus sham acupuncture on false acupoints | 0.10 [–1.19, 1.59] | 13.67% | |
| Assefi NP 200516 | Acupuncture versus sham acupuncture without insertion | –0.30 [–1.64, 1.04] | 13.18% | |
| Deluze C 199219 | Electroacupuncture versus sham electroacupuncture on false acupoints | –1.39 [–1.64, –1.14] | 35.09% | |
| Harris RE 200524 | Acupuncture on traditional site versus acupuncture on nontraditional site | –1.30 [–2.07, 0.10] | 13.01% | |
| Harris RE 200524 | Acupuncture on traditional site with stimulation versus acupuncture on nontraditional site with stimulation | 0.92 [–0.59, 2.43] | 11.70% | |
| Martin DP 200632 | Electroacupuncture versus sham electroacupuncture without insertion | –0.70 [–2.06, 0.66] | 13.34% | |
| Overall (FEM, I2 = 69%) | MD –1.24 [–1.47, –1.01] | 100% | <0.00001 | |
| Overall (REM, I2 = 69%) | MD –0.55 [–1.35, 0.24] | 100% | 0.17 | |
| 1.1.2 Acupuncture versus conventional medications | ||||
| Guo Y 200523 | Acupuncture versus amitriptyline | –1.71 –2.39, –1.03] | 39.69% | |
| Guo Y 2005a | Acupuncture versus amitriptyline | –1.66 [–2.97, –0.35] | 21.63% | |
| Liu Q 200231 | Acupuncture versus ibuprofen | –1.90 [–2.61, –1.19] | 38.68% | |
| Overall (FEM, I2 = 0%) | MD –1.78 [–2.24, –1.32] | 100% | <0.00001 | |
| 1.2 Combination of acupuncture and cupping therapy + conventional medications versus medications alone | ||||
| Cao JY 200318 | Acupuncture + cupping therapy and seroxat versus seroxat alone | –1.63 [–2.18, –1.08] | 44.62% | |
| Li CD 200628 | Acupuncture + cupping therapy and amitriptyline versus amitriptyline | –1.77 [–2.74, 0.80] | 55.38% | |
| Overall (FEM, I2 = 0%) | MD –1.66 [–2.14, 1.19] | 100% | <0.00001 | |
| 2. # of tender points after treatment | ||||
| Therapeutic effect of acupuncture | ||||
| Guo Y 200523 | Acupuncture versus amitriptyline | –4.00 [–6.73, –1.27] | 16.4% | |
| Guo Y 2005a | Acupuncture versus amitriptyline | –3.30 [–6.02, –0.58] | 16.5% | |
| Liu Q 200231 | Acupuncture versus ibuprofen | –3.00 [–4.35, –1.65] | 67.1% | |
| Overall (FEM, I2 = 0%) | MD –3.21 [–4.23, –2.11] | 100% | <0.00001 | |
| 3. HAMD scores after treatment | ||||
| Combination of acupuncture and cupping therapy + conventional medications versus conventional medications alone | ||||
| Cao JY 200318 | Acupuncture plus cupping therapy and seroxat versus seroxat alone | –6.00 [–8.36, –3.64] | 44.62% | |
| Li CD 200628 | Acupuncture plus cupping therapy and amitriptyline versus amitriptyline | –4.04 [–6.16, –1.92] | 55.38% | |
| Overall (FEM, I2 = 32%) | MD –4.92 [−6.49, –3.34] | 100% | <0.00001 | |
| 4. Relapse rate after 6 months of treatment | ||||
| Acupuncture versus conventional medications | ||||
| Guo XJ 200322 | TENS versus oryzanol, vitamin B1, and amitriptyline | 0.30 [0.06, 1.44] | 32.6% | |
| Guo XJ 200322 | Electroacupuncture versus oryzanol, vitamin B1 and amitriptyline | 0.30 [0.06, 1.44] | 32.6% | |
| Guo Y 200523 | Acupuncture versus amitriptyline | 0.24 [0.05, 1.03] | 34.7% | |
| Overall (FEM, I2 = 0%) | RR 0.28 [0.11, 0.67] | 100% | 0.005 | |
Guo Y, Sun YZ. Clinical observation of therapeutic effect of penetration needling at the back in treating with fibromyalgia syndrome [dissertation for Master's degree from Heilongjiang University of Traditional Chinese Medicine, Heilongjiang, China]. 2005.
VAS, visual analogue scale; FEM, fixed effect model; MD, mean difference; REM, random effect model; HAMD; Hamilton Depression Scale; TENS, transcutaneous electrical nerve stimulation; RR, risk ratio.
Therapeutic effect of acupuncture
Twelve trials16,19,22–24,26,31–34,38,† tested acupuncture for treating FM. Six trials 16,19,24,26,32,33 compared acupuncture or electroacupuncture with sham acupuncture or sham electroacupuncture, and another six trials22,23,31,34,38,† compared acupuncture with conventional medications.
A pooling analysis of four trials16,19,24,32 showed a significant effect of acupuncture compared to sham acupuncture for reducing pain according to VAS scores after treatment (MD, –1.24; 95% CI, –1.47 to –1.01; p < 0.00001). However, this effect became nonsignificant (MD, –0.55; 95% CI, –1.35–0.24, p = 0.17) when using a random-effects model because of significant heterogeneity (I2 = 69%). Three trials23,31,† compared acupuncture with conventional medications, and the pooling results showed that acupuncture was significantly better than conventional medications for reducing pain (MD, –1.78; 95% CI –2.24 to –1.32, p < 0.00001; I2 = 0%) and number of tender points (MD, –3.21; 95% CI, –4.23 to –2.11; p < 0.00001; I2 = 0 %).
Two trials22,23 reported the relapse rate after 6 months, suggesting that acupuncture (including transcutaneous electrical nerve stimulation [TENS] and electroacupuncture) was significantly better than amitriptyline for preventing relapse (RR 0.28; 95% CI, 0.11–0.67; p = 0.005; I2 = 0%).
Data from four trials26,33,34,38 were not included in the meta-analysis because of poor reporting. The main findings of those trials are presented in Table 4.
Table 4.
Characteristics of Randomized Controlled Trials outside Meta-Analysis
| Lead author, year & ref. # | Comparisons | Main findings |
|---|---|---|
| Acupuncture versus sham acupuncture | ||
| Lautenschlager J 198926 | Acupuncture versus sham laser acupuncture | Significant difference between acupuncture and sham treatment in pain reduction measured by all 3 methods by end of treatment. At follow-up of 3 months after last treatment, no significant changes were observed (p > 0.05). |
| Sprott H 199833 | Acupuncture versus sham laser acupuncture | Data for pain reduction by tender points were not completely reported, but # of tender points was not significantly decreased after acupuncture treatment, compared to sham treatment (p > 0.05). Intensity of pain, measured by VAS, was not significantly reduced, neither immediately at end of treatment or 2 months after treatment (p > 0.05). |
| Acupuncture versus no treatment | ||
| Sprott H 199833 | Acupuncture versus no treatment | # of tender points was significantly decreased after acupuncture treatment, compared to no treatment (p > 0.05). |
| Acupuncture versusconventional medication | ||
| Zhang YG 200138 | Acupuncture versus amitriptyline | No significant difference in total effective rate between the two groups (88.2% versus 83.3%; p > 0.05), but at follow-up at 6 months after end of the treatment, the total effective rate in the acupuncture group was higher than in the amitriptyline group (67.6% versus 40.0%; p < 0.05). |
| Acupuncture + other interventions versus other interventions | ||
| Targino RA 200834 | Acupuncture plus tricyclic antidepressants and exercise with tricyclic antidepressants and exercise | Patients in acupuncture group were significantly better than the control group in terms of VAS scores (p < 0.001), PPT (p < 0.001), # of tender points below 4 kg/cm2 (p < 0.001), and in 5 subscales of the SF-36 (p < 0.05). |
| Massage versus no treatment | ||
| Brattberg G 199917 | Connective tissue massage versus no treatment or discussion | No significant difference between connective tissue massage and no treatment for reducing pain according to VAS scores after treatment (MD, –0.58; 95% CI, –1.76 to 0.60; p = 0.34). |
| Herbal medicine versus conventional medications | ||
| Fu HW 200620 | Shugan Jieyu Huoxue Tongluo decoction versus amitriptyline | Herbal decoction superior to amitriptyline for reducing depression according to HAMD after treatment (MD, –3.70; 95% CI, –6.09 to –1.31; p = 0.002) |
| Guo GM 200721 | Total flavones of Rhizoma Drynariae versus meloxicam | No difference between two groups in pain reduction according to VAS scores after treatment (MD, –0.80; 95% CI, –1.66 to 0.06; p > 0.05). |
| Total flavones of Rhizoma Drynariae versus meloxicam and amitriptyline | No difference between two groups on pain reduction according to VAS scores after treatment (MD, –0.10; 95% CI, –0.87 to 0.64; p > 0.05). | |
| Liu JZ 200230 | Zhengqing Fengtong Ning tablet versus doxepin | According to category outcome measurement, herbal medicine was significantly better than doxepin (91.2% versus 76.7%; p < 0.05) in total effective rate (markedly effective plus effective rate). |
| Yang HB 200836 | Xiaoyao Qianghuo Chushi decoction versus indometacin and carbamazepine | In terms of total effective rate, herbal medicine produced a better effect than conventional medication (94.74% versus 86.84%; p < 0.05). |
| Yang TG 200737 | Jiawei Xiaoyao powder versus amitriptyline and ibuprofen sustained release capsules | Therapeutic effect (MD, –1.89; 95% CI, –2.62 to –1.16; p < 0.05) and reduction of symptoms (90.9% versus 64.7%; p < 0.05) in the treatment group were more marked than in the control group. |
| Herbal medicine + other interventions versus other interventions | ||
| Guo GM 200721 | Total flavones of Rhizoma Drynariae and amitriptyline versus meloxicam and amitriptyline | Significant difference between two groups in pain reduction according to VAS scores after treatment (MD, –2.00; 95% CI, –2.69 to –1.31; p < 0.05). |
| Meloxicam, total flavones of Rhizoma Drynariae and amitriptyline versus meloxicam and amitriptyline | Significant difference between two groups in pain reduction according to VAS scores after treatment (MD, –1.10; 95% CI, –1.83 to –0.37; p < 0.01). | |
| Jiang F 200425 | QoL | According to change of VAS scores, HAMD, and SCL-90, herbal medicine combined with conventional medications was significantly better than conventional medications alone for reducing pain and improving QoL for patients with FM (p < 0.05). |
| Combination of acupuncture and other TCM therapies versus conventional medications | ||
| Fu XY 2004a | Acupuncture + cupping therapy versus amitriptyline | Combination of acupuncture + cupping therapy was significantly better than conventional medications for reducing VAS scores (MD = –1.96; 95% CI, –2.91 to –1.01; p < 0.0001) and HAMD scores (MD, –3.99; 95% CI –5.47 to 2.51; p < 0.00001). |
| Li AL 200427 | Ding Tong decoction plus acupuncture and psychologic therapy with amitriptyline and psychologic therapy | According to the scores of self-rating evaluation of reduction of symptoms and calculation of pain intensive and # of tender points, there were no significant differences between two groups (p > 0.05). |
| Li J 200529 | Acupuncture and computer intermediate frequency (electromagnetic wave) treatment versus amitriptyline, with psychologic therapy in both groups. | No significant difference between two groups in total effective rate (<3 scores on a 10-point VAS scale, or symptoms disappeared or markedly relieved, or # of tender points decreased > 6 points; 95.65% versus 95.65%; p > 0.05). |
| Wang CM 200835 | Acupuncture plus laser radiation versus amitriptyline | According to VAS scores after treatment, acupuncture + laser radiation were significantly better than amitriptyline for pain reduction (MD = –2.27; 95% CI, –3.05 to –1.49; p < 0.00001). |
Fu XY, Li CD. Clinical randomized controlled trial on combination of acupuncture, cupping and medicine for treatment of fibromyalgia syndrome [dissertation for Master's degree from Chengdu University of Traditional Chinese Medicine, Chengdu, China]. 2004.
VAS, visual analogue scale; PPT, pressure pain threshold; SF-36, Short Form–36; MD, mean difference; CI, confidence interval; HAMD, Hamilton Depression Scale; SCL-90, symptom checklist 90; QoL, quality of life; FM, fibromyalgia; TCM, Traditional Chinese Medicine.
As a result of the insufficient number of included trials in one meta-analysis, a meaningful funnel plot analysis was not feasible.
Therapeutic effect of herbal medicine
Six trials20,21,25,30,36,37 tested herbal medicine against Western medicine for FM. Three trials20,36,37 tested herbal decoctions, two trials25,30 tested a Chinese patent medicine, and one trial21 tested active components of an herbal medicine. As a result of the variation of herbal medicines, the data were not combined. The main findings of the six trials are presented in Table 4.
Therapeutic effect of massage
Only one small trial17 tested massage for treatment of FM and showed no significant difference between “connective tissue” massage and no treatment for reducing pain according to VAS scores after treatment (MD, –0.58; 95% CI, –1.76–0.60; p = 0.34).
Therapeutic effect of combination therapies of TCM
Six trials17,27–29,35,* tested the therapeutic effect of combination TCM therapies for treating FM. Three trials18,28,* compared acupuncture plus cupping therapy with medications, one trial29 compared acupuncture plus computerized intermediate frequency treatment with amitriptyline, one trial35 compared acupuncture plus laser treatment with amitriptyline, and one trial27 compared acupuncture plus herbal medicine with Western medications.
Two trials18,28 showed that a combination of acupuncture and cupping therapy plus medications was significantly better than conventional medications alone for reducing pain (MD, –1.66, 95% CI, 2.14 to –1.19, p < 0.00001, I2 = 0%) and HAMD scores (MD, –4.92, 95% CI, –6.49 to –3.34, p < 0.00001, I2 = 32%).
Four trials27,29,35,* were not included in the meta-analysis as a result of the data being unavailable. The main findings of these trials are presented in Table 4.
Adverse effects
An outcome of adverse events was described in 11 trials.16,20,21,25,27,29,30,34,36,*,† Adverse effects from eight trials16,21,25,29,30,34,*,† were related to TCM therapies, including four16,29,34,†related to acupuncture, three to herbal medicine, and one* to cupping therapy. The adverse effects of acupuncture were bruising, nausea, fainting, discomfort at the sites of needle insertions or simulated needle insertions, and temporary edema of the hand. Nausea, fainting, dry mouth, bimalleolar edema, and skin rash were reported as adverse effects of herbal medicines. One trial* reported that 1 patient had mild scalding on the skin after being included in a cupping group (n = 33).
Lethargy, nausea, fainting, dry mouth, fatigue, blurred vision, hyperhydrosis, and constipation were reported adverse effects of conventional medications.
No serious adverse event was reported in any of the included trials.
Discussion
The data from the 25 RCTs that were analyzed demonstrate that, acupuncture, acupuncture combined with cupping therapy, or acupuncture combined with cupping and conventional medication were significantly more effective than conventional medication alone for reducing pain and number of tender points in subjects with FM. The therapeutic effect of acupuncture appears to be similar to sham acupuncture for pain reduction, but more data are needed to prove this finding. The therapeutic effects of herbal medicine and massage are uncertain due to limited numbers of clinical trials.
There are several limitations in this review. The quality of the included studies is generally poor, which indicates an unclear risk of bias resulting from insufficient reporting of methodological components in the trials. There were unclear descriptions of randomization procedures and lack of blinding in the majority of trials, which may have created potential performance biases and detection biases, as patients and researchers might have been aware of the therapeutic interventions. Intention-to-treat analysis was not applied in most of the included trials, and although it was not possible to perform a meaningful funnel-plot analysis because of the insufficient number of included trials in the meta-analysis, there remained the possible existence of publication bias. To the ability to perform meta-analysis was limited because of the heterogeneity of the interventions among the included trials and the variance of composite outcome measures used in 15 of the included trials. This was particularly relevant to the outcome classifications as cure, markedly effective, effective or ineffective, which were used in six trials and but was not validated; thus the findings were hard to interpret. Consequently, interpretation of these positive findings should be cautious, and the study methodology needs to be improved for future confirming studies.
The searches conducted in the present study identified four systematic reviews of acupuncture for treating FM. The latest one50 published in 2009 included only six trials, which were all included in this systematic review. In this systematic review five high-quality trials compared acupuncture with sham acupuncture, which may not be appropriate as a placebo against which to evaluate the therapeutic effect of real acupuncture.51 There were 12 trials evaluating acupuncture for FM in this review, but only two of them used syndrome-differentiation for acupuncture-point selection. The data suggesting that acupuncture is effective for FM should be taken as being tentative and further randomized trials are warranted. Control interventions in such trials should be carefully selected, as, at the present time, there is not a proper “acupuncture placebo.”
Nine of the included trials16,17,22,23,25,32–34,38 reported the results of follow-up. One trial34 followed all the patients for 2 years, reporting that the acupuncture group was significantly better than the control group with respect to numbers of tender points after 6 months, but, at 2 years, noting that there was no significant difference in any outcomes. One trial32 followed all patients for 7 months and showed no difference between acupuncture and sham acupuncture for pain reduction. Assefi et al.16 followed all patients for 6 months, suggesting that the observed effect was probably driven by the higher mean score in the simulated-acupuncture group compared with the sham-needling group. Another trial17 followed patients for up to6 months and showed no statistically significant differences between massage and no treatment for the tested parameters at 3 and 6 months. Two trials22,23 followed the patients for 6 months, suggesting that acupuncture was significantly better than amitriptyline for preventing relapse after treatment, although the number of patients who were followed was too small for substantial statistical analysis. There is no evidence for a long-term effect of herbal medicine or cupping therapy.
Most of the existing trials are of small size and have an unclear risk of bias or a high risk of bias. Further rigorously designed trials are needed to confirm the effectiveness of TCM therapy for treating FM. Randomization methods need to be described clearly and reported fully. Although blinding of patients and practitioners might be very difficult for acupuncture or herbal medicine, blinding of outcome assessors should be attempted as far as possible to minimize performance and assessment biases. Choosing outcome measures should be based on an international consensus and should include continuous data and daily average pain scores from baseline to study completion. Analysis of outcomes based on the intention-to-treat principle is vital as is the application of well-defined diagnostic criteria, such as ACR 1990, thus, increasing comparability between trials. Reporting of trials should follow Consolidated Standards of Reporting Trials (CONSORT)52 standards to explain the processes involved explicitly and in a transparent manner.
Conclusions
The preliminary conclusions of the current study suggest that patents with FM might benefit from TCM treatment. FM is a chronic disease and better, larger trials will be the basis for demonstrating the effectiveness and long-term effects of TCM therapies.
Footnotes
This is a full-text article of a presentation for the 5th International Congress on Complementary Medicine Research, Tromsø, Norway, May 19–21, 2010.
Fu XY, Li CD. Clinical randomized controlled trial on combination of acupuncture, cupping and medicine for treatment of fibromyalgia syndrome [dissertation for Master's degree from Chengdu University of Traditional Chinese Medicine, Chengdu, China]. 2004.
Guo Y, Sun YZ. Clinical observation of therapeutic effect of penetration needling at the back in treating with fibromyalgia syndrome [dissertation for Master's degree from Heilongjiang University of Traditional Chinese Medicine, Heilongjiang, China]. 2005.
Disclosure Statement
No competing financial conflicts exist.
Acknowledgments
H.J. Cao and Liu JP were supported by a grant from the National Basic Research Program of China (“973” Program, No. 2006CB504602) and an international cooperation project from the Ministry of Science and Technology of China (2009DFA31460). Liu JP was in part supported by the Grant Number R24 AT001293 from the National Center for Complementary and Alternative Medicine (NCCAM) of the U.S. National Institutes of Health. Lewith GT was supported by the Rufford Maurice Laing Foundation.
References
- 1.Russell IJ. Raphael KG. Fibromyalgia syndrome: Presentation, diagnosis, differential diagnosis, and vulnerability. CNS Spectr. 2008;13(3suppl 5):6–11. doi: 10.1017/s1092852900026778. [DOI] [PubMed] [Google Scholar]
- 2.Wolfe F. Smythe HA. Yunus MB, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia: Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33:160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 3.Miller LJ. Kubes KL. Serotonogenic agents in the treatment of fibromyalgia syndrome. Ann Pharmacother. 2002;36:707–712. doi: 10.1345/aph.1A184. [DOI] [PubMed] [Google Scholar]
- 4.Argoff CE. Pharmacologic management of chronic pain. J Am Osteopathic Assoc. 2002;102(9suppl3):521–526. [PubMed] [Google Scholar]
- 5.Hauser W. Bernardy K. Ueeyler N. Sommer C. Treatment of fibromyalgia syndrome with antidepressants: A meta-analysis. JAMA. 2009;301:198–209. doi: 10.1001/jama.2008.944. [DOI] [PubMed] [Google Scholar]
- 6.Uceyler N. Hauser W. Sommer C. A systematic review on the effectiveness of treatment with antidepressants in fibromyalgia syndrome. Arthritis Rheum. 2008;59:1279–1298. doi: 10.1002/art.24000. [DOI] [PubMed] [Google Scholar]
- 7.Tofferi JK. Jackson JL. O'Malley PG. Treatment of fibromyalgia with cyclobenzaprine: A meta-analysis. Arthritis Rheum. 2004;51:9–13. doi: 10.1002/art.20076. [DOI] [PubMed] [Google Scholar]
- 8.Moore RA. Straube S. Wiffen PJ, et al. Pregabalin for acute and chronic pain in adults. Cochrane Database Syst Rev. 2009;3 doi: 10.1002/14651858.CD007076.pub2. CD007076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sim J. Adams N. Systematic review of randomized controlled trials of nonpharmacological interventions for fibromyalgia. Clin J P. 2002;18:324–336. doi: 10.1097/00002508-200209000-00008. ; [DOI] [PubMed] [Google Scholar]
- 10.Fu XY. Li Y. Yang JJ. A survey of acupuncture for fibromyalgia syndrome. Shanghai J Acupunct Moxibustion. 2004;237:46–48. [Google Scholar]
- 11.U.S. Department of Health and Human Services Public Health Service. Acupuncture for Fibromyalgia. Maryland: U.S. Department of Health and Human Services Public Health Service, Agency for Healthcare Research and Quality. 2003.
- 12.Mayhew E. Ernst E. Acupuncture for fibromyalgia—a systematic review of randomized clinical trials. Rheumatology. 2007;46:201–204. doi: 10.1093/rheumatology/kel406. [DOI] [PubMed] [Google Scholar]
- 13.Wahner-Roedler DL. Elkin PL. Vincent A. Thompson JM, et al. Use of complementary and alternative medical therapies by patients referred to a fibromyalgia treatment program at a tertiary care center. Mayo Clin Proc. 2005;80:55–60. doi: 10.1016/S0025-6196(11)62958-3. [DOI] [PubMed] [Google Scholar]
- 14.Higgins JPT, editor; Green S, editor. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.0.1 [updated September 2008] The Cochrane Collaboration, 2008. www.cochrane-handbook.org. [Mar 27;2010 ]. www.cochrane-handbook.org
- 15.Higgins JP. Thompson SG. Quantifying heterogeneity in a meta-analysis. Statistics Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 16.Assefi NP. Sherman KJ. Jacobsen C. Goldberg J. Smith WR. Buchwald D. A randomized clinical trial of acupuncture compared with sham acupuncture in fibromyalgia. Ann Intern Med. 2005;143:10–19. doi: 10.7326/0003-4819-143-1-200507050-00005. [DOI] [PubMed] [Google Scholar]
- 17.Brattberg G. Connective tissue massage in the treatment of fibromyalgia. Eur J Pain. 1999;3:235–245. doi: 10.1053/eujp.1999.0123. [DOI] [PubMed] [Google Scholar]
- 18.Cao JY. Li Y. Combination of acupuncture and antidepressant medications in treating of 56 cases of fibromyalgia. Chin Arch Trad Chi Med. 2003;21:813. —817. [Google Scholar]
- 19.Deluze C. Bosia L. Zirbs A, et al. Electroacupuncture in fibromyalgia: Results of a controlled trial. BMJ. 1992;305:1249–1252. doi: 10.1136/bmj.305.6864.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fu HW. Jin ML. Hong J. Herbal decoction with function of relieving qi stagnancy in liver and promoting Blood circulation to remove meridian obstruction in treating 21 cases of fibromyalgia. Zhejiang J Trad Chin Med. 2006;41:204–205. [Google Scholar]
- 21.Gao GM. Jiang L. Liu SY, et al. A randomized and controlled study of clinical efficacy for total flavone of Rhizoma Drynariae on fibromyalgia syndrome. Chin J New Drug Clin Remedies. 2007;26:837–840. [Google Scholar]
- 22.Guo XJ. Jia J. Comparison of therapeutic effects of transcutaneous electrical nerve stimulation and electroacupuncture on fibromyalgia syndrome. Chin Acupunct Moxibustion. 2003;23:653–655. [Google Scholar]
- 23.Guo Y. Sun YZ. Clinical study on treatment of fibromyalgia syndrome with penetration needling at the back. ChinAcupunct Moxibustion. 2005;25:98–100. [PubMed] [Google Scholar]
- 24.Harris RE. Tian X. Williams DA, et al. Treatment of fibromyalgia with formula acupuncture: Investigation of needle placement, needle stimulation, and treatment frequency. J Altern Complement Med. 2005;11:663–671. doi: 10.1089/acm.2005.11.663. [DOI] [PubMed] [Google Scholar]
- 25.Jiang F. Liu JB. An observation on clinical efficacy in fibromyalgia syndrome. Chin J Rheumatol. 2004;8:750–752. [Google Scholar]
- 26.Lautenschlager J. Schnorrenberger CC. Muller W. Acupuncture with general fibromyalgia syndrome. Dtsch Zschr Akup. 1989;32:122–128. [Google Scholar]
- 27.Li AL. Wang ZL. Ping Y. Clinical observation of the treatment of primary fibrositis syndrome by Ding Tongtang combined with acupuncture. Chin J Curr Clin Medic. 2004;2(9A):1387–1388. [Google Scholar]
- 28.Li CD. Fu XY. Jiang ZY, et al. Clinical study on combination of acupuncture, cupping and medicine for treatment of fibromyalgia syndrome. Chin Acupunct Moxibustion. 2006;26:8–10. [PubMed] [Google Scholar]
- 29.Li J. Yu HB. She T. The clinical effect of acupuncture and computer [sic] intermediate frequency for fibromyalgia syndrome. Modern Med J China. 2005;7:42–44. [Google Scholar]
- 30.Liu JZ. Liu YF. Liu JJ. Clinical observation of Zhengqing Fengtong Ning tablet for fibromyalgia syndrome. Chin J Integr Med. 2002;22:316. [Google Scholar]
- 31.Liu Q. Li F. Clinical observation of acupuncture for 30 cases of fibromyalgia. Anthol Med. 2002;21:183. [Google Scholar]
- 32.Martin DP. Sletten CD. Williams BA. Berger IH. Improvement in fibromyalgia symptoms with acupuncture: Results of a randomized controlled trial. Mayo Clin Proc. 2006;81:749–757. doi: 10.4065/81.6.749. [DOI] [PubMed] [Google Scholar]
- 33.Sprott H. Efficiency of acupuncture in patients with fibromyalgia. Clin Bull Myofascial Ther. 1998;3:37–43. [Google Scholar]
- 34.Targino RA. Imamura M. Kaziyama HH, et al. A randomized controlled trial of acupuncture added to usual treatment for fibromyalgia. J Rehabil Med. 2008;40:582–588. doi: 10.2340/16501977-0216. [DOI] [PubMed] [Google Scholar]
- 35.Wang CM. Combination of acupuncture and semiconductor laser in treating 28 cases of fibromyalgia syndrome. J Practical Trad Chin Intern Med. 2008;22:58. [Google Scholar]
- 36.Yang HB. Combination of Xiaoyao Qianghuo Chushi decoction and Suanzao Mugua Sanqi Medicinal Liquor in treating 38 cases of fibromyalgia syndrome. J Clin Exper Med. 2008;7:146–147. [Google Scholar]
- 37.Yang TG. Feng XH. Clinical study on Jiaweixiaoyao powder [sic] treat the fibromyalgia syndrome. Liaoning J Trad Chin Med. 2001;20:438. [Google Scholar]
- 38.Zhang YG. Clinical observation on acupuncture treatment of primary fibromyalgia syndrome. Zhongguo Zhen Jiu. 2008;8:7619–7620. [Google Scholar]
- 39.Guo XJ. Jia J. Clinical observation of therapeutic effects of transcutaneous electrical nerve stimulation on fibromyalgia syndrome. Clin J Phys Med Rehabil. 2004;26:126–127. [Google Scholar]
- 40.Guo XJ. Jia J. Comparison of therapeutic effects of transcutaneous electrical nerve stimulation and electroacupuncture on fibromyalgia syndrome. Chin J Clin Rehabil. 2005;9:171–173. [Google Scholar]
- 41.Chen HJ. Wang GF. Gao M. Medium frequency electrotherapy combined with semiconductor laser in treating with psoas fibrositis. Chin J Phys Med Rehabil. 2004;26:739. [Google Scholar]
- 42.Liang Q. Combination of acupuncture with warm needle and cupping therapy in treating of 42 cases of fibrositis. J Practical Tradit Chin Intern Med. 1999;13:50. [Google Scholar]
- 43.Liu LJ. Combination of electroacupuncture and cupping therapy on treatment of 40 cases of fibrositis. Chin Acupunct Moxibustion. 1995:20. [Google Scholar]
- 44.Ma TW. Pei JZ. Combination of massage and moxibustion in treating 57 cases of shoulder fibrositis. Chin Manipulation Qi Gong Ther. 2003;19:23. [Google Scholar]
- 45.Wang LQ. Combination of cupping and auricular therapy in treating 60 cases of fibrositis. Shandong J Tradit Chin Med. 1996;15:24. [Google Scholar]
- 46.Wang SP. Wang XF. Zhang DX, et al. Clinical observation on therapeutic effect of acupuncture treatment based on syndrome differentiation of meridians on fibromyalgia syndrome. Chin Acupunct Moxibustion. 2002;22:807–809. [Google Scholar]
- 47.Yang NH. Wang W. Combination of herbal tincture and TDP irradiation for fibrositis. Herald Med. 2001;20:438. [Google Scholar]
- 48.Zuo YM. Clinical observation of Jinbitong capsule for fibrositis. Clin J Misdiagnostics. 2008;8:7619–620. [Google Scholar]
- 49.Ronald K. Pain Management Secrets. Beijing: China Ocean Press; 1999. p. 149. [Google Scholar]
- 50.Martin-Sanchez E. Torralba E. Diaz DE, et al. Efficacy of acupuncture for the treatment of fibromyalgia: Systematic review and meta-analysis of randomized trials. Open Rheumatol J. 2009;3:25–29. doi: 10.2174/1874312900903010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Madsen MV. Gotzsche PC. Hrobjartsson A. Acupuncture treatment for pain: Systematic review of randomized clinical trials with acupuncture, placebo acupuncture and no acupuncture groups. BMJ. 2009;338:a3115. doi: 10.1136/bmj.a3115. ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.CONSORT Statement 2001—Checklist. Items to Include When Reporting a Randomized trial. www.consort-statement.org. [Aug 31;2009 ]. www.consort-statement.org