Abstract
Objectives
Bone marrow aspiration and biopsy (BMAB) is painful when performed with only local anesthetic. Our objective was to determine whether viewing nature scenes and listening to nature sounds can reduce pain during BMAB.
Design
This was a randomized, controlled clinical trial. Adult patients undergoing outpatient BMAB with only local anesthetic were assigned to use either a nature scene with accompanying nature sounds, city scene with city sounds, or standard care. The primary outcome was a visual analog scale (0–10) of pain. Prespecified secondary analyses included categorizing pain as mild and moderate to severe and using multiple logistic regression to adjust for potential confounding variables.
Results
One hundred and twenty (120) subjects were enrolled: 44 in the Nature arm, 39 in the City arm, and 37 in the Standard Care arm. The mean pain scores, which were the primary outcome, were not significantly different between the three arms. A higher proportion in the Standard Care arm had moderate-to-severe pain (pain rating ≥4) than in the Nature arm (78.4% versus 60.5%), though this was not statistically significant (p = 0.097). This difference was statistically significant after adjusting for differences in the operators who performed the procedures (odds ratio = 3.71, p = 0.02).
Conclusions
We confirmed earlier findings showing that BMAB is poorly tolerated. While mean pain scores were not significantly different between the study arms, secondary analyses suggest that viewing a nature scene while listening to nature sounds is a safe, inexpensive method that may reduce pain during BMAB. This approach should be considered to alleviate pain during invasive procedures.
Introduction
Pain is a common complication of cancer and is multifactorial in origin, with medical procedures contributing significantly to patient discomfort.1,2 In one prospective study of patients with cancer undergoing invasive procedures, 40% of patients who underwent bone marrow aspirate and biopsy (BMAB) reported moderate to severe pain during the procedure.3
There are a number of reasons medical personnel do not provide adequate sedation and analgesia during painful procedures. Practitioners may not recognize that procedures are painful or they may be concerned about possible adverse effects of medications such as respiratory depression or nausea and vomiting.4–6 Additionally, sedation requires closer monitoring of patients and requires more time and personnel than procedures done without sedation and analgesics.7 While systemic analgesics and sedatives are generally well tolerated, effective, and should be used, they may not provide complete pain relief.8–10 Complementary approaches to pain management during painful procedures may enhance the patient experience.
Nonpharmacologic approaches such as guided imagery, hypnosis, and distraction have been effective in improving patient experiences during stressful or painful medical encounters.11,12 The biologist E.O. Wilson in his biophilia hypothesis suggested that humans have an innate attraction to nature and interactions with nature have a therapeutic effect.13 Use of pastoral images has been successful for reducing pain in a variety of patient settings including perioperative care, phlebotomy, and burn care.14–16 The present authors found that use of a static, pastoral image with complementary nature sounds reduced pain in patients undergoing fiberoptic bronchoscopy.17
It is not known whether distraction with pastoral images and sounds offer benefit over comparable urban images and sounds, nor is it known whether nature sights and sounds are effective in reducing pain during BMAB. This study was designed to determine whether nature sights and sounds could improve pain control compared to standard care and city sights and sounds in patients undergoing BMAB.
Methods
Design
This was a single-center, randomized controlled trial in which patients referred for outpatient BMAB were recruited to participate. Written informed consent was obtained from all participants. The study was approved by the Johns Hopkins Institutional Review Board. This study is registered with clinical trials.gov, Identifying number: NCT00315796. Eligible subjects were randomly assigned to one of three treatment groups: (1) Nature Sights and Sounds (Nature), (2) City Sights and Sounds (City), or (3) Standard Care. Subjects had to be 18 years or older with a diagnosis of cancer. Patients were excluded if they received sedatives for the procedure, had visual or hearing impairment that would interfere with the use of the study intervention, altered mental status (Mini-Mental Status Exam <25), English language illiteracy, contact isolation for infection control, or Karnofsky performance score below 60. Blocked randomization was performed using variable block sizes. The randomization sequence was created using the computer program Blocked Stratified Randomization Version 5.0 (Johns Hopkins Oncology Center, Baltimore, MD). Treatment assignments were kept in sealed envelopes, which were opened at the time of enrollment. A single research assistant enrolled the subjects.
Intervention
The nature sights and sounds intervention consisted of a 42-inch × 52-inch, high-resolution photographic mural of a mountain stream in a spring meadow (Fig. 1). The mural was mounted on a moveable stand and positioned for viewing next to the patient's head when they were lying prone on the procedure table. Subjects listened to a tape of nature sounds using a personal cassette player through standard headphones (Panasonic Corporation of America). Subjects were encouraged to adjust the volume to a level they found comfortable. The biophilic nature scene and sounds are produced and marketed under the trade name Bedscapes® (Healing Environments Inc., Elkins Park, PA; www.bedscapes.com). Subjects assigned to the city sights and sounds viewed a similar sized and positioned photograph of an urban scene with buildings and cars (Fig. 1) and listened to a recording of city sounds through headphones. The city scene and sounds were designed specifically for this study. The city scene photograph deliberately lacked images of nature (e.g., trees, plants, and water). Subjects in the two intervention arms were encouraged to view the scenes and listen to the recordings the entire time they were in the procedure room; however, patients were allowed to close their eyes, look away from the murals, or turn off the cassette if they so desired. No subjects were given any oral or parenteral sedatives or analgesics before or during the procedure. This is consistent with the usual practice at our institution. Given the features of the intervention, there was no feasible way to mask treatment assignments. Bone marrow biopsies were performed by physician assistants and nurse practitioners who comprise a BMAB clinical service. Local anesthetic was administered by the operators to all subjects independently of the study protocol. The dosage of lidocaine administered was recorded, as was the duration of the procedure. A research assistant obtained consent for the study prior to the procedure and administered a brief survey. The research assistant was present during the procedures and measured vital signs during the procedure. Vital signs were measured before the procedure and every 15 minutes during the procedure. Subjects were given a questionnaire to complete immediately following the BMAB but were allowed to take it home for completion.
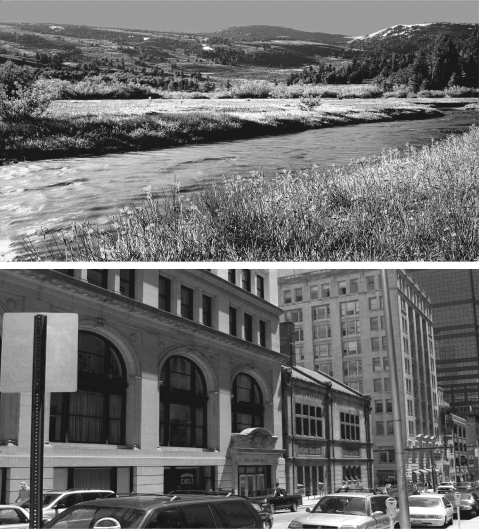
FIG. 1.
The Nature Scene and the City Scene. These are copies of the two images used in the study. During the study, these large photographic-quality murals were mounted on stands next to the procedure table.
Outcome measures
The primary outcome in this study was pain as recorded using the Hopkins Pain Rating Instrument (HPRI), a validated visual analog scale with a sliding marker that moves within a groove.18 The side facing the patient has a 10-cm line with the anchors “No Pain” and “Worst Pain Imaginable.” The opposite side of the instrument is a 10-cm scale with markings every 0.5 cm that enables the clinician to read and record numerical values. Scores were recorded to the nearest 0.5 cm. Subjects rated their pain immediately before the procedure and immediately after the procedure. For the post-procedure HPRI recording, subjects were asked to rate the worst pain experienced during the procedure. The HPRI scores were dichotomized into mild pain (<4) and moderate to severe pain (≥4). This was a prespecified outcome, and these cut points have been reported previously.3 Other outcomes included patient satisfaction measured using 5-point Likert-type scales,8 psychologic distress measured with the Brief Symptom Index (BSI),19 and negative mood states and anxiety measured with the Profile of Mood States (POMS).20 Other objective outcomes included heart rate, blood pressure, and salivary cortisol levels.21 Two (2) saliva samples were collected 20 minutes apart prior to the procedure and three samples were collected 15 minutes apart following the procedure. The Pain Catastrophizing Scale (PCS) was obtained to identify potential individual differences in subjects' cognitive emotional responses to pain, which could mediate outcome.22
Statistical analyses and sample size
Recruitment goals were based on having 80% power to detect a 2-point difference in pain rating on the HPRI between the Nature Sights and Sounds arm and the Standard Care arm with an α error level of 0.05. This assumed a standard deviation of 2.5 for the HPRI. Meeting these goals required 29 subjects per group or 87 patients total. The plan was to enroll 120 subjects to allow for study withdrawal and missing data.
Data were analyzed based on the principle of intention to treat. Descriptive statistics were compiled on demographics, disease characteristics, education, self-reported health status, percentage of time subjects used the study intervention, and prior complementary/alternative medicine use. Bivariate analyses comparing pain ratings, POMS scores, BSI scores, PCS scores, heart rate, blood pressure, and salivary cortisol by study arm were performed using Fisher's exact test or the Kruskal-Wallis test. Prespecified multivariate analyses using logistic regression were performed to adjust for potential confounders that were statistically significant in bivariate analysis or were significant predictors of pain in earlier studies.8 The multivariate logistic regression model used mild versus moderate-to-severe pain as the outcome variable. The predictor variables in the model were study arm assignment, operator, procedure duration, patient age, gender, and prior use of pain medications. Multiple imputation using switching regression was performed to account for predictor and outcome variables that had greater than 10% of values missing. There were no missing data for the primary outcome, and in general missing data were rare. Missing data occurred primarily because 22 subjects did not return the postprocedure questionnaire (Fig. 2). This resulted in missing data from the POMS, BSI, PCS instruments and questions regarding satisfaction. The response rate for these questionnaires was 82%. Analyses were performed with and without imputation and the results did not differ qualitatively between the two approaches. The results shown are without imputation. Results are reported as mean ± standard deviation unless specified otherwise. A p-value <0.05 was considered statistically significant. Analyses were performed with Stata statistical software, release 8.0 SE (StataCorp, College Station, TX, 2003).
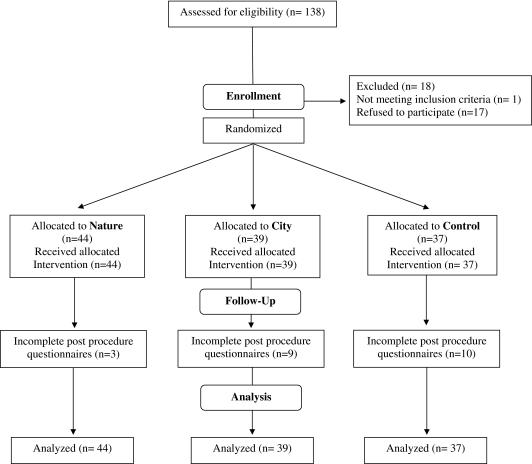
FIG. 2.
Patient flow. Eighty-seven percent (87%) of patients screened were randomly assigned to one of the three study arms.
Results
The majority (87%) of patients screened were enrolled in the study (Fig. 3). Forty-four (44) entered the Nature arm, 39 City, and 37 Standard Care. Enrollment began in August 2004 and concluded in June 2005. The subjects in the different arms were similar with respect to age, race, gender, education, income, and health status. The one significant difference was that subjects in the Standard Care arm had had significantly more prior BMAB (Table 1). The range of prior BMAB was large (0–25) and most subjects had prior BMAB. In the Standard Care arm, 2 subjects (5%) had no prior BMAB, compared to 4 (9%) in the Nature arm and 3 (8%) in the City arm. The mean baseline pain levels were low (<1) and were not significantly different between the three study groups. Similarly, use of prescription analgesics at baseline did not differ between the groups (Table 1).
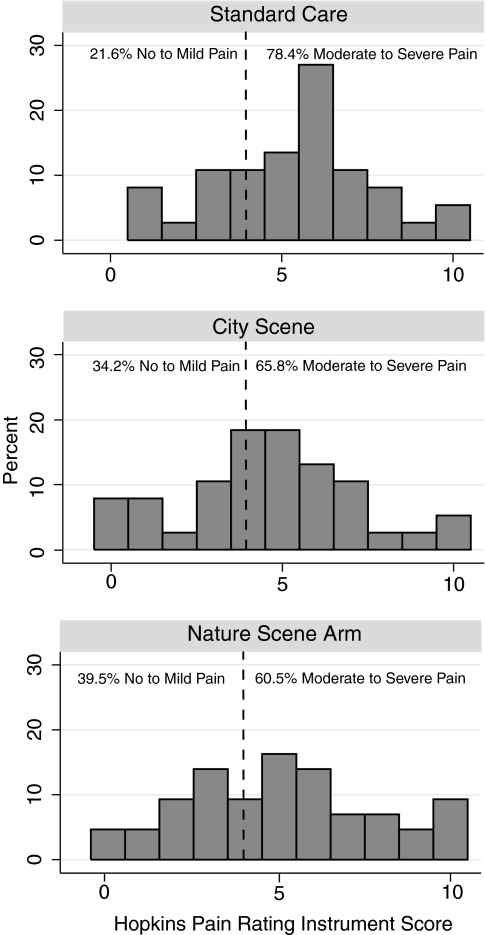
FIG. 3.
Pain ratings. Histograms of pain ratings during bone marrow biopsies showing less moderate and severe pain in the Nature arm compared to the Standard Care arm.
Table 1.
Patient Characteristics
| Nature (n = 44) | City (n = 39) | Standard care (n = 37) | p-Value, N v. SC | p-Value, C v. SC | p-Value, N v. C | |
|---|---|---|---|---|---|---|
| Gender (% male) | 24 (54.6) | 24 (61.5) | 25 (67.6) | 0.26 | 0.64 | 0.66 |
| Age (mean ± SD) | 58.1 ± 13.5 | 55.9 ± 14.7 | 55.3 ± 12.7 | 0.31 | 0.78 | 0.59 |
| Race (% white) | 36 (90.0) | 24 (82.8) | 23 (88.5) | 0.53 | 0.60 | 0.74 |
| Education (% college graduate) | 19 (70.4) | 15 (60.0) | 17 (77.3) | 0.52 | 0.52 | 0.31 |
| Annual household income (% >$75,000) | 19 (52.8) | 15 (51.7) | 16 (61.5) | 0.24 | 0.25 | 0.31 |
| General health status (% poor/fair) | 21 (53.8) | 10 (34.5) | 13 (50.0) | 0.80 | 0.24 | 0.11 |
| Use of pain meds | 7 (15.9) | 4 (10.3) | 6 (16.2) | 1.0 | 0.51 | 0.53 |
| >4 prior biopsies | 19 (43.2) | 23 (59.0) | 26 (70.3) | 0.02 | 0.64 | 0.09 |
| Upper quartile of PCS | 13 (33.3) | 5 (17.9) | 6 (23.1) | 0.82 | 0.54 | 0.21 |
Poor/fair health is self-reported health status, use of pain meds indicates use of analgesics prior to the procedure, PCS is the Pain Catastrophizing Index—higher scores indicate greater likelihood to have a negative response to a noxious stimulus. N v. SC is comparing Nature to Standard Care, C v. SC is City compared to Standard Care, and N v. C is comparison of Nature to City.
SD, standard deviation.
The procedure characteristics were very similar between the three study groups with respect to indications, duration, and lidocaine dosing. All subjects underwent bone marrow aspiration and approximately 15% also underwent biopsy. The rate of biopsy did not differ significantly between the study groups. The differences in lidocaine dose (Table 2) and procedure duration between study groups were not statistically significant and did not change after taking into account whether subjects had both bone marrow biopsy and aspirate performed or only an aspirate. Subjects in the Nature and City arms were allowed to view the murals and listen to the sounds as much or as little as they wanted. Sixty-eight percent (68%) of subjects used the interventions more than 50% of the time. Use of the interventions did not differ between the Nature and City groups. The one process of care factor that was significantly different between the groups was the operator who performed the procedures (Table 3). There were 10 different people who performed bone marrow aspirates and biopsies during the study, but 5 operators accounted for over 85% of all procedures. Operator 1 performed 42 or 35% of the procedures and 4 others performed a total of 62 procedures or 51.7% of the total. The pain ratings during the procedure also differed significantly between the operators. Patients of operator 4 generally reported less pain, and patients of operators 2 and 3 generally had more pain.
Table 2.
Procedure Characteristics
| Nature | City | Standard | p-Value, N v. SC | p-Value, C v. SC | p-Value, N v. C | |
|---|---|---|---|---|---|---|
| Duration (min) | 9.5 ± 5.5 | 9.9 ± 5.2 | 10.7 ± 4.7 | 0.09 | 0.34 | 0.31 |
| Lidocaine (mg) | 138.0 ± 76.6 | 171.3 ± 120.3 | 156.8 ± 69.8 | 0.17 | 0.89 | 0.30 |
| Family present | 29 (65.9) | 28 (71.8) | 24 (64.9) | 1.0 | 0.62 | 0.56 |
| Bx & aspirate | 35 (79.5) | 33 (86.8) | 34 (91.9) | 0.21 | 0.71 | 0.56 |
N v. SC is comparing Nature to Standard Care, C v. SC is City compared to Standard Care, N v. C is comparison of Nature to City.
Bx, biopsy.
Table 3.
Distribution of Procedures and Pain Ratings of the Five Busiest Operators
| Operator | Nature | City | Standard | HPRI ≥4 (moderate/severe) | Total BMAB |
|---|---|---|---|---|---|
| 1 | 12 (29.3%) | 14 (45.2%) | 17 (51.2%) | 29 (67.4%) | 42 |
| 2 | 8 (19.5%) | 8 (25.8%) | 4 (12.1%) | 15 (75.0%) | 20 |
| 3 | 11 (26.8%) | 4 (12.9%) | 5 (15.2%) | 15 (75.0%) | 20 |
| 4 | 5 (12.2%) | 5 (16.1%) | 1 (3.0%) | 6 (54.6%) | 11 |
| 5 | 5 (12.2%) | 0 | 6 (18.2%) | 8 (72.7%) | 11 |
The percentages reported for Nature, City, and Standard represent the percentage of the total bone marrow biopsy/aspirates done in each arm (i.e., column percents). The percentages under HPRI (Hopkins Pain Rating Instrument) represent the percentage of procedures for that operator (i.e., row percents). The number of procedures done in each arm differed by operator (p = 0.05), and pain ratings differed significantly between operators (p = 0.04).
BMAB, bone marrow aspiration and biopsy.
Overall, BMAB resulted in moderate to severe pain. The average pain rating during the procedure was 4.8 ± 2.5 on a scale of 0–10, with 0 being no pain and 10 being the “worst pain imaginable.” The mean pain score was 4.86 ± 2.8 for the Nature Scene arm, 4.45 ± 2.5 for the City Scene arm, and 5.14 ± 2.3 for the Standard Care arm. These values were not statistically significantly different. Twenty-seven percent (27%) of subjects reported poor to fair satisfaction with pain control. Seventeen or 39.5% of subjects in the Nature arm reported no pain to mild pain (HPRI <4), compared to 13 (34.2%) in the City arm and 8 (21.6%) in the Standard Care arm (Fig. 3). In bivariable analyses, these differences were not statistically significantly different, (p = 0.097 comparing Nature to Standard Care). Notably, prior experience with BMAB was not associated with pain ratings. After stratifying for the different operators, subjects assigned to the Standard arm had worse pain ratings than the nature scene arm. The mean pain score in subjects treated by the 2 operators with the best ratings were 3.9 ± 2.2 in the Nature arm versus 5.7 ± 2.4 in the Standard Care arm, p = 0.046. The mean pain ratings did not differ significantly between Nature and City or City and Standard Care even after stratifying by operators. Using logistic regression analysis to adjust for different operators also revealed significantly higher odds of moderate to severe pain in the Standard Care subjects than subjects in the Nature Care arm (odds ratio [OR] = 3.71 [95% confidence interval (CI) 1.2–11.4] p = 0.02). This difference remained significant after adjusting for procedure duration, patient age, gender, and use of pain medications. Odds of moderate to severe pain were not significantly different between the Standard Care arm and the City arm (OR = 2.6 [95% CI 0.8–8.5] p = 0.11).
Negative mood states including anxiety did not differ significantly between the treatment groups (Table 4), nor did cortisol levels, blood pressure, heart rate, or respiratory rates. Patients in the Nature arm had a trend toward higher satisfaction with their procedures, as indicated by the willingness to refer others to this institution for the same procedure. Ninety percent (90%) of subjects in the Nature arm reported they would definitely refer a friend or family member to this institution for the same procedure, compared to 79% of the City arm and 73% of the Standard Care group. These differences were not statistically significant (p = 0.09).
Table 4.
Physiologic and Behavioral Outcomes
| Measure | Nature | City | Standard Care | p-Value, N v. SC | p-Value, C v. SC | p-Value, N v. C |
|---|---|---|---|---|---|---|
| Δ Cortisol (μg/dL) | 0.008 ± 0.2 | 0.035 ± 0.4 | .028 ± 0.1 | 0.90 | 0.88 | 0.98 |
| Blood pressure | 92.8 ± 13.3 | 94.0 ± 11.6 | 91.5 ± 10.8 | 0.53 | 0.33 | 0.83 |
| Heart rate | 99.2 ± 5.0 | 101.0 ± 3.8 | 98.6 ± 13.1 | 0.59 | 0.29 | 0.66 |
| Respiratory rate | 22.8 ± 4.1 | 21.4 ± 4.4 | 22.8 ± 3.9 | 0.94 | 0.15 | 0.17 |
| Composed/anxious | 26.0 ± 7.7 | 27.6 ± 4.2 | 25.6 ± 7.4 | 0.75 | 0.28 | 0.33 |
| Agreeable/hostile | 29.0 ± 6.4 | 30.5 ± 4.2 | 29.3 ± 5.8 | 0.94 | 0.54 | 0.57 |
| Elated/depressed | 25.1 ± 6.2 | 26.3 ± 6.5 | 24.8 ± 8.0 | 0.88 | 0.61 | 0.45 |
Δ Cortisol is the difference between cortisol after the procedure and before the procedure (units); blood pressure is the average of the highest mean arterial pressure recorded during the procedure; heart rate is the highest heart rate recorded during the procedure; respiratory rate is the highest breathing rate per minute recorded during the procedure; composed/anxious, agreeable/hostile, and elated/depressed are subscales of the Profile of Mood States. Higher scores indicate more negative moods. N v. SC is comparing Nature to Standard Care, C v. SC is City compared to Standard Care, and N v. C is comparison of Nature to City.
There were no adverse reactions to the study interventions.
Discussion
This randomized trial demonstrated that viewing a nature scene and listening to accompanying pastoral sounds may reduce pain during bone marrow aspiration and biopsy. While the primary outcome was negative, a prespecified analysis controlling for the person who performed the procedure yielded significant results. The subjects randomized to the Nature arm were significantly more likely to report only mild pain on a visual analog scale than the group assigned to Standard Care. Pain rating in subjects assigned to view a city scene and listen to city sounds did not differ significantly from the Standard Care arm.
Prior research has shown that higher education, better health status, and lower scores on the PCS are associated with better pain tolerance.8,22 In the present study, these factors were not substantially different between groups, and did not explain differences in the treatment arms. The differences in pain rating were not explained by differences in local anesthetic dosing or use of other pain medications, as both lidocaine dose and chronic pain medication use did not differ significantly between the groups and on average were lower in the Nature arm than in the Standard Care arm. This study also compared the biophilic nature scene and sound to a nonbiophilic image and sound. The proportion of subjects in the City Scene arm reporting moderate to severe pain was slightly lower than the Control arm and slightly higher than the Nature intervention, but these differences were not statistically significant. We cannot draw any firm conclusions from these data on whether nature imagery conveys any specific benefits over other forms of distraction.
Pain ratings during BMAB in the current study were very similar to pain ratings from an earlier study at our institution,3 suggesting that the pain ratings in this study are reflective of the general population of patients undergoing bone marrow biopsy at our institution and that the study procedures did not interfere with pain reports. BMAB is a painful procedure that is not well tolerated using only local anesthetic. Several studies in pediatric populations have shown that use of intravenous sedation or general anesthesia can improve tolerance of bone marrow aspirates.23–25 However, there are many reasons why sedation and general anesthesia are not used more frequently. Sedation and anesthesia carry small risks of adverse reactions and complications.23 They require additional preparation time before the procedure and substantial recovery time afterward and they require additional specialized personnel such as nurses, nurse anesthetists, and anesthesiologists. All of these factors increase the cost of procedures and make institutions less likely to use sedation and anesthesia if they can avoid it. Furthermore, patients may want to avoid nausea, drowsiness, and other effects of sedation. Nevertheless, pain was still substantial, even in the subjects assigned to the Nature scene. Previous studies have shown sedation and analgesics to be safe and effective at reducing pain during BMAB.26 More consideration should be given to the routine use of sedation and analgesics during BMAB.
Having a low-cost, safe intervention such as Nature Sights and Sounds that can improve the patient experience during BMAB is valuable. Complementary interventions have been studied for other invasive, painful procedures. However, many of the interventions that have been evaluated are either costly or require specialized training to implement. For example, virtual reality has been investigated for burn patients,27 and structured attention and hypnosis have been evaluated in patients undergoing interventional radiology procedures.12 Virtual reality requires specialized equipment and training for patients, and hypnosis requires specialized personnel. The Nature Sights and Sounds intervention is extremely portable, compact, and does not require training to use.
Following our previous study of a nature intervention for bronchoscopy, we had several unresolved questions. Nature Sights and Sounds were only compared to usual care and not another active intervention. In the present study, pain ratings were not significantly different between the Nature arm and the City arm. However, the City intervention was created specifically for this study and has not been tested in other settings. It is possible that the Nature Sights and Sounds intervention may simply be a better-designed distraction tool. Our primary outcome measure yielded negative results. This study was powered to detect a 2-point change on a 10-point visual analog scale. This is a large effect to anticipate and may have been overly ambitious. Repeating this study on a larger scale would allow the detection of a smaller treatment effect.
This study had several limitations. We chose to evaluate patients undergoing bone marrow biopsy and aspiration because this is a frequently performed, painful procedure and sedation is not frequently used. However, since patients are positioned on their abdomens, their ability to view the interventions may have been limited. Additionally, we quantified subjects' use of the intervention and found that 32% used the interventions for less than 50% of the procedure. Both of these factors may have reduced our ability to detect an effect from the intervention. Possible approaches to overcoming these obstacles would be to use glasses or goggles that display images and sounds. However, this type of approach becomes more costly. This study was not blinded. While subjects in the Standard Care arm were not explicitly told what other interventions were being used, they may have felt slighted since they did not receive anything beyond standard care. This could have biased the results in favor of the two intervention arms. One solution would be to develop an appropriate “placebo” intervention for future studies. However, this will require fairly extensive validation studies to find a scene and sound intervention that clearly has no effect on pain or satisfaction. Lastly, we wanted to assess differences between the Nature arm and the City arm. We powered the study to detect a 2-point difference on the pain scale. This was an overly optimistic effect size, especially between two active interventions, and therefore the study was too small to adequately compare the Nature arm and City arm.
Bone marrow biopsy and aspirate is a painful procedure when only local anesthetic is used, and some patients with hematologic malignancies need to have many repeated procedures. We have completed a randomized, controlled clinical trial of an inexpensive, safe, easy-to-use intervention, namely, Nature Sights and Sounds. We found that after adjusting for differences in the operator performing the procedure, the risk of moderate to severe pain during bone marrow aspiration and biopsy was lower in subjects assigned to the Nature Sights and Sounds arm. Consideration should be given to more routine use of similar complementary interventions during invasive procedures.
Acknowledgments
This study was generously funded through a research grant from the Johns Hopkins Center for Complementary and Alternative Medicine and was supported in part by Grant Number AT00437 from the National Center for Complementary and Alternative Medicine (NCCAM). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NCCAM. The authors thank Dr. Steven Piantadosi for his expert statistical advice, Dr. Christian Merlo for his photographic skills, and Yosaif August for his commitment to biophilia.
The Clinical Trials Registration Number for this study is NCT00315796.
Disclosure Statement
The research described in this manuscript is the original work of the authors and has not been presented or published elsewhere. None of the authors have any conflicts of interest with material related to this study or manuscript. Specifically, none of the investigators have a financial relationship with any business related to this research and there was no commercial funding or support for this study.
References
- 1.Portenoy RK. Lesage P. Management of cancer pain. Lancet. 1999;353:1695–1700. doi: 10.1016/S0140-6736(99)01310-0. [DOI] [PubMed] [Google Scholar]
- 2.Foley KM. Advances in cancer pain. Arch Neurol. 1999;56:413–417. doi: 10.1001/archneur.56.4.413. [DOI] [PubMed] [Google Scholar]
- 3.Portnow J. Lim C. Grossman SA. Assessment of pain caused by invasive procedures in cancer patients. J Natl Compr Canc Netw. 2003;1:435–439. doi: 10.6004/jnccn.2003.0037. [DOI] [PubMed] [Google Scholar]
- 4.Yaster M. Pain relief. Pediatrics. 1995;95:427–428. [PubMed] [Google Scholar]
- 5.Colt HG. Morris JF. Fiberoptic bronchoscopy without premedication: A retrospective study. Chest. 1990;98:1327–1330. doi: 10.1378/chest.98.6.1327. [DOI] [PubMed] [Google Scholar]
- 6.Schechter NL. Weisman SJ. Rosenblum M, et al. The use of oral transmucosal fentanyl citrate for painful procedures in children. Pediatrics. 1995;95:335–339. [PubMed] [Google Scholar]
- 7.American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;96:1004–1017. doi: 10.1097/00000542-200204000-00031. [DOI] [PubMed] [Google Scholar]
- 8.Lechtzin N. Rubin HR. Jenckes M, et al. Predictors of pain control in patients undergoing flexible bronchoscopy. Am J Respir Crit Care Med. 2000;162(2 pt 1):440–445. doi: 10.1164/ajrccm.162.2.9910022. [DOI] [PubMed] [Google Scholar]
- 9.Milligan DW. Howard MR. Judd A. Premedication with lorazepam before bone marrow biopsy. J Clin Pathol. 1987;40:696–698. doi: 10.1136/jcp.40.6.696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wolanskyj AP. Schroeder G. Wilson PR, et al. A randomized, placebo-controlled study of outpatient premedication for bone marrow biopsy in adults with lymphoma. Clin Lymphoma. 2000;1:154–157. doi: 10.3816/clm.2000.n.014. [DOI] [PubMed] [Google Scholar]
- 11.Tusek DL. Church JM. Strong SA, et al. Guided imagery: A significant advance in the care of patients undergoing elective colorectal surgery. Dis Colon Rectum. 1997;40:172–178. doi: 10.1007/BF02054983. [DOI] [PubMed] [Google Scholar]
- 12.Lang EV. Benotsch EG. Fick LJ, et al. Adjunctive non-pharmacological analgesia for invasive medical procedures: A randomised trial. Lancet. 2000;355:1486–1490. doi: 10.1016/S0140-6736(00)02162-0. [DOI] [PubMed] [Google Scholar]
- 13.Kellert S, editor; Wilson E, editor. The Biophilia Hypothesis. Washington: Island Press/Shearwater Books; 1993. [Google Scholar]
- 14.Ulrich RS. View through a window may influence recovery from surgery. Science. 1984;224:420–421. doi: 10.1126/science.6143402. [DOI] [PubMed] [Google Scholar]
- 15.Miller AC. Hickman LC. Lemasters GK. A distraction technique for control of burn pain. J Burn Care Rehabil. 1992;3:576–580. doi: 10.1097/00004630-199209000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Rusy LM. Weisman SJ. Complementary therapies for acute pediatric pain management. Pediatr Clin North Am. 2000;47:589–599. doi: 10.1016/s0031-3955(05)70227-3. [DOI] [PubMed] [Google Scholar]
- 17.Diette GB. Lechtzin N. Haponik E, et al. Distraction therapy with nature sights and sounds reduces pain during flexible bronchoscopy: A complementary approach to routine analgesia. Chest. 2003;123:941–948. doi: 10.1378/chest.123.3.941. [DOI] [PubMed] [Google Scholar]
- 18.Grossman SA. Sheidler VR. McGuire DB, et al. A comparison of the Hopkins Pain Rating Instrument with standard visual analogue and verbal descriptor scales in patients with cancer pain. J Pain Symptom Manage. 1992;7:196–203. doi: 10.1016/0885-3924(92)90075-s. [DOI] [PubMed] [Google Scholar]
- 19.Zabora J. BrintzenhofeSzoc K. Jacobsen P, et al. A new psychosocial screening instrument for use with cancer patients. Psychosomatics. 2001;42:241–246. doi: 10.1176/appi.psy.42.3.241. [DOI] [PubMed] [Google Scholar]
- 20.Baker F. Denniston M. Zabora J, et al. A POMS short form for cancer patients: Psychometric and structural evaluation. Psychooncology. 2002;11:273–281. doi: 10.1002/pon.564. [DOI] [PubMed] [Google Scholar]
- 21.Raff H. Raff JL. Findling JW. Late-night salivary cortisol as a screening test for Cushing's syndrome. J Clin Endocrinol Metab. 1998;83:2681–2686. doi: 10.1210/jcem.83.8.4936. [DOI] [PubMed] [Google Scholar]
- 22.Sullivan M. Bishop S. Pivik J. The Pain Catastrophizing Scale: Development and validation. Psychol Assess. 1995;7:524–532. [Google Scholar]
- 23.Iannalfi A. Bernini G. Caprilli S, et al. Painful procedures in children with cancer: Comparison of moderate sedation and general anesthesia for lumbar puncture and bone marrow aspiration. Pediatr Blood Cancer. 2005;45:933–938. doi: 10.1002/pbc.20567. [DOI] [PubMed] [Google Scholar]
- 24.Antmen B. Sasmaz I. Birbicer H, et al. Safe and effective sedation and analgesia for bone marrow aspiration procedures in children with alfentanil, remifentanil and combinations with midazolam. Paediatr Anaesth. 2005;15:214–219. doi: 10.1111/j.1460-9592.2004.01411.x. [DOI] [PubMed] [Google Scholar]
- 25.Holdsworth MT. Raisch DW. Winter SS, et al. Pain and distress from bone marrow aspirations and lumbar punctures. Ann Pharmacother. 2003;37:17–22. doi: 10.1345/aph.1C088. [DOI] [PubMed] [Google Scholar]
- 26.Dunlop TJ. Deen C. Lind S, et al. Use of combined oral narcotic and benzodiazepine for control of pain associated with bone marrow examination. South Med J. 1999;92:477–480. doi: 10.1097/00007611-199905000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Hoffman HG. Patterson DR. Carrougher GJ. Use of virtual reality for adjunctive treatment of adult burn pain during physical therapy: A controlled study. Clin J Pain. 2000;16:244–250. doi: 10.1097/00002508-200009000-00010. [DOI] [PubMed] [Google Scholar]